Abstract
Objective:
To evaluate the analgesic efficacy of low-dose radiotherapy in refractory cases of trochanteritis.
Methods:
We evaluated a total of 60 consecutive patients who received low-dose radiotherapy to achieve an anti-inflammatory and analgesic effect for recurrent trochanteritis following scarce response to conventional therapy. All patients were evaluated at baseline (prior to radiotherapy) and at 1 and 4 months after radiotherapy and then yearly thereafter for pain assessment using a visual analogue scale (VAS) and to determine the administration of analgesic treatment.
Results:
An improvement in the symptomatology was observed in 62% of the patients with a significant reduction in the VAS (8 ± 2 vs 4 ± 2; p < 0.0001), which was largely maintained until the second evaluation at 4 months. In the cases responding to radiotherapy, the probability of maintaining improvement beyond 24 months was 70%.
Conclusion:
Low-dose anti-inflammatory radiation may be used in the treatment of the recurrent cases of relapse or no response of trochanteritis to conventional treatments, with a high probability of remission of pain. These preliminary results indicate the need for evaluating the use of radiotherapy in patients with trochanteritis refractory to conventional treatment in a long-term controlled study.
Advances in knowledge:
Radiotherapy provides effective analgesic treatment for patients refractory to standard treatment for trochanteritis.
INTRODUCTION
Trochanteritis is a relatively frequent clinical condition which predominantly presents in middle aged or elderly subjects, with an estimated prevalence of around 6/1000 adults. This syndrome is characterized by the presence of generally moderate to intense pain localized in the area of the trochanter, which often irradiates to different neighbouring inferior and posterior zones. Trochanteritis is debilitating, hinders walking and mobility in general and produces discomfort when lying on the affected side. This syndrome is also known as the greater tronchanteric pain syndrome, since it can be caused by a wide spectrum of aetiologies, such as tendinopathies, muscle tears, iliotibial friction disorders and trochanteric bursitis, among others, with microtrauma seeming to play a triggering role. Tuberculosis has also been reported as an aetiology of this syndrome1–3 in historic series from the middle of the 20th century.
The frequency and diversity of radiologic findings including ultrasonography, CT and MRI in trochanteritis vary, with the most frequent being enthesopathies of the gluteal musculature, calcifications, tendon rupture and trochanteric bursal inflammation and effusion.
The treatment of trochanteritis also varies greatly with variable results. Apart from the use of anti-inflammatory analgesics and opiates, the most common procedure is local injection of a corticosteroid drug and local anaesthetics ranging in efficacy from 49 to 100%.4 Other treatments include physical therapy with infrared rays, shock waves, ultrasound, cryotherapy and thermotherapy. In patients not responding to conservative measures, surgical procedures such as endoscopic bursectomy and open reduction trochanteric osteotomy may be performed. Although most patients improve with anti-inflammatory treatment and/or local corticosteroid injection, trochanteric pain may become chronic and invalidating in a relatively high percentage of cases with a significant decline in the quality of life of the patient.
Anti-inflammatory radiotherapy has been widely used in numerous non-neoplasic degenerative, chronic inflammatory or proliferative diseases such as scapulohumeral periarthritis, epicondylitis, plantar fasciitis, osteoarthrosis and joint pain, among others.5,6 The mechanism of action, albeit not well known, is based on the blockade of different inflammatory mediators; for example, radiation inhibits the adhesion of the mononuclear leucocytes by acting on the regulating molecules such as L-selectin.7–9 In a recent study, Wunderlich et al10 reported that an anti-inflammatory cytokine milieu is created at low doses. Apart from functional modulation of the mechanisms of adhesion, Trott and Kamprad11 have described the role of nitric oxide synthase in activated macrophages, supporting the results of Rödel et al12 with nitric oxide. Although anti-inflammatory radiotherapy has classically been performed at low doses compared with antineoplasic radiotherapy, in which the usual schedules are of 5–10 Gy in 10 fractions, lower total doses and fractions seem to be more effective.
At present, however, data on the effect of radiotherapy in the treatment of refractory trochanteritis are scarce. Considering the potential benefits of radiotherapy, the aim of this study was to analyze the analgesic efficacy of low-dose radiotherapy in a series of patients with trochanteritis refractory to conventional treatment.
METHODS AND MATERIALS
From July 2010 to August 2014, we included a total of 60 consecutive patients with recurrent trochanteritis refractory to conventional therapy referred from the Departments of Rheumatology, Anesthesiology (Pain Clinic) and Orthopedic Surgery. The inclusion criteria for treatment included: failure of previous conventional treatment, the presence of intense debilitating pain in daily life activities and patients older than 60 years of age.
The diagnosis of trochanteritis was made according to clinical and radiological criteria (increased tenderness to trochanter palpation with compatible radiological/ultrasonographic images).
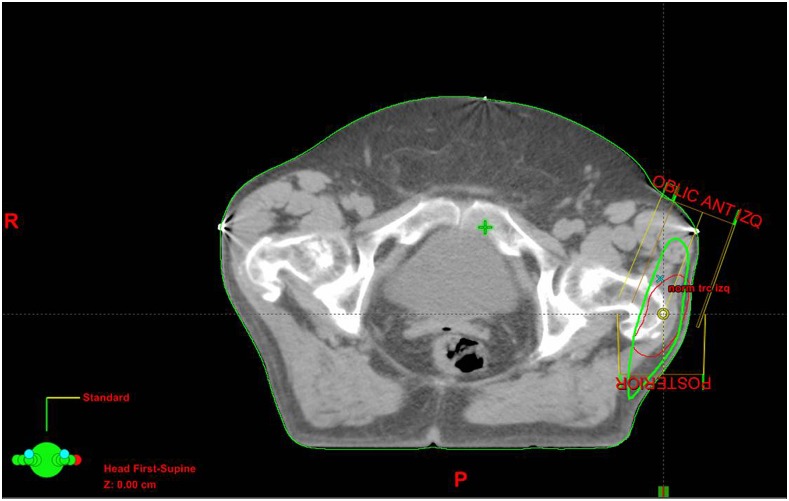
All patients received low-dose radiotherapy for the reduction of inflammation and pain. The radiotherapy was designed using CT-based treatment planning systems. The target treatment volume included the trochanteric region, bursas and fasciotendinous areas affected. The radiation was administered using a multiple-field technique made up of multilayer collimators using a linear accelerator photon beam of 6 or 18 MV (Figure 1).
Figure 1.
Irradiation planning for left trochanteritis: patients received a total dose of 10 Gy divided into 10 sessions. ANT, anterior; IZQ, left; OBLIC, oblique; P, posterior; R, right.
The patients received a total dose of 10 Gy in 10 fractions (doses of 1 Gy /day/5 days a week). After irradiation, the patients were followed at 1 and 4 months for the evaluation of treatment response. Patients requiring reirradiation, owing to the reappearance of pain or lack of response, were treated with a total additional dose of 3 Gy in 10 fractions (fractionation of 0.3 Gy day−1).
The following parameters were evaluated: associated processes, previous treatment, radiological alterations, radiotherapy treatment received (dose and length of treatment), clinical outcome as well as the need for reirradiation or not and patient outcome.
We recorded medication details and categorized analgesics as analgesics and minor and major opiate derivatives. Pain assessment was based on the visual analogue scale (VAS), which evaluates pain on a scale from 0 to 10, in which 0 indicates no pain and 10 indicates the maximum level of pain.
Patients were clinically assessed according to the VAS and the evolution of mobility at baseline and at 1 and 4 months after radiation treatment and then yearly thereafter. Analgesia and subjective response of pain were classified into three categories: complete response, partial response and no response.
The statistical analyses were performed using the SPSS® v. 18.0 program (IBM Corp., New York, NY; formerly SPSS Inc., Chicago, IL). Quantitative variables are described using means and standard deviations and frequencies and percentages are reported for qualitative variables. Means were compared with the Student's t-test for paired samples and Kaplan–Meier analysis, with p-values <0.05 being considered as significant.
Ethical approval
Ethical approval was obtained from the ethics committee of our hospital, and all participants provided written informed consent to participate in the study.
RESULTS
A total of 60 consecutive patients diagnosed with recurrent trochanteritis refractory to conventional therapy underwent treatment with low-dose irradiation and were followed for a mean of 18.5 ± 10 months.
90% of the patients treated were females (54 females/6 males) with a median age of 68 years (40–89 years). The clinical conditions most frequently associated with trochanteritis were: osteoporosis (27%), polyarthrosis (37%), obesity (20%) and fibromyalgia (12%), with 72% (43 patients) concomitantly presenting chronic lumbar pain. All the patients were refractory to the usual therapies; 81% patients had undergone previous treatment with local corticosteroid injections, and nearly half of the patients required major opiate analgesic treatment (38% patients received minor opiate derivatives and anti-inflammatories and 44% patients received major opiate derivatives) (Table 1).
Table 1.
Clinical characteristics of the whole group
| Clinical characteristics | ||
|---|---|---|
| Females/males | 54/6 | 90/10 |
| Age (years) | ||
| Mean (range) | 69 (40–89) | |
| Comorbidities (%) | ||
| Osteoporosis | 16 | 27% |
| Obesity | 12 | 20% |
| Fibromyalgia | 7 | 12% |
| Low back pain | 43 | 72% |
| Osteoarthritis | 22 | 37% |
| Radiological findings (%) | ||
| No MRI | 16 | 26% |
| Enthesopathy | 16 | 26% |
| Tendon rupture | 7 | 12% |
| Bursal disease | 7 | 12% |
| Calcifications | 14 | 22% |
| Pre-/post-VAS (median) | 8/4 | |
| Reirradiation (n/%) | 17 | 28% |
VAS, visual analogue scale.
The pain presented was predominantly unilateral (75% of the patients), being exclusively localized in the trochanter area in 60% patients and most frequently with anterior radiation (37% patients). Baseline evaluation with the VAS was carried out on the first visit to the Department of Oncologic Radiotherapy, with a mean score of 8 being observed (range 4–10).
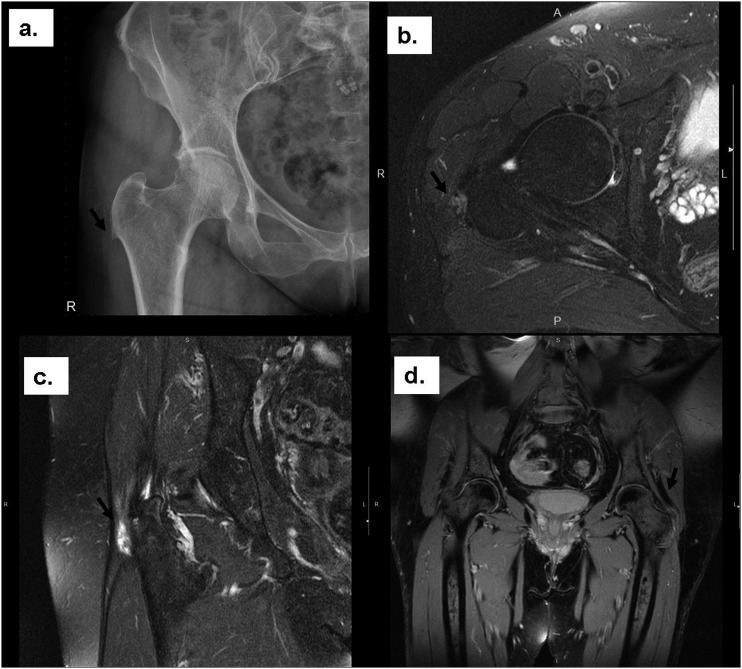
The radiological evaluation involved a simulation CT in all the patients included in the study, with most patients (73%) also undergoing MRI and ultrasonography evaluation studies. The most relevant findings were gluteal enthesopathy (25%), tendon calcifications (21%), tendon rupture (12%) and bursitis (58%) (Figure 2).
Figure 2.
Radiological findings prior to radiotherapy: (a) ossificans enthesopathy in the right trochanter; (b) partial tendon rupture in the gluteus insertion on the right trochanter; (c) increased signal insertion in the gluteal tendons and half proximate to its insertion into the right trochanter; (d) a hyperintense area in the insertion of the gluteal muscles in the left trochanter. P, posterior; R, right.
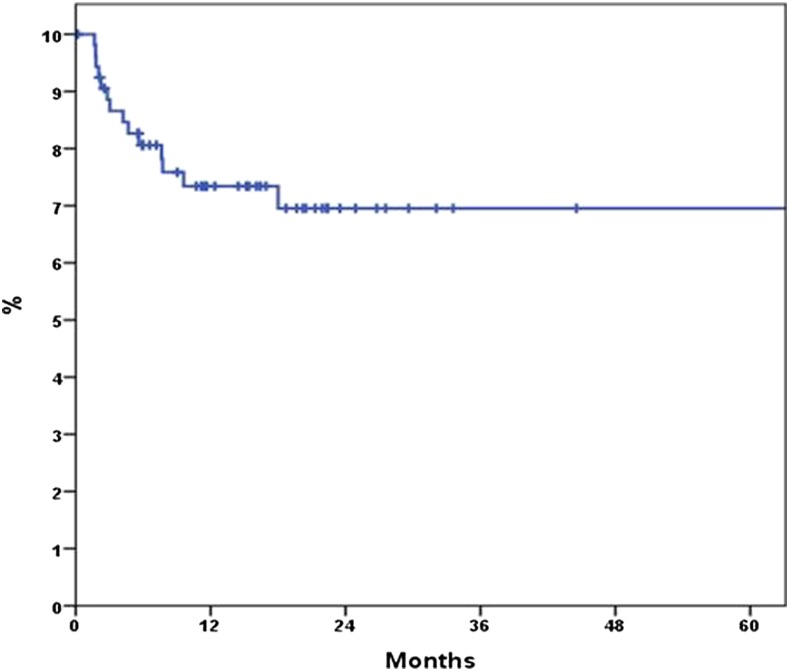
The first evaluation of response was made on completing the radiation therapy. An improvement in the symptomatology was observed in 62% of the patients with a significant reduction in the VAS (8 ± 2 vs 4 ± 2; p < 0.0001) 1 month after radiotherapy, which was usually maintained at 4 months (VAS 4 ± 2 vs 4 ± 2; p = 147). In this second evaluation, 17% of the patients presented re-exacerbation of the pain. In the cases responding to radiotherapy, the probability of maintaining improvement beyond 24 months was 70% (Figure 3 and Table 2). Although no significant differences were observed in relation to the radiological findings and the probability of re-exacerbation, most patients with clinical relapse after treatment had gluteal enthesopathy and/or tendon calcifications at baseline. In addition, positive clinical response did not seem to be related to associated comorbidities, such as the presence of fibromyalgia, obesity or chronic lumbar pain.
Figure 3.
The probability of maintenance of the response of improvement of radiotherapy beyond 24 months was 70%.
Table 2.
Evaluation of response to irradiation treatment, 1 month and 4 months, in total numbers and percentage
| 1 month (n/%) | 4 months (n/%) | |
|---|---|---|
| Complete response | 11/18 | 14/23 |
| Partial response | 36/60 | 33/55 |
| No response | 13/22 | 13/22 |
In the subjective evaluation, 24% of patients reported complete response and 75% patients reported partial response, with only 1% of patients having no response to radiotherapy. 4 months after treatment, 23% of the patients reported complete withdrawal of analgesics.
17 (28%) patients required reirradiation owing to exacerbation of pain within a mean of 5.8 months after the initial irradiation treatment. Complete response to treatment was observed in all these cases except in two. During follow-up, 50% patients with fibromyalgia required reirradiation, whereas this was necessary in 27% of patients with polyarthrosis, 26% of patients with chronic back pain and 31% of subjects with osteoporosis.
No secondary effects related to irradiation therapy were observed during follow-up.
DISCUSSION
The use of radiotherapy to reduce inflammation and the need for analgesics is a classic treatment in degenerative and inflammatory processes. Multiple indications have been described,13 and it has been estimated that 50,000 patients are treated annually with this method in Germany,5,6 albeit with great variability among institutions.
The results of our study suggest that radiotherapy can be used in patients with recurrent or refractory trochanteritis and associated severe pain, in whom conventional treatment has failed. Indeed, most of the patients in the present series showed significant clinical improvement after this therapeutic approach, not only at 4 months after radiotherapy, but also in the long term after treatment.
The doses usually reported are much lower than that in antineoplasic radiotherapy, ranging from 5 to 10 Gy in several fractions over 1 or more weeks.14 Although the analgesic anti-inflammatory effect is not well known, it seems to be related to the blockade of macrophage and monocyte adhesion to the vascular endothelium and posterior penetration into the intercellular space.6–8 The modulation of nitric oxide production and inflammatory mediators as well as immunomodulatory effects may play an important role in the effects observed with low-dose radiotherapy.
The most effective dose and fractionation also remains controversial, with there currently being a trend to use even lower doses.15 In previous studies by our group,7,8 we found that a dose of only 0.3 Gy to the intestinal wall of mice was the most effective in the blockade of adhesion molecules (P-selectin, Intercellular adhseion molecule-1, among others). Nonetheless, further studies are needed to investigate the immunomodulatory role that these microdoses might play in chronic inflammatory processes. The fractionation originally used in our study was of 10 Gy in 10 fractions, with a decrease to 3 Gy in 10 fractions in cases requiring reirradiation.
The treatment of trochanteritis initially consists of local infiltrations and/or rehabilitation in association with anti-inflammatory treatment or analgesics with a variable efficacy. Lievense et al16 reported a rate of response (total or partial improvement in pain) of 66% with corticosteroid injections, similar to what was found in another study which described 61% of maintained response at 6 months.17 Brinks et al18 performed a randomized study including 60 cases in each study arm. One group was treated with injections of triamcinolone acetonide and physiotherapy if necessary, while the other group received analgesia and physiotherapy. The rate of response at 6 months in the first group was 55 vs 34% in the second group, rising to 61 and 60%, respectively, at 12 months.
In 1970, Goldie et al19 performed a double-blind study on the utility of radiation in pain syndromes of the locomotor apparatus. Likewise, two series on radiotherapy in the treatment of trochanteritis have been published only in abstract form, both with lower number of patients than that in our series (26 and 34 patients, respectively) and similar results to ours.6,14 The first and only systematic review of the efficacy of the different treatments applied in trochanteritis was published 40 years later.4 This review included 24 studies with a total of 950 cases and described the variable efficacy of conservative measures and the greater effectiveness of corticosteroid injections as the initial treatment. This review also described the utility of low-energy shock-wave therapy and different surgical approaches in refractory cases. The percentage of response ranged from 40 to 100% according to the treatment applied, although few data were available on the duration of response.
In the present study, all the patients had severe trochanteric pain, with a mean VAS score of 8 at baseline, and nearly half the patients required major opiate derivative treatment. In addition, it should be pointed out that all the subjects had recurrent trochanteritis refractory to previous conventional therapies. Therefore, the significant improvement presented by 70% of patients after radiation therapy, together with the long-term response and the possibility of further improvement with reirradiation in cases of relapse (15/17, 88% patients), suggests that radiotherapy may be an alternative therapeutic approach when non-invasive methods are unsuccessful.
Likewise, it seems logical to assume that associated comorbidities could influence the response to treatment in these patients. Indeed, Brinks et al18 reported that patients with associated osteoarthritis presented a lower response to corticosteroid injections. Although no significant differences were observed in the clinical response to irradiation therapy in our study, 50% of the patients with fibromyalgia required a second reirradiation treatment during follow-up.
In relation to possible radiation-induced carcinogenesis, no previous data in this specific localization are available, although it has been described in the coxofemoral articulation. The only study published to date is that of Sheybani et al20 including a series of 2749 patients with hip replacement, 7% of whom had undergone preventive heterotopic ossification radiotherapy. During the 12-year follow-up with matched pairs (2 : 1), no increase was observed in the risk of carcinogenesis in any particular localization. The doses used were similar to those in our series, although the mean age of the patients differed, with those in our study being more elderly (56 vs 68 years, respectively). In a general review published prior to the present study, Leer et al21 concluded that the risk of radio-induced carcinogenesis has been overestimated. To the contrary, during infancy, the risks advise against the use of anti-inflammatory radiotherapy.22 Considering the possible, albeit improbable, long-term risk of carcinogenesis, patients who are young are usually ruled out from this therapy, and it is generally reserved for populations over 55–60 years of age.
This study has several limitations, such as the absence of a control group with conventional treatment, nevertheless the patients included were refractory to previous conventional therapy, including corticoid local injections and major opiate derivatives. Thereby indicating the need for a long-term study.
At present, there are no studies evaluating the effectiveness of treatment with low-dose irradiation in recurrent refractory trochanteritis. Our results show that anti-inflammatory radiation may be considered an adequate therapeutic option in clinical practice in cases of conventional treatment failure and indicate the need for further studies on this entity.
CONCLUSION
Low-dose anti-inflammatory radiation may be used in the treatment of recurrent cases of relapse or no response of trochanteritis to conventional treatments, with a high probability of achieving total or partial sustained remission of pain. Moreover, in patients who are refractory, rescue treatment may be performed to achieve additional benefits.
Contributor Information
Izaskun Valduvieco, Email: ivalduvi@clinic.ub.es.
Albert Biete, Email: abiete@clinic.cat.
Luis A Moreno, Email: lamoreno@clinic.cat.
Xavier Gallart, Email: xgallart@clinic.cat.
Angels Rovirosa, Email: rovirosa@clinic.cat.
Jordi Saez, Email: josaez@clinic.cat.
Carlos Plana, Email: cplana@clinic.cat.
Pilar Peris, Email: pperis@clinic.cat.
REFERENCES
- 1.Prikhod'ko AK, Sokol GM. Surgical treatment of tuberculous trochanteritis. [In Russian.] Ortop Travmatol Protez 1961; 22: 35–9. [PubMed] [Google Scholar]
- 2.Rovinskii MS. Surgical treatment of tuberculous trochanteritis. [In Russian.] Sov Med 1963; 26: 52–4. [PubMed] [Google Scholar]
- 3.Sorkin AZ. Incidence of tuberculous trochanteritis. [In Russian.] Probl Tuberk 1958; 36: 67–70. [PubMed] [Google Scholar]
- 4.Lustenberger DP, Ng VY, Best TM, Ellis TJ. Efficacy of treatment of trochanteric bursitis: a systematic review. Clin J Sport Med 2011; 21: 447–53. doi: https://doi.org/10.1097/JSM.0b013e318221299c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seegenschmiedt MH, Katalinic A, Makoski H, Haase W, Gademann G, Hassenstein E. Radiation therapy for benign diseases: patterns of care study in Germany. Int J Radiat Oncol Biol Phys 2000; 47: 195–202. doi: https://doi.org/10.1016/S0360-3016(99)00537-4 [DOI] [PubMed] [Google Scholar]
- 6.Seegenschmiedt MH, Micke O, Muecke R. Radiotherapy for non-malignant disorders: state of the art and update of the evidence-based practice guidelines. Br J Radiol 2015; 88: 20150080. doi: https://doi.org/10.1259/bjr.20150080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kern PM, Keilholz L, Forster C, Hallmann R, Herrmann M, Seegenschmiedt MH. Low-dose radiotherapy selectively reduces adhesion of peripheral blood mononuclear cells to endothelium in vitro. Radiother Oncol 2000; 54: 273–82. doi: https://doi.org/10.1016/s0167-8140(00)00141-9 [DOI] [PubMed] [Google Scholar]
- 8.Arenas M, Sabater S, Hernández V, Rovirosa A, Lara PC, Biete A, et al. Anti-inflammatory effects of low-dose radiotherapy. Indications, dose, and radiobiological mechanisms involved. Strahlenther Onkol 2012; 188: 975–81. doi: https://doi.org/10.1016/j.rpor.2013.04.003 [DOI] [PubMed] [Google Scholar]
- 9.Mollà M, Panés J, Casadevall M, Salas A, Conill C, Biete A, et al. Influence of dose-rate on inflammatory damage and adhesion molecule expression after abdominal radiation in the rat. Int J Radiat Oncol Biol Phys 1999; 45: 1011–18. [DOI] [PubMed] [Google Scholar]
- 10.Wunderlich R, Ernst A, Rödel F. Low and moderate doses of ionizing radiation up to 2 Gy modulate transmigration and chemotaxis of activated macrophages, provoke an anti-inflammatory cytokine milieu, but do not impact upon viability and phagocytic function. Clin Exp Immunol 2015; 179: 50–61. doi: https://doi.org/10.1111/cei.12344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trott KR, Kamprad F. Radiobiological mechanisms of anti-inflammatory radiotherapy. Radiother Oncol 1999; 51: 197–203. doi: https://doi.org/10.1016/s0167-8140(99)00066-3 [DOI] [PubMed] [Google Scholar]
- 12.Rödel F, Keilholz L, Herrmann M, Sauer R, Hildebrandt G. Radiobiological mechanisms in inflammatory diseases of low-dose radiation therapy. Int J Radiat Biol 2007; 83: 357–66. doi: https://doi.org/10.1080/09553000701317358 [DOI] [PubMed] [Google Scholar]
- 13.Buprim VV, Zvetkova VV, Novopashinnaya OV. Anti-inflammatory radiotherapy of non-cancer diseases. Radiother Oncol 2004; 71: S25. [Google Scholar]
- 14.Olschewski T, Klein H. Functional radiotherapy for bursitis trochanterica. [In German.] Strahlenther Onkol 2010; 186(Suppl. 1): S40. [Google Scholar]
- 15.Yakoveva N, Kondratyeva T, Moskvin N. Radiotherapy for non-malignant diseases. Radiother Oncol 2004; 71(Suppl. 1): S44. [Google Scholar]
- 16.Lievense A, Bierma-Zeinstra S, Schouten B, Bohnen A, Verhaar J, Koes B. Prognosis of trochanteric pain in primary care. Br J Gen Pract 2005; 55: 199–204. [PMC free article] [PubMed] [Google Scholar]
- 17.Shbeeb MI, O'Duffy JD, Michet CJ, Jr, O'Fallon WM, Matteson EL. Evaluation of glucocorticosteroid injection for the treatment of trochanteric bursitis. J Rheumatol 1996; 23: 2104–6. [PubMed] [Google Scholar]
- 18.Brinks A, van Rijn RM, Willemsen SP, Bohnen AM, Verhaar JA, Koes BW, et al. Corticosteroid injections for greater trochanteric pain syndrome: a randomized controlled trial in primary care. Ann Fam Med 2011; 9: 226–34. doi: https://doi.org/10.1370/afm.1232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldie I, Rosengren B, Moberg E, Hedelin E. Evaluation of radiation treatment of painful conditions of the locomotor system. A double blind study. Acta Radiol Ther Phys Biol 1970; 9: 311–22. doi: https://doi.org/10.3109/02841867009129108 [DOI] [PubMed] [Google Scholar]
- 20.Sheybani A, TenNapel MJ, Lack WD, Clerkin P, Hyer DE, Sun W, et al. Risk of radiation-induced malignancy with heterotopic ossification prophylaxis: a case-control analysis. Int J Radiat Oncol Biol Phys 2014; 89: 584–9. doi: https://doi.org/10.1016/j.ijrobp.2014.03.008 [DOI] [PubMed] [Google Scholar]
- 21.Leer JW, van Houtte P, Seegenschmiedt H. Radiotherapy of non-malignant disorders: where do we stand? Radiother Oncol 2007; 83: 175–7. doi: https://doi.org/10.1016/j.radonc.2007.04.008 [DOI] [PubMed] [Google Scholar]
- 22.Evans DG, Birch JM, Ramsden RT, Sharif S, Baser ME. Malignant transformation and new primary tumours after therapeutic radiation for benign disease: substantial risks in certain tumour prone syndromes. J Med Genet 2006; 43: 289–94. doi: https://doi.org/10.1136/jmg.2005.036319 [DOI] [PMC free article] [PubMed] [Google Scholar]