Abstract
Context
The severity of Sjögren’s syndrome has been evaluated using a wide variety of clinical measures and patient-reported outcomes (PROs). This may contribute to the lack of clarity concerning the burden of Sjögren’s from the patient perspective.
Objective
To perform a comprehensive peer-reviewed literature analysis of the patient aspects of Sjögren’s, focusing on PROs, to investigate the complexity underlying the evaluation of the syndrome and to elucidate the discordance between the different measures.
Methods
We searched Embase for articles published between January 2005 and September 2015. Research articles, clinical and diagnostic reviews, and validation studies with a focus on patient aspects of Sjögren’s were selected as the primary information source.
Results
157 articles met the eligibility criteria. A wide variety of assessment measures used to evaluate glandular, extraglandular and functional domains were observed. Many different, non-validated Visual Analogue Scales, with a wide range of anchor words, were used in the quantification of Sjögren’s disease burden, impeding comparisons between studies. Relatively few clinical trials of drug therapies used validated scales: European League Against Rheumatism Sjögren’s Syndrome Patient Reported Index was used most often for symptom assessment and 36 Item Short Form Survey for quality of life (QoL).
Conclusion
A wide range and diversity of measures are used to evaluate the patient burden of Sjögren’s; most are not validated for use in this disease. PRO endpoints, validated specifically in Sjögren’s, that demonstrate improvement are needed. These measures should focus on QoL aspects important to patients and will most likely involve gauging change in function rather than patient-reported symptoms.
Keywords: Sjögren’s Syndrome, Patient Perspective, Outcomes Research, Quality of Life
Key messages.
What is already known about this subject?
The clinical burden of Sjögren’s has been well described and measured using validated clinical scales; however, the patient burden of Sjögren’s has not yet been fully elucidated.
This observation regarding patient burden is strengthened by studies in Sjögren’s which have revealed a disconnection between clinician-reported and patient-reported outcomes (PROs).
What does this study add?
This study shows the need for PRO endpoints validated specifically in Sjögren’s that can demonstrate improvement in a clearly defined patient subset.
Such measures should focus on the quality-of-life aspects that are important to patients and will most likely involve gauging change in function rather than patient-reported symptoms.
How might this impact on clinical practice?
Clear and well-defined PROs in Sjögren’s will enable a more personalised approach to therapy in which glandular, systemic symptoms and functioning, important to the patient, as well as patient well-being, will play a more central role in successful drug therapy.
Introduction
Sjögren’s syndrome: disease description and patient burden
Sjögren’s is a female-predominant systemic autoimmune rheumatic disease that affects the entire body. Symptoms can include extensive dryness, profound fatigue, chronic pain and neuropathies, with complications including major organ involvement and lymphoma.1–4 After rheumatoid arthritis (RA), Sjögren’s is considered to be the most common rheumatic autoimmune disorder,1 5 with reported prevalence rates around the world ranging from 0.03% in Japan and 0.09% in Greece to 2.7% in Sweden.3 It should be noted, however, that reported prevalence rates vary widely with regard to geographical region and the classification criteria used.3
The traditional classification of Sjögren’s as primary or secondary, dependent on the absence or presence of other major autoimmune diseases (eg, RA, systemic lupus erythematosus), may be obsolete, meaning that a diagnosis of Sjögren’s should be made for all patients fulfilling consensus criteria, irrespective of the presence of comorbidities.6 This approach towards a single, unifying definition of Sjögren’s is supported by the Sjögren’s Syndrome Foundation (SSF).7
The manifestations of Sjögren’s range from classic symptoms of dryness throughout the body (eyes, mouth, sinuses, oesophagus, gastrointestinal (GI) tract, lungs, skin and vagina), and extraglandular manifestations resulting from infiltration of lymphocytes into organs (eg, liver, kidney), to more severe extra-epithelial manifestations resulting from immune complex deposition in the tissues (eg, glomerulonephritis, peripheral neuro-pathy).1–4 8 Up to 70% of patients with Sjögren’s report debilitating fatigue,9 10 and a significantly increased prevalence of depression has been reported among female patients compared with controls.11
A serious complication of Sjögren’s linked with increased mortality is the elevated risk of lymphoma. Patients with Sjögren’s have been reported to have up to a 6.5%–16% increased risk of developing non-Hodgkin’s lymphoma12 13 and a 1000-fold increased risk of developing parotid gland marginal zone lymphoma.13
Challenges for the diagnosis of Sjögren’s
Diagnosing Sjögren’s presents many challenges related both to the different classification criteria that have been used and to the wide range of signs and symptoms and their similarities with signs and symptoms associated with other diseases. Up to now, several classification systems have been used, with the 2002 American and European Consensus Group being currently the most widely used, although classification criteria continue to evolve with collaborations between international Sjögren’s and Rheumatologic Societies proposing new criteria.14 15 The latest classification criteria for Sjögren’s, jointly approved by the American College for Rheumatology and the European League Against Rheumatism (EULAR), were published recently.16
While patients often present with classic symptoms of dryness, others present with systemic manifestations. Peripheral neuropathies have been shown to be the presenting symptom in 25% of patients with Sjögren’s.17 In one study of patients with Sjögren’s-associated neuropathy, most (93%) had clinical manifestations of neuropathy that preceded either the development of sicca symptoms or laboratory findings consistent with Sjögren’s.18 Younger patients are more frequently diagnosed on the basis of systemic involvement (eg, parotitis, peripheral neuropathy and arthralgia), and are less likely to have classic sicca symptoms.19 20 All of the above challenges can lead to lack of diagnosis or misdiagnosis, or to delays in diagnosis, which have been reported to range from 3 to 11 years.21 The SSF 5-year Breakthrough Goal to shorten the time to diagnose Sjögren’s by 50% in 5 years will have reduced the time from 4.7 years in 2012 to 3 years by the end of 2016 (personal communication).
Patient-reported outcomes
In recent years, there has been a growing trend towards patient-centred care (ie, determining what is important from the patient’s perspective) as a means to improve the quality of healthcare and ensure the provision of value-based medicine. The Food and Drug Administration (FDA) recommends that patient-reported outcome (PRO) instruments be used to assess efficacy in clinical trials as some effects of an illness or treatment can only be known to the patient. It emphasises, however, that the adequacy of any PRO instrument (as a measure to support medical product labelling claims) depends on whether its characteristics, conceptual framework, content validity and other measurement properties can be shown to be satisfactory.22 Development of a valid PRO instrument is grounded in a foundational understanding of the experiences of the patients themselves. This framework, known as content validity, is achieved by patient interviews and focus groups which lead to the concepts of interest and ultimately the exact question(s) that comprise an instrument. Further construct validity is demonstrated through assessment of correlation with other ‘gold standard’ instruments measuring similar concepts, and finally, assessment of the measurement properties of the instrument (eg, reliability and responsiveness) completes the validation steps.23
Measurement of patient-reported symptoms in Sjögren’s
The measurement of patient-reported symptoms in Sjögren’s has evolved since the first consensus-building conference of specialists in 2000 identified the key features of the disease that they felt were important to include in a disease-specific measurement instrument.24 Subsequent to this, from the patient perspective, the Profile of Fatigue and Discomfort (PROFAD) and Sicca Symptoms Inventory (SSI) were developed which, when used together, encompassed 64 individual questions assessing the patient’s worst symptoms over the past 2 weeks related to eight domains (physical fatigue, mental fatigue, arthralgia, vascular discomfort, and oral, ocular, cutaneous and vaginal dryness) with each question being rated on a 0–7 numerical rating scale.25 26 Due to the perceived burden of a lengthy questionnaire, the questions were consolidated to shorten the PROFAD-SSI to 19 questions covering the same eight domains as the original. This was further reduced to a shortened SSI (10 questions) and five individual Visual Analogue Scales (VAS) assessing the worst dryness symptoms (overall dryness, dry mouth, dry eyes, dry skin, vaginal dryness) over the past 2 weeks.27 This finally culminated in the development of the EULAR Sjögren’s Syndrome Patient Reported Index (ESSPRI), which was further condensed to three numeric rating scales (0–10) assessing overall severity of dryness, fatigue and pain over the past 2 weeks. The three individual questions of the ESSPRI were found to be strongly correlated with their corresponding domain scores of the PROFAD and SSI.28
While reporting of symptoms directly from the patient’s perspective is recognised as important in Sjögren’s, there have only been weak associations found between patient-reported symptoms of dry eyes and dry mouth and objective measures of the corresponding gland functions.25 29 Similarly, the ESSPRI has been shown to have low correlation with its corresponding disease activity measure ESSDAI (EULAR Sjögren’s Syndrome Disease Activity Index), suggesting that they are two complementary components.30 While ESSPRI and ESSDAI accurately measure Sjögren’s severity from patient and physician perspectives, respectively, they do assess different constructs. Consequently, there is discordance between them such that severity according to one scale does not necessarily correspond to severity according to the other scale.
Rationale and objectives
The range and heterogeneity of measures used to evaluate the patient burden of Sjögren’s has not been investigated in depth.
The objectives of this analysis were twofold: (1) to perform a comprehensive literature analysis of the patient aspects of Sjögren’s, focusing on patient outcomes and the measures used to evaluate them, and (2) to investigate the complexity underlying the evaluation of Sjögren’s and elucidate the discordance between different measures.
Methods
We performed a search of Embase using the following search string, aiming to identify original clinical and observational research papers and review articles that included patient-reported measures of the patient burden of Sjögren’s:
‘sjoegren syndrome’/mj AND (‘quality of life’ OR qol OR ‘patient reported’ OR burden OR functional OR mental OR preference OR satisfaction OR attitude OR expectations OR ‘unmet need’ OR scale OR measure OR psychometric OR caregiver OR ‘standard of care’ OR cost OR economic OR productivity OR absenteeism OR ‘medical leave’ OR hospitali* OR disabl*) AND [humans]/lim AND [english]/lim AND (2005–2015)/py AND (article/it OR ‘article in press’/it OR review/it).
During the search, we used the following inclusion criteria: language (English), date (January 2005–September 2015) and studies in humans. Only original articles, articles in press and reviews were included in the search key.
Article titles identified by the search strategy were downloaded into a Microsoft Excel file. RWMB scanned the titles and, where available, abstracts of the articles identified by the search, and selected articles for inclusion in the study. Titles and/or abstracts that did not meet the inclusion criteria were identified and removed. Exclusion was based on the following criteria: no primary focus on Sjögren’s, non-original research (letters, commentaries, etc), case studies/series and small studies (<10 patients), narrative/opinion-based reviews and articles that did not report on patient burden. JAB and ANN independently validated the selected and deselected articles. When a discrepancy arose, the authors discussed the respective article, and a consensus was reached about the inclusion/exclusion of the study. Additionally, the authors searched through their own collections of literature to ensure that no relevant articles known to them had been omitted.
Full articles for the titles and abstracts positively identified above were analysed and data were extracted (by RWMB) and entered into the Excel file. The following general variables were extracted: first author, title, journal, year of publication, type of article, type of study, study size, country of origin (patient population), database source and type, and criteria for disease diagnosis. The following patient aspects and specific variables were extracted: intervention, health-related quality-of-life (QoL) scale used, clinical signs (physician rated), clinical signs (laboratory tests), general disease PRO scales, exocrine gland PRO scales, extraglandular PRO scales, validation, patient satisfaction, productivity and disability. If no information on the patient aspects or specific variables could be retrieved, the articles were excluded from the analysis. Extraction of the above variables allowed for the identification of patient-reported symptoms and their impact on functional status, factors that impacted QoL, disease-specific outcomes and patient preferences. Furthermore, those studies that reported change in PRO measures and/or validated the use of PRO measures were identified.
Results
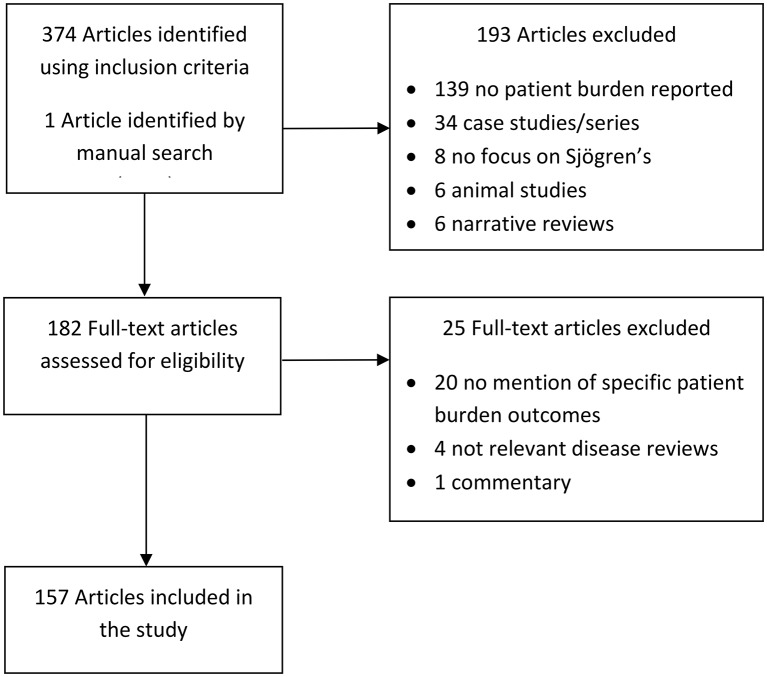
The search strategy using inclusion criteria intended to select articles dealing with patient burden of Sjögren’s yielded 374 articles, 193 of which were excluded based on the title and/or abstract (figure 1). One article was added by one of the authors (KMH). In all, 182 full-text articles were assessed for eligibility, 25 of which were excluded based on no information being available regarding patient aspects (figure 1).
Figure 1.
Flow diagram of Embase searches.
Results of individual articles
Sjögren’s disease description
A total of 157 articles included in the study described patient-reported symptoms associated with Sjögren’s and/or their impact on functional status. These consisted of 128 research articles (20 open-label studies, 16 place-bo-controlled trials, 85 prospective cohort studies, six retrospective cohort studies, one group concept mapping study), 21 clinical reviews, four validation studies, two diagnostic reviews and two article type not specified. The articles reported four domains of glandular symptoms (sicca overall, oral dryness, ocular dryness, general dryness in systems other than oral or ocular), 18 domains of extraglandular symptoms (fatigue, pain, depression, anxiety, sleep, sexual function, emotional function, cognitive performance, discomfort, impact of symptoms, learned helplessness, physical activity, personality, relationship status, autonomic function, headache, GI disease, lung involvement) and four domains of patient functional status (QoL, physical functioning, employment, utility) (table 1; online supplementary tables S1 and S2).
Table 1.
Symptoms of Sjögren’s syndrome and related patient-reported outcome measures
| Symptoms | Number of measures |
| Glandular symptoms | |
| Sicca symptoms | 4 |
| General dryness | 7 |
| Oral symptoms | 24 |
| Ocular symptoms | 11 |
| Extraglandular symptoms | |
| Fatigue | 14 |
| Pain | 14 |
| Depression | 8 |
| Anxiety | 5 |
| Sleep | 7 |
| Sexual function | 4 |
| Emotional function | 6 |
| Cognitive performance | 4 |
| Discomfort | 1 |
| Impact of symptoms | 1 |
| Learned helplessness | 1 |
| Physical activity | 2 |
| Personality | 2 |
| Relationship status | 1 |
| Autonomic function | 3 |
| Headache | 3 |
| Gastrointestinal disease | 1 |
| Lung involvement | 1 |
| Patient functional status | |
| Quality of life | 11 |
| Physical functioning | 3 |
| Employment | 4 |
| Utility | 1 |
Of the 157 articles, 32 reported on factors that had an impact on QoL (online supplementary table S3).9 31–57 The most commonly mentioned factor affecting QoL was fatigue (seven articles), followed by pain (five articles) and depression (five articles). Only 4 of the 157 articles reported on the impact of Sjögren’s burden on work productivity.11 40 51 58
rmdopen-2017-000443supp003.pdf (317.6KB, pdf)
In total, 143 PRO measures were used to measure glandular symptoms, extraglandular symptoms and functional status (37 VAS and 106 non-VAS; online supplementary table S1). These consisted of 46 measuring glandular symptoms (23 VAS, 23 non-VAS; online supplementary table S1), 78 measuring extraglandular symptoms (12 VAS, 66 non-VAS; online supplementary table S1) and 19 measuring functional status (2 VAS, 17 non-VAS; online supplementary table S1). In the evaluation of most of the commonly reported symptom domains, a wide variety of different assessment measures were used, including 24 measures for oral symptoms, 14 measures for fatigue, 14 measures for pain and 11 measures for QoL (table 1; online supplementary table S1). Very few of these measures have been validated.
rmdopen-2017-000443supp001.pdf (338.8KB, pdf)
Many VAS were used to evaluate various different symptom domains of Sjögren’s (eg, oral dryness, ocular dryness, pain, fatigue) (figure 2). However, even within a specific symptom (eg, ocular dryness or fatigue), a wide range of response anchor words were used across different publications and in some cases no anchor words were specified, making it difficult to compare VAS results across studies. Online supplementary table S2 shows a detailed overview of wording for symptoms used in VAS across different studies.9 12 31–34 59–100
Figure 2.
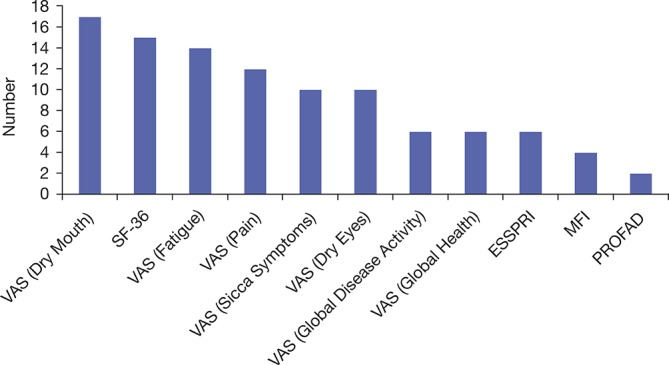
Most commonly used PRO scales across Sjögren’s drug therapy trials. ESSPRI, European League Against Rheumatism Sjögren’s Syndrome Patient Reported Index; MFI, Multidimensional Fatigue Inventory; PRO, patient-reported outcome; PROFAD, Profile of Fatigue and Discomfort; SF-36, 36 Item Short Form Survey; VAS, Visual Analogue Scale.
rmdopen-2017-000443supp002.pdf (360.2KB, pdf)
Patient perspective and preferences
Only two articles mentioned patient ‘satisfaction’ or ‘preference’.
In a single-blind crossover study of the efficacy of artificial saliva (Xialine) to treat patients with Sjögren’s, Alpöz et al stated that patients’ satisfaction was measured using a VAS, increased by 16.37% with Xialine and decreased by 25.63% with placebo.69
In a randomised, double-blind, placebo-controlled crossover study of the efficacy of cevimeline hydrochloride for the treatment of xerostomia in Chinese patients with Sjögren’s, Leung et al measured satisfaction using a VAS with the anchor words ‘no benefit’ to ‘extremely beneficial’.101 They found no significant differences in patient satisfaction or patient preference between cevimeline and placebo.
Measuring change in symptoms with use of therapies
Of the 157 articles, 33 reported on clinical trials (including controlled and open label) of drug ther-apies for Sjögren’s. PROs have played a prominent role in these studies. The most commonly used PRO scales were oral dryness/dry mouth VAS (n=17), followed by 36 Item Short Form Survey (SF-36; n=15), fatigue VAS (n=14), pain VAS (n=12), sicca symptoms/dryness VAS (n=10) and ocular dryness/dry eyes VAS (n=10). Figure 2 shows the frequency of use of all the PRO measures from the trials identified in this review. Controlled trials of biological therapies identified for this review have used PROs as both secondary and primary endpoints with a 20%–30% improvement in at least two VAS most commonly being included as part of a composite primary endpoint. None of the studies of biological therapies reported during the time frame of this review achieved a statistically significant improvement over placebo using such a PRO composite primary endpoint, and mixed results were seen across the studies with other individual PROs (online supplementary table S4).75 82 85 91 93 102 103
rmdopen-2017-000443supp004.pdf (287.9KB, pdf)
Measuring disease burden: validation of measures
The more recently developed PRO measures have been extensively validated in the past for use in patients with Sjögren’s and are trusted by clinicians as valuable tools to assess disease severity. Validation studies identified during the time frame of this review were short form PROFAD-SSI,27 ESSPRI,104 Multidimensional Fatigue Inventory (MFI-20)89 and the Swedish version of Profile of Fatigue (ProF).105
Bowman et al compared a short version (19 questions) of the PROFAD-SSI to the previously validated longer version (64 questions) and found statistically significant correlations (Spearman’s ρ ranging from 0.779 to greater than 0.90; p<0.01) for all eight domain scores and the three summary scores (PROF, PROFAD and SSI). Principal components analysis found high internal consistency for the PROFAD-SSI short form. This study also compared the shortened SSI part of this instrument (containing one item measuring dry skin, one for vaginal dryness, three for ocular dryness and five for oral dryness) with individual VAS representing each dryness domain and one overall dryness VAS, and determined that a single VAS is representative of the multiple items in each domain of the SSI. The authors also performed a correlation analysis between all the individual domains of the PROFAD-SSI short form and one individual VAS of fatigue and found the strongest correlation with somatic fatigue domain. The conclusions from this study were that a seven-item VAS may be useful for clinical trials.27
Seror et al evaluated the construct validity, responsiveness and reliability of the ESSPRI compared with the PROFAD and SSI and found the ESSPRI correlated well with the Patient Global Assessment, PROFAD and SSI (r=0.70, 0.68 and 0.59, respectively), although correlation with the ESSDAI was low (r=0.20). The ESSPRI had low responsiveness in patients experiencing improvement in symptoms (−0.37), but it was better than the responsiveness of the PROFAD or SSI (−0.16, –0.04, respectively), and much lower than the ESSDAI (−0.72). The authors concluded that the ESSPRI had good construct validity and was reliable, but had a small sensitivity to change and correlated poorly with systemic symptoms.104
d’Elia et al assessed the construct validity of the MFI in patients with Sjögren’s through correlation with a global fatigue VAS, assessed test–retest reliability through intraclass correlation coefficients and compared the associations between clinical variables and subscales of the MFI. The authors found that all subscales of the MFI correlated with the global fatigue VAS, with general fatigue showing the highest correlation (rs=0.70). The authors concluded that the MFI was a valid and reliable tool for the measurement of fatigue in Sjögren’s.89
Strömbeck et al translated the ProF into Swedish and evaluated the reliability and validity of the translation.105 They found that the test–retest reliability was moderate to good and the internal consistency was high. Construct validity was demonstrated by the significant correlation between questionnaire items and the fatigue VAS, and the physical function and vitality scales of SF-36. The authors concluded that the Swedish translation of ProF was a relatively reliable and valid instrument for the measurement of fatigue in patients with Sjögren’s.
Discussion
Sjögren’s is a largely unrecognised but highly prevalent disease that imposes a considerable burden on patients and has many unmet medical needs in terms of diagnosis and therapy. The complete burden of Sjögren’s from the patient perspective has not yet been fully elucidated. This comprehensive review of 157 published articles describing patient-reported symptoms of Sjögren’s and/or their impact on functional status revealed, for the first time, the wide range and diversity of PRO measures that have been used to quantify disease severity across studies. A lack of qualitative research was revealed with regard to patient preferences, patient satisfaction with therapy and the risks that patients are willing to accept. Only two studies included in this literature review reported any data on patient preferences/satisfaction, and only one provided information about caregiver burden in Sjögren’s. However, it is important to note that evaluation of these aspects of care is not included in current tools to assess the severity of Sjögren’s.
The heterogeneous nature of the condition results in a wide range of signs and symptoms which have been evaluated using an equally wide range of outcome measures, which may be a reflection of the considerable worldwide interest in Sjögren’s. During the time frame of this literature review (January 2005–September 2015), 106 different (non-VAS) instruments were used to measure patient-perceived disease burden in Sjögren’s covering sicca symptoms, fatigue, pain, emotional function, sleep, sexual function, cognitive performance, physical activity and QoL, among others. VAS were used to measure 35 different concepts from extent of dryness across different body systems to more functional assessments, such as difficulty chewing, denture retention or ability to sleep. The variability in use of response anchor words or lack of specification of the anchor words for each end of the VAS makes these difficult to compare across studies. While VAS have been the most commonly used PRO measure in drug therapy trials, formal validation of such scales in patients with Sjögren’s, including which degree of improvement constitutes a clinically meaningful change, does not appear to have been documented yet.
More recently, patient-reported symptoms of overall dryness, fatigue and pain have become the focus (ie, ESSPRI), consistent with the literature demonstrating these symptoms to have a strong impact on patient QoL. However, lack of correlation between instruments measuring these symptoms and clinician-measured outcomes as well as a low sensitivity to measure an improvement in symptoms has called into question the usefulness and validity of PROs as measurement tools in therapeutic clinical trials.30 104 However, as demonstrated by Seror et al, lack of correlation between Patient Global Assessment score and Physician Global Assessment score in patients with Sjögren’s underscores the fact that some aspects of the disease can only be known and assessed by the patient.106
Insensitivity of a PRO instrument could be related to content validity within the specific population being studied. Patient input as to the importance of the three domains measured by the ESSPRI was obtained during its development as well as during the development of the predecessor measures (PROFAD and SSI). Other reasons why a particular PRO measure could lack sensitivity could be related to the response options provided, or the recall period. While the ESSPRI uses a relatively short (2-week) recall period, symptoms that could be variable over time (eg, fatigue and pain) may warrant a daily measurement strategy, or an alternative to reduce recall bias, for example, focusing the patient’s attention on extremes, such as worst or best symptoms over the recall period, noting that the PROFAD does measure worst symptoms. In the absence of reliable, validated outcome measures that are capable of demonstrating disease change from the patient perspective, it is difficult to ascertain if the failure of a therapy to provide efficacy in a clinical trial is due to the therapy itself, to the particular patient population studied or to the endpoints included in the clinical trial design. It should be noted, however, that no therapy has yet been shown to result in significant improvements of the signs or symptoms of Sjögren’s, suggesting that the lack of demonstrable improvement in clinical trials may well be due to lack of efficacy rather than lack of ability to measure change in disease severity.
Instrument development for Sjögren’s clinical trials continues to progress with a responder index recently being developed,59 as well as alternative measurement approaches, such as the Patient Reported Outcomes Measurement Information System.107 Lendrem et al suggested that future research should be conducted to develop a primary Sjögren’s disease-specific QoL measure.108 We would like to expand on that idea to suggest a QoL assessment approach based on a patient’s ability to function. Given the wide range of body systems affected and symptoms experienced, assessing function may be more valuable than assessing severity of individual symptoms, and may provide a more realistic picture of the patient burden of Sjögren’s in the real world. Such a concept, based on function, has recently been developed for ankylosing spondylitis.109
For PRO assessments to be broadly useful, they not only need to represent symptoms that are most relevant to patients, but also demonstrate the ability to detect improvement in response to therapeutic intervention, and have sufficient documented evidence on their content and construct validity in the Sjögren’s population to meet the current regulatory requirements. Future research efforts to further understand the patient experience in Sjögren’s could provide information to refine existing or develop new instruments to more specifically and sensitively assess patient symptoms.
Study strengths/limitations
To the best of the authors’ knowledge, this comprehensive review is the first of its kind to catalogue the breadth of patient-reported symptoms that have been assessed in patients with Sjögren’s, as well as the wide range and diversity of measures that have been used to evaluate symptom severity. This study has identified gaps in the literature related to attitudes of patients with Sjögren’s towards the current standard of care, their preferences regarding therapy, the drivers of patient satisfaction and the burden of Sjögren’s on caregivers.
This study has a number of possible limitations. The search strategy was limited to one database (Embase), although the research was performed through exhaustive and comprehensive searching. The search was also restricted to articles published in the English language, with a 10-year time frame. An assessment of the validity of included articles through a risk-of-bias analysis was not performed. However, the goal of this study was not to produce a best-evidence synthesis (relevant effects of interventions) but rather to provide evidence of the range and heterogeneity of assessments used, which may be an impediment to a clear understanding of patient burden. While the authors feel that this review represents an important step towards understanding the complexity of measures used to evaluate severity of Sjögren’s, a formal systematic review involving searches of multiple databases would undoubtedly be of great value and should be considered as a future line of research.
Conclusions
A clear understanding of the burden of Sjögren’s is needed to provide optimal care and support for patients. This understanding is currently hampered by the use of a wide range of heterogeneous measures of glandular and extraglandular symptoms, QoL and functional status, most of which have not been validated for use in Sjögren’s. Because factors affecting QoL of patients with Sjögren’s can be among the most difficult to measure, endpoints that are validated specifically in patients with Sjögren’s are needed to demonstrate improvement. These measures should focus on the QoL aspects that are important to patients, and may involve gauging change in function rather than patient-reported symptoms.
Acknowledgments
Data collection, data analyses and quality control were performed by Excerpta Medica B.V. on behalf of Eli Lilly and Company. Editorial support during the writing of this manuscript was provided by Patrick Crowley, PhD, on behalf of Excerpta Medica B.V
Footnotes
Contributors: All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. KMH had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study conception and design: KMH, RWMB, ANN, JAB. Acquisition of data: RWMB, ANN, JAB. Analysis and interpretation of data: KMH, RWMB, ANN, JAB.
Funding: This study was funded by Eli Lilly and Company.
Competing interests: KMH is Vice President of Medical and Scientific Affairs of the Sjögren’s Syndrome Foundation. ANN and JAB are employees and stockholders of Eli Lilly and Company. RWMB is employed by Excerpta Medica B.V.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. Fox RI. Syndrome Sjögren’s. Lancet 2005;366:321–31. 10.1016/S0140-6736(05)66990-5 [DOI] [PubMed] [Google Scholar]
- 2. Bayetto K, Logan RM. Sjögren’s syndrome: a review of aetiology, pathogenesis, diagnosis and management. Aust Dent J 2010;55(Suppl 1):39–47. 10.1111/j.1834-7819.2010.01197.x [DOI] [PubMed] [Google Scholar]
- 3. Patel R, Shahane A. The epidemiology of Sjögren’s syndrome. Clin Epidemiol 2014;6:247–55. 10.2147/CLEP.S47399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ienopoli S, Carsons SE. Extraglandular manifestations of primary Sjögren’s syndrome. Oral Maxillofac Surg Clin North Am 2014;26:91–9. 10.1016/j.coms.2013.09.008 [DOI] [PubMed] [Google Scholar]
- 5. Helmick CG, Felson DT, Lawrence RC, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum 2008;58:15–25. 10.1002/art.23177 [DOI] [PubMed] [Google Scholar]
- 6. Shiboski SC, Shiboski CH, Criswell LA, et al. American College of Rheumatology classification criteria for Sjögren’s syndrome: a data-driven, expert consensus approach in the Sjögren’s International Collaborative Clinical Alliance Cohort. Arthritis Care Res 2012;64:475–87. 10.1002/acr.21591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hammitt K. Should I treat my Sjögren’s different if I have primary vs secondary Sjögren’s? The Moisture Seekers 2014;32:1–6. [Google Scholar]
- 8. Tzioufas AG, Voulgarelis M. Update on Sjögren’s syndrome autoimmune epithelitis: from classification to increased neoplasias. Best Pract Res Clin Rheumatol 2007;21:989–1010. 10.1016/j.berh.2007.09.001 [DOI] [PubMed] [Google Scholar]
- 9. Ng WF, Stangroom AJ, Davidson A, et al. Primary Sjogrens syndrome is associated with impaired autonomic response to orthostasis and sympathetic failure. QJM 2012;105:1191–9. 10.1093/qjmed/hcs172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ng WF, Bowman SJ. Primary Sjogren’s syndrome: too dry and too tired. Rheumatology 2010;49:844–53. 10.1093/rheumatology/keq009 [DOI] [PubMed] [Google Scholar]
- 11. Westhoff G, Dörner T, Zink A. Fatigue and depression predict physician visits and work disability in women with primary Sjögren’s syndrome: results from a cohort study. Rheumatology 2012;51:262–9. 10.1093/rheumatology/ker208 [DOI] [PubMed] [Google Scholar]
- 12. Theander E, Henriksson G, Ljungberg O, et al. Lymphoma and other malignancies in primary Sjögren’s syndrome: a cohort study on cancer incidence and lymphoma predictors. Ann Rheum Dis 2006;65:796–803. 10.1136/ard.2005.041186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ekström Smedby K, Vajdic CM, Falster M, et al. Autoimmune disorders and risk of non-Hodgkin lymphoma subtypes: a pooled analysis within the InterLymph Consortium. Blood 2008;111:4029–38. 10.1182/blood-2007-10-119974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Baldini C, Talarico R, Tzioufas AG, et al. Classification criteria for Sjogren’s syndrome: a critical review. J Autoimmun 2012;39:9–14. 10.1016/j.jaut.2011.12.006 [DOI] [PubMed] [Google Scholar]
- 15. Shiboski SC, Shiboski CH, Criswell L, et al. American College of Rheumatology classification criteria for Sjögren’s syndrome: a data-driven, expert consensus approach in the Sjögren’s International Collaborative Clinical Alliance cohort. Arthritis Care Res 2012;64:475–87. 10.1002/acr.21591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shiboski SC, Shiboski SC, Seror R, et al. 2016 Classification criteria for primary Sjögren’s syndrome: a consensus and data-driven methodology involving three international patient cohorts. Arthritis Rheumatol 2017;69:35–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sène D, Jallouli M, Lefaucheur JP, et al. Peripheral neuropathies associated with primary Sjögren syndrome: immunologic profiles of nonataxic sensory neuropathy and sensorimotor neuropathy. Medicine 2011;90:133–8. 10.1097/MD.0b013e31820fd2d1 [DOI] [PubMed] [Google Scholar]
- 18. Mori K, Iijima M, Koike H, et al. The wide spectrum of clinical manifestations in Sjögren’s syndrome-associated neuropathy. Brain 2005;128:2518–34. 10.1093/brain/awh605 [DOI] [PubMed] [Google Scholar]
- 19. Movva S, Carsons S. Review of pediatric Sjögren’s syndrome. Pediatr Allergy Immunol Pulmonol 2014;27:111–4. 10.1089/ped.2013.0326 [DOI] [PubMed] [Google Scholar]
- 20. Yokogawa N, Lieberman SM, Sherry DD, et al. Features of childhood Sjögren’s syndrome in comparison to adult Sjögren’s syndrome: considerations in establishing child-specific diagnostic criteria. Clin Exp Rheumatol 2016;34:343–51. [PubMed] [Google Scholar]
- 21. Mignogna MD, Fedele S, Lo Russo L, et al. Sjögren’s syndrome: the diagnostic potential of early oral manifestations preceding hyposalivation/xerostomia. J Oral Pathol Med 2005;34:1–6. 10.1111/j.1600-0714.2004.00264.x [DOI] [PubMed] [Google Scholar]
- 22. FDA Guidance for Industry. Patient-reported outcome measures: use in medical product development to support labeling claims. 2009. http://www.fda.gov/downloads/Drugs/Guidances/UCM193282.pdf (accessed 13 May 2016). [DOI] [PMC free article] [PubMed]
- 23. Rothrock NE, Kaiser KA, Cella D. Developing a valid patient-reported outcome measure. Clin Pharmacol Ther 2011;90:737–42. 10.1038/clpt.2011.195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bowman SJ, Pillemer S, Jonsson R, et al. Revisiting Sjögren’s syndrome in the new millennium: perspectives on assessment and outcome measures. report of a workshop held on 23 March 2000 at Oxford, UK. Rheumatology 2001;40:1180–8. [DOI] [PubMed] [Google Scholar]
- 25. Bowman SJ, Booth DA, Platts RG, et al. Validation of the Sicca Symptoms Inventory for clinical studies of Sjögren’s syndrome. J Rheumatol 2003;30:1259–66. [PubMed] [Google Scholar]
- 26. Bowman SJ, Booth DA, Platts RG, et al. Measurement of fatigue and discomfort in primary Sjogren’s syndrome using a new questionnaire tool. Rheumatology 2004;43:758–64. 10.1093/rheumatology/keh170 [DOI] [PubMed] [Google Scholar]
- 27. Bowman SJ, Hamburger J, Richards A, et al. Patient-reported outcomes in primary Sjogren’s syndrome: comparison of the long and short versions of the Profile of Fatigue and Discomfort - Sicca Symptoms Inventory. Rheumatology 2009;48:140–3. 10.1093/rheumatology/ken426 [DOI] [PubMed] [Google Scholar]
- 28. Seror R, Ravaud P, Mariette X, et al. EULAR Sjogren’s Syndrome Patient Reported Index (ESSPRI): development of a consensus patient index for primary Sjogren’s syndrome. Ann Rheum Dis 2011;70:968–72. 10.1136/ard.2010.143743 [DOI] [PubMed] [Google Scholar]
- 29. Hay EM, Thomas E, Pal B, et al. Weak association between subjective symptoms or and objective testing for dry eyes and dry mouth: results from a population based study. Ann Rheum Dis 1998;57:20–4. 10.1136/ard.57.1.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Seror R, Theander E, Bootsma H, et al. Outcome measures for primary Sjögren’s syndrome: a comprehensive review. J Autoimmun 2014;51:51–6. 10.1016/j.jaut.2013.12.010 [DOI] [PubMed] [Google Scholar]
- 31. van Leeuwen N, Bossema ER, van Middendorp H, et al. Dealing with emotions when the ability to cry is hampered: emotion processing and regulation in patients with primary Sjögren’s syndrome. Clin Exp Rheumatol 2012;30:492–8. [PubMed] [Google Scholar]
- 32. Hur J, Chung SW, Yj H, et al. Association between insomnia and EULAR Sjögren’s syndrome patient-reported index in Korean patients with primary Sjögren’s syndrome [abstract]. Arthritis Rheumatol 2015;67(suppl 10). [Google Scholar]
- 33. Ibn Yacoub Y, Rostom S, Laatiris A, et al. Primary Sjögren’s syndrome in Moroccan patients: characteristics, fatigue and quality of life. Rheumatol Int 2012;32:2637–43. 10.1007/s00296-011-2009-5 [DOI] [PubMed] [Google Scholar]
- 34. Champey J, Corruble E, Gottenberg JE, et al. Quality of life and psychological status in patients with primary Sjögren’s syndrome and sicca symptoms without autoimmune features. Arthritis Rheum 2006;55:451–7. 10.1002/art.21990 [DOI] [PubMed] [Google Scholar]
- 35. van Nimwegen JF, Arends S, van Zuiden GS, et al. The impact of primary Sjögren’s syndrome on female sexual function. Rheumatology 2015;54:1286–93. 10.1093/rheumatology/keu522 [DOI] [PubMed] [Google Scholar]
- 36. Tanner K, Pierce JL, Merrill RM, et al. The quality of life burden associated with voice disorders in Sjögren’s syndrome. Ann Otol Rhinol Laryngol 2015;124:721–7. 10.1177/0003489415579911 [DOI] [PubMed] [Google Scholar]
- 37. Priori R, Minniti A, Derme M, et al. Quality of sexual life in women with primary Sjögren syndrome. J Rheumatol 2015;42:1427–31. 10.3899/jrheum.141475 [DOI] [PubMed] [Google Scholar]
- 38. Koh JH, Kwok SK, Chung MK, et al. Pain, xerostomia, and younger age are major determinants of fatigue in Korean primary Sjögren’s syndrome patients: a comprehensive analysis of a cohort study. Arthritis Rheumatol 2015;67(Suppl 10). abstract 641. [Google Scholar]
- 39. Lendrem D, Mitchell S, McMeekin P, et al. Health-related utility values of patients with primary Sjögren’s syndrome and its predictors. Ann Rheum Dis 2014;73:1362–8. 10.1136/annrheumdis-2012-202863 [DOI] [PubMed] [Google Scholar]
- 40. Dias LH, Miyamoto ST, Valim V, et al. SAT0422 Impact of symptoms and disease activity on quality of life in primary Sjögren’s syndrome. Ann Rheum Dis 2015;74(Suppl 2):812.2–812. 10.1136/annrheumdis-2015-eular.5063 [DOI] [Google Scholar]
- 41. Fernandez Castro M, Andreu JL, Martínez Taboada V, et al. AB0597 Sjogrenser cohort: clinical and epidemiological features of primary Sjögren’s syndrome in Spanish rheumathology departments. Ann Rheum Dis 2015;74(Suppl 2):1099.3–1099. 10.1136/annrheumdis-2015-eular.2003 [DOI] [Google Scholar]
- 42. Maddali Bongi S, Del Rosso A, Orlandi M, et al. Gynaecological symptoms and sexual disability in women with primary Sjögren’s syndrome and sicca syndrome. Clin Exp Rheumatol 2013;31:683–90. [PubMed] [Google Scholar]
- 43. Palm O, Garen T, Berge Enger T, et al. Clinical pulmonary involvement in primary Sjogren’s syndrome: prevalence, quality of life and mortality--a retrospective study based on registry data. Rheumatology 2013;52:173–9. 10.1093/rheumatology/kes311 [DOI] [PubMed] [Google Scholar]
- 44. Wu GL, Li TY, Fan YS, et al. Therapeutic effect of Chinese herbal medicine for strengthening qi, nourishing yin, and removing stasis on serum osteopontin and quality of life of patients with primary Sjogren’s syndrome. Chin J Integr Med 2011;17:710–4. 10.1007/s11655-011-0850-8 [DOI] [PubMed] [Google Scholar]
- 45. Enger TB, Palm Ø, Garen T, et al. Oral distress in primary Sjögren’s syndrome: implications for health-related quality of life. Eur J Oral Sci 2011;119:474–80. 10.1111/j.1600-0722.2011.00891.x [DOI] [PubMed] [Google Scholar]
- 46. Hyphantis T, Mantis D, Voulgari PV, et al. The psychological defensive profile of primary Sjögren’s syndrome patients and its relationship to health-related quality of life. Clin Exp Rheumatol 2011;29:485–93. [PubMed] [Google Scholar]
- 47. Hartkamp A, Geenen R, Kruize AA, et al. Serum dehydroepiandrosterone sulphate levels and laboratory and clinical parameters indicating expression of disease are not associated with fatigue, well-being and functioning in patients with primary Sjögren’s syndrome. Clin Exp Rheumatol 2011;29:318–21. [PubMed] [Google Scholar]
- 48. Inal V, Kitapcioglu G, Karabulut G, et al. Evaluation of quality of life in relation to anxiety and depression in primary Sjögren’s syndrome. Mod Rheumatol 2010;20:588–97. 10.3109/s10165-010-0329-z [DOI] [PubMed] [Google Scholar]
- 49. Kamel UF, Maddison P, Whitaker R. Impact of primary Sjogren’s syndrome on smell and taste: effect on quality of life. Rheumatology 2009;48:1512–4. 10.1093/rheumatology/kep249 [DOI] [PubMed] [Google Scholar]
- 50. Baturone R, Soto MJ, Márquez M, et al. Health-related quality of life in patients with primary Sjögren’s syndrome: relationship with serum levels of proinflammatory cytokines. Scand J Rheumatol 2009;38:386–9. 10.1080/03009740902973821 [DOI] [PubMed] [Google Scholar]
- 51. Meijer JM, Meiners PM, Huddleston Slater JJ, et al. Health-related quality of life, employment and disability in patients with Sjogren’s syndrome. Rheumatology 2009;48:1077–82. 10.1093/rheumatology/kep141 [DOI] [PubMed] [Google Scholar]
- 52. Segal B, Bowman SJ, Fox PC, et al. Primary Sjögren’s syndrome: health experiences and predictors of health quality among patients in the United States. Health Qual Life Outcomes 2009;7:46 10.1186/1477-7525-7-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Fox PC, Bowman SJ, Segal B, et al. Oral involvement in primary Sjögren syndrome. J Am Dent Assoc 2008;139:1592–601. 10.14219/jada.archive.2008.0101 [DOI] [PubMed] [Google Scholar]
- 54. Barry RJ, Sutcliffe N, Isenberg DA, et al. The Sjögren’s Syndrome Damage Index--a damage index for use in clinical trials and observational studies in primary Sjögren’s syndrome. Rheumatology 2008;47:1193–8. 10.1093/rheumatology/ken164 [DOI] [PubMed] [Google Scholar]
- 55. Stewart CM, Berg KM, Cha S, et al. Salivary dysfunction and quality of life in Sjögren syndrome: a critical oral-systemic connection. J Am Dent Assoc 2008;139:291–9. [DOI] [PubMed] [Google Scholar]
- 56. Bowman SJ, Sutcliffe N, Isenberg DA, et al. Sjögren’s Systemic Clinical Activity Index (SCAI)--a systemic disease activity measure for use in clinical trials in primary Sjögren’s syndrome. Rheumatology 2007;46:1845–51. 10.1093/rheumatology/kem280 [DOI] [PubMed] [Google Scholar]
- 57. Belenguer R, Ramos-Casals M, Brito-Zerón P, et al. Influence of clinical and immunological parameters on the health-related quality of life of patients with primary Sjögren’s syndrome. Clin Exp Rheumatol 2005;23:351–6. [PubMed] [Google Scholar]
- 58. Bowman SJ, St Pierre Y, Sutcliffe N, et al. Estimating indirect costs in primary Sjögren’s syndrome. J Rheumatol 2010;37:1010–5. 10.3899/jrheum.090734 [DOI] [PubMed] [Google Scholar]
- 59. Cornec D, Devauchelle-Pensec V, Mariette X, et al. Development of the Sjögren’s Syndrome Responder Index, a data-driven composite endpoint for assessing treatment efficacy. Rheumatology 2015;54:1699–708. 10.1093/rheumatology/kev114 [DOI] [PubMed] [Google Scholar]
- 60. Shi H, Zheng LY, Zhang P, et al. miR-146a and miR-155 expression in PBMCs from patients with Sjögren’s syndrome. J Oral Pathol Med 2014;43:792–7. 10.1111/jop.12187 [DOI] [PubMed] [Google Scholar]
- 61. Seitsalo H, Niemelä RK, Marinescu-Gava M, et al. Effectiveness of low-dose doxycycline (LDD) on clinical symptoms of Sjögren’s syndrome: a randomized, double-blind, placebo controlled cross-over study. J Negat Results Biomed 2007;6:11 10.1186/1477-5751-6-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Hartkamp A, Geenen R, Godaert GL, et al. Effect of dehydroepiandrosterone administration on fatigue, well-being, and functioning in women with primary Sjögren syndrome: a randomised controlled trial. Ann Rheum Dis 2008;67:91–7. 10.1136/ard.2007.071563 [DOI] [PubMed] [Google Scholar]
- 63. Seror R, Ravaud P, Bowman SJ, et al. EULAR Sjögren’s Task Force. EULAR Sjogren’s syndrome disease activity index: development of a consensus systemic disease activity index for primary Sjogren’s syndrome. Ann Rheum Dis 2010;69:1103–9. Erratum in Ann Rheum Dis 2011;70:880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Forsblad-d’Elia H, Carlsten H, Labrie F, et al. Low serum levels of sex steroids are associated with disease characteristics in primary Sjogren’s syndrome; supplementation with dehydroepiandrosterone restores the concentrations. J Clin Endocrinol Metab 2009;94:2044–51. 10.1210/jc.2009-0106 [DOI] [PubMed] [Google Scholar]
- 65. Theander E, Andersson SI, Manthorpe R, et al. Proposed core set of outcome measures in patients with primary Sjögren’s syndrome: 5 year follow up. J Rheumatol 2005;32:1495–502. [PubMed] [Google Scholar]
- 66. Segal BM, Pogatchnik B, Henn L, et al. Pain severity and neuropathic pain symptoms in primary Sjögren’s syndrome: a comparison study of seropositive and seronegative Sjögren’s syndrome patients. Arthritis Care Res 2013;65:1291–8. 10.1002/acr.21956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Aliko A, Alushi A, Tafaj A, et al. Evaluation of the clinical efficacy of Biotène oral balance in patients with secondary Sjögren’s syndrome: a pilot study. Rheumatol Int 2012;32:2877–81. 10.1007/s00296-011-2085-6 [DOI] [PubMed] [Google Scholar]
- 68. Kasama T, Shiozawa F, Isozaki T, et al. Effect of the H2 receptor antagonist nizatidine on xerostomia in patients with primary Sjögren’s syndrome. Mod Rheumatol 2008;18:455–9. 10.3109/s10165-008-0078-4 [DOI] [PubMed] [Google Scholar]
- 69. Alpöz E, Güneri P, Onder G, et al. The efficacy of Xialine in patients with Sjögren’s syndrome: a single-blind, cross-over study. Clin Oral Investig 2008;12:165–72. 10.1007/s00784-007-0159-3 [DOI] [PubMed] [Google Scholar]
- 70. Wu CH, Hsieh SC, Lee KL, et al. Pilocarpine hydrochloride for the treatment of xerostomia in patients with Sjögren’s syndrome in Taiwan--a double-blind, placebo-controlled trial. J Formos Med Assoc 2006;105:796–803. 10.1016/S0929-6646(09)60266-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Cankaya H, Alpöz E, Karabulut G, et al. Effects of hydroxychloroquine on salivary flow rates and oral complaints of Sjögren patients: a prospective sample study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;110:62–7. 10.1016/j.tripleo.2010.02.032 [DOI] [PubMed] [Google Scholar]
- 72. Hammenfors DS, Brun JG, Jonsson R, et al. Diagnostic utility of major salivary gland ultrasonography in primary Sjögren’s syndrome. Clin Exp Rheumatol 2015;33:56–62. [PubMed] [Google Scholar]
- 73. Cho HJ, Yoo JJ, Yun CY, et al. The EULAR Sjogren’s syndrome patient reported index as an independent determinant of health-related quality of life in primary Sjogren’s syndrome patients: in comparison with non-Sjogren’s sicca patients. Rheumatology 2013;52:2208–17. 10.1093/rheumatology/ket270 [DOI] [PubMed] [Google Scholar]
- 74. Haldorsen K, Bjelland I, Bolstad AI, et al. A five-year prospective study of fatigue in primary Sjögren’s syndrome. Arthritis Res Ther 2011;13:R167 10.1186/ar3487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Meijer JM, Meiners PM, Vissink A, et al. Effectiveness of rituximab treatment in primary Sjögren’s syndrome: a randomized, double-blind, placebo-controlled trial. Arthritis Rheum 2010;62:960–8. 10.1002/art.27314 [DOI] [PubMed] [Google Scholar]
- 76. Nakayamada S, Saito K, Umehara H, et al. Efficacy and safety of mizoribine for the treatment of Sjögren’s syndrome: a multicenter open-label clinical trial. Mod Rheumatol 2007;17:464–9. 10.3109/s10165-007-0627-2 [DOI] [PubMed] [Google Scholar]
- 77. Devauchelle-Pensec V, Pennec Y, Morvan J, et al. Improvement of Sjögren’s syndrome after two infusions of rituximab (anti-CD20). Arthritis Rheum 2007;57:310–7. 10.1002/art.22536 [DOI] [PubMed] [Google Scholar]
- 78. Willeke P, Schlüter B, Becker H, et al. Mycophenolate sodium treatment in patients with primary Sjögren syndrome: a pilot trial. Arthritis Res Ther 2007;9:R115 10.1186/ar2322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Vriezekolk JE, Geenen R, Hartkamp A, et al. Psychological and somatic predictors of perceived and measured ocular dryness of patients with primary Sjögren’s syndrome. J Rheumatol 2005;32:2351–5. [PubMed] [Google Scholar]
- 80. Caffery B, Joyce E, Boone A, et al. Tear lipocalin and lysozyme in Sjögren and non-Sjögren dry eye. Optom Vis Sci 2008;85:661–7. 10.1097/OPX.0b013e318181ae4f [DOI] [PubMed] [Google Scholar]
- 81. Tuisku IS, Konttinen YT, Konttinen LM, et al. Alterations in corneal sensitivity and nerve morphology in patients with primary Sjögren’s syndrome. Exp Eye Res 2008;86:879–85. 10.1016/j.exer.2008.03.002 [DOI] [PubMed] [Google Scholar]
- 82. Devauchelle-Pensec V, Mariette X, Jousse-Joulin S, et al. Treatment of primary Sjögren syndrome with rituximab: a randomized trial. Ann Intern Med 2014;160:233–42. 10.7326/M13-1085 [DOI] [PubMed] [Google Scholar]
- 83. Devauchelle-Pensec V, Morvan J, Rat AC, et al. Effects of rituximab therapy on quality of life in patients with primary Sjögren’s syndrome. Clin Exp Rheumatol 2011;29:6–12. [PubMed] [Google Scholar]
- 84. Mariette X, Seror R, Quartuccio L, et al. Efficacy and safety of belimumab in primary Sjögren’s syndrome: results of the BELISS open-label phase II study. Ann Rheum Dis 2015;74:526–31. 10.1136/annrheumdis-2013-203991 [DOI] [PubMed] [Google Scholar]
- 85. Carubbi F, Cipriani P, Marrelli A, et al. Efficacy and safety of rituximab treatment in early primary Sjögren’s syndrome: a prospective, multi-center, follow-up study. Arthritis Res Ther 2013;15:R172 10.1186/ar4359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Gottenberg JE, Seror R, Benessiano J, et al. Is fatigue immunemediated in primary Sjögren’s syndrome? Data from the Prospective assess cohort. Ann Rheum Dis 2015;74(Suppl 2):796. [Google Scholar]
- 87. De Vita S, Quartuccio L, Seror R, et al. Efficacy and safety of belimumab given for 12 months in primary Sjögren’s syndrome: the BELISS open-label phase II study. Rheumatology 2015;54:338–9. 10.1093/rheumatology/kev257 [DOI] [PubMed] [Google Scholar]
- 88. George A, Pope JE. The minimally important difference (MID) for patient-reported outcomes including pain, fatigue, sleep and the health assessment questionnaire disability index (HAQ-DI) in primary Sjögren’s syndrome. Clin Exp Rheumatol 2011;29:248–53. [PubMed] [Google Scholar]
- 89. d’Elia HF, Rehnberg E, Kvist G, et al. Fatigue and blood pressure in primary Sjogren’s syndrome. Scand J Rheumatol 2008;37:284–92. 10.1080/03009740801907995 [DOI] [PubMed] [Google Scholar]
- 90. Kedor C, Hagemann A, Zernicke J, et al. THU0399 Effectiveness and safety of low-dose cyclosporine a in patients with primary Sjögren’s syndrome (PSS) with articular involvement – results of a pilot study. Ann Rheum Dis 2015;74(Suppl 2):341.1–341. 10.1136/annrheumdis-2015-eular.2806 24285491 [DOI] [Google Scholar]
- 91. Norheim KB, Harboe E, Gøransson LG, et al. Interleukin-1 inhibition and fatigue in primary Sjögren’s syndrome--a double blind, randomised clinical trial. PLoS One 2012;7:e30123 10.1371/journal.pone.0030123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Segal B, Thomas W, Rogers T, et al. Prevalence, severity, and predictors of fatigue in subjects with primary Sjögren’s syndrome. Arthritis Rheum 2008;59:1780–7. 10.1002/art.24311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Dass S, Bowman SJ, Vital EM, et al. Reduction of fatigue in Sjögren syndrome with rituximab: results of a randomised, double-blind, placebo-controlled pilot study. Ann Rheum Dis 2008;67:1541–4. 10.1136/ard.2007.083865 [DOI] [PubMed] [Google Scholar]
- 94. Strömbeck BE, Theander E, Jacobsson LT. Effects of exercise on aerobic capacity and fatigue in women with primary Sjogren’s syndrome. Rheumatology 2007;46:868–71. 10.1093/rheumatology/kem004 [DOI] [PubMed] [Google Scholar]
- 95. Tjensvoll AB, Harboe E, Gøransson LG, et al. Headache in primary Sjøgren’s syndrome: a population-based retrospective cohort study. Eur J Neurol 2013;20:558–63. 10.1111/ene.12033 [DOI] [PubMed] [Google Scholar]
- 96. Iannuccelli C, Spinelli FR, Guzzo MP, et al. Fatigue and widespread pain in systemic lupus erythematosus and Sjögren’s syndrome: symptoms of the inflammatory disease or associated fibromyalgia? Clin Exp Rheumatol 2012;30(6 Suppl 74):117–21. [PubMed] [Google Scholar]
- 97. Theander L, Strömbeck B, Mandl T, et al. Sleepiness or fatigue? Can we detect treatable causes of tiredness in primary Sjögren’s syndrome? Rheumatology 2010;49:1177–83. 10.1093/rheumatology/keq023 [DOI] [PubMed] [Google Scholar]
- 98. Harboe E, Tjensvoll AB, Vefring HK, et al. Fatigue in primary Sjögren’s syndrome--a link to sickness behaviour in animals? Brain Behav Immun 2009;23:1104–8. 10.1016/j.bbi.2009.06.151 [DOI] [PubMed] [Google Scholar]
- 99. Pertovaara M, Korpela M. ESSPRI and other patient-reported indices in patients with primary Sjogren’s syndrome during 100 consecutive outpatient visits at one rheumatological clinic. Rheumatology 2014;53:927–31. 10.1093/rheumatology/ket476 [DOI] [PubMed] [Google Scholar]
- 100. Hackett KL, Newton JL, Frith J, et al. Impaired functional status in primary Sjögren’s syndrome. Arthritis Care Res 2012;64:1760–4. 10.1002/acr.21738 [DOI] [PubMed] [Google Scholar]
- 101. Leung KC, McMillan AS, Wong MC, et al. The efficacy of cevimeline hydrochloride in the treatment of xerostomia in Sjögren’s syndrome in southern Chinese patients: a randomised double-blind, placebo-controlled crossover study. Clin Rheumatol 2008;27:429–36. 10.1007/s10067-007-0723-x [DOI] [PubMed] [Google Scholar]
- 102. Sankar V, Brennan MT, Kok MR, et al. Etanercept in Sjögren’s syndrome: a twelve-week randomized, double-blind, placebo-controlled pilot clinical trial. Arthritis Rheum 2004;50:2240–5. 10.1002/art.20299 [DOI] [PubMed] [Google Scholar]
- 103. Mariette X, Ravaud P, Steinfeld S, et al. Inefficacy of infliximab in primary Sjögren’s syndrome: results of the randomized, controlled Trial of Remicade in Primary Sjögren’s Syndrome (TRIPSS). Arthritis Rheum 2004;50:1270–6. 10.1002/art.20146 [DOI] [PubMed] [Google Scholar]
- 104. Seror R, Theander E, Brun JG, et al. Validation of EULAR primary Sjögren’s syndrome disease activity (ESSDAI) and patient indexes (ESSPRI). Ann Rheum Dis 2015;74:859–66. 10.1136/annrheumdis-2013-204615 [DOI] [PubMed] [Google Scholar]
- 105. Strömbeck B, Theander E, Jacobsson LT. Assessment of fatigue in primary Sjögren’s syndrome: the Swedish version of the Profile of Fatigue. Scand J Rheumatol 2005;34:455–9. 10.1080/03009740510026571 [DOI] [PubMed] [Google Scholar]
- 106. Seror R, Gottenberg JE, Devauchelle-Pensec V, et al. European League Against Rheumatism Sjögren’s Syndrome Disease Activity Index and European League Against Rheumatism Sjögren’s Syndrome Patient-Reported Index: a complete picture of primary Sjögren’s syndrome patients. Arthritis Care Res 2013;65:1358–64. 10.1002/acr.21991 [DOI] [PubMed] [Google Scholar]
- 107. Witter JP. The Promise of Patient-Reported Outcomes Measurement Information System-Turning Theory into Reality: A Uniform Approach to Patient-Reported Outcomes Across Rheumatic Diseases. Rheum Dis Clin North Am 2016;42:377–94. 10.1016/j.rdc.2016.01.007 [DOI] [PubMed] [Google Scholar]
- 108. Lendrem D, Mitchell S, McMeekin P, et al. Do the EULAR Sjögren’s syndrome outcome measures correlate with health status in primary Sjögren’s syndrome? Rheumatology 2015;54:655–9. 10.1093/rheumatology/keu361 [DOI] [PubMed] [Google Scholar]
- 109. Kiltz U, van der Heijde D, Cieza A, et al. Developing and validating an index for measuring health in patients with ankylosing spondylitis. Rheumatology 2011;50:894–8. 10.1093/rheumatology/keq315 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2017-000443supp003.pdf (317.6KB, pdf)
rmdopen-2017-000443supp001.pdf (338.8KB, pdf)
rmdopen-2017-000443supp002.pdf (360.2KB, pdf)
rmdopen-2017-000443supp004.pdf (287.9KB, pdf)