Abstract
Purpose
Assess effects of team training on operational efficiency during outpatient MRI.
Materials and Methods
In this IRB-approved HIPAA-compliant study, 6 MRI outpatient sites of a Midwestern hospital system were randomized to serve as controls or have their teams trained in advanced communication skills. The 4th quarter fiscal year 2015 (Q4FY15) was the trial baseline. The trial ended Q3FY16. Equipment utilization (completed scans/available slots), hourly scan rates (total orders completed per machine per hour of operation), and no-show rates stratified by time were analyzed using the Cochran-Mantel-Haenszel method, with individual comparisons performed with Bonferroni correction.
Results
The study encompassed 27,425 MRI examinations. Overall volume peaked at baseline and then declined over the next quarters. Compared to baseline, untrained sites experienced significant drops in equipment utilization (p<0.01 [Q1FY16]; p<0.0001 [Q2 FY16, Q3FY16]), decreasing from 77% to 65% over the study period, corresponding to a decrease from 1.15 to 0.97 in hourly scan rates. For trained sites, these metrics showed no significant change, with maintenance of hourly scan rates of 1.23 and 1.27 and equipment utilization rates of 83% and 85% between baseline and Q3FY16. No-show rates remained stable at trained sites but increased at untrained sites in the last two quarters (p<0.05). Nationally benchmarked patient satisfaction percentile ranking gradually increased at trained sites from 56th at baseline to 70th and successively decreased at untrained sites from 66th to 44th.
Conclusion
MRI outpatient facilities trained in advanced communication techniques may have more favorable operational efficiency than untrained sites in a saturated market.
Keywords: interpersonal skills, communication, MRI, equipment utilization, patient satisfaction
INTRODUCTION
Team training of MRI staff in advanced communication and calmative techniques has been associated with significant improvements in patient throughput and increased patient satisfaction in longitudinal clinical trials [1–3]. In these studies, improved efficiency was achieved by reducing incompletion rates among claustrophobic and distressed patients, fewer no-shows, and greater ability to keep patients longer in the scanner for more novel time-intensive and/or combined studies in the same setting. When assessing quality improvement initiatives for enhancing imaging centers’ efficiency, however, general trends in healthcare can significantly affect MRI usage and account for observed outcomes in longitudinal non-randomized trials.
After imaging experienced rapid growth early in the last decade, drastic reductions in reimbursement, cost-sharing of patients in medical cost, and the economic recession reverted the trend by 2007 [4–6]. By 2012, market saturation with enough or more scanners than needed for the populations served led to closures of free-standing MRI facilities in some large urban areas [4]. Now, high-end construction projects in healthcare, with their associated state-of-the art MRI facilities, are booming [7], fueled in part by philanthropic concerns with cancer care and other specialty diseases [8]. Further effects on imaging usage are to be expected from recent reforms in health policy and implementation of the Affordable Care Act shifting payer focus toward value-based care, with emphasis on bundled payments, capitation, integrated care, and shared accountability [9]. In this context, patient satisfaction has become a measure of quality of care and determinant of payment by the Centers for Medicare and Medicaid Services (CMS) [10, 11]. Improvement in operational efficiency therefore cannot be brought on by actions that adversely affect the patient experience.
This study was undertaken to assess whether team-training in patient-centric communication positively affects overall patient throughput while providing a positive patient experience in a randomized trial. Equipment utilization and patient satisfaction ratings were primary outcome parameters. Coincidentally, the trial began around the time when new MRI capacity was added in the urban environment in which the trial sites operated, offering a rare glimpse at the transition point towards market saturation.
MATERIALS AND METHODS
The study was approved by the Institutional Review Board and is Health Insurance Portability and Accountability (HIPAA) compliant. The project was supported by a Small Business Innovation in Research (SBIR) Phase II Grant awarded by NIH/NCCIH to EVL, who is the owner of a small business as required by the grant mechanism. All study data were controlled and analyzed by the authors at the academic sites who did not have a relationship or conflict of interest with the small business. The small business conducted the team training.
Sites and Randomization
A large urban hospital system provided the study sites, which all used the same data capture methods and did not have overlap of their technical personnel. There were 9 existing sites plus one slated to open during the trial period. To enhance comparability of outpatient operations, three hospital-based sites (two existing sites and one to be opened) were excluded. Excluded also was one previously commercially trained outpatient site. Thus 6 MRI satellites were enrolled. There was no change in hours of operations, number of available examination slots, or full-time equivalents of personnel throughout the trial.
Data from 1 November 2014 to 30 March 2015 were used to match three best fitting pairs of sites. Randomization among the pairs then determined which 3 sites would be trained in July 2015 and which would serve as controls.
Data Collection
All site activities, financials, and satisfaction data were overseen centrally by the same information technology (IT) group using the same data collection tools. The IT group was not aware of the ongoing study. Hourly scan rate was calculated as total orders completed per machine available per hour of operation. Equipment utilization was calculated as number of completed exams per number of available slots. Slot length was based on case mix, acuity level, and available personnel per site and centrally determined to be 0.67 hrs as best reflective of an operational average of room time across the offered examinations. Since the slot length was stable at 0.67 hours for all sites throughout the trial, hourly scan rate (total orders completed per machine hour of operation) is equal to the equipment utilization rate multiplied by 1.5.
MRI Scheduling
Central scheduling handled appointments for all 10 system-wide sites. The schedulers were not aware of the ongoing study. Taking into account patient preferences, the schedulers offered the next available opening. Should any sites system-wide fall into low utilization ranges (a relatively lower fraction of booked slots), schedulers would steer patients towards those sites as alternatives to waiting longer for a more desirable but already heavily booked site.
None of the MRI units in the study provided sedation drugs for outpatients. Examinations requested with intravenous sedation were directed to the main hospital. Patients who wished to take oral medications had to have those prescribed by their referring physicians and bring the medications with them to their exams.
Training
The teams received two 8-hr intensive classroom sessions, one in mid-June and one in mid-July 2015, during working hours. In all, 18 technologists including their managers were trained. Team training followed a blueprint of advanced communication and interpersonal skills training (Comfort Talk®, LLC, Brookline, MA) [2]. The sessions included scientific background information, group discussions, live and video demonstrations, extensive small group practice and role play. The classroom sessions were each followed by 2 days on-site supervision.
The first session emphasized gaining rapid rapport through short initial matching of the patient’s verbal and nonverbal behaviors before leading to a more relaxed state, use of encouragement toward achieving patient cooperation, integration of room stimuli, particularly noise, into a patient’s preferred scenario of choice, and basic pain and anxiety management techniques with integration of hypnoidal language. The second 8-hr session emphasized advanced techniques in management of anxiety and resistance. The new sets were practiced in videoed interactions of role play in a microteaching approach.
Trainees further had access to an online training support portal and an online course for those who were not able to attend all live sessions. A post-training spaced-learning module in the form of a team and individual competition provided two weekly short snippets of teaching points via an app or email for the 11 weeks [12].
Data Analysis
The last quarter of the 2015 fiscal year between April and June 2015 (Q4 FY15) served as baseline. July 2015 to September 2015 represented the first post-training quarter (Q1 FY16). Data were collected to include Q3 FY16.
Analysis of categorical data (equipment utilization and no-show rates) was performed using the chi square method or its variants as described herein. When stratifying categorical data by time, the Cochran-Mantel-Haenszel test for repeated 2×2 tests of independence was performed, with continuity correction, to compute χ2MH. Pairwise differences between trained sites and untrained sites at each of 4 time points and differences between baseline and each of 3 FY2016 time points for both trained sites and untrained sites were assessed using the chi square method; the p-values reported for these comparisons represent Bonferroni-corrected p-values obtained by multiplying uncorrected p-values by 10 to adjust for multiple comparisons. A p-value of less than 0.05 was considered statistically significant. Statistical computations were performed manually using Microsoft Excel 2010.
Patient Satisfaction
The hospital system contracted with Press Ganey Associates, Inc. (Wakefield, MA) for their routine collection of patient satisfaction assessments. Patients’ assessment of services on a Likert scale between 0 (very poor) and 5 (very good) were translated by multiplication into raw scores between 0 (lowest) and 100 (highest level of satisfaction) and translated into nationally benchmarked percentile rankings [3].
RESULTS
Site Selection and Volume
Table 1 depicts the pairs that were deemed to be best comparable based on volume, completed exams, and scanner types and their group allocation after randomization. Between November 2014 and March 2015, the training site group performed 8,918 MRI examinations with an average utilization rate of 72%, the control group 7,408 exams with an average utilization rate of 71%.
Table 1.
Outpatient MRI site characteristics and determination of randomization.
| Pairs | Treatment | MRI Volume* |
Completed Exams* |
Scanner Numbers per Site and Type |
Scan Hours/Week |
|
|---|---|---|---|---|---|---|
|
| ||||||
| 1A | Control | 2,015 | 71.1% | 1 | Siemens Verio | 53.5 |
|
| ||||||
| 1B | Training | 2,713 | 74.3% | 1 | Siemens Verio | 90.0 |
|
| ||||||
| 2A | Control | 3,813 | 66.3% | 2 | Siemens Skyra; Siemens Avanto Mobile | 67.5 |
| 53.5 | ||||||
|
| ||||||
| 2B | Training | 4,785 | 70.0% | 3 | Siemens Verio, Avanto, and Trio | 52.5 |
| 90.0 | ||||||
| 47.5 | ||||||
|
| ||||||
| 3A | Training | 1,420 | 72.2% | 1 | GE Signa HDxt | 45.0 |
|
| ||||||
| 3B | Control | 1,580 | 75.8% | 1 | GE Signa HDxt | 55.0 |
Data on MRI volume and completion rates were collected prior to randomization, between November 2014 and March 2015.
During the trial period (baseline Q4FY15 through Q3FY16) 27,425 examinations were performed at all sites, 15,590 training sites and 11,835 control sites. The average paired difference in study volume between paired trained and untrained sites of 237 per quarter at baseline increased monotonically to 404 per quarter at the last time point.
Hourly Scan Rates and Equipment Utilization
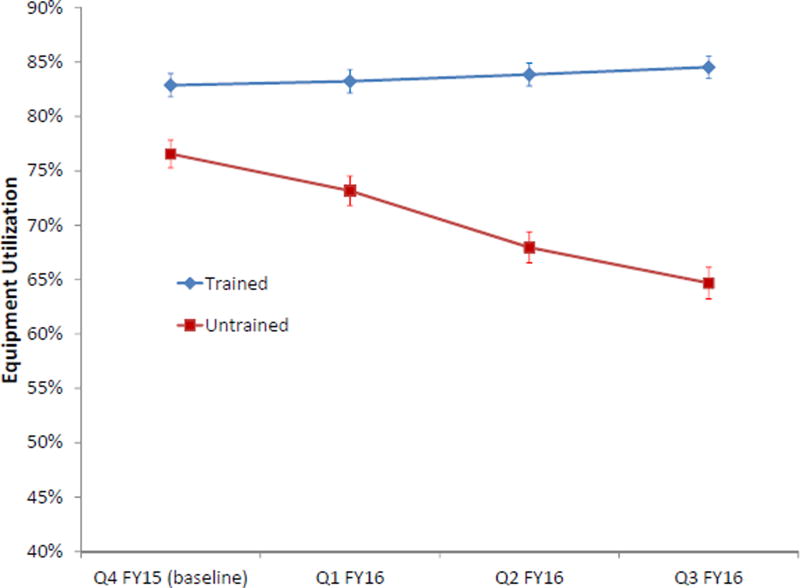
On average, scanners at the trained sites were available for imaging 65 hrs per week and at the untrained sites 57.4 hrs per week (Table 1). Trained sites maintained hourly scan rates and equipment utilization over time, whereas untrained sites experienced a significant decline that became more pronounced with each quarter (Fig. 1). Chi square analysis showed significantly higher equipment utilization rates, analyzed as a proportion of completed imaging time slots relative to total available time slots, at trained sites compared to untrained sites when stratifying by time (χ2MH=858.2; p<0.0001). Pairwise chi square analyses demonstrated statistically significant higher equipment utilization at trained sites at each of the 4 quarters (p<0.0001). Pairwise comparisons of equipment utilization at each FY2016 quarter to baseline (Q4 FY15) yielded no significant difference from baseline at any of the trained sites, but there were significant decreases from baseline at untrained sites (p<0.01 for Q1 FY16 and p<0.0001 for Q2 FY16 and Q3 FY16).
Fig 1.
Equipment utilization rates at trained and untrained sites over time. Since the slot length was stable at 0.67 hours for all sites throughout the trial, hourly scan rate (total orders completed per machine hour of operation) is equal to the equipment utilization rate multiplied by 1.5. Thus a 100% scan utilization rate would equal a 1.5 hourly scan rate. Error bars denote 95% confidence intervals for proportions based on the binomial distribution.
The utilization rates of 83% at baseline and 85% in Q3 FY16 at trained sites, as seen in Figure 1, translate into hourly scan rates for trained sites of 1.23 and 1.27. The significant drop in utilization rates at untrained sites from 77% at baseline to 65% in Q3 FY2016 corresponds to decreased hourly scan rates from 1.15 to 0.97 for the untrained sites.
No-show Rates
Training demonstrated significantly lower no-show rates at trained sites compared to untrained sites when stratifying by time (χ2MH =28.7; p<0.0001) (Fig. 2). Pairwise contrasts between trained and untrained sites show no significant difference at the first two time points, but there were significantly lower no-show rates with training for Q2 FY16 (p<0.05) and Q3 FY16 (p<0.01).
Fig 2.
No-show rates at trained and untrained sites over time. Error bars denote 95% confidence intervals for proportions based on the binomial distribution.
Patient Satisfaction
Figure 3 demonstrates the raw scores and percentiles of patients’ overall satisfaction with the MRI operation, with upward trends for trained sites and downward trends for untrained sites.
Fig 3.
Patient satisfaction raw scores (a) and percentile rankings (b) benchmarked on 1028 centers nationally.
System-wide Changes
In Q3FY15, the 10th MRI site was opened in a brand-new flagship cancer hospital in the main hospital complex, adding approximately 500 outpatient imaging hours per quarter. At the same time, a major competitor added MRI capacity in the state-of-the-art nine-story tower of a Neuroscience Treatment Center and recruited away a group of six neurologists. Until Q3 FY15, the hospital-wide system, including the test and control sites of this study, had seen a steady increase in quarterly MRI volumes since 2012. Volume peaked in Q4 FY15 (the baseline of the randomized trial data collection) and then declined, suggesting saturation of capacity (Fig. 4). Figure 5 shows the winners and losers with regard to volume. Of note is that site D in the figure, an outpatient facility that had been trained in 2014, also held its volume steady as did the trained sites in the current study. Site C within the hospital complex, which had been trained in 2012 and received a refresher training in August 2016, increased its volume. The untrained hospital sites, including the brand-new facility (site A in Fig. 4), and untrained outpatient sites from the study saw a decrease in volume.
Fig 4.
Total quarterly volume of outpatient MRIs within the entire hospital system. Opening of a new MRI facility within the hospital system and a new MRI facility at a local competitor occurred in Q3 FY15.
Fig 5.
Within-system outpatient MRI volumes during the study period. Sites A, B, and C are based in the main hospital complex. A is the newly added site at the Cancer Center. The teams at the hospital-based site C and the outpatient imaging center site D had previously undergone team training.
DISCUSSION
In this study, MRI sites trained in advanced communication skills fared significantly better than untrained sites with regard to efficiency parameters while providing a positive patient experience. Trained sites maintained their equipment utilization and hourly scan rates with relatively constant total MRI volumes, whereas untrained sites saw a significant decline in equipment utilization, scan completions, and total volume.
The Medicare Payment Advisory Commission (MedPAC) and the Centers for Medicare and Medicaid Services (CMS) use the “equipment utilization assumption rate” to determine the overhead cost for operating expensive equipment such as MR scanners [13]. The equipment utilization assumption rate is defined by how many hours in a 50-hr work week a scanner is used for imaging – the higher the utilization rate, the lower the reimbursement for individual scans. After passage of the Patient Protection and Affordable Care Act in 2010, the rate was increased from 50% to 75% and now stands at 90%, assuming machines being used at full capacity 45 out of 50 hrs a week. After team training, equipment utilization at trained sites was 85%.
Considering that the trained sites had an average 65-hr availability week, this is equivalent to operation at full capacity for 55.25 hrs/week. Although this exceeds the usage assumed for purposes of technical fee reimbursement, the additional disbursement for technologists, facility staff and overhead for the extra 15hrs/week has to be taken into the equation. Untrained sites were far below at 65% for their equipment utilization. This latter number mirrors closely the median 63% that the Radiology Business Management Association (RBMA) found in a 2009 survey of 261 machines in 46 centers [13]. In 2010, the American College of Radiology, RBMA, and Access to Medical Imaging Coalition jointly surveyed 2,843 machines in 720 facilities and found an even lower median equipment utilization rate of 45% for the time an office was open for business [13].
The assumed slot length of 0.67 hrs (40 min) is within the customary range of the industry and represents an average over a mixture of shorter and longer exams and includes completing the paperwork, prescreening, and postprocessing of images. Getting the patient into the room and onto the table, positioned, and examined can take extra time when patients are upset, claustrophobic, hurting, or moving. Better resource utilization in terms of equipment utilization and completed exams thus can be expected when personnel are at greater ease handling such cases faster, as offered by the training. The alternative would be shortening slot length and imaging time [14, 15], which however would make the operation more vulnerable to disruption by patients needing extra time and placing extra stress on already stressed personnel [16, 17]. Furthermore it may risk poor patient satisfaction ratings.
Efficient throughput depends on multiple factors: number of referrals in relation to available slots, willingness of patients to accept and keep their appointment, and sufficiently skilled personnel enabling a smooth transition from registration to discharge. In this study, the departure of the neurologists may have adversely affected referrals. Based on the scheduling algorithm this event should have affected all outpatient sites similarly. All sites in the randomized trial had free and convenient parking; all were very well maintained and meticulously clean; and all scans were read by University-based faculty, diminishing potential impact of these factors as discriminators in patients’ site preferences. One may suggest the ability of trained personnel to better guide patients through their exams as a factor for creating preference. Willingness of satisfied customers to return and their word-of-mouth advertising to others [3] may also have been a contributor to the increasing differential among sites over time.
Increased patient satisfaction with team training in advanced communication skills has been described in a non-randomized study [3]. It is possible that the improved patient experience contributed to avert a loss in volume at the trained sites. It is conceivable that at the untrained sites, a loss in volume may have made the personnel concerned about staff cuts. Concerns about job security among personnel have been shown to increase patients’ noncompletion rates of MRI due to claustrophobia [1], and possible similar subconscious changes in the patient-provider interactions may have adversely affected satisfaction rankings over the duration of the study.
The trend toward increased no-show rates, as found for the untrained sites, may have been due to expectations by patients to be accommodated quickly for a new appointment when supply exceeds demand. The training may have offset that effect in analogy to a prior longitudinal study where training in calmative techniques resulted in decreased no-show rates [2]. Patients who do not show tend to do so repeatedly and miss on average four appointments [18]. One may speculate that patients who were able to complete their scans the first time may therefore not have joined the pool of repeat no-shows among the trained sites.
When calculating return-on-investment (ROI), the argument may be easier to make in a case where patient throughput and volume increases as compared to preventing greater inefficiency and volume loss. Using the avoidance of loss of throughput as a criterion, assuming a single exam per patient at a base-facility case cost of $444 [19] and including personnel cost for the training, a commercial training would have amortized in about 100 days. Although improved patient satisfaction directly affects reimbursement by CMS and affects willingness to return to and recommend a site, it is complex to identify ROI for defined improvements.
The study has limitations. Even though it included 6 randomized sites and >27,000 examinations, they were all from within the same healthcare system. Conclusions are thus not necessarily generalizable to other settings. The coincidence of the creation of new capacity at the host institution and of a competitor at baseline further created an unexpected situation, which fortuitously enabled the assessment of that circumstance. It is also not possible to exactly gauge the effect of the competitor on the perception of market saturation.
Trained and untrained groups were not entirely homogenous as evidenced by different total volumes and equipment utilizations rates at baseline, a risk we had worked to minimize by pairing the most comparable sites prior to randomization.
It is difficult to fully gauge the role of centralized scheduling in the distribution of patients to sites. The faster turnaround at trained sites may have opened up more available slots in the centralized scheduling system, favoring trained sites. On the other hand the algorithm had schedulers steer patients to lower utilization sites, off-setting such effects and potentially contributing to untrained sites having more throughput than they would have had otherwise. Since central scheduling was not aware of the ongoing trial, it is unlikely that the trial introduced intentional preferential treatment of any sites beyond the prevailing routine algorithms.
We conclude that team training in advanced communication and interpersonal skills provides an advantage in patient throughput and patient satisfaction, particularly in a saturated market where shifts in productivity may threaten viability of operations.
Acknowledgments
We gratefully acknowledge the leadership of the site leads in support of the trial and implementation of training at the training sites. Our thanks go to Andrea Burt, RT (R,CT,MR), Wendy Eley, BA, RT, (R,CT,MR), Catharine Ferritto, RT(R), Tonette Orsini, AS, RT(R,MR,CT), Carlye Bell, AS, RT(R,MR,CT) and Daphne Davis, BS, RT(R,CT,MR). We appreciate the assistance of Luke MacAdam, MBA in providing the patient satisfaction data.
We appreciate the expert clinical trial support by Barbara McCracken-Bussa, CCRP, Research Manager, The Ohio State University Wexner Medical Center.
The project described was supported by NIH Award Number R44AT006296 from the National Center for Complementary & Integrative Medicine (NCCIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of NCCIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest:
Elvira Lang, MD: Founder and President, Hypnalgesics, LLC
Nothing to disclose for any of the remaining authors.
References
- 1.Lang EV, Ward C, Laser E. Effect of team training on patients' ability to complete MRI examinations. Acad Radiol. 2010;17(1):18–23. doi: 10.1016/j.acra.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 2.Norbash A, Yucel K, Yuh W, et al. Effect of team training on improving MRI study completion rates and no show rates. J Magn Reson Imaging. 2016;44(4):1040–7. doi: 10.1002/jmri.25219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lang EV, Yuh WT, Ajam A, et al. Understanding patient satisfaction ratings for radiology services. AJR Am J Roentgenol. 2013;201(6):1190–5. doi: 10.2214/AJR.13.11281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duszak R. Medical imaging: Is the growth boom over? [Accessed 05/27/2016];The Neiman Report, No. 1, October 2012. Studies in Health Care and Economics [Internet] Available at: http://www.acr.org/~/media/ACR/Documents/PDF/Research/Brief%2001/PolicyBriefHPI092012.pdf.
- 5.Zheng S, Ren ZJ, Heineke J, et al. Reductions in diagnostic imaging with high deductible health plans. Med Care. 2016;54(2):110–7. doi: 10.1097/MLR.0000000000000472. [DOI] [PubMed] [Google Scholar]
- 6.Thrall JH. Appropriateness and imaging utilization: "computerized provider order entry and decision support". Acad Radiol. 2014;21(9):1083–7. doi: 10.1016/j.acra.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 7.Morse S. [Accessed June 06, 2016];Top healthcare construction projects of 2015; building surges as demand picks up, Revista says. 2015 Nov 09; Available at: http://www.healthcarefinancenews.com/news/top-healthcare-construction-projects-2015-buidling-surges-demand-picks-revista-says.
- 8.Dietsche E. [Accessed July 06, 2016];10 largest donations from individuals to healthcare organizations in 2015. 2015 updated Dec 07, 2015. Available at: http://www.beckershospitalreview.com/finance/10-largest-donations-from-individuals-to-healthcare-organizations-in-2015.html.
- 9.Skinner J, Chandra A. The past and future of the Affordable Care Act. JAMA. 2016;316(5):497–9. doi: 10.1001/jama.2016.10158. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Medicare and Medicaid Services. [Accessed December 5, 2012];Roadmap for implementing value driven healthcare in the traditional Medicare Fee-for-Service Program. 2009 Available at: http://www.cms.hhs.gov/QualityInitiativesGenInfo/downloads/VBPRoadmap_OEA_1-16_508.pdf.
- 11.Centers for Medicare and Medicaid Services. Hospital Value-Based Purchasing Program (VBP) Washington, DC: Medicare Learning Network; 2011. [Accessed January 20, 2013]. updated November 2012. Available at: http://www.cms.gov/Hospital-Value-Based-Purchasing. [Google Scholar]
- 12.Scales CD, Jr, Moin T, Fink A, et al. A randomized, controlled trial of team-based competition to increase learner participation in quality-improvement education. Int J Qual Health Care. 2016;28(2):227–32. doi: 10.1093/intqhc/mzw008. [DOI] [PubMed] [Google Scholar]
- 13.American College of Radiology. Equipment utilization rate assumption rate issue brief. [Accessed 06/13/2016];Equipment utilization rate changes adversely affect patients and radiologists. Available at: http://www.acr.org/~/media/ACR/Documents/PDF/Advocacy/Fed%20Relations/EquipmentUtilizationAssumptionRateIssueBrief.pdf.
- 14.Thrall JH. Trends and developments shaping the future of diagnostic medical imaging: 2015 Annual Oration in Diagnostic Radiology. Radiology. 2016;279(3):660–6. doi: 10.1148/radiol.2016160293. [DOI] [PubMed] [Google Scholar]
- 15.Cabral-Goncales I. [Accessed 07/18/2016];MRI department efficiency: Process and protocol improvement. Available at: http://www.bidmc.org/~/media/Files/QualityandSafety/2015%20Silverman%20Symposium/BIDMC/MRI%20Department%20Efficiency%20-%20Process%20and%20Protocol%20Improvement.pdf.
- 16.Graham J, Ramirez AJ, Field S, et al. Job stress and satisfaction among clinical radiologists. Clin Radiol. 2000;55(3):182–5. doi: 10.1053/crad.1999.0379. [DOI] [PubMed] [Google Scholar]
- 17.McDonald RJ, Schwartz KM, Eckel LJ, et al. The effects of changes in utilization and technological advancements of cross-sectional imaging on radiologist workload. Acad Radiol. 2015;22(9):1191–8. doi: 10.1016/j.acra.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 18.Lacy NL, Paulman A, Reuter MD, et al. Why we don't come: patient perceptions on no-shows. Ann Fam Med. 2004;2(6):541–5. doi: 10.1370/afm.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andre JB, Bresnahan BW, Mossa-Basha M, et al. Toward quantifying the prevalence, severity, and cost associated with patient motion during clinical MR examinations. J Am Coll Radiol. 2015;12(7):689–95. doi: 10.1016/j.jacr.2015.03.007. [DOI] [PubMed] [Google Scholar]