Abstract
Objective:
To describe a new technique to prevent skin laceration during ultrasound-guided vacuum-assisted breast biopsy with the insertion of a spinal needle between the mass and the skin.
Methods:
The study includes 118 patients with 118 breast imaging-reporting and data system Category 3 masses located very close to the skin or areola, which were excised using the mammotome system with a spinal needle inserted just above the site of insertion of the probe.
Results:
The mean distance between the most superficial portion of the mass to the under surface of the overlying skin was 1.3 ± 0.4 mm. The average procedure time was 13.5 ± 4.2 min. A complete excision was achieved in 100% of the cases, and the procedure was well tolerated by all the patients. No patient experienced serious adverse events such as a skin laceration.
Conclusion:
This is the first study to prevent skin laceration during vacuum assisted breast biopsy.
Advances in knowledge:
The method described in this study is simple, safe and well tolerated by patients.
INTRODUCTION
Probably benign breast masses are detected frequently on ultrasound examination due to the increase in ultrasound studies in young females and in the evaluation of lesions detected by breast cancer screening programmes.1 According to the American College of Radiology2 breast imaging-reporting and data system (BI-RADS), Category 3 (probably benign) on ultrasound is defined as a solid mass with an oval shape, circumscribed margin, parallel orientation and no suspicious malignant features. Follow-up is usually recommended for BI-RADS Category 3 lesions detected on ultrasound. However, depending on the ability of each radiologist, the possibility of malignancy is variable, although <2%, and vacuum-assisted breast biopsy (VABB) excision is recommended instead of a core-needle biopsy if patients want a complete excision.3 Furthermore, VABB is recommended in the following: (1) patients with a low probability of regular follow-up, (2) patients planning a pregnancy, (3) extremely restless patients, (4) patients with a lesion increasing in size during follow-up and (5) patients who have subjective symptoms or pain with BI-RADS Categories 3–4 lesions.4 VABB has become recognized in recent years as a safe, cost-effective alternative to open surgery for the removal of benign breast lesions.4–7 It can therefore be performed for diagnostic and therapeutic purposes.
Ultrasound-guided VABB is regarded as a feasible, effective, minimally invasive and safe method for the removal of benign breast lesions without the occurrence of serious complications.8,9 In lesions located very close to the skin or areola, infiltration of infiltrate anaesthetic or saline between the lesion and skin is recommended to increase the distance between them and to avoid iatrogenic injury to the skin.5,6,8 However, serious complications may occur during VABB such as skin laceration.10 To our knowledge, there is no report in the literature concerning the prevention of skin tear. The aim of the present study is to describe a procedure to prevent the risk of skin laceration using ultrasound-guided insertion of a spinal needle between the breast and skin.
METHODS
Patients' selection
Over a period of 18 months, 123 consecutive patients referred from the local breast unit with 123 breast masses located very close to the skin or areola underwent ultrasound-guided VABB for diagnostic and therapeutic purposes. Our institutional review board approved the research study, and informed consent for the procedure was obtained in the Department of Radiology just before the procedure, after explanation of the procedure itself, its potential complications and alternative therapies. Inclusion criteria were masses very close to the skin (<2.5 mm), masses of maximum diameter ≤23 mm and probably benign masses (BI-RADS 3). Excluded from the study were two patients with lesions suspected of malignancy and another three cases of probably benign lesions: one in a pregnant female and two in females with implants. Our study cohort finally included 118 females and 73 cases had a palpable mass. Of this group, 21 had multiple masses. We performed excision on the single mass with the greatest diameter.
Description of procedure
Ultrasound examinations were performed by two radiologists, with 4 and 27 years' breast imaging experience, using an Acuson S2000 ultrasound system (Siemens, Erlangen, Germany) equipped with an 18L6HD transducer. All the procedures were performed using a Mammotome® device and 10-G needles. Before the procedure, a careful breast ultrasound examination was performed to determine the puncture site and direction for the probe to avoid blood vessels on colour Doppler signals. Rigorous aseptic measures were applied. Local anaesthetic (2% mepivacaine) was injected in the probe puncture site without air bubbles in the syringe to avoid ultrasound artefacts and then further injected around the mass and along the planned pathway of the probe using a 22-G spinal needle. The spinal needle was then removed and inserted just above the probe insertion site (Figure 1) and the anaesthetic injected between the mass and the skin to increase the tissue thickness for needle passage. Usually, the spinal needle is inserted between the most superficial portion of the mass and the undersurface of the dermis, although in cases where the mass is in contact with the dermis, the needle is inserted in the skin, as can be seen in Figure 2. To increase safety and avoid skin lacerations in the case of masses located in the subareolar area (n = 14), we inserted two parallel spinal needles, a few millimetres apart just above the probe. The probe was inserted and advanced to just beneath the mass, and to remove the most superficial portion of the mass, we turned the probe obliquely or laterally until the mass was completely excised. Once the VABB was finished, the probe was removed and then the spinal needle was removed. A post-procedure ultrasound evaluation was performed to confirm complete excision (Figure 2). The biopsy site and probe trajectory were compressed for 5–10 min for bleeding control. Finally, the puncture site was covered with a dressing, and an instant cold pack applied.
Figure 1.

Photograph showing the spinal needle inserted just above the probe.
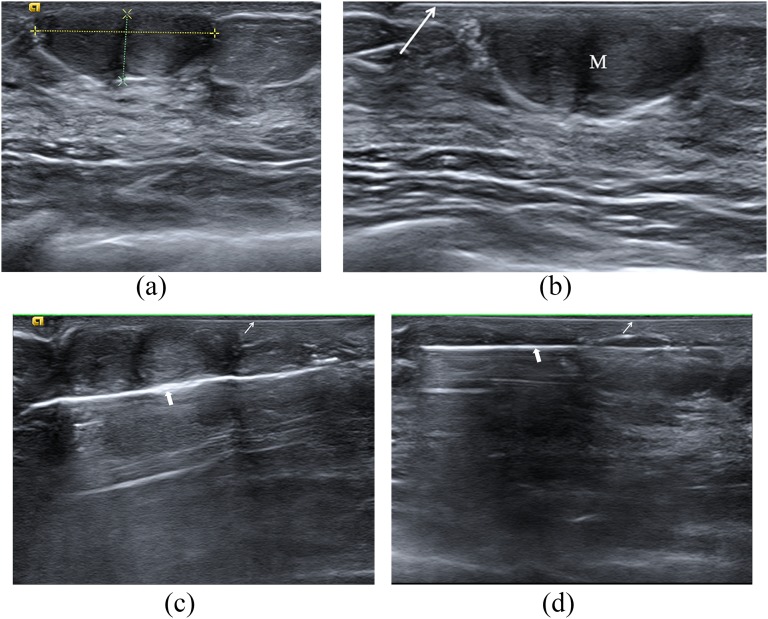
Figure 2.
A 43-year-old female with fibroadenoma. Ultrasonographic images of the mass just below the areola. (a) Mass (between callipers). (b) Insertion of the spinal needle (arrow) between the mass (M) and the areola. (c) Probe below the mass (thick arrow) and spinal needle (thin arrow). (d) Complete removal of the mass: probe (thick arrow) and spinal needle (thin arrow).
A histological examination was performed of all the specimens, and a repeat ultrasound examination was performed 1 day after the procedure.
Data collection
The information recorded for each patient includes age and ultrasound findings: distance between the most superficial portion of the nodular lesion to the under surface of the overlying skin, maximum diameter of the mass and complete mass excision. The duration of the procedure was recorded. At the end of the procedure, pain intensity was registered using a visual analogue scale of 0–10, where 0 meant no pain and 10 meant the worst possible pain. Pathological diagnoses were verified. Moreover, complications were recorded, including haematomas, ecchymosis and skin tears. A haematoma was defined as a fluid collection of >2 cm in maximum diameter at the removal sites on the ultrasound examinations performed at 24 h. The examinations were performed routinely by the same radiologist who conducted the procedure, since the visualization and evaluation of haematomas is better and more accurate than on ultrasound examination performed after VABB.
Statistical analysis
The SPSS® v. 15.0 software package for Windows® (IBM Corp., New York, NY; formerly SPSS Inc., Chicago, IL) was used for statistical analysis of the data. A descriptive statistical analysis of each variable was conducted to give the frequency of distribution. The usual parameters were also calculated for the quantitative variables: mean ± standard deviation, maximum and minimum. The Student's t-test, χ2 test and Kruskal–Wallis test were used for statistical analysis. p < 0.05 was considered statistically significant.
RESULTS
The mean age of the patients was 34.5 ± 12.7 years (range: 16–52 years). The average distance between the mass and the skin was 1.3 ± 0.4 mm (range: 0–2.4 mm), and the mean maximum diameter of the masses was 14.6 ± 5.3 mm (range: 8–23 mm).
The mean number of cores needed to achieve removal was 9.7 ± 5.6 (range: 5–18). The average duration of the procedure was 13.5 ± 4.2 min (range: 8–25 min). At no time did the probe touch the spinal needle, and no migration of the spinal needle was observed. A complete excision was achieved in 100% of the cases, and the procedure was well tolerated by all patients. The mean pain intensity registered on the visual analogue scale was 1.3 ± 0.4 (range: 0–3). Patients with larger-diameter masses were associated with increased discomfort (p = 0.02). Furthermore, younger females had a greater degree of discomfort (p = 0.009).
The histopathological examinations revealed fibroadenoma in 110 cases (93.2%) and papilloma without atypia in 8 cases (6.7%). The post-procedure complications included 9 cases of ecchymosis (7.6%) and 13 cases of haematoma (11%), which did not require treatment and resolved spontaneously. No patient experienced any serious adverse events such as a skin laceration. No significant association was observed between lesion diameter and the presence of haematoma (p = 0.64).
DISCUSSION
This study describes for the first time an innovative method to prevent skin lacerations during ultrasound-guided VABB in BI-RADS Category 3 masses very close to the skin using a spinal needle placed between the mass and skin. All the masses in our study were located very close to the skin or areola (between 0 and 2.4 mm). However, successful complete excision was achieved in all 118 masses, and none of the patients suffered skin laceration. Skin lacerations are serious adverse events of VABB that require skin closure10,11 and occur with an incidence of 0.7%.6 Our historical rate of skin laceration is 1.2%, with lacerations occurring in the region of the areola, which required closure with absorbable sutures. In lesions located very close to the skin or areola, injection of anaesthetic or saline is currently used between the lesion and skin to artificially increase the distance between them and to avoid iatrogenic injury to the skin.5,6,8 In our experience, this is not sufficient to prevent such injuries due to the rapid diffusion of liquid favoured by compression with the ultrasound probe and the artificial distance created disappears. Therefore, great care should be taken to avoid a skin laceration during the VABB technique.
The prevention of complications during VABB is a challenge. Haematoma is the most frequent complication with VABB, ranging from 8% to 27%.5,6,9 In the present study, haematoma was observed in 11% of the patients and the size of the mass did not influence haematoma formation. The most effective method for preventing haematoma at the biopsy site was considered to be application of compression by the operator. VABB is shown to be well tolerated by patients, in addition to being efficient and with relatively few complications.
Benign breast disease has a high prevalence and a substantial impact on females's quality of life.6 Ultrasound-guided VABB is a useful and efficient tool for diagnosis and treatment with complete excision of benign or probably benign breast lesions. The advantages of this minimally invasive procedure vs open surgery include comfort of the patients, few complications, low rate of residual scars and low cost.4,7–9 Excision biopsies are recommended for patients with palpable breast lesions because they cause a great deal of patient uncertainty and anxiety. Inconclusive radiological or clinical reports aggravate these conditions, and a strong family history of cancer is also an aggravating factor.12 Often, at the patient's request, the decision is made to surgically remove a lesion that looks benign on imaging.9 VABB can be a better and less expensive alternative for lesion removal in these situations. Furthermore, the use of VABB to excise benign breast lesions is another treatment option for patients with benign breast masses.9,12 However, not all BI-RADS 3 lesions need excision. We usually recommend follow-up of BI-RADS 3 lesions, since the possibility of malignancy of these lesions is <2%. However, in the present study, VABB was performed for diagnostic and therapeutic purposes when patients required excision of the lesion instead of the recommended follow-up. VABB was also performed in the following cases: anxiety or extreme restlessness at the fear of having breast cancer, palpable mass, lesion increasing in size during follow-up, family history of breast cancer, patients carrying the BRCA1 or BRCA2 gene, and dialysis patients awaiting a kidney transplant.
One limitation of this study was the small sample size. However, the breast masses in this study were located very close to the skin (1.3 ± 0.4 mm), and in no case was skin laceration observed. The present study shows, therefore, that skin tears can be prevented by inserting a spinal needle between the mass and skin. In our experience, these injuries often occur especially in masses located in the subareolar area. For this reason, we recommend the insertion of two parallel spinal needles to increase security and avoid iatrogenesis.
In conclusion, to our knowledge, a study describing a procedure to prevent skin tear during VABB, with insertion of a spinal needle between the skin and the mass, has not been reported previously. The procedure is simple, safe and well tolerated by patients. We recommend the insertion of two needles in the subareolar masses to increase the safety of the technique, as these cases carry the highest risk of skin laceration.
Acknowledgments
ACKNOWLEDGMENTS
The authors thank Bernardo Cerrato for his technical assistance.
Contributor Information
Juan de D Berná-Serna, Email: jdberna@um.es.
Florentina Guzmán-Aroca, Email: florentina.guzman@gmail.com.
Juan de D Berná-Mestre, Email: mesjubermu@hotmail.com.
Dolores Hernández-Gómez, Email: lhgomez00@hotmail.com.
REFERENCES
- 1.Lui CY, Lam HS. Review of ultrasound-guided vacuum-assisted breast biopsy: techniques and applications. J Med Ultrasound 2010; 18: 1–10. [Google Scholar]
- 2.American College of Radiology. Breast imaging reporting and data system (BI-RADS). 5th edn. Reston, VA: American College of Radiology; 2013. [Google Scholar]
- 3.Park HL, Kim LS. The current role of vacuum assisted breast biopsy system in breast disease. J Breast Cancer 2011; 14: 1–7. doi: https://doi.org/10.4048/jbc.2011.14.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baez E, Huber A, Vetter M, Hackelöer BJ. Minimal invasive complete excision of benign breast tumors using a three-dimensional ultrasound-guided mammotome vacuum device. Ultrasound Obstet Gynecol 2003; 21: 267–72. doi: https://doi.org/10.1002/uog.74 [DOI] [PubMed] [Google Scholar]
- 5.Wang ZL, Liu G, Li JL, Ding Q, Su L, Tang J, et al. Sonographically guided percutaneous excision of clinically benign breast masses. J Clin Ultrasound 2011; 39: 1–5. doi: https://doi.org/10.1002/jcu.20752 [DOI] [PubMed] [Google Scholar]
- 6.Yao F, Li J, Wan Y, Zhong Y, Wei W, Tu Y, et al. Sonographically guided vacuum-assisted breast biopsy for complete excision of presumed benign breast lesions. J Ultrasound Med 2012; 31: 1951–57. [DOI] [PubMed] [Google Scholar]
- 7.Ding B, Chen D, Li X, Zhang H, Zhao Y. Meta analysis of efficacy and safety between Mammotome vacuum-assisted breast biopsy and open excision for benign breast tumor. Gland Surg 2013; 2: 69–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krainick-Strobel U, Huber B, Majer I, Bergmann A, Gall C, Gruber I, et al. Complete extirpation of benign breast lesions with an ultrasound-guided vacuum biopsy system. Ultrasound Obstet Gynecol 2007; 29: 342–6. [DOI] [PubMed] [Google Scholar]
- 9.Jiang Y, Lan H, Ye Q, Jin K, Zhu M, Hu X, et al. Mammotome® biopsy system for the resection of breast lesions: clinical experience in two high-volume teaching hospitals. Exp Ther Med 2013; 6: 759–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fine RE, Boyd BA, Whitworth PW, Kim JA, Harness JK, Burak WE. Percutaneous removal of benign breast masses using a vacuum-assisted hand-held device with ultrasound guidance. Am J Surg 2002; 184: 332–36. [DOI] [PubMed] [Google Scholar]
- 11.Parker SH, Klaus AJ, McWey PJ, Schilling KJ, Cupples TE, Duchesne N, et al. Sonographically guided directional vacuum-assisted breast biopsy using a handheld device. AJR Am J Roentgenol 2001; 177: 405–8. doi: https://doi.org/10.2214/ajr.177.2.1770405 [DOI] [PubMed] [Google Scholar]
- 12.Park HL, Hong J. Vacuum-assisted breast biopsy for breast cancer. Gland Surg 2014; 3: 120–27. doi: https://doi.org/10.3978/j.issn.2227-684X.2014.02.03 [DOI] [PMC free article] [PubMed] [Google Scholar]