Abstract
Objective:
We investigated the impact of deep inspiration breath-hold (DIBH) and tumour baseline shifts on image quality and registration uncertainty in image-guided DIBH radiotherapy (RT) for locally advanced lung cancer.
Methods:
Patients treated with daily cone beam CT (CBCT)-guided free-breathing (FB) RT had an additional CBCT in DIBH at three fractions. These CBCT scans were offline rigidly registered (on tumour) to FB and DIBH CT scans acquired at planning. All registrations were repeated to evaluate the intraobserver uncertainty. CBCT scans were scored on degree of streak artefacts and visualization of tumour and anatomical structures. We examined the impact of tumour baseline shift between consecutive DIBHs on CBCT image quality.
Results:
CBCT scans from 15 patients were analysed. Intraobserver image registration uncertainty was approximately 2 mm in both FB and DIBH, except for the craniocaudal direction in FB, where it was >3 mm. On the 31st fraction, the intraobserver uncertainty increased compared with the second fraction. This increase was more pronounced in FB. Image quality scores improved in DIBH compared with FB for all parameters in all patients. Simulated tumour baseline shifts ≤2 mm did not affect the CBCT image quality considerably.
Conclusion:
DIBH CBCT improved image quality and reduced registration uncertainty in the craniocaudal direction in image-guided RT of locally advanced lung cancer. Baseline shifts ≤2 mm in DIBH during CBCT acquisition did not affect image quality.
Advances in knowledge:
DIBH RT has dosimetric advantages over FB; this work demonstrates an additional benefit of DIBH in terms of registration accuracy because of improved image quality.
INTRODUCTION
In modern radiotherapy (RT), daily image guidance is crucial to ensure safe and precise treatment with minimized margins. For RT of lung cancer, daily cone beam CT (CBCT) is considered the optimal choice for image guidance, since it enables visualization of the tumour and the bony anatomy.1
The volumetric acquisition of a CBCT reduces the image quality compared with a diagnostic CT, mainly due to scattered radiation. In the thoracic region, the image quality is further impaired by the motion of the organs during the relatively long acquisition time, resulting in blurring and streak artefacts.2,3
The image quality of thoracic CBCT can be improved by managing the respiratory motion, for example, using deep inspiration breath-hold (DIBH); however, this is feasible only if the patient is treated in DIBH as well. RT delivery in DIBH has been reported for stereotactic body RT (SBRT) of lung tumours,4–8 as well as for fractionated radiation of locally advanced lung cancer9–12 and shows a potential for lung toxicity reduction as the lung volume increases in DIBH.13,14 Initial experience with DIBH CBCT as image guidance has been reported for SBRT,6,8,15,16 whereas the only study focusing on image guidance in DIBH for locally advanced disease used continuous CBCT acquisition, including both DIBH and periods of free breathing (FB) during CBCT acquisition.17
Although geometrical uncertainties in both voluntary18 and forced DIBH have been reported,19,20 uncertainties of the image registration process have not yet been investigated. Since CBCT acquisition typically takes 1 min, it exceeds the maximum tolerable DIBH duration, and therefore, several DIBHs are needed to acquire a single CBCT. Owing to intrafractional tumour baseline shifts between repeated DIBHs,18,21 image quality may be impaired. In this study, the impact of both DIBH and tumour baseline shifts between consecutive DIBHs on image quality of CBCT was investigated. We compared the CBCT image quality in FB and DIBH and investigated its impact on image registration uncertainties throughout the RT course for patients with locally advanced lung cancer.
METHODS AND MATERIALS
17 patients with locally advanced non-small-cell lung cancer referred for radical RT were included in a study on evaluation of geometrical uncertainties in the tumour position during DIBH, measured from consecutive DIBH CT scans.18 The inclusion criterion was the ability to perform voluntary DIBH for 20 s. The study was approved by the local ethical committee (H-2-2011-153).
Phantom study
The observed tumour baseline shifts between consecutive DIBHs in this patient cohort were <2 mm for 85% of the cases but ranged up to 5 mm.18 In order to investigate the influence of inter-DIBH baseline shifts on CBCT image quality without the presence of deformations, we acquired CBCT scans of a phantom (Intensity-modulated RT thorax phantom; Computerized Imaging Reference Systems Inc., Norfolk, VA) with a cylindrical 9-mm-high nodule with half-sphere (radius 9 mm) on top, inserted to emulate a lung tumour. A planning CT scan and four CBCT scans were acquired: one with continuous CBCT acquisition (CBCT0) and three with CBCT acquisition interrupted after 120° and 240° to mimic 20-s DIBHs. After each interruption inter-DIBH baseline shifts of 1, 2 or 5 mm were simulated, resulting in scans CBCT1, CBCT2, and CBCT5. The size and shape of the tumour nodule on the CBCT scans was compared with its size and shape on planning CT.
Patients study
Standard imaging protocol at Rigshospitalet's Department of Oncology for RT planning of patients with locally advanced non-small-cell lung cancer consists of a FB fluorine-18 fludeoxyglucose positron emission tomography/CT, a four-dimensional CT and a voluntary DIBH CT with the patient immobilized in a chest board (ConChest; Candor ApS, Gislev, Denmark). The patients were treated in FB (66 Gy in 33 fractions) using the midventilation approach22. Daily CBCT scans were used as image guidance, and were registered onto the planning CT scans, with focus on the tumour area. Daily treatments and CBCT scans were performed using Varian iX trilogy linear accelerators (Varian Medical Systems Inc., Palo Alto, CA). At treatment fractions 2, 16 and 31, 1 additional CBCT scan in visually guided DIBH was obtained immediately after radiation delivery. Both FB and DIBH CBCT scans were acquired with low thorax protocol (110 kV, 20 mA, 20 ms and full gantry rotation). As it takes 60 s to acquire a CBCT, the acquisition was split into three segments of approximately 20 s DIBH (each acquiring 120° of image projections). After each DIBH the CBCT acquisition was manually interrupted, the patient breathed freely, and after his/her regular respiration was restored, the patient was asked to take another DIBH, and CBCT acquisition was resumed.
The patients' respiration during four-dimensional CT and DIBH was monitored with Real-time Position Management™ system (Varian Medical Systems Inc., Palo Alto, CA), which consists of an infrared camera, tracking the respiratory signal from an optical marker placed at the xiphoid process. Each patient had one 15-min long coaching session, which took place just before imaging for treatment planning; during this session, the DIBH level was individually set to a comfortable level. For all DIBH acquisitions, the patient was prompted by the radiation therapist to take a DIBH, and the DIBH level was provided to the patient through visual feedback for all imaging sessions, as described in Damkjær et al.23
Image registration uncertainty and image quality were evaluated in the image registration module of the Eclipse™ treatment planning system (Varian Medical Systems Inc., Palo Alto, CA), using pre-defined window settings (Hounsfield unit range between −1000 and 250). CBCT scans in FB and DIBH from treatment fractions 2, 16 and 31 were offline rigidly registered based on tumour gray values, not the delineated gross tumour volume to the planning day's FB CT and DIBH CT, respectively. All registrations were performed twice by the same observer at different time points; the standard deviation of the differences between two repeated sets of image registration uncertainty was considered a measure of intraobserver variation in image registration. We evaluated the intraobserver uncertainties for FB and DIBH, and for potential time trend throughout the treatment course.
To assess the image quality, the CBCT scans were visually evaluated by a single observer and scored on degree of streak artefacts, and visualization of tumour, main bronchi, lung vessels, and fissures. Since there is no golden standard for evaluation of image quality in patient images, we chose criteria similar to those of Sweeney et al,24 using a scale of 1–3, scoring 1 for best and 3 for worst quality. We applied these criteria on each of the five image quality parameters stated above. Image with the ideal quality would score 5, whereas worst score would be 15. The detailed description of the scoring criteria is presented in Table 1.
Table 1.
Scoring criteria for cone beam CT image quality assessment
| Image quality parameter | Score 1 = comparable to planning CT | Score 2 = fair | Score 3 = bad |
|---|---|---|---|
| Streak artefacts | Absent | Medium degree | High degree |
| Visualization of primary tumour | Clearly visible/distinguished border between tumour and background | Visible, but border between tumour and background not clearly distinguished | Tumour smeared out/non-distinguished border between tumour and background |
| Visualization of carina and main bronchi | Clearly visible | Visible, but without clear borders | Not visible |
| Visualization of larger vessels | Clearly visible | Visible to a certain degree | Not visible |
| Visualization of lung fissures | Clearly visible | Visible to a certain degree | Not visible |
RESULTS
Phantom study
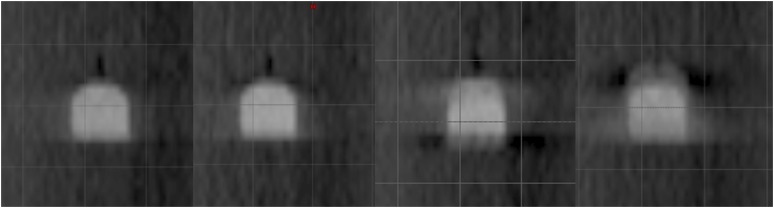
Simulating tumour baseline shift on the thorax phantom resulted in elongated visualization of the tumour, approximately 3 mm for 2-mm baseline shifts and approximately 8 mm for 5-mm baseline shifts. Simulated tumour baseline shifts ≤2 mm did not affect the image quality considerably, whereas the 5-mm shifts smeared out the tumour nodule, with only the middle part of it maintaining the density comparable to that of the planning CT (Figure 1).
Figure 1.
Simulation of baseline shifts between consecutive deep inspiration breath-holds for cone beam CT acquisition. From left to right: no baseline shifts, 2 × 1-mm shift, 2 × 2-mm shift and 2 × 5-mm shift. Note the deterioration in image quality with baseline shift increase.
Patient results
Data from 15 patients were eligible for this analysis (patient no. 2 left the study due to decrease in general performance status, patient no. 12 could no longer comply with DIBH). 2 patients (nos. 4 and 8) did not receive the full course of RT and therefore imaging at the 31st fraction was not possible. Owing to logistical issues, eight DIBH CBCT scans were not acquired. Therefore, only 35 sets (of the potential 45) of FB and DIBH CBCT were available for the analysis of image quality. The DIBH CT in patient no. 7 was erroneously reconstructed with 10-mm slices instead of 2 mm, and this data set was excluded because the decreased longitudinal image resolution would have a large impact on the registration uncertainty. Therefore, only 33 image sets were available for the evaluation of the image registration uncertainty. The CBCT acquisition in FB took 1 min and in DIBH took 2–3 min.
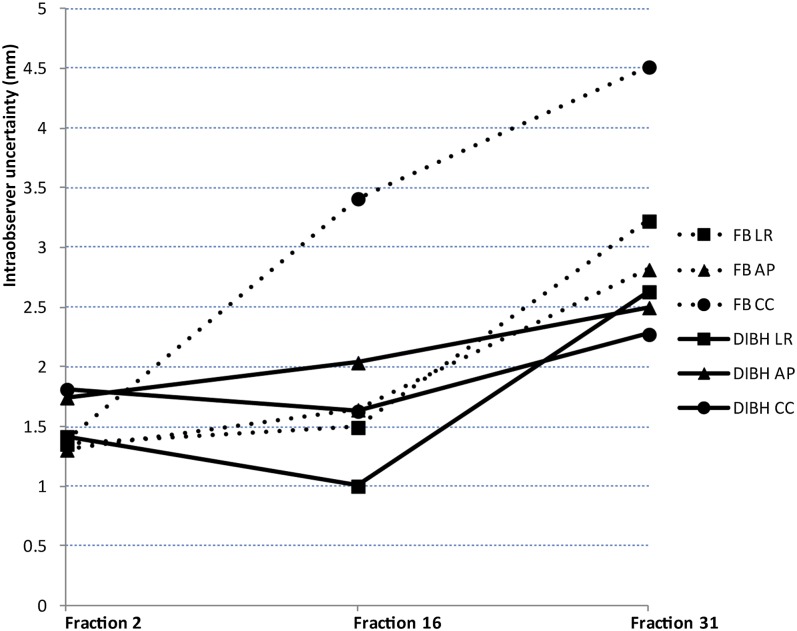
Overall intraobserver uncertainty in image registration was approximately 2 mm in both FB and DIBH CBCT, with the exception of the craniocaudal (CC) direction of FB, where it exceeded 3 mm (Table 2). Intraobserver uncertainty in image registration at Fraction 31 increased compared with the uncertainty at Fraction 2; this increase was most pronounced in the CC direction for FB CBCT and the least pronounced in the anteroposterior (AP) and CC directions for DIBH CBCT (Figure 2).
Table 2.
Overall intraobserver uncertainties in image registration
| Image acquisition type | LR (mm) | AP (mm) | CC (mm) |
|---|---|---|---|
| FB | 2.2 | 1.9 | 3.2 |
| DIBH | 1.7 | 2.1 | 1.9 |
LR, left–right; AP, anteroposterior; CC, craniocaudal; FB, free breathing; DIBH, deep inspiration breath-hold.
Figure 2.
The intraobserver uncertainty in image registration throughout the treatment course. LR, left–right; AP, anteroposterior; CC, craniocaudal; FB, free breathing; DIBH, deep inspiration breath-hold.
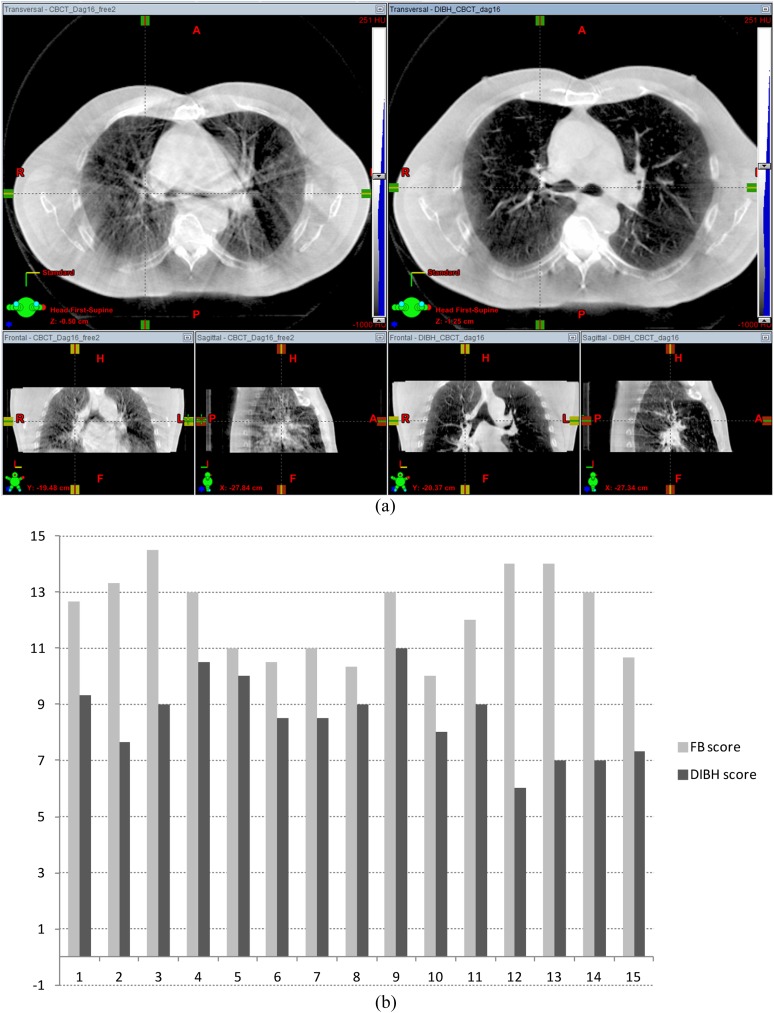
For all image quality parameters, DIBH CBCT scored better than FB CBCT, with summed averaged scores for all parameters 8.4 for DIBH vs 12.2 in. A typical patient example is shown in Figure 3a. The DIBH improved image quality of the CBCT in all patients (Figure 3b). The impact of DIBH was the largest on visibility of large vessels and the absence of streak artefacts: large vessels were clearly visible on 11% of the FB and 94% of the DIBH CBCT scans, whereas a high degree of streak artefacts was reduced from 57% in FB to 6% in the DIBH CBCT scans.
Figure 3.
Deep inspiration breath-hold (DIBH) improved the image quality. (a) Cone beam CT (CBCT) of patient no. 4, taken at the 16th fraction; on the left—free breathing (FB) CBCT (maximum image quality score of 15) and on the right—DIBH CBCT (image quality Score 8, corresponding to the median score for DIBH). (b) CBCT image quality score improvement presented per patient. High score corresponds to poor image quality. Range of possible scores: 3–15.
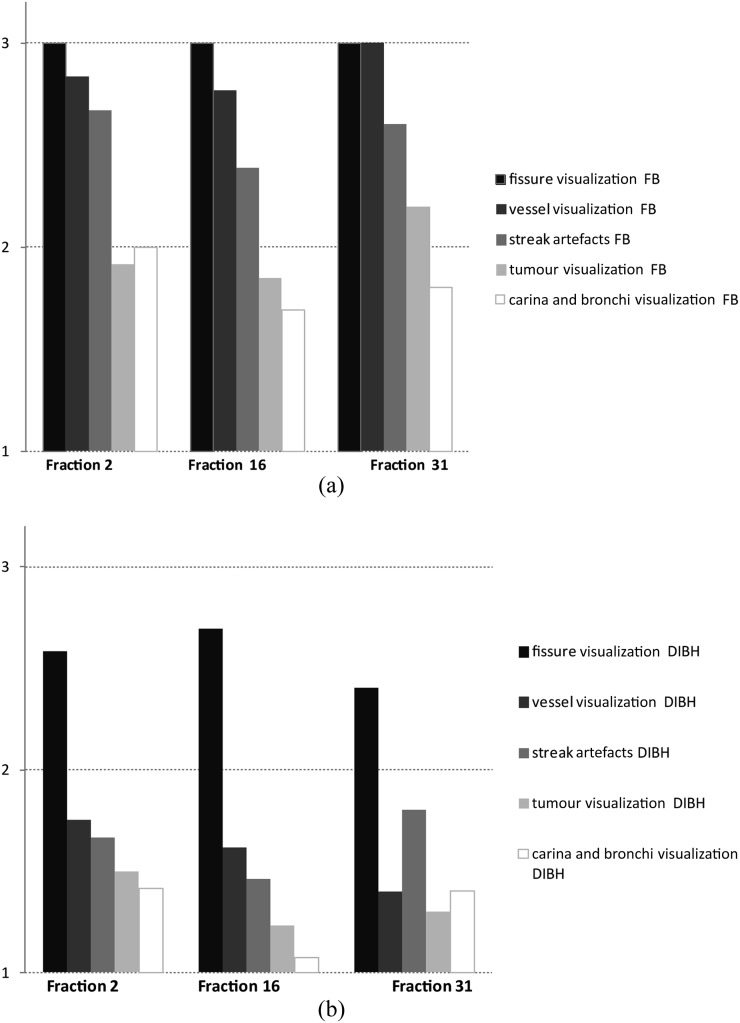
Tumour visualization was very good on 20% of FB and 66% of DIBH CBCT scans and very poor on 14% of the FB CBCT scans. The visualization of the main bronchi and carina was very clear on 40% of the FB and 74% of the DIBH CBCT scans and impossible on 14% of the FB and 3% of the DIBH CBCT scans. The impact of DIBH was the smallest on lung fissures visibility. Overall, the DIBH either improved or did not affect every single image quality parameter compared with the FB CBCT acquired on the same day and hence improved the image quality score. More details are presented in Figure 4.
Figure 4.
Normalized image quality scores averaged over all patients, presented for (a) free breathing (FB) and (b) deep inspiration breath-hold (DIBH): high score corresponds to poor image quality. The range of possible scores was 1 (optimal image quality) to 3 (bad quality).
Overall image quality scores did not differ between CBCT scans acquired at Fractions 2 and 31; however, the tumour visibility score in FB CBCT was worse at the 31st than at the 2nd fraction.
Image quality scores in FB CBCT had a moderate correlation with the FB tumour motion amplitude in the CC direction (Pearson correlation coefficient 0.43) and a weak correlation in the AP and left–right direction (Pearson correlation coefficients 0.23 and 0.08). The correlation between image quality scores and three-dimensional intrafractional baseline shift (as reported in Josipovic et al18) was weak (0.22).
DISCUSSION
RT in DIBH for patients with locally advanced lung cancer is not a common practice; however, the patients are highly compliant.12,18 In this study, we compared the image quality of CBCT in DIBH and FB for this patient group and assessed its impact on registration uncertainty. DIBH improved CBCT image quality in all patients. The visibility of both the primary tumour and the carina with main bronchi was improved. Furthermore, the DIBH CBCT enabled visualization of larger vessels and lung lobe fissures and decreased streak artefacts making the image quality comparable to that of the planning CT scans.
Duggan et al6 reported excellent image quality in DIBH for lung SBRT; however, they focused on image quality improvement compared with planar images (either radiographs or portal images), where a small tumour often is not visible, regardless of motion management. Zhong et al16 investigated image quality during a shorter CBCT acquisition without full gantry rotation, requiring a single DIBH of 40 s. Image quality was found sufficient for visualization of small tumours, but no comparison with other acquisition techniques was made. Our patients' DIBH durations were 20–30 s, only one patient performed a longer DIBH, therefore a 40-s DIBH acquisition may only be possible in very few selected patients, unless mechanical oxygen enhanced ventilation is applied.25 Boda-Heggemann et al15 reported on continuous acquisition of CBCT while the patient's respiration varied between DIBH and FB. They found the method produced a blurred tumour image with additional presence of a ghost tumour, representing the tumour's position in the FB. Nonetheless, they found the image quality acceptable for correct image registration on the tumour in SBRT. However, this may not be the case in locally advanced disease due to target complexity and occurrence of anatomical changes during 7 weeks of RT.
Li et al21 acquired CBCT scans during the treatment delivery of 20 patients receiving SBRT treated in either DIBH or FB. They observed a 2- to 3-mm blur surrounding the tumour, which indicated the presence of baseline shift. No separate results were presented for patients treated in DIBH (where the blur may result from a shift between several sequential DIBHs) or patients treated in FB (where the blur would be caused by continuous respiration motion). In our phantom measurements, similar blur was seen in simulated 2-mm baseline shifts. Still, the tumour baseline shifts ≤2 mm only had a minor effect on the image quality, and the correlation between the image quality scores and actual baseline shifts in DIBH was very weak. The patient with the worst DIBH CBCT image score of 12 was 1 of the 3 patients with baseline shifts >3 mm (as reported in Josipovic et al18); however, the other 2 patients had DIBH CBCT image scores of 8 and 11.
The increased image quality in DIBH per se in our patient cohort translated into a reduced registration uncertainty in the CC direction, whereas it remained similar in the AP and left–right directions. The observed increased registration uncertainty at the 31st fraction was more pronounced in FB than in DIBH, especially in the CC direction. It is possible that the presence of blur induced by FB respiration motion, combined with the tissue changes caused by irradiation, aggravated the image registration. The image quality score for tumour visibility at the 31st fraction for FB CBCT scans was inferior to that of DIBH CBCT scans.
Yeoh et al17 compared different strategies for automatic image registration with manual registration of several observers and found agreement within 2 mm for 80–90% of the cases, depending on the choice of the region of interest for the automatic registration; CBCT scans in this study were acquired with continuous acquisition during DIBH and FB in a mixed patient population. In our cohort, the agreement between the two image registrations in FB was within 2 mm for 69–86% of image sets and within 3 mm for 83–94% of image sets, depending on the direction (and slightly higher for DIBH registrations, 73–88% and 88–97%, respectively).
Sweeney et al24 investigated the interobserver uncertainty between FB CBCT and respiratory-correlated four-dimensional CBCT (4D-CBCT) in lung SBRT and found decreased uncertainty in 4D-CBCT registration. The interobserver variability in FB CBCT in their study was the largest in the CC direction, which corresponds to our findings; however, the magnitudes of interobserver uncertainties in their study were smaller than our data. This may be due to difference in complexity between their and our patient cohort (SBRT vs locally advanced disease) but may also be a result of the higher image quality scores that they reported for both FB CBCT and 4D-CBCT (comparable to our DIBH scores). However, they scored images only on visibility of the pulmonary target, and 19% of the FB CBCT received the highest score of 3, for unacceptable image quality. In our cohort, 17% of FB CBCT scans received the highest score of 3 and no DIBH CBCT scans were scored with 3 for tumour visibility.
4D-CBCT acquisition is time consuming and prone to motion artefacts,26 and a new approach with motion-compensating CBCT was shown to be quicker, with improved image quality compared both with FB CBCT and 4D-CBCT. Furthermore, the image registration was improved compared with FB CBCT. However, motion-compensating CBCT requires more computing and a prior deformable registration of CBCT.
A potential drawback of our study may be the manual image registration process. However, results of automatic registration were shown to yield inconsistent results, since it highly depends on the choice of several, also vendor-specific, parameters.17,27
We compared image quality of the CBCT scans acquired in FB and visually guided DIBH. Comparison with 4D-CBCT or motion-compensating CBCT would add value for FB image registration uncertainties, especially since these were only investigated for patients receiving SBRT.24
Another limitation of our study is that we investigated intraobserver uncertainties of a single observer. Investigating interobserver uncertainties would have added the information on the registration uncertainty. The study could not have been performed blinded due to obvious differences in the image quality between FB and CBCT.
Even if improved image quality only reduced the image registration uncertainty in the CC direction, the improved overall image quality could have made a difference for some patients. Since the anatomical structures are better visualized, decision making regarding treatment adaptation may be improved.
This report highlights another reason to carefully select DIBH candidates: poor compliance and hence reproducibility of DIBH will also impact image-guided RT (IGRT). But it remains that DIBH offers dosimetric benefits well beyond IGRT for compliant patients.13,14
CONCLUSION
To conclude, DIBH improved image quality of the CBCT scans and reduced the image registration uncertainty in IGRT of locally advanced lung cancer in the CC direction.
FUNDING
The study was supported by a master research agreement with Varian Medical Systems Inc. and by a grant from the Danish Cancer Society (R90-A6009-14-S2).
Contributor Information
Mirjana Josipovic, Email: mirjana.josipovic@regionh.dk.
Gitte F Persson, Email: gitte.persson@regionh.dk.
Jens P Bangsgaard, Email: jens.peter.bangsgaard@regionh.dk.
Lena Specht, Email: lena.specht@regionh.dk.
Marianne C Aznar, Email: mirjana.josipovic@regionh.dk.
REFERENCES
- 1.Boda-Heggemann J, Lohr F, Wenz F, Flentje M, Guckenberger M. kV cone-beam CT-based IGRT: a clinical review. Strahlenther Onkol 2011; 187: 284–91. doi: https://doi.org/10.1007/s00066-011-2236-4 [DOI] [PubMed] [Google Scholar]
- 2.Bissonnette JP, Balter PA, Dong L, Langen KM, Lovelock DM, Miften M, et al. Quality assurance for image-guided radiation therapy utilizing CT-based technologies: a report of the AAPM TG-179. Med Phys 2012; 39: 1946–63. doi: https://doi.org/10.1118/1.3690466 [DOI] [PubMed] [Google Scholar]
- 3.Song JY, Nam TK, Ahn SJ, Chung WK, Yoon MS, Nah BS. Respiratory motional effect on cone-beam CT in lung radiation surgery. Med Dosim 2009; 34: 117–25. doi: https://doi.org/10.1016/j.meddos.2008.07.004 [DOI] [PubMed] [Google Scholar]
- 4.Murphy MJ, Martin D, Whyte R, Hai J, Ozhasoglu C, Le QT. The effectiveness of breath-holding to stabilize lung and pancreas tumors during radiosurgery. Int J Radiat Oncol Biol Phys 2002; 53: 475–82. doi: https://doi.org/10.1016/S0360-3016(01)02822-X [DOI] [PubMed] [Google Scholar]
- 5.Onishi H, Kuriyama K, Komiyama T, Tanaka S, Sano N, Marino K, et al. Clinical outcomes of stereotactic radiotherapy for stage I non-small cell lung cancer using a novel irradiation technique: patient self-controlled breath-hold and beam switching using a combination of linear accelerator and CT scanner. Lung Cancer 2004; 45: 45–55. doi: https://doi.org/10.1016/j.lungcan.2004.01.004 [DOI] [PubMed] [Google Scholar]
- 6.Duggan DM, Ding GX, Coffey CW, 2nd, Kirby W, Hallahan DE, Malcolm A, et al. Deep-inspiration breath-hold kilovoltage cone-beam CT for setup of stereotactic body radiation therapy for lung tumors: initial experience. Lung Cancer 2007; 56: 77–88. doi: https://doi.org/10.1016/j.lungcan.2006.11.012 [DOI] [PubMed] [Google Scholar]
- 7.Wong VY, Tung SY, Ng AW, Li FA, Leung JO. Real-time monitoring and control on deep inspiration breath-hold for lung cancer radiotherapy—combination of ABC and external marker tracking. Med Phys 2010; 37: 4673–83. doi: https://doi.org/10.1118/1.3476463 [DOI] [PubMed] [Google Scholar]
- 8.Peng Y, Vedam S, Chang JY, Gao S, Sadagopan R, Bues M, et al. Implementation of feedback-guided voluntary breath-hold gating for cone beam CT-based stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys 2011; 80: 909–17. doi: https://doi.org/10.1016/j.ijrobp.2010.08.011 [DOI] [PubMed] [Google Scholar]
- 9.Rosenzweig KE, Hanley J, Mah D, Mageras G, Hunt M, Toner S, et al. The deep inspiration breath-hold technique in the treatment of inoperable non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 2000; 48: 81–7. [DOI] [PubMed] [Google Scholar]
- 10.McNair HA, Brock J, Symonds-Tayler JR, Ashley S, Eagle S, Evans PM, et al. Feasibility of the use of the active breathing coordinator (ABC) in patients receiving radical radiotherapy for non-small cell lung cancer (NSCLC). Radiother Oncol 2009; 93: 424–9. doi: https://doi.org/10.1016/j.radonc.2009.09.012 [DOI] [PubMed] [Google Scholar]
- 11.Sager O, Beyzadeoglu M, Dincoglan F, Oysul K, Kahya YE, Gamsiz H, et al. Evaluation of active breathing control-moderate deep inspiration breath-hold in definitive non-small cell lung cancer radiotherapy. Neoplasma 2012; 59: 333–40. doi: https://doi.org/10.4149/neo_2012_043 [DOI] [PubMed] [Google Scholar]
- 12.Giraud P, Morvan E, Claude L; STIC Study Centers. Respiratory gating techniques for optimization of lung cancer radiotherapy. J Thorac Oncol 2011; 6: 2058–68. doi: https://doi.org/10.1097/JTO.0b013e3182307ec2 [DOI] [PubMed] [Google Scholar]
- 13.Josipovic M, Persson GF, Håkansson K, Damkjær SM, Bangsgaard JP, Westman G, et al. Deep inspiration breath hold radiotherapy for locally advanced lung cancer: comparison of different treatment techniques on target coverage, lung dose and treatment delivery time. Acta Oncol 2013; 52: 1582–6. doi: https://doi.org/10.3109/0284186X.2013.813644 [DOI] [PubMed] [Google Scholar]
- 14.Marchand V, Zefkili S, Desrousseaux J, Simon L, Dauphinot C, Giraud P. Dosimetric comparison of free-breathing and deep inspiration breath-hold radiotherapy for lung cancer. Strahlenther Onkol 2012; 188: 582–9. doi: https://doi.org/10.1007/s00066-012-0129-9 [DOI] [PubMed] [Google Scholar]
- 15.Boda-Heggemann J, Fleckenstein J, Lohr F, Wertz H, Nachit M, Blessing M, et al. Multiple breath-hold CBCT for online image guided radiotherapy of lung tumors: simulation with a dynamic phantom and first patient data. Radiother Oncol 2011; 98: 309–16. doi: https://doi.org/10.1016/j.radonc.2011.01.019 [DOI] [PubMed] [Google Scholar]
- 16.Zhong R, Wang J, Zhou L, Xu F, Liu L, Zhou J, et al. Implementation of single-breath-hold cone beam CT guided hypofraction radiotherapy for lung cancer. Radiat Oncol 2014; 9: 77. doi: https://doi.org/10.1186/1748-717X-9-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yeoh KW, McNair HA, McDonald F, Hawkins M, Hansen VN, Ramos M, et al. Cone beam CT verification for active breathing control (ABC)-gated radiotherapy for lung cancer. Acta Oncol 2014; 53: 716–19. doi: https://doi.org/10.3109/0284186X.2013.861610 [DOI] [PubMed] [Google Scholar]
- 18.Josipovic M, Persson GF, Dueck J. Geometric uncertainties in voluntary deep inspiration breath hold radiotherapy for locally advanced lung cancer. Radiother Oncol 2016; 118: 510–14. doi: https://doi.org/10.1016/j.radonc.2015.11.004 [DOI] [PubMed] [Google Scholar]
- 19.Glide-Hurst CK, Gopan E, Hugo GD. Anatomic and pathologic variability during radiotherapy for a hybrid active breath-hold gating technique. Int J Radiat Oncol Biol Phys 2010; 77: 910–17. doi: https://doi.org/10.1016/j.ijrobp.2009.09.080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weiss E, Robertson S, Mukhopadhayaym N, Hugo GD. Tumor, lymph node and lymph node-to-tumor displacements over a radiotherapy series: analysis of inter- and intrafraction variations using active breathing control (ABC) in lung cancer. Int J Radiat Oncol Biol Phys 2012; 82: e639–45. doi: https://doi.org/10.1016/j.ijrobp.2011.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li R, Han B, Meng B, Maxim PG, Xing L, Koong AC, et al. Clinical implementation of intrafraction cone beam computed tomography imaging during lung tumor stereotactic ablative radiation therapy. Int J Radiat Oncol Biol Phys 2013; 87: 917–23. doi: https://doi.org/10.1016/j.ijrobp.2013.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wolthaus JW, Schneider C, Sonke JJ, van Herk M, Belderbos JS, Rossi MM, et al. Mid-ventilation CT scan construction from four-dimensional respiration-correlated CT scans for radiotherapy planning of lung cancer patients. Int J Radiat Oncol Biol Phys 2006; 65: 1560–71. doi: https://doi.org/10.1016/j.ijrobp.2006.04.031 [DOI] [PubMed] [Google Scholar]
- 23.Damkjær SM, Aznar MC, Pedersen AN, Vogelius IR, Bangsgaard JP, Josipovic M. Reduced lung dose and improved inspiration level reproducibility in visually guided DIBH compared to audio coached EIG radiotherapy for breast cancer patients. Acta Oncol 2013; 52: 1458–63. doi: https://doi.org/10.3109/0284186X.2013.813073 [DOI] [PubMed] [Google Scholar]
- 24.Sweeney RA, Seubert B, Stark S, Homann V, Müller G, Flentje M, et al. Accuracy and inter-observer variability of 3D versus 4D cone-beam CT based image-guidance in SBRT for lung tumors. Radiat Oncol 2012; 7: 81. doi: https://doi.org/10.1186/1748-717X-7-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parkes MJ, Green S, Stevens AM, Parveen S, Stephens R, Clutton-Brock TH. Safely prolonging single breath-holds to >5 min in patients with cancer; feasibility and applications for radiotherapy. Br J Radiol 2016; 89: 20160194. doi: https://doi.org/10.1259/bjr.20160194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rit S, Nijkamp J, van Herk M, Sonke JJ. Comparative study of respiratory motion correction techniques in cone-beam computed tomography. Radiother Oncol 2011; 100: 356–9. doi: https://doi.org/10.1016/j.radonc.2011.08.018 [DOI] [PubMed] [Google Scholar]
- 27.Grams MP, Brown LC, Brinkmann DH, Pafundi DH, Mundy DW, Garces YI, et al. Analysis of automatic match results for cone-beam computed tomography localization of conventionally fractionated lung tumors. Pract Radiat Oncol 2014; 4: 35–42. doi: https://doi.org/10.1016/j.prro.2013.02.008 [DOI] [PubMed] [Google Scholar]