Abstract
Introduction
Adolescents and young adults (AYA) with cancer require dedicated clinical management and care. Little is known about the training and practice of European healthcare providers in regard to AYA and the availability of specialised services.
Methods
A link to an online survey was sent to members of the European Society for Medical Oncology (ESMO) and the European Society for Paediatric Oncology (SIOPE). The link was also sent to ESMO National Representatives and circulated to other European oncology groups. Questions covered the demographics and clinical training of respondents, their definition of AYA, education about AYA cancer, access to specialised clinical and supportive care, research and further education. Data from Europe were analysed by region.
Results
Three hundred tweenty two questionnaires were submitted and we focused on data from the 266 European healthcare professionals. Responses revealed considerable variation both within and between countries in the definition of AYA. Over two-thirds of respondents did not have access to specialised centres for AYA (67%), were not aware of research initiatives focusing on AYA with cancer (69%) and had no access to specialist services for managing the late effects of treatment (67%). The majority of the respondents were able to refer AYA patients to professional psychological support and specialised social workers. However, more than half had no access to an age-specialised nurse or specialised AYA education. Overall, 38% of respondents reported that their AYA patients did not have access to fertility specialists. This figure was 76% in Eastern Europe. Lack of specialised AYA care was particularly evident in Eastern and South-Eastern Europe.
Conclusion
There is important underprovision and inequity of AYA cancer care across Europe. Improving education and research focused on AYA cancer care should be a priority.
Keywords: cancer care, professional education, cancer In adolescents and young adults
Key questions.
What is already known about this subject?
Little is known about the training, practice and needs of European healthcare providers in relation to care of adolescents and young adults (AYA) with cancer.
What does this study add?
This survey revealed important underprovision and inequity of specialised AYA cancer care across Europe. This was particularly evident in Eastern and South-Eastern Europe.
How might this impact on clinical practice?
AYA with cancer require particular clinical management and care in relation to fertility preservation and other treatment sequelae. Improving care through education and research focused on AYA should be a priority for both European Society for Medical Oncology and European Society for Paediatric Oncology.
Introduction
Adolescents and young adults (AYA) are a distinct group at the interface between children’s and adult’s cancer services. Although the definition of AYA differs from country to country, a recent authoritative review of cancer epidemiology adopts the age limits of 15–39 years.1 In 2014, 31% of the population of Europe was aged between 15 and 39. Numbers were relatively evenly spread throughout this range, with 5%–7% of the population falling within each quintile.
Cancer in the AYA population is uncommon,2%–4% of all invasive malignancies overall depending on precise definitions. However, the annual incidence of cancer in the 15–39 years age group is significant and estimated to be 50–70 000 in Europe2 and 1 million worldwide.3 The incidence of cancer increases with age, from childhood to adulthood; between the ages of 15 and 30, cancer is 2.7 times more frequent than in the under 15 age group.4 More worrisome is the observation that the incidence of AYA cancer is rising for both males and females and in all age quintiles between 15 and 39 years.5 The distribution of cancer types among AYA differs from that in both older and younger people. The peak incidence of Hodgkin’s lymphoma, germ cell tumours and bone sarcomas occurs within the AYA range. Among 15–39-year-olds as a whole, the most frequent diagnoses are breast carcinoma (18% of cases), melanoma (14%), germ cell tumours (13%), carcinomas of the female genital tract (11%), thyroid cancer (7%) and Hodgkin and non-Hodgkin lymphomas (7% and 5%, respectively).1
Survival rates for AYA have not improved to the extent that they have for younger children or older adult cancer populations,1 6 but recent data have shown that the gap is reducing.2 Poorer outcomes in AYA (particularly those with colon or breast cancer) may be in part related to their biology, including different genomic risk, tumour histopathology, oncogenic pathway activation and sensitivity to chemotherapy.7 In addition, AYA patients tend to be diagnosed at later stages compared with older patients.8 9
Increasing numbers of AYA are long-term cancer survivors, given the high survival rate for AYA with cancer, and the fact that younger patients have low mortality from other diseases. Therefore, several issues arise in this group and include the effects of the disease and its treatment on fertility, cognitive function and mental health, and the risks of late-occurring adverse events such as cardiotoxicity, nephrotoxicity and second primary tumours.10 11 The specific circumstances and needs of AYA survivors are now being increasingly recognised and, internationally, various recent priorities have been set in this field. In the USA in 2013, an update meeting was held to review evidence, scientific data and priorities for individuals aged 15–39 at cancer diagnosis.12 A group of 60 experts identified the large increase in published research in 7 years, and prioritised next steps.
In 2016, the European Society for Medical Oncology (ESMO) and the European Society for Paediatric Oncology (SIOPE) recognised these issues and created a joint working group on Cancer in Adolescents and Young Adults. Its aims are to provide educational content to members interested in care of AYA with cancer, to increase wider professional awareness of the needs of AYAs with cancer and to cultivate sensitive collaborative relations between medical and paediatric oncologists as well as with other healthcare professionals involved in AYA cancer care. The results from an online survey reported here is among the first fruits of this collaboration in the effort to record the current situation of AYA cancer care in Europe. Our objectives were to record the current situation in AYA cancer care in Europe, to ensure the ESMO and SIOPE Joint Working Group provides educational content on AYA issues that is of interest to members of both societies, and finally to increase professional awareness of AYA cancer related issues.
Methods
The ESMO/SIOPE Working Group conducted an online survey in the last quarter of 2016. The questionnaire aimed to obtain data on the availability of the services specialised to AYA cancer care and clinical management, cancer risk assessment and gentic counseling management, educational activities available to healthcare providers interested in the AYA field, efforts to maintain the health of AYAs living after cancer and means of raising awareness and improving care and outcome. The demographic characteristics of the responders as well as their views on the age range that should be considered ‘AYA’ were also recorded.
The survey was freely available on the open-access ESMO website (to which the SIOPE site was linked) and a link sent by email to all members of ESMO and SIOPE. The link was also sent to ESMO National Representatives in each European country, so that it could be promoted nationally, and to several European oncology groups. It was also promoted at several conferences, such as the 48th Annual Congress of the International Society of Paediatric Oncology and the 1st Global Conference on Cancer in Adolescents and Young Adults. The survey was therefore not confined exclusively to people who had a known interest in AYA patients with cancer.
Data from Europe were analysed by region using χ2 and Fisher’s exact test. Analyses were performed using the statistical software R. European regions were defined according to the WHO geographical distribution.13
Results
Characteristics of respondents
From the outset, the survey was intended primarily as a way of obtaining information on the current situation in Europe relating to the care of AYA patients. However, the online availability of the questionnaire meant that responses were also spontaneously obtained from a small number of clinicians outside Europe (n=56) who were excluded from this analysis. There were 266 respondents from Europe, 55% women and 45% men (figure 1). The age distribution was as follows: 20–29 years, 11%; 30–39 years, 29%; 40–49 years, 26%; 50–59 years, 25%; 60 years or more, 9%. Almost half (48%) were medical oncologists and 21% paediatric oncologists. Eight per cent were in training, 5% were haematologists, 4% were radiation oncologists and 2% were surgical oncologists. The remainder were spread through other professional roles such as oncology nursing.
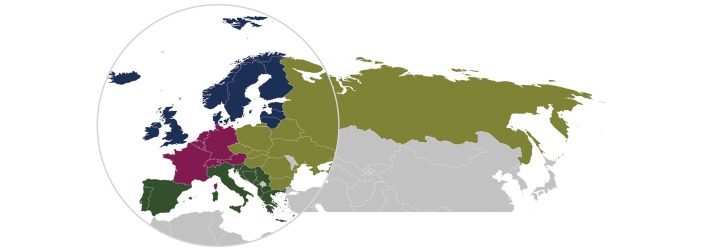
Figure 1.
European survey respondents by region. Region respondents, n (%): Eastern Europe 35 (13.2), Northern Europe 49 (18.4), Southern Europe 85 (32.0), Western Europe 97 (36.6), TT 266 (100). Eastern Europe: Belarus (n=2), Bulgaria (n=2), Czech Republic (n=3), Georgia (n=1), Hungary (n=3), Poland (n=5), Romania (n=8), Russia (n=5), Slovakia (n=3), Ukraine (n=3). Northern Europe: Denmark (n=5), Estonia (n=2), Finland (n=1), Iceland (n=1), Ireland (n=5), Latvia (n=2), Lithuania (n=4), Norway (n=1), Sweden (n=4), UK (n=24). Southern Europe: Albania (n=2), Andorra (n=1), Bosnia and Herzegovina (n=1), Croatia (n=6), Cyprus (n=3), Greece (n=27), Italy (n=15), Malta (n=2), Montenegro (n=1), Portugal (n=11), Serbia (n=3), Slovenia (n=2), Spain (n=9), (Former Yugoslavic Republic of) Macedonia (n=2). Western Europe: Austria (n=2), Belgium (n=13), France (n=26), Germany (n=37), Luxembourg (n=1), Netherlands (n=9), Switzerland (n=9).
The majority of respondents (52%) worked in general academic centres, with 19% in specialised cancer hospitals and 11% in paediatric hospitals. Sixty per cent had been trained to treat adult patients with cancer, 25% to treat paediatric cases and 15% both. There were wide differences in the number of patients aged 15–39 years that they had treated over the past year: Thirty-two per cent had treated between 1 and 10 such patients, 28% had treated 11–20, 17% had treated between 21 and 50 cases and 16% had more than 50. Given that patients aged 15 to 39 represent only 2% of the total cancer population, these data suggest that our respondents were predominantly those with a particular interest in the AYA cancer field. Twenty-four participants (9%) provided no further information. Data for the remaining questions are therefore based on 242 respondents.
Age range considered as AYA, management and clinical outcome
There was considerable variation both within and between countries in the age range considered as covered by the term ‘AYA’. In Belgium, for example, the ages thought appropriate to define the lower limit varied from 10 to 16 years, and the upper limit ranged from 24 to 35 years. In the case of Germany, the lower limit ranged from 10 to 18 years and the upper limit from 22 to 39 years. Overall, there was little consistency in defining the lowest age thought to define the start of the AYA group, but some consistency in seeing its upper limit as lying between 35 and 39 years.
Respondents were presented with three hypothetical patients—all aged 17 years—and asked whether (in their country) the doctor leading patient management would have been trained in adult or paediatric oncology. In the case of a patient with metastatic soft tissue sarcoma, 56% of respondents said that the lead clinician would have been paediatrics trained. This figure rose to 71% when the patient had acute lymphoblastic leukaemia, but fell to 44% when the patient had metastatic embryonal carcinoma of the testis.
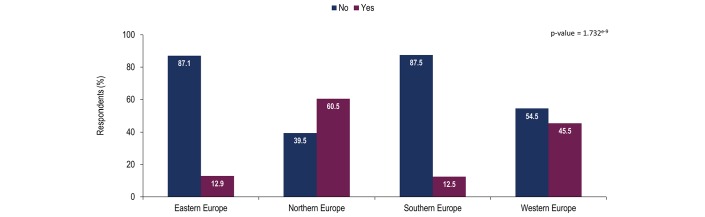
When asked if their patients could access to specialised services for AYA with cancer, or if such services were in development, 67% of respondents overall said they could not. This figure rose to 87% in Eastern and South-Eastern Europe. For Western Europe, the figure was 55%. In contrast, only 40% of respondents from Northern Europe said they did not have access to specialist services for AYA patients with cancer (figure 2).
Figure 2.
Awareness of respondents about the availability or development of specialised services for AYA where adult and paediatric cancer specialists work together to plan treatment and deliver care.
There was also a significant difference in knowledge about having access to such services according to the specialty of respondent: 62% of haematologists reported to have access to AYA services, 44% of paediatric oncologists but only 27% of medical oncologists (p=0.007 for interaction according to specialty). Hospital type and number of patients treated did not significantly influence perceived access to specialised services (p=0.50 and 0.15, respectively).
When asked whether they were aware of how trends in outcome for AYA with cancer compared with those for children or older adults, 62% said they were not.
Alarmingly, more than two-thirds of respondents were not aware of research initiatives, clinical trials or studies (near them or further afield) focused on the specific clinical, epidemiological or psychosocial features of AYA with cancer. This figure was highest among respondents from Eastern and Southern Europe (90% and 88%, respectively) and lowest (46%) among those from Northern Europe (test for interaction according to region, p<0.001). There were also major differences between specialties (p<0.001), with haematologists being the most likely (62%) to be aware of relevant clinical trials or studies, while this was true for only 38% of paediatric oncologists and 23% of medical oncologists.
Sources of support for AYA patients
Eighty-six per cent of respondents said their AYA patients had access to professional psychological support. In total, 78% of respondents said their AYA patients had access to a social worker and 76% had access to a physiotherapist or occupational therapist (PT/OT). In relation to services of particular relevance to young people, 54% of respondents said their AYA patients had access to a support group with other young people, 36% had access to an education or training mentor and 36% had access to age-specific specialist nurse.
Access to supporting specialists was significantly different across European regions but (as detailed in table 1) regional differences varied depending on the nature of the support. At least 50% of respondents across all four European regions reported that professional psychological support and access to social workers and PT/PO were available to AYA patients. According to respondents, education or training mentors were not generally available in Eastern, Northern and Southern Europe, and they were available in only 50% of cases in Western Europe. In Eastern and Southern Europe, access to an age-specific specialist nurse and a support group with other young people is available in fewer than 50% of cases, but the majority of AYA patients in Northern and Western Europe have such access. Social workers and age-specific nursing availability was significantly related to specialty, and access to PT/OTs and mentors varied by type of hospital. Access to a support group of other young people was significantly related to the number of patients treated by the respondent.
Table 1.
Access of AYA patients to professional supportive care, by European region
| Type of accessible support specialist (%) | Eastern Europe | Northern Europe | Southern Europe | Western Europe | |||||
| No | Yes | No | Yes | No | Yes | No | Yes | p Value | |
| Professional psychological support | 26 | 74 | 19 | 81 | 17 | 82 | 3 | 97 | 0.0011 |
| Social worker | 48 | 52 | 9 | 91 | 34 | 66 | 9 | 91 | <0.001 |
| Physiotherapist/occupational therapist | 29 | 71 | 23 | 77 | 35 | 65 | 14 | 86 | 0.0108 |
| Education or training mentor | 68 | 32 | 67 | 33 | 76 | 24 | 50 | 50 | 0.0041 |
| Age-specific specialist nursing | 68 | 32 | 49 | 51 | 90 | 10 | 47 | 53 | <0.001 |
| Support group with other young people | 52 | 48 | 19 | 81 | 66 | 34 | 40 | 60 | <0.001 |
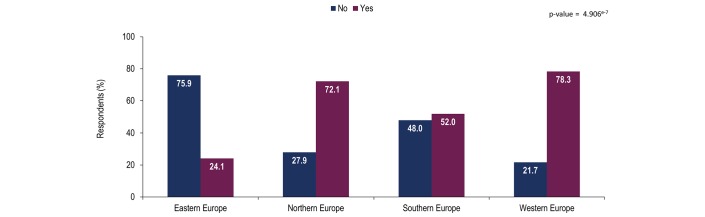
Long-term consequences of treatment and disease prevention
Sixty-two per cent of respondents said that their institution provided AYA patients with access to a fertility specialist who could be consulted in relation to their wishes about having children after cancer therapy. This figure was highest in Northern Europe (72%) and lowest in Eastern Europe (24%), representing a significant discrepancy across the four European regions (figure 3; p<0.001).
Figure 3.
Availability of a fertility specialist providing consultation to adolescents and young adults willing to have children after their cancer treatment at respondent’s institution.
Ninety-one per cent reported that patients who had had potentially cardiotoxic treatment were evaluated for modifiable cardiovascular risk factors such as high blood pressure, high cholesterol and obesity. Similar proportions of patients were advised on the importance of a healthy approach to maintain normal body weight, limit alcohol consumption, adopt a healthy diet, increase physical activity and enjoy the sun safely.
Sixty-nine per cent of respondents said they asked patients about their smoking habits at every visit, and 96% advised smokers to quit. Sixty-six per cent suggested referral to a smoking cessation service.
In relation to vaccination, only 6% of respondents said that they reviewed the vaccination status of all AYA patients at every visit, while 25% reviewed it annually and 50% occasionally. Seventy-eight per cent advocated human papilloma virus (HPV) vaccination for female patients aged 9–26 years, but only 20% advocated this for male patients in the same age range. This may reflect the fact that in many countries, HPV vaccination of boys is not part of the cancer prevention strategy.
Only one-third of respondents overall (33%) had access to a specialist service to which they could refer patients some years after completion of cancer treatment. This service was envisaged as providing education and minimising the risk of late effects or enhancing their management. Even in Northern Europe, only 47% of respondents reported that they had access to such a service.
Family history
Seventy-one per cent of respondents overall said they felt competent in using a family history to screen AYA patients for the more frequent hereditary syndromes that predispose to young-onset cancer. In addition, 89% had access to a genetic service for AYA patients with a family history that suggested a hereditary cancer syndrome. Among respondents in Northern and Western Europe, this figure was as high as 95%, falling slightly but not significantly to 83% and 81% in respondents from Eastern and Southern Europe, respectively.
Improving the service
Forty-four per cent of respondents said that their unit, hospital, region or country asked AYA patients about the quality of their care as part of an effort to improve services, but only 18% of healthcare professionals reported having access to education and training courses (online or face-to-face) that were focused on the management of AYA with cancer. Haematologists (31%) and paediatric oncologists (27%) were more likely to have such access, as were health professionals seeing more than 50 AYA patients per annum. In Northern Europe, this figure was only 39%.
When asked to rank their interest in educational activities that ESMO and SIOPE might jointly undertake, 53% gave their highest priority to activities that will assist them to improve cancer treatment for AYA. Survivorship issues for AYA after cancer, cancer risk assessment and prevention and basic science and clinical research into AYA with cancer received lower rankings overall, with top priority being assigned by similar proportions (30%–35%) of respondents (table 2).
Table 2.
Prioritisation of respondents’ interests in educational activities that the European Society for Medical Oncology and the European Society for Paediatric Oncology could offer together
| 1 (top priority) | 2 | 3 | 4 (least priority) | |
| Cancer treatment services and their quality improvement for AYA (%) | 53 | 19 | 17 | 11 |
| Survivorship health for AYA after cancer (%) | 35 | 27 | 20 | 18 |
| Cancer risk assessment and cancer prevention in AYA (%) | 31 | 27 | 23 | 19 |
| Basic science and clinical research about AYA cancer (%) | 30 | 33 | 21 | 16 |
AYA, adolescents and young adults.
Discussion
Cancer in AYA represents a unique disease constellation with distinct epidemiological, clinical and biological characteristics that resemble neither to childhood cancer nor cancer in older adults.1 2 5 7 The lower incidence of AYA-onset cancer, along with the paucity of data from cancer clinical trials in this age group, limit substantially our knowledge on this group of patients with cancer. In the present study, we tried to record the current status of AYA cancer care across Europe and to identify potential gaps in education, clinical services and psychosocial support availability for these patients. We found that over two-thirds of respondents did not have access to specialised centres for AYA (67%), were not aware of research initiatives focusing on AYA with cancer (69%) and had no access to specialist services for managing the late effects of treatment (67%). We also identified alarming rates of lack of specialised supporting services, with more than half of respondents reporting that they had no access to an age-specialised nurse or specialised AYA education, and 38% reported that their AYA patients did not have access to fertility specialists. This lack of services was particularly evident in Eastern and South-Eastern Europe.
Regarding age range considered as AYA, the data obtained from this survey broadly agree with those of Desandes and Stark who report AYA services in France and the UK as being directed at patients aged 15–24/25 years,1 while in Spain, the figures were 14–30 years, and in the Netherlands, 18–35 years.14 Similar variation in the definition of the patient age range has been documented in the e-Delphi survey, in which 75% agreement on a single definition of the patient age range within AYA cancer care has been reached.15 Since the optimal AYA age range remains an elusive topic on which to agree, we believe that treating physicians should treat according to the needs of the community they serve, ensuring that those who fall in the interface between children and adult service have their needs met.14
Our survey uncovered the lack of access of the responders to centres that specialise to treat AYA with cancer. The need for specific services for this population of patients has been appreciated in the replies to a recent questionnaire for AYA with cancer that has been designed by AYA oncology specialists in the UK and translated into 11 other European languages.16 Two-thirds of the 301 participants from 25 countries agreed with the need for AYA-specific services. Participants reported that important aspects of teenage and adolescents care included access to psychological care, youth workers and physiotherapists, higher levels of staffing and healthcare workers who understand the needs of this population and communicate effectively. Given the importance of psychosocial issues in AYA, it is comforting to identify that the majority of respondents were able to refer AYA patients to professional psychological support and specialised social workers. However, more than half had no access to an age-specialised nurse, specialised AYA education or a learning mentor, which is extremely important for these patients who feel that they lag behind in their education. Moreover, 38% of respondents said their AYA patients did not have access to fertility specialists. This figure rose to 76% in Eastern Europe. Given the youth of the population being treated, the latter findings are perhaps the most disturbing and identify a gap where future efforts from both societies should be concentrated.
Teenage and young adults with cancer have endorsed ‘monitoring after treatment’, ‘communication between professionals and young people’, ‘research about cancer’, ‘fertility preservation’ and ‘back to work/school’ as areas of priorities for future research.16 There is, therefore, an agreement with the interests of the responders to our survey about the educational activities that ESMO and SIOPE should offer together. In our ESMO and SIOPE joint Working Group, we are currently elaborating on how to increase professional awareness on AYA cancer issues to provide adequate educational material by means of E-learning, developing guidelines, practical guides for clinicians and congress activities such as educational lectures and interactive sessions focusing on AYA.
Intriguingly, there were certain marked differences between respondents in different branches of cancer medicine. Haematologists included in this survey were more likely than medical or paediatric oncologists to have patients who could access specialist services for AYA patients, and more aware of research involving the specific situation of AYAs with cancer. The proportion of respondents whose patients had access to fertility specialists was lowest among medical oncologists (54%), similar for radiation oncologists and haematologists (67% and 69%) and highest among paediatric oncologists (75%). Paediatric oncologists were also the most likely (46% vs an overall figure of 33%) to have access to a service that aimed to minimise and manage the late effects of cancer treatment. These findings may reflect the more specialised and multidisciplinary care of paediatric patients with cancer as compared with adults, given the fact that many paediatric cancer centres are more likely to offer a large number of support services, including psychologists, social workers, fertility specialists and access to cancer clinical trials.
Among the strengths of the current work are the international profile of respondents that covers all areas of Europe, and the representative nature of our sample that includes all professional disciplines that provide care to AYA with cancer, rendering our results reliable for ‘real world’ clinical practice. Notably, the questionnaire was available jointly by both ESMO and SIOPE, providing thus the opportunity for equal distribution of respondents. However, it should be noted that an inevitable selection bias should have occurred, given the fact that healthcare professionals with a special interest in AYA were more likely to undertake the questionnaire as compared with general specialists. In addition, as shown in figure 1, the number of responses was not equally distributed across European countries, with countries known to have more developed AYA services being more likely to have a higher number of responses, which may have introduced an additional bias.
Inclusion in the analysis of data from the 56 respondents who practised outside Europe at this stage would not be informative at statistical level, but probably makes little substantive difference to conclusions about underprovision of AYA cancer-specific services. Egypt (six respondents), India (four respondents) and Brazil (three respondents) were the countries that were most frequently represented. The remaining respondents were widely spread across countries of the USA, Africa, Middle East and Asia. Numbers were too few to allow subdivision by global region. However, the willingness of clinicians from outside Europe to respond to a survey focused on Europe shows global interest in issues relating to the better management of AYA patients with cancer. We plan to collaborate with colleagues from overseas and map the AYA care and needs in other continents.
This survey, while not definitive, is a helpful starting point. It suggests the need to expand awareness of the particular needs of AYA patients with cancer among health professionals and to encourage provision of specialist services that will improve their lives after cancer. There is considerable opportunity for ESMO and SIOPE to work together in raising the profile of AYA cancer-related issues, in providing educational materials (perhaps focused initially on those who express a particular interest in AYA patients) and in encouraging research.
Acknowledgments
The authors and the ESMO/SIOPE AYA Working Group gratefully acknowledge the assistance of Dr Fatima Cardoso (Chair of the ESMO National Representatives Committee), Nicola Latino, Roberta Candiani, Gracemarie Bricalli, Klizia Marinoni (ESMO staff members) and Giulia Petrarulo (SIOPE staff member). Rob Stepney (medical writer, Charlbury, UK) and Gaia Piraccini (MEDERIS, Ruvigliana, Switzerland) assisted in preparation of initial draft of the manuscript. Both were funded by ESMO. We also thank the following respondents who agreed to release of their names: Abdelmalik N, Agarwal S, Agerbaek M, Alhumiqani A, Andreadou A, Androulakis N, Artac M, Aurer I, Ayachi S, Bajciova V, Baka M, Baker J, Bamias A, Bardi E, Bebek M, Bertolini P, Beslija S, Bironzo P, Boissel N, Bokun J, Boyle H, Bozovic I, Brice P, Brummel B, Bult M, Bunskoek S, Calvagna V, Capela A, Castanon E, Castro D, Ceballos I, Cevallos-Reyna N, Chansriwong P, Chiriac V, Chitalkar P, Chitic M, Choneska-Jovanova B, Claici C, Codacci-Pisanelli G, Collard O, Condorelli R, Cony-Makhoul P, Corradini N, Cruz M, David C, De Araujo R, de Azambuja E, de Ville M, Deo R, Dewart J, Diamantopoulos N, Dragomit M, Dudzisz-Sledz M, Duhoux F, Duran I, Durbaku A, Durutovic I, Ehlert K, Elme A, Elnagar U, Erdlenbruch B, Escherich G, Espirito-Santo J, Evangelou G, Ferrari V, Fernandes J, Fletcher A, Flippot R, Foukakis T, Fountzilas C, Frakulli R, Friedrich-Classen C, Galea N, Galvez-Montosa F, Gander M, Ganser A, Gaspar N, Georgoulias V, Gil-da-Costa MJ, Gleeson J, Gofti-Laroche L, Gouda M, Greene H, Gruettner HP, Harris F, Harttrampf A, Hasnere S, Herceg-Horvatic G, Hindi N, Hockings H, Htay S, Huguet F, Inomistova M, Jamnasi J, Kabickova E, Kamposioras K, Karamitrousis V, Kasper B, Kävrak Salim D, Kiladze I, Kisialeu L, Klouvas G, Kölzer B, Komarov Y, Kontopodis E, Kontos M, Korobeinikova E, Koskela K, Kosmidis H, Kudaba I, Kühnle I, Kuzmenko V, Lahmar C, Landaverde D, Langenaeken C, Lanznaster J, Laurence V, Levva S, Longo F, Luis M, Lykka M, Maass E, Mallaev M, Manir K, Marec-Berard P, Marinello A, Marques T, Martinova K, Massard C, Mauz-Koerholz C, Mazzotta M, McCabe M, Meattini I, Merki R, Mermershtain W, Milanovic N, Milde T, Mishinkin P, Molina A, Morales M, Moryl-Bujakowska A, Mostafa A, Muhammed A, Müller B, Nezha T, Nosworthy A, O'Donnell D, Obeng P, Olsson M, Omar S, Padrik P, Padua T, Papamichael D, Parvu D, Paydas S, Petrova M, Pfitzner-Dempfle S, Pourtsidis A, Pracht M, Prevezanou M, Rahim K, Rascon J, Rauh S, Razi E, Renard M, Ribeiro J, Riis-Olsen P, Riotorto R, Rischewski J, Rodehüser M, Romanidou O, Romeira D, Rubovsky G, Salim G, Scepanovic D, Schilling G, Schultheis B, Schur S, Serescu R, Serrano A, Setola E, Sheikh A, Sianou KP, Sibon D, Simon A, Soares M, Sohaib A, Soumeyya G, Sousa B, Specht L, Srinivas-Maddali L, Stein A, Stevens M, Sukor S, Suttorp M, Sverrisdottir A, Tamamyan G, Torday L, Tryakin A, Tsyhyka D, Tupayachi R, Turobova T, Vaitiekus D, Van Belle S, van der Graaf W, van Hoef M, Vansteene D, Vardakis N, Veramo J, Vieth S, Vitiello PP, von Bueren A, Westermann A, White J, Williams D, Wong A, Yaniv I, Yildirim A, Younger E, Zborovskaya A.
Footnotes
Contributors: ES conceived the idea, drafted the survey, analysed the data and drafted the manuscript. DS drafted the survey. KM analysed the data. SJ and SE coordinated the circulation of the survey, collected the data and assisted in the preparation of the manuscript. JYD, GM and SB coordinated the work. All authors edited and approved the manuscript.
Competing interests: DS: Research support from the National Institute for Health Research, Cancer Research UK, the Teenage Cancer Trust, Pharmamar and Astra-Zeneca. SB: Fees for Advisory Boards from Pfizer, Bayer, Lilly, Novartis, Isofol. FAP: Fees from Roche, Astra Zeneca, Clovis and Ipsen. ES, LB, SJ, KM, J-YD, GM, SE: No relevant disclosures to declare.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1.Desandes E, Stark DP. Epidemiology of adolescents and young adults with cancer in Europe. Prog Tumor Res 2016;43:1–15. 10.1159/000447037 [DOI] [PubMed] [Google Scholar]
- 2.Trama A, Botta L, Foschi R, et al. Survival of European adolescents and young adults diagnosed with cancer in 2000-07: population-based data from EUROCARE-5. Lancet Oncol 2016;17:896–906. 10.1016/S1470-2045(16)00162-5 [DOI] [PubMed] [Google Scholar]
- 3.Barr RD, Ferrari A, Ries L, et al. Cancer in adolescents and young adults: a narrative review of the current status and a view of the future. JAMA Pediatr 2016;170:495–501. 10.1001/jamapediatrics.2015.4689 [DOI] [PubMed] [Google Scholar]
- 4.Smith AW, Seibel NL, Lewis DR, et al. Next steps for adolescent and young adult oncology workshop: An update on progress and recommendations for the future. Cancer 2016;122:988–99. 10.1002/cncr.29870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birch JM, Alston RD, Kelsey AM, et al. Classification and incidence of cancers in adolescents and young adults in England 1979-1997. Br J Cancer 2002;87:1267–74. 10.1038/sj.bjc.6600647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bleyer A, O'Leary M, Barr R, et al. Cancer epidemiology in older adolescents and young adults 15 to 29 years of age, including SEER incidence and survival: 1975 - 2000. Bethesda, MD: National Cancer Institute, 2006:06-5767. [Google Scholar]
- 7.Bleyer A, Barr R, Hayes-Lattin B, et al. The distinctive biology of cancer in adolescents and young adults. Nat Rev Cancer 2008;8:288–98. 10.1038/nrc2349 [DOI] [PubMed] [Google Scholar]
- 8.Hubbard JM, Grothey A. Adolescent and young adult colorectal cancer. J Natl Compr Canc Netw 2013;11:1219–25. 10.6004/jnccn.2013.0144 [DOI] [PubMed] [Google Scholar]
- 9.Steele SR, Park GE, Johnson EK, et al. The impact of age on colorectal cancer incidence, treatment, and outcomes in an equal-access health care system. Dis Colon Rectum 2014;57:303–10. 10.1097/DCR.0b013e3182a586e7 [DOI] [PubMed] [Google Scholar]
- 10.Skinner R, Mulder RL, Kremer LC, et al. Recommendations for gonadotoxicity surveillance in male childhood, adolescent, and young adult cancer survivors: a report from the international late effects of childhood cancer guideline harmonization Group in collaboration with the PanCareSurFup consortium. Lancet Oncol 2017;18:e75–90. 10.1016/S1470-2045(17)30026-8 [DOI] [PubMed] [Google Scholar]
- 11.Keegan THM, Bleyer A, Rosenberg AS, et al. Second primary malignant neoplasms and survival in adolescent and young adult cancer survivors. JAMA Oncol 2017;20 10.1001/jamaoncol.2017.0465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith AW, Seibel NL, Lewis DR, et al. Next steps for adolescent and young adult oncology workshop: An update on progress and recommendations for the future. Cancer 2016;122:988–99. 10.1002/cncr.29870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. http://www.euro.who.int/en/countries (assessed 29 Jul 2017).
- 14.Stark D, Brugieres L, Dirksen U, et al. Teenagers and young adults with cancer in Europe: from national programmes to a European integrated coordinated project. Eur J Cancer Care 2016;25:419–27. 10.1111/ecc.12365 [DOI] [PubMed] [Google Scholar]
- 15.Pini SA, Gibson F, Fern LA, et al. Multi-professional perspectives on adolescent and young adult oncology across Europe: an e-Delphi survey. J Adolesc Young Adult Oncol 2017;6:178–85. 10.1089/jayao.2016.0051 [DOI] [PubMed] [Google Scholar]
- 16.Jones LJ, Pini SA, Morgan SJ, et al. How do teenagers and young adults with cancer experience their care? a European survey. J Adolesc Young Adult Oncol 2017;6:102–10. 10.1089/jayao.2016.0011 [DOI] [PubMed] [Google Scholar]