Abstract
Vietnamese women experience a significant health disparity in incidence and mortality rates and screening of cervical cancer. This study is to evaluate the effectiveness of a multifaceted and culturally appropriate intervention in increasing Pap testing rates to reduce cervical cancer disparity in this high-risk population.
Methods
A total of 30 Vietnamese community organizations were randomized to either intervention or control condition. Participants (n=1,416) completed 12-month follow-up of Pap testing, their self-reported and medical record data were collected and analyzed.
Results
The findings showed a statistically significant increase in Pap testing among intervention group than control group (significance p< .0001). The self-reported Pap test screening rate is in high agreement with that of validated medical records.
Conclusion
Results indicate the screening rate was significantly higher in Vietnamese women in the intervention group compared with the control. Despite large intervention effect, there still remains a gap to reach Healthy People 2020 goal of 93% screening rate.
Keywords: Vietnamese, Pap test, cervical cancer disparity, CBPR
Despite the wide use of the Papanicolaou (Pap) test and significant decrease in cervical cancer incidence rate in recent decades, significant disparities remain in screening, incidence, and mortality rates of this disease between Asian American women and women in the general population. Screening for cervical cancer in Asian American women lags far behind screening in the general population1–4 and the screening rate in Vietnamese women of the U.S. is even lower. Our recent study indicated that the ever-Pap test rate for Vietnamese women aged 21 and above is 53%, compared with 85% for non-Hispanic White women.5 The U.S. Healthy People 2020 goal for cervical cancer screening is to increase the proportion of women who receive cervical cancer screening based on the most recent guidelines to 93%.6
In comparison with other racial and ethnic groups in the U.S., Vietnamese women experience the highest incidence rate of invasive cervical cancer.7,8 The recent U.S. Cancer Registry data indicated that the incidence rate of cervical cancer among Vietnamese American women is over twice that among non-Hispanic White women (16.8 vs. 88.1 per 100,000).7 Due to potential underreporting, the cancer incidence rates among Vietnamese women may be higher.9 The disparities in cervical cancer rate may have been attributed to the differences in screening uptake.
Vietnamese Americans constitute one of the fastest growing immigrant populations in the United States, representing the fourth largest subgroup of Asian Americans in the U.S. (11% of the Asian American population, or 1.5 million individuals), a 39.6% increase from 2000.10,11 Compared with other Asian American subgroups and the general U.S. population, Vietnamese Americans are more likely to have limited English proficiency, high levels of poverty, lower rates of health insurance coverage, and lower levels of knowledge about general health and the American health care system.12–14 The factors contributing to poor screening are complex, including lack of knowledge and misinformation about cervical cancer; psychosocial beliefs about cervical cancer and perceived barriers to screening; and structural barriers to health care access.15,16 Therefore, it should be a significant public health priority to test and implement innovative strategies to address these multilevel barriers to increase cervical screening and early detection for the underserved Vietnamese American women.
Reaching this population requires a community-based approach because of significant sociocultural and language barriers. Community-based participatory research (CBPR) is a process where communities are engaged to be participants in all phases of research. 17,18 This includes working with representatives from community-based organizations and community members to create advisory groups that prioritizing health concerns, monitor steps to collect focus group and needs assessment data, review findings and assist disseminating study results to the community. Community-based organizations (CBOs) who work directly with the target population often become partners that facilitate the collection of needs assessment data and promote information about the study to potential research participants. Vietnamese community organizations (VCOs) represent an important resource to increase cancer screening among Vietnamese women. The multifaceted intervention reported on here included community health educator19 (CHE)-led group education with culturally relevant visual aids, patient navigation, client-physician communication via videotape, referral to Pap-test sites, and six-month screening reminders.
We conducted one of the first largest randomized community-based intervention trials, aimed to increase cervical cancer screening and reduce multilevel barriers among medically underserved and low-income Vietnamese women. This randomized controlled trial (RCT) is a five-year study conducted at 30 Vietnamese CBOs in the Eastern region of the U.S. The intervention trial, guided by a conceptual framework derived from Health Belief Model (HBM) and Social Cognitive Theory (SCT), addresses both individual choices and health care system barriers through multifaceted innovative program elements. In this article, we will report primary outcome findings from our randomized controlled trial that evaluated the effectiveness of a multifaceted and culturally appropriate intervention in increasing cervical cancer screening among Vietnamese women.
Methods
Setting and community-based intervention
The Center for Asian Health (Center) has an enduring collaborative relationship with over 285 Asian American organizations represented by the Asian Community Health Coalition (ACHC). The VCOs included in this study as part of the Coalition serve important social functions, and they represent the ideal milieu for obtaining information on accessibility to needed health services. Their unique status in these communities underscores their importance as an ideal avenue for recruiting community-based participants for the study and intervention delivery.
About 42 Vietnamese community leaders were directly involved in the planning, development, and implementation of the project. Specifically, VCOs were invited to send at least one representative to be part of a planning and advisory group. At the initial meeting, VCO representatives discussed health issues for Vietnamese, specifically the need to address cancer screening for women. The group suggested that focus groups be conducted: 1) to identify barriers to cancer screening; 2) to review messages that may motivate Vietnamese women to obtain screening; and 3) to discuss how to revise a health intervention workshop effectively to include cultural images and themes that would be appealing to Vietnamese women. In the next meeting of the planning and advisory group, Center staff presented the intervention and the group suggested further modifications as well as recommendations for recruitment and retention.
The intervention was based on a conceptual framework guided by the Health Belief Model (HBM) and Social Cognitive Theory (SCT).20,21,22 It addresses both individual choices and health care system barriers through multifaceted innovative program elements. Participants in the control group were given information for general health issues including a mention of a routine health exam such as an annual general health exam. Materials available from federal agencies and community-based organizations were translated into Vietnamese but the information covered general health and did not specifically mention a Pap test. All control group participants were offered the opportunity to receive the full intervention components upon the completion of control group protocols.
Intervention group participants met in small groups and went over information about the female body such as cervical cancer, risks of cervical cancer nationally and in the Vietnamese population, and procedures for Pap testing. Visual aids included pictures of Vietnamese women and doctors and were available in English and Vietnamese. The intervention group participants received group education by professionally-trained community health educators (CHEs); use of supplemental visual aids, and multimedia cervical cancer education materials in Vietnamese language; client-physician communication via videotaping; patient navigation (e.g., language, appointment scheduling and transportation assistance); referral to Pap-test sites; and six-month screening reminders. At the time of the study, cervical cancer guidelines suggested annual exams (which were a focus of each intervention session).
Study design and randomization
We examined the outcomes of 1) Pap-test cervical cancer screening rate, 2) knowledge and beliefs (perceived risks and susceptibility, perceived benefits, and self-efficacy), and 3) perceived health care barriers to adherence to cervical cancer screening (this article only focused on the primary outcome of increase in cervical cancer screening (receipt of Pap test during the past 12 months).
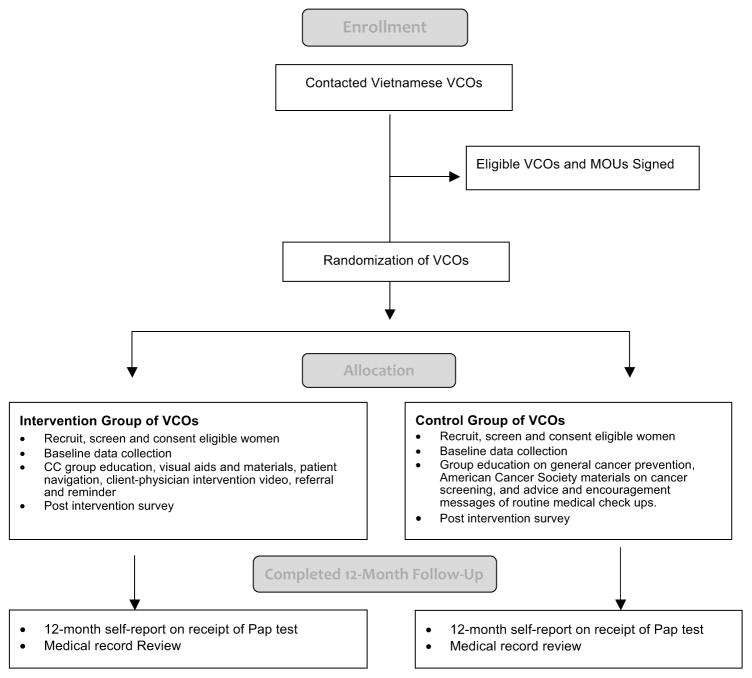
This study is a two-arm group randomized trial with community organizations as the unit of randomization. A total of 36 VCOs were recruited and 30 VCOs consented and enrolled in the study. Vietnamese community organizations (N=30) were randomized to either intervention or control condition (Figure 1). A random sample of eligible participants were selected from each VCO. Assessment data were collected at baseline, post-intervention, and 12-month. Validation of medical record for self-report screening was conducted at the point of 12th month post-randomization. The study was approved by Temple University Institutional Review Board approval.
Figure 1.
Study design.
Study participants
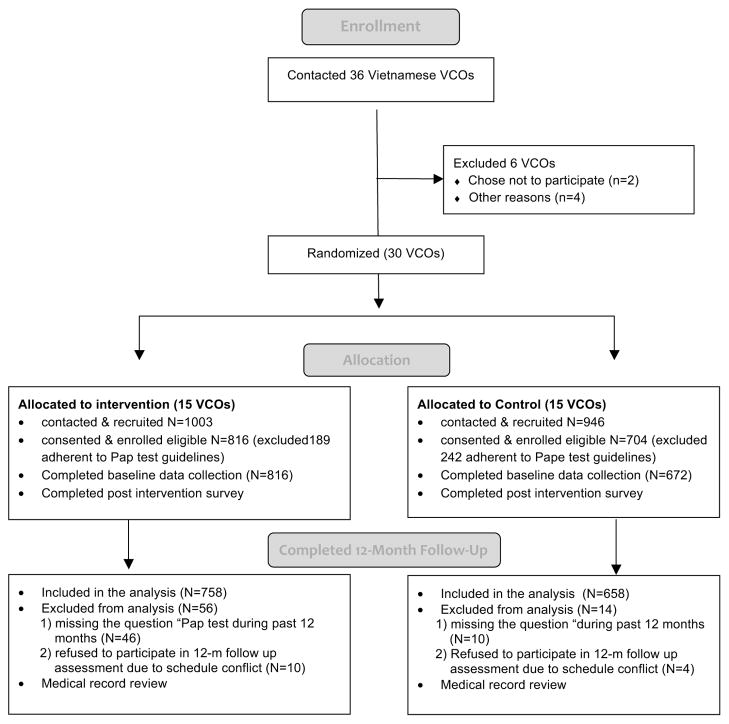
The VCOs varied in size, with the number of female Vietnamese members in each of these 30 organizations ranging from 80 to 2,500 women. Vietnamese women (n=1,949) were recruited from participating Vietnamese community organizations (n=30 VCOs). Specifically, 1,003 Vietnamese women were recruited from 15 VCOs of intervention condition and 946 were recruited from 15 VCOs of control condition. Among all recruited Vietnamese women who were assessed for study eligibility, 1,518 met the inclusion criteria of self-identified Vietnamese identity; women age 21 to 70; had not been adherent to Pap test guidelines; and had not been diagnosed with cervical cancer. The average age of study participants was 52 years and ranged from 20 years to 70 years. Of the total 1,518 eligible women, 1,488 consented and completed the baseline survey, including 816 women for intervention group and 672 women for control group. The baseline assessment response rate is 98% (Figure 2).
Figure 2.
Study flow diagram.
Among the total participants (N=1,488) who completed the baseline assessment, 1,416 participants completed 12-month follow-up assessment were included in the data analysis for this article (intervention group n=758 and control group n = 658). About 72 participants were excluded from the data analysis for two major reasons: 1) missed the question of having had Pap test during the past 12 months (n=56), and 2) refused to complete the 12-month assessment due to schedule conflicts (n=14). The study response rate is 95% among participants who completed baseline, intervention and 12-month follow-up (Figure 2).
Measures and data collection
The primary outcome in this study was whether or not a participant completed a Pap test by self-reporting and review of medical record at 12-month follow up. The measures collected at baseline assessment include: (1) demographic characteristics and acculturation; (2) health care access; (3) health behavior and Pap test; (4) perceptions related to Health Belief Model constructs; (5) knowledge, attitudes, and beliefs of Vietnamese women about cervical cancer; and (6) human papillomavirus (HPV) related questions. Our research team investigators hypothesized that the factors mentioned above would affect cervical cancer screening behaviors by serving either as barriers or facilitators to health-seeking behavior change. This paper primarily examines the association of demographic and acculturation characteristics (measured using eight items as in Table 1), health care access barriers (six items, including having a regular doctor, having health insurance, having or able to get transportation to the health clinic for check-ups), and knowledge, attitudes and beliefs about cervical cancer screening (13 items, including I am scared to have a Pap test because I might learn that I have cancer) and HPV-specific knowledge (10 items, including link between HPV and cancer) with ever having had a Pap test. These measures were validated in a number of our previous studies.23–27 The findings of HBM constructs and other variables’ association with cervical cancer screening behaviors are reported separately.28
Table 1.
BASELINE COMPARISON ON DEMOGRAPHIC FACTORS BETWEEN TWO GROUPS
| Demographic factors | Control group
|
Intervention group
|
Difference between groupsa | ||
|---|---|---|---|---|---|
| Number | percent | Number | Percent | ||
| Age ranges | 612 | 753 | |||
| <=40 | 143 | 23.37 | 194 | 25.76 | |
| 41~50 | 134 | 21.90 | 158 | 20.98 | |
| 51~60 | 169 | 27.61 | 188 | 24.97 | |
| >60 | 166 | 27.12 | 213 | 28.29 | |
| School levels | 600 | 717 | *** | ||
| Below high school | 240 | 40.00 | 202 | 28.17 | |
| High school | 317 | 52.83 | 469 | 65.41 | |
| High education | 43 | 7.17 | 46 | 6.42 | |
| Employment status | 613 | 753 | |||
| Employed | 369 | 60.20 | 470 | 62.42 | |
| Home maker | 153 | 24.96 | 169 | 22.44 | |
| Retired | 38 | 6.20 | 34 | 4.52 | |
| unemployed | 53 | 8.65 | 80 | 10.60 | |
| English speaking ability | 615 | 755 | |||
| Not at all | 245 | 39.84 | 285 | 37.75 | |
| Not well | 325 | 52.85 | 426 | 56.42 | |
| Well | 45 | 7.32 | 44 | 5.83 | |
| Marriage status | 613 | 751 | |||
| Married | 452 | 73.74 | 564 | 75.43 | |
| Devoiced/separated | 26 | 4.24 | 36 | 5.19 | |
| Never married | 86 | 14.03 | 100 | 12.72 | |
| Widowed | 49 | 7.99 | 51 | 6.67 | |
| Born in USA | 611 | 751 | ** | ||
| No | 550 | 90.02 | 747 | 99.47 | |
| Yes | 61 | 9.98 | 4 | 0.53 | |
| Living years in USA | 624 | 758 | * | ||
| <=10 | 243 | 38.94 | 255 | 33.64 | |
| 11~20 | 339 | 54.33 | 455 | 60.03 | |
| >20 | 42 | 6.73 | 48 | 6.33 | |
| English reading ability | 610 | 756 | |||
| Not at all | 333 | 54.59 | 436 | 57.67 | |
| Not well | 246 | 40.33 | 282 | 37.30 | |
| Well | 31 | 5.08 | 38 | 5.03 | |
| PAP test | 604 | 715 | |||
| No | 278 | 46.03 | 303 | 42.38 | |
| Yes | 326 | 53.97 | 412 | 57.62 | |
The test was done by either χ2 or fisher’s exact test.
<.001
<.01
<.05
For the post-intervention survey, we collected all measures of baseline survey except demographic characteristics and acculturation. For the 12-month follow-up assessment, bilingual interviewers contacted participants for telephone interviews. Outcome measures were assessed. In addition, women’s self-reported adherence to cervical cancer screening was recorded. Specifically, women were asked whether they obtained a Pap-test during the past 12 months. The assessment took about 10 minutes. A measure of intention to undergo cervical cancer screening was obtained at 12-month follow-up only for those participants who reported non-receipt of screening. This allowed us to have a better understanding of these participants’ decision-making status.
For the review of medical record to validate self-report screening, study participants who reported their receipts of Pap test were asked to sign the medical release consent form to grant project staff permission to contact their health providers to validate their self-reported testing with written confirmation, as well as provide information about the date and location of their tests.
Process evaluation was conducted at different points post-intervention to document the study process and quality. Specifically, the process evaluation included a short survey assessing participant acceptability and satisfaction with the intervention, quality control, and treatment fidelity using a standardized observation form to ensure that all components of the intervention were delivered, assessment of intervention exposure (e.g., attendance), and tracking intervention costs in consideration of program transportability in the future.
For data collection procedures, prior to project implementation, community leaders and volunteers participated in training sessions focused on re-visitation of project aims and significance to Vietnamese women, recruitment strategies, and guidelines for administration of research instrument as well as data collection, accuracy and confidentiality. All measures in English were translated, back-translated, and pre-tested in Vietnamese to ensure the scientific and cultural appropriateness of the instrument for community Vietnamese participants. The 20–30 minute in-person baseline and post-intervention surveys were provided in Vietnamese or English versions, and bilingual assistance was available at all sites.
Data analysis
The primary outcome of this study is the proportion of baseline Pap-test noncompliant women who had a Pap test during the 12 months after the end of intervention. Secondary outcomes are: ever had a Pap test at the baseline survey, plan to have a Pap test within 12 months following the assessments at the baseline, post-prevention, and 12-month follow up.
Chi-square tests were used to compare between intervention and control groups for the proportion of ever-had Pap test, and demographic factors that are known to be significantly associated with Pap test.5,24
To acknowledge the fact that the randomization was conducted at community site level in a matched pair design, the community site was used as the unit of analysis. The p-value for testing null hypothesis of no intervention effect (i.e., the limiting case, where intervention and control groups have the same proportion of women having a Pap test during the 12 months after the end of intervention) is calculated by permuting the sign of difference between two proportions for each pair. Permutation tests calculate the set of possible outcomes for randomly generated distributions. The value of the permutation test is that the distribution of the outcome does not need to be known as in most statistical tests that use standardized distributions (such as z-scores or Poisson distributions). Here the binomially distributed outcome (having a Pap test or not) is generated for all possible combinations of the sites.29 The average difference over 15 pairs is calculated for each of the 215 = 32,768 permutations. The p-value is the proportion of the permutations that had the absolute value of the average difference equal to or larger than the observed average from the observed data. In addition, secondary outcomes were also examined by permutation tests using community as the unit of analysis for baseline compatibility between intervention group and control group in the proportion of women who ever had a Pap test and their plan for having a Pap test at the baseline survey. They were also examined in the proportion of women who planned for a Pap test at the end-of-intervention survey and at the end-of-12-month follow-up survey.
In order to adjust the impact of the significant demographic factors on the primary study outcomes, the GLIMMIX model in SAS 9.2 was used to build a logistic model in which the community center and matched pair were treated as random effects.30 Intervention effect and six demographic variables identified at the baseline data analysis to be significantly associated with Pap testing were treated as independent effects. With this model, the covariate adjusted Pap test rates and odds ratio were estimated.
Though only 72 out of 1,488 (4.8%) randomized women did not report the primary outcome of Pap test receipt in the 12-month follow-up assessment, the same permutation test was performed to compare the statistical significance between intervention and control groups in their dropout rates. All the statistical tests and summary data described above were computed using SAS 9.4,31 except the permutation test, which was calculated in R.32
Results
The study flow of participants diagram (Figure 2) indicated the number of VCOs re cruited, assessed for eligibility, enrolled and randomized, as well as the number of Vietnamese women recruited, assessed for eligibility, consented, enrolled, assessed for the primary and secondary outcomes at the baseline, post-intervention and 12-month follow-ups. In addition, it presented the reasons for not being included in the data analysis.
The baseline demographic characteristics of intervention and control groups are shown in Table 1. Nearly all participants of both intervention and control groups are age 40 and older. A majority of participants only received high school education or less (93%) and more than half of the study participants were employed (61%). Most did not speak English well or at all and were foreign-born immigrants. A majority of the participants were married (74%) and had lived in the U.S. between 10 and 20 years (93%).
With regard to the baseline comparability, there were no significant differences between the intervention and control groups in distributions for age ranges, employment status, English speaking ability, marriage status, or English reading ability. However, there were significant differences in education (p<.001), having been born in the U.S. (p<.001), and years living in U.S. (p<.05). Most importantly, the two arms did not have significant differences in the baseline outcome of ever having had a Pap test (Table 1).
Intervention effect of Pap test rates at study completion is displayed in Table 2. The average rate of Pap test within the 12-month follow-up period was 1.6% in the control group and 60.1% in the intervention group. The difference between two groups was 58.5% (95% CI: 44.7–72.3%) with a two-sided p-value = .00012. The covariate adjusted Pap test rate difference from a GLIMMIX model was 64%, similar to the unadjusted raw rate difference. The covariate adjusted odd ratio is 191 (95% CI: 171–212), p-value < .0001.
Table 2.
PAP TEST RATE AT 12-MONTH POST INTERVENTION IN BASELINE SCREENING NON-COMPLIANT WOMEN
| Pair | Control (n=658)
|
Intervention(n=758)
|
|||||
|---|---|---|---|---|---|---|---|
| Community
|
Test rate (%) | community | No. | Test rate (%) | Rate difference (%) | ||
| ID | Sample size | ||||||
| 1 | 1 | 74 | 0.0 | 7 | 51 | 66.7 | 66.67 |
| 2 | 5 | 36 | 0.0 | 2 | 81 | 80.3 | 80.25 |
| 3 | 10 | 19 | 0.0 | 23 | 54 | 81.5 | 81.48 |
| 4 | 11 | 33 | 12.1 | 27 | 33 | 9.1 | −3.03 |
| 5 | 13 | 44 | 0.0 | 15 | 58 | 55.2 | 55.17 |
| 6 | 14 | 70 | 0.0 | 18 | 50 | 46.0 | 46.00 |
| 7 | 16 | 37 | 2.7 | 3 | 41 | 73.2 | 70.47 |
| 8 | 17 | 82 | 0.0 | 28 | 31 | 41.9 | 41.94 |
| 9 | 20 | 38 | 0.0 | 29 | 44 | 25.0 | 25.00 |
| 10 | 21 | 34 | 0.0 | 19 | 47 | 38.3 | 38.30 |
| 11 | 22 | 42 | 0.0 | 9 | 60 | 65.0 | 65.00 |
| 12 | 24 | 44 | 6.8 | 25 | 46 | 89.1 | 82.31 |
| 13 | 26 | 29 | 0.0 | 12 | 40 | 65.0 | 65.00 |
| 14 | 31 | 38 | 0.0 | 6 | 62 | 82.3 | 82.26 |
| 15 | 33 | 38 | 2.6 | 32 | 60 | 83.3 | 80.70 |
| Average | 44 | 1.6 | 51 | 60.1 | 58.5 | ||
| Overalla | 658 | 1.4 | 758 | 63.3 | 61.9 | ||
| P_permb | 00.00012 | ||||||
| 95% CI | 44.71~72.29 | ||||||
| Estimated ratec | 1.0 | 65 | 64 | ||||
| Odds ratio (95% CI) | 191(171, 212) p < .0001 | ||||||
the overall values was calculated from all individual subject data pooled together within the intervention or control group.
P_perm is the p value based on permutation test.
the covariate adjusted test rate was estimated from mixed effect logistic regression using SAS GLIMMIX adjusted for demographic covariates (age, education, marriage status, employment status, country of birth, and English speaking ability).
There were no significant differences between the two arms in baseline Pap test rate (i.e., ever having had a Pap test) (p-value=.87) or plan to have a Pap test (p-value=.53). There were significant differences between the two arms in planning to have a Pap test within 12 months at the post-intervention assessment (p=.0017) and at the 12-month follow-up (p=.001), with significantly more women in intervention group planning to take a Pap test (Table 3).
Table 3.
BASELINE COMPATIBILITY IN PAP TEST RATE AND PLAN TO HAVE PAP TEST. INTERVENTION EFFECT IN PLAN TO HAVE PAP TEST AT POST INTERVENTION AND AT 12 MONTH AFTER INTERVENTION BETWEEN INTERVENTION (I) AND CONTROL (C) GROUPS
| pair | Rate differences between two groups (I–C)
|
|||
|---|---|---|---|---|
| Ever having test | Baseline plan | Post plan | Follow up plan | |
| 1 | −24.08 | −11.69 | 12.99 | 60.78 |
| 2 | −12.94 | −71.91 | −3.24 | 100.00 |
| 3 | 81.13 | 100.00 | 98.15 | 72.22 |
| 4 | −13.23 | 2.04 | 100.00 | −38.26 |
| 5 | 19.66 | 10.75 | 6.59 | 100.00 |
| 6 | −17.69 | 7.95 | 1.49 | 38.00 |
| 7 | −64.86 | −70.27 | 17.73 | 14.37 |
| 8 | −46.70 | −93.65 | 17.95 | 25.81 |
| 9 | −54.28 | −100.00 | −2.08 | 22.73 |
| 10 | −24.71 | −56.67 | 37.50 | 10.64 |
| 11 | 1.74 | 1.99 | 3.84 | 35.00 |
| 12 | 32.50 | 6.90 | 24.39 | 93.18 |
| 13 | 70.73 | 56.10 | 97.56 | 12.50 |
| 14 | 25.89 | 70.37 | 88.71 | 45.16 |
| 15 | −1.25 | −1.87 | −5.00 | 97.37 |
| average | −1.87 | −10.00 | 33.11 | 45.97 |
| P_perma | 0.87 | 0.53 | 0.0017 | 0.0010 |
| 95%CI | −25.19–21.45 | −42.78–22.78 | 10.42–55.79 | 23.42~68.52 |
P_perm is the p value when using permutation test.
The dropout rates between the intervention and control groups were not significantly different (8% in intervention versus 2% in control, p=.07).
For medical record validation of Pap test, 456 of 758 (60.1%) participants in the intervention group self-reported the receipt of Pap test during the past 12 months. Participants were asked to provide information about if, where and when they had obtained Pap test. The question about past 12-month Pap test behavior included a description of the procedures to ensure the participants’ comprehension. Identified health care facilities were then contacted for verifying this information. We were able to request and verify 92.10% (n=420) of 456 Vietnamese women who reported obtaining a Pap test. Three hundred and ninety-five (94.0%) of these 420 women’s medical records matched the accuracy of self-report screening. Among all women (n=456) with self-reported Pap testing, 395 (86.6%) were verified by medical records.
Discussion
Cervical cancer is one of the most preventable cancers among women in the U.S.; it is also highly responsive to treatment if detected early. The occurrence of deaths from cervical cancer has declined significantly over the last 20 to 30 years.33–35 Significant disparities in incidence and mortality remain, between ethnic minority women and White women,36 particularly Vietnamese women, who present with cervical cancer much later and have the highest cervical cancer mortality rates of all ethnic groups.37 In this randomized controlled trial, we tested the efficacy of a multifaceted community-based participatory intervention with CHE-led group education, patient navigation, bilingual CBOs and physician engagement to increase cervical cancer screening (Pap test) and reduce health access barriers for underserved, high-risk, and hard-to-reach Vietnamese women recruited from 30 Vietnamese community-based organizations in the eastern region of the United States.
The study results indicate a large intervention effect significantly increasing Pap test screening in Vietnamese women in the intervention group in comparison with the control group, who were non-adherent to cervical cancer screening guidelines. The self-reported Pap test screening rate is in high agreement with that of validated medical records. The intervention effect achieved high statistical significance (p<.0001). This study showed larger intervention effect than other cervical cancer randomized controlled trial studies.38,39
One of the major factors contributing to the high quality and accuracy of the medical record matching the self-reported screening rate is patient navigation: a majority (85.2%) of the women who self-reported screening had received our patient navigation assistance for navigating them through the health care system to obtain the Pap test. Another factor that contributed to a high agreement between self-report and validation of medical record may be the consistent and intensive training about definition and procedures of Pap test to health educators and research data collection staff.
Although patient navigation has been recognized as an instrumental component in facilitating access to appropriate health care and treatment, few programs have been well developed and tested for this population, particularly in the prevention setting. This is so despite the fact that obtaining preventive care can be a formidable challenge for Vietnamese women who face not only psychosocial, but also access and language barriers. Therefore, adapting the navigator concept for cancer prevention is an extremely important element to be incorporated into future programs for the Vietnamese American community.
Even though our multifaceted intervention is highly effective and we observed a significant increase in the receipt of Pap test (60.1%) in the intervention group of Vietnamese participants, there still remains a gap between 60.1% and 93% cervical cancer screening of Healthy People 2020. In future studies, we can explore various strategies to improve the screening rate of the over 30% non-adherent Vietnamese women.
This study’s findings demonstrated that using a community-based participatory research (CBPR) approach is more likely to increase the intervention effect on the receipt of Pap tests and the sustainability of an intervention research program. It is imperative that community partners participate in all phases of the research project so that the academic-community research team can work together to respond more effectively to the needs of targeted communities and adopt community input into the program. Although our intervention was successful, we did encounter a number of expected and unexpected challenges and learned some critical lessons during the process; some of these might be unique to this community. For example, some of the important challenges we faced during the implementation included financial constraints and access barriers encountered by underinsured and uninsured program participants. We were able to overcome the challenges through our collective efforts and innovative strategies. It is also clear that trust, mutual respect, and commitments are foundational elements for us to engage the community partners in this project. Balancing research goals while meeting community needs can be challenging.40 Assessing the effectiveness of interventions often requires a rigorous scientific design and concrete data collection procedures. For example, our academic-community partners co-designed an HBV intervention program and found ways to both adhere to evidence-based research rigor and to incorporate community needs, such as offering the intervention to the control group after the follow-up, data collection period was completed.17,41
The present study has limitations. Despite the fact that a majority of Vietnamese Americans are not born in the U.S., this study’s participants are predominately foreign-born immigrants who have little education and low incomes, and who have limited English proficiency. The intervention effect of receiving Pap tests may not be as strong among second generation, U.S.-born Vietnamese women. In addition, the results of the study may not be generalizable to the Vietnamese women nor other Asian American women outside the community setting of the U.S. Eastern region. Adaptations will be needed for disseminating the intervention to similar populations in other settings and geographic locations. Using the organization as the unit of analysis may provide slightly different results compared with individual results. However, this analytic strategy both controls for differences across sites and provides researchers with site-specific information. Researchers who implement programs at the organizational level using different sites may benefit from knowing the range outcomes for organizations. The fidelity of the intervention was assessed as part of the process evaluation which should minimize differences between implementation at each CBO. However, given the variation among sites, some differences in implementation may have accounted for the differences in Pap testing rates.
Despite the aforementioned limitations, there are several unique strengths and an overall significance to this study. For example, this study represents one of the first very few large-scale community-based randomized controlled trials that focused on the effectiveness of a culturally appropriate community-based intervention to increase cervical cancer screening and reduce health care access barriers among this high-risk population. This study addressed the health disparities suffered by high-risk medically underserved Vietnamese women, who experience the highest incidence rates of invasive cervical cancer in the U.S. and low Pap test screening rates. The study built on a strong partnership between the Vietnamese community leaders of 30 Vietnamese CBOs in the U.S. Eastern region and a multidisciplinary research team, using CBPR approach to engage community partners in project planning, recruitment, delivery and evaluation. Furthermore, the patient navigation assistance in translation, appointment scheduling for Pap test and transportation helped address the critical barriers facing the target women. In addition to the rigor of RCT, the use of both self-report and medical record data to validate the primary outcome of Pap test receipt is a strength of this study given the self-report bias in screening is well documented in previous studies.39,42–47
Last but not the least, the application of the combined HBM and SCT models that emphasize both individual and environmental system elements to guide intervention and measures may have led to a larger intervention effect than we would otherwise have seen. Based on the theoretical framework, we were able to examine the predictors of obtaining a Pap test over the course of the intervention (over the past 12 months after the randomization), the impact of the intervention on knowledge, barriers, perceived risks and self-efficacy, as well as mediating factors that are associated with the primary outcome, which is published in a separate article.24,48,49
Overall, the long-term potential benefit of this study may lead to improving accessibility and quality of health care—specifically cervical cancer screening—for Vietnamese women. The study allowed us to identify health system access barriers and demonstrated the evidence-based culturally appropriate strategies for adherence to cancer screening behaviors in this high-risk population.
Acknowledgments
This research was partially supported by National Institutes of Health, National Cancer Institute grants R01 CA 111570 (Grace X. Ma, Ph.D., Principal Investigator), U54 CA153513 Asian Community Cancer Health Disparities Center (PI: Dr. Grace Ma). The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the NCI or NIH. The authors wish to thank Asian Community Health Coalition and its member organizations for collaboration.
Contributor Information
Grace X. Ma, Department of Public Health, Center for Asian Health, Temple University, Philadelphia, PA.
Carolyn Fang, Fox Chase Cancer Center, Temple University Health System, Philadelphia, PA.
Yin Tan, Department of Public Health, Center for Asian Health, Temple University, Philadelphia, PA.
Ziding Feng, Formerly Biostatistics Program, Fred Hutchinson Cancer Research Center, Settle, Washington.
Shaokui Ge, Formerly Biostatistics Program, Fred Hutchinson Cancer Research Center, Settle, Washington.
Cuc Nguyen, Asian Community Health Coalition, Philadelphia, PA and the Vietnamese Women Association of Eastern Region, Marlton, NJ.
References
- 1.American Cancer Society. Cancer prevention and early detection facts and figures. Atlanta, GA: American Cancer Society; 2014. [Google Scholar]
- 2.McPhee SJ, Bird JA, Davis T, et al. Barriers to breast cancer and cervical cancer screening among Vietnamese-American women. Am J Prev Med. 1997 May-Jun;13:205–13. [PubMed] [Google Scholar]
- 3.Wismer BA, Moskowitz JM, Chen AM, et al. Rates and independent correlates of Pap smear testing among Korean American women. Am J Public Health. 1998 Apr;88:656–60. doi: 10.2105/ajph.88.4.656. http://dx.doi.org/10.2105/AJPH.88.4.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McPhee SJ, Stewart S, Brock KC, et al. Factors associated with breast and cervical cancer screening practices among Vietnamese American women. Cancer Detec Prev. 1997;21(6):510–21. [PubMed] [Google Scholar]
- 5.Ma GX, Fang CY, Feng Z, et al. Correlates of Cervical Cancer Screening among Vietnamese American Women. Infectious Diseases in Obstetrics and Gynecology. 2012;2012 doi: 10.1155/2012/617234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services. Healthy People 2020. Washington, DC: U.S. Department of Health and Human Services; 2015. Available at: http://www.healthypeople.gov/2020/data-search/Search-the-Data?nid=4053. [DOI] [PubMed] [Google Scholar]
- 7.Miller BA, Chu KC, Hankey BF, et al. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control. 2008 Apr;19(3):227–56. doi: 10.1007/s10552-007-9088-3. Epub 2007 Nov 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kagawa-Singer M, Pourat N. Asian American and Pacific Islander breast and cervical carcinoma screening rates and healthy people 2000 objectives. Cancer. 2000 Aug 1;89:696–705. doi: 10.1002/1097-0142(20000801)89:3<696::aid-cncr27>3.0.co;2-7. http://dx.doi.org/10.1002/1097-0142(20000801)89:3<696::AID-CNCR27>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 9.Parker SL, Tong T, Bolden S, et al. Cancer statistics, 1997. CA Cancer J Clin. 1997;47:5–27. doi: 10.3322/canjclin.47.1.5. http://dx.doi.org/10.3322/canjclin.47.1.5. [DOI] [PubMed] [Google Scholar]
- 10.United States Census Bureau. American FactFinder. Washington, DC: U.S. Census Bureau; 2010. “Summary File 1, Tables PCT5, PCT6, and PCT7.”. Available at: http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=CF. [Google Scholar]
- 11.Hoeffel EM, Rastogi S, Kim MO, et al. The Asian Population: 2010. Washington, DC: U.S. Census Bureau; Available at: http://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf. [Google Scholar]
- 12.Ma GX, Shive SE, Wang M, et al. Cancer screening behaviors and barriers in Asian Americans. Am J Health Behav. 2009 Nov-Dec;33(6):650–60. doi: 10.5993/ajhb.33.6.3. http://dx.doi.org/10.5993/AJHB.33.6.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ma GX, Tan Y, Toubbeh JI, et al. Asian Tobacco Education and Cancer Awareness Research Special Population Network. A model for reducing Asian American cancer health disparities. Cancer. 2006 Oct 15;107(8 Suppl):1995–2005. doi: 10.1002/cncr.22150. http://dx.doi.org/10.1002/cncr.22150. [DOI] [PubMed] [Google Scholar]
- 14.Asian American Federation of New York Census Information Center. Census Profile: New York City’s Asian American Population, 2004. New York, NY: Asian American Federation of New York Census Information Center; 2004. [Google Scholar]
- 15.Johnson CE, Mues KE, Mayne SL, et al. Cervical cancer screening among immigrants and ethnic minorities: a systematic review using the Health Belief Model. J Low Genit Tract Dis. 2008 Jul;12(3):232–41. doi: 10.1097/LGT.0b013e31815d8d88. http://dx.doi.org/10.1097/LGT.0b013e31815d8d88. [DOI] [PubMed] [Google Scholar]
- 16.Fang CY, Ma GX, Tan Y. Overcoming Barriers to Cervical Cancer Screening Among Asian American Women. N Am J Med Sci (Boston) 2011;4(2):77–83. doi: 10.7156/v4i2p077. http://dx.doi.org/10.7156/v4i2p077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Israel BA, Eng E, Schults AJ, et al. Methods for community-based participatory research for health. San Francisco, CA: John Wiley & Sons; 2013. [Google Scholar]
- 18.Braun KL, Nguyen TT, Tanjasiri SP, et al. Operationalization of community-based participatory research principles: assessment of the national cancer institute’s community network programs. Am J Public Health. 2012 Jun;102(6):1195–203. doi: 10.2105/AJPH.2011.300304. Epub 2011 Nov 28. http://dx.doi.org/10.2105/AJPH.2011.300304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mosavel M, Sanders KD. Community-engaged research: cancer survivors as community researchers. J Empir Res Hum Res Ethics. 2014 Jul;9(3):74–8. doi: 10.1177/1556264614540598. [DOI] [PubMed] [Google Scholar]
- 20.Bandura A. Social cognitive theory: an agentic perspective. Ann Rev Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. http://dx.doi.org/10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 21.Becker MH. The health belief model and personal health behavior. Thorofare, NJ: Slack; 1974. [Google Scholar]
- 22.Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984 Spring;11(1):1–47. doi: 10.1177/109019818401100101. http://dx.doi.org/10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 23.Ma GX, Shive SE, Wang MQ, et al. Cancer screening behaviors and barriers in Asian Americans. Am J Health Behav. 2009 Nov-Dec;33:650–60. doi: 10.5993/ajhb.33.6.3. http://dx.doi.org/10.5993/AJHB.33.6.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ma GX, Toubbeh JI, Wang MQ, et al. Factors associated with cervical cancer screening compliance and noncompliance among Chinese, Korean, Vietnamese, and Cambodian women. J Natl Med Assoc. 2009 Jun;101(6):541–51. doi: 10.1016/s0027-9684(15)30939-1. [DOI] [PubMed] [Google Scholar]
- 25.Fang CY, Ma GX, Tan Y, et al. A multifaceted intervention to increase cervical cancer screening among underserved Korean women. Cancer Epidemiol Biomarkers Prev. 2007 Jun;16(6):1298–302. doi: 10.1158/1055-9965.EPI-07-0091. http://dx.doi.org/10.1158/1055-9965.EPI-07-0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ma GX, Shive SE, Tan Y, et al. The impact of acculturation on smoking in Asian American homes. J Health Care Poor Underserved. 2004 May;15(2):267–80. doi: 10.1353/hpu.2004.0024. http://dx.doi.org/10.1353/hpu.2004.0024. [DOI] [PubMed] [Google Scholar]
- 27.Ma GX, Tan Y, Toubbeh JI, et al. Acculturation and smoking behavior in Asian-American populations. Health Educ Res. 2004 Dec;19(6):615–25. doi: 10.1093/her/cyg070. Epub 2004 Jun 15. http://dx.doi.org/10.1093/her/cyg070. [DOI] [PubMed] [Google Scholar]
- 28.Ma GX, Gao W, Fang CY, et al. Health beliefs associated with cervical cancer screening among Vietnamese Americans. J Women’s Health (larchmt) 2013 Mar;22(3):276–88. doi: 10.1089/jwh.2012.3587. Epub 2013 Feb 21. http://dx.doi.org/10.1089/jwh.2012.3587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kabacoff R. R in Action. 2. Shelter Island, NY: Manning Publications; 2011. [Google Scholar]
- 30.SAS/STAT software. Version 9.4. Cary, NC: SAS Institute Inc; 2013. The GLIMMIX procedure. [Google Scholar]
- 31.SAS software. Version 9.4. Cary, NC: SAS Institute Inc; [Google Scholar]
- 32.Revolution Analytics. R Software Package. Mountain View, CA: Revolution Analytics; 2015. Available at: http://www.revolutionanalytics.com/products. [Google Scholar]
- 33.Centers for Disease Control and Prevention. Cervical cancer and Pap test information. Atlanta, GA: Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 34.Centers for Disease Control and Prevention. The national breast and cervical cancer early detection program: reducing mortality through screening. Atlanta, GA: Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 35.U.S. Department of Health and Human Services. Before the House Committee on Commerce, Subcommittee on Health and Environment. Washington, DC: U.S. Department of Health and Human Services; 1999. Testimony on cervical cancer by Nancy C. Lee, MD. [Google Scholar]
- 36.Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2011. Bethesda, MD: National Cancer Institute; 2014. Available at: http://seer.cancer.gov/csr/1975_2011/ [Google Scholar]
- 37.Kagawa-Singer M, Pourat N. Asian American and Pacific Islander breast and cervical carcinoma screening rates and healthy people 2000 objectives. Cancer. 2000 Aug 1;89(3):696–705. doi: 10.1002/1097-0142(20000801)89:3<696::aid-cncr27>3.0.co;2-7. http://dx.doi.org/10.1002/1097-0142(20000801)89:3<696::AID-CNCR27>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 38.Taylor VM, Jackson JC, Yasui Y, et al. Evaluation of a cervical cancer control intervention using lay health workers for Vietnamese American Women. Am J Public Health. 2010 Oct;100(10):1924–9. doi: 10.2105/AJPH.2009.190348. Epub 2010 Aug 19. http://dx.doi.org/10.2105/AJPH.2009.190348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Paskett ED, McLaughlin JM, Lehman AM, et al. Evaluating the efficacy of lay health advisors for increasing risk-appropriate Pap test screening: a randomized controlled trial among Ohio Appalachian women. Cancer Epidemiol Biomarkers Prev. 2011 May;20(5):835–43. doi: 10.1158/1055-9965.EPI-10-0880. Epub 2011 Mar 23. http://dx.doi.org/10.1158/1055-9965.EPI-10-0880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Leff SS, Thomas DE, Vaughn NA, et al. Using community-based participatory research to develop the PARTNERS youth violence prevention program. Prog Community Health Partnersh. 2010 Fall;4(3):207–16. doi: 10.1353/cpr.2010.0005. http://dx.doi.org/10.1353/cpr.2010.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ma GX, Gao W, Tan Y, et al. A community-based participatory approach to a hepa titis B intervention for Korean Americans. Prog Community Health Partnersh. 2012 Spring;6(1):7–16. doi: 10.1353/cpr.2012.0002. http://dx.doi.org/10.1353/cpr.2012.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gordon NP, Hiatt RA, Lampert DI. Concordance of self-reported data and medical record audit for six cancer screening procedures. J Natl Cancer Inst. 1993 Apr;85(7):566–70. doi: 10.1093/jnci/85.7.566. http://dx.doi.org/10.1093/jnci/85.7.566. [DOI] [PubMed] [Google Scholar]
- 43.Bowman JA, Redman S, Dickinson JA, et al. The accuracy of Pap smear utilization self-report: a methodological consideration in cervical screening research. Health Serv Res. 1991 Apr;26(1):97–107. [PMC free article] [PubMed] [Google Scholar]
- 44.McGovern PG, Lurie N, Margolis KL, et al. Accuracy of self-report of mammography and Pap smear in a low-income urban population. Am J Prev Med. 1998 Apr;14(3):201–8. doi: 10.1016/s0749-3797(97)00076-7. http://dx.doi.org/10.1016/S0749-3797(97)00076-7. [DOI] [PubMed] [Google Scholar]
- 45.Howard M, Agarwal G, Lytwyn A. Accuracy of self-reports of Pap and mammography screening compared to medical record: a meta-analysis. Cancer Causes Control. 2009 Feb;20(1):1–13. doi: 10.1007/s10552-008-9228-4. Epub 2008 Sep 19. http://dx.doi.org/10.1007/s10552-008-9228-4. [DOI] [PubMed] [Google Scholar]
- 46.Pizarro J, Schneider TR, Salovey P. A source of error in self-reports of Pap test utilization. J Community Health. 2002 Oct;27(5):351–6. doi: 10.1023/a:1019888627113. http://dx.doi.org/10.1023/A:1019888627113. [DOI] [PubMed] [Google Scholar]
- 47.Sawyer JA, Earp JA, Fletcher RH, et al. Accuracy of women’s self-report of their last Pap smear. Am J Public Health. 1989 Aug;79(8):1036–7. doi: 10.2105/ajph.79.8.1036. http://dx.doi.org/10.2105/AJPH.79.8.1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ma GX, Fang CY, Tan Y, et al. Health beliefs mediate the effects of a cervical cancer screening intervention on uptake of the pap smear among vietnamese American women. New Orleans, LA. Conference Presentation at American Public Health Association; 2014. [Google Scholar]
- 49.Wang X, Fang C, Tan Y, et al. Evidence-based intervention to reduce access barriers to cervical cancer screening among underserved Chinese American women. J Womens Health (Larchmt) 2010 Mar;19(3):463–9. doi: 10.1089/jwh.2009.1422. http://dx.doi.org/10.1089/jwh.2009.1422. [DOI] [PMC free article] [PubMed] [Google Scholar]