Abstract
Objective:
The aim of the study was to investigate the feasibility of sonoelastography to show muscle stiffness in post-stroke spasticity, and the relationship between sonoelastography findings and clinical spasticity scores in the spastic forearm muscles.
Methods:
This study was carried out in a university rehabilitation centre. 23 patients with stroke with forearm muscle spasticity (≥1+ using the Modified Ashworth scale score and ≥1 using the Tardieu scale) were included. Sonoelastography parameters (elasticity index and elasticity ratio) were measured from the flexor digitorum superficialis, flexor digitorum profundus, flexor carpi radialis and flexor carpi ulnaris muscles on the affected and unaffected sides.
Results:
Both elasticity index and elasticity ratio of the wrist and finger flexors on the hemiplegic side were significantly increased compared with those on the healthy side (p < 0.05). The Tardieu angle of finger flexors was negatively correlated with the elasticity index and elasticity ratio measured in the spastic flexor digitorum profundus (r = −0.418 and r = −0.469, respectively). Tardieu angle of finger flexors was negatively correlated with the elasticity index measured in the spastic flexor digitorum superficialis (r = −0.435). There was no correlation between other parameters.
Conclusion:
Sonoelastography may provide objective assessment of spasticity both in diagnosis and follow-up. To strengthen this prediction, further studies are necessary.
Advances in knowledge:
The results of this study represent that sonoelastography is a promising evaluation method for forearm muscle spasticity.
INTRODUCTION
Stroke is defined as a neurological deficit due to an acute focal injury of the central nervous system caused by a vascular aetiology, including infarction, intracerebral hemorrhage or subarachnoid hemorrhage.1 It is a well-known cause of morbidity and mortality all over the world. Injury of the pyramidal and parapyramidal fibres in stroke results with upper motor neuron syndrome, which includes negative and positive features.2 Spasticity is one of the positive features such as spastic dystonia, extensor or flexor spasms, clonus and exaggerated deep tendon reflexes.3,4 According to the definition of Lance,2 spasticity is defined as a velocity-dependent hyperexcitability of muscles to stretch and is characterized by exaggerated deep tendon reflexes, increased resistance to passive movement and hypertonia resulting from loss of upper motor neuron inhibitory control.
A recent study has reported that 30% of patients with stroke have spasticity, which occurs within the first weeks of disease.5 Spastic symptoms may cause pain, joint stiffness, tendon retraction and muscle weakness and thus interfere with success of rehabilitation and daily activities. When the prevalence rates and the results of spasticity are taken into consideration, exact assessment and management of this disorder become more of an issue.
There are several assessment methods developed for spasticity. The most commonly used ones are the Modified Ashworth scale (MAS) and the Modified Tardieu Scale.6,7 However, these methods are subjective and the reliability is questionable for this reason. The other methods are neuroimaging techniques and electrophysiological studies, but they are not practical in daily routine for spasticity assessment.8
Ultrasound elastography is a recently developed imaging technique, which measures tissue elasticity. This technique uses the principle that application of stress to the tissue produces a strain (displacement), which is lower in hard tissues and higher in soft tissues.9,10 There are several elastography techniques which differ according to the type of stress application and to the method used to detect tissue strain and to gain the image of the tissue. These are sonoelastography, shear wave elastography, transient elastography and acoustic radiation force elastography.11–13 Sonoelastography is the most commonly used one, which is based on low-frequency compression of tissue. It is applied via free-hand (hand-held) ultrasound transducer.9,14 In the literature, application of sonoelastography is described in post-stroke spasticity of lower extremity,15 carpal tunnel syndrome16 and other musculoskeletal disorders.14
The aim of this study was to assess the sonoelastographic properties of spastic forearm muscles in patients with stroke in comparison with the unaffected side and to define the correlation of sonoelastography findings with clinical spasticity assessment tools.
METHODS AND MATERIALS
Study design and participants
To compare the elastic properties of upper extremity muscles [flexor carpi radialis, flexor carpi ulnaris, flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP)] of hemiplegic side with that of the healthy side in stroke patients, a cross-sectional experimental design was undertaken. 23 stroke patients who were admitted to our rehabilitation centre were included. The inclusion criteria were: (1) wrist and finger flexor muscle spasticity at least MAS 1+ and Tardieu grade 1 on the hemiplegic side and (2) age of 18–70 years. Patients were excluded if they had (1) previous stroke affecting upper extremities on both sides, (2) a history of botulinum toxin or neurolytic agents (phenol, alcohol) injection within 6 months, (3) previous surgery or major trauma to the upper extremity muscles and (4) any other neurological or muscular disorders. All participants provided written informed consent. Approval for the study was granted by the local ethics committee.
Procedures
Patient characteristics including age, gender, body mass index, time since stroke, stroke aetiology and affected side were noted. Immediately before performing ultrasound measurements, the degree of spasticity of the wrist and finger flexor muscles was assessed by a single physiatrist (EA) with MAS and Tardieu scale determined with the patient in the sitting position. The MAS and Tardieu scale were analyzed separately for wrist flexors and finger flexors at proximal interphalangeal joints. The MAS was described as the degree of resistance to quick passive movement and was rated as follows: [0 (MAS 0) = no increased resistance; 1 (MAS 1) = minimal resistance at the end of range of motion; 2 (MAS 1+) = minimal resistance throughout less than half of the range of motion; 3 (MAS 2) = clear resistance throughout most of the range of motion; 4 (MAS 3) = strong resistance, passive movement is difficult; and 5 (MAS 4) = rigid ankle flexion].17 The Tardieu Scale includes two stretch manoeuvres: one is performed as slowly as possible to measure the passive joint range of motion and the other is performed as fast as possible. The Tardieu scale measures both spasticity grade and spasticity angle. The spasticity grade is rated according to muscle reaction to fast stretch and rated as follows: 0 = no resistance throughout passive movement; 1 = slight resistance throughout passive movement; 2 = clear catch at a precise angle, interrupting of the passive movement, followed by release; 3 = fatiguable clonus occurring at a precise angle; and 4 = unfatiguable clonus occurring at a precise angle. The spasticity angle represents the velocity-dependent stretch reflex. It is determined as the difference between angles of arrest at slowest speed and of catch and release at fastest speed.18,19
The same ultrasound system with a 5–12 MHz linear transducer (GE LOGIQ S7; GE Healthcare, Beijing, China) was used for ultrasound measurements. The patients were sitting on the examination table and at a standardized resting position of the wrist and fingers (without any movement of wrist and finger flexors), the transducer was transversely placed over the target muscles. After that, B-mode ultrasound and sonoelastography measurements of bilateral sides were performed at the needle electromyography insertion sites, which are also accepted as botulinum toxin injection sites.20 Sonoelastographic images of flexor carpi radialis muscle were obtained in the transverse plane in the point of four fingerbreadths distal to the point of midpoint of a line connecting the medial epicondyle and biceps tendon on the anterior aspect; and sonoelastographic images of flexor carpi ulnaris muscle were obtained in the transverse plane in the point of two fingerbreadths volar to the ulna at the junction of the upper and middle thirds of the forearm on the anterior aspect. Sonoelastographic images of FDP and FDS muscles were obtained in the same cross section in the transverse plane in the point of mid-forearm halfway from the ventral midline to the medial border of the forearm on the anterior aspect.
The sonoelastographic assessment was performed between the superficial and deeper border of the muscle with minimum compression of the transducer in the transverse view and the thickest level was determined. If any muscle movement or contraction was detected during measurement, the scanning was quit. When the sonographer was sure that there was no muscle movement at all, the scanning was restarted. The same physiatrist (SK) who was blind to the MAS scores, Tardieu grades and angles conducted all the scans.
Sonoelastography technique, which is described in the previous study, was used.15 Light repetitive compression was applied manually with the hand-held transducer by providing visual feedback from the quality bar indicator. The elastogram of the region of interest (ROI) was performed according to the colour-coded real-time image of the ROI.
Transverse plane of the muscles was used for sonoelastography. For each muscle, at least three compression-relaxation cycles were applied until reproducible findings were confirmed. The images were recorded in the memory of the ultrasound device. By replaying the recorded images, the best representative image was selected. On the selected images, two ROIs were set. The first ROI was set on subcutaneous tissue as reference, which is recommended to be the less elastic tissue for a better ratio calculation. Before setting the first ROI, the skin area was examined to ensure that there was no oedema in the subcutaneous tissue or skin dystrophy that could affect the sonoelastographic measurements. The second ROI was set to cover the target muscles excluding the perimysium.
Elastography quantitative analysis21 was used to measure the elasticity. It is a software feature of the ultrasound system which quantifies the colour distribution numerically in a selected ROI over a single or multiple frames and computes an elasticity index for the measured area. The elasticity index is defined as a value from 0.0 to 6.0., which is created by the reflected colour distribution within the ROI. A higher value indicates “higher stiffness”, and dominant colour in the screen is blue. The elasticity index was provided separately for the reference area (E1) and muscle (E2). The system automatically calculates the elasticity ratio (E2/E1) (Figures 1–4).
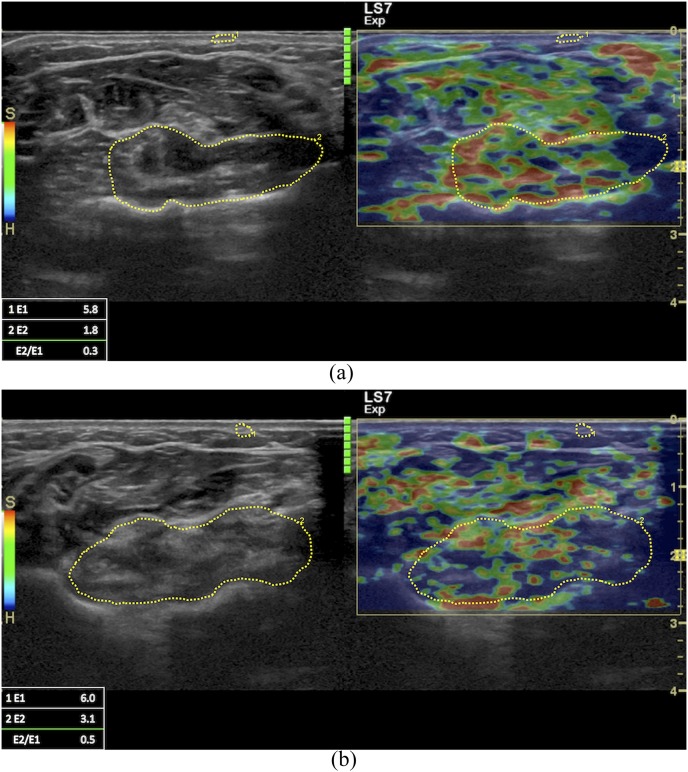
Figure 1.
Sonoelastographic images of healthy (a) and spastic (b) flexor carpi radialis in the transverse plane in the point of four fingerbreadths distal to the point of the midpoint of a line connecting the medial epicondyle and biceps tendon on the anterior aspect. Elastogram showed yellow to red colouring in healthy muscles and green to blue colouring in spastic muscles. Elasticity index (E2) and elasticity ratio (E2/E1) are higher in spastic muscles and lower in healthy muscles.
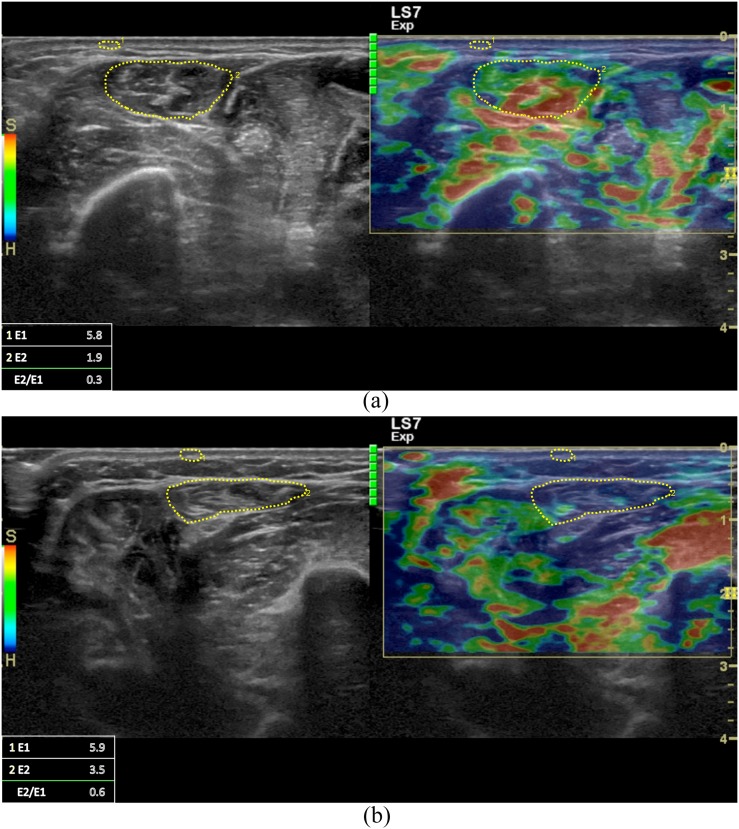
Figure 4.
Sonoelastographic images of healthy (a) and spastic (b) flexor digitorum profundus in the transverse plane in the point of mid-forearm halfway from the ventral midline to the medial border of the forearm on the anterior aspect. Elastogram showed yellow to red colouring in healthy muscles and green to blue colouring in spastic muscles. Elasticity index (E2) and elasticity ratio (E2/E1) are higher in spastic muscles and lower in healthy muscles.
Figure 2.
Sonoelastographic images of healthy (a) and spastic (b) flexor carpi ulnaris in the transverse plane in the point of two fingerbreadths volar to the ulna at the junction of the upper and middle thirds of the forearm on the anterior aspect. Elastogram showed yellow to red colouring in healthy muscles and green to blue colouring in spastic muscles. Elasticity index (E2) and elasticity ratio (E2/E1) are higher in spastic muscles and lower in healthy muscles.
Figure 3.
Sonoelastographic images of healthy (a) and spastic (b) flexor digitorum superficialis in the transverse plane in the point of mid-forearm halfway from the ventral midline to the medial border of the forearm on the anterior aspect. Elastogram showed yellow to red colouring in healthy muscles and green to blue colouring in spastic muscles. Elasticity index (E2) and elasticity ratio (E2/E1) are higher in spastic muscles and lower in healthy muscles.
To obtain the interrater and intrarater reliability, the sonoelastographic parameters that were used throughout the study (E1, E2 and E2/E1) were measured according to the study protocol in 10 hemiplegic patients. The measurements of two different raters were used to determine interrater reliability. The first rater took the measurements twice. After 1 day, all the measurements were repeated twice with the raters blinded to the first measurements. A total of four measurements by the first rater were used to determine the intrarater reliability. The interrater and intrarater reliability were found to be moderate to good [1.76–8.9% coefficient of variation and 1.72–7.9% coefficient of variation, respectively] for the sonoelastographic measurements.
Statistical analyses
Data were expressed as mean ± standard deviation. Kolmogorov–Smirnov test was used to test normality of data. The mean differences of imaging findings between the affected and unaffected sides were compared by Student's t-test. The correlation of sonoelastographic findings with the MAS scores, Tardieu grades and angles was assessed using Pearson correlation coefficient. The significance level was determined at p < 0.05. All statistical tests were performed using IBM SPSS® statistics software program (IBM Corp., New York, NY; formerly SPSS Inc., Chicago, IL) for Mac v. 20.0.
RESULTS
23 patients with a mean age of 52.4 ± 15.4 years were included in this study. There were 17 male (73.9%) and 6 female (26.1%) patients. The mean disease duration was 33.1 ± 35.9 months. Demographic and clinic data of the patients are presented in Tables 1 and 2.
Table 1.
Patient characteristics
| Characteristic | Patients (n = 23) |
|---|---|
| Sex | |
| Male | 17 (73.9%) |
| Female | 6 (26.1%) |
| Age (years)a | 52.4 ± 15.4 |
| Body mass index (kg m−2)a | 26.5 ± 3.5 |
| Time since stroke (months)a | 33.1 ± 35.9 |
| Stroke aetiology | |
| Ischaemic | 13 (56.5%) |
| Haemorrhagic | 10 (43.5%) |
| Affected side | |
| Right | 11 (47.8%) |
| Left | 12 (52.2%) |
Mean ± standard deviation.
Table 2.
Clinical data of the patients
| Spasticity assessment | Patients (n = 23) |
|---|---|
| Spasticity degree measured using MAS | |
| 1 | 0 (0.0%) |
| 1+ | 3 (13.0%) |
| 2 | 6 (26.1%) |
| 3 | 11 (47.8%) |
| 4 | 3 (13.0%) |
| Tardieu spasticity grade at wrist | |
| 1 | 8 (34.8%) |
| 2 | 12 (52.2%) |
| 3 | 3 (13.0%) |
| Tardieu spasticity angle at wrist (degree)a | 11.9 ± 8.0 |
| Tardieu spasticity grade at fingers | |
| 1 | 3 (13.0%) |
| 2 | 12 (52.2%) |
| 3 | 8 (34.8%) |
| Tardieu spasticity angle at fingers (degree)a | 24.3 ± 17.2 |
MAS, Modified Ashworth scale.
Mean ± standard deviation.
Both of the elasticity index and elasticity ratio of the wrist and finger flexors on the hemiplegic side significantly increased compared with those on the healthy side (p < 0.05; Table 3).
Table 3.
Sonoelastographic findings of the patients
| Muscle | Elasticity index |
Elasticity ratio |
||||
|---|---|---|---|---|---|---|
| Affected sidea | Unaffected sidea | p-value | Affected sidea | Unaffected sidea | p-value | |
| FCR | 2.81 ± 0.63 | 2.01 ± 0.55 | <0.001b | 0.50 ± 0.11 | 0.36 ± 0.11 | <0.001b |
| FCU | 2.99 ± 0.79 | 2.03 ± 0.45 | <0.001b | 0.53 ± 0.13 | 0.37 ± 0.09 | <0.001b |
| FDS | 2.55 ± 0.49 | 2.10 ± 0.49 | 0.002b | 0.47 ± 0.85 | 0.38 ± 0.77 | 0.001b |
| FDP | 2.89 ± 0.63 | 2.02 ± 0.61 | <0.001b | 0.53 ± 0.10 | 0.36 ± 0.12 | <0.001b |
FCR, flexor carpi radialis; FCU, flexor carpi ulnaris; FDP, flexor digitorum profundus; FDS, flexor digitorum superficialis.
Mean ± standard deviation.
Statistically significant.
The Tardieu angle of finger flexors was negatively correlated with the elasticity index and elasticity ratio measured in the spastic FDP (r = −0.418 and r = −0.469, respectively). The Tardieu angle of the finger flexors was negatively correlated with the elasticity index measured in the spastic FDS (r = −0.435; Table 4). There was no correlation between the other parameters.
Table 4.
Correlations of sonoelastography parameters with Modified Ashworth scale (MAS) scores, Tardieu spasticity grades and angles on the hemiplegic side
| Muscle | Wrist flexors |
Finger flexors |
||||
|---|---|---|---|---|---|---|
| MAS | Tardieu grade | Tardieu angle | MAS | Tardieu grade | Tardieu angle | |
| FCU | ||||||
| Elasticity index | 0.181 | 0.077 | −0.012 | 0.212 | 0.004 | −0.104 |
| Elasticity ratio | 0.106 | −0.001 | −0.116 | −0.216 | 0.345 | 0.106 |
| FCR | ||||||
| Elasticity index | 0.123 | −0.014 | 0.101 | −0.015 | −0.081 | −0.199 |
| Elasticity ratio | 0.105 | −0.028 | 0.132 | −0.058 | −0.043 | −0.189 |
| FDP | ||||||
| Elasticity index | 0.248 | 0.390 | 0.244 | 0.140 | 0.023 | −0.418a |
| Elasticity ratio | 0.257 | 0.281 | 0.287 | −0.046 | −0.014 | −0.469a |
| FDS | ||||||
| Elasticity index | 0.268 | −0.005 | −0.027 | 0.121 | −0.077 | −0.435a |
| Elasticity ratio | 0.267 | 0.003 | −0.076 | −0.042 | −0.114 | −0.408 |
FCR, flexor carpi radialis; FCU, flexor carpi ulnaris; FDP, flexor digitorum profundus; FDS, flexor digitorum superficialis.
Correlation is significant at the 0.05 level.
DISCUSSION
The results of this study revealed that stiffness evaluated with sonoelastography was increased in both the wrist and finger flexors on the hemiplegic side compared with the healthy side in patients with stroke. Although not found in all parameters, there was moderate correlation between clinical and sonoelastographic measurements.
To our knowledge, sonoelastographic assessment of spastic upper extremity muscles in stroke was not studied previously. In a recent study of Kesikburun et al,15 assessment of sonoelastographic findings in the gastrocnemius muscle of patients with stroke using the same technique described above showed that both the elasticity index and elasticity ratio of the spastic muscles were increased compared with those on the unaffected side. The findings of the current study were in concordance with these previous results. Kwon et al22 also investigated elasticity of the gastrocnemius muscle in patients with cerebral palsy. Sonoelastographic parameters in that study showed higher stiffness in spastic muscles.
In this study, it was aimed to define the usefulness of sonoelastography in assessment of spastic muscles, both the MAS scores and the Tardieu scaling were also used for spasticity evaluation. The Tardieu scaling has not been used in previous sonoelastography studies.15,22 The Tardieu angle of finger flexors showed moderate correlation with elasticity index and elasticity ratio of the FDP muscles and the elasticity index of the FDS muscle. These findings of correlation could be taken into consideration as supporting the value of sonoelastographic assessment in upper extremity spastic muscles. But, on the contrary, we did not find any correlation between MAS scores and elastic properties of the finger flexor muscles. This confounding data could have been due to subjective and qualitative properties of MAS assessment.23,24
In the present study, we assessed sonoelastographic properties of upper extremity muscles in only the transverse plane; we did not perform longitudinal assessment. Needle electromyography insertion sites, which are also accepted for botulinum toxin injections were selected for sonoelastographic assessments because we supposed that these points might be the most probable sites to find effectiveness of sonoelastography as these sites are known to be the thickest sites of these muscles. In this aspect, one can ask the usefulness of sonoelastographic measurements to assess the effectiveness of botulinum toxin injections. But for this consideration, future research is necessary.
There are some limitations of this study. Disease duration of participants has a wide range. The spastic and elastic properties of the evaluated muscles might be affected by disease duration. We performed sonoelastography in only the transverse plane; additional longitudinal assessment could provide more information about the muscle. Small sample size is also a limitation. Another limitation is the free-hand compression technique due to the difficulty of controlling the applied tissue stress. But interrater and intrarater reliability was found to be good to moderate, and this could be considered a strength of the study.
In conclusion, sonoelastography is a diagnostic tool to assess stiffness in spastic muscles, and the results of this study represent that it is a promising evaluation method for forearm muscle spasticity. Sonoelastography may provide objective assessment of spasticity both in diagnosis and follow-up. To strengthen this prediction, further studies are necessary.
Contributor Information
Evren Yaşar, Email: evrenyasar@yahoo.com.
Emre Adigüzel, Email: dremreadiguzel@gmail.com.
Serdar Kesikburun, Email: serdarkb@gmail.com.
Itır Yenihayat, Email: itiryenihayat@yahoo.com.
Rıdvan Alaca, Email: ridvanalaca@hotmail.com.
Arif K Tan, Email: aktan@gat.edu.tr.
REFERENCES
- 1.Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013; 44: 2064–89. doi: https://doi.org/10.1161/STR.0b013e318296aeca [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lance JW. The control of muscle tone, reflexes, and movement: Robert Wartenberg lecture. Neurology 1980; 30: 1303–13. doi: https://doi.org/10.1212/WNL.30.12.1303 [DOI] [PubMed] [Google Scholar]
- 3.McComas AJ. Human neuromuscular adaptations that accompany changes in activity. Med Sci Sports Exerc 1994; 26: 1498–509. [PubMed] [Google Scholar]
- 4.Sommerfeld DK, Eek EU, Svensson AK, Holmqvist LW, von Arbin MH. Spasticity after stroke: its occurrence and association with motor impairments and activity limitations. Stroke 2004; 35: 134–9. doi: https://doi.org/10.1161/01.STR.0000105386.05173.5E [DOI] [PubMed] [Google Scholar]
- 5.Mayer NH, Esquenazi A. Muscle overactivity and movement dysfunction in the upper motoneuron syndrome. Phys Med Rehabil Clin N Am 2003; 14: 855–83. doi: https://doi.org/10.1016/S1047-9651(03)00093-7 [DOI] [PubMed] [Google Scholar]
- 6.Tardieu G, Shentoub S, Delarue R. A la recherche d'une technique de mesure de la spasticite. [In French.] Rev Neurol 1954; 91: 143–4. [PubMed] [Google Scholar]
- 7.Held J, Pierrot-Deseilligny E, eds. Reeducation motrice des affections neurologiques. Paris, France: JB Bailliere; 1969. [Google Scholar]
- 8.Thibaut A, Chatelle C, Ziegler E, Bruno MA, Laureys S, Gosseries O. Spasticity after stroke: physiology, assessment and treatment. Brain Inj 2013; 27: 1093–105. doi: https://doi.org/10.3109/02699052.2013.804202 [DOI] [PubMed] [Google Scholar]
- 9.Park GY, Kwon DR. Application of real-time sonoelastography in musculoskeletal diseases related to physical medicine and rehabilitation. Am J Phys Med Rehabil 2011; 90: 875–86. doi: https://doi.org/10.1097/PHM.0b013e31821a6f8d [DOI] [PubMed] [Google Scholar]
- 10.Ophir J, Cespedes I, Ponnekanti H, Yazdi Y, Li X. Elastography: a quantitative method for imaging the elasticity of biological tissues. Ultrason Imaging 1991; 13: 111–34. doi: https://doi.org/10.1177/016173469101300201 [DOI] [PubMed] [Google Scholar]
- 11.Li Y, Snedeker JG. Elastography: modality-specific approaches, clinical applications, and research horizons. Skeletal Radiol 2011; 40: 389–97. doi: https://doi.org/10.1007/s00256-010-0918-0 [DOI] [PubMed] [Google Scholar]
- 12.Garra BS. Imaging and estimation of tissue elasticity by ultrasound. Ultrasound Q 2007; 23: 255–68. doi: https://doi.org/10.1097/ruq.0b013e31815b7ed6 [DOI] [PubMed] [Google Scholar]
- 13.Garra BS. Elastography: current status, future prospects, and making it work for you. Ultrasound Q 2011; 27: 177–86. doi: https://doi.org/10.1097/RUQ.0b013e31822a2138 [DOI] [PubMed] [Google Scholar]
- 14.Drakonaki EE, Allen GM, Wilson DJ. Ultrasound elastography for musculoskeletal applications. Br J Radiol 2012; 85: 1435–45. doi: https://doi.org/10.1259/bjr/93042867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kesikburun S, Yaşar E, Adiguzel E, Güzelküçük Ü, Alaca R, Tan AK. Assessment of spasticity with sonoelastography following stroke: a feasibility study. PM R 2015; 7: 1254–60. doi: https://doi.org/10.1016/j.pmrj.2015.05.019 [DOI] [PubMed] [Google Scholar]
- 16.Kesikburun S, Adigüzel E, Kesikburun B, Yaşar E. Sonoelastographic assessment of median nerve in longitudinal plane for carpal tunnel syndrome. PM R 2016; 8: 183–5. doi: https://doi.org/10.1016/j.pmrj.2015.07.012 [DOI] [PubMed] [Google Scholar]
- 17.Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther 1987; 67: 206–7. [DOI] [PubMed] [Google Scholar]
- 18.Gracies JM, Marosszeky JE, Renton R, Sandanam J, Gandevia SC, Burke D. Short-term effects of dynamic lycra splints on upper limb in hemiplegic patients. Arch Phys Med Rehabil 2000; 81: 1547–55. doi: https://doi.org/10.1053/apmr.2000.16346 [DOI] [PubMed] [Google Scholar]
- 19.Gracies JM, Burke K, Clegg NJ, Browne R, Rushing C, Fehlings D, et al. Reliability of the tardieu scale for assessing spasticity in children with cerebral palsy. Arch Phys Med Rehabil 2010; 91: 421–8. doi: https://doi.org/10.1016/j.apmr.2009.11.017 [DOI] [PubMed] [Google Scholar]
- 20.Delagi EF, Perotto A, Iazetti J, Morrison D. Anatomic guide for the electromyographer: the limbs and trunk. 4th edn. Springfield, IL: CC Thomas; 2005. [Google Scholar]
- 21.LOGIQ S7 Expert/Pro Basic User Manual. Milwaukee, WI: GE Healthcare; 2012. [Google Scholar]
- 22.Kwon DR, Park GY, Lee SU, Chung I. Spastic cerebral palsy in children: dynamic sonoelastographic findings of medial gastrocnemius. Radiology 2012; 263: 794–801. doi: https://doi.org/10.1148/radiol.12102478 [DOI] [PubMed] [Google Scholar]
- 23.Ansari NN, Naghdi S, Arab TK, Jalaie S. The interrater and intrarater reliability of the modified Ashworth scale in the assessment of muscle spasticity: limb and muscle group effect. NeuroRehabilitation 2008; 23: 231–7. [PubMed] [Google Scholar]
- 24.Ansari NN, Naghdi S, Moammeri H, Jalaie S. Ashworth scales are unreliable for the assessment of muscle spasticity. Physiother Theory Pract 2006; 22: 119–25. doi: https://doi.org/10.1080/09593980600724188 [DOI] [PubMed] [Google Scholar]