Abstract
Contrast-enhanced ultrasound (CEUS) represents a complementary technique to greyscale and colour Doppler ultrasonography which allows for real-time visualization and characterization of tissue perfusion. Its inherent advantages in the child makes ultrasonography an ideal imaging modality; repeatability and good tolerance along with the avoidance of CT, a source of ionizing radiation, renders ultrasonography imaging desirable. Although currently paediatric CEUS is principally used in an “off-label” manner, ultrasonography contrast agents have received regulatory approval for assessment of paediatric focal liver lesions (FLL) in the USA. The safety of ultrasound contrast-agents is well documented in adults, as safe as or even surpassing the safety profile of CT and MR contrast agents. Except for the established intracavitary use of CEUS in voiding urosonography, i.v. paediatric applications have been introduced with promising results in the abdominal trauma initial diagnosis and follow-up, characterization and differential diagnosis of FLL and characterization of lung, pleura, renal and splenic pathology. CEUS has also been used to detect complications after paediatric transplantation, evaluate inflammatory bowel disease activity and assess tumour response to antiangiogenic therapy. The purpose of this review was to present these novel i.v. paediatric applications of CEUS and discuss their value.
INTRODUCTION
Ultrasonography is a well-established first-line imaging modality for a series of diseases affecting various systems in the paediatric population. Its suitability relies on the relatively lower proportion of fat and overall small body habitus of children, which allows the acquisition of images of excellent resolution.1 The use of ultrasonography in children is also advantageous owing to its repeatability, lack of ionizing radiation and use of nephrotoxic contrast agents, the lack of sedation and the versatility, allowing use in various settings including in the emergency department, the bedside and operating room, according to the child's clinical needs.2 Certainly, CT and MRI maintain an important position in the investigation of paediatric pathology, but are expensive and have inherent limitations in the child. Radiation-induced malignancy in the child is important; there is evidence that 1/1000 children at 15 years of age undergoing a single CT examination will develop a malignancy during their lifetime, whereas the same risk for children at 1 year of age is 2.5/1000.3,4 With MRI, disadvantages include high cost, the need for sedation and use of gadolinium-based contrast agents which have been related to nephrogenic systemic fibrosis.5 Ideally, CT and MRI should only be performed in children with inconclusive ultrasonography examinations or complicated clinical needs requiring assessment with particular detail only afforded by CT or MRI.
Contrast-enhanced ultrasound (CEUS) has been established as a complementary ultrasonography technique offering a number of advantages over conventional ultrasonography including improved spatial resolution and excellent real-time dynamic evaluation of both macrovascularity and microvascularity of perfused normal and abnormal tissues.6 CEUS has been applied successfully in a wide spectrum of conditions in adults, documented in the guidelines of the European Federation of Societies for Ultrasound in Medicine and Biology.7,8 Although the i.v. use of ultrasonography contrast agents is still “off-label” for the paediatric population in Europe, it has been widely used with documented safety and accuracy.1,9,10 A recent and important development has been the approval by the Food and Drug Administration of the use of CEUS for liver examination in children in the USA,11 and this will alter application not only in the USA but also across the world. Ultrasound practitioners should be mindful that many drugs are used “off-label” in children, and this is not prohibited by medical regulatory authorities. If there is sufficient evidence for their efficacy and safety and parental informed consent is given, their use is permissible with the prescribing physician assuming responsibility for their administration.1,12 In fact, any pharmaceutical product can be used in an “off-licence” manner if the benefit to the patient is greater than the risk associated with an inaccurate diagnosis and possible unsuccessful management. Given the potential negative aspects of CT and MRI in children, it would be highly beneficial to find alternative solutions for the diagnostic work-up, and CEUS would be the obvious alternative.
The purpose of this review was to present and discuss the various i.v. applications of CEUS in children, highlighting the advantages of this modality. Initially, we will explain technical aspects of CEUS peculiar to children and we will document safety of CEUS contrast agents. Then, we will discuss the value of CEUS in blunt abdominal trauma, characterization of focal liver lesions (FLL), transplantation, chest and other novel applications.
CONTRAST-ENHANCED ULTRASOUND: TECHNIQUE AND SAFETY IN CHILDREN
Technique
The CEUS examination follows the i.v. administration of an ultrasonography contrast agent and should follow a detailed conventional ultrasonography examination including greyscale and colour Doppler imaging.7 Ultrasound contrast agents consist of microbubbles of an inert gas encapsulated by a phospholipid shell. SonoVue™ (Bracco SpA, Milan, Italy) is the most widely used ultrasonography contrast agent in Europe.7 These microbubbles are too large (10 µm) to pass through the vascular endothelium, rendering the contrast agent purely intravascular.6 The dose of the ultrasonography contrast agent in adults depends on the organ under examination, but is generally 2.4 ml. With paediatric dosage, there are no standardized recommendations, a consequence of the “off-label” use of CEUS in children.7 According to the Food and Drug Administration recommendation, the dose of SonoVue™ should be based on the body weight and is 0.03 ml per kg, with a maximum of 2.4 ml per injection.13 In our department, the dose administered is adapted to the patient body size, broadly correlating with the child age. We administer 0.6 ml in children <6 years old, 1.2 ml in children between 6 and 12 years of age and 2.4 ml in children >12 years of age. Other suggested dosage schemes are as follows: (a) 0.1 ml of SonoVue™ for every year of age14 and (b) standard single doses of 0.1, 0.5, 1.0, 1.2, 2.4 and 4.8 ml of SonoVue™.15–17 The microbubbles are administered through an i.v. 20-gauge cannula placed in the antecubital fossa and flushed with 5–10 ml of normal saline. The microbubbles can be administered through 16–24-gauge catheters or 18–25-gauge needles, although the manufacturer recommendation is for a catheter >20 gauge. However, no significant difference was found on enhancement or microbubble concentration with catheter or needle sizes ranging from 18 to 21 gauge.18 Contrast-specific ultrasonography imaging modes are deployed, which specifically discriminate the non-linear response from microbubbles and suppress the linear signal originating from the static tissues, thus creating an image containing only signals from the microbubbles.7 Particular advantages of the use of CEUS in children and technical aspects of this examination are summarized in Tables 1 and 2, respectively.
Table 1.
Contrast-enhanced ultrasound advantages, making it particularly beneficial for children
| Potential problem-solving tool within the same day/visit for the ultrasonography examination |
| Cost effective |
| No sedation |
| No ionizing radiation |
| No nephrotoxic contrast agent |
| Body habitus ideal for ultrasonography |
| Repeatable |
| Can be performed in a variety of settings (bedside, etc.) |
| Fewer adverse events than CT and MR contrast agents |
Table 2.
Remarks on i.v. contrast-enhanced ultrasound technique according to the organ under examination
| Organ | Remarks on technique |
|---|---|
| Liver | Targeted evaluation of the enhancement pattern of a focal lesion in real time |
| Timing of vascular phases different from adults and varies based on age | |
| Arterial phase may start as quickly as 5 s following the administration of microbubbles | |
| May need to do a “sweep scan” to search for focal lesions or trauma | |
| Transplantation | Knowledge of the surgical technique and the exact type of vascular anastomosis is essential for accurate diagnosis |
| Colour and spectral Doppler imaging is still required to assess clinically significant vascular stenosis | |
| Kidney | Rapid cortical enhancement followed by medullary phase lasting up to 2 min post-injection |
| No evaluation of pelvicalyceal system as microbubbles are not excreted | |
| Spleen | Targeted evaluation of the perfusion pattern of a focal lesion |
| Keep in mind the peculiar enhancement pattern of spleen including inhomogeneous (“zebra-like”) initial phase and long-lasting homogeneous delayed enhancement | |
| May need to do a “sweep scan” to detect focal lesions particularly in trauma | |
| Trauma | Two separate doses of microbubbles administered for liver and right kidney and then spleen and left kidney ± pancreas |
| Examination starting from side of clinical concern | |
| Kidneys should be evaluated first owing to earlier enhancement, in the arterial phase, whereas liver and spleen can be assessed during the portal venous phases | |
| Traumatic lesions appear as well-demarcated hypoechoic (non-enhancing) areas | |
| Careful evaluation of the vasculature will detect any pseudoaneurysms | |
| Bowel | 4 h of fasting required |
| Conventional ultrasonography precedes to detect thickened loops | |
| Lower dose of microbubbles are administered when low-frequency transducers are used | |
| Higher dose of microbubbles are administered when high-frequency transducers are used | |
| Quantification of mural enhancement is valuable | |
| Lung/pleura | Targeted evaluation can be performed using coronal plane, similarly to conventional ultrasonography |
Safety
Ultrasound contrast administration requires no preliminary laboratory examinations and has limited contraindications.7 The main contraindications include history of allergic reaction to the contrast agent itself, known right-to-left shunt, severe pulmonary hypertension, uncontrolled systemic hypertension and unclear pregnancy status.13 Nevertheless, the contraindication regarding known right-to-left shunt is currently considered controversial with published recommendations for its removal, as there is not enough evidence to support this.19
The SonoVue™ contrast agent has a proven safety record in adults, documented in a large study of >23,000 patients.20 In this study, serious adverse reactions occurred in 0.0086% patients and only four of the patients with an allergic reaction required treatment.20 This rate is comparable with that reported for MR contrast agents (0.0088%)21 and significantly lower than that associated with CT contrast agents (0.6%).22 In the paediatric population, limited studies evaluated the safety profile of ultrasonography contrast agents.23–28 The largest series involved 167 CEUS examinations using SonoVue™ in 137 children, which documented 1 (0.6%) severe allergic reaction. However, no other haemodynamic and oxygenation status changes were documented in this study, and no other subjective complaints were recorded following the CEUS examination.26 In a retrospective questionnaire-based survey among paediatric radiologists in Europe, only six minor adverse reactions were recorded after the i.v. administration of the ultrasonography contrast. These reactions affected the skin, taste and respiratory frequency.27 In a series of 37 paediatric patients undergoing CEUS for various reasons including lesion characterization, trauma and infection, there was only 1 child who reported self-limiting nausea requiring no treatment.14 In a group of children with solid malignancies, the administration of ultrasonography contrast did not significantly affect the haemodynamic parameters of any patient, while only mild and transient adverse reactions including taste alteration and light-headedness were observed in <2.2% of examinations.24 A study based on a single-centre experience showed no immediate adverse reactions in 305 paediatric CEUS examinations and only 2 (0.7%) delayed adverse reactions.9 In another study examining children with malignancies, only 2 of the 13 children undergoing CEUS complained of minor and self-limiting symptoms. No change attributable to the ultrasonography contrast was detected on neurological, funduscopic examination, electrocardiography and continuous pulse oximetry.23 In an older study of contrast-enhanced echocardiography examining 20 patients, no children showed adverse haemodynamic reactions, change in taste or flushing episodes, whereas headache was reported in only 3 cases.25 Based on these studies, ultrasonography contrast agents can be considered equally safe for adults and children. Nonetheless, resuscitation equipment should be available where CEUS is performed.
CLINICAL APPLICATIONS
Blunt abdominal trauma
Trauma represents an important cause of morbidity and mortality in the paediatric population.29,30 Blunt abdominal trauma accounts for 80% of cases, with liver and spleen being the most frequently injured organs.30 Initial diagnostic work-up depends on severity of trauma. Children with low-energy or localized trauma can be adequately managed using ultrasonography alone, although considered inadequate by some authors.30 Focused assessment with sonography for trauma is valuable in detecting haemoperitoneum and crucial for the initial evaluation of patients who are haemodynamically unstable,31,32 with reported 80% sensitivity and 96% specificity for detecting haemoperitoneum.32 However, up to 30% of solid organ traumatic lesions can be missed on a focused assessment with sonography for trauma scan.33,34 CT is characterized by excellent diagnostic accuracy for the detection of abdominal traumatic injuries but should be limited by ionizing radiation in children.29,31,35 CT imaging may not be appropriate for low- or moderate-energy isolated trauma where the diagnostic yield is insignificant.35,36 CEUS could be an alternative modality as a complementary technique to greyscale ultrasonography and has been shown to improve the detection of solid organ injuries in adults.29 CEUS is perfectly suited for the follow-up of patients with paediatric trauma, without the need for ionizing radiation, sedation and nephrotoxic contrast agents and no compromise in terms of diagnostic accuracy.31
A recently published retrospective analysis of 73 haemodynamically stable children sustaining minor abdominal trauma compared CEUS with baseline ultrasonography and CT.37 In this study, ultrasonography detected only 26/67 (38.8%) parenchymal traumatic lesions involving the liver, spleen and kidneys, whereas CEUS was concordant with CT in every patient (Figure 1). CEUS also identified active parenchymal bleeding in 50% of cases seen on CT and one case of partial devascularization.37 CEUS has been shown to detail renal cortical necrosis in a child following blunt abdominal trauma. CEUS findings were correlated and confirmed by gadolinium-enhanced MRI, indicating its excellent spatial resolution.38 One of the first prospective studies regarding blunt abdominal trauma in 27 children also compared ultrasonography and CEUS for the depiction of solid organ injuries, with CT as the reference method.39 CEUS was 92.2% sensitive and 100% specific, with 100% positive- and negative-predictive values, outperforming conventional ultrasonography and being nearly as accurate as CT.39 CEUS accurately detects splenic injuries not seen on conventional ultrasonography, often negating imaging with CT.40 Another multicentre study enrolling 156 patients with trauma, both adults and children, evaluated the diagnostic accuracy of ultrasonography and CEUS for the diagnosis of solid viscera injuries. CEUS showed superior diagnostic accuracy to ultrasonography in terms of renal, liver and spleen trauma, often averting further imaging. The limited false-negative results of CEUS in this study were caused by minor injuries having no implications for patient management.41 Similarly, another mixed population study concluded that CEUS was significantly better than ultrasonography both in diagnosing and accurately staging traumatic lesions affecting the liver, spleen and kidneys. On the other hand, CEUS only marginally increased diagnostic accuracy for the detection of haemoperitoneum, where ultrasonography alone was sufficiently accurate.42 Similar conclusions regarding the accuracy of CEUS for the detection of solid organ traumas were drawn by other mixed populations studies.35,43–45 As a consequence, it is reasonable to assume that CEUS could replace ultrasonography for the initial screening of low- or moderate-energy, isolated abdominal trauma and CT should be used only for the exclusion of active haemorrhage in a patient who is haemodynamically unstable with negative ultrasonography for active bleeding.35,40–42
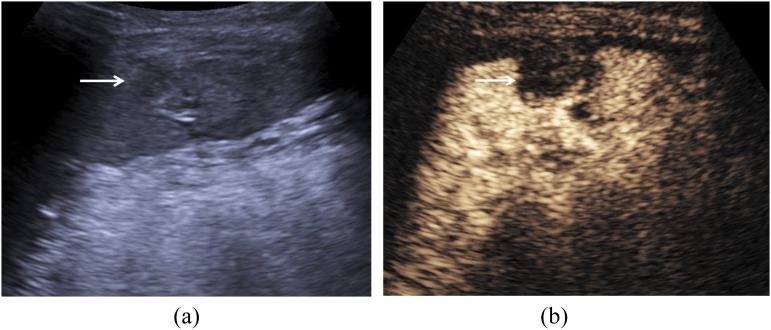
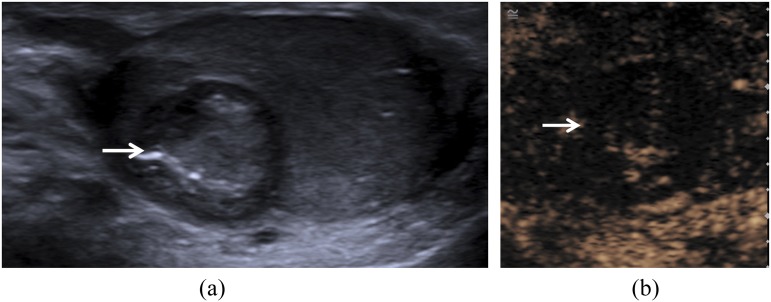
Figure 1.
A 7-year-old male sustaining blunt abdominal trauma: B-mode ultrasonography (a) has identified an area of increased echogenicity and ill-defined borders (arrow) in the spleen. Contrast-enhanced ultrasound (b) is showing normal enhancement of the splenic parenchyma but no enhancement within the previously described area (arrow), establishing the diagnosis of a haematoma.
Besides parenchymal injuries, CEUS has been found valuable for the identification of traumatic pseudoaneurysms.46 In a series of 101 children with blunt or penetrating trauma, CEUS detected liver and splenic pseudoaneurysms with 83% sensitivity, 92% specificity, 71% positive-predictive value and 96% negative-predictive value. Although these values are inferior to CT, CEUS is superior to conventional ultrasonography, particularly for the follow-up of these pseudoaneurysms.46
CEUS can also be used for the follow-up of blunt abdominal trauma in adults and children, with a study demonstrating successful monitoring to complete resolution in minor traumatic lesions of the liver and spleen in patients being treated conservatively.47 CEUS was also found useful in identifying and following up pancreatic injuries missed on ultrasonography but diagnosed on CT and MRI.48
Focal liver lesions
FLL can be readily characterized by CEUS in the adult population.8 Although primarily referring to adult patients, the European Federation of Societies for Ultrasound in Medicine and Biology guidelines can be extrapolated to the paediatric population. Although representing an “off-label” use of CEUS in Europe, unlike in the USA, the liver is the most frequently examined organ and FLL characterization the commonest indication for paediatric CEUS examinations.27,49
A small number of studies dedicated to the characterization of paediatric FLL are available. One study evaluated CEUS in 44 children with inconclusive greyscale FLL having consensus multimodality imaging or histology as reference method.16 This study showed an agreement with the reference imaging in 85% of cases. The majority of indeterminate FLL were identified as focal fatty sparing and infiltration, focal nodular hyperplasia (Figure 2), regenerative nodules and adenoma.16 Another study included 37 children undergoing CEUS for multiple indications including FLL characterization; CEUS was suitable for discrimination of cystic and solid lesions and demonstration of parenchymal perfusion.14 In a paediatric multimodality study comparing CEUS, CT and MRI, CEUS accurately differentiated benign from malignant lesions in the majority of patients and often provided the correct final diagnosis. Concordance between CEUS and MRI and between CEUS and CT was good and in nearly half of the cases, CEUS could have been the only modality used.50 CEUS is also useful in identifying non-enhancing necrotic parts and enhancing septae within liver abscesses (Figure 3).
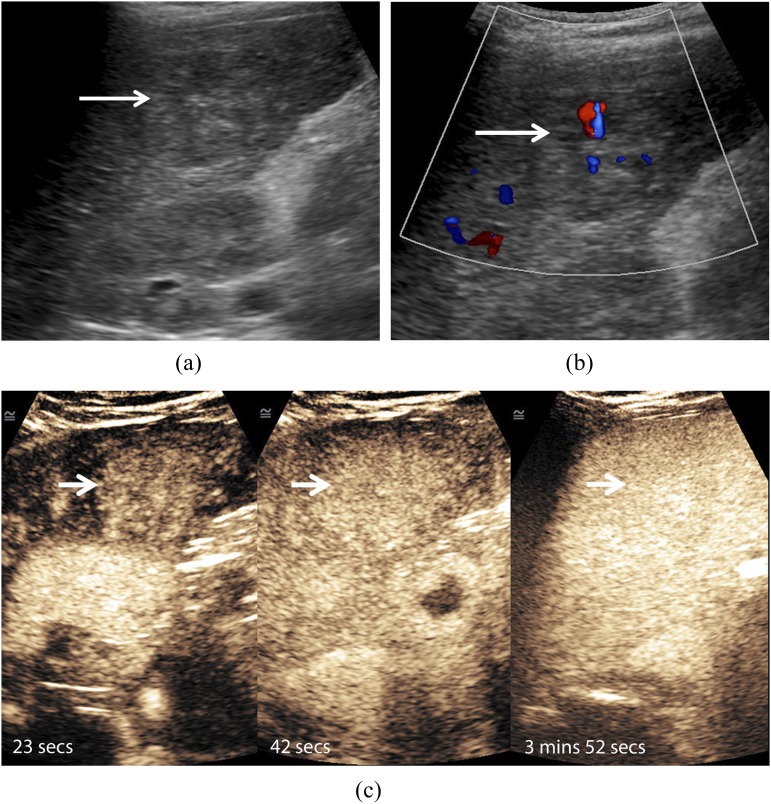
Figure 2.
A 12-year-old male diagnosed with focal nodular hyperplasia (FNH): B-mode ultrasonography (a) has identified a heterogeneous ill-defined focal liver lesion (arrow). Colour Doppler technique (b) is revealing the presence of blood vessels in the central part of the lesion (arrow). Following the administration of 2.4 ml of SonoVue™ (Bracco SpA, Milan, Italy), contrast-enhanced ultrasound (c) is demonstrating a centrifugal pattern of enhancement of the lesion (arrows) and no washout in the late phase, establishing the diagnosis of an FNH.
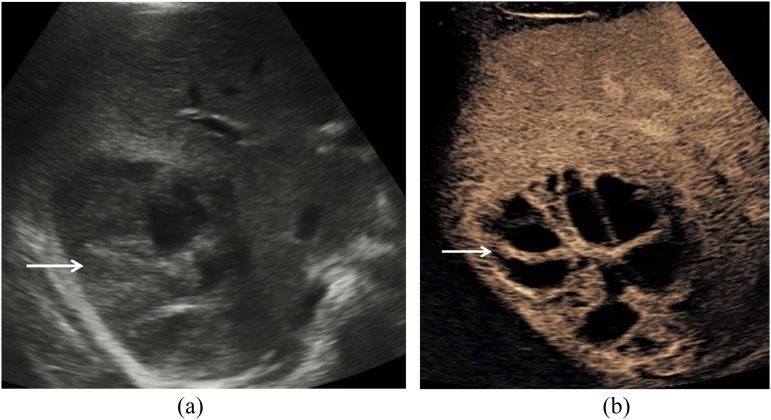
Figure 3.
An 11-year-old male diagnosed with a liver abscess: B-mode ultrasonography (a) is demonstrating a heterogeneous focal liver lesion (arrow) situated in the right liver lobe. Contrast-enhanced ultrasound (b) is highlighting the presence of unenhanced parts of the lesion and enhancing internal septae (arrow), with findings in keeping with an abscess.
Part of the existing evidence in the CEUS characterization of paediatric FLL also derives from studies enrolling both adults and children.51–58 A recent study comparing conventional ultrasonography, CEUS and elastography with histology as the reference method concluded that CEUS was 92% sensitive and 89% specific for the diagnosis of malignant liver lesions, significantly outperforming unenhanced ultrasonography and elastography.51 Likewise, another study examining CEUS for the differentiation of benign and malignant FLL showed a sensitivity of 95% and specificity of 97.9%.57
Paediatric transplantation
Similarly to adults where official guidelines and recommendations have been issued,8 CEUS can be used in paediatric patients after transplantation. The main purposes include evaluation of vascular patency and complications, transplanted tissue perfusion and identification of necrotic areas, characterization of new focal lesions and evaluation of post-operative complications including fluid collections.8,17,59–62
A study of a mixed adult and paediatric population following liver transplantation assessed CEUS contribution when there was uncertainty on other imaging modalities. CEUS could further characterize suspected findings in all patients while it detected new clinically significant findings in about half of the patients. Diagnoses established with the use of CEUS included stenosis of the portal vein or hepatic artery, local cholestasis, intestinal bleeding, benign tumours and assessment of perfusion abnormality of the liver.60 One dedicated paediatric study evaluated the potential use of CEUS for the detection of post-operative complications after liver transplantation, using invasive modalities including CT and angiography as the reference methods. CEUS successfully diagnosed all but one case of hepatic artery thrombosis and all patients with portal and hepatic vein thrombosis. A case of hepatic artery stenosis was missed while the false-negative result of hepatic artery thrombosis was caused by collateral circulation originating from the phrenic artery. Although ultrasonography contrast agents improved visualization of bile leaks, the authors felt that CEUS was not significantly helpful in the identification of biliary complications. However, they concluded that it can confidently detect important post-operative complications, averting the need for invasive techniques.17
Lung and pleura
The evaluation of lung and pleural space with CEUS has been primarily investigated in adults and represents a novel application for children. It can be used for either lung consolidation or pleural-based lesion characterization. In the former case, CEUS is highly sensitive for distinguishing perfused and viable tissues from avascular necrotic tissues and delineation of parapneumonic fluid collections (Figure 4).63,64 Consequently, CEUS can be used to differentiate uncomplicated lung consolidation from cavitating pneumonia63 and provides clinically significant information, addressing specific clinical questions and guiding patient management, an important use in the child with complicated pneumonia. Careful evaluation of the enhancement pattern of pleural lesions also contributes to the accurate diagnosis of pleuropneumonia.65
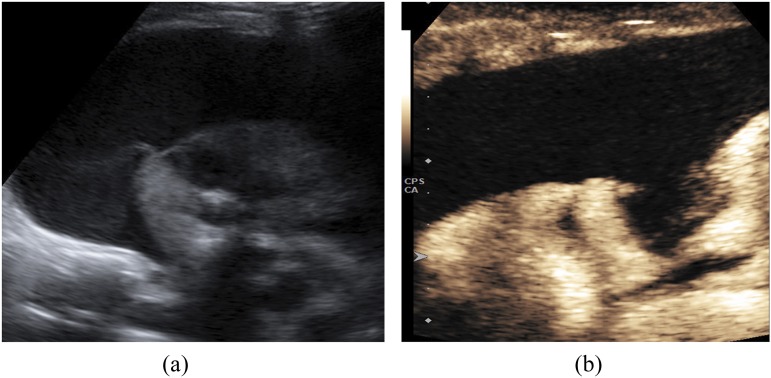
Figure 4.
A 4-year-old male with pneumonia complicated with empyema: B-mode ultrasound (a) is showing lung consolidation and the presence of an anechoic parapneumonic effusion. Contrast-enhanced ultrasound (b) is demonstrating the enhancement of the consolidated lung parenchyma and has accurately delineated the empyema, which showed no enhancement.
Assessing tumour response to antiangiogenic therapy
The inherent property of microbubbles to be strictly intravascular agents renders them ideal for sensitive identification of tumoral vascularity. As a result, CEUS could be potentially used to evaluate tumour perfusion and monitor tumour response to antiangiogenic treatment.66 A recent mixed adult and child pilot study has showed that quantification CEUS parameters like peak enhancement or rate of enhancement could predict time to progression of recurrent solid tumours treated with antiangiogenic therapy. Malignancies included in this study affected the liver, pleura, soft tissues, lung, retroperitoneum and peritoneum, lymph nodes and others.67 These novel promising results need further validation before widespread use in the paediatric population.
OTHER APPLICATIONS
The potential use of CEUS in the characterization of adrenal lesions in children is documented in an individual report, where it was found to correlate well with CT and MRI.68 The application of CEUS to trauma of the adrenal gland in children shows good correlation with CT imaging.69 Nevertheless, it is characterized by limited accuracy in differentiating benign and malignant adrenal lesions in adults.7,70
The i.v. applications of CEUS in the kidneys have been mainly evaluated in adults and include differentiation of tumours from pseudotumours, benign and malignant lesions and characterization of complex cysts.7,71 CEUS was reported to accurately delineate renal cortical necrosis in a child sustaining trauma38 and could be used for the diagnosis of acute renal transplant rejection or other vascular complications after transplantation in the future.72
Based on currently available recommendations, CEUS can be used to grade disease activity and extent in adult patients with inflammatory bowel disease and differentiate active inflammation from chronic fibrosis in intestinal loops.7,73,74 Mural perfusion can be quantified, providing repeatable parameters which accurately represent disease activity, monitor response to treatment75 and detect post-operative recurrence.76 Based on the scarce available evidence, CEUS can be used for the same purpose in the paediatric population.77,78
CEUS has been introduced to accurately evaluate and follow up inflammatory changes in paediatric patients with rheumatism. Response to treatment could also be assessed using ultrasonography contrast agents.79 CEUS has also been occasionally used for diagnostic approach of vascular malformations of the extremities80 and characterization of scrotal lesions81 (Figure 5).
Figure 5.
A 15-year-old male with incidentally found testicular lesion: B-mode ultrasonography (a) is showing a rounded isoechoic lesion (arrow) with a hypoechoic halo and central hyperechoic parts. Contrast-enhanced ultrasound (b) is showing limited internal echoes excluding the presence of a malignant tumour and establishing the diagnosis of an epidermoid tumour (arrow).
CONCLUSION
CEUS has distinct advantages over both CT and MRI when it comes to the paediatric population.1,6,16,82 It is well established that radiation-induced malignancy constitutes a potential problem,3,4 the long-term effects of gadolinium deposition in the paediatric population are unclear,83 sedation is required in MRI and the use of nephrotoxic contrast agents in patients with reduced renal function should be avoided. CEUS offers a valuable alternative albeit with limited existing evidence. It is expected that as evidence grows around adult CEUS applications, this will guide research in the paediatric population. CEUS although should not be regarded as a panacea or a technique capable of completely replacing CT or MRI in children It is a technique characterized by certain limitations associated with ultrasonography while CT and MRI still maintain an important place in paediatric diagnostic pathways although entailing the aforementioned drawbacks. Nevertheless, CEUS has recently emerged as an ultrasonographic complementary technique which could be potentially used to increase the information provided by ultrasonography or as an alternative to CT or MRI in certain clinical scenarios, as presented in this review.
The setting in which paediatric CEUS should be ideally performed is within an established department, with ultrasonography machines having contrast-specific ultrasonography modes such as pulse inversion or amplitude modulation. Of paramount importance is the availability of equipment and facilities to treat allergic reactions, as although rare, practitioners must be prepared for such an eventuality. Paediatric CEUS can be performed by anyone who is trained and has experience in current paediatric applications. Although paediatric radiologists are more familiar with paediatric applications, it is our belief that even general radiologists familiar with techniques of CEUS, and after specific training, are equipped to perform paediatric CEUS examinations.
CONFLICTS OF INTEREST
Annamaria Deganello—Bracco Speaker. Paul S Sidhu—Bracco, Hitachi, Siemens, GE Healthcare, Philips Speaker. Maria E Sellars–Bracco Speaker.
Contributor Information
Vasileios Rafailidis, Email: billraf@hotmail.com.
Annamaria Deganello, Email: adeganello@nhs.net.
Tom Watson, Email: tom.watson@gosh.nhs.uk.
Paul S Sidhu, Email: paulsidhu@nhs.net.
Maria E Sellars, Email: maria.sellars@nhs.net.
REFERENCES
- 1.Sellars ME, Deganello A, Sidhu PS. Paediatric contrast-enhanced ultrasound (CEUS): a technique that requires co-operation for rapid implementation into clinical practice. Ultraschall Med 2014; 35: 203–6. doi: https://doi.org/10.1055/s-0034-1366567 [DOI] [PubMed] [Google Scholar]
- 2.McCarville MB. Contrast-enhanced sonography in pediatrics. Pediatr Radiol 2011; 41(Suppl. 1): S238–42. doi: https://doi.org/10.1007/s00247-011-2005-7 [DOI] [PubMed] [Google Scholar]
- 3.Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012; 380: 499–505. doi: https://doi.org/10.1016/S0140-6736(12)60815-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001; 176: 289–96. doi: https://doi.org/10.2214/ajr.176.2.1760289 [DOI] [PubMed] [Google Scholar]
- 5.Nardone B, Saddleton E, Laumann AE, Edwards BJ, Raisch DW, McKoy JM, et al. Pediatric nephrogenic systemic fibrosis is rarely reported: a RADAR report. Pediatr Radiol 2014; 44: 173–80. doi: https://doi.org/10.1007/s00247-013-2795-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cantisani V, Wilson SR. CEUS: where are we in 2015? Eur J Radiol 2015; 84: 1621–2. doi: https://doi.org/10.1016/j.ejrad.2015.05.028 [DOI] [PubMed] [Google Scholar]
- 7.Piscaglia F, Nolsoe C, Dietrich CF, Cosgrove DO, Gilja OH, Bachmann Nielsen M, et al. The EFSUMB guidelines and recommendations on the clinical practice of contrast enhanced ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med 2012; 33: 33–59. doi: https://doi.org/10.1055/s-0031-1281676 [DOI] [PubMed] [Google Scholar]
- 8.Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsoe CP, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver—update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultrasound Med Biol 2013; 39: 187–210. doi: https://doi.org/10.1016/j.ultrasmedbio.2012.09.002 [DOI] [PubMed] [Google Scholar]
- 9.Yusuf GT, Sellars ME, Deganello A, Cosgrove DO, Sidhu PS. A retrospective analysis of the safety and cost implications of pediatric contrast enhanced ultrasound (CEUS) in a single centre. AJR Am J Roentgenol 2016. [DOI] [PubMed] [Google Scholar]
- 10.Sidhu PS, Cantisani V, Deganello A, Dietrich CF, Duran C, Franke D, et al. Role of contrast-enhanced ultrasound (CEUS) in paediatric practice: an EFSUMB position statement. Ultraschall Med 2016. doi: https://doi.org/10.1055/s-0042-110394 [DOI] [PubMed] [Google Scholar]
- 11.Food and Drug Administration. Approved Drug Product List 2016. Available from: http://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/ucm071118.pdf
- 12.Pandolfini C, Bonati M. A literature review on off-label drug use in children. Eur J Pediatr 2005; 164: 552–8. doi: https://doi.org/10.1007/s00431-005-1698-8 [DOI] [PubMed] [Google Scholar]
- 13.Bracco. Lumason Prescribing Information 2016. Available from: http://imaging.bracco.com/sites/braccoimaging.com/files/technica_sheet_pdf/US-20160330-LUMASON-PI_0.pdf
- 14.Stenzel M. Intravenous contrast-enhanced sonography in children and adolescents—a single center experience. J Ultrason 2013; 13: 133–44. doi: https://doi.org/10.15557/JoU.2013.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Piskunowicz M, Kosiak W, Batko T. Intravenous application of second-generation ultrasound contrast agents in children: a review of the literature. Ultraschall Med 2012; 33: 135–40. doi: https://doi.org/10.1055/s-0031-1281936 [DOI] [PubMed] [Google Scholar]
- 16.Jacob J, Deganello A, Sellars ME, Hadzic N, Sidhu PS. Contrast enhanced ultrasound (CEUS) characterization of grey-scale sonographic indeterminate focal liver lesions in pediatric practice. Ultraschall Med 2013; 34: 529–40. doi: https://doi.org/10.1055/s-0033-1355785 [DOI] [PubMed] [Google Scholar]
- 17.Bonini G, Pezzotta G, Morzenti C, Agazzi R, Nani R. Contrast-enhanced ultrasound with SonoVue in the evaluation of postoperative complications in pediatric liver transplant recipients. J Ultrasound 2007; 10: 99–106. doi: https://doi.org/10.1016/j.jus.2007.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eisenbrey JR, Daecher A, Kramer MR, Forsberg F. Effects of needle and catheter size on commercially available ultrasound contrast agents. J Ultrasound Med 2015; 34: 1961–8. doi: https://doi.org/10.7863/ultra.14.11008 [DOI] [PubMed] [Google Scholar]
- 19.Parker JM, Weller MW, Feinstein LM, Adams RJ, Main ML, Grayburn PA, et al. Safety of ultrasound contrast agents in patients with known or suspected cardiac shunts. Am J Cardiol 2013; 112: 1039–45. doi: https://doi.org/10.1016/j.amjcard.2013.05.042 [DOI] [PubMed] [Google Scholar]
- 20.Piscaglia F, Bolondi L, Italian society for ultrasound in medicine and biology (SIUMB) study group on ultrasound contrast agents. The safety of SonoVue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol 2006; 32: 1369–75. doi: https://doi.org/10.1016/j.ultrasmedbio.2006.05.031 [DOI] [PubMed] [Google Scholar]
- 21.Prince MR, Zhang H, Zou Z, Staron RB, Brill PW. Incidence of immediate gadolinium contrast media reactions. AJR Am J Roentgenol 2011; 196: W138–43. doi: https://doi.org/10.2214/AJR.10.4885 [DOI] [PubMed] [Google Scholar]
- 22.Wang CL, Cohan RH, Ellis JH, Caoili EM, Wang G, Francis IR. Frequency, outcome, and appropriateness of treatment of nonionic iodinated contrast media reactions. AJR Am J Roentgenol 2008; 191: 409–15. doi: https://doi.org/10.2214/AJR.07.3421 [DOI] [PubMed] [Google Scholar]
- 23.McCarville MB, Kaste SC, Hoffer FA, Khan RB, Walton RC, Alpert BS, et al. Contrast-enhanced sonography of malignant pediatric abdominal and pelvic solid tumors: preliminary safety and feasibility data. Pediatr Radiol 2012; 42: 824–33. doi: https://doi.org/10.1007/s00247-011-2338-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coleman JL, Navid F, Furman WL, McCarville MB. Safety of ultrasound contrast agents in the pediatric oncologic population: a single-institution experience. AJR Am J Roentgenol 2014; 202: 966–70. doi: https://doi.org/10.2214/AJR.13.12010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McMahon CJ, Ayres NA, Bezold LI, Lewin MB, Alonzo M, Altman CA, et al. Safety and efficacy of intravenous contrast imaging in pediatric echocardiography. Pediatr Cardiol 2005; 26: 413–17. doi: https://doi.org/10.1007/s00246-004-0795-1 [DOI] [PubMed] [Google Scholar]
- 26.Piskunowicz M, Kosiak W, Batko T, Piankowski A, Polczynska K, Adamkiewicz-Drozynska E. Safety of intravenous application of second-generation ultrasound contrast agent in children: prospective analysis. Ultrasound Med Biol 2015; 41: 1095–9. doi: https://doi.org/10.1016/j.ultrasmedbio.2014.11.003 [DOI] [PubMed] [Google Scholar]
- 27.Riccabona M. Application of a second-generation US contrast agent in infants and children—a European questionnaire-based survey. Pediatr Radiol 2012; 42: 1471–80. doi: https://doi.org/10.1007/s00247-012-2472-5 [DOI] [PubMed] [Google Scholar]
- 28.Darge K, Papadopoulou F, Ntoulia A, Bulas DI, Coley BD, Fordham LA, et al. Safety of contrast-enhanced ultrasound in children for non-cardiac applications: a review by the society for pediatric radiology (SPR) and the international contrast ultrasound society (ICUS). Pediatr Radiol 2013; 43: 1063–73. doi: https://doi.org/10.1007/s00247-013-2746-6 [DOI] [PubMed] [Google Scholar]
- 29.Miele V, Piccolo CL, Trinci M, Galluzzo M, Ianniello S, Brunese L. Diagnostic imaging of blunt abdominal trauma in pediatric patients. Radiol Med 2016; 121: 409–30. doi: https://doi.org/10.1007/s11547-016-0637-2 [DOI] [PubMed] [Google Scholar]
- 30.Sivit CJ. Imaging children with abdominal trauma. AJR Am J Roentgenol 2009; 192: 1179–89. doi: https://doi.org/10.2214/AJR.08.2163 [DOI] [PubMed] [Google Scholar]
- 31.Cagini L, Gravante S, Malaspina CM, Cesarano E, Giganti M, Rebonato A, et al. Contrast enhanced ultrasound (CEUS) in blunt abdominal trauma. Crit Ultrasound J 2013; 5(Suppl. 1): S9. doi: https://doi.org/10.1186/2036-7902-5-S1-S9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Holmes JF, Gladman A, Chang CH. Performance of abdominal ultrasonography in pediatric blunt trauma patients: a meta-analysis. J Pediatr Surg 2007; 42: 1588–94. doi: https://doi.org/10.1016/j.jpedsurg.2007.04.023 [DOI] [PubMed] [Google Scholar]
- 33.Poletti PA, Kinkel K, Vermeulen B, Irmay F, Unger PF, Terrier F. Blunt abdominal trauma: should US be used to detect both free fluid and organ injuries? Radiology 2003; 227: 95–103. doi: https://doi.org/10.1148/radiol.2271020139 [DOI] [PubMed] [Google Scholar]
- 34.Richards JR, Knopf NA, Wang L, McGahan JP. Blunt abdominal trauma in children: evaluation with emergency US. Radiology 2002; 222: 749–54. doi: https://doi.org/10.1148/radiol.2223010838 [DOI] [PubMed] [Google Scholar]
- 35.Thorelius L. Emergency real-time contrast-enhanced ultrasonography for detection of solid organ injuries. Eur Radiol 2007; 17(Suppl. 6): F107–11. [DOI] [PubMed] [Google Scholar]
- 36.Pinto F, Miele V, Scaglione M, Pinto A. The use of contrast-enhanced ultrasound in blunt abdominal trauma: advantages and limitations. Acta Radiol 2014; 55: 776–84. doi: https://doi.org/10.1177/0284185113505517 [DOI] [PubMed] [Google Scholar]
- 37.Menichini G, Sessa B, Trinci M, Galluzzo M, Miele V. Accuracy of contrast-enhanced ultrasound (CEUS) in the identification and characterization of traumatic solid organ lesions in children: a retrospective comparison with baseline US and CE-MDCT. Radiol Med 2015; 120: 989–1001. doi: https://doi.org/10.1007/s11547-015-0535-z [DOI] [PubMed] [Google Scholar]
- 38.Yusuf GT, Sellars ME, Huang DY, Deganello A, Sidhu PS. Cortical necrosis secondary to trauma in a child: contrast-enhanced ultrasound comparable to magnetic resonance imaging. Pediatr Radiol 2014; 44: 484–7. doi: https://doi.org/10.1007/s00247-013-2818-7 [DOI] [PubMed] [Google Scholar]
- 39.Valentino M, Serra C, Pavlica P, Labate AM, Lima M, Baroncini S, et al. Blunt abdominal trauma: diagnostic performance of contrast-enhanced US in children—initial experience. Radiology 2008; 246: 903–9. doi: https://doi.org/10.1148/radiol.2463070652 [DOI] [PubMed] [Google Scholar]
- 40.Oldenburg A, Hohmann J, Skrok J, Albrecht T. Imaging of paediatric splenic injury with contrast-enhanced ultrasonography. Pediatr Radiol 2004; 34: 351–4. doi: https://doi.org/10.1007/s00247-003-1092-5 [DOI] [PubMed] [Google Scholar]
- 41.Catalano O, Aiani L, Barozzi L, Bokor D, De Marchi A, Faletti C, et al. CEUS in abdominal trauma: multi-center study. Abdom Imaging 2009; 34: 225–34. doi: https://doi.org/10.1007/s00261-008-9452-0 [DOI] [PubMed] [Google Scholar]
- 42.Sessa B, Trinci M, Ianniello S, Menichini G, Galluzzo M, Miele V. Blunt abdominal trauma: role of contrast-enhanced ultrasound (CEUS) in the detection and staging of abdominal traumatic lesions compared to US and CE-MDCT. Radiol Med 2015; 120: 180–9. doi: https://doi.org/10.1007/s11547-014-0425-9 [DOI] [PubMed] [Google Scholar]
- 43.Miele V, Buffa V, Stasolla A, Regine G, Atzori M, Ialongo P, et al. Contrast enhanced ultrasound with second generation contrast agent in traumatic liver lesions. [In Italian.] Radiol Med 2004; 108: 82–91. [PubMed] [Google Scholar]
- 44.Catalano O, Lobianco R, Sandomenico F, Mattace Raso M, Siani A. Real-time, contrast-enhanced sonographic imaging in emergency radiology. [In Italian.] Radiol Med 2004; 108: 454–69. [PubMed] [Google Scholar]
- 45.Catalano O, Lobianco R, Sandomenico F, D'Elia G, Siani A. Real-time contrast-enhanced ultrasound of the spleen: examination technique and preliminary clinical experience. [In Italian.] Radiol Med 2003; 106: 338–56. [PubMed] [Google Scholar]
- 46.Durkin N, Deganello A, Sellars ME, Sidhu PS, Davenport M, Makin E. Post-traumatic liver and splenic pseudoaneurysms in children: diagnosis, management, and follow-up screening using contrast enhanced ultrasound (CEUS). J Pediatr Surg 2016; 51: 289–92. doi: https://doi.org/10.1016/j.jpedsurg.2015.10.074 [DOI] [PubMed] [Google Scholar]
- 47.Manetta R, Pistoia ML, Bultrini C, Stavroulis E, Di Cesare E, Masciocchi C. Ultrasound enhanced with sulphur-hexafluoride-filled microbubbles agent (SonoVue) in the follow-up of mild liver and spleen trauma. Radiol Med 2009; 114: 771–9. doi: https://doi.org/10.1007/s11547-009-0406-6 [DOI] [PubMed] [Google Scholar]
- 48.Valentino M, Galloni SS, Rimondi MR, Gentili A, Lima M, Barozzi L. Contrast-enhanced ultrasound in non-operative management of pancreatic injury in childhood. Pediatr Radiol 2006; 36: 558–60. doi: https://doi.org/10.1007/s00247-006-0157-7 [DOI] [PubMed] [Google Scholar]
- 49.Rosado E, Riccabona M. Off-label use of ultrasound contrast agents for intravenous applications in children: analysis of the existing literature. J Ultrasound Med 2016; 35: 487–96. doi: https://doi.org/10.7863/ultra.15.02030 [DOI] [PubMed] [Google Scholar]
- 50.Pschierer K, Grothues D, Rennert J, da Silva NP, Schreyer AG, Melter M, et al. Evaluation of the diagnostic accuracy of CEUS in children with benign and malignant liver lesions and portal vein anomalies. Clin Hemorheol Microcirc 2015; 61: 333–45. doi: https://doi.org/10.3233/CH-152003 [DOI] [PubMed] [Google Scholar]
- 51.Zhang P, Zhou P, Tian SM, Qian Y, Li JL, Li RZ. Diagnostic performance of contrast-enhanced sonography and acoustic radiation force impulse imaging in solid liver lesions. J Ultrasound Med 2014; 33: 205–14. doi: https://doi.org/10.7863/ultra.33.2.205 [DOI] [PubMed] [Google Scholar]
- 52.Rennert J, Georgieva M, Schreyer AG, Jung W, Ross C, Stroszczynski C, et al. Image fusion of contrast enhanced ultrasound (CEUS) with computed tomography (CT) or magnetic resonance imaging (MRI) using volume navigation for detection, characterization and planning of therapeutic interventions of liver tumors. Clin Hemorheol Microcirc 2011; 49: 67–81. doi: https://doi.org/10.3233/CH-2011-1458 [DOI] [PubMed] [Google Scholar]
- 53.Seitz K, Bernatik T, Strobel D, Blank W, Friedrich-Rust M, Strunk H, et al. Contrast-enhanced ultrasound (CEUS) for the characterization of focal liver lesions in clinical practice (DEGUM multicenter trial): CEUS vs MRI—a prospective comparison in 269 patients. Ultraschall Med 2010; 31: 492–9. doi: https://doi.org/10.1055/s-0029-1245591 [DOI] [PubMed] [Google Scholar]
- 54.Seitz K, Strobel D, Bernatik T, Blank W, Friedrich-Rust M, Herbay A, et al. Contrast-enhanced ultrasound (CEUS) for the characterization of focal liver lesions—prospective comparison in clinical practice: CEUS vs CT (DEGUM multicenter trial). Parts of this manuscript were presented at the Ultrasound Dreilandertreffen 2008, Davos. Ultraschall Med 2009; 30: 383–9. doi: https://doi.org/10.1055/s-0028-1109673 [DOI] [PubMed] [Google Scholar]
- 55.Wang ZL, Tang J, Weskott HP, Li JL, Wang W, Luo YK, et al. Undetermined focal liver lesions on gray-scale ultrasound in patients with fatty liver: characterization with contrast-enhanced ultrasound. J Gastroenterol Hepatol 2008; 23: 1511–19. doi: https://doi.org/10.1111/j.1440-1746.2008.05435.x [DOI] [PubMed] [Google Scholar]
- 56.Ungermann L, Elias P, Zizka J, Ryska P, Klzo L. Focal nodular hyperplasia: spoke-wheel arterial pattern and other signs on dynamic contrast-enhanced ultrasonography. Eur J Radiol 2007; 63: 290–4. doi: https://doi.org/10.1016/j.ejrad.2007.01.026 [DOI] [PubMed] [Google Scholar]
- 57.Soye JA, Mullan CP, Porter S, Beattie H, Barltrop AH, Nelson WM. The use of contrast-enhanced ultrasound in the characterisation of focal liver lesions. Ulster Med J 2007; 76: 22–5. [PMC free article] [PubMed] [Google Scholar]
- 58.Wu W, Chen MH, Yin SS, Yan K, Fan ZH, Yang W, et al. The role of contrast-enhanced sonography of focal liver lesions before percutaneous biopsy. AJR Am J Roentgenol 2006; 187: 752–61. doi: https://doi.org/10.2214/AJR.05.0535 [DOI] [PubMed] [Google Scholar]
- 59.Masetti R, Zama D, Gasperini P, Morello W, Prete A, Colecchia A, et al. Focal nodular hyperplasia of the liver in children after hematopoietic stem cell transplantation. Pediatr Transplant 2013; 17: 479–86. doi: https://doi.org/10.1111/petr.12091 [DOI] [PubMed] [Google Scholar]
- 60.Rennert J, Dornia C, Georgieva M, Roehrl S, Fellner C, Schleder S, et al. Identification of early complications following liver transplantation using contrast enhanced ultrasound (CEUS). First results. J Gastrointestin Liver Dis 2012; 21: 407–12. [PubMed] [Google Scholar]
- 61.Geis S, Prantl L, Dolderer J, Lamby P, Mueller S, Jung EM. Postoperative monitoring of local and free flaps with contrast-enhanced ultrasound (CEUS)—analysis of 112 patients. Ultraschall Med 2013; 34: 550–8. doi: https://doi.org/10.1055/s-0033-1355758 [DOI] [PubMed] [Google Scholar]
- 62.Riccabona M, Avni FE, Damasio MB, Ording-Muller LS, Blickman JG, Darge K, et al. ESPR uroradiology task force and ESUR paediatric working group—imaging recommendations in paediatric uroradiology, part V: childhood cystic kidney disease, childhood renal transplantation and contrast-enhanced ultrasonography in children. Pediatr Radiol 2012; 42: 1275–83. doi: https://doi.org/10.1007/s00247-012-2436-9 [DOI] [PubMed] [Google Scholar]
- 63.Di Vece F, Tombesi P, Ermili F, Sartori S. Contrast-enhanced ultrasound (CEUS) and CEUS-guided biopsy in the diagnosis of lung abscess in a patient with achalasia: case report. Interv Med Appl Sci 2013; 5: 31–3. doi: https://doi.org/10.1556/IMAS.5.2013.1.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gorg C. Transcutaneous contrast-enhanced sonography of pleural-based pulmonary lesions. Eur J Radiol 2007; 64: 213–21. [DOI] [PubMed] [Google Scholar]
- 65.Gorg C, Bert T, Gorg K. Contrast-enhanced sonography for differential diagnosis of pleurisy and focal pleural lesions of unknown cause. Chest 2005; 128: 3894–9. [DOI] [PubMed] [Google Scholar]
- 66.Lassau N, Chebil M, Chami L, Bidault S, Girard E, Roche A. Dynamic contrast-enhanced ultrasonography (DCE-US): a new tool for the early evaluation of antiangiogenic treatment. Target Oncol 2010; 5: 53–8. doi: https://doi.org/10.1007/s11523-010-0136-7 [DOI] [PubMed] [Google Scholar]
- 67.McCarville MB, Coleman JL, Guo J, Li Y, Li X, Honnoll PJ, et al. Use of quantitative dynamic contrast-enhanced ultrasound to assess response to antiangiogenic therapy in children and adolescents with solid malignancies: a pilot study. AJR Am J Roentgenol 2016; 206: 933–9. doi: https://doi.org/10.2214/AJR.15.15789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Al Bunni F, Deganello A, Sellars ME, Schulte KM, Al-Adnani M, Sidhu PS. Contrast-enhanced ultrasound (CEUS) appearances of an adrenal phaeochromocytoma in a child with Von Hippel-Lindau disease. J Ultrasound 2014; 17: 307–11. doi: https://doi.org/10.1007/s40477-014-0083-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rafailidis V, Deganello A, Sellars ME, Makin E, Sidhu PS. Pediatric adrenal trauma: evaluation and follow-up with contrast-enhanced ultrasound (CEUS). J Ultrasound 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Friedrich-Rust M, Glasemann T, Polta A, Eichler K, Holzer K, Kriener S, et al. Differentiation between benign and malignant adrenal mass using contrast-enhanced ultrasound. Ultraschall Med 2011; 32: 460–71. [DOI] [PubMed] [Google Scholar]
- 71.Harvey CJ, Alsafi A, Kuzmich S, Ngo A, Papadopoulou I, Lakhani A, et al. Role of US contrast agents in the assessment of indeterminate solid and cystic lesions in native and transplant kidneys. Radiographics 2015; 35: 1419–30. doi: https://doi.org/10.1148/rg.2015140222 [DOI] [PubMed] [Google Scholar]
- 72.Harvey CJ, Sidhu PS, Bachmann Nielsen M. Contrast-enhanced ultrasound in renal transplants: applications and future directions. Ultraschall Med 2013; 34: 319–21. doi: https://doi.org/10.1055/s-0033-1350138 [DOI] [PubMed] [Google Scholar]
- 73.Girlich C, Jung EM, Huber E, Ott C, Iesalnieks I, Schreyer A, et al. Comparison between preoperative quantitative assessment of bowel wall vascularization by contrast-enhanced ultrasound and operative macroscopic findings and results of histopathological scoring in Crohn's disease. Ultraschall Med 2011; 32: 154–9. doi: https://doi.org/10.1055/s-0029-1245398 [DOI] [PubMed] [Google Scholar]
- 74.Quaia E, De Paoli L, Stocca T, Cabibbo B, Casagrande F, Cova MA. The value of small bowel wall contrast enhancement after sulfur hexafluoride-filled microbubble injection to differentiate inflammatory from fibrotic strictures in patients with Crohn's disease. Ultrasound Med Biol 2012; 38: 1324–32. doi: https://doi.org/10.1016/j.ultrasmedbio.2012.04.008 [DOI] [PubMed] [Google Scholar]
- 75.Quaia E, Cabibbo B, De Paoli L, Toscano W, Poillucci G, Cova MA. The value of time-intensity curves obtained after microbubble contrast agent injection to discriminate responders from non-responders to anti-inflammatory medication among patients with Crohn's disease. Eur Radiol 2013; 23: 1650–9. doi: https://doi.org/10.1007/s00330-012-2754-1 [DOI] [PubMed] [Google Scholar]
- 76.Paredes JM, Ripolles T, Cortes X, Moreno N, Martinez MJ, Bustamante-Balen M, et al. Contrast-enhanced ultrasonography: usefulness in the assessment of postoperative recurrence of Crohn's disease. J Crohns Colitis 2013; 7: 192–201. doi: https://doi.org/10.1016/j.crohns.2012.03.017 [DOI] [PubMed] [Google Scholar]
- 77.Chiorean L, Schreiber-Dietrich D, Braden B, Cui XW, Buchhorn R, Chang JM, et al. Ultrasonographic imaging of inflammatory bowel disease in pediatric patients. World J Gastroenterol 2015; 21: 5231–41. doi: https://doi.org/10.3748/wjg.v21.i17.5231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Anupindi SA, Podberesky DJ, Towbin AJ, Courtier J, Gee MS, Darge K, et al. Pediatric inflammatory bowel disease: imaging issues with targeted solutions. Abdom Imaging 2015; 40: 975–92. doi: https://doi.org/10.1007/s00261-015-0423-y [DOI] [PubMed] [Google Scholar]
- 79.Madej T. 3D imaging options and ultrasound contrast agents for the ultrasound assessment of pediatric rheumatic patients. J Ultrason 2013; 13: 431–7. doi: https://doi.org/10.15557/JoU.2013.0046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Oe Y, Orr L, Laifer-Narin S, Hyodo E, Koczo A, Homma S, et al. Contrast-enhanced sonography as a novel tool for assessment of vascular malformations. J Angiogenes Res 2010; 2: 25. doi: https://doi.org/10.1186/2040-2384-2-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Patel K, Sellars ME, Clarke JL, Sidhu PS. Features of testicular epidermoid cysts on contrast-enhanced sonography and real-time tissue elastography. J Ultrasound Med 2012; 31: 115–22. [DOI] [PubMed] [Google Scholar]
- 82.Schreiber-Dietrich DG, Cui XW, Piscaglia F, Gilja OH, Dietrich CF. Contrast enhanced ultrasound in pediatric patients: a real challenge. Z Gastroenterol 2014; 52: 1178–84. doi: https://doi.org/10.1055/s-0034-1366766 [DOI] [PubMed] [Google Scholar]
- 83.Kanal E, Tweedle MF. Residual or retained gadolinium: practical implications for radiologists and our patients. Radiology 2015; 27: 630–4. doi: https://doi.org/10.1148/radiol.2015150805 [DOI] [PubMed] [Google Scholar]