Abstract
The purpose of this study is to define the incidence of hip arthroscopy-related procedures in the United States prior to and following 2011 and to determine if the rise in incidence has coincided with an increase in the complexity and diversity of procedures performed. Patients who underwent hip arthroscopy were identified from a publicly available US database. A distinction was made between ‘traditional’ and ‘extended’ codes. CPT-29999 (unlisted arthroscopy) was considered extended and counted only if associated with a hip pathology diagnosis. Codes directed toward femoroacetabular impingement pathology were also considered extended codes and were analyzed separately based on increased technical skill. Unpaired student t-tests and z-score tests were performed. From 2007 to 2014, there were a total of 2581 hip arthroscopies performed in the database (1.06 cases per 10 000 patients). The number of hip arthroscopies increased 117% from 2007 to 2014 (P < 0.001) and 12.5% from 2011 to 2014 (P = 0.045). Hip arthroscopies using extended codes increased 475% from 2007 to 2014 (P < 0.001) compared to 24% for traditional codes (P < 0.001). Codes addressing femoroacetabular impingement (FAI) pathology increased 55.7% between 2011 to 2014 (P < 0.001). The ratio of labral repair to labral debridement in patients younger than 50 years exceeded >1.0 starting in 2011 (P < 0.001). The total number of hip arthroscopies in addition to the complexity and diversity of hip arthroscopy procedures performed in the United States continues to rise. FAI-based procedures and labral repairs are being performed more frequently in younger patients, likely reflecting both improved technical ability and current evidence-based research.
INTRODUCTION
There has been a rapid increase in the number of hip arthroscopies performed in the United States over the past two decades [1–4]. Indications for hip arthroscopy continue to expand due in part to a better understanding of hip joint pathology [5–7], better ability to evaluate the hip, including advanced imaging, as well as an improved technical ability to treat these conditions with minimally invasive techniques.
In recent years, new current procedural terminology (CPT) codes have been incorporated in an attempt to match the growing indications and complexity of hip arthroscopy. CPT codes are billing codes maintained by the American Medical Association that identify services rendered on a claim. New editions are released each October. In 2011, CPT codes for procedures such as labral repair, femoroplasty and acetabuloplasty were added [1]. Previous studies have reported that the number of hip arthroscopy procedures is on the rise, but the majority of these were based on data collected prior to the introduction of these new codes[1, 4]. As such, they are unable to provide a detailed description of which specific procedures are being performed.
The purpose of this study is to define the incidence of hip arthroscopy-related procedures in the United States prior to and following 2011 and to determine if the rise in incidence has coincided with an increase in complexity and diversity of procedures performed. We hypothesized that the incidence of hip arthroscopy overall and the incidence of new procedure codes will increase following 2011, demonstrating that more advanced procedures are being performed more frequently. We also hypothesize that the growth of labral repair will exceed debridement, especially in younger patient populations as a reflection of evidence-based practices.
MATERIALS AND METHODS
Patients who underwent hip arthroscopy were identified from the Humana Claims database using PearlDiver search technology. (PearlDiver Technologies, Warsaw, IN) The Humana Claims database is composed of 20.9 million patients and includes private/commercially insured and Medicare Advantage patients. Patients extend all regions of the United States: 54% from the South, 24% from the Midwest, 14% from the West and 8% from the Northeast. Approximately 57% of patients are listed as having private/commercial insurance, 39% Medicare Advantage and 3% Medicaid. Within the Humana Claims database 47.6% of patients are younger than 65 years of age. PearlDiver technology allows personalized queries of the Humana Claims database including distinction of reimbursement claims for inpatient and outpatient care as well as a breakdown of both facility and physician costs. Returned data is automatically de-identified and thus exempt from institutional review board approval. At the time of query (January 2016), data was available from 2007 through the second quarter of 2015. Data were arranged by year and gender, and incidence was calculated per 10 000 persons, allowing comparisons to previous investigations using other billing-derived datasets [1, 2]. Codes were queried such that the number of patients receiving treatment were uniquely identified, regardless of the number of codes that were present.
COHORTS
Those patients having a CPT code for hip arthroscopy (Table I) were identified from the Humana Claims database. For CPT code 29999, which is an unlisted procedure code utilized for hip arthroscopy, patients were only included if associated with an International Classification of Diseases, ninth revision (ICD-9) code related to hip pathology, as described in previous literature within 90 days of hip arthroscopy [1, 2].
Table I.
Common CPT codes and hip-related ICD-9 codes used for hip arthroscopy
| Summary of CPT codes queried for analysis | |
|---|---|
| Traditional | |
| CPT-29860 | Hip arthroscopy, diagnostic with or without biopsy |
| CPT-29861 | Hip arthroscopy, removal of loose body or foreign body |
| CPT-29862 | Hip arthroscopy, chondroplasty, abrasion arthroplasty and/or resection of labrum |
| CPT-29863 | Hip arthroscopy, synovectomy |
| Extended | |
| CPT-29914 | Hip arthroscopy, femoroplasty |
| CPT-29915 | Hip arthroscopy, osteoplasty acetabulum |
| CPT-29916 | Hip arthroscopy, labral repair |
| CPT-29999 | Unlisted procedure arthroscopy |
| FAI | |
| CPT-29914 | Hip arthroscopy, femoroplasty |
| CPT-29915 | Hip arthroscopy, osteoplasty acetabulum |
| CPT-29916 | Hip arthroscopy, labral repair |
| CPT - current procedural terminology | |
| FAI - femoroacetabular impingement | |
Hip-related ICD-9 Codes: ICD-9-D-71515, ICD-9-D-71525, ICD-9-D-71535, ICD-9-D-71595, ICD-9-D-71605, ICD-9-D-71615, ICD-9-D-71625, ICD-D-71635, ICD-9-D-71645, ICD-9-D-71655, ICD-9-D-71665, ICD-9-D-71685, ICD-9-D-71695, ICD-9-D-71805, ICD-9-D-71845, ICD-9-D-71855, ICD-9-D-71865, ICD-9-D-71875, ICD-9-D-71885, ICD-9-D-71895, ICD-9-D-71985, ICD-9-D-71995.
ICD-9, International Classification of Diseases, ninth revision.
VARIABLES OF INTEREST
Individual codes associated with hip arthroscopy were tracked by year and patient age between the years of 2007–2014 (2015 was not included since data was only available through Q2). Coding changes between the years of 2007–2014, 2009–2014 and 2011–2014 were calculated to allow for comparison to prior publications. A distinction was made between ‘traditional’ codes and ‘extended’ codes based on the history of coding practices. Traditional codes were defined as CPT-29860, CPT-29861, CPT-29862 and CPT-29863, representing codes available early in the development of hip arthroscopy (Table I). Extended codes were defined as CPT-29914, CPT-29915, CPT-29916 and CPT-29999 with an associated hip pathology code (Table I). This grouping incorporated codes introduced after 2011 along with CPT-29999. CPT-29999 was included with extended codes as the represented procedures were assumed to be newer in scope or previously less commonly performed, therefore not accounted for in traditional or more recent coding. Codes directed toward femoroacetabular impingement pathology (CPT-29914, CPT-29915, CPT-29916) were also combined for analysis as these codes were considered to require more technical skill and experience to perform.
STATISTICAL ANALYSIS
Groups were analysed using unpaired student’s t-tests and z-score tests. Statistical significance was set at alpha less than 0.05. MedCalc V16.2 (MedCalc Software, Ostend, Belgium) was used for statistical analysis.
Data were reported as incidence per 10 000 orthopaedic patients and percent change was defined as (total number of yearafter patients – total number of yearearlier patients)/total number of yearafter patients) × 100.
RESULTS
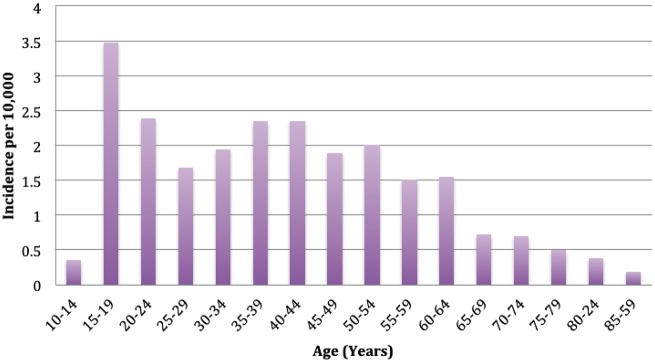
There were a total of 24 237 142 patients screened from the years 2007–2014, with a total of 2581 hip arthroscopies identified (overall incidence of 1.06 per 10 000 patients). Female patients made up 62.5% of the total returned population (P < 0.001). The age distribution of patients undergoing hip arthroscopy from 2007 to 2014 is shown in Fig. 1, with the highest incidence occurring between the ages of 15–24 years and 35–44 years.
Fig. 1.
Incidence of hip arthroscopy stratified by age (years) from 2007 to 2014. The highest incidence of hip arthroscopy was in patients 15–24 years of age, followed by 35–44 years of age.
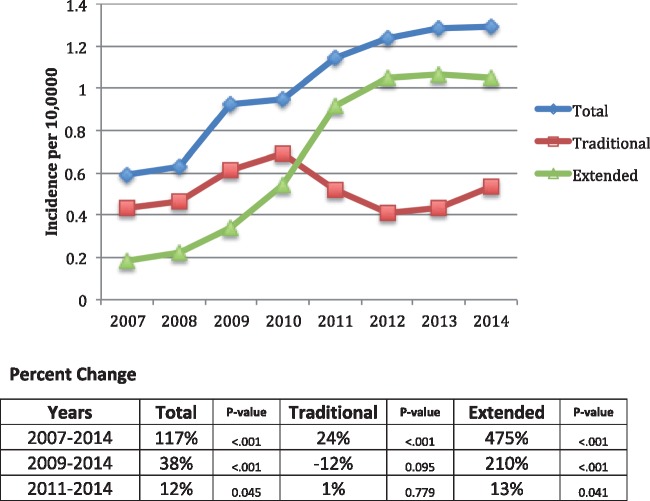
Figure 2 shows the incidence of all hip arthroscopies performed annually between 2007 and 2014, including those specifically considered representative of traditional and extended codes. Overall, an increase was observed for all procedures between 2007 and 2014. Similarly, a 475% increase in incidence for extended cases was observed between 2007 and 2014 and a 210% increase was observed from 2009 to 2014. In contrast, a decrease in incidence for traditional codes was found over the same time period, with an inflection point occurring in association with the introduction of the new codes in 2011. Starting in 2011, a higher incidence of extended cases was observed in comparison to traditional cases. By 2014, there were almost double the number of extended codes billed compared to traditional codes (P < 0.001).
Fig. 2.
Incidence of hip arthroscopy based on category and percent change from 2007 to 2014. The graph demonstrates the increase in hip arthroscopy between 2007 and 2014. With the introduction of billing codes for more extended procedures, particularly FAI and labral repair, in 2011, there was an initial drop in traditional procedures followed by a small, gradual rise in traditional procedures, though still lower than its peak in 2010. On the other hand, extended procedures rose with the introduction of the new codes and have continued to rise or stay steady since 2012.
Table II shows the demographics of hip arthroscopies performed. Regional variations did not appear to differ for traditional and extended codes. A higher proportion of patients receiving traditional procedures billed under private insurance versus extended codes (P < 0.001). Patients receiving femoroacetabular impingement (FAI) specific codes had the highest percentage of private codes (77%). CPT-29999 favored Medicare patients (56%) versus private/commercial patients (44%).
Table II.
Demographics of CPT codes grouped by type (traditional, extended, FAI) compared by region and insurance type
| Arthroscopy type | Insurance type (%Total) |
Region (% Region) |
|||||
|---|---|---|---|---|---|---|---|
| Private/commercial (%) | Medicare (%) | All (%) | Northeast (%) | South (%) | Midwest (%) | West (%) | |
| Scope traditional | 65 | 34 | 39 | 39 | 41 | 37 | 36 |
| Extended | 56 | 43 | 61 | 61 | 59 | 63 | 64 |
| FAI | 77 | 23 | |||||
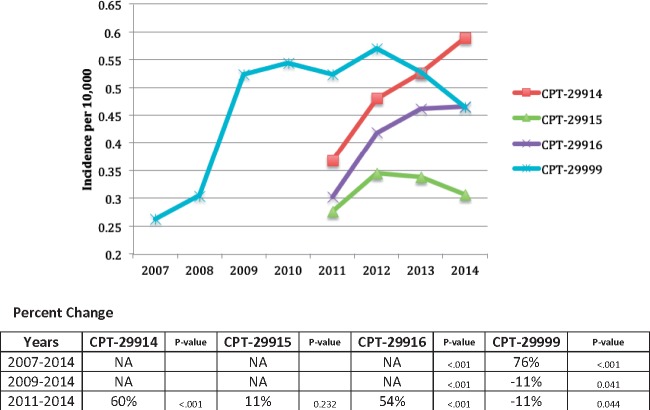
From 2011 to 2014, there were a total of 965 hip arthroscopies for FAI reported. Of these, 78.5% included femoroplasty, 48.2% included acetabuloplasty and 65% included labral repair. Figure 3 shows the annual incidences for all hip arthroscopies related to FAI pathology. Codes for femoroplasty (CPT-29914), acetabuloplasty (CPT 29915) and labral repair (CPT-29916) all increased in incidence between 2011 and 2014, although only changes for femoroplasty and labral repair were significant. The biggest increase was seen in femoroplasty. Acetabuloplasty was performed in association with a labral repair 60% of the time and with a partial labrectomy 27% of the time. Femoroplasty was performed with a labral repair 64% of the time and with partial labral resection 26% of the time.
Fig. 3.
Incidence and percent change in billing of extended codes. This graph suggests that many of the unlisted codes had been related to FAI prior to 2011, as reflected by the decrease in that code following the introduction of new codes in 2011. While femoroplasty and labral repairs continue to be performed more frequently since the introduction of those codes, acetabuloplasty has declined after an initial increase in incidence.
Specific age-related changes were also observed for FAI. Approximately 70% of all hip arthroscopies addressing FAI pathology between 2011 and 2014 were performed in patients under 50 years of age (Table III). Mild upward trends were observed across all ages.
Table III.
Incidence of FAI codes and ratio of labral repair (CPT 29916) to labral resection (CPT 29862) stratified by age (per 10 000)
| FAI Codes (per 10 000) |
Ratio (CPT-29916/29862) |
|||||
|---|---|---|---|---|---|---|
| Year | <30 | 30–50 | >50 | <30 | 30–50 | >50 |
| 2011 | 0.140 | 0.210 | 0.140 | 1.12 | 0.98 | 0.32 |
| 2012 | 0.170 | 0.230 | 0.240 | 2.63 | 1.89 | 0.71 |
| 2013 | 0.220 | 0.290 | 0.170 | 2.86 | 2.16 | 0.58 |
| 2014 | 0.200 | 0.310 | 0.230 | 2.25 | 1.60 | 0.71 |
| P valuea | <0.001 | <0.001 | <0.001 | |||
Ratio of > 1 signifies labral repair being performed more than labral debridement.
aComparing rate of change (2011-2014) for CPT-29916 versus CPT-29862.
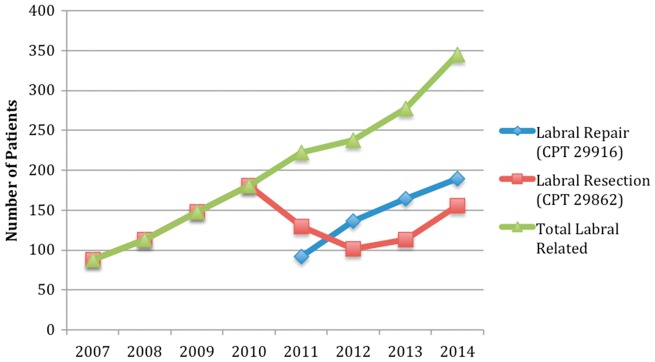
In regards to labral repair versus debridement, an increasing percentage of all hip arthroscopies included a labral repair through 2014 (Fig. 4). From 2011 to 2014, the ratio of labral repair to debridement in patients younger than 30 years and between 30 and 50 years increased with a ratio above 1.0 (thus more labral repairs than debridements) (Table III). In patients over the age of 50, debridement was the predominant treatment with a ratio less than 1.0, although the incidence of labral repair has increased in this older age group as well. Incidence rates were also found to be significantly higher for labral repair versus debridement between 2011 and 2014 for patients less than 30 years and between 30 and 50 years (Table III) (P < 0.001).
Fig. 4.
Number of patients undergoing labral repair and labral debridement by year. Labral surgery has continued to increase in incidence, with labral repair being performed more commonly than labral resection.
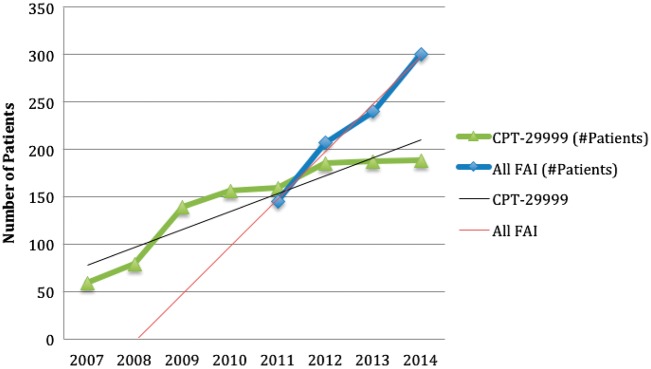
The incidence of CPT code 29999 (unlisted procedure, arthroscopy) increased by 76.6% from 2007 to 2014 (P < 0.001), although the majority of this increase was seen prior to 2011, as coding decreased 11.1% from 2011 to 2014 (Fig. 3). Starting in 2012, the number of patients coded with CPTs related to FAI pathology and labral repair exceeded the number of patients coded with CPT-29999 (Fig. 5). The rate of change of FAI codes between 2011 and 2014 (y = 50.1x − 102.4, R2 = 0.99) exceeded the rate of change for CPT-29999 between 2007 and 2011 as well as between 2011-2014 (y = 18.857x + 59.143, R2 = 0.86) (P < 0.01).
Fig. 5.
Number of patients with FAI-related codes compared to CPT–29999 (Unlisted). With the introduction of the FAI codes, the incidence of recorded FAI surgery has continued to rise. The use of unlisted codes in hip arthroscopy has also increased, although much less frequently, likely reflecting the development of new techniques that lack specific coding, such as capsular plication or closure, decompression of ischiofemoral space, sciatic nerve endoscopy and labral reconstruction, and performance of other procedures, such as iliopsoas lengthening, microfracture, trochanteric bursectomy and gluteus tendon repair.
DISCUSSION
This study adds to the growing literature endorsing a continued rapid increase in the number of hip arthroscopies being performed in the United States (Fig. 2) and provides new data suggesting an overall increase in complexity and diversity of hip arthroscopies. Our results agree with previous reports including Montgomery et al., who found an increase of 365% in the incidence of hip arthroscopies from 2004 to 2009 based on the UnitedHealth Payer database [2]. Sing et al. used the same database query to show a 150% percent change in incidence of hip arthroscopies from 2007 to 2011 [1]. Another study found an 18-fold increase between 1999 and 2009 using Part II of the American Board of Orthopaedic Surgery certification exam, but only a 230% change from 2007 to 2009 [4]. While the data from our study showed a total increase of 117%, less than that of prior studies, there was an increase in extended codes of 475%. This study similarly shows continuation of an upward trend and is the first to report on the CPT code changes made in 2011 from a national database. Moreover, our data is further validated by the observation of a slowing rate of growth consistent across all studies, which may explain our lower overall incidence rate.
The advance of the field of hip arthroscopy has afforded new indications and increased complexity of cases. When distinguishing between traditional and extended codes, we found a greater increase in extended codes compared to traditional codes following 2011 (Fig. 2). Whether these changes are truly a reflection of new decision making, improving skills and techniques of surgeons as this field continues to grow and evolve, or changes to coding structure is difficult to extrapolate. It is most likely a combination of many factors. For example, studies have suggested that although requiring a higher level of skill to perform, labral preservation is favorable to debridement for the prevention of progression of arthritis in younger patients [8, 9]. Larson and Giveans found that one year after labral refixation versus resection for the treatment of FAI, modified Harris Hip Scores (mHHS) scores were significantly higher in the refixation group [10]. This difference was even greater at longer-term follow-up [11]. Philippon et al. [12] also showed that labral refixation was an independent predictor of better outcomes for FAI surgery when compared with labral resection. The overall similar upward trend for labral repair compared to debridement in our study (Table III;Fig. 4) is further evidence that clinical decisions have followed evidence-based recommendations, especially when noting the age-related differences discussed previously. Additionally, as described by Beck et al. [13], labral chondral separation is more common in cam FAI, and therefore more likely amenable to repair, explaining the slightly higher association of repair than debridement with femoroplasty observed in our study.
A number of valuable trends were observed with regard to hip arthroscopy related to FAI pathology. For one, following the initiation of new coding in 2011, the number of FAI based codes (22914, 22915, 22916) has continued to rise. A similar trend has been found in the number of FAI publications per year, further supporting the rapid interest and increased understanding of this disease [14, 15]. Observed trends in coding also may reflect changes in decision making and surgical indications for FAI. Numerous studies have argued for intervention in younger patients prior to the development of joint space narrowing [16, 17]; our data reflects such recommendations with a clear majority of codes geared to FAI pathology under the age of 50 years. Alternatively, the increasing number of FAI surgeries may be the result of increased awareness of FAI, and thus appropriate diagnosis of hip pain in younger patients, as well as an increasing number of orthopaedic surgeons learning hip arthroscopy and advancing to become more comfortable with performing arthroscopic FAI surgery.
Data regarding CPT-29999 is difficult to interpret given the code’s inherent lack of specificity. We hoped to correlate the introduction of new codes in 2011 with a downtrend of CPT-29999 in subsequent years (Fig. 5). While we found that the coding of CPT-29999 associated with hip pathology slowed following 2011, FAI-related codes did not become dominant until 2012. This is likely, in part, explained by a lag in code use following introduction. We also recognize that the significantly higher growth of FAI-related surgery compared to the growth of CPT-29999 starting in 2011 (Fig. 5) cannot be explained solely by a conversion in coding practices. As such we believe this provides further evidence that FAI surgery is on the rise. Similarly, it is possible that the remaining regularity of CPT-29999 is due to a next generation of complex procedures that are not represented presently with available codes. For example, procedures such as capsular plication, which are becoming a routine component of hip arthroscopy, can be bundled with FAI codes or performed separately. Procedures such as labral reconstruction, capsular reconstruction, iliopsoas fractional lengthening, trochanteric bursectomy and iliotibial band plasty are procedures currently without CPT codes and thus would require a 29999 billing code. In all, trends of CPT-29999, while non-specific, may point to a shift in complexity of procedures and, indirectly, FAI-related pathology.
The data regarding coding practices and insurance coverage is also difficult to interpret. We found that a higher percentage of patients with private insurance received traditional codes compared to extended codes. However, this difference is likely explained by a higher percentage of patients associated with code CPT-29999 receiving coverage from Medicare. Interestingly, the highest percentage of patients with private insurance was observed with FAI only codes. As this is the first study to our knowledge to look at insurance practices with hip arthroscopy, further research is required to understand these findings. Regional differences were not observed between traditional and extended coding practices.
LIMITATIONS
Limitations in this study stem primarily from inherent deficiencies in using a national database registry. For example, we are limited by the specificity of available coding such as CPT-29862, which could include chondroplasty with or without an associated labral resection. However, we also recognize that the most common reason for hip arthroscopy is labral pathology (50%) [18] and that chondroplasty is readily performed with some concurrent procedure on the labrum. Therefore, we do not feel that the vagueness of coding in this particular case detracts from our comparisons with cases including CPT-29916 (labral repair) given that most CPT-29862 instances likely include the labrum.
We elected to use the Humana database given its diverse patient population including private and public payers as opposed to a strict Medicare/public based format. Unfortunately, previous work in this area used the UnitedHealth dataset, which is no longer offered by the data provider. We tried to standardize our data by converting to incidence per 10 000 patients, which would allow for comparison to prior work. While we do not believe this impacts the ability to extract trends, the incidence numbers vary from previous reports and thus may not fully reflect all payer systems. There may also be a geographical bias related to the different databases, including lack of international data. Moreover, incidence may not always be calculated similarly and therefore may not be amenable to direct comparison.
Our analysis also lacks functional outcomes for patients. Payer-based databases are uniformly deficient of this information. While we primarily attempted to address trends across the American population, we were not able to comment on whether particular procedures lead to better outcomes. Similarly, efficacy of individual surgical techniques can vary widely and lead to differences in costs and outcomes for patients that cannot be assessed with this data.
The database also does not account for laterality. As such, treatment of bilateral disease at the same or different time points would not be detected with our evaluation. However, while this may be a source of error in our data, it would lead to under-representation as we cannot isolate a single patient with two independent procedures. Therefore, we feel that any existing trends would still hold should this information become available.
Lastly, in order to safeguard patient confidentiality, the PearlDiver database does not provide patient numbers for categories with fewer than 11 patients. This limited our ability to analyse particular subsets of patients or those with less common problems.
CONCLUSION
The number of hip arthroscopies performed in the United States continues to rise and with an increased complexity and diversity of procedures. FAI-based procedures and labral repair are being performed more frequently in younger patients, likely reflecting both improved technical ability as well as adherence to current evidence-based research. While these findings are from the United States only, as new CPT codes are introduced, it will be increasingly important to monitor and understand the trends of patient care and surgical decision-making in order to accurately assess and benefit from outcome related research.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Sing DC, Feeley BT, Tay B. et al. Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy 2015; 31: 2307–13.e2. [DOI] [PubMed] [Google Scholar]
- 2. Montgomery SR, Ngo SS, Hobson T. et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy 2013; 29: 661–5. [DOI] [PubMed] [Google Scholar]
- 3. Bozic KJ, Chan V, Valone FH. et al. Trends in hip arthroscopy utilization in the United States. J Arthroplasty 2013; 28(8 Suppl.): 140–3. [DOI] [PubMed] [Google Scholar]
- 4. Colvin AC, Harrast J, Harner C.. Trends in hip arthroscopy. J Bone Joint Surg 2012; 94: e23.. [DOI] [PubMed] [Google Scholar]
- 5. Kelly BT, Williams RJ, Philippon MJ.. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med 2003; 31: 1020–37. [DOI] [PubMed] [Google Scholar]
- 6. Safran MR. Advances in hip arthroscopy. Sports Med Arthrosc Rev 2010; 18: 55.. [DOI] [PubMed] [Google Scholar]
- 7. Stevens MS, Legay DA, Glazebrook MA. et al. The evidence for hip arthroscopy: grading the current indications. Arthroscopy 2010; 26: 1370–83. [DOI] [PubMed] [Google Scholar]
- 8. Espinosa N, Rothenfluh DA, Beck M. et al. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am 2006; 88: 925–35. [DOI] [PubMed] [Google Scholar]
- 9. Krych AJ, Thompson M, Knutson Z. et al. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy 2013; 29: 46–53. [DOI] [PubMed] [Google Scholar]
- 10. Larson CM, Giveans MR.. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy 2009; 25: 369–76. [DOI] [PubMed] [Google Scholar]
- 11. Larson CM, Giveans MR, Stone RM.. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med 2012; 40: 1015–21. [DOI] [PubMed] [Google Scholar]
- 12. Philippon MJ, Briggs KK, Yen YM. et al. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg 2009; 91: 16–23. [DOI] [PubMed] [Google Scholar]
- 13. Beck M, Kalhor M, Leunig M. et al. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 2005; 87: 1012–8. [DOI] [PubMed] [Google Scholar]
- 14. Ayeni OR, Chan K, Al-Asiri J. et al. Sources and quality of literature addressing femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc 2013; 21: 415–9. [DOI] [PubMed] [Google Scholar]
- 15. Yeung M, Khan M, Schreiber VM. et al. Global discrepancies in the diagnosis, surgical management, and investigation of femoroacetabular impingement. Arthroscopy 2014; 30: 1625–33. [DOI] [PubMed] [Google Scholar]
- 16. Philippon MJ, Briggs KK, Carlisle JC. et al. Joint space predicts THA after hip arthroscopy in patients 50 years and older. Clin Orthop Relat Res 2013; 471: 2492–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Domb BG, Gui C, Lodhia P.. How much arthritis is too much for hip arthroscopy: a systematic review. Arthroscopy 2015; 31: 520–9. [DOI] [PubMed] [Google Scholar]
- 18. Harris JD, McCormick FM, Abrams GD. et al. Complications and reoperations during and after hip arthroscopy: a systematic review of 92 studies and more than 6,000 patients. Arthroscopy 2013; 29: 589–95. [DOI] [PubMed] [Google Scholar]