Abstract
Objective
To evaluate safety, pharmacokinetics and pharmacodynamics of anti-interferon (IFN)-γ monoclonal antibody AMG 811 in subjects with SLE without or with lupus nephritis (LN).
Methods
In this phase Ib, randomised, multiple-dose escalation study (NCT00818948), subjects without LN were randomised to subcutaneous AMG 811 (6, 20 or 60 mg) or placebo and subjects with LN were randomised to subcutaneous AMG 811 (20, 60 or 120 mg) or placebo every four weeks for three total doses. Outcomes included incidence of adverse events (AEs); pharmacokinetics; levels of serum proteins (CXCL-10, interleukin 18, monocyte chemotactic protein-1); changes in gene transcript profiles and clinical parameters (Safety of Estrogen in Lupus Erythematosus National Assessment-Systemic Lupus Erythematosus Disease Activity Index (SELENA-SLEDAI) scores, proteinuria, anti-double-stranded DNA (anti-dsDNA) antibodies, C3 complement, C4 complement).
Results
Fifty-six subjects enrolled (28 SLE without LN; 28 with LN). Baseline mean SELENA-SLEDAI scores were 2.2 and 12.0 for SLE subjects without and with LN, respectively. Most subjects reported an AE; no meaningful imbalances were observed between AMG 811 and placebo. Pharmacokinetic profiles were similar and mostly dose-proportional in subjects without or with LN. AMG 811 treatment reduced CXCL-10 protein levels and blood-based RNA IFN-γ Blockade Signature compared with placebo. Reductions were less pronounced and not sustained in subjects with LN, even at the highest dose tested, compared with subjects without LN. No effect on SELENA-SLEDAI scores, proteinuria, C3 or C4 complement levels, or anti-dsDNA antibodies was observed.
Conclusion
AMG 811 demonstrated favourable pharmacokinetics and acceptable safety profile but no evidence of clinical impact. IFN-γ-associated biomarkers decreased with AMG 811; effects were less pronounced and not sustained in LN subjects.
Trial registration number
NCT00818948; results.
Introduction
SLE is an autoimmune disease that affects multiple organs and presents with a variety of clinical manifestations.1 2 Lupus nephritis (LN) affects up to 60% of patients with SLE overall,3 with lower risk in patients of European genetic ancestry,4 and portends poor clinical outcomes as LN can lead to severe acute kidney injury and chronic kidney failure.5
Multiple lines of evidence in animal models and patients with SLE strongly support the role of interferon (IFN)-γ in the pathogenesis of SLE, and of LN in particular.6 In the MRL-Faslpr mouse, IFN-γ is required for lupus-like disease and blockade of IFN-γ shows beneficial effects.7 Similarly, in New Zealand Black (NZB)/New Zealand White (NZW) F1 mice, blockade or reduction of IFN-γ was beneficial.8 Deletion of a regulatory element in the 3′ untranslated region of the IFN-γ gene in mice leads to congenital overexpression of IFN-γ and development of serological and cellular features characteristic of SLE.9 Individuals treated with IFN-γ for several disorders (eg, bladder cancer, myeloproliferative disorders) developed or had potentiated autoimmune responses including SLE-like syndromes.10–12 Emerging human genetic information implicates IFN-γ in disease pathogenesis, with evidence that an IFN-γ +874 T/A polymorphism may play a significant role in modifying the risk of autoimmune diseases, including SLE, and that the IFN-γ gene is a genetic factor determining the histological phenotype of LN.13
IFN-γ or molecules that are upregulated by IFN-γ, such as IFN-γ-inducible protein 10 (CXCL-10), human leukocyte antigen (HLA) class II and neopterin, are present at increased levels in patients with SLE, including those with LN, and have been associated with disease activity and flares.14–20
AMG 811 is a fully human (IgG1) anti-IFN-γ antibody. In patients with mild-to-moderate SLE, single doses of AMG 811 normalised IFN-regulated gene expression, led to dose-related reductions in serum CXCL-10, and were well tolerated.21 22 The objective of this study was to evaluate safety, pharmacokinetics, pharmacodynamics and clinical parameters of multiple-dose administration of AMG 811 in SLE patients without or with LN.
Methods
Study design
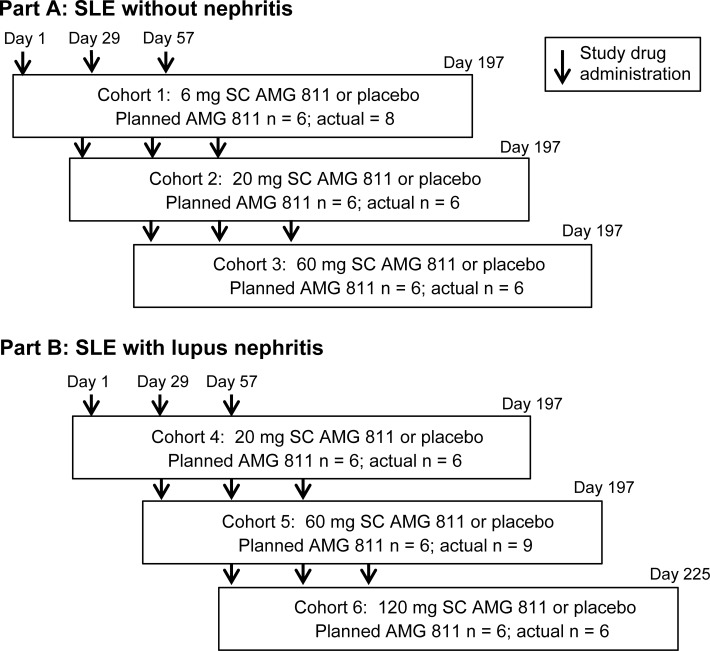
This was a phase Ib, randomised, double-blind, placebo-controlled, multiple dose escalation study conducted in SLE subjects without or with LN. SLE subjects without LN were randomly assigned to AMG 811 or placebo (planned 6:2 ratio) in cohorts 1–3 and received subcutaneous placebo or AMG 811 at doses of 6, 20 or 60 mg in part A (figure 1). SLE subjects with LN were randomly assigned to AMG 811 or placebo (planned 6:2 ratio) in cohorts 4–6 and received placebo or AMG 811 at 20, 60 or 120 mg administered subcutaneously in part B. All subjects received study drug (AMG 811 or placebo) every four weeks for a total of three injections. After completion of study drug administrations, subjects in cohorts 1–5 were followed for 5 months, and subjects in cohort 6 were followed for 6 months. Escalation to higher dose cohorts proceeded after the previous dose regimen was found to be safe and well tolerated by the Dose Level Review Team. Enrolment for LN cohort 4 was initiated after the first four subjects in cohort 2 (SLE subjects receiving 20 mg AMG 811 or placebo) had received at least two doses of study drug with no concerning safety issues. This study was conducted in accordance with the Declaration of Helsinki. The study protocol and consent forms were approved by the institutional review board at each study site. All subjects provided written informed consent before initiation of study-related procedures. This study was registered under the ClinicalTrials.gov identifier NCT00818948.
Figure 1.
Study schema. Arrows indicate times of study drug administration. SC, subcutaneous.
Subjects
Key inclusion criteria included age 18–70 years (inclusive); a diagnosis of SLE as defined by the American College of Rheumatology criteria with the presence of ANA at least 6 months before randomisation. Any concurrent SLE medications (eg, mycophenolate mofetil, azathioprine, leflunomide, methotrexate, antimalarials) were at a stable dose for ≥30 days before randomisation; concurrent prednisone was ≤20 mg/day (or equivalent) and for subjects without LN could be increased or decreased once by ≤5 mg/day within 30 days before randomisation. Subjects met current recommendations for immunisations.23 Subjects with LN were required to have biopsy-proven active disease within 18 months of randomisation according to WHO or International Society of Nephrology/Renal Pathology Society classification of SLE with glomerulonephritis class III or IV; urine protein:creatinine ratio >1 or 24-hour urine protein >1 g following ≥12 weeks of standard-of-care induction treatment with prednisone plus cyclophosphamide or mycophenolate mofetil, then maintained on prednisone at ≤20 mg/day (or equivalent) and mycophenolate or azathioprine. Exclusion criteria included any disorder that would interfere with study evaluations including unstable or severe disease; presence or history of vasculitis or active central nervous system lupus requiring therapy within 3 years; uncontrolled hypertension; low creatinine clearance (<50 mL/min); low haemoglobin levels, thrombocytopenia, neutropenia or low total white blood cell counts; poorly controlled diabetes; evidence of viral, bacterial or fungal infection within 30 days of randomisation or evidence of parasitic infestation; history of repeated infections or predisposition to infections; receipt of cyclophosphamide, cyclosporine, tacrolimus, sirolimus, intravenous immunoglobulins or plasmapheresis within 3 months of randomisation; or receipt of an investigational drug or device within 30 days or 5 half-lives of randomisation.
Study outcomes
Safety endpoints included the incidence of treatment-emergent adverse events (AEs), clinically significant changes in vital signs, clinical laboratory tests and the development of neutralising anti-AMG 811 antibodies. Severity of AEs was graded based on Common Terminology Criteria for Adverse Events V. 3.0.
Serum AMG 811 concentrations were measured and pharmacokinetic endpoints were analysed as previously described.21 Blood samples for pharmacokinetic testing were collected predose on day 1 and at 0.5, 1, 6, 24, 48 and 96 hours postdose, and on days 8, 15, 22, 29, 43, 56, 84 (end of study for cohort 1), 112 (end of study for cohort 2), 140 (end of study for cohort 3), 168 (end of study for cohort 4), 196 (end of study for cohort 5) and 225 (end of study for cohort 6).
Pharmacodynamic endpoints included levels of serum proteins CXCL-10, interleukin (IL)-18, monocyte chemotactic protein-1 (MCP-1), C3 complement, C4 complement and anti-double-stranded (ds) DNA antibodies and changes in the IFN-γ Blockade Signature (IGBS) transcript score. IL-18, CXCL10 and MCP-1 were measured as previously described.22 In addition to subjects from this study, SLE subjects enrolled in the AMG 557 single ascending dose and multiple ascending dose studies (protocols 20060132 and 20060169, respectively24) as well as commercially procured SLE samples were included in IL-18, CXCL-10 and MCP-1 testing. The IGBS was derived from results of two prior microarray experiments: (1) whole blood from healthy volunteers stimulated in vitro with IFN-γ was used to identify genes that were upregulated by IFN-γ and (2) whole blood from subjects in a phase Ia study22 was used to identify genes that were reduced following AMG 811 treatment among the genes that were identified in the first experiment. The IGBS is a weighted average of the top 10 genes identified in those experiments, including ANKRD22, GBP1, BATF2, ETV7, FCGR1B, ATF3, SERPING1, GBP5, PDK4 and CD274 (PD-L1), as previously described.22 These genes are all upregulated by IFN-γ and are downregulated by AMG 811. Clinical endpoints included changes in the Safety of Estrogen in Lupus Erythematosus National Assessment-Systemic Lupus Erythematosus Disease Activity Index (SELENA-SLEDAI, including the physician global assessment) and British Isles Lupus Assessment Group (BILAG) scores.
Statistical considerations
The planned sample size of 48 subjects (8 subjects per cohort) was based on practical considerations. No formal statistical hypotheses were tested in this study. Following review of the data, subjects receiving placebo were combined for the SLE without LN cohorts and separately for the LN cohorts.
The safety analysis set comprised all subjects who received study drug. Treatment-emergent AEs were assigned a body system and preferred term within a body system according to the Medical Dictionary for Regulatory Activities V. 17.0. The number and percentage of subjects reporting AEs were tabulated. No AEs of interest were prespecified for this study. Changes in 24-hour urine protein and urinary protein:creatinine ratio from baseline were summarised for subjects in part B. IGBS mean scores were estimated using a mixed effects linear model with factors for visit, dose and interaction between visit and dose; subject was included as a random effect.
Non-compartmental pharmacokinetic analyses were performed using Phoenix WinNonlin Professional, V.6.3 (Pharsight, St. Louis, Missouri, USA). Statistical analyses were performed using SAS V.9.2 and MATLAB release 2013b (MathWorks, Natick, Massachusetts, USA).
Results
Subjects
This study was conducted between 3 March 2009 (first subject enrolled) and 3 June 2014 (last subject follow-up) at 11 sites in the USA, Mexico, France, Malaysia and Hong Kong. A total of 28 SLE subjects without LN were enrolled in part A: 20 subjects received AMG 811 (8 subjects in cohort 1, 6 in cohort 2 and 6 in cohort 3) and 8 subjects received placebo. A total of 28 subjects with LN were enrolled in part B: 21 subjects received AMG 811 (6 subjects in cohort 4, 9 in cohort 5 and 6 in cohort 6) and 7 subjects received placebo. Of SLE subjects without LN, five subjects discontinued from the study, including two subjects on placebo (both due to administrative decision) and three on AMG 811 (due to administrative decision (n=2; cohort 1) and loss to follow-up (n=1; cohort 3)). Of subjects with LN, two subjects discontinued the study, including one subject on placebo and one on AMG 811 (cohort 6); both subjects discontinued because of an AE. All 56 subjects were included in the safety analysis set.
Most subjects were women (93%), and the duration of SLE ranged from 0.7 to 27.5 years (table 1). Subjects without LN had relatively inactive disease compared with subjects with LN based on SELENA-SLEDAI and BILAG scores: for example, baseline mean (SD) SELENA-SLEDAI scores were 2.2 (2.7) for all SLE subjects without LN and 12.0 (4.7) for all SLE subjects with LN. Most SLE subjects with LN (but not those without LN) were receiving prednisone and mycophenolate. For SLE subjects without LN on placebo and AMG 811, mean (SD) dose of prednisone was 2.5 (3.5) mg/day and 7.4 (6.0) mg/day, respectively. For subjects with LN on placebo and AMG 811, mean (SD) dose of prednisone was 11.3 (7.4) mg/day and 14.8 (8.2) mg/day, respectively.
Table 1.
Demographics and clinical characteristics at baseline
| SLE subjects without LN | SLE subjects with LN | |||
| Placebo (n = 8) |
AMG 811 (n = 20) |
Placebo (n = 7) |
AMG 811 (n = 21) |
|
| Age, mean years (SD) | 47.6 (11.6) | 37.6 (14.1) | 36.9 (11.7) | 30.0 (8.1) |
| Sex, no of female (%) | 8 (100) | 19 (95.0) | 4 (57.1) | 21 (100) |
| Race, n (%) | ||||
| White/Caucasian | 7 (87.5) | 10 (50.0) | 2 (28.6) | 6 (28.6) |
| Black/African-American | 1 (12.5) | 4 (20.0) | 0 | 0 |
| Hispanic/Latino | 0 | 5 (25.0) | 2 (28.6) | 12 (57.1) |
| Asian | 0 | 0 | 3 (42.9) | 3 (14.3) |
| Other | 0 | 1 (5.0) | 0 | 0 |
| Duration of SLE, mean years (SD) | 7.0 (3.2) | 6.5 (4.9) | 12.0 (5.5) | 6.2 (6.3) |
| ANA ≥ 1:40, n (%) | 8 (100) | 17 (85.0) | 6 (85.7) | 16 (76.2) |
| Anti-dsDNA ≥ 99 IU/mL, n (%) | 0 | 3 (15.0) | 4 (57.1) | 11 (52.4) |
| C3 below LLN, n (%) | 2 (25.0) | 3 (15.0) | 3 (42.9) | 11 (52.4) |
| C4 below LLN, n (%) | 0 | 2 (10.0) | 3 (42.9) | 5 (23.8) |
| BILAG global score, mean (SD) | 0.88 (0.64) | 2.50 (3.02) | 7.71 (2.93) | 8.76 (3.40) |
| SELENA-SLEDAI, mean score (SD) | 1.25 (1.49) | 2.60 (3.05) | 9.71 (4.68) | 12.71 (4.53) |
| Concomitant medications, n (%) | ||||
| Prednisone | 3 (37.5) | 8 (40.0) | 6 (85.7) | 21 (100) |
| Mycophenolate | 2 (25.0) | 2 (10.0) | 6 (85.7) | 15 (71.4) |
| Azathioprine | 0 | 0 | 3 (42.9) | 5 (23.8) |
| Methotrexate | 1 (12.5) | 1 (5.0) | 0 | 0 |
| Antimalarials | 6 (75.0) | 19 (95.0) | 3 (42.9) | 11 (52.4) |
ANA, antinuclear antibodies; BILAG, British Isles Lupus Assessment Group; dsDNA, double-stranded DNA antibodies; LLN, lower limit of normal; LN, lupus nephritis; SLE, systemic lupus erythematosus; SELENA-SLEDAI, Safety of estrogen in lupus erythematosus national assessment- Systemic Lupus Erythematosus Disease Activity Index.
Safety
Most subjects reported a treatment-emergent AE during the study (table 2). Most AEs were grade 2 or 3 and no deaths were reported.
Table 2.
Treatment-emergent AEs
| SLE subjects without LN | SLE subjects with LN | |||
| Placebo (n = 8) |
AMG 811 (n = 20) |
Placebo (n = 7) |
AMG 811 (n = 21) |
|
| All treatment-emergent AEs, n (%) | 7 (87.5) | 18 (90.0) | 6 (85.7) | 20 (95.2) |
| Grade ≥ 2 | 5 (62.5) | 9 (45.0) | 6 (85.7) | 16 (76.2) |
| Grade ≥ 3 | 1 (12.5) | 4 (20.0) | 4 (57.1) | 8 (38.1) |
| Grade ≥ 4 | 0 | 0 | 1 (14.3) | 1 (4.8) |
| Treatment-emergent SAEs, n (%) | 0 | 3 (15.0) | 2 (28.6) | 7 (33.3) |
| Fatal AEs | 0 | 0 | 0 | 0 |
| AEs reported by ≥ 15% of subjects, n (%) | ||||
| Arthralgia | 0 | 3 (15.0) | 0 | 7 (33.3) |
| Headache | 0 | 5 (25.0) | 0 | 6 (28.6) |
| Lupus nephritis worsening | NA | NA | 0 | 6 (28.6) |
| Cough | 0 | 3 (15.0) | 2 (28.6) | 5 (23.8) |
| Fatigue | 0 | 1 (5.0) | 0 | 5 (23.8) |
| Hypertension | 0 | 1 (5.0) | 1 (14.3) | 4 (19.0) |
| Mouth ulceration | 1 (12.5) | 1 (5.0) | 0 | 4 (19.0) |
| Nausea | 1 (12.5) | 1 (5.0) | 1 (14.3) | 4 (19.0) |
| Oral herpes | 0 | 1 (5.0) | 0 | 4 (19.0) |
| Pyrexia | 0 | 1 (5.0) | 1 (14.3) | 4 (19.0) |
| Sinusitis | 0 | 6 (30.0) | 0 | 0 |
| Urinary tract infection | 1 (12.5) | 3 (15.0) | 0 | 2 (9.5) |
AEs, adverse events; NA, not available; SAE, serious AEs.
Serious AEs (SAEs) were reported by three SLE subjects without LN on AMG 811 (subarachnoid haemorrhage, impetigo and migraine). SAEs were reported by two (28.6%) subjects with LN on placebo (hyperglycaemia, worsening of LN (leading to discontinuation from the study)) and by seven (33.3%) subjects with LN on AMG 811 (neutropenia; posterior reversible encephalopathy syndrome (PRES); hypokalaemia, salmonella gastroenteritis and worsening of LN; headache and vomiting; ascites, acute renal failure, cutaneous flare, hypotension, pancreatitis and pleural effusion (leading to discontinuation from the study); complicated migraine; and worsening of LN). The event of subarachnoid haemorrhage was in the setting of a motor vehicle accident approximately 4 months after the last administration of AMG 811. The subject with salmonella gastroenteritis was hospitalised for hypokalaemia approximately 1 month after receiving the first dose of AMG 811 and was discharged after appropriate treatment on the same day. This subject was subsequently hospitalised for fever approximately 1 month after administration of the second dose of AMG 811 and was diagnosed with disseminated Salmonella group D infection; the subject was hospitalised for 18 days. The subject with PRES was admitted to the hospital with cephalea (severe headache) approximately 2 months after receiving the third dose of AMG 811 and was diagnosed with PRES during hospitalisation; the subject was discharged from the hospital after 13 days.
No trends were observed in laboratory values or measured vital signs that suggested an impact of AMG 811 (data not shown). No subject developed anti-AMG 811 antibodies.
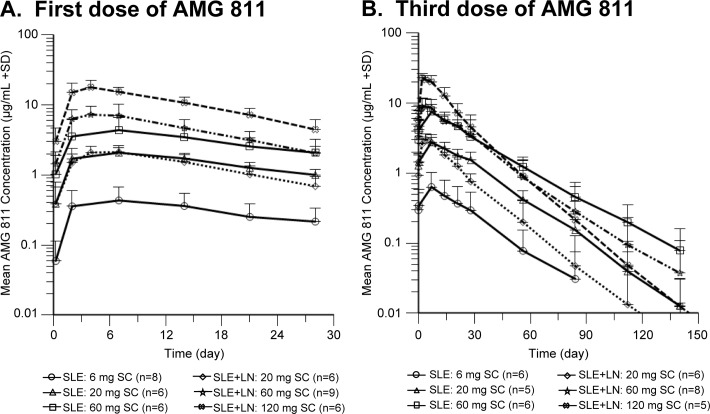
AMG 811 pharmacokinetics
Multiple-dose pharmacokinetics of AMG 811 showed generally similar exposures in SLE subjects without and with LN (figure 2). The median time to maximum AMG 811 serum concentration (tmax) ranged from 4.0 to 8.1 days following a single subcutaneous dose. There was minimal accumulation and the mean terminal half-life (t1/2) after the third dose was between 12 and 24 days. In SLE subjects without LN, exposures increased in an approximately dose-proportional manner across the 6–60 mg dose range. In subjects with LN, exposures increased in a slightly greater than dose-proportional manner across the 20–120 mg dose range. Although AMG 811 exposures, as measured by maximum serum concentration (Cmax) and area under the concentration time curve (AUC), appeared to be slightly higher (range 1.2-fold to 1.8-fold) in subjects with LN at the 60 mg dose after the first and third doses, the overall pharmacokinetic profiles of subjects with LN compared with those without LN were comparable with no apparent impact of renal damage or loss of renal function due to LN on AMG 811 pharmacokinetics.
Figure 2.
Pharmacokinetics of AMG 811 following the first and third doses. Serum AMG 811 concentrations are shown following the (A) first dose and (B) third dose of AMG 811. Data are shown as mean values, error bars represent SDs and the number of subjects per group is indicated in parentheses. LN, lupus nephritis; SC, subcutaneous.
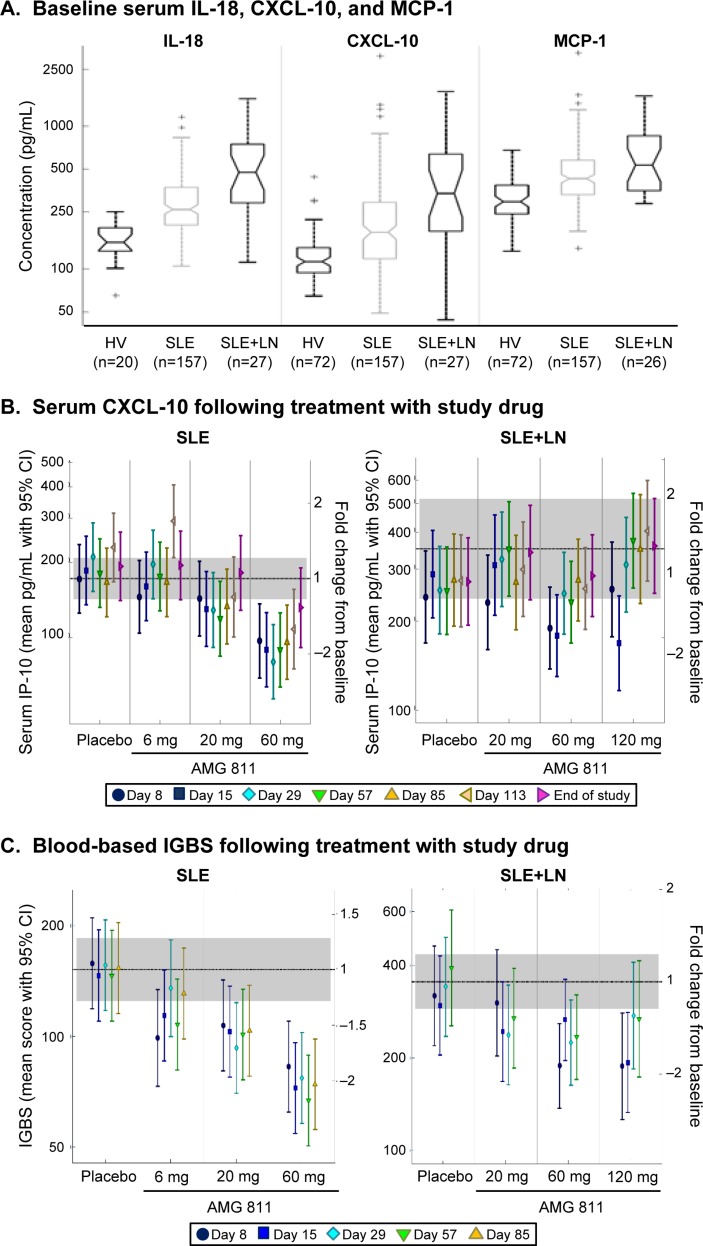
Biomarkers
Baseline serum levels of IL-18, CXCL-10 and MCP-1 were elevated in SLE subjects compared with healthy volunteers, with the highest levels observed in subjects with LN (figure 3A). Treatment with AMG 811 resulted in a dose-related reduction in mean serum CXCL-10 levels compared with placebo in SLE subjects without LN; the decrease was as low as twofold from baseline and was sustained for >85 days. In subjects with LN, the reduction was less pronounced, with an inconsistent and non-sustained decrease in CXCL-10, even with multiple administrations of a high dose of AMG 811 (120 mg) (figure 3B). There were no apparent changes in IL-18 or MCP-1 following multiple doses of AMG 811. AMG 811 treatment was associated with a significant dose-related reduction in the mean blood-based IGBS compared with placebo in SLE subjects without LN, down to twofold below the baseline level. The reduction in IGBS was less pronounced and not sustained in subjects with LN (figure 3C).
Figure 3.
Biomarker levels in SLE subjects without and with lupus nephritis (LN). Protein levels of (A) serum interleukin (IL)-18, interferon-γ-inducible protein 10 (CXCL-10) and monocyte chemotactic protein-1 (MCP-1) at baseline, (B) serum CXCL-10 following treatment and (C) blood-based IFN-γ Blockade Signature (IGBS) transcript score following treatment are shown. For box plots in (A), the centre horizontal lines represent median values, notches in the boxes represent an estimate of the uncertainty about the median, the upper and lower ends of the boxes represent the 75% and 25% quartiles, respectively, the whiskers represent the farthest observed data points within 1.5 times the IQR and the + signs represent outliers. In (B) and (C), error bars represent 95% CIs and the dashed horizontal lines represent mean baseline values. In (B) and (C), the shaded rectangle represents the 95% CI around the baseline values. All panels are shown on a log scale. HV, healthy volunteers; PD, pharmacodynamic.
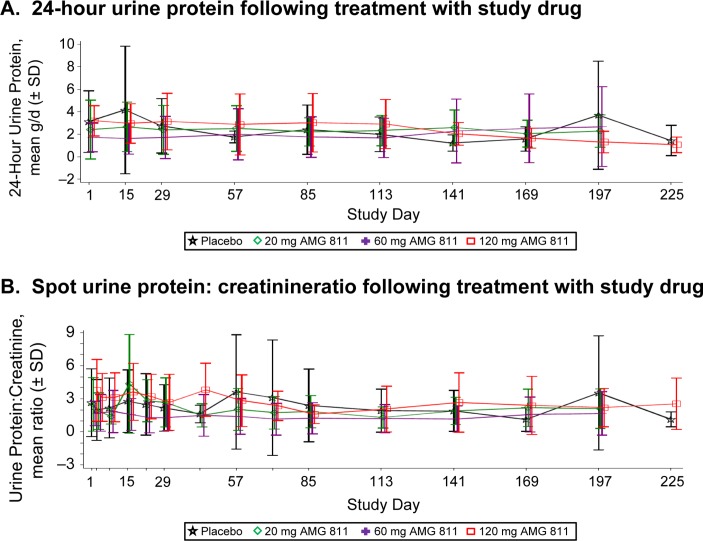
Clinical outcomes
In SLE subjects with LN, no effect on 24-hour urine protein (figure 4A) or urine protein:creatinine ratio (figure 4B) was observed. While normalisation of proteinuria was observed in some subjects, no treatment-associated effects were apparent when subjects were assessed in the aggregate or by dose level. No meaningful changes in levels of C3 complement, C4 complement or anti-dsDNA antibodies were observed with AMG 811 treatment (data not shown). Baseline mean (SD) SELENA-BILAG scores were 2.2 (2.7) for SLE subjects and 12.0 (4.7) for subjects with LN. There were no clinically meaningful differences in changes of SELENA-SLEDAI or BILAG scores between the AMG 811 and placebo groups at any postbaseline visit, though the baseline levels were low in the SLE subjects without LN (data not shown).
Figure 4.
Clinical outcomes in SLE subjects with lupus nephritis. Effects of placebo or AMG 811 on (A) 24-hour urine protein and (B) urine protein:creatinine ratio are shown. Error bars represent SDs.
Discussion
Dysregulation of the IFN-γ-related pathways in patients with SLE and normalisation of the IFN-γ-regulated genes with single-dose administration of AMG 81122 provided the rationale for this multiple ascending dose study in SLE subjects without or with LN. LN subjects with elevated proteinuria and up to 20 mg of prednisone and at least 1.5 g mycophenolate mofetil per day were included in part B of the study. The goal was to obtain safety and pharmacodynamic information about AMG 811 and to potentially obtain a preliminary indication of clinical effect. Although clinical trials in SLE have been marked by numerous failures and are notably difficult to execute (in large part due to the heterogeneity of the manifestations, complex composite clinical measures and strong influence of background corticosteroids and disease-modifying antirheumatic drugs), proteinuria represents an objective and clinically useful measure for LN. This study enrolled patients who were on mycophenolate mofetil for at least 12 weeks with persistent proteinuria, a predictor of long-term non-responsiveness to mycophenolate mofetil.25 We did not observe any indication of clinical impact with AMG 811 treatment in the LN cohorts as assessed by proteinuria, although the duration of treatment was short and the sample size was small. It should also be noted that the presence of renal scarring as the primary driver of proteinuria in some patients could confound the interpretation of these results. Although a renal biopsy was required with no evidence of significant chronicity, a relatively long interval was allowed between the renal biopsy and inclusion in the trial (up to 18 months) because of significant challenges in enrolment.
The overall safety profile of AMG 811 is considered acceptable. The interpretation of the safety results should take into account the small sample size of the cohorts and the inclusion of active patients on background immunosuppressants. Similar incidences of AEs in the treated and placebo arms were observed. The AMG 811-treated groups reported more SAEs than placebo-treated subjects, but the overall number of events was small. The cases of PRES and salmonella gastroenteritis are notable and both occurred in the setting of LN. Salmonella has been isolated in a significant proportion of subjects with adult-onset immunodeficiency associated with anti-IFN-γ antibodies.26 The number and nature of AEs may reflect the underlying disease state, and the contribution of additional immunosuppression through IFN-γ blockade will need to be better characterised through further study in a larger number of subjects.
Key differences in the pharmacodynamic effects were observed in the two populations of SLE subjects enrolled in the study. Cohorts 1–3 enrolled SLE subjects without LN, and the highest AMG 811 dose was 60 mg. The SLE subjects without LN in these cohorts had considerably milder disease than those in cohorts 4–6 of LN subjects, which was reflected in the SELENA-SLEDAI and global BILAG scores as well as by the background immunosuppressive drugs and dose of prednisone. In SLE cohorts 1–3, both the IGBS, a composite score reflecting the impact of inhibiting IFN-γ on gene expression, and serum CXCL-10 protein levels decreased approximately twofold from baseline. These decreases were sustained through at least day 85. In the LN cohorts, although the IGBS and CXCL-10 both decreased to approximately twofold below baseline at the 60 mg dose, the effect was not maintained over time despite continued dosing. Additionally, a plateau effect was observed as there was no further decrease of these markers at the higher dose of 120 mg, and maximal coverage may have been achieved with the 60 mg dose. Notably, the baseline IGBS was approximately twofold higher in the LN subjects compared with those without LN (as indicated by the left Y-axis and grey bars in figure 3C) and likely represent the more active disease documented in the patients with LN. Although there was a twofold decrease in IGBS score in AMG 811-dosed subjects in cohorts 5 and 6, the absolute score remained relatively high and comparable to the baseline levels of SLE subjects in cohorts 1–3. No changes in IL-18 or MCP levels were observed with AMG 811 treatment. Pharmacokinetic data do not support differences in AMG 811 pharmacokinetics between SLE subjects without or with LN. The relative failure to suppress CXCL-10 levels or IGBS score in subjects with LN suggests that there may be other pathways in addition to IFN-γ that are driving these dysregulated mediators in subjects with LN, and that targeting IFN-γ alone may be insufficient to produce a therapeutic impact in this subpopulation of patients with SLE.
This study provides a detailed characterisation of the pharmacokinetic and pharmacodynamic profiles of multiple-dose administration of AMG 811 across a broad dose range in two clinically distinct SLE subpopulations. Given the small size of the study, no firm conclusions can be drawn about the clinical impact of AMG 811 in SLE; however, sufficiently overcoming the IFN-related abnormalities associated with LN, in particular, with targeted inhibition of the IFN-γ pathway to achieve a clinical impact may be challenging.
Acknowledgments
The authors thank Dikran Toroser (Amgen) and Julia R Gage (on behalf of Amgen) for assistance with writing the manuscript.
Footnotes
Contributors: MJB, BAS, BLK and JBC contributed to the conception and design of the study. All authors contributed to the analysis and interpretation of the data. DAM, ZA, JS-G, JR-D, AK, CA, TMC and YBC contributed to patient data collection/data acquisition. All authors participated in revisions of the manuscript for intellectual content, and all authors approved the draft for submission.
Funding: This study was sponsored by Amgen.
Patient consent: Obtained.
Ethics approval: The study protocol and consent forms were approved by the institutional review board at each study site.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Please contact the study sponsor for details regarding current data availability and data sharing processes.
References
- 1.Rahman A, Isenberg DA. Systemic lupus erythematosus. N Engl J Med 2008;358:929–39. doi:10.1056/NEJMra071297 [DOI] [PubMed] [Google Scholar]
- 2.Kotzin BL. Systemic lupus erythematosus. Cell 1996;85:303–6. doi:10.1016/S0092-8674(00)81108-3 [DOI] [PubMed] [Google Scholar]
- 3.Hahn BH, McMahon MA, Wilkinson A, et al. American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res 2012;64:797–808. doi:10.1002/acr.21664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richman IB, Taylor KE, Chung SA, et al. European genetic ancestry is associated with a decreased risk of lupus nephritis. Arthritis Rheum 2012;64:3374–82. doi:10.1002/art.34567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoover PJ, Costenbader KH. Insights into the epidemiology and management of lupus nephritis from the US rheumatologist’s perspective. Kidney Int 2016;90:487–92. doi:10.1016/j.kint.2016.03.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Theofilopoulos AN, Dixon FJ. Murine models of systemic lupus erythematosus. Adv Immunol 1985;37:269–390. [DOI] [PubMed] [Google Scholar]
- 7.Balomenos D, Rumold R, Theofilopoulos AN. Interferon-gamma is required for lupus-like disease and lymphoaccumulation in MRL-lpr mice. J Clin Invest 1998;101:364–71. doi:10.1172/JCI750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmidt T, Paust HJ, Krebs CF, et al. Function of the Th17/interleukin-17A immune response in murine lupus nephritis. Arthritis Rheumatol 2015;67:475–87. doi:10.1002/art.38955 [DOI] [PubMed] [Google Scholar]
- 9.Hodge DL, Berthet C, Coppola V, et al. IFN-gamma AU-rich element removal promotes chronic IFN-gamma expression and autoimmunity in mice. J Autoimmun 2014;53:33–45. doi:10.1016/j.jaut.2014.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Machold KP, Smolen JS. Interferon-gamma induced exacerbation of systemic lupus erythematosus. J Rheumatol 1990;17:831–2. [PubMed] [Google Scholar]
- 11.Graninger WB, Hassfeld W, Pesau BB, et al. Induction of systemic lupus erythematosus by interferon-gamma in a patient with rheumatoid arthritis. J Rheumatol 1991;18:1621–2. [PubMed] [Google Scholar]
- 12.Wandl UB, Nagel-Hiemke M, May D, et al. Lupus-like autoimmune disease induced by interferon therapy for myeloproliferative disorders. Clin Immunol Immunopathol 1992;65:70–4. doi:10.1016/0090-1229(92)90250-R [DOI] [PubMed] [Google Scholar]
- 13.Miyake K, Nakashima H, Akahoshi M, et al. Genetically determined interferon-gamma production influences the histological phenotype of lupus nephritis. Rheumatology 2002;41:518–24. doi:10.1093/rheumatology/41.5.518 [DOI] [PubMed] [Google Scholar]
- 14.al-Janadi M, al-Balla S, al-Dalaan A, et al. Cytokine profile in systemic lupus erythematosus, rheumatoid arthritis, and other rheumatic diseases. J Clin Immunol 1993;13:58–67. doi:10.1007/BF00920636 [DOI] [PubMed] [Google Scholar]
- 15.Funauchi M, Sugishima H, Minoda M, et al. Serum level of interferon-gamma in autoimmune diseases. Tohoku J Exp Med 1991;164:259–67. doi:10.1620/tjem.164.259 [DOI] [PubMed] [Google Scholar]
- 16.Lim KL, Jones AC, Brown NS, et al. Urine neopterin as a parameter of disease activity in patients with systemic lupus erythematosus: comparisons with serum sIL-2R and antibodies to dsDNA, erythrocyte sedimentation rate, and plasma C3, C4, and C3 degradation products. Ann Rheum Dis 1993;52:429–35. doi:10.1136/ard.52.6.429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Narumi S, Takeuchi T, Kobayashi Y, et al. Serum levels of IFN-inducible protein-10 relating to the activity of systemic lupus erythematosus. Cytokine 2000;12:1561–5. doi:10.1006/cyto.2000.0757 [DOI] [PubMed] [Google Scholar]
- 18.Samsonov MY, Tilz GP, Egorova O, et al. Serum soluble markers of immune activation and disease activity in systemic lupus erythematosus. Lupus 1995;4:29–32. doi:10.1177/096120339500400107 [DOI] [PubMed] [Google Scholar]
- 19.Yokoyama H, Takabatake T, Takaeda M, et al. Up-regulated MHC-class II expression and gamma-IFN and soluble IL-2R in lupus nephritis. Kidney Int 1992;42:755–63. doi:10.1038/ki.1992.344 [DOI] [PubMed] [Google Scholar]
- 20.Munroe ME, Vista ES, Guthridge JM, et al. Proinflammatory adaptive cytokine and shed tumor necrosis factor receptor levels are elevated preceding systemic lupus erythematosus disease flare. Arthritis Rheumatol 2014;66:1888–99. doi:10.1002/art.38573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen P, Vu T, Narayanan A, et al. Pharmacokinetic and pharmacodynamic relationship of AMG 811, an anti-IFN-γ IgG1 monoclonal antibody, in patients with systemic lupus erythematosus. Pharm Res 2015;32:640–53. doi:10.1007/s11095-014-1492-2 [DOI] [PubMed] [Google Scholar]
- 22.Welcher AA, Boedigheimer M, Kivitz AJ, et al. Blockade of interferon-γ normalizes interferon-regulated gene expression and serum CXCL10 levels in patients with systemic lupus erythematosus. Arthritis Rheumatol 2015;67:2713–22. doi:10.1002/art.39248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Recommended adult immunization schedule, United States, October 2006-September 2007. MMWR 2006;55:Q1–Q4. [PubMed] [Google Scholar]
- 24.Sullivan BA, Tsuji W, Kivitz A, et al. Inducible T-cell co-stimulator ligand (ICOSL) blockade leads to selective inhibition of anti-KLH IgG responses in subjects with systemic lupus erythematosus. Lupus Sci Med 2016;3:e000146 doi:10.1136/lupus-2016-000146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Appel GB, Contreras G, Dooley MA, et al. Mycophenolate mofetil versus cyclophosphamide for induction treatment of lupus nephritis. J Am Soc Nephrol 2009;20:1103–12. doi:10.1681/ASN.2008101028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Browne SK, Burbelo PD, Chetchotisakd P, et al. Adult-onset immunodeficiency in Thailand and Taiwan. N Engl J Med 2012;367:725–34. doi:10.1056/NEJMoa1111160 [DOI] [PMC free article] [PubMed] [Google Scholar]