Abstract
Background
Many patients with osteoarthritis (OA) of the knee and/or hip undergo total joint replacement (TJR) because of severely progressed symptoms.
Aim
To determine patient and disease characteristics associated with undergoing TJR in participants with recent-onset knee and/or hip OA.
Design and setting
Participants with hip or knee pain from the nationwide prospective Cohort Hip and Cohort Knee (CHECK) study were included.
Method
The outcome measure was total hip arthroplasty (THA) or total knee arthroplasty (TKA) during 6 years of follow-up. Joint-dependent characteristics were compared using generalised estimating equations (GEE). Multivariable models were built for both subgroups. Differences in symptomatic and radiographic progression were determined between baseline and 2-year follow-up (T2).
Results
The knee subgroup included 751 participants (1502 knees), and there were 538 participants in the hip subgroup (1076 hips). Nineteen participants (22 knees) underwent TKA and 53 participants (62 hips) THA. Participants who underwent TKA had higher baseline body mass index, painful knee flexion, and higher Kellgren and Lawrence scores. Participants who underwent THA had painful internal hip rotation and showed more severe radiographic OA features. Participants who underwent TKA or THA showed more rapid symptomatic and radiographic OA progression at T2.
Conclusion
In patients with recent-onset knee or hip pain, radiographic OA features already exist and a substantial number of patients fulfil existing criteria for knee and hip OA. A trend was observed in rapid progression of radiographic and symptomatic OA severity among patients with TKA and THA. Early detection of OA by the GP is important in managing knee and hip OA.
Keywords: arthroplasty, replacement; osteoarthritis, hip; osteoarthritis, knee; primary health care
INTRODUCTION
Knee and/or hip osteoarthritis (OA) are among the most common diagnoses in general practice.1 Consequently, every year thousands of patients are at risk of progression of OA, and many of these patients become eligible for total joint replacement (TJR) because of severely progressed and disabling symptoms.2 Tens of thousands of TJRs are performed on a yearly basis in the Netherlands and the UK.3 However, not all patients with lower-joint OA undergo surgery, suggesting that OA progression is dependent on patient characteristics and/or variations between so-called phenotypes of OA,4 or is dependent on the physician’s choice to refer or operate. Predicting severe OA progression in the early stages of disease would aid the GP in initiation and implementation of early intervention strategies to prevent further structural damage to the joints.5 Patients with recent-onset OA who have a low risk of OA progression and subsequent TJR can be better reassured, and unnecessary interventions or referral can be avoided. Vice versa, patients with high risk of progression who are eligible for TJR can be referred sooner for specialist treatment. The aim of the present research was to determine patient and disease characteristics associated with undergoing TJR within 6 years of follow-up in a study population aged 45 to 65 years at baseline, with recent-onset knee and/or hip OA.
METHOD
Study design and population
The present data were obtained from participants enrolled in the Cohort Hip and Cohort Knee (CHECK) study. CHECK is a nationwide prospective, 10-year follow-up cohort of 1002 participants with early symptomatic OA of the knee and/or hip, who were referred for study inclusion by their GPs if they were eligible for inclusion.6 The inclusion period ran from October 2002 until September 2005. Inclusion criteria for the CHECK study were pain and/or stiffness of the knee and/or hip; aged between 45 and 65 years; and never having, or less than 6 months prior to entry of the study, consulted a physician for these symptoms. Participants were excluded if they had any other known pathological condition that could explain the existing complaints (for example, other rheumatic disease, previous hip or knee joint replacement, congenital dysplasia, osteochondritis dissecans, intra-articular fractures, septic arthritis, Perthes disease, ligament or meniscus damage, plica syndrome, or Baker’s cyst); comorbidity that did not allow physical evaluation and/or follow-up of at least 10 years; malignancy in the past 5 years; and inability to understand the Dutch language.6
All CHECK participants filled in questionnaires and underwent physical examination, X-rays, and laboratory examinations at five different time points during the 10-year follow-up. These time points were at baseline, at T2 (2 years), T5 (5 years), T8 (8 years), and T10 (10 years). Details of these examinations are specified in the following paragraphs and in Table 1.
Table 1.
Baseline characteristics of the participants with a completed follow-up of 6 yearsa
| Baseline characteristics | Total cohort | Knee pain subgroup | Hip pain subgroup | ||||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| N= 908 | TKA− n= 732 | TKA+ n= 19 | P -value | THA− n= 485 | THA+ n= 53 | P-value | |
| Age, years; mean ± SD | 55.8 ± 0.2 | 55.8 ± 0.2 | 58.0 ± 1.1 | 0.07 | 55.4 ± 0.2 | 58.0 ± 0.6 | <0.01b |
|
| |||||||
| Sex: female, % | 79 | 79 | 95 | 0.10 | 82% | 68% | 0.01b |
|
| |||||||
| Body mass index, kg/m2; mean ± SD | 26.2 ± 0.1 | 26.3 ± 0.2 | 29.1 ± 1.0 | <0.01b | 26.3 ± 0.2 | 25.9 ± 0.5 | 0.60 |
|
| |||||||
| Ethnic group (white versus other), % | 98 | 97 | 100 | 0.47 | 98 | 100% | 0.32 |
|
| |||||||
| Education level | |||||||
| % ≤ high school graduate, % | 73 | 73 | 84 | 73 | 77 | ||
| % college or university degree, % | 27 | 27 | 16 | 0.29 | 27 | 23 | 0.55 |
|
| |||||||
| Participants (%) with >1 comorbidity, % | 45 | 46 | 47 | 0.91 | 52 | 40 | 0.13 |
|
| |||||||
| NRS of the past week, mean (IQR) | 3.5 (2.0–5.0) | 3.5 (2.0–5.0) | 4.5 (3.0–6.0) | 0.04b | 3.6 (2.0–5.0) | 4.3 (2.0–6.0) | 0.03b |
|
| |||||||
| WOMAC pain, mean (IQR) | 25 (10–35) | 25 (10–35) | 35 (20–40) | 0.02b | 27 (15–40) | 31 (15–45) | 0.07 |
|
| |||||||
| WOMAC physical function, mean (IQR) | 23 (10–34) | 24 (10–34) | 34 (20–44) | <0.01b | 25 (10–35) | 31 (18–40) | 0.02b |
|
| |||||||
| WOMAC joint stiffness, mean (IQR) | 33 (25–50) | 33 (25–50) | 47 (38–63) | <0.01b | 34 (25–50) | 38 (25–50) | 0.30 |
|
| |||||||
| Pain coping strategies, mean (IQR) | |||||||
| Pain transformation | 2.1 (1.8–2.5) | 2.2 (1.8–2.8) | 2.2 (1.8–2.5) | 0.67 | 2.2 (1.8–2.8) | 2.2 (1.8–2.7) | 0.67 |
| Distracting | 2.2 (1.8–2.6) | 2.2 (1.8–2.6) | 2.3 (1.8–2.8) | 0.69 | 2.2 (1.8–2.6) | 2.2 (1.8–2.8) | 0.55 |
| Reducing demands | 2.0 (1.7–2.3) | 2.0 (1.7–2.3) | 2.0 (1.3–2.7) | 0.83 | 2.0 (1.7–2.3) | 1.9 (1.7–2.3) | 0.16 |
| Resting/avoidance | 1.8 (1.4–2.2) | 1.8 (1.4–2.2) | 2.0 (1.6–2.4) | 0.09 | 1.8 (1.4–2.2) | 1.8 (1.5–2.0) | 0.93 |
| Worrying | 1.6 (1.2–1.8) | 1.6 (1.2–1.8) | 1.6 (1.2–2.0) | 0.87 | 1.6 (1.2–1.8) | 1.6 (1.2–1.9) | 0.79 |
| Retreating | 1.5 (1.1–1.9) | 1.6 (1.1–1.9) | 1.5 (1.1–1.7) | 0.56 | 1.5 (1.1–1.9) | 1.5 (1.0–1.7) | 0.34 |
|
| |||||||
| Smoker or previous smoker, % | 14 | 15 | 0 | 0.07 | 15 | 6 | 0.07 |
|
| |||||||
| Alcohol consumption, % | 78 | 77 | 65 | 0.23 | 79 | 71 | 0.18 |
|
| |||||||
| Use of pain medication, % | 38 | 38 | 21 | 0.13 | 39 | 34 | 0.45 |
|
| |||||||
| Morning stiffness knees <30 minutes, % | 53 | 62 | 83 | 0.06 | – | – | – |
|
| |||||||
| Morning stiffness hips <60 minutes, % | 36 | – | – | – | 55 | 64 | 0.20 |
|
| |||||||
| Heberden nodes hands, % | 48 | 48 | 56 | 0.53 | 50 | 59 | 0.22 |
|
| |||||||
| Bouchard swellings hands, % | 19 | 19 | 21 | 0.81 | 22 | 17 | 0.42 |
|
| |||||||
| ESR, mm/hour ± SD | 9.8 ± 0.3 | 10.1 ± 0.3 | 10.7 ± 1.7 | 0.77 | 9.9 ± 0.4 | 12.9 ± 1.4 | 0.05b |
|
| |||||||
| TKA− 1480 knees | TKA+ 22 knees | P1-value | THA− 1014 hips | THA+ 62 hips | P1-value | ||
|
| |||||||
| Palpable warmth of the knee joint, % | – | 3 | 18 | <0.01b | – | – | – |
|
| |||||||
| Joint space tenderness of the knee, % | – | 12 | 18 | 0.59 | – | – | – |
|
| |||||||
| Bony enlargements of the knee, % | – | 2 | 0 | 0.51 | – | – | – |
|
| |||||||
| Crepitus during knee flexion, % | – | 10 | 23 | <0.01b | – | – | – |
|
| |||||||
| Positive knee refill test (effusion), % | – | 4 | 14 | 0.02b | – | – | – |
|
| |||||||
| Painful active knee flexion, % | – | 13 | 36 | <0.01b | – | – | – |
|
| |||||||
| Painful active knee extension, % | – | 8 | 23% | 0.04b | – | – | – |
|
| |||||||
| ROM knee flexion, mean ± SD | – | 135° ± 0.2° | 127° ± 2.6° | <0.01b | – | – | – |
|
| |||||||
| ROM knee extension, mean ± SD | – | 3° ± 0.1° | 3° ± 0.8° | 0.94 | – | – | – |
|
| |||||||
| JSN knee score >0, % | – | 55 | 86 | 0.03b | – | – | – |
|
| |||||||
| Femoral or tibial OP score >0, % | – | 45 | 91 | <0.01b | – | – | – |
|
| |||||||
| Tibial attrition, % | – | 0 | 10 | <0.01b | – | – | – |
|
| |||||||
| Femoral or tibial sclerosis, % | – | 1 | 10 | <0.01b | – | – | – |
|
| |||||||
| Tibial spiking, % | – | 32 | 63 | 0.03b | – | – | – |
|
| |||||||
| K/L score 1 (versus K/L score 0), % | – | 39 | 86 | <0.01b | 26 | 72 | <0.01b |
|
| |||||||
| ROM hip flexion ≤ 115°, % | – | – | – | – | 41 | 68 | <0.01b |
|
| |||||||
| ROM hip internal rotation ≤ 15°, % | – | – | – | – | 4 | 26 | <0.01b |
|
| |||||||
| Painful active hip flexion, % | – | – | – | – | 17 | 48 | <0.01b |
|
| |||||||
| Painful active hip internal rotation, % | – | – | – | – | 16 | 46 | <0.01b |
|
| |||||||
| JSN hip score>0 (AP), % | – | – | – | – | 31 | 79 | <0.01b |
|
| |||||||
| JSN hip score>0 (FP), % | – | – | – | – | 11 | 60 | <0.01b |
|
| |||||||
| Acetabular or femoral OP score >0, % | – | – | – | – | 35 | 78 | <0.01b |
|
| |||||||
| Femoral subchondral sclerosis, % | – | – | – | – | 1 | 26 | <0.01b |
|
| |||||||
| Cam-type deformity (α angle >60°),c % | – | – | – | – | 11 | 38 | <0.01b |
|
| |||||||
| Dysplasia (Wiberg angle <25°),b % | – | – | – | – | 5 | 17 | <0.01b |
Subgroups are participants who did (+) or did not (−) undergo arthroplasty during the 6-year follow-up. P-values obtained with Student’s t-test or Pearson’s χ2 when appropriate. P1-values obtained with generalised estimating equations (GEE).
P-value <0.05.
Lower-quality radiographs mean that these angles were determined in fewer hips (THA+: 781 hips, THA−: 45 hips). AP = anteroposterior pelvic view radiograph. ESR = erythrocyte sedimentation rate. FP = faux profile radiograph. JSN = joint space narrowing. K/L = Kellgren and Lawrence. NRS = Numeric Rating Scale. OP = osteophyte. ROM = range of motion. THA = total hip arthroplasty. TKA = total knee arthroplasty. WOMAC = Western Ontario and McMaster osteoarthritis index.
How this fits in
Every year thousands of patients are at risk of incidence and progression of osteoarthritis (OA) and many become eligible for total joint replacement (TJR) because of severely progressed and disabling symptoms. Not all patients with lower joint OA undergo surgery, however. In many patients with recent-onset knee or hip pain, radiographic OA features already exist. Patients with more severe clinical or radiographic symptoms have an increased risk for undergoing TJR, within 6 years of onset of symptoms.
For the analyses of the current study, data were used from baseline (T0), T2, and T5. Two study subgroups were created: a subgroup of participants who reported knee pain at baseline and a subgroup who reported hip pain at baseline. An individual could be included in both the knee and hip subgroups.
Baseline characteristics
The CHECK study included a baseline medical history, physical examination, and radiographs of the knees and hips, which formed the different variables.6 The medical history was taken through questionnaires with which participant-specific self-reported data were assessed. The following diseases were considered to be comorbidities: asthma, chronic sinusitis, cardiovascular disease, high blood pressure, gastric ulcer, gallstones, liver disease, renal disease, diabetes, thyroid gland disease, epilepsy, cancer, severe skin disease, and other chronic musculoskeletal diseases. Symptom severity was assessed by the Numeric Rating Scale (NRS, range 0–10) and the Western Ontario and McMaster osteoarthritis index (WOMAC) for pain, stiffness, and physical functioning (range 0–100, with a higher score indicating worse health).6 To assess pain-coping behaviour, a six-scale Pain-Coping Inventory (PCI) was used: pain transformation; distraction; reducing demands; retreating; worrying; and resting. All six scales (33 items) were scored according to a four-point Likert scale ranging from 1 (hardly ever) to 4 (very often) in terms of frequency with which strategies are applied when dealing with pain.7 Physical examination of the joints was based on the clinical criteria for knee and hip OA.8,9 Regarding the knee this encompassed range of motion (ROM) of knee flexion and extension measured in degrees with a goniometer, palpable warmth, crepitus, joint space tenderness, bony enlargements, effusion, and painful ROM. The hip examination included ROM of hip internal and external rotation, measured in degrees with a goniometer, and painful ROM.
Radiographs
Radiographs were read paired and in sequence, but with the observers blinded to all other patient characteristics.10 Standardised radiographs of the tibiofemoral joints were made by a weight-bearing posteroanterior (PA) view, semi-flexed (7–10°) according to Buckland-Wright,6,11 and standardised weight-bearing anteroposterior (AP) radiographs of the pelvis were made along with a weight-bearing single faux profile (FP) radiograph of the hip.6,12 Radiographs were scored for individual OA features according to criteria described by Altman.13 Radiographic OA severity was defined by the Kellgren and Lawrence (K/L) classification.14 With regards to the knee, baseline medial or lateral joint space narrowing (JSN), femoral medial or lateral osteophytes (OP), and tibial medial or lateral OP are generally scored on a four-point scale (0 = normal; 1 = mild; 2 = moderate; and 3 = severe). In the present study, however, these variables were dichotomised into absent (score 0) and present (score 1–3). In addition, medial or lateral tibial bone attrition, and medial or lateral tibial or femoral sclerosis were scored as absent or present. Presence of spiking of the tibial spines was scored according to the atlas by Burnett.15 The hip radiographs were scored in a similar manner to the knees: superior or medial hip JSN, superior or inferior acetabular OP, superior or inferior femoral OP, inferior acetabular OP, and femoral subchondral sclerosis, were scored as absent or present.15 The α angles on AP pelvic view hip radiographs were measured to determine whether a cam-type deformity was present at baseline.16 The α angle measures the deviation of the femoral head from a normal spherical-shaped femoral head. Cam-type deformity is one of two types of femoroacetabular impingement, which is associated with the development of hip OA. For this analysis, an α angle >60° was defined as a cam-type deformity.16–18 In addition, the Wiberg angles on AP pelvic view radiographs were measured to determine the degree of dysplasia.19 The centre-edge angle of Wiberg is formed by a vertical line through the centre of the femoral head, perpendicular to the transverse axis of the pelvis (radiographic ‘teardrop’ landmark),20 and a line joining the head centre with the lateral rim of the acetabulum.21 Hips with Wiberg angle <25° were considered to be dysplastic.22 On the FP radiographs, superior or posterior JSN was scored as absent (that is, normal) or present.
Statistical analysis
Total knee arthroplasty (TKA) was assigned as the primary outcome measure in the knee subgroup and total hip arthroplasty (THA) in the hip subgroup. Whether TKA or THA was performed was registered through questionnaires and confirmed on radiographs. Differences in participant baseline characteristics were calculated using Student’s t-test or Pearson’s χ2 test when appropriate. In addition, joint-dependent characteristics were compared using generalised estimating equation (GEE) analysis, which adjusts for the existing correlation between the left and right knees of the same individual. To determine possible associations with study outcomes, multivariable models were built for both subgroups, taking into account the number of events (TJRs) per subgroup to avoid overfitting the models. The selection for including variables into the models was dependent on: statistically large differences in baseline value; clinical relevance of the variables; and no large co-linearity between variables (cut-off R>0.7). Attempts were made to select various types of characteristics (that is anamnestic, clinical, and radiographic findings) as variables for the final models.
Lastly, to assess possible more rapid clinical OA progression in patients from the TJR groups, the mean change in WOMAC pain and physical functioning scores were calculated (using Student’s t-test or GEE when appropriate). Comparisons were made between baseline and 2-year follow-up (T2) as WOMAC scores are not useful after TJR, and most TJR had not taken place by T2. The P-values indicate whether the change in mean WOMAC scores differed significantly between the TJR and non-TJR groups. Assessments were made of whether or not the change in distribution of K/L scores for the knees and hips between baseline and T2 differed between the groups, by calculating the difference in number of participants who progressed in or maintained the same K/L score, distinguishing participants with severe progression (that is, increase K/L score by >1 or >2, and so on, from those with slight progression (that is, increase K/L score by 1). Participants who underwent TJR before T2 were excluded from this last analysis. All analyses were performed using SPSS Statistical Package PASW version 20.0.
RESULTS
Baseline characteristics
In total, 1002 participants were initially included in CHECK, of whom 94 (9%) were lost to follow-up after 6 years. Of those lost to follow-up, 44 had been allocated to the knee subgroup, 16 to the hip subgroup, and 34 to both subgroups. One of those lost to follow-up had undergone TJR (one TKA at T2). There were no significant differences in baseline age, sex, body mass index (BMI), symptom severity (NRS, WOMAC pain, WOMAC-PF), and K/L score between those lost to follow-up (n = 94) and the rest of the cohort (n = 908). All those lost to follow-up were excluded from analyses. In total, 829 participants reported knee pain (knee subgroup) and 588 reported hip pain (hip subgroup) at baseline (415 participants reported pain in both knee and hip). After 6 years of follow-up, 72 participants underwent TJR: 19 participants underwent TKA in 22 knees; 53 participants underwent THA in 61 hips, and one participant underwent both TKA (one knee) and THA (one hip). Hence, in total 23 knees underwent TKA and 62 hips THA. All participants who underwent TJR reported pain at baseline in the corresponding hip or knee joint. Table 1 provides an overview of the baseline characteristics of the total cohort (n = 908), and the characteristics of the participants in the knee and hip subgroups. Most of the joint-dependent clinical findings and radiographic features for both the knees and hips differed significantly for participants who underwent TJR and those who did not.
Knee subgroup
The small number of events in the knee subgroup meant that only three variables were selected for the multivariable knee model. Multiple clinical findings differed significantly among the two knee groups; however, the difference in prevalence of painful active knee flexion was the largest. With regards to radiographic findings, JSN and osteophytes were strongly correlated with K/L score. Therefore, only K/L score was included in the multivariable model. BMI, painful active knee flexion, and K/L score all significantly contributed to the multivariable model. The obtained odds ratios (OR) presented in Table 2 indicate a higher risk for undergoing TKA.
Table 2.
Multivariable model of the knee pain subgroup for the association with total knee arthroplasty (TKA)a
| β | OR (95% CI) | P-value | |
|---|---|---|---|
| BMI, kg/m2 | 0.10 | 1.1 (1.0 to 1.2) | <0.01 |
| Painful active knee flexion | 1.35 | 3.8 (1.6 to 9.5) | <0.01 |
| K/L score 1 (versus K/L score 0) | 1.86 | 6.4 (1.7 to 23.4) | <0.01 |
Model obtained with generalised estimating equations (GEE). The obtained OR are unadjusted for age and sex; however, all three variables do remain significant after adjustment (data not presented). An OR >1 indicates an increased risk for undergoing TKA. β = regression coefficient (beta). BMI = body mass index. K/L = Kellgren and Lawrence. OR = odds ratio.
Hip subgroup
JSN (AP pelvic view) and osteophytes were strongly correlated with K/L score, hence only K/L score was included. A cam-type deformity proved not to contribute to the final model and was excluded. All other radiographic hip features were not strongly correlated and were included in the multivariable hip model. As for clinical findings of the hip, painful internal rotation and reduced hip flexion ≤115° had the largest differences in distribution and were not strongly correlated. This model was adjusted for age and sex. Table 3 provides the obtained OR, with a higher OR indicating a higher risk for undergoing THA.
Table 3.
Multivariable model of the hip pain subgroup for the association with total hip arthroplasty (THA)a
| β | OR (95% CI)b | P-value | |
|---|---|---|---|
| Painful active hip internal rotation | 1.65 | 5.2 (2.3 to 11.8) | <0.01 |
| ROM hip flexion ≤115° | 0.99 | 2.7 (1.2 to 6.2) | 0.02 |
| K/L score 1 (vs. 0) | 1.22 | 3.4 (1.2 to 9.4) | 0.02 |
| JSN on faux profile radiograph | 2.53 | 12.6 (4.8 to 33.2) | <0.01 |
| Dysplasia (Wiberg angle <25°) | 2.10 | 8.2 (2.6 to 25.5) | <0.01 |
| Femoral subchondral sclerosis | 2.18 | 8.8 (2.9 to 26.7) | <0.01 |
Model obtained with generalised estimating equations (GEE). An OR >1 indicates an increased risk for undergoing TKA (total knee arthroplasty).
OR adjusted for age and sex. β = regression coefficient (beta). JSN = joint space narrowing. K/L = Kellgren and Lawrence. OR = odds ratio. ROM = range of motion.
WOMAC change between baseline and T2
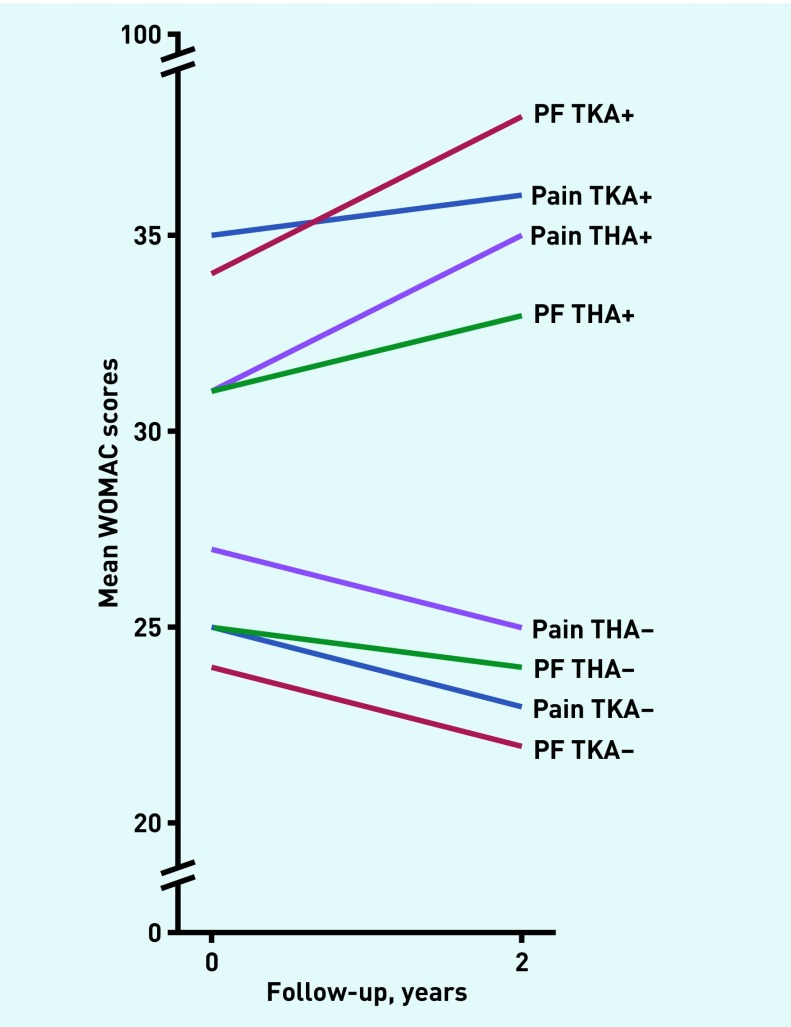
Table 4 provides an overview of the mean change in WOMAC pain and physical function score between baseline (T0) and T2 values for the different groups. One participant (one knee) from the knee subgroup underwent TKA and 13 participants (14 hips) from the hip subgroup underwent THA before T2. They were excluded from this analysis. Only the mean change in WOMAC pain score differs significantly between the THA and non-THA groups. There is a noticeable trend in WOMAC score increase among participants from the TJR groups, and a decrease among participants from the non-TJR group (Figure 1). The change in distribution of K/L scores between baseline (T0) and T2 for both the knees and hips differed significantly among the TJR and non-TJR groups: more joints in the TJR groups showed radiographic progression (Table 4).
Table 4.
Mean change in WOMAC score and change in K/L distribution between baseline (T0) and 2-year follow up (T2)a
| Knee pain at baseline | Hip pain at baseline | ||||||
|---|---|---|---|---|---|---|---|
| TKA− | TKA+ | THA− | THA+ | ||||
| Variable | T0–T2 (n= 732) | T0–T2 (n= 18) | P-value mean Δ | T0–T2 (n= 485) | T0–T2 (n= 40) | P-value mean Δ | |
| WOMAC pain | −1.7 (0.6) | 4.4 (3.5) | 0.12b | −1.2 (0.8) | 4.7 (2.7) | 0.04b | |
| WOMAC physical function | −1.3 (0.5) | 4.9 (4.8) | 0.07b | −1.1 (0.7) | 3.0 (2.1) | 0.10b | |
| Distribution of K/L score 0/1/2/3/4 (%) | T0 T2 |
1479 knees 61/39/0/0/0 50/36/13/1/0 |
21 knees 14/86/0/0/0 5/15/55/20/5 |
<0.01c | 1002 hips 74/26/0/0/0 68/30/2/0/0 |
48 hips 28/72/0/0/0 23/23/35/14/5 |
<0.01c |
Values are mean change between T0 and T2 (standard error), or percentages %. P-values obtained with
Student’s t-test or
generalised estimating equations (GEE) and indicate whether the change in mean values (Δ) or in distribution of K/L score differ significantly. Progression of K/L score adjusted for baseline K/L score. K/L = Kellgren and Lawrence. T0 = baseline. T2 = 2-year follow-up. THA = total hip arthroplasty. TKA = total knee arthroplasty. WOMAC = Western Ontario and McMaster osteoarthritis index.
Figure 1.
Depiction of the mean change in WOMAC scores from baseline to 2-year follow-up (T2). PF = physical functioning. THA = total hip arthroplasty. TKA = total knee arthroplasty. WOMAC = Western Ontario and McMaster osteoarthritis index.
DISCUSSION
Summary
Relevant patient and disease characteristics associated with undergoing TJR were found in comparatively young participants with recent-onset knee and/or hip OA in a nationwide prospective cohort study. In participants with recent-onset knee OA, significant differences in baseline BMI, symptom severity (NRS and all three WOMAC subscales), clinical findings, and radiographic OA severity were seen between participants who underwent TKA during follow-up and those who did not. In a subgroup of participants with recent-onset hip OA, significant differences in baseline age, sex distribution, symptom severity (NRS and WOMAC physical function), clinical findings, hip morphology, and radiographic OA severity were found between participants who underwent THA during follow-up and those who did not. The participants who underwent THA were slightly, but statistically significantly, older at baseline (mean difference 2.6 years). The association between a higher age and hip OA progression has previously been established in a systematic review by Wright et al.23 There remains conflicting evidence with regards to the association between sex and hip OA progression.23–25
Strengths and limitations
A limitation to the data under study is that, although participants were asked where the pain was located (knee and/or hip; left and/or right), the participants were not asked to which joint the NRS and WOMAC subscales assessments refer to. Consequently, an individual with both hip and knee, or bilateral symptoms, could experience more pain and as a result have higher symptom scores. On the other hand, it might be difficult for an individual to score his or her pain separately for affected joints. Nevertheless, the above-mentioned limitation could have led to some bias in the data.
Comparison with existing literature
In two systematic reviews on prognostic factors for knee OA progression the authors report conflicting evidence for the association between BMI and knee OA progression.26,27 In the knee subgroup in the present study, there was a significant, and perhaps more importantly, clinically relevant difference in baseline mean BMI between the TJR and non-TJR groups (mean difference 2.8 kg/m2). Moreover, BMI remained significantly associated with undergoing TKA in the multivariable model. In accordance with existing literature, no association was found between BMI and hip OA. This suggests that biomechanical factors such as hip dysplasia or cam-type deformity could play a greater role in the development of hip OA.
Baseline symptoms (NRS and WOMAC subscales) were significantly more severe in both TJR groups. This is in line with previous longitudinal studies showing that patients with higher pain or disability scores at baseline are more likely to undergo TJR.28–30 The mean age of these study populations (72, 65, and 67 years, respectively), however, were higher than in the TJR groups (58 years). Unfortunately, symptom severity remains subjective and subsequently does not always form a clear indication for the GP to distinguish which patients are eligible for referral for TJR.
The participants from both the TJR groups significantly more often had typical OA symptoms during physical examination of the knee or hip, consistent with the criteria for clinical knee and hip OA.8,9 In longitudinal studies by Birrell et al 31 and Lievense et al,32 the authors found associations for hip ROM and painful hip movements with hip replacement surgery in similar study populations. This is in line with the present findings, but again the mean age of the present THA group was comparatively low (58 years compared with 63 and 66 years, respectively).
Participants who underwent TKA significantly more often showed radiographic knee OA features.9 The corresponding radiographs also had worse JSN, sclerosis, tibial attrition, and tibial spiking. Participants who underwent THA significantly showed more radiographic features of hip OA.8 They also more often showed JSN on the faux profile, dysplasia, and femoral subchondral sclerosis. Furthermore, the radiographs from the TJR groups more often showed cam-type deformity (α angle >60°) and hip dysplasia (Wiberg angle <25°), of which the associations with hip OA have previously been established.16,18,24,33,34 Additionally, the present study found that participants from both the TJR groups showed earlier, more rapid radiographic progression of OA. All these above-mentioned findings suggest that participants who underwent TJR were in a more advanced stage of the disease at baseline. Alternatively, these findings could also suggest that participants from the TJR groups had a different underlying pathophysiology or phenotype of OA and therefore were prone to more rapid deterioration of the joint.4,5
Lastly, at T2 a comparatively large percentage of patients from the TJR groups still only had K/L score <2 (20% of the TKA group and 46% of the THA group). This is a rather remarkable observation from the data, considering that most clinical guidelines advise GPs not to request radiographic investigations at an early stage of OA,35–37 and that structural damage to the joint has proven to be a strong indicator for orthopaedic surgeons to consider TJR.38 This causes a discrepancy between evidence-based guidelines and clinical practice, and should be further evaluated in future studies. Unfortunately, necessary additional information to clarify this finding was not incorporated in the present data. Until this discrepancy is better understood, it seems justifiable that the existing recommendations not to request radiographs at an early stage should be enforced.
Implications for research and practice
This study has established in a comparatively young OA study population that, in many patients with recent-onset knee or hip pain, radiographic OA features already exist. Moreover, patients with more severe clinical or radiographic symptoms have an increased risk for undergoing TJR within a 6-year follow-up. These findings suggest that the cascade of joint destruction may commence at a far earlier stage than the onset of symptomatic disease,39 given that many participants showed radiographic OA features at baseline. Future research should be aimed at establishing clear criteria, both symptomatic and radiographic, for undergoing TJR, which will better guide the GP in their decision for referral. Until these criteria are developed, GPs should refrain from unnecessary X-rays in accordance with the current OA guidelines.35–37 It somehow seems justifiable, however, for a GP to request X-rays if they are consulted by a comparatively young patient (<55 years) with severe-onset hip or knee pain caused by OA (NRS >5).
Acknowledgments
The authors would like to thank all participants of the CHECK cohort and all collaborators of the different sites for their efforts. CHECK is funded by the Dutch Arthritis Association and led by a steering committee comprising 16 members with expertise in different fields of osteoarthritis chaired by Professor JWJ Bijlsma and coordinated by J Wesseling. Involved are: Erasmus MC University Medical Center Rotterdam; Academic Hospital Maastricht; Jan van Breemen Institute/VU Medical Center Amsterdam; Kennemer Gasthuis Haarlem; Martini Hospital Groningen/Allied Health Care Center for Rheumatology and Rehabilitation Groningen; Medical Spectrum Twente Enschede/Twenteborg Hospital Almelo; St Maartenskliniek Nijmegen; Leiden University Medical Center; University Medical Center Utrecht; and Wilhelmina Hospital Assen.
Funding
This study is partly funded by a programme grant from the Dutch Arthritis Foundation for its centre of excellence ‘Osteoarthritis in primary care’. The entire research department for general practice is partly funded by the Dutch Arthritis Foundation.
Ethical approval
Medical ethics committees of all participating centres of the Cohort Hip and Cohort Knee (CHECK) study approved the study, and all participants in CHECK gave written informed consent.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Hsiao CJ, Cherry DK, Beatty PC, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2007 summary. Natl Health Stat Report. 2010;27:1–32. [PubMed] [Google Scholar]
- 2.Neogi T, Zhang Y. Epidemiology of osteoarthritis. Rheum Dis Clin North Am. 2013;39(1):1–19. doi: 10.1016/j.rdc.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Delaunay C. Registries in orthopaedics. Orthop Traumatol Surg Res. 2015;101(1 Suppl):S69–S75. doi: 10.1016/j.otsr.2014.06.029. [DOI] [PubMed] [Google Scholar]
- 4.Kinds MB, Marijnissen AC, Viergever MA, et al. Identifying phenotypes of knee osteoarthritis by separate quantitative radiographic features may improve patient selection for more targeted treatment. J Rheumatol. 2013;40(6):891–902. doi: 10.3899/jrheum.121004. [DOI] [PubMed] [Google Scholar]
- 5.Bijlsma JW, Berenbaum F, Lafeber FP. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377(9783):2115–2126. doi: 10.1016/S0140-6736(11)60243-2. [DOI] [PubMed] [Google Scholar]
- 6.Wesseling J, Dekker J, van den Berg WB, et al. CHECK (Cohort Hip and Cohort Knee): similarities and differences with the Osteoarthritis Initiative. Ann Rheum Dis. 2009;68(9):1413–1419. doi: 10.1136/ard.2008.096164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kraaimaat FW, Evers AW. Pain-coping strategies in chronic pain patients: psychometric characteristics of the pain-coping inventory (PCI) Int J Behav Med. 2003;10(4):343–363. doi: 10.1207/s15327558ijbm1004_5. [DOI] [PubMed] [Google Scholar]
- 8.Altman R, Alarcon G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34(5):505–514. doi: 10.1002/art.1780340502. [DOI] [PubMed] [Google Scholar]
- 9.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29(8):1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 10.Damen J, Schiphof D, Wolde ST, et al. Inter-observer reliability for radiographic assessment of early osteoarthritis features: the CHECK (cohort hip and cohort knee) study. Osteoarthritis Cartilage. 2014;22(7):969–974. doi: 10.1016/j.joca.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 11.Buckland-Wright C. Protocols for precise radio-anatomical positioning of the tibiofemoral and patellofemoral compartments of the knee. Osteoarthritis Cartilage. 1995;3(Suppl A):71–80. [PubMed] [Google Scholar]
- 12.Lequesne MG, Laredo JD. The faux profil (oblique view) of the hip in the standing position. Contribution to the evaluation of osteoarthritis of the adult hip. Ann Rheum Dis. 1998;57(11):676–681. doi: 10.1136/ard.57.11.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15(Suppl A):A1–A56. doi: 10.1016/j.joca.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 14.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burnett S, Hart DJ, Cooper C, Spector TD. A radiographic atlas of osteoarthritis. London: Springer Verlag; 1994. [Google Scholar]
- 16.Agricola R, Heijboer MP, Bierma-Zeinstra SM, et al. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK) Ann Rheum Dis. 2013;72(6):918–923. doi: 10.1136/annrheumdis-2012-201643. [DOI] [PubMed] [Google Scholar]
- 17.Allen D, Beaule PE, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg Br. 2009;91(5):589–594. doi: 10.1302/0301-620X.91B5.22028. [DOI] [PubMed] [Google Scholar]
- 18.Agricola R, Waarsing JH, Thomas GE, et al. Cam impingement: defining the presence of a cam deformity by the alpha angle: data from the CHECK cohort and Chingford cohort. Osteoarthritis Cartilage. 2014;22(2):218–225. doi: 10.1016/j.joca.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 19.Wiberg G. Shelf operation in congenital dysplasia of the acetabulum and in subluxation and dislocation of the hip. J Bone Joint Surg Am. 1953;35-A(1):65–80. [PubMed] [Google Scholar]
- 20.Vare VB., Jr The anatomy of the pelvic tear figure. J Bone Joint Surg Am. 1952;34-A(1):167–169. [PubMed] [Google Scholar]
- 21.Laborie LB, Engesaeter IO, Lehmann TG, et al. Radiographic measurements of hip dysplasia at skeletal maturity — new reference intervals based on 2,038 19-year-old Norwegians. Skeletal Radiol. 2013;42(7):925–935. doi: 10.1007/s00256-013-1574-y. [DOI] [PubMed] [Google Scholar]
- 22.Tonnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976;119:39–47. [PubMed] [Google Scholar]
- 23.Wright AA, Cook C, Abbott JH. Variables associated with the progression of hip osteoarthritis: a systematic review. Arthritis Rheum. 2009;61(7):925–936. doi: 10.1002/art.24641. [DOI] [PubMed] [Google Scholar]
- 24.Bierma-Zeinstra SM, Koes BW. Risk factors and prognostic factors of hip and knee osteoarthritis. Nat Clin Pract Rheumatol. 2007;3(2):78–85. doi: 10.1038/ncprheum0423. [DOI] [PubMed] [Google Scholar]
- 25.Lievense AM, Bierma-Zeinstra SM, Verhagen AP, et al. Prognostic factors of progress of hip osteoarthritis: a systematic review. Arthritis Rheum. 2002;47(5):556–562. doi: 10.1002/art.10660. [DOI] [PubMed] [Google Scholar]
- 26.Bastick AN, Runhaar J, Belo JN, Bierma-Zeinstra SM. Prognostic factors for progression of clinical osteoarthritis of the knee: a systematic review of observational studies. Arthritis Res Ther. 2015;17:152. doi: 10.1186/s13075-015-0670-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chapple CM, Nicholson H, Baxter GD, Abbott JH. Patient characteristics that predict progression of knee osteoarthritis: a systematic review of prognostic studies. Arthritis Care Res (Hoboken) 2011;63(8):1115–1125. doi: 10.1002/acr.20492. [DOI] [PubMed] [Google Scholar]
- 28.Hawker GA, Guan J, Croxford R, et al. A prospective population-based study of the predictors of undergoing total joint arthroplasty. Arthritis Rheum. 2006;54(10):3212–3220. doi: 10.1002/art.22146. [DOI] [PubMed] [Google Scholar]
- 29.McHugh GA, Campbell M, Luker KA. GP referral of patients with osteoarthritis for consideration of total joint replacement: a longitudinal study. Br J Gen Pract. 2011. DOI: https://doi.org/10.3399/bjgp11X588420. [DOI] [PMC free article] [PubMed]
- 30.Conaghan PG, D’Agostino MA, Le Bars M, et al. Clinical and ultrasonographic predictors of joint replacement for knee osteoarthritis: results from a large, 3-year, prospective EULAR study. Ann Rheum Dis. 2010;69(4):644–647. doi: 10.1136/ard.2008.099564. [DOI] [PubMed] [Google Scholar]
- 31.Birrell F, Afzal C, Nahit E, et al. Predictors of hip joint replacement in new attenders in primary care with hip pain. Br J Gen Pract. 2003;53(486):26–30. [PMC free article] [PubMed] [Google Scholar]
- 32.Lievense AM, Koes BW, Verhaar JA, et al. Prognosis of hip pain in general practice: a prospective followup study. Arthritis Rheum. 2007;57(8):1368–1374. doi: 10.1002/art.23094. [DOI] [PubMed] [Google Scholar]
- 33.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 34.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466(2):264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.NHG. The Dutch College of General Practitioners. NHG Standard for non-traumatic knee complaints. [In Dutch] Huisarts Wet. 2008;5:229–240. [Google Scholar]
- 36.National Institute for Health and Care Excellence. Osteoarthritis: care and management. CG177. London: NICE; 2014. https://www.nice.org.uk/guidance/cg177 (accessed 12 Jul 2017) [Google Scholar]
- 37.[No authors listed]. Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Arthritis Rheum. 2000;43(9):1905–1915. doi: 10.1002/1529-0131(200009)43:9<1905::AID-ANR1>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 38.Maillefert JF, Roy C, Cadet C, et al. Factors influencing surgeons’ decisions in the indication for total joint replacement in hip osteoarthritis in real life. Arthritis Rheum. 2008;59(2):255–262. doi: 10.1002/art.23331. [DOI] [PubMed] [Google Scholar]
- 39.Wluka AE. Remember the Titanic: what we know of knee osteoarthritis is but the tip of the iceberg. J Rheumatol. 2006;33(11):2110–2112. [PubMed] [Google Scholar]