Abstract
Objective:
Pancreatic cancer is a difficult to treat disease with a persistently high mortality rate. We evaluated dose distribution simulation with respiratory-gated carbon-ion pencil beam scanning (C-PBS) with a simultaneous integrated boost (SIB) to increase tumour dose, sparing organs at risk (OARs).
Methods:
Using four-dimensional CT data of 12 patients, we delineated gross tumour volume and two clinical target volumes (CTVs). To consider beam range intrafractional uncertainty, we calculated field-specific target volumes, from which two planning target volumes (PTVs) were generated. PTV1 would receive a planned dose of 55.2 Gy [relative biological effectiveness (RBE)-weighted absorbed dose] in 12 fractions, and PTV2 would receive an SIB dose up to 67.2 Gy (RBE). Dose assessments were conducted with regard to the targets and OARs.
Results:
CTV2 dose covering 95% of the volume (D95%) increased from 50.3 ± 5.1 Gy (RBE) to 62.5 ± 3.5 Gy (RBE) for a planned dose from 55.2 Gy (RBE) to 67.2 Gy (RBE). For 4 of 12 patients with a distance of ≥5 mm between the tumour and the gastrointestinal tract, CTV2 D95% was ≥95% of planned dose at all dose levels.
Conclusion:
We quantified dose escalation with respiratory-gated C-PBS using SIB for pancreatic cancer and revealed that OAR dose was not affected to the same degree as the tumour dose.
Advances in knowledge:
A simulation study on respiratory-gated C-PBS with SIB for pancreatic cancer was performed. The results indicated the feasibility of dose escalation for pancreatic cancer, which should be confirmed in clinical trials.
INTRODUCTION
Pancreatic cancer has one of the highest mortality rates of all cancers, with more than 40,000 deaths estimated for 2015 in the USA alone.1 Surgical resection is the only potentially curative treatment, but cannot be performed in many cases due to locally advanced lesions or metastasis (or both) at the time of diagnosis.2
Standard treatment for locally advanced, unresectable pancreatic cancer is chemotherapy or chemoradiotherapy.3,4 As local recurrence after radiation therapy (RT) is frequent, one strategy to improving disease control is boosting the dose to the tumour without increasing exposure to organs at risk (OARs). Techniques to accomplish this have been reported, including intensity-modulated radiation therapy (IMRT), stereotactic body radiation therapy (SBRT) and proton beam therapy (PBT).5–10 Compared with IMRT, SBRT and PBT, carbon-ion (C-ion) beams can provide a more conformal dose distribution to the target owing to their lower degree of lateral scattering, and better biological effects owing to their higher linear energy transfer.11 We have administered passive scattering C-ion RT to pancreatic cancer at our institution with gradually increasing doses up to 55.2 Gy relative biological effectiveness (RBE)-weighted absorbed dose12 in 12 fractions. Increasing doses has had a tendency to improve local control and overall survival (OS).13 In dose escalation, it appears reasonable to prioritize the primary tumour, since irradiating the planning target volume (PTV) as a whole, which includes the neural plexus region and locoregional elective lymph node area, with an escalated dose could cause damage to normal tissues.
As tumours and OARs in the thoracic and abdominal region are strongly affected by intrafractional respiratory motion14 and bowel gas,15 these factors need to be factored into treatment planning. Since 2011, our institution has implemented carbon-ion pencil beam scanning (C-PBS) treatment for tumours unaffected by intrafractional motion.16 Pancreatic tumours are challenging because they tend to move in a more complicated fashion than lung or liver tumours and are located in much closer proximity to OARs.
Our group previously reported four-dimensional C-ion boost irradiation to the primary tumour with a layer-stacking technique.17 As a new approach to increasing dose, we have developed a respiratory-gated C-PBS technique with a simultaneous integrated boost (SIB) to the tumour. In this study, we evaluated the dosimetry involved in this new SIB technique.
METHODS AND MATERIALS
Patients
12 patients with pancreatic cancer who underwent conventional passive C-ion RT at our institution were randomly selected for inclusion in this study. All patients gave informed consent to participate in the study, which was approved by the institutional review board of our institution. The patient characteristics are shown in Table 1.
Table 1.
Patient characteristics (n = 12)
| Characteristic | Value |
|---|---|
| Age (years) | |
| Median (range) | 66.5 (35–80) |
| Gender, n (%) | |
| Male | 6 (50) |
| Female | 6 (50) |
| Tumour stage (UICC 7th), n (%) | |
| T4 | 7 (58) |
| T3 | 5 (42) |
| Tumour location, n (%) | |
| Head | 6 (50) |
| Body | 6 (50) |
| GTV volume (cc) | |
| Median (range) | 10.9 (1.7–47.3) |
| Closest distance between GTV and stomach or duodenum, n (%) | |
| ≥5 mm | 4 (33) |
| <5 mm | 8 (67) |
GTV, gross tumour volume; UICC, Union for International Cancer Control.
Image acquisition
Patients underwent four-dimensional CT (4DCT) under free-breathing conditions. 4DCT images were acquired using a 320-row detector CT (Aquilion One™ Vision, Toshiba Medical Systems, Otawara, Japan), which can scan 16 cm in the axial direction in a single rotation. Respiration was monitored with a respiratory gating system (AZ-733V®, Anzai Medical, Tokyo, Japan). 4DCT data sets were subdivided into 10 phases (T00 = peak inhalation; T50 = peak exhalation), with T50 used for the reference phase.
Treatment planning
All contouring was conducted by certified radiation oncologists. Gross tumour volume (GTV) was delineated for the primary tumour. OARs including the stomach, the duodenum (D1–D2: the first and second portions, D3–D4: the third and fourth portions), the kidneys and the spinal cord were manually delineated on the T50 images for each patient. We defined two clinical target volumes (CTVs): CTV1 included the GTV plus a 5-mm margin, neural plexus region and locoregional elective lymph node area; and CTV2 included the GTV with a uniform 2-mm margin. CTVs were adjusted with respect to anatomical boundaries. A gating window was selected with a 30% duty cycle around T50 (T40 to T60), and the contours were transferred from the reference phase to the other phases using B-spline-based deformable image registration.18 To take intrafractional beam range uncertainty into account, we calculated a field-specific target volume (FTV) and delineated field-specific organs at risk (FOARs) from the 4DCT images. FTV was designed by calculating water-equivalent path length (WEPL) values at the proximal and distal edges of the target at the respective phases of respiration, and maximum and minimum WEPL values at the proximal and distal sides were selected for projection on CT images in the reference phase.19,20 FOARs were generated in the same way as FTVs.21 As a result, FTV1, FTV2 and FOARs were created for CTV1, CTV2 and the OARs, respectively. A setup margin of 2-mm WEPL was also added when the FTVs and FOARs were generated. Thus, we regarded FTVs as PTVs and generated PTV1 and PTV2 from FTV1 and FTV2, respectively.
A dose of 55.2 Gy (RBE) in 12 fractions to PTV1, and SIB dose to PTV2 was planned at up to 67.2 Gy (RBE) in 12 fractions, increasing in 2.4-Gy (RBE) steps. A single-field uniform dose plan was performed.12 In their study on dose escalation with photon or proton radiation treatment for pancreatic cancer, Bouchard et al6 reported dose fractionation of 72 Gy in 36 fractions. To compare various dose fraction sizes, biological effective dose (BED) can be calculated according to the formula:
where n is the number of fractions, d is the dose per fraction and α and β are the linear and quadratic coefficients of the linear quadratic model. We applied an α/β value of 10 Gy to biological effective dose (BED10) in this analysis. The dose used by Bouchard et al6 was converted to BED10 86.4 Gy. Krishnan et al7 reported a dose escalation for locally advanced pancreatic cancer using IMRT and patients who received BED10 ≥70 Gy had a better OS. As for SBRT, Mahadevan et al9 reported a fractionated SBRT with CyberKnife for pancreatic cancer. The overall mean prescription dose they used was 28.75 Gy (range, 24–36 Gy) in three fractions, which was converted to BED10 56.4 Gy (range, 43.2–79.2 Gy). Our planned SIB dose of 55.2–67.2 Gy (RBE) converts to BED10 80.6–104.8 Gy (RBE). Taking into account the RBE dependence on various physical and biological parameters including linear energy transfer, dose level and type of tissue,12 the planned dose used in this study was equal to or greater than that of their study based on RBE. C-PBS treatment would be administered via four beam ports (0°, 165°, 180° and 270°), with three, two, four and three fractions per beam angle, respectively. To reduce uncertainty associated with bowel gas, a beam from the left side (90°) was not used.15 Accumulated dose distribution was calculated in each gating window of T40–60 and integrated on the reference phase using deformable image registration. The dose constraints were the minimum dose received by the most exposed 2 cc volume of the organ (D2 cc) <46 Gy (RBE) for the gastrointestinal (GI) tract (the stomach and the duodenum), maximum dose to the organ (Dmax) <30 Gy (RBE) for the spinal cord and volume of organ receiving more than 30 Gy (V30) (RBE) <50% for the kidneys, respectively.
Dose assessments
Dose assessments were evaluated with regard to dose covering 95% of the volume (D95%) for GTV, CTV1 and CTV2; D2 cc of the stomach, D1–D2 and D3–D4; Dmax to the spinal cord; and volume of organ receiving more than n Gy (RBE) of the stomach, D1–D2, D3–D4 and the kidneys in the dose–volume histograms. As the tumour location can influence the dose to the tumour and OARs, we compared the differences in dosimetry between patients with a tumour in the pancreatic head and those with a tumour in the pancreatic body. These values were analyzed statistically by a t-test, with a p-value ≤0.05 considered statistically significant. The statistical analysis was performed using SPSS® v. 22 (IBM Corp., New York, NY; formerly SPSS Inc., Chicago, IL). Because the distance between the tumour and the GI tract (the stomach and the duodenum) is a source of difficulty in escalating tumour dose, we measured the closest distance between the tumour and the GI tract and analyzed the impact of distance (≥5 mm or <5 mm) on CTV2 D95%.
RESULTS
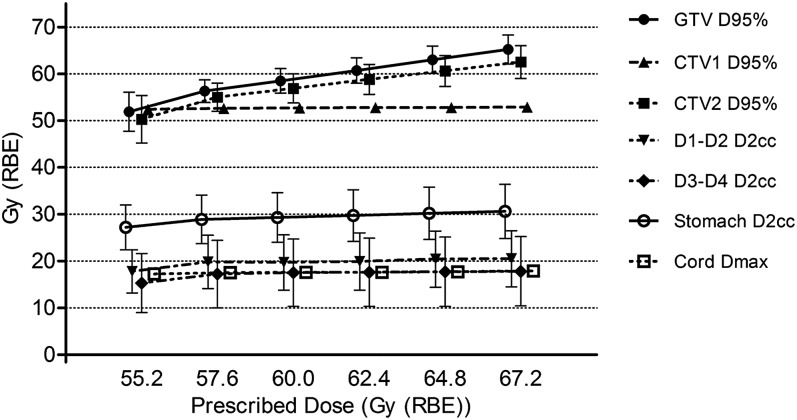
Dose assessment metrics averaged over all patients are summarized in Figure 1. Calculating mean ± standard deviation values of the dose assessment metrics averaged over all patients revealed that D95% of GTV and CTV2 increased linearly from 51.9 ± 4.2 Gy (RBE) and 50.3 ± 5.1 Gy (RBE) to 65.2 ± 3.1 Gy (RBE) and 62.5 ± 3.5 Gy (RBE), respectively, in accordance with the increase in the planned dose from 55.2 Gy (RBE) to 67.2 Gy (RBE), while D95% of CTV1 was approximately constant throughout the dose escalation with an average of 52.7 ± 0.2 Gy (RBE). We did not identify any case beyond the dose constraints for OARs. D2 cc of the stomach, D1–D2 and D3–D4 slightly changed from 27.2 ± 4.8 Gy (RBE), 17.8 ± 4.6 Gy (RBE) and 15.3 ± 6.3 Gy (RBE), respectively, at a planned dose of 55.2 Gy (RBE) to 30.6 ± 5.8 Gy (RBE), 20.5 ± 6.0 Gy (RBE) and 17.8 ± 7.4 Gy (RBE), respectively, at the planned dose of 67.2 Gy (RBE). Dmax to the spinal cord was almost constant from 17.2 ± 0.9 Gy (RBE) at the planned dose of 55.2 Gy (RBE) to 17.9 ± 0.8 Gy (RBE) at 67.2 Gy (RBE). V30 of the right and left kidneys were <1% and 2%, respectively, throughout the dose escalation. Summarizing the above, increasing the planned dose from 55.2 Gy (RBE) to 67.2 Gy (RBE), which was about 20% increase, resulted in increase in D95% of GTV and CTV2 by about the same ratio, while the dose to most OARs increased approximately by 10%.
Figure 1.
Mean dosimetry at each prescribed dose level. CTV, clinical target volume; D1–D2, first and second portions of the duodenum; D3–D4, third and fourth portions of the duodenum; GTV, gross tumour volume.
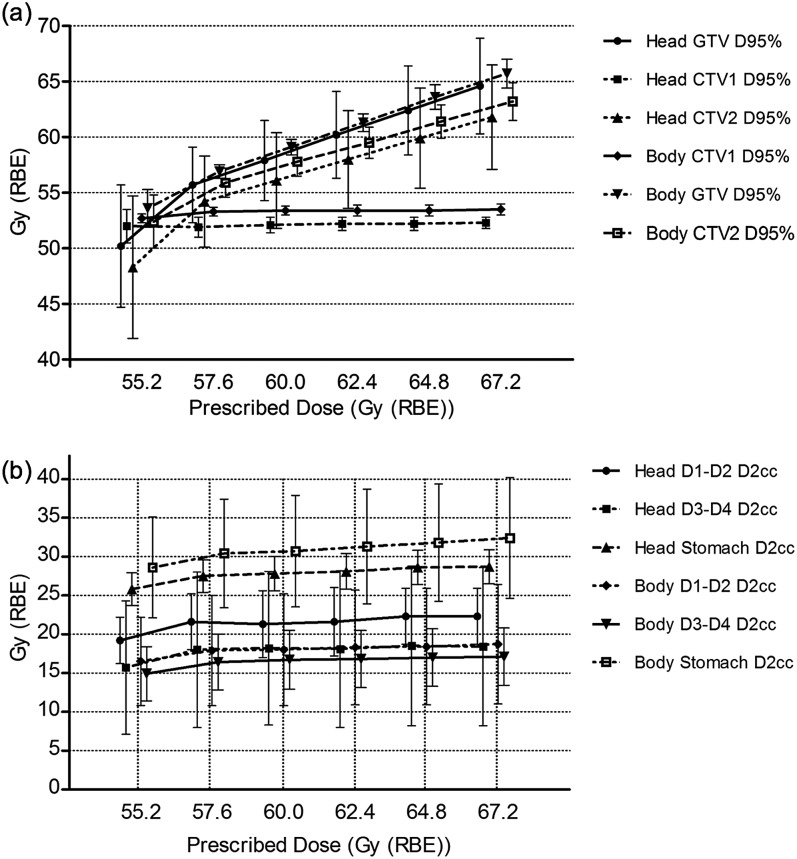
There were no significant differences in mean D95% to GTV, CTV1 and CTV2 for the patients with pancreatic body tumours compared with those with pancreatic head tumours at each prescribed dose level (p > 0.05) (Figure 2a). There were also no significant differences in mean stomach D2 cc or D2 cc of D1–D2 and D3–D4 (p > 0.05) (Figure 2b). Mean Dmax to the spinal cord and V30 of the kidneys did not show clear differences between tumour locations (p > 0.05).
Figure 2.
Dosimetry by tumour location: (a) dose covering 95% of the volume (D95%) of the gross tumour volume (GTV), clinical target volume (CTV)1 and CTV2; (b) the minimum dose received by the most exposed 2 cc volume of the organ (D2 cc) of the stomach, first and second portions of the duodenum (D1–D2) and third and fourth portions of the duodenum (D3–D4) averaged over the patients. RBE, relative biological effectiveness.
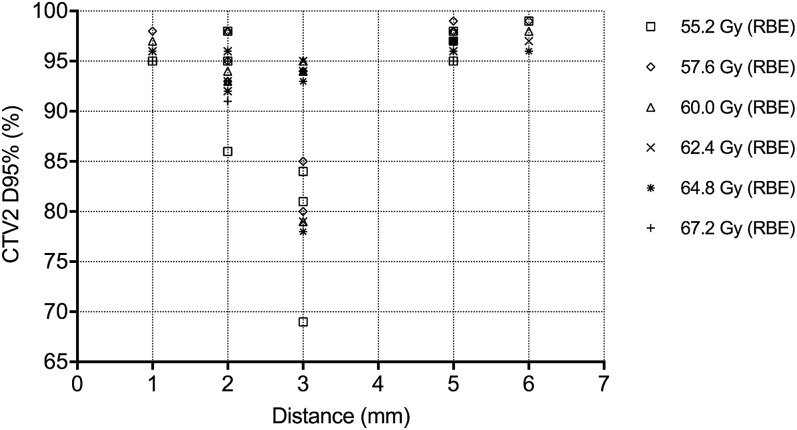
In the analysis of impact of the distance between the tumour and the GI tract on CTV2 D95%, for the four patients with a distance of ≥5 mm, 95% or more of the dose covered CTV2 D95% at all prescribed dose levels. On the other hand, for the five of eight patients with a distance of <5 mm, coverage of CTV2 D95% was <95% of the planned dose at some or all dose levels (Figure 3).
Figure 3.
Plot of clinical target volume (CTV)2 dose covering 95% of the volume (D95%) corresponding to the distance between the tumour and the digestive tract. RBE, relative biological effectiveness
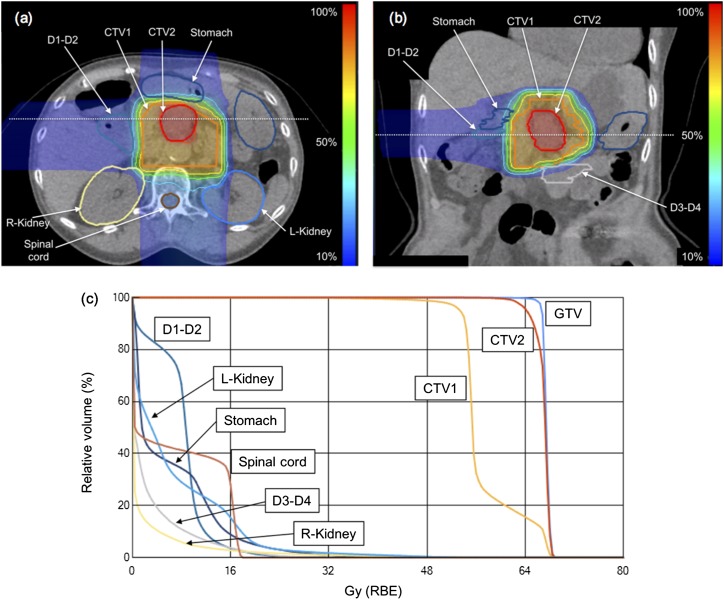
Figure 4 shows a representative case with a planned dose of 67.2 Gy (RBE). The primary tumour was located in the body of the pancreas with a volume of 19.0 cc. The distance between the tumour and the closest GI organ, the stomach in this case, was 5 mm. The D95% of GTV, CTV1 and CTV2 was higher than 95% for all patient plans, and the plans satisfied the dose constraints for all OARs. Similar results were obtained with the other planned dose levels.
Figure 4.
A representative case of respiratory-gated carbon-ion pencil beam scanning irradiation with a simultaneous integrated boost dose of 67.2 Gy [relative biological effectiveness (RBE)]: (a, b) axial and coronal images of dose distribution, respectively; and (c) a dose–volume histogram for this treatment plan. CTV, clinical target volume; GTV, gross tumour volume.
DISCUSSION
In this study, we analyzed the use of dose escalation with respiratory-gated C-PBS irradiation using the SIB technique for pancreatic cancer. The dose–volume histogram analysis averaged over the patients suggested that dose escalation with this technique would successfully deliver the planned doses to the targets while satisfying the dose constraints for OARs. The present analysis revealed that the ratio of increase in the dose to OARs remained relatively low, compared with the dose escalation to the target. Considering the result, C-PBS irradiation with the SIB technique has the potential to deliver higher doses to the target, while the dose to OARs does not increase so much.
In addition, although the conventional passive scattering C-ion irradiation technique requires separate compensator boli for both the initial and boost irradiation targets,17 C-PBS irradiation with the SIB technique can irradiate two targets, namely CTV1 and CTV2, with a dose gradient in one session, resulting in less time and work needed for implementation of treatment.
Our group previously evaluated the dose distribution of a 4DCT-generated C-ion boost irradiation plan for pancreatic cancer with the layer-stacking technique.17 Comparing the results of our present study with those of the layer-stacking technique, mean dosimetry tended to be similar with respect to GTV, CTV1 and CTV2. Doses to the GTV and CTV2 increased linearly in accordance with the prescribed dose escalation, while the dose to CTV1 was almost constant around the planned dose in both studies. Some differences in OAR dose were found, however,: doses to the stomach, D1–D2, and D3–D4 increased along with dose escalation in the layer-stacking technique, while a significant increase in the dose to these OARs was not seen with C-PBS. Dose to the spinal cord was almost constant in accordance with dose escalation in both techniques.
Recent advances in high-precision photon radiotherapy such as IMRT and SBRT offer the possibility to irradiate escalated dose to the target while reducing dose to OARs. Some dose escalation studies for pancreatic cancer using IMRT and SBRT have been reported. Krishnan et al7 reported that patients who received BED10 >70 Gy had a better OS than those who received BED10 ≤70 Gy. As for SBRT, Mahadevan et al9 reported a fractionated SBRT with CyberKnife for pancreatic cancer. The overall mean prescription dose they used was 28.75 Gy (range, 24–36 Gy) in three fractions. Although some uncertainty in the linear quadratic model for a large fraction size should be considered, BED10 for the SBRT doses they used was 56.4 Gy (range, 43.2–79.2 Gy). Another study on SBRT was conducted by Herman et al10 They irradiated with linear accelerators and prescribed 33 Gy in 5 fractions, which corresponded to BED10 54.8 Gy. The doses irradiated in the SBRT studies were relatively low, and this may have led to similar clinical outcomes with conventional chemoradiation. Here, SIB dose increased from 55.2 Gy (RBE) to 67.2 Gy (RBE), which corresponded to an increase from BED10 80.6 Gy (RBE) to 104.8 Gy (RBE). These SIB doses were comparable with or higher than those used in IMRT and SBRT studies and may improve local control and OS. However, our present study is a simulation, and its clinical outcome is still uncertain. In the future, it needs to be confirmed whether C-ion RT with higher BED10 correlates to superior local control and OS to photon RT in a clinical trial.
Bouchard et al6 compared three-dimensional photon RT, IMRT and PBT and reported that the optimal choice of RT modality for safe dose increases depended on the pancreatic tumour position in relation to OAR anatomy. Given the report by Shinoto et al that C-ion RT for pancreatic cancer under an upper GI dose constraint of D2 cc <46 Gy (RBE) decreased the risk of GI ulcer,22 tumours located in close proximity to the GI tract make it difficult to deliver the planned dose. In the present study, we found that difficulty in delivery of the boost dose with SIB was not associated with whether the tumour was located in the head or body of the pancreas. Our analysis showed that a dose increase is more likely to be accomplished if the smallest distance between the tumour and the GI tract is ≥5 mm. Similarly, Krishnan et al7 also reported that the distance between the tumour and the GI tract influenced dose escalation and that only tumours located more than 1 cm from the GI tract were selected for dose escalation IMRT.
With regard to dose constraints of the GI tract, we used D2 cc <46 Gy (RBE) in our present study, as this was the same as our daily clinical practice. To compare the dose constraint with that of photon SBRT, Herman et al10 was referenced. They described in their report a comparison of the delivered dose of 33 Gy in 5 fractions with 25 Gy in a single fraction of SBRT, which was reported by Schellenberg et al8 for unresectable pancreatic cancer. Assuming an α/β value of 3 Gy for evaluating the normal tissues, the BED3 of fractionated SBRT 33 Gy in five fractions (BED3 105.6 Gy) was lower than 25 Gy in six fraction (BED3 233.3 Gy), and they showed a decrease in late toxicities compared to Schellenberg et al. Considering this result, the dose constraint of the GI tract in our present study of D2 cc <46 Gy (RBE) in 12 fractions (BED3 104.8 Gy) was comparable with the dose delivered by Herman et al and seemed to be reasonable.
We recognize some limitations of this study. First, interfractional changes and respiratory pattern variation were not considered owing to the acquisition of data during a single respiratory cycle with 4DCT. Although Brevet et al23 recently reported treatment planning for non-small-cell lung cancer considering both intrafractional tumour motion and interfractional anatomic changes using serial 4DCT data sets, there are few such reports on treatment planning with multiple 4DCT data sets acquired on different days. We recognize that treatment planning with serial 4DCT data sets could provide more accurate information on respiratory motion; however, increasing the number of 4DCT image acquisitions would lead to an increase in patient radiation dose, and the trade-off between the possibility of more accurate treatment planning and increased radiation dose to patients must be considered. It is necessary to determine how many 4DCT data sets need to be acquired to maximize accuracy. In order to reduce respiratory pattern variation, Parkes et al24 reported that a mechanical ventilator successfully regularized patient breathing and reduced the within-patient variability of breathing in conscious, unsedated patients. At our institution, we prefer free-breathing conditions owing to patient comfort and convenience. The effect of breathing on the quality of acquired treatment planning CT images improved to a great degree with a 320-row detector CT, which had a 16-cm scan range in a single rotation.
Second, we have been using an external gating method to monitor respiration, namely a light-emitting diode marker set on the patient abdominal surface. For the amplitude-based respiratory-gated C-PBS technique used in this study, it may be necessary to implant fiducial markers in the pancreas and monitor the tumour position with X-ray fluoroscopic imaging in real time using internal gating. We have already described respiratory-gated markerless tumour tracking for lung and liver tumours.25 However, precise treatment for the pancreas probably requires fiducial markers for fluoroscopy. The feasibility of implanting fiducial markers in the pancreas and using the internal gating system before implementing dose increases requires confirmation.
Patient selection by tumour type
It has been reported that intact small mothers against decapentaplegic 4 (SMAD4) gene expression is associated with a locally dominant pattern of disease progression.26,27 A Phase II study led by NRG Oncology, namely Radiation Therapy Oncology Group 1201, was conducted between 2012 and 2016 to investigate the efficacy of intensified chemoradiotherapy for locally advanced pancreatic cancer according to SMAD4 status. Unfortunately, this study was closed prematurely owing to slow accrual, but analysis of the data obtained will still provide valuable information about identifying patients who are unlikely to develop distant metastasis, the results will also serve as a motivation for our dose increase with respiratory-gated C-PBS using the SIB technique.
CONCLUSION
Our study generated valuable information on planning dose increases using respiratory-gated C-PBS with SIB for pancreatic cancer. The feasibility and efficacy of this treatment should be confirmed and compared with photon techniques in future clinical trials.
FUNDING
This research was funded by the National Institute of Radiological Sciences.
Acknowledgments
ACKNOWLEDGMENTS
The authors would like to thank Daniel K Ebner for the English language review.
Contributor Information
Shohei Kawashiro, Email: shohei.kawashiro@gmail.com.
Shinichiro Mori, Email: mori.shinichiro@qst.go.jp.
Shigeru Yamada, Email: yamada.shigeru@qst.go.jp.
Kentaro Miki, Email: miki.kentaro@qst.go.jp.
Kenji Nemoto, Email: knemoto@ymail.plala.or.jp.
Hiroshi Tsuji, Email: tsuji.hiroshi@qst.go.jp.
Tadashi Kamada, Email: kamada.tadashi@qst.go.jp.
REFERENCES
- 1.Siegel RL, Miller KD, Jernal A. Cancer statistics, 2015. CA Cancer J Clin 2015; 65: 5–29. doi: https://doi.org/10.3322/caac.21254 [DOI] [PubMed] [Google Scholar]
- 2.Sener SF, Fremgen A, Menck HR, Winchester DP. Pancreatic cancer: a report of treatment and survival trends for 100,313 patients diagnosed from 1985–1995, using the National Cancer Database. J Am Coll Surg 1999; 189: 1–7. [DOI] [PubMed] [Google Scholar]
- 3.Crane CH, Varadhachary G, Settle SH, Fleming JB, Evans DB, Wolff RA. The integration of chemoradiation in the care of patient with localized pancreatic cancer. Cancer Radiother 2009; 13: 123–43. doi: https://doi.org/10.1016/j.canrad.2008.11.008 [DOI] [PubMed] [Google Scholar]
- 4.Ishii H, Furuse J, Boku N, Okusaka T, Ikeda M, Ohkawa S, et al. Phase II study of gemcitabine chemotherapy alone for locally advanced pancreatic carcinoma: JCOG0506. Jpn J Clin Oncol 2010; 40: 573–79. [DOI] [PubMed] [Google Scholar]
- 5.Brown MW, Ning H, Arora B, Albert PS, Poggi M, Camphausen K, et al. A dosimetric analysis of dose escalation using two intensity-modulated radiation therapy techniques in locally advanced pancreatic carcinoma. Int J Radiat Oncol Biol Phys 2006; 65: 274–83. [DOI] [PubMed] [Google Scholar]
- 6.Bouchard M, Amos RA, Briere TM, Beddar S, Crane CH. Dose escalation with proton or photon radiation treatment for pancreatic cancer. Radiother Oncol 2009; 92: 238–43. doi: https://doi.org/10.1016/j.radonc.2009.04.015 [DOI] [PubMed] [Google Scholar]
- 7.Krishnan S, Chadha AS, Suh Y, Chen HC, Rao A, Das P, et al. Focal radiation therapy dose escalation improves overall survival in locally advanced pancreatic cancer patients receiving induction chemotherapy and consolidative chemoradiation. Int J Radiat Oncol Biol Phys 2016; 94: 755–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schellenberg D, Goodman KA, Lee F, Chang S, Kuo T, Ford JM, et al. Gemcitabine chemotherapy and single-fraction stereotactic body radiotherapy for locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys 2008; 72: 678–86. [DOI] [PubMed] [Google Scholar]
- 9.Mahadevan A, Jain S, Goldstein M, Miksad R, Pleskow D, Sawhney M, et al. Stereotactic body radiotherapy and gemcitabine for locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys 2010; 78: 735–42. doi: https://doi.org/10.1016/j.ijrobp.2009.08.046 [DOI] [PubMed] [Google Scholar]
- 10.Herman JM, Chang DT, Goodman KA, Dholakia AS, Raman SP, Hacker-Prietz A, et al. Phase 2 multi-institutional trial evaluating gemcitabine and stereotactic body radiotherapy for patients with locally advanced unresectable pancreatic adenocarcinoma. Cancer 2015; 12: 1128–37. doi: https://doi.org/10.1002/cncr.29161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kanai T, Endo M, Minohara S, Miyahara N, Koyama-Ito H, Tomura H, et al. Biophysical characteristics of HIMAC clinical irradiation system for heavy-ion radiation therapy. Int J Radiat Oncol Biol Phys 1999; 44: 201–10. [DOI] [PubMed] [Google Scholar]
- 12.Inaniwa T, Kanematsu N, Matsufuji N, Kanai T, Shirai T, Noda K, et al. Reformulation of a clinical-dose system for carbon-ion radiotherapy treatment planning at the National Institute of Radiological Sciences, Japan. Phys Med Biol 2015; 60: 3271–86. doi: https://doi.org/10.1088/0031-9155/60/8/3271 [DOI] [PubMed] [Google Scholar]
- 13.Shinoto M, Yamada S, Terashima K, Yasuda S, Shioyama Y, Honda H, et al. Carbon ion radiation therapy with concurrent gemcitabine for patients with locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys 2016; 95: 498–504. [DOI] [PubMed] [Google Scholar]
- 14.Mori S, Hara R, Yanagi T, Sharp GC, Kumagai M, Asakura H, et al. Four-dimensional measurement of intrafractional respiratory motion of pancreatic tumors using a 256 multi-slice CT scanner. Radiother Oncol 2009; 92: 231–7. [DOI] [PubMed] [Google Scholar]
- 15.Kumagai M, Hara R, Mori S, Yanagi T, Asakura H, Kishimoto R, et al. Impact of intrafractional bowel gas movement on carbon ion beam dose distribution in pancreatic radiotherapy. Int J Radiat Oncol Biol Phys 2009; 73: 1276–81. doi: https://doi.org/10.1016/j.ijrobp.2008.10.055 [DOI] [PubMed] [Google Scholar]
- 16.Mori S, Shibayama K, Tanimoto K, Kumagai M, Matsuzaki Y, Furukawa T, et al. First clinical experience in carbon ion scanning beam therapy: retrospective analysis of patient positional accuracy. J Radiat Res 2012; 53: 760–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mori S, Shinoto M, Yamada S. Four-dimensional treatment planning in layer-stacking boost irradiation for carbon-ion pancreatic therapy. Radiother Oncol 2014; 111: 258–63. [DOI] [PubMed] [Google Scholar]
- 18.Shackleford JA, Kandasamy N, Sharp GC. On developing B-spline registration algorithms for multi-core processors. Phys Med Biol 2010; 55: 6329–51. doi: https://doi.org/10.1088/0031-9155/55/21/001 [DOI] [PubMed] [Google Scholar]
- 19.Knopf AC, Boye D, Lomax A, Mori S. Adequate margin definition for scanned particle therapy in the incidence of intrafractional motion. Phys Med Biol 2013; 58: 6079–94. doi: https://doi.org/10.1088/0031-9155/58/17/6079 [DOI] [PubMed] [Google Scholar]
- 20.Graeff C, Durante M, Bert C. Motion mitigation in intensity modulated particle therapy by internal target volumes covering range changes. Med Phys 2012; 39: 6004–13. doi: https://doi.org/10.1118/1.4749964 [DOI] [PubMed] [Google Scholar]
- 21.Mori S, Inaniwa T, Miki K, Shirai T, Noda K. Implementation of a target volume design function for intrafractional range variation in a particle beam treatment planning system. Br J Radiol 2014; 87: 20140233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shinoto M, Shioyama Y, Matsunobu A, Okamoto K, Suefuji H, Toyama S, et al. Dosimetric analysis of upper gastrointestinal ulcer after carbon-ion radiotherapy for pancreatic cancer. Radiother Oncol 2016; 120: 140–4. [DOI] [PubMed] [Google Scholar]
- 23.Brevet R, Richter D, Graeff C, Durante M, Bert C. Treatment parameters optimization to compensate for interfractional anatomy variability and intrafractional tumor motion. Front Oncol 2015; 5: 291. doi: https://doi.org/10.3389/fonc.2015.00291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parkes MJ, Green S, Stevens AM, Parveen S, Stephens R, Clutton-Brock TH. Reducing the within-patient variability of breathing for radiotherapy delivery in conscious, unsedated cancer patients using a mechanical ventilator. Br J Radiol 2016; 89: 20150741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mori S, Karube M, Shirai T, Tajiri M, Takekoshi T, Miki K, et al. Carbon-ion pencil beam scanning treatment with gated markerless tumor tracking: an analysis of positional accuracy. Int J Radiat Oncol Biol Phys 2016; 95: 258–66. [DOI] [PubMed] [Google Scholar]
- 26.Iacobuzio-Donahue CA, Fu B, Yachida S, Luo M, Abe H, Henderson CM, et al. DPC4 gene status of the primary carcinoma correlates with patterns of failure in patients with pancreatic cancer. J Clin Oncol 2009; 27: 1806–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crane CH, Varadhachary GR, Yordy JS, Staerkel GA, Javle MM, Safran H, et al. Phase II trial of cetuximab, gemcitabine, and oxaliplatin followed by chemoradiation with cetuximab for locally advanced (T4) pancreatic adenocarcinoma: correlation of Smad4(Dpc4) immunostaining with pattern of disease progression. J Clin Oncol 2011; 29: 3037–43. doi: https://doi.org/10.1200/JCO.2010.33.8038 [DOI] [PMC free article] [PubMed] [Google Scholar]