Abstract
A large body of research has been dedicated to the effects of gastrointestinal peptides on vagal afferent fibres, yet multiple lines of evidence indicate that gastrointestinal peptides also modulate brainstem vagal neurocircuitry, and that this modulation has a fundamental role in the physiology and pathophysiology of the upper gastrointestinal tract. In fact, brainstem vagovagal neurocircuits comprise highly plastic neurons and synapses connecting afferent vagal fibres, second order neurons of the nucleus tractus solitarius (NTS), and efferent fibres originating in the dorsal motor nucleus of the vagus (DMV). Neuronal communication between the NTS and DMV is regulated by the presence of a variety of inputs, both from within the brainstem itself as well as from higher centres, which utilize an array of neurotransmitters and neuromodulators. Because of the circumventricular nature of these brainstem areas, circulating hormones can also modulate the vagal output to the upper gastrointestinal tract. This Review summarizes the organization and function of vagovagal reflex control of the upper gastrointestinal tract, presents data on the plasticity within these neurocircuits after stress, and discusses the gastrointestinal dysfunctions observed in Parkinson disease as examples of physiological adjustment and maladaptation of these reflexes.
A rich body of literature spanning the past few decades describes the intrinsic neural circuits of the myenteric and submucosal plexuses as well as the interstitial cells of Cajal (ICCs), and the role these structures have in confer ring the gastrointestinal tract with substantial autonomy over physiological functions including motility, secretion and absorption1–3. Extrinsic neural inputs originating in the central nervous system (CNS) provide fine modulation of these functions, especially in the upper gastrointestinal tract. In particular, brainstem vagovagal parasympathetic neurocircuits have the most prominent role in the CNS-mediated control of upper gastrointestinal tract motility; the lower third of the oesophagus and stomach are heavily dependent on extrinsic neural pathways originating in the CNS3–5.
Historically, vagovagal neurocircuits and reflexes were believed to be ‘static’ in their contribution to the control of gastrointestinal functions, whereby sensory signals conveyed from the gut to the brainstem generate a motor response that is relayed back to the gut in a reflexive manner (that is, the synaptic signal is not modulated by input from other neurocircuits). However, this viewpoint has changed in the past few years and the plasticity and integrative capacities of these neurocircuits are now recognized in both physiological and pathological states5–8. The importance of vagal reflexes is also highlighted by observations that increased vagal tone is linked with higher resilience and adaptation to stress, whereas low vagal tone reflects vulnerability to pathological states9–11.
Vagovagal neurocircuits
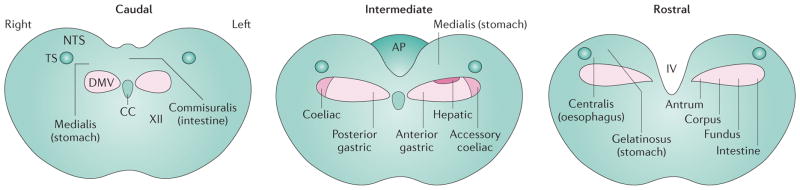
Vagovagal neurocircuits comprise specific nuclei, all of which are located within the caudal brainstem: the nucleus tractus solitarius (NTS), the dorsal motor nucleus of the vagus (DMV) and the nucleus ambiguus (FIG. 1). NTS neurons receive visceral sensory information, whereas the DMV and the nucleus ambiguus are the nuclei of origin of vagal motor fibres. The efferent fibres from the nucleus ambiguus and the DMV form synaptic contacts with postganglionic neurons located in the target organ and, ultimately, modulate gastric motility as well as other visceral functions.
Figure 1. Anatomical organization of the nucleus tractus solitarius and the dorsal motor nucleus of the vagus.
Coronal sections of the brainstem at caudal (caudal to area postrema), intermediate (at the level of the area postrema) and rostral (rostral to area postrema) levels. Brainstem areas lateral and ventral to the dorsal vagal complex (DVC) have not been represented. The location of the rostrocaudal columns representing areas of origin of the vagal branches within the dorsal motor nucleus of the vagus (DMV, pink areas) are shown in the intermediate coronal section, and the projections of rostrocaudal groups of motor neurons are shown in the rostral coronal section. The nucleus tractus solitarius (NTS) subnuclei and their main gastrointestinal-related inputs are shown in their approximate rostrocaudal locations. AP, area postrema; cc, central canal; IV, fourth ventricle; TS, tractus solitarius; XII, nucleus of the hypoglossus.
NTS
Second-order neurons of the NTS comprise neurochemically and biophysically distinct neurons that receive sensory information conveyed by vagal, aortic depressor and glossopharyngeal nerves from the subdiaphragmatic gastrointestinal viscera, as well as from gustatory, oesophageal and cardiorespiratory areas4,12–14. Several types of vagal afferent fibres carry a large volume of mechanical, chemical or osmotic information from the viscera to the NTS, where it undergoes integration with brainstem, limbic and hypothalamic signals and, ultimately, provides appropriate coordination of gastric reflexes, motility and emptying15,16. Independently of the type of sensory information relayed to the CNS, afferent vagal fibres use glutamate as their main neurotransmitter, which activates ionotropic and metabotropic receptors5,12,13. However, the NTS subnucleus receiving the afferent input varies according to the visceral source. For example, the NTS centralis subnucleus receives information exclusively related to the oesophagus, whereas subsets of neurons of the NTS medialis receive information from the stomach as well as from the aortic depressor nerve. The NTS intermedialis and interstitialis sub nuclei receive sensory information from both the larynx and pharynx, and neurons of the rostral NTS integrate taste-related signals. The separate sub nuclei within the NTS are therefore more easily identified by the origin of the visceral inputs than the morpho logical, neurochemical or biophysical characteristics of the NTS neuron itself12,14,17–21. Although subgroups of neurons have defined neurochemical phenotypes, these neurons are not located in defined NTS subnuclei nor are they linked to specific visceral organs18,22–25.
NTS neurons are of medium size (10–15 μm diameter) and contain a large array of receptors and neurotransmitters, including fast neurotransmitters such as γ-aminobutyric acid (GABA), glutamate, catecholamines and glycine, as well as a vast range of neuropeptides such as somatostatin, glucagon-like peptide 1 (GLP-1) and enkephalins, which have fundamental roles in the modulation of neuronal activity5,23,26–28. The majority of NTS neurons do not fire action potentials spontaneously, and are instead activated by synaptic activity originating from vagal afferent inputs and circulating hormones that reach the circumventricular areas of the NTS12,29,30 or by inputs from other brainstem areas or higher nuclei, such as the paraventricular nucleus (PVN) of the hypothalamus or the medullary raphe nuclei5. NTS neurons integrate this information and send axonal projections to adjacent motor nuclei, such as the DMV (involved in the fine modulation of gastric motility) or the caudal ventrolateral medulla (involved in baroreceptor neurocircuits), as well as more distant higher CNS centres, such as the hypothalamus (involved in homeostasis)5,31–33.
Nucleus ambiguus
Neurons of the nucleus ambiguus provide the parasympathetic innervation of the pharynx and larynx—and the lower third of the oesophagus in species in which this organ is composed of striated muscle, such as the rat13,34. As in the NTS, nucleus ambiguus neurons are organized in a viscerotopic manner, whereby neurons innervating the oesophagus are located in the rostral compact formation, whereas neurons innervating the pharynx and the larynx are located in the intermediate and caudal semi-compact portions of the nucleus, respectively13. In rodents, nucleus ambiguus neurons have no direct projections to the stomach and do not seem to play a prominent part in the control of upper gastrointestinal and gastric motility; we refer the reader to more specialized reviews on motor control of the oesophagus13,35.
DMV
In humans, cats, rabbits and ferrets, in which the lower oesophagus is composed of smooth muscle, the DMV encompasses the preganglionic parasympathetic neurons that provide the vagal motor output to the gastro intestinal tract, from the lower oesophagus to the transverse colon36 (FIG. 1). DMV neurons are organized in rostrocaudal spanning columns, which represent the five subdiaphragmatic branches of the vagus nerve: the anterior gastric, hepatic and accessory coeliac branches originate from neurons of the left DMV, whereas the posterior gastric and the coeliac branches originate from neurons of the right DMV37,38. In humans, the DMV comprises nine subnuclei with six different neuronal groups that can be distinguished based on their cytoarchitectural and chemoarchitectural features39. In rats and mice, DMV neurons do not seem to be segregated into distinguishable subnuclei, although in rats DMV neurons can be differentiated based on a combination of their morphological and biophysical features40–42, which seem to be related to the organs they project to rather than the function they control40,43.
A distinguishing feature of DMV neurons is their slow, spontaneous intrinsic pacemaking activity44, a corollary of which is that major changes in vagal motor output to the stomach can be obtained by synaptically driven changes in the membrane potential of DMV neurons of only a few millivolts45. The synaptic inputs to DMV neurons that are most relevant to the modulation of vagovagal reflexes originate in the NTS44. Of these synapses, GABAergic projections seem to have the most important role in the control of DMV neuronal action potential firing rate and hence regulation of vagal efferent output that controls gastric tone and motility45,46. Indeed, blockade of GABAergic transmission between the NTS and DMV by the GABAA antagonist bicuculline increases the firing rate of most DMV neurons45 and increases gastric motility and tone46.
The size of DMV neurons seems similar across species (~20–25 μm in diameter)39–41,43 and their membranes contain a vast assortment of receptors that are activated by diverse ligands. These ligands include circulating hormones such as cholecystokinin (CCK) or GLP-1 (discussed later) and neurotransmitters released by synaptic projections arising from adjacent structures, such as the NTS17,44, the area postrema47 and the medullary raphe nuclei48, as well as by projections from higher centres such as the PVN of the hypothalamus5.
The vast majority of DMV neurons are cholinergic18,49 and release acetylcholine onto nicotinic receptors located on the postganglionic neurons within the organ of interest50. Other neurotransmitter-synthesizing enzymes are also found within the DMV, including nitric oxide synthase and tyrosine 3-monooxygenase (also known as tyrosine 3-hydroxylase). Both of these enzymes are found in the medial–caudal or the rostrolateral areas of the DMV, areas that purportedly send inhibitory projections to the stomach; the role of brainstem nitrergic or catecholaminergic DMV neurons in the control of gastric motility, however, is still unclear18,49,51,52.
Gastric vagal efferent fibres contact nearly all postganglionic neurons within the ganglionated myenteric plexus of the rat stomach and proximal duodenum36. The number of neuronal contacts and thereby the influence of the efferent vagus on gastrointestinal motor and secretory functions declines dramatically in the aboral direction, such that a direct vagal influence seems absent in structures distal to the splenic flexure4,36. Postganglionic neurons of the myenteric plexus are embedded between the longitudinal and circular smooth muscle of the gastrointestinal tract, and form two distinct effector pathways that influence gastrointestinal motility: a tonic excitatory pathway that uses acetylcholine to induce muscarinicreceptor-mediated contraction of the smooth muscle; and a nonadrenergic noncholinergic (NANC) inhibitory pathway that, upon stimulation, induces smooth muscle relaxation via release of vasoactive intestinal poly peptide (VIP) or nitric oxide4,53. Notably, the postganglionic cholin ergic pathway seems to have a major role in setting the level of basal gastric tone and motility. Systemic administration of the muscarinic receptor antagonist atropine markedly reduces both gastric tone and motility4. Conversely, systemic administration of nitric oxide synthase or VIP inhibitors has minimal effect on gastric tone and motility4, suggesting the NANC inhibitory pathway is not active tonically.
Neuroanatomy of vagovagal reflexes
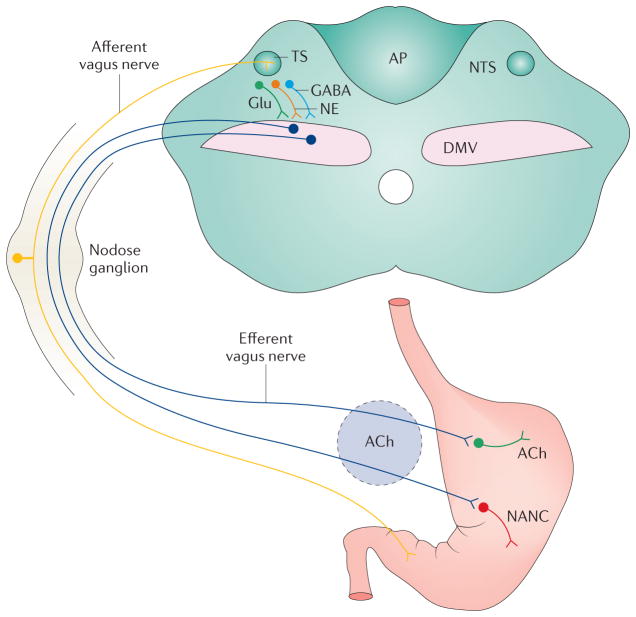
The proper pattern of gastric contractile activity is determined by the complex interplay between the enteric nervous system (ENS), ICCs, smooth muscle cells and their vagal inputs. Although there are many types of vagovagal reflexes, including oesophagogastric (receptive relaxation), gastrogastric (accommodation) and duodenogastric (duodenal brake) reflexes, they share common features, notably the activation of mechanoceptors and/or chemoreceptors within the walls of the gastrointestinal tract, followed by feedback regulation of gastric compliance, motility and emptying. Although the fine details of the neurocircuitry underlying these reflexes remains elusive, it probably involves a sensory–motor loop that comprises the NTS and the DMV, which together with the area postrema make up the brainstem vagal structures of the dorsal vagal complex (DVC) (FIG. 2).
Figure 2. The brainstem neurocircuit comprising vagovagal reflexes.
Vagal afferent fibres relay sensory information from the upper gastrointestinal tract, entering the CNS via the TS and transmitting sensory information to neurons of the NTS using glutamate as their main neurotransmitter5,13. The NTS neurons integrate this visceral sensory information, which is then conveyed to higher centres, such as the PVN, as well to the adjacent neurons of the DMV. Although a large array of neurotransmitters are used by NTS neurons, the main neurotransmitters are GABA, Glu and NE. Of these neurotransmitters, GABA seems to play a major part in controlling DMV neuronal firing rate and, by consequence, regulates vagal efferent outflow and modulation of gastric tone and motility45,46. Preganglionic parasympathetic neurons of the DMV use ACh, which interacts with nicotinic receptors, to excite postganglionic myenteric neurons and/or interstitial cells of Cajal. Vagal motor activation can induce both excitatory and inhibitory effects via stimulation of postganglionic neurons, which either release ACh onto excitatory muscarinic receptors or release inhibitory NANC neurotransmitters such as nitric oxide or vasoactive intestinal polypeptide onto gastric smooth muscles. Notably, NANC neurotransmission has an effect on gastric tone and motility, but not secretion. Ach, acetylcholine; AP, area postrema; DMV, dorsal motor nucleus of the vagus; GABA, γ-aminobutyric acid; Glu, glutamate; NANC, non-adrenergic non-cholinergic; NE, noradrenaline; NTS, nucleus tractus solitaries; PVN, paraventricular nucleus of the hypothalamus; TS, tractus solitarius.
The receptive relaxation reflex
One of the brainstem vagovagal neurocircuits that has provided a wealth of neurophysiological information in the past few years is the oesophagogastric or receptive relaxation reflex (RRR), first described by Walter Cannon in seminal manuscripts at the beginning of the 20th century54,55. The RRR is triggered by distention of the distal oesophagus and induces an increase in gastric compliance (that is, a reduction of gastric tone), thereby allowing the bolus of ingested material to enter the gastric fundus with, under physiological conditions, a minimal increase in intragastric pressure. The RRR has been modelled experimentally; for example, inflation of a latex balloon inserted into the lower oesophagus decreases fundic motility and tone56. Neurophysiological and anatomical studies have shown that the initial stimulation of low threshold mechanoreceptive vagal sensory oesophageal afferents activates catecholaminergic neurons of the NTS centralis which, in turn, excite preganglionic neurons of the DMV, resulting in the activation of inhibitory NANC vagal efferent projections and gastric relaxation via release of nitric oxide. At the same time, a distinct and separate subgroup of DMV neurons is inhibited by oesophageal inflation; inhibition of these preganglionic vagal neurons of the DMV probably induces reduced activity in the tonically active excitatory cholinergic, muscarinic efferent motor pathways. The result obtained upon oeso phageal distention is the vagally mediated gastric relaxation characteristic of the RRR4,56–58.
The RRR is probably altered in pathological conditions; for example, alterations of vagal sensory–motor functions are found in many patients with functional dyspepsia and underlie the presence of symptoms such as early satiety, impaired gastric emptying and reduced gastric compliance59–62. However, the mechanism(s) responsible for these pathophysiological alterations in vagal neurocircuitry are unclear and in dire need of further investigation in animal models. One such investigation using an animal model was described a few years ago in a study by Liu et al.63. Neonatal rat pups were gavaged for 6 days with a mild irritant (0.1% iodoacetamide); 8–10 weeks later, gastric motor function and behavioural, visceromotor and nerve fibre responses follow ing gastric balloon distention were investigated. This model demonstrated that early gastric irritation induced delayed hypersensitivity and gastric motor dysfunction similar to observations in patients with functional dyspepsia. Surprisingly, given the paucity of alternative models, this animal model has not been investigated further and experimental progress on the mechanistic understanding of functional dyspepsia in rodents has not continued as expected.
One immediate implication that can be derived from the neurophysiological organization of vagovagal reflexes is that the stomach, even at rest, is the recipient of a vagal motor outflow that is continuously sculpted by either sensory vagal, descending CNS or humoral afferent inputs. This postulate infers that a large degree of adaptive plasticity is required to ensure that vagally mediated gastrointestinal reflexive functions respond appropriately to both intrinsic and external factors.
Modulation of neurotransmitter release
As mentioned previously, vagal afferent fibres use fast synaptic transmission by ionotropic glutamate receptors to relay sensory signals to NTS neurons. In addition, these vagal afferent fibres probably also project onto the dendrites of DMV neurons that extend into the NTS gelatinosus64, although the neurotransmitter used has not yet been identified. Concomitant to the activation of ionotropic receptors, glutamate released from vagal afferent fibres also activates metabotropic glutamate receptors (mGluRs), which produce long-lasting effects on the excitability of vagal afferent fibres and synaptic transmission to NTS and DMV neurons7,65–70. Of particu lar importance for the vagally mediated modu lation of gastric motility is the ongoing activation of group II and III mGluRs, which inhibit adenylate cyclase and consequently inhibit GABAergic synaptic transmission selectively71,72.
Levels of cAMP in the brainstem neurocircuits comprising GABA synapses between the NTS and DMV are also important modulators of neurotransmitter release within brainstem vagal nerve terminals, and under certain circumstances such as stress or following food ingestion (discussed later), cAMP can control the release of neurotransmitters or the insertion of receptors into the neuronal membrane5. Several studies have shown that the interplay between vagal afferent fibres, mGluRs and cAMP levels within the DVC has the ability to modulate GABAergic synaptic trans mission between the NTS and the DMV. In vitro experi ments have shown that vagal afferent fibres provide tonic activation of group II mGluRs68,73; overcoming the effects of group II mGluR activation and increasing levels of cAMP within the DVC can be achieved by surgical removal of vagal afferent fibres, pharmacological blockade of group II mGluRs or by direct activation of adenylyl cyclase68,73–76. Interestingly, levels of cAMP within the DVC are modulated not only by vagal afferent fibre activity or mGluR activation but also by neurohormones released from adjacent CNS structures, such as thyrotropin releasing hormone (TRH) or the stress-related hormone corticotropin-releasing factor (CRF, BOX 1)5, and/or by circulating gastrointestinal peptides, such as CCK or GLP-1, that reach DVC neurons either through the surround ing leaky blood–brain barrier or via specialized transporters and ultimately activate adenylyl cyclase77–81.
Box 1. Corticotropin-releasing factor as a mediator of stress.
The effect of stress on the function of visceral organs is well recognized, as is the pivotal role that corticotropin-releasing factor (CRF) plays in a large number of stress-related disorders155,219,220. CRF and urocortins (urocortin 1 and 3) are members of the CRF family that activate two distinct receptors: corticotropin-releasing factor receptor (CRFR)1 and CRFR2. These receptors are part of the seven-transmembrane domain G protein receptor family, share a high level of homology with each other, undergo a high level of alternative splicing and stimulate adenylyl cyclase activity. CRF and urocortin 1 have a high affinity for CRFR1, whereas CRFR2 has a high affinity for urocortin 1, 2 and 3 but a lower affinity for CRF itself.
In experimental conditions, injections of CRF in the lateral ventricles, cisterna magna, the paraventricular nucleus of the hypothalamus (PVN) or the dorsal vagal complex (DVC) mimic stereotypical stressor behaviour, including slowed gastric and small intestinal motility but accelerated colonic motility155,179. These responses are consistent with the localization of CRF-immunoreactive neurons in the PVN and Barrington nuclei projecting to the DVC and spinal cord221,222. The importance of CRF signalling is further emphasized by the observations that CRF levels are upregulated in acute and repetitive heterotypic (variable) stress165,166, and both CRF-induced and stress-related gastric effects are blocked by pretreatment with selective CRFR2 receptor antagonists156,179. Interestingly, CRF does not seem to have a role in controlling basal gastrointestinal tone and motility as CRFR antagonists do not modulate gastrointestinal functions in non-stressed animals, suggesting that the effects of CRF are restricted to central modulation of gastrointestinal functions in time of stress only223,224.
The functional consequence of increased cAMP levels in the NTS–DMV synapse is the trafficking of G protein-coupled receptors and exposure of the modulation of GABAergic currents by neurotransmitters, such as serotonin82, opioids83 or neuropeptide Y84, which otherwise do not modulate GABAergic synaptic transmission82,85,86. As a result, vagal afferent fibres, via activation of mGluRs, modulate the levels of cAMP within the GABAergic NTS–DMV synapse, thereby providing a metabolically inexpensive means by which brainstem neurocircuits can adapt and provide appropriate responses to nutritional, environmental and/or pathophysiological conditions originating in the gastrointestinal tract. For example, the interdigestive period (phase III of the migrating motor complex) necessitates dampening the influence of the vagus nerve and a potential, albeit speculative, means by which this goal could be achieved is via the tonic release of low levels of glutamate in the NTS. By activating group II mGluRs, this process would reduce cAMP levels and maintain the vagovagal neurocircuitry in a resting state, preventing the modulation of GABAergic currents by circulating neuroactive substances. Conversely, following the release of neurohormones after food ingestion, the resulting increase in cAMP levels within the DVC would enable activation and modulation of vagal neurocircuits and prime the upper gastrointestinal tract for proper digestive processes. However, in pathophysiological conditions such as functional dyspepsia, inappro priate activation of vagal inputs could result in elevated cAMP levels that might enable an increased state of activation of GABAergic synaptic transmission, which could consequently affect vagal efferent outflow and hence gastric motility and tone. The experimental testing of this possible arrangement could be conducted using the Liu et al.63 model of functional dyspepsia described previously.
Gastrointestinal peptides
A large number of neuroactive peptides are released from specialized intestinal cells following ingestion of nutrients; several of these gastrointestinal peptides induce physiological, vagally mediated alterations in gastric motility, promote pancreatic secretions, and/or modulate satiety87–90. Overall, the role of gastro intestinal peptides is to modulate the gastrointestinal reaction, whether motility or secretion, to produce an appropriate response to ingested substances.
For some of these gastrointestinal peptides, the site and mechanism of action is controversial. In fact, on the basis of data from capsaicin administration experiments, many studies have proposed that the vagally mediated effects of peptides such as CCK (which is used as the main example of a neuroactive gastrointestinal peptide from here onwards), GLP-1 or ghrelin occur almost exclusively via a paracrine action on the peripheral endings of capsaicin-sensitive vagal C-type afferent fibres87,88,91–95. The postulate for this almost exclusively paracrine effect of CCK on C-type vagal afferent fibres stems from the belief that administration of cap saicin, either systemically (15–50 mg/kg bodyweight) or directly onto the vagus nerve (1% perivagal capsaicin, 33 mmol/l88,96–99), induces selective ablation of only C-type fibres. With this presumption in mind, abolition of the effects of CCK on gastric or pancreatic functions by capsaicin pretreatment was assumed as proof of a paracrine site of action88,96–104.
A large body of evidence (summarized later) indicates that capsaicin is not selective for vagal afferent fibres at the concentration or doses used in these studies, suggesting that caution should be used in the interpretation of the resulting data. Despite this evidence, the use of systemic or perivagal capsaicin for the assessment of a vagal afferent fibre-mediated mechanism of action has been de facto accepted, while toxicological, anatomical, functional and electrophysiological evidence of capsaicin and CCK-mediated alterations of visceral function via action at sites other than vagal afferent fibres has been downplayed or dismissed. The off-target effects of perivagal capsaicin application might be even more troubling than its systemic administration; the efferent (motor) vagus nerve comprises less than 15–20% of the total vagal fibres, hence even minor capsaicin-induced damage has a major effect on the vagal motor output105.
Anatomical and toxicological experiments have shown that systemic capsaicin administration induces mitochondrial and perikarya degeneration, thereby suggesting nonspecific actions of capsaicin in many areas: nonsensory regions, such as mesencephalic dopaminergic neurons; brainstem and pontine nuclei; hypothalamic areas including the anterior preoptic area; as well as nuclei that do not contain vanilloid receptors106–112. Functional experiments have shown that systemic or perivagal capsaicin administration reduces the vagally mediated gastric secretion response induced by 2-deoxy-d-glucose treatment113 or by intracisternal administration of TRH analogues114. Likewise, selective vagal deafferentation or perivagal capsaicin treatment does not prevent the DVC-mediated effects of CCK or its segretagogue, casein, on either c-Fos activation or pancreatic secretion115–118. A physiological study published in 2013 also demonstrated that perivagal capsaicin administration induces degeneration of DMV neurons, reduces their membrane response and diminishes the increase in gastric tone and motility induced in response to central activation of vagal efferent motor neurons by TRH105. Finally, electrophysiological studies have shown excitatory effects of CCK on nodose or brainstem vagal neurons119–126; similar excitatory actions are also reported as a consequence of capsaicin administration127–129.
Although the presence of CCK receptors on vagal afferent fibres and the contribution of paracrine actions of CCK on peripheral vagal terminals of C-fibres is not disputed, it should be borne in mind that, as discussed previously, there are major drawbacks with capsaicin as a tool to determine the mechanism of action of vagally dependent gastrointestinal neurohormones such as CCK. Other sites of CCK action, including vagal neurons of the nodose ganglia, NTS and DMV, should be considered.
In this regard, it is important to remember that large areas of the DVC, as well as the whole adjacent area postrema, are located outside the blood–brain barrier, have a large network of fenestrated capillaries and contact specialized neurons lining the ependymal layer of the central canal and fourth ventricle29,78,79,130. This anatomi cal arrangement, combined with the non-selective toxicity of capsaicin, suggests strongly that the mechanism(s) of action of CCK, as well as that of many other gastrointestinal peptides, is not exclusively para crine and involves other areas, including neurons of the DVC, where CCK receptors and CCK-containing neurons are also located22,131,132.
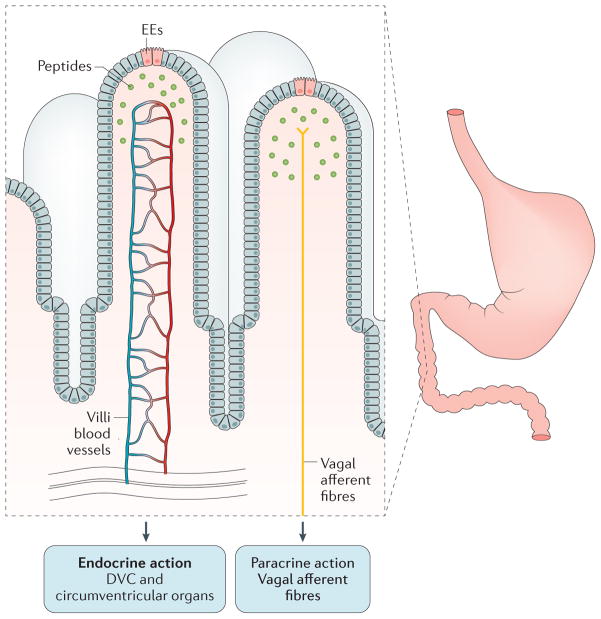
The data provide strong support for circulating CCK exerting effects through both paracrine and non-paracrine mechanisms of action (FIG. 3). A hormonal effect of CCK on DVC neurons is probable; in rats, brainstem microinjections of CCK8s decrease gastric tone and motility, reduce the gastric response to oesophageal distention (the RRR)133 and increase pancreatic exocrine secretion118. Underestimating the potentially adverse effects of capsaicin on vagal efferent function would, therefore, lead to overestimation of the vagal afferent contribution to the actions of CCK and other gastrointestinal neuropeptides.
Figure 3. Neurocircuits activated by gastrointestinal peptides.
The vagus nerve has a major role in the feedback control of gastric motility. After ingestion of nutrients, specialized enteroendocrine cells within the small intestine release gastrointestinal peptides, which, in most cases, induce a robust gastroinhibition (that is, feedback control). In the past few years, studies have shown that the mechanism of action of many of these peptides involves hormonal as well as paracrine effects. The hormonal activity of these peptides is facilitated by the close proximity of these specialized cells to the villi vasculature. Gastrointestinal hormones can therefore act at sites other than vagal afferent fibres, including the portions of the dorsal vagal complex (DVC) and the hypothalamus that lie outside the blood–brain barrier. DVC, dorsal vagal complex; EEs, enteroendocrine cells.
Indeed, other peptides such as GLP-1 and ghrelin are also released from specialized enteroendocrine cells in the gastrointestinal tract and supposedly influence gastrointestinal functions via a paracrine action on capsaicin-sensitive vagal afferent fibres91,92,134,135 (FIG. 3). However, as described previously for CCK, a large body of evidence demonstrates that these peptides also affect neurons in the nodose ganglia, NTS, DMV or area postrema to regulate neural excitability, exocrine pancreatic secretion or gastric motility136–142.
Peptide YY (PYY) is released from enteroendocrine L-cells in the distal small intestine and proximal colon143,144. These cells colocalize with GLP-1 and α-gustducin145 and are probably chemosensors. PYY is released in response to lipid ingestion as part of the ileal brake reflex mechanism; because PYY release occurs before the arrival of dietary lipids to the distal small intestine146, its actions to induce gastric relaxation and delayed emptying probably include neural mechanisms, possibly via vagally mediated pathways. Upon release from L-cells, PYY is cleaved to PYY3-36 by the enzyme dipeptidyl peptidase 4. Of the neuropeptide-Y-selective receptors, circulating PYY3-36 interacts with neuropeptide Y receptor type 2 (NPY2R) preferentially, rather than with type 1, type 3, type 4 or type 5 receptors143, to inhibit gastrointestinal motility and transit. As PYY3-36 readily crosses the blood–brain barrier146, an effect on neurons of the DMV is probable; in fact, brainstem microinjections of PYY induce either excitation or inhib ition of gastric motility, depending on the basal activity of the stomach147–151. Electrophysiological recordings confirm a Y2 receptor-mediated response of PYY on identified vagal motor neurons84,86 as well as on enteric neurocircuits152. The mechanism of action of PYY on vagal motor neurons varied in concert with brainstem levels of cAMP84, suggesting a means to explain the puzzling opposing responses (either excitation or inhibition of gastric motility) observed in the in vivo experiments on gastric motility147,148. For a more detailed analysis of the aforementioned and other gastrointestinal peptides, we refer the reader to more comprehensive and specialized reviews elsewhere153,154.
Vagal neuroplasticity in stress
An extensive network of interconnected neurocircuits regulate visceral, emotional and feeding vagal pathways, and include projections originating from cortical, subcortical and midbrain areas that impinge on brainstem vagal neurons5. These neurocircuits theoretically offer a high degree of integrative capacity to facilitate adaptive processes. Furthermore, bidirectional communication between the brain and the gut influences homeostasis through alterations in gastrointestinal, immune, central and autonomic nervous systems. These brainstem vagal neurocircuits, however, have long been thought of as static and only in the past decade has it been recognized that they are neuroplastic.
A rapid response to either acute internal or external stressors is a reflexive protective mechanism that necessitates adaptive modifications of relatively brief dur ation. As described previously, the DVC undergoes rapid (activated within ~5 min) and short-lasting (inactiv ated within ~60 min) cAMP-mediated neuroplastic changes of the availability to modulation of receptors that control the GABAergic synapse between the NTS and DMV82–84. A situation of acute stress can therefore be mimicked by a temporally restricted exposure to CRF, which results in decreased gastric motility155. Conversely, prolonged stress represents a more serious challenge and requires the ability to adapt to ongoing insults. However, the lack of resilience or adaptability to adverse events results frequently in dysfunction of gastric (delayed emptying) and colonic (accelerated) motility156. Such a dichotomy in the adaptive response to stress whereby some individuals demonstrate a high degree of resistance whereas others show vulnerability presents a unique opportunity to investigate the neurocircuits underlying stress and address the question of why some people are more prone to gastrointestinal-related dysfunctions than others.
Functional gastrointestinal disorders, including functional dyspepsia and IBS, are correlated highly with stress157,158, and stressful situations exacerbate gastro intestinal symptoms in susceptible individuals156. At times of stressful life events, positive social interactions help to reduce stress, and empathic responses as well as physical contact between human partners is positively correlated with increased circulating oxytocin levels159,160. Thus, many studies have suggested that central oxytocin represents a potent anxiolytic, amelior ating both cortisol (corticosterone in non-human animals) release and anxiety-like states and, by consequence, might have an important role in buffering physio logical responses to stressful life experiences161,162. A series of studies have demonstrated a prominent role for oxytocin in modulating human and non-human social behaviour163,164 with relevant anxiolytic-like effects in rodents, including recovery of gastrointestinal motility to pre-stress levels165,166.
In a series of elegant manuscripts, Takahashi’s group has shown the central role of oxytocinergic neurons of the PVN in the gastrointestinal-related anxiolytic effects of oxytocin and their role in favouring stress resilience165–168. Although some of the restoration of gastric motility mediated by oxytocin is related to its effects on the hypothalamus–pituitary–adrenal axis and/or decreased release of CRF from PVN neurons163,169,170, one also has to consider the direct influence of hypothalamic oxytocin on vagal brainstem neurocircuits. Preautonomic PVN neurons are the sole source of oxyto cinergic innervation to the DVC171 and are excited by stressful stimuli, social attachment and food intake172. Targeting these neurons could therefore represent a valuable pharmacological approach for alleviating stress-induced gastrointestinal dysmotility.
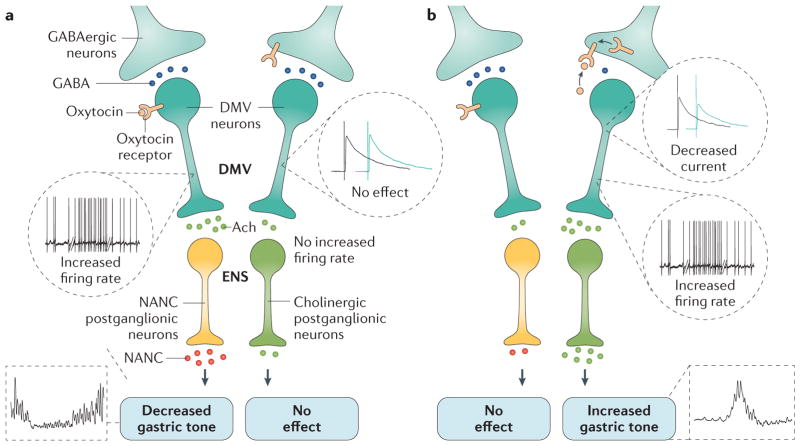
Upon its release onto brainstem vagal neurons, oxyto cin interacts with its own Gq-coupled receptor (the oxytocin receptor) to depolarize DMV neurons via a cAMP-dependent mechanism173,174, resulting, ultimately, in gastric relaxation and reduced motility171,175–177 (FIG. 4) mediated by the NANC pathway177. Interestingly, central administration of oxytocin antagonists increases gastric motility, suggesting that the PVN–DMV pathway is active tonically175,176.
Figure 4. Oxytocin receptor trafficking in the dorsal vagal complex and changes in gastric motility.
a | In control animals, oxytocin activates the oxytocin receptor on the surface of the subset of DMV neurons that control the NANC nitric oxide pathway. This interaction increases their firing rate and activates NANC postganglionic neurons, which ultimately decrease gastric tone and motility. The GABAergic terminals impinging on the subset of DMV neurons controlling pathways other than the NANC nitric oxide pathway are unaffected by oxytocin. b | Following the increase in cAMP levels, the oxytocin receptors present in the subset of GABAergic terminals impinging onto the previously unresponsive DMV neurons that control pathways other than the NANC nitric oxide pathway are translocated to the terminal surface. Oxytocin binding to these translocated receptors reduces the amplitude of the GABA current and increases the firing rate of the DMV neurons, leading to increased release of acetylcholine in enteric neurons and increased gastric tone and motility. The relative influence of the NANC nitric oxide pathway is probably diminished by the increased activation of the cholinergic pathway, thereby resulting in the overall increase in tone and motility observed upon oxytocin perfusion. Ach, acetylcholine; DMV, dorsal motor nucleus of the vagus; ENS, enteric nervous system; GABA, γ−aminobutyric acid; NANC, nonadrenergic noncholinergic
As hypothalamic oxytocin has a major role in the recovery of gastric and colonic motility after stress adaptation165,166,178, the question arises as to the vagally mediated mechanism of this anti-stress action. Either stress per se or central administration of CRF decreases gastric tone and motility156,179, an outcome similar to the gastric inhibitory effects on gastric tone and motility following central administration of oxytocin. This apparent conundrum has been partially resolved with a series of manuscripts published in the past few years that have demonstrated a differential engagement of postganglionic vagal neurocircuits by oxytocin177,180 (FIG. 4). In control, non-stressed rats, microinjection of oxytocin into the DVC decreases gastric tone and motility via activation of a nitric-oxide-mediated pathway; however, following surgical or pharmacological reduction of vagal afferent fibre input, or pretreatment with CRF, this effect of oxytocin on gastric motility and tone is attenuated, abolished or even reversed, such that an increase in gastric tone is observed177,180. The mech anism of action of this inverted effect includes activation of peripheral VIP–vagal and cholinergic–vagal pathways177,180, which become engaged via a cAMP-dependent translocation of oxytocin receptors on brainstem vagal synapses180. This translocation of receptors seems to be a mech anism common to other neurotransmitters, both in the DVC82–84,181 and in other CNS areas182.
Thus, it seems that the adaptive plasticity that promotes the anti-stress effects of oxytocin might do so by restoring coordinated, vagally determined gastric motility. This functional restoration of gastric motility is achieved via translocation of oxytocin receptors to the terminals of subsets of GABAergic NTS–DMV synapses, which leads to oxytocin-dependent inhibition of GABAergic transmission. Inhibition of GABAergic transmission results in disinhibition of vagal outputs and promotes a counter-regulatory effect that dampens and self-limits the actions of CRF under conditions of acute stress.
Although it is clear that an individual’s ability to cope with stress is determined by neuroendocrine, neuroimmunological and psychological responses that combine to determine the degree of stress resilience or susceptibility, the biological basis, the cellular mechanisms of adaptation and the factors that determine a pathophysiological outcome after stress have not yet been defined in detail. Certainly, a great deal of adaptive plasticity occurs in vagal brainstem neurocircuits, although several unresolved issues still linger. For example, in an acute stressful situation, what determines the engagement by oxytocin of one vagal neurocircuit rather than another? What are the effects on vagal neurocircuits of long-term exposure to high CRF levels or to repetitive chronic stress? How are these vagal neurocircuits rearranged in chronic pathologies such as functional dyspepsia? More gener ally, what determines the relative balance of strength between the inhibitory NANC and the excitatory cholin ergic neurocircuits? How are these functionally segregated NANC and cholinergic neurocircuits primed to convey the appropriate gastric motility response as a consequence of environmental stimuli? A closer investigation of the interface between basic and clinical science is needed to elucidate which factors determine the pathophysio logical response of vagal neurocircuits controlling gastric motility, and even closer collaborations should be encouraged between bench and clinical researchers.
Parkinson disease
Over the past decade a growing interest has been placed on degenerative disorders of the CNS that affect the gastrointestinal tract, possibly related to pathologies that affect the vagus nerve183–187. Of particular interest is the observation that altered swallowing, constipation, dysphagia, early satiety and nausea, delayed gastric emptying and reduced gastric motility are core components of the parkinsonian clinical picture and can affect patients up to 10–15 years before the clinical diagnosis. Indeed, the occurrence of these disturbances in otherwise healthy people has been associated with an increased Parkinson disease risk187–189.
Most experimental effort in the context of parkinsonian signs has been devoted to the study of abnormalities of the lower gastrointestinal tract190–192, with less attention placed upon gastric dysfunctions. However, delayed gastric emptying occurs at all stages of Parkinson disease, affecting up to 90% of patients193,194, and contributes to the problematic fluctuations in absorption rate, and therefore response to pharmaceutical treatments. Levodopa, for example, is absorbed in the proximal small intestine and its effective dosage is determined by the rate of gastric emptying, which can be further slowed by dopaminergic medications such as levodopa itself. Thus, it is necessary to conduct tightly regulated studies in the search for effective prokinetic agents to use in patients with parkinsonian signs, and/or resume studies on proven, effective prokinetics, such as domperidone, whose mechanisms of action are yet to be determined in full.
Although several mouse and rat models can be utilized for Parkinson disease research195, gastrointestinal research in the context of Parkinson disease, in particular gastric research, has been focused on immunohistochemical studies of the ENS, with less attention being paid to functional studies or investigations at the level of the DVC196–204. One of the most common rat models of non-motor Parkinsonian defects involves the unilateral degeneration of dopaminergic neurons by micro-injection of the toxin 6-hydroxydopamine (6-OHDA) into either the substantia nigra pars compacta or the medial forebrain bundle. In this model, gastrointestinal-related dysfunctions can be observed after ~4 weeks and consist primarily of neurochemical alterations in the colon197,198 — consistent with the reported constipation observed in patients with parkinsonian syndromes — and delayed gastric emptying, possibly due to changes in the neurochemical phenotype of gastric myenteric and DVC neurons202,204.
However, the prodromic involvement of the gastrointestinal tract suggests that the aetiology of Parkinson disease also involves a ‘bottom-up’ pathogenesis. The morphological hallmark of Parkinson disease is the presence of Lewy bodies and Lewy neurites in dopaminergic neurons of the basal ganglia205. Lewy bodies and Lewy neurites are characteristic intracellular proteinaceous inclusions composed primarily of misfolded α-synuclein protein206. When present in dopaminergic neurons of the basal ganglia, these inclusions are linked directly to the typical neuronal degeneration of Parkinson disease. Interestingly, several studies show a broad presence of Lewy bodies and Lewy neurites in the soma and processes of both enteric neurons and vagal motor neurons, as well as tissues from the submandibular gland and colon207,208.
On the basis of this distinct distribution pattern of Lewy bodies within the ENS and DMV, and the early onset of gastrointestinal symptoms, Braak and colleagues have suggested that idiopathic Parkinson disease begins with absorption of an ingested environmental ‘unknown pathogen’ into the ENS, which is then transported to the CNS via the vagus nerve and, starting from the DMV, spreads to higher CNS areas209–211 (BOX 2). In this model, the DMV would represent the main intersection point in the CNS network affected by Parkinson disease. Indeed, although the Lewy body pathology in the DMV has been shown in Parkinson disease experimental models and in patients with the condition, and the involvement of the DMV in the disease is accepted200,204,212–214, the direct involvement of the vagus nerve is highly possible (although the evidence is as yet circumstantial). Braak’s hypothesis is still controversial; some authors and experimental evidence are supportive, whereas others are more sceptical215–218.
Box 2. The spread of α-synuclein.
In both the enteric nervous system (ENS) and central nervous systems (CNS), the neurons that develop α-synuclein inclusions are projection neurons with long, poorly myelinated axons211. Together with the presence of Lewy bodies, this set of observations led Braak’s group to formulate the hypothesis that ENS neurons (as well as neurons in the olfactory bulb) might provide the first pathogenic link in Lewy body pathology, which would then spread to the dorsal motor nucleus of the vagus (DMV) at the earliest stages of Parkinson disease211.
According to this hypothesis, the involvement of other CNS areas rostral to the DMV occurs progressively in six pathological stages, which include three premotor stages when α-synuclein is present in the ENS and lower brainstem (including the DMV and A6 area, among others), and the final stages of Parkinson disease, when Lewy body pathology affects both motor and cognitive areas, such as the substantia nigra pars compacta, the mesocortex and neocortex, and the functions of these regions213.
The spread of Lewy body pathology between CNS areas occurs in a retrograde, prion-like manner210,225–227, jumping synapses between adjacent neurons and ultimately causing their degeneration227,228. Indeed, Olanow and Brundin have hypothesized that some types of Parkinson disease are due to a prion-like disorder, suggesting that native α-synuclein undergoes a conformational change that promotes its misfolding229.
The spread of α-synuclein from grafted to resident neurons, or from neurons to astroglia, in both humans and in animals217,225,230,231 makes the progression of Parkinson disease via neural connections a possibility that needs to be explored and exploited in the quest for novel therapeutic targets to treat patients with gastrointestinal-related parkinsonian symptoms.
Despite exerting a prominent burden on patient quality of life, parkinsonian-related gastrointestinal dysfunctions represent an underserved and understudied area of research, and progress in understanding both the aetiology and treatment of these gastrointestinal disorders has been hampered by a lack of rigorous, focused effort to understand the disease pathophysiology as well as the testing of therapeutic interventions. For example, what is the unknown pathogen(s) hypothesized by Braak’s group to be responsible for the retrograde transport of α-synuclein inclusions? Environmental toxins, such as herbicides or pesticides, or exposure to high levels of manganese are known to induce Parkinson-disease-like motor symptoms195. However, investigations into the Parkinson-disease-like gastric effects of these substances are still in their infancy. Similarly, the mechanisms responsible for the gastric neuronal degeneration observed following administration of 6-OHDA in the basal ganglia are still unresolved. What is the role of central dopaminergic neurotransmission in the development of parkinsonian gastrointestinal dysfunctions? Despite the common use of dopaminergic antagonists as prokinetic agents, few, if any, dopaminergic neurons are found within the ENS, suggesting that either these drugs target central dopaminergic neuro-circuits that are involved in the control of gastrointestinal motility or that the prokinetic actions of these drugs are not due to actions at dopamine receptors. Both of these cases represent an opportunity to focus research effort on characterizing the role of central dopaminergic transmission in the pathophysiology of the gastrointestinal tract and the preservation of dopaminergic neurons in Parkinson disease. In fact, the role of central dopaminergic neurotransmission in the control of gastrointestinal functions has not been investigated in either healthy or Parkinson disease experimental models. Which prokinetic agents can be used to tackle the gastrointestinal-related disturbances of patients with Parkinson disease effectively? Are there differences in the gastrointestinal-related disturbances between genetic and environmental origins of Parkinson disease? Providing answers to these, as well as other questions related to Parkinson disease aetiology, should be a prime target of interest not only for understanding the neural mechanisms of Parkinson-disease-related gastrointestinal dysfunctions but also for elucidating other neurodegenerative pathologies that result in an alteration of gastrointestinal functionality.
Conclusions
Although vagovagal reflex control of the gut is understood at a basic mechanistic level, there are many factors (for example, place in the environment, time of day, taste and absorption of food, stress, pain, hormonal background and pathophysiological status, including presence of neurological degenerative diseases) that can radically alter gastrointestinal function. However, the neural mechanisms responsible for remodelling of gastrointestinal function as a result of these factors are poorly understood.
Functional gastrointestinal motility disorders are common conditions, often chronic and disabling, and they account for a large proportion of consultations with primary care and specialist physicians. The pathophysiology of these disorders remains incompletely understood, but several lines of evidence point toward impairment of the vagal sensory–motor loop connecting the gut to the CNS and vice versa. Nonetheless, big gaps in our knowledge still prevent an approach that goes beyond treating the symptoms of functional gastrointestinal motility disorders.
In summary, we are only just beginning to understand the mechanisms involved in the response of gastrointestinal vagovagal circuits to intrinsic and extrinsic factors. At first glance, the permutations for modification in these systems seem almost limitless. Although adaptive responses are essential to adjust to ever-changing physiological conditions, derangements or untimely deviations can have pathophysiological consequences, such as exacerbation of stress-induced functional dyspepsia. Similarly, neurodegenerative alterations of the vagal neurocircuitry induce dramatic impairments of gastrointestinal functions that, given the lack of insight into the underlying physiological mechanisms, are difficult to manage in clinical practice.
Key points.
Brainstem vagovagal neurocircuits modulate the functions of the upper gastrointestinal tract
Neuronal communications between vagal sensory (nucleus tractus solitarius, NTS) and motor (dorsal motor nucleus of the vagus, DMV) nuclei are highly specialized and probably specific for function and target organ
NTS–DMV synaptic contacts are not static but undergo plastic changes to ensure that vagally regulated gastrointestinal functions respond appropriately to ever-changing physiological conditions or derangements
Gastrointestinal peptides influence vagovagal circuits via actions on both vagal afferent fibres and brainstem nuclei
Neurodegenerative alterations of the vagal neurocircuitry induce marked impairments of gastrointestinal functions
Acknowledgments
The authors wish to thank NIH grants DK 55530, DK 78364 and DK 99350 and the Michael J. Fox Foundation for Parkinson’s Disease for their support; we are also very grateful to K. N. Browning for critical comments on previous versions of the manuscript and for checking the grammar (because we do not want to “write as we speak”). We also thank C. M. Travagli and Z. Travagli for support and encouragement.
Footnotes
Competing interests statement<
The authors declare no competing interests.
Review criteria
For this Review we conducted PubMed database searches involving combinations of terms that included “vagus, brainstem, gastric motility, stress, Parkinson’s disease, Huntington, ALS, fibromyalgia”. Together, the authors have a combined ~30 years of experience in the field of vagal pathophysiology with much of their work associated with electrophysiology, pharmacology, immunohistochemistry and in vivo animal models of gastrointestinal motility. This combined experience formed the basis of this Review.
References
- 1.Sanders KM, Ward SM, Koh SD. Interstitial cells: regulators of smooth muscle function. Physiol Rev. 2014;94:859–907. doi: 10.1152/physrev.00037.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharkey KA. Emerging roles for enteric glia in gastrointestinal disorders. J Clin Invest. 2015;125:918–925. doi: 10.1172/JCI76303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Furness JB. The enteric nervous system and neurogastroenterology. Nat Rev Gastroenterol Hepatol. 2012;9:286–294. doi: 10.1038/nrgastro.2012.32. [DOI] [PubMed] [Google Scholar]
- 4.Travagli RA, Hermann GE, Browning KN, Rogers RC. Brainstem circuits regulating gastric function. Annu Rev Physiol. 2006;68:279–305. doi: 10.1146/annurev.physiol.68.040504.094635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Browning KN, Travagli RA. Central nervous system control of gastrointestinal motility and secretion and modulation of gastrointestinal functions. Compr Physiol. 2014;4:1339–1368. doi: 10.1002/cphy.c130055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pavlov VA, Tracey KJ. The vagus nerve and the inflammatory reflex — linking immunity and metabolism. Nat Rev Endocrinol. 2012;8:743–754. doi: 10.1038/nrendo.2012.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Babic T, Travagli RA. Role of metabotropic glutamate receptors in the regulation of pancreatic functions. Biochem Pharmacol. 2014;87:535–542. doi: 10.1016/j.bcp.2013.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kentish SJ, Page AJ. Plasticity of gastrointestinal vagal afferent endings. Physiol Behav. 2014;136:170–178. doi: 10.1016/j.physbeh.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 9.Doheny KK, et al. Diminished vagal tone is a predictive biomarker of necrotizing enterocolitis-risk in preterm infants. Neurogastroenterol Motil. 2014;26:832–840. doi: 10.1111/nmo.12337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation. 1996;93:1043–1065. [PubMed] [Google Scholar]
- 11.Souza GG, et al. Resilience and vagal tone predict cardiac recovery from acute social stress. Stress. 2007;10:368–374. doi: 10.1080/10253890701419886. [DOI] [PubMed] [Google Scholar]
- 12.Andresen MC, Kunze DL. Nucleus tractus solitarius — gateway to neural circulatory control. Annu Rev Physiol. 1994;56:93–116. doi: 10.1146/annurev.ph.56.030194.000521. [DOI] [PubMed] [Google Scholar]
- 13.Jean A. Brainstem control of swallowing: neuronal network and cellular mechanisms. Physiol Rev. 2001;81:929–969. doi: 10.1152/physrev.2001.81.2.929. [DOI] [PubMed] [Google Scholar]
- 14.Bradley RM, King MS, Wang L, Shu W. Neurotransmitter and neuromodulator activity in the gustatory zone of the nucleus tractus solitarius. Chem Senses. 1996;21:377–385. doi: 10.1093/chemse/21.3.377. [DOI] [PubMed] [Google Scholar]
- 15.Brookes SJ, Spencer NJ, Costa M, Zagorodnyuk VP. Extrinsic primary afferent signalling in the gut. Nat Rev Gastroenterol Hepatol. 2013;10:286–296. doi: 10.1038/nrgastro.2013.29. [DOI] [PubMed] [Google Scholar]
- 16.Berthoud HR, Blackshaw LA, Brookes SJ, Grundy D. Neuroanatomy of extrinsic afferents supplying the gastrointestinal tract. Neurogastroenterol Motil. 2004;16(Suppl 1):28–33. doi: 10.1111/j.1743-3150.2004.00471.x. [DOI] [PubMed] [Google Scholar]
- 17.Kalia M, Sullivan JM. Brainstem projections of sensory and motor components of the vagus nerve in the rat. J Comp Neurol. 1982;211:248–264. doi: 10.1002/cne.902110304. [DOI] [PubMed] [Google Scholar]
- 18.Kalia M, Fuxe K, Goldstein M. Rat medulla oblongata. II Dopaminergic, noradrenergic (A1 and A2) and adrenergic neurons, nerve fibers, and presumptive terminal processes. J Comp Neurol. 1985;233:308–332. doi: 10.1002/cne.902330303. [DOI] [PubMed] [Google Scholar]
- 19.Altschuler SM, Bao X, Bieger D, Hopkins DA, Miselis RR. Viscerotopic representation of the upper alimentary tract in the rat: sensory ganglia and nuclei of the solitary and spinal trigeminal tracts. J Comp Neurol. 1989;283:248–268. doi: 10.1002/cne.902830207. [DOI] [PubMed] [Google Scholar]
- 20.Barraco R, El-Ridi M, Parizon M, Bradley D. An atlas of the rat subpostremal nucleus tractus solitarius. Brain Res Bull. 1992;29:703–765. doi: 10.1016/0361-9230(92)90143-l. [DOI] [PubMed] [Google Scholar]
- 21.Zhang X, Fogel R, Renehan WE. Relationships between the morphology and function of gastric- and intestine-sensitive neurons in the nucleus of the solitary tract. J Comp Neurol. 1995;363:37–52. doi: 10.1002/cne.903630105. [DOI] [PubMed] [Google Scholar]
- 22.Kubota Y, et al. The distribution of cholecystokinin octapeptide-like structures in the lower brain stem of the rat: an immunohistochemical analysis. Neuroscience. 1983;9:587–604. doi: 10.1016/0306-4522(83)90176-8. [DOI] [PubMed] [Google Scholar]
- 23.Maley BE. Immunohistochemical localization of neuropeptides and neurotransmitters in the nucleus solitarius. Chem Senses. 1996;21:367–376. doi: 10.1093/chemse/21.3.367. [DOI] [PubMed] [Google Scholar]
- 24.Lin LH, Talman WT. Nitroxidergic neurons in rat nucleus tractus solitarii express vesicular glutamate transporter 3. J Chem Neuroanat. 2005;29:179–191. doi: 10.1016/j.jchemneu.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 25.Larsen PJ, Tang-Christensen M, Holst JJ, Orskov C. Distribution of glucagon-like peptide-1 and other preproglucagon- derived peptides in the rat hypothalamus and brainstem. Neurosci. 1997;77:257–270. doi: 10.1016/s0306-4522(96)00434-4. [DOI] [PubMed] [Google Scholar]
- 26.Kessler JP, Baude A. Distribution of AMPA receptor subunits GluR1-4 in the dorsal vagal complex of the rat: a light and electron microscope immunocytochemical study. Synapse. 1999;34:55–67. doi: 10.1002/(SICI)1098-2396(199910)34:1<55::AID-SYN7>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 27.Glass MJ, Huang J, Speth RC, Iadecola C, Pickel VM. Angiotensin, I. I AT-1A receptor immunolabeling in rat medial nucleus tractus solitarius neurons: subcellular targeting and relationships with catecholamines. Neuroscience. 2005;130:713–723. doi: 10.1016/j.neuroscience.2004.08.057. [DOI] [PubMed] [Google Scholar]
- 28.Fong AY, Stornetta RL, Foley CM, Potts JT. Immunohistochemical localization of GAD67-expressing neurons and processes in the rat brainstem: subregional distribution in the nucleus tractus solitarius. J Comp Neurol. 2005;493:274–290. doi: 10.1002/cne.20758. [DOI] [PubMed] [Google Scholar]
- 29.Gross PM, Wall KM, Pang JJ, Shaver SW, Wainman DS. Microvascular specializations promoting rapid interstitial solute dispersion in nucleus tractus solitarius. Am J Physiol. 1990;259:R1131–R1138. doi: 10.1152/ajpregu.1990.259.6.R1131. [DOI] [PubMed] [Google Scholar]
- 30.Smith BN, Dou P, Barber WD, Dudek FE. Vagally evoked synaptic currents in the immature rat nucleus tractus solitarii in an intact in vitro preparation. J Physiol. 1998;512:149–162. doi: 10.1111/j.1469-7793.1998.149bf.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rinaman L, Roesch MR, Card JP. Retrograde transynaptic pseudorabies virus infection of central autonomic circuits in neonatal rats. Brain Res Rev Brain Res. 2000;114:207–216. doi: 10.1016/s0165-3806(99)00039-5. [DOI] [PubMed] [Google Scholar]
- 32.Buijs RM, Chun SJ, Niijima A, Romijn HJ, Nagai K. Parasympathetic and sympathetic control of the pancreas; a role for the suprachiasmatic nucleus and other hypothalamic centers that are involved in the regulation of food intake. J Comp Neurol. 2001;431:405–423. doi: 10.1002/1096-9861(20010319)431:4<405::aid-cne1079>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 33.Guyenet PG. The sympathetic control of blood pressure. Nat Rev Neurosci. 2006;7:335–346. doi: 10.1038/nrn1902. [DOI] [PubMed] [Google Scholar]
- 34.Goyal RK, Chaudhury A. Physiology of normal esophageal motility. J Clin Gastroenterol. 2008;42:610–619. doi: 10.1097/MCG.0b013e31816b444d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mittal RK. Motor Function of the Pharynx, Esophagus, and its Sphincters. Colloquium Life Science; 2011. [PubMed] [Google Scholar]
- 36.Berthoud HR, Carlson NR, Powley TL. Topography of efferent vagal innervation of the rat gastrointestinal tract. Am J Physiol. 1991;260:R200–R207. doi: 10.1152/ajpregu.1991.260.1.R200. [DOI] [PubMed] [Google Scholar]
- 37.Fox EA, Powley TL. Longitudinal columnar organization within the dorsal motor nucleus represents separate branches of the abdominal vagus. Brain Res. 1985;341:269–282. doi: 10.1016/0006-8993(85)91066-2. [DOI] [PubMed] [Google Scholar]
- 38.Shapiro RE, Miselis RR. The central organization of the vagus nerve innervating the stomach of the rat. J Comp Neurol. 1985;238:473–488. doi: 10.1002/cne.902380411. [DOI] [PubMed] [Google Scholar]
- 39.Huang X, Tork I, Paxinos G. Dorsal motor nucleus of the vagus nerve: a cyto- and chemoarchitectonic study in the human. J Comp Neurol. 1993;330:158–182. doi: 10.1002/cne.903300203. [DOI] [PubMed] [Google Scholar]
- 40.Browning KN, Renehan WE, Travagli RA. Electrophysiological and morphological heterogeneity of rat dorsal vagal neurones which project to specific areas of the gastrointestinal tract. J Physiol. 1999;517:521–532. doi: 10.1111/j.1469-7793.1999.0521t.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fogel R, Zhang X, Renehan WE. Relationships between the morphology and function of gastric and intestinal distention-sensitive neurons in the dorsal motor nucleus of the vagus. J Comp Neurol. 1996;364:78–91. doi: 10.1002/(SICI)1096-9861(19960101)364:1<78::AID-CNE7>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 42.Gao H, et al. Morphological and electrophysiological features of motor neurons and putative interneurons in the dorsal vagal complex of rats and mice. Brain Res. 2009;1291:40–52. doi: 10.1016/j.brainres.2009.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Browning KN, Coleman FH, Travagli RA. Characterization of pancreas-projecting rat dorsal motor nucleus of the vagus neurons. Am J Physiol Gastrointest Liver Physiol. 2005;288:G950–G955. doi: 10.1152/ajpgi.00549.2004. [DOI] [PubMed] [Google Scholar]
- 44.Travagli RA, Gillis RA, Rossiter CD, Vicini S. Glutamate and GABA-mediated synaptic currents in neurons of the rat dorsal motor nucleus of the vagus. Am J Physiol. 1991;260:G531–G536. doi: 10.1152/ajpgi.1991.260.3.G531. [DOI] [PubMed] [Google Scholar]
- 45.Babic T, Browning KN, Travagli RA. Differential organization of excitatory and inhibitory synapses within the rat dorsal vagal complex. Am J Physiol Gastrointest Liver Physiol. 2011;300:G21–G32. doi: 10.1152/ajpgi.00363.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sivarao DV, Krowicki ZK, Hornby PJ. Role of GABAA receptors in rat hindbrain nuclei controlling gastric motor function. Neurogastroenterol Motil. 1998;10:305–313. doi: 10.1046/j.1365-2982.1998.00110.x. [DOI] [PubMed] [Google Scholar]
- 47.Browning KN, Coleman FH, Travagli RA. Effects of pancreatic polypeptide on pancreas-projecting rat dorsal motor nucleus of the vagus neurons. Am J Physiol Gastrointest Liver Physiol. 2005;289:G209–G219. doi: 10.1152/ajpgi.00560.2004. [DOI] [PubMed] [Google Scholar]
- 48.Hornby PJ, et al. Medullary raphe: a new site for vagally mediated stimulation of gastric motility in cats. Am J Physiol. 1990;258:G637–G647. doi: 10.1152/ajpgi.1990.258.4.G637. [DOI] [PubMed] [Google Scholar]
- 49.Armstrong DM, Manley L, Haycock JW, Hersh LB. Co-localization of choline acetyltransferase and tyrosine hydroxylase within neurons of the dorsal motor nucleus of the vagus. J Chem Neuroanat. 1990;3:133–140. [PubMed] [Google Scholar]
- 50.Schemann M, Grundy D. Electrophysiological identification of vagally innervated enteric neurons in guinea pig stomach. Am J Physiol. 1992;263:G709–G718. doi: 10.1152/ajpgi.1992.263.5.G709. [DOI] [PubMed] [Google Scholar]
- 51.Guo JJ, Browning KN, Rogers RC, Travagli RA. Catecholaminergic neurons in rat dorsal motor nucleus of vagus project selectively to gastric corpus. Am J Physiol Gastrointest Liver Physiol. 2001;280:G361–G367. doi: 10.1152/ajpgi.2001.280.3.G361. [DOI] [PubMed] [Google Scholar]
- 52.Krowicki ZK, Sharkey KA, Serron SC, Nathan NA, Hornby PJ. Distribution of nitric oxide synthase in rat dorsal vagal complex and effects of microinjection of NO compounds upon gastric motor function. J Comp Neurol. 1997;377:49–69. doi: 10.1002/(sici)1096-9861(19970106)377:1<49::aid-cne6>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 53.Chang HY, Mashimo H, Goyal RK. Musings on the wanderer: what’s new in our understanding of vagovagal reflex?: IV Current concepts of vagal efferent projections to the gut. Am J Physiol Gastrointest Liver Physiol. 2003;284:G357–G366. doi: 10.1152/ajpgi.00478.2002. [DOI] [PubMed] [Google Scholar]
- 54.Cannon WB, Leib CW. The receptive relaxation of the stomach. Am J Physiol. 1911;29:267–273. [Google Scholar]
- 55.Langley JN. On inhibitory fibres in the vagus for the end of the oesophagus and the stomach. J Physiol. 1898;23:407–414. doi: 10.1113/jphysiol.1898.sp000737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rogers RC, Hermann GE, Travagli RA. Brainstem pathways responsible for oesophageal control of gastric motility and tone in the rat. J Physiol. 1999;514:369–383. doi: 10.1111/j.1469-7793.1999.369ae.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Abrahamsson H. Studies on the inhibitory nervous control of gastric motility. Acta Physiol Scand. 1973;390(Suppl):1–38. [PubMed] [Google Scholar]
- 58.Desai KM, Sessa WC, Vane JR. Involvement of nitric oxide in the reflex relaxation of the stomach to accommodate food or fluid. Nature. 1991;351:477–479. doi: 10.1038/351477a0. [DOI] [PubMed] [Google Scholar]
- 59.Tack J, Caenepeel P, Piessevaux H, Cuomo R, Janssens J. Assessment of meal induced gastric accommodation by a satiety drinking test in health and in severe functional dyspepsia. Gut. 2003;52:1271–1277. doi: 10.1136/gut.52.9.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Delgado-Aros S, et al. Contributions of gastric volumes and gastric emptying to meal size and postmeal symptoms in functional dyspepsia. Gastroenterology. 2004;127:1685–1694. doi: 10.1053/j.gastro.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 61.Troncon LE, Thompson DG, Ahluwalia NK, Barlow J, Heggie L. Relations between upper abdominal symptoms and gastric distension abnormalities in dysmotility like functional dyspepsia and after vagotomy. Gut. 1995;37:17–22. doi: 10.1136/gut.37.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Holtmann G, Goebell H, Jockenhoevel F, Talley NJ. Altered vagal and intestinal mechanosensory function in chronic unexplained dyspepsia. Gut. 1998;42:501–506. doi: 10.1136/gut.42.4.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu LS, et al. A rat model of chronic gastric sensorimotor dysfunction resulting from transient neonatal gastric irritation. Gastroenterology. 2008;134:2070–2079. doi: 10.1053/j.gastro.2008.02.093. [DOI] [PubMed] [Google Scholar]
- 64.Rinaman L, Card JP, Schwaber JS, Miselis RR. Ultrastructural demonstration of a gastric monosynaptic vagal circuit in the nucleus of the solitary tract in rat. J Neurosci. 1989;9:1985–1996. doi: 10.1523/JNEUROSCI.09-06-01985.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Blackshaw LA, Page AJ, Young RL. Metabotropic glutamate receptors as novel therapeutic targets on visceral sensory pathways. Front Neurosci. 2011;5:40. doi: 10.3389/fnins.2011.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hallock RM, Martyniuk CJ, Finger TE. Group III metabotropic glutamate receptors (mGluRs) modulate transmission of gustatory inputs in the brainstem. J Neurophysiol. 2009;102:192–202. doi: 10.1152/jn.00135.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Young RL, Cooper NJ, Blackshaw LA. Anatomy and function of group III metabotropic glutamate receptors in gastric vagal pathways. Neuropharmacology. 2008;54:965–975. doi: 10.1016/j.neuropharm.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 68.Browning KN, Zheng Z, Gettys TW, Travagli RA. Vagal afferent control of opioidergic effects in rat brainstem circuits. J Physiol. 2006;575:761–776. doi: 10.1113/jphysiol.2006.111104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Page AJ, et al. Metabotropic glutamate receptors inhibit mechanosensitivity in vagal sensory neurons. Gastroenterology. 2005;128:402–410. doi: 10.1053/j.gastro.2004.11.062. [DOI] [PubMed] [Google Scholar]
- 70.Jin YH, Bailey TW, Andresen MC. Cranial afferent glutamate heterosynaptically modulates GABA release onto second-order neurons via distinctly segregated metabotropic glutamate receptors. J Neurosci. 2004;24:9332–9340. doi: 10.1523/JNEUROSCI.1991-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gerber U, Gee CE, Benquet P. Metabotropic glutamate receptors: intracellular signaling pathways. Curr Opin Pharmacol. 2007;7:56–61. doi: 10.1016/j.coph.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 72.Niswender CM, Conn PJ. Metabotropic glutamate receptors: physiology, pharmacology, and disease. Annu Rev Pharmacol Toxicol. 2010;50:295–322. doi: 10.1146/annurev.pharmtox.011008.145533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Browning KN, Travagli RA. Functional organization of presynaptic metabotropic glutamate receptors in vagal brainstem circuits. J Neurosci. 2007;27:8979–8988. doi: 10.1523/JNEUROSCI.1105-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Berthoud HR, Sutton GM, Townsend RL, Patterson LM, Zheng H. Brainstem mechanisms integrating gut-derived satiety signals and descending forebrain information in the control of meal size. Physiol Behav. 2006;89:517–524. doi: 10.1016/j.physbeh.2006.08.018. [DOI] [PubMed] [Google Scholar]
- 75.Drucker DJ. The biology of incretin hormones. Cell Metab. 2006;3:153–165. doi: 10.1016/j.cmet.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 76.Dufresne M, Seva C, Fourmy D. Cholecystokinin and gastrin receptors. Physiol Rev. 2006;86:805–847. doi: 10.1152/physrev.00014.2005. [DOI] [PubMed] [Google Scholar]
- 77.Banks WA. The blood–brain barrier as a regulatory interface in the gut–brain axes. Physiol Behav. 2006;89:472–476. doi: 10.1016/j.physbeh.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 78.Kastin AJ, Akerstrom V, Pan W. Interactions of glucagon-like peptide-1 (GLP-1) with the blood–brain barrier. J Mol Neurosci. 2002;18:7–14. doi: 10.1385/JMN:18:1-2:07. [DOI] [PubMed] [Google Scholar]
- 79.Orts-Del’immagine A, et al. Properties of subependymal cerebrospinal fluid contacting neurones in the dorsal vagal complex of the mouse brainstem. J Physiol. 2012;590:3719–3741. doi: 10.1113/jphysiol.2012.227959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Noble F, et al. International Union of Pharmacology. XXI Structure, distribution, and functions of cholecystokinin receptors. Pharmacol Rev. 1999;51:745–781. [PubMed] [Google Scholar]
- 81.Campbell JE, Drucker DJ. Pharmacology, physiology, and mechanisms of incretin hormone action. Cell Metab. 2013;17:819–837. doi: 10.1016/j.cmet.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 82.Browning KN, Travagli RA. The peptide TRH uncovers the presence of presynaptic 5-HT1A receptors via activation of a second messenger pathway in the rat dorsal vagal complex. J Physiol. 2001;531:425–435. doi: 10.1111/j.1469-7793.2001.0425i.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Browning KN, Kalyuzhny AE, Travagli RA. Muopioid receptor trafficking on inhibitory synapses in the rat brainstem. J Neurosci. 2004;24:9344–9352. doi: 10.1523/JNEUROSCI.1676-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Browning KN, Travagli RA. Modulation of inhibitory neurotransmission in brainstem vagal circuits by NPY and PYY is controlled by cAMP levels. Neurogastroenterol Motil. 2009;21:1309–e1126. doi: 10.1111/j.1365-2982.2009.01367.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Browning KN, Kalyuzhny AE, Travagli RA. Opioid peptides inhibit excitatory but not inhibitory synaptic transmission in the rat dorsal motor nucleus of the vagus. J Neurosci. 2002;22:2998–3004. doi: 10.1523/JNEUROSCI.22-08-02998.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Browning KN, Travagli RA. Neuropeptide Y and peptide YY inhibit excitatory synaptic transmission in the rat dorsal motor nucleus of the vagus. J Physiol. 2003;549:775–785. doi: 10.1113/jphysiol.2003.042036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Berthoud HR. Vagal and hormonal gut–brain communication: from satiation to satisfaction. Neurogastroenterol Motil. 2008;20(Suppl 1):64–72. doi: 10.1111/j.1365-2982.2008.01104.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Raybould HE, Tache Y. Cholecystokinin inhibits gastric motility and emptying via a capsaicin-sensitive vagal pathway in rats. Am J Physiol. 1988;255:G242–G246. doi: 10.1152/ajpgi.1988.255.2.G242. [DOI] [PubMed] [Google Scholar]
- 89.Woods SC. Gastrointestinal satiety signals I. An overview of gastrointestinal signals that influence food intake. Am J Physiol Gastrointest Liver Physiol. 2004;286:G7–G13. doi: 10.1152/ajpgi.00448.2003. [DOI] [PubMed] [Google Scholar]
- 90.Owyang C, Logsdon CD. New insights into neurohormonal regulation of pancreatic secretion. Gastroenterology. 2004;127:957–969. doi: 10.1053/j.gastro.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 91.Andrews PL, Sanger GJ. Abdominal vagal afferent neurones: an important target for the treatment of gastrointestinal dysfunction. Curr Opin Pharmacol. 2002;2:650–656. doi: 10.1016/s1471-4892(02)00227-8. [DOI] [PubMed] [Google Scholar]
- 92.Imeryuz N, et al. Glucagon-like peptide-1 inhibits gastric emptying via vagal afferent-mediated central mechanisms. Am J Physiol. 1997;273:G920–G927. doi: 10.1152/ajpgi.1997.273.4.G920. [DOI] [PubMed] [Google Scholar]
- 93.Grill HJ. Leptin and the systems neuroscience of meal size control. Front Neuroendocrinol. 2010;31:61–78. doi: 10.1016/j.yfrne.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Owyang C, Heldsinger A. Vagal control of satiety and hormonal regulation of appetite. J Neurogastroenterol Motil. 2011;17:338–348. doi: 10.5056/jnm.2011.17.4.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Czaja K, Burns GA, Ritter RC. Capsaicin-induced neuronal death and proliferation of the primary sensory neurons located in the nodose ganglia of adult rats. Neuroscience. 2008;154:621–630. doi: 10.1016/j.neuroscience.2008.03.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Holzer P. Capsaicin-sensitive afferent neurones and gastrointestinal propulsion in the rat. Arch Pharmacol. 1986;332:62–65. doi: 10.1007/BF00633198. [DOI] [PubMed] [Google Scholar]
- 97.South EH, Ritter RC. Capsaicin application to central or peripheral vagal fibers attenuates CCK satiety. Peptides. 1988;9:601–612. doi: 10.1016/0196-9781(88)90171-4. [DOI] [PubMed] [Google Scholar]
- 98.Holzer HH, Turkelson CM, Solomon TE, Raybould HE. Intestinal lipid inhibits gastric emptying via CCK and a vagal capsaicin-sensitive afferent pathway in rats. Am J Physiol. 1994;267:G625–G629. doi: 10.1152/ajpgi.1994.267.4.G625. [DOI] [PubMed] [Google Scholar]
- 99.Blackshaw LA, Page AJ, Partosoedarso ER. Acute effects of capsaicin on gastrointestinal vagal afferents. Neuroscience. 2000;96:407–416. doi: 10.1016/s0306-4522(99)00547-3. [DOI] [PubMed] [Google Scholar]
- 100.Li Y, Owyang C. Endogenous cholecystokinin stimulates pancreatic enzyme secretion via vagal afferent pathway in rats. Gastroenterology. 1994;107:525–531. doi: 10.1016/0016-5085(94)90180-5. [DOI] [PubMed] [Google Scholar]
- 101.Blackshaw LA, Grundy D. Effects of cholecystokinin (CCK-8) on two classes of gastroduodenal vagal afferent fibre. J Auton Nerv Syst. 1990;31:191–202. doi: 10.1016/0165-1838(90)90185-l. [DOI] [PubMed] [Google Scholar]
- 102.Zittel TT, Rothenhofer I, Meyer JH, Raybould HE. Small intestinal capsaicin-sensitive afferents mediate feedback inhibition of gastric emptying in rats. Am J Physiol Gastrointest Liver Physiol. 1994;267:G1142–G1145. doi: 10.1152/ajpgi.1994.267.6.G1142. [DOI] [PubMed] [Google Scholar]
- 103.Lloyd KC, Holzer HH, Zittel TT, Raybould HE. Duodenal lipid inhibits gastric acid secretion by vagal, capsaicin-sensitive afferent pathways in rats. Am J Physiol. 1993;264:G659–G663. doi: 10.1152/ajpgi.1993.264.4.G659. [DOI] [PubMed] [Google Scholar]
- 104.Moran TH. Gut peptide signaling in the controls of food intake. Obesity (Silver Spring) 2006;14:250S–253S. doi: 10.1038/oby.2006.318. [DOI] [PubMed] [Google Scholar]
- 105.Browning KN, Babic T, Holmes GM, Swartz EM, Travagli RA. A critical re-evaluation of the specificity of action of perivagal capsaicin. J Physiol. 2013;591:1563–1580. doi: 10.1113/jphysiol.2012.246827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Szolcsanyi J, Joo F, Jancso-Gabor A. Mitochondrial changes in preoptic neurons after capsaicin desensitization of the hypothalamic thermodetectors in rats. Nature. 1971;229:116–117. doi: 10.1038/229116a0. [DOI] [PubMed] [Google Scholar]
- 107.Ritter S, Dinh TT. Capsaicin-induced neuronal degeneration in the brain and retina of preweanling rats. J Comp Neurol. 1990;296:447–461. doi: 10.1002/cne.902960310. [DOI] [PubMed] [Google Scholar]
- 108.Ritter S, Dinh TT. Capsaicin-induced neuronal degeneration: silver impregnation of cell bodies, axons, and terminals in the central nervous system of the adult rat. J Comp Neurol. 1988;271:79–90. doi: 10.1002/cne.902710109. [DOI] [PubMed] [Google Scholar]
- 109.Holzer P. Neural injury, repair, and adaptation in the GI tract. II The elusive action of capsaicin on the vagus nerve. Am J Physiol. 1998;275:G8–G13. doi: 10.1152/ajpgi.1998.275.1.G8. [DOI] [PubMed] [Google Scholar]
- 110.Kim SR, et al. Transient receptor potential vanilloid subtype 1 mediates cell death of mesencephalic dopaminergic neurons in vivo and in vitro. J Neurosci. 2005;25:662–671. doi: 10.1523/JNEUROSCI.4166-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jancso-Gabor A, Szolcsanyi J, Jancso N. Stimulation and desensitization of the hypothalamic heat-sensitive structures by capsaicin in rats. J Physiol. 1970;208:449–459. doi: 10.1113/jphysiol.1970.sp009130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hajos M, Obal F, Jr, Jancso G, Obal F. Capsaicin impairs preoptic serotonin-sensitive structures mediating hypothermia in rats. Neurosci Lett. 1985;54:97–102. doi: 10.1016/s0304-3940(85)80124-5. [DOI] [PubMed] [Google Scholar]
- 113.Evangelista S, Santicioli P, Maggi CA, Meli A. Increase in gastric secretion induced by 2-deoxy-d-glucose is impaired in capsaicin pretreated rats. Br J Pharmacol. 1989;98:35–37. doi: 10.1111/j.1476-5381.1989.tb16858.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Raybould HE, Holzer P, Reddy SN, Yang H, Tache Y. Capsaicin-sensitive vagal afferents contribute to gastric acid and vascular responses to intracisternal TRH analog. Peptides. 1990;11:789–795. doi: 10.1016/0196-9781(90)90196-c. [DOI] [PubMed] [Google Scholar]
- 115.Baptista V, Browning KN, Travagli RA. Effects of cholecystokinin-8s in the nucleus tractus solitarius of vagally deafferented rats. Am J Physiol Regul Integr Comp Physiol. 2007;292:R1092–R1100. doi: 10.1152/ajpregu.00517.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sayegh AI, Ritter RC. Vagus nerve participates in CCK-induced Fos expression in hind brain but not myenteric plexus. Brain Res. 2000;878:155–162. doi: 10.1016/s0006-8993(00)02731-1. [DOI] [PubMed] [Google Scholar]
- 117.van de Wall EH, Duffy P, Ritter RC. CCK enhances response to gastric distension by acting on capsaicin-insensitive vagal afferents. Am J Physiol Regul Integr Comp Physiol. 2005;289:R695–R703. doi: 10.1152/ajpregu.00809.2004. [DOI] [PubMed] [Google Scholar]
- 118.Viard E, Zheng Z, Wan S, Travagli RA. Vagally-mediated, non paracrine effects of cholecystokinin-8s on rat pancreatic exocrine secretion. Am J Physiol Gastrointest Liver Physiol. 2007;293:G494–G500. doi: 10.1152/ajpgi.00118.2007. [DOI] [PubMed] [Google Scholar]
- 119.Branchereau P, Champagnat J, Denavit-Saubie M. Cholecystokinin-gated currents in neurons of the rat solitary complex in vitro. J Neurophysiol. 1993;70:2584–2595. doi: 10.1152/jn.1993.70.6.2584. [DOI] [PubMed] [Google Scholar]
- 120.Baptista V, Zheng Z, Coleman FH, Rogers RC, Travagli RA. Cholecystokinin octapeptide increases spontaneous glutamatergic synaptic transmission to neurons of the nucleus tractus solitarius centralis. J Neurophysiol. 2005;94:2763–2771. doi: 10.1152/jn.00351.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Appleyard SM, et al. Proopiomelanocortin neurons in nucleus tractus solitarius are activated by visceral afferents: regulation by cholecystokinin and opioids. J Neurosci. 2005;25:3578–3585. doi: 10.1523/JNEUROSCI.4177-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Browning KN, Wan S, Baptista V, Travagli RA. Vanilloid, purinergic, and CCK receptors activate glutamate release on single neurons of the nucleus tractus solitarius centralis. Am J Physiol Regul Integr Comp Physiol. 2011;301:R394–R401. doi: 10.1152/ajpregu.00054.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zheng Z, Lewis MW, Travagli R. A In vitro analysis of the effects of cholecystokinin (CCK) on rat brainstem motorneurons. Am J Physiol Gastrointest Liver Physiol. 2005;288:G1066–G1073. doi: 10.1152/ajpgi.00497.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Plata-Salaman CR, Fukuda A, Oomura Y, Minami T. Effects of sulphated cholecystokinin octapeptide (CCK-8) on the dorsal motor nucleus of the vagus. Brain Res Bull. 1988;21:839–842. doi: 10.1016/0361-9230(88)90054-8. [DOI] [PubMed] [Google Scholar]
- 125.Wan S, Coleman FH, Travagli RA. Cholecystokinin-8s excites identified rat pancreatic-projecting vagal motoneurons. Am J Physiol Gastrointest Liver Physiol. 2007;293:G484–G492. doi: 10.1152/ajpgi.00116.2007. [DOI] [PubMed] [Google Scholar]
- 126.Simasko SM, Ritter RC. Cholecystokinin activates both A- and C-type vagal afferent neurons. Am J Physiol Gastrointest Liver Physiol. 2003;285:G1204–G1213. doi: 10.1152/ajpgi.00132.2003. [DOI] [PubMed] [Google Scholar]
- 127.Derbenev AV, Monroe MJ, Glatzer NR, Smith BN. Vanilloid-mediated heterosynaptic facilitation of inhibitory synaptic input to neurons of the rat dorsal motor nucleus of the vagus. J Neurosci. 2006;26:9666–9672. doi: 10.1523/JNEUROSCI.1591-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Peters JH, McDougall SJ, Fawley JA, Smith SM, Andresen MC. Primary afferent activation of thermosensitive TRPV1 triggers asynchronous glutamate release at central neurons. Neuron. 2010;65:657–669. doi: 10.1016/j.neuron.2010.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Evans C, Baxi S, Neff R, Venkatesan P, Mendelowitz D. Synaptic activation of cardiac vagal neurons by capsaicin sensitive and insensitive sensory neurons. Brain Res. 2003;979:210–215. doi: 10.1016/s0006-8993(03)02937-8. [DOI] [PubMed] [Google Scholar]
- 130.Roth GI, Yamamoto WS. The microcirculation of the area postrema of the rat. J Comp Neurol. 1968;133:329–340. doi: 10.1002/cne.901330304. [DOI] [PubMed] [Google Scholar]
- 131.Dockray GJ. Immunochemical evidence of cholecystokinin-like peptides in brain. Nature. 1976;264:568–570. doi: 10.1038/264568a0. [DOI] [PubMed] [Google Scholar]
- 132.Takagi H, et al. Fine structural studies of cholecystokinin-8-like immunoreactive neurons and axon terminals in the nucleus of tractus solitarius of the rat. J Comp Neurol. 1984;227:369–379. doi: 10.1002/cne.902270307. [DOI] [PubMed] [Google Scholar]
- 133.Holmes GM, Tong M, Travagli RA. Effects of brainstem cholecystokinin-8s on gastric tone and esophageal-gastric reflex. Am J Physiol Gastrointest Liver Physiol. 2009;296:G621–G631. doi: 10.1152/ajpgi.90567.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Stanley S, Wynne K, McGowan B, Bloom S. Hormonal regulation of food intake. Physiol Rev. 2005;85:1131–1158. doi: 10.1152/physrev.00015.2004. [DOI] [PubMed] [Google Scholar]
- 135.Date Y, et al. The role of the gastric afferent vagal nerve in ghrelin-induced feeding and growth hormone secretion in rats. Gastroenterology. 2002;123:1120–1128. doi: 10.1053/gast.2002.35954. [DOI] [PubMed] [Google Scholar]
- 136.Holmes GM, Browning KN, Tong M, Qualls-Creekmore E, Travagli RA. Vagally mediated effects of glucagon-like peptide 1: in vitro and in vivo gastric actions. J Physiol. 2009;587:4749–4759. doi: 10.1113/jphysiol.2009.175067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kakei M, Yada T, Nakagawa A, Nakabayashi H. Glucagon-like peptide-1 evokes action potentials and increases cytosolic Ca2+ in rat nodose ganglion neurons. Auton Neurosci. 2002;102:39–44. doi: 10.1016/s1566-0702(02)00182-0. [DOI] [PubMed] [Google Scholar]
- 138.Wan S, Coleman FH, Travagli RA. Glucagon-like peptide-1 (GLP-1) excites pancreas-projecting preganglionic vagal motoneurons. Am J Physiol Gastrointest Liver Physiol. 2007;292:G1474–G1482. doi: 10.1152/ajpgi.00562.2006. [DOI] [PubMed] [Google Scholar]
- 139.Grabauskas G, et al. KATP channels in the nodose ganglia mediate the orexigenic actions of ghrelin. J Physiol. 2015;593:3973–3989. doi: 10.1113/JP270788. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 140.Arnold M, Mura A, Langhans W, Geary N. Gut vagal afferents are not necessary for the eating-stimulatory effect of intraperitoneally injected ghrelin in the rat. J Neurosci. 2006;26:11052–11060. doi: 10.1523/JNEUROSCI.2606-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Fry M, Ferguson AV. Ghrelin modulates electrical activity of area postrema neurons. Am J Physiol Regul Integr Comp Physiol. 2008;296:R485–R492. doi: 10.1152/ajpregu.90555.2008. [DOI] [PubMed] [Google Scholar]
- 142.Li Y, Wu X, Zhao Y, Chen S, Owyang C. Ghrelin acts on the dorsal vagal complex to stimulate pancreatic protein secretion. Am J Physiol Gastrointest Liver Physiol. 2006;290:G1350–G1358. doi: 10.1152/ajpgi.00493.2005. [DOI] [PubMed] [Google Scholar]
- 143.Holzer P, Reichmann F, Farzi A. Neuropeptide Y, peptide YY and pancreatic polypeptide in the gut–brain axis. Neuropeptides. 2012;46:261–274. doi: 10.1016/j.npep.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Michel MC, et al. XVI. International union of pharmacology reccommendations for the nomenclature of neuropeptide Y, peptide YY, and pancreatic polypeptide receptors. Pharmacol Rev. 1999;50:143–150. [PubMed] [Google Scholar]
- 145.Rozengurt E, Sternini C. Taste receptor signaling in the mammalian gut. Curr Opin Pharmacol. 2007;7:557–562. doi: 10.1016/j.coph.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Maljaars PW, Peters HP, Mela DJ, Masclee AA. Ileal brake: a sensible food target for appetite control. A review. Physiol Behav. 2008;95:271–281. doi: 10.1016/j.physbeh.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 147.Chen CH, Stephens RL, Jr, Rogers RC. PYY and NPY control of gastric motility via action on Y1 and Y2 receptors in the DVC. Neurogastroenterol Motil. 1997;9:109–116. doi: 10.1046/j.1365-2982.1997.d01-26.x. [DOI] [PubMed] [Google Scholar]
- 148.Chen CH, Rogers RC. Central inhibitory action of peptide YY on gastric motility in rats. Am J Physiol. 1995;269:R787–R792. doi: 10.1152/ajpregu.1995.269.4.R787. [DOI] [PubMed] [Google Scholar]
- 149.Yang H, Li WP, Reeve JR, Rivier J, Tache Y. PYY-preferring receptor in the dorsal vagal complex and its involvement in PYY stimulation in gastric acid secretion in rats. Br J Pharmacol. 1998;123:1549–1554. doi: 10.1038/sj.bjp.0701767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Adrian TE, et al. Effect of peptide YY on gastric, pancreatic, and biliary function in humans. Gastroenterology. 1985;89:494–499. doi: 10.1016/0016-5085(85)90442-1. [DOI] [PubMed] [Google Scholar]
- 151.Yang H, et al. Peripheral PYY inhibits intracisternal TRH-induced gastric acid secretion by acting in the brain. Am J Physiol Gastrointest Liver Physiol. 2000;279:G575–G581. doi: 10.1152/ajpgi.2000.279.3.G575. [DOI] [PubMed] [Google Scholar]
- 152.Schemann M, Tamura K. Presynaptic inhibitory effects of the peptides NPY, PYY and PP on nicotinic EPSPs in guinea-pig gastric myenteric neurones. J Physiol. 1992;451:79–89. doi: 10.1113/jphysiol.1992.sp019154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Avau B, Carbone F, Tack J, Depoortere I. Ghrelin signaling in the gut, its physiological properties, and therapeutic potential. Neurogastroenterol Motil. 2013;25:720–732. doi: 10.1111/nmo.12193. [DOI] [PubMed] [Google Scholar]
- 154.Latorre R, Sternini C, De GR, Greenwood-van MB. Enteroendocrine cells: a review of their role in brain–gut communication. Neurogastroenterol Motil. 2016;28:620–630. doi: 10.1111/nmo.12754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Stengel A, Tache Y. Corticotropin-releasing factor signaling and visceral response to stress. Exp Biol Med (Maywood) 2010;235:1168–1178. doi: 10.1258/ebm.2010.009347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Stengel A, Tache Y. Neuroendocrine control of the gut during stress: corticotropin-releasing factor signaling pathways in the spotlight. Annu Rev Physiol. 2008;71:219–239. doi: 10.1146/annurev.physiol.010908.163221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Fukudo S. IBS: autonomic dysregulation in IBS. Nat Rev Gastroenterol Hepatol. 2013;10:569–571. doi: 10.1038/nrgastro.2013.166. [DOI] [PubMed] [Google Scholar]
- 158.Khoo J, Rayner CK, Feinle-Bisset C, Jones KL, Horowitz M. Gastrointestinal hormonal dysfunction in gastroparesis and functional dyspepsia. Neurogastroenterol Motil. 2010;22:1270–1278. doi: 10.1111/j.1365-2982.2010.01609.x. [DOI] [PubMed] [Google Scholar]
- 159.Franklin TB, Saab BJ, Mansuy IM. Neural mechanisms of stress resilience and vulnerability. Neuron. 2012;75:747–761. doi: 10.1016/j.neuron.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 160.Panksepp J, Panksepp JB. Toward a cross-species understanding of empathy. Trends Neurosci. 2013;36:489–496. doi: 10.1016/j.tins.2013.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kelly AM, Goodson JL. Social functions of individual vasopressin-oxytocin cell groups in vertebrates: what do we really know? Front Neuroendocrinol. 2014;35:512–529. doi: 10.1016/j.yfrne.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 162.Ulrich-Lai YM, Herman JP. Neural regulation of endocrine and autonomic stress responses. Nat Rev Neurosci. 2009;10:397–409. doi: 10.1038/nrn2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Churchland PS, Winkielman P. Modulating social behavior with oxytocin: how does it work? What does it mean? Horm Behav. 2012;61:392–399. doi: 10.1016/j.yhbeh.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Gordon I, Martin C, Feldman R, Leckman JF. Oxytocin and social motivation. Dev Cogn Neurosci. 2011;1:471–493. doi: 10.1016/j.dcn.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Zheng J, et al. Hypothalamic oxytocin mediates adaptation mechanism against chronic stress in rats. Am J Physiol Gastrointest Liver Physiol. 2010;299:G946–G953. doi: 10.1152/ajpgi.00483.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Babygirija R, Zheng J, Ludwig K, Takahashi T. Central oxytocin is involved in restoring impaired gastric motility following chronic repeated stress in mice. Am J Physiol Regul Integr Comp Physiol. 2010;298:R157–R165. doi: 10.1152/ajpregu.00328.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Bulbul M, Babygirija R, Ludwig K, Takahashi T. Central oxytocin attenuates augmented gastric postprandial motility induced by restraint stress in rats. Neurosci Lett. 2010;479:302–306. doi: 10.1016/j.neulet.2010.05.085. [DOI] [PubMed] [Google Scholar]
- 168.Babygirija R, Bulbul M, Cerjak D, Ludwig K, Takahashi T. Sustained acceleration of colonic transit following chronic homotypic stress in oxytocin knockout mice. Neurosci Lett. 2011;495:77–81. doi: 10.1016/j.neulet.2011.03.045. [DOI] [PubMed] [Google Scholar]
- 169.Bulbul M, et al. Hypothalamic oxytocin attenuates CRF expression via GABAA receptors in rats. Brain Res. 2011;1387:39–45. doi: 10.1016/j.brainres.2011.02.091. [DOI] [PubMed] [Google Scholar]
- 170.Murphy D, et al. The hypothalamic–neurohypophyseal system: from genome to physiology. J Neuroendocrinol. 2012;24:539–553. doi: 10.1111/j.1365-2826.2011.02241.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Richar P, Moos F, Freund-Mercier MJ. Central effects of oxytocin. Physiol Rev. 1991;71:331–370. doi: 10.1152/physrev.1991.71.2.331. [DOI] [PubMed] [Google Scholar]
- 172.Herman JP, Flak J, Jankord R. Chronic stress plasticity in the hypothalamic paraventricular nucleus. Prog Brain Res. 2008;170:353–364. doi: 10.1016/S0079-6123(08)00429-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Raggenbass M, Dubois-Dauphin M, Charpak S, Dreifuss JJ. Neurons in the dorsal motor nucleus of the vagus nerve are excited by oxytocin in the rat but not in the guinea pig. Proc Natl Acad Sci USA. 1987;84:3926–3930. doi: 10.1073/pnas.84.11.3926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Raggenbass M, Dreifuss JJ. Mechanism of action of oxytocin in rat vagal neurones: induction of a sustained sodium-dependent current. J Physiol. 1992;457:131–142. doi: 10.1113/jphysiol.1992.sp019368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Flanagan LM, Olson BR, Sved AF, Verbalis JG, Stricker EM. Gastric motility in conscious rats given oxytocin and an oxytocin antagonist centrally. Brain Res. 1992;578:256–260. doi: 10.1016/0006-8993(92)90255-8. [DOI] [PubMed] [Google Scholar]
- 176.Fujimiya M, Inui A. Peptidergic regulation of gastrointestinal motility in rodents. Peptides. 2001;21:1565–1582. doi: 10.1016/s0196-9781(00)00313-2. [DOI] [PubMed] [Google Scholar]
- 177.Holmes GM, et al. Vagal afferent fibres determine the oxytocin-induced modulation of gastric tone. J Physiol. 2013;591:3081–3100. doi: 10.1113/jphysiol.2013.253732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Babygirija R, Bulbul M, Yoshimoto S, Ludwig K, Takahashi T. Central and peripheral release of oxytocin following chronic homotypic stress in rats. Auton Neurosci. 2012;167:56–60. doi: 10.1016/j.autneu.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 179.Lewis MW, Hermann GE, Rogers RC, Travagli R. A In vitro and in vivo analysis of the effects of corticotropin releasing factor on rat dorsal vagal complex. J Physiol. 2002;543:135–146. doi: 10.1113/jphysiol.2002.019281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Browning KN, et al. Plasticity in the brainstem vagal circuits controlling gastric motor function triggered by corticotropin releasing factor. J Physiol. 2014;592:4591–4605. doi: 10.1113/jphysiol.2014.278192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Blake CB, Smith BN. cAMP-dependent insulin modulation of synaptic inhibition in neurons of the dorsal motor nucleus of the vagus is altered in diabetic mice. Am J Physiol Regul Integr Comp Physiol. 2014;307:R711–R720. doi: 10.1152/ajpregu.00138.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Shuster SJ, Riedl M, Li X, Vulchanova L, Elde R. Stimulus-dependent translocation of κ opioid receptors to the plasma membrane. J Neurosci. 1999;19:2658–2664. doi: 10.1523/JNEUROSCI.19-07-02658.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Baltadzhieva R, Gurevich T, Korczyn AD. Autonomic impairment in amyotrophic lateral sclerosis. Curr Opin Neurol. 2005;18:487–493. doi: 10.1097/01.wco.0000183114.76056.0e. [DOI] [PubMed] [Google Scholar]
- 184.Slim M, Calandre EP, Rico-Villademoros F. An insight into the gastrointestinal component of fibromyalgia: clinical manifestations and potential underlying mechanisms. Rheumatol Int. 2015;35:433–444. doi: 10.1007/s00296-014-3109-9. [DOI] [PubMed] [Google Scholar]
- 185.Aziz NA, et al. Weight loss in neurodegenerative disorders. J Neurol. 2008;255:1872–1880. doi: 10.1007/s00415-009-0062-8. [DOI] [PubMed] [Google Scholar]
- 186.Heemskerk AW, Roos RA. Dysphagia in Huntington’s disease: a review. Dysphagia. 2011;26:62–66. doi: 10.1007/s00455-010-9302-4. [DOI] [PubMed] [Google Scholar]
- 187.Fasano A, Visanji NP, Liu LW, Lang AE, Pfeiffer RF. Gastrointestinal dysfunction in Parkinson’s disease. Lancet Neurol. 2015;14:625–639. doi: 10.1016/S1474-4422(15)00007-1. [DOI] [PubMed] [Google Scholar]
- 188.Pfeiffer RF. Gastrointestinal involvement in Parkinson’s disease: the horse or the cart. Acta Physiol (Oxf) 2014;211:271–272. doi: 10.1111/apha.12300. [DOI] [PubMed] [Google Scholar]
- 189.Natale G, Pasquali L, Ruggieri S, Paparelli A, Fornai F. Parkinson’s disease and the gut: a well known clinical association in need of an effective cure and explanation. Neurogastroenterol Motil. 2008;20:741–749. doi: 10.1111/j.1365-2982.2008.01162.x. [DOI] [PubMed] [Google Scholar]
- 190.Wedel T, et al. Enteric nerves and interstitial cells of Cajal are altered in patients with slow-transit constipation and megacolon. Gastroenterology. 2002;123:1459–1467. doi: 10.1053/gast.2002.36600. [DOI] [PubMed] [Google Scholar]
- 191.Lebouvier T, et al. Pathological lesions in colonic biopsies during Parkinson’s disease. Gut. 2008;57:1741–1743. doi: 10.1136/gut.2008.162503. [DOI] [PubMed] [Google Scholar]
- 192.Edwards LL, Quigley EM, Harned RK, Hofman R, Pfeiffer RF. Characterization of swallowing and defecation in Parkinson’s disease. Am J Gastroenterol. 1994;89:15–25. [PubMed] [Google Scholar]
- 193.Pfeiffer RF. Gastrointestinal dysfunction in Parkinson’s disease. Lancet Neurol. 2003;2:107–116. doi: 10.1016/s1474-4422(03)00307-7. [DOI] [PubMed] [Google Scholar]
- 194.Hardoff R, et al. Gastric emptying time and gastric motility in patients with Parkinson’s disease. Mov Disord. 2001;16:1041–1047. doi: 10.1002/mds.1203. [DOI] [PubMed] [Google Scholar]
- 195.McDowell K, Chesselet MF. Animal models of the non-motor features of Parkinson’s disease. Neurobiol Dis. 2012;46:597–606. doi: 10.1016/j.nbd.2011.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Kuo YM, et al. Extensive enteric nervous system abnormalities in mice transgenic for artificial chromosomes containing Parkinson disease-associated α-synuclein gene mutations precede central nervous system changes. Hum Mol Genet. 2010;19:1633–1650. doi: 10.1093/hmg/ddq038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Blandini F, et al. Functional and neurochemical changes of the gastrointestinal tract in a rodent model of Parkinson’s disease. Neurosci Lett. 2009;467:203–207. doi: 10.1016/j.neulet.2009.10.035. [DOI] [PubMed] [Google Scholar]
- 198.Colucci M, et al. Intestinal dysmotility and enteric neurochemical changes in a Parkinson’s disease rat model. Auton Neurosci. 2012;169:77–86. doi: 10.1016/j.autneu.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 199.Derkinderen P, et al. Parkinson disease: the enteric nervous system spills its guts. Neurology. 2011;77:1761–1767. doi: 10.1212/WNL.0b013e318236ef60. [DOI] [PubMed] [Google Scholar]
- 200.Zheng LF, et al. Alterations in TH- and ChAT-immunoreactive neurons in the DMV and gastric dysmotility in an LPS-induced PD rat model. Auton Neurosci. 2013;177:194–198. doi: 10.1016/j.autneu.2013.04.012. [DOI] [PubMed] [Google Scholar]
- 201.Stott SR, Barker RA. Time course of dopamine neuron loss and glial response in the 6-OHDA striatal mouse model of Parkinson’s disease. Eur J Neurosci. 2014;39:1042–1056. doi: 10.1111/ejn.12459. [DOI] [PubMed] [Google Scholar]
- 202.Zhu HC, Zhao J, Luo CY, Li QQ. Gastrointestinal dysfunction in a Parkinson’s disease rat model and the changes of dopaminergic, nitric oxidergic, and cholinergic neurotransmitters in myenteric plexus. J Mol Neurosci. 2012;47:15–25. doi: 10.1007/s12031-011-9560-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Annerino DM, et al. Parkinson’s disease is not associated with gastrointestinal myenteric ganglion neuron loss. Acta Neuropathol. 2012;124:665–680. doi: 10.1007/s00401-012-1040-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Toti L, Travagli RA. Gastric dysregulation induced by microinjection of 6-OHDA in the substantia nigra pars compacta of rats is determined by alterations in the brain–gut axis. Am J Physiol Gastrointest Liver Physiol. 2014;307:G1013–G1023. doi: 10.1152/ajpgi.00258.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Goedert M, Spillantini MG, Del TK, Braak H. 100 years of Lewy pathology. Nat Rev Neurol. 2013;9:13–24. doi: 10.1038/nrneurol.2012.242. [DOI] [PubMed] [Google Scholar]
- 206.George JM. The synucleins. Genome Biol. 2002;3:3002.1–3002.6. doi: 10.1186/gb-2001-3-1-reviews3002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Wakabayashi K, Takahashi H, Ohama E, Ikuta F. Parkinson’s disease: an immunohistochemical study of Lewy body-containing neurons in the enteric nervous system. Acta Neuropathol. 1990;79:581–583. doi: 10.1007/BF00294234. [DOI] [PubMed] [Google Scholar]
- 208.Braak H, De Vos RA, Bohl J, Del Tredici K. Gastric α-synuclein immunoreactive inclusions in Meissner’s and Auerbach’s plexuses in cases staged for Parkinson’s disease-related brain pathology. Neurosci Lett. 2006;396:67–72. doi: 10.1016/j.neulet.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 209.Hawkes CH, Del TK, Braak H. A timeline for Parkinson’s disease. Parkinsonism Relat Disord. 2010;16:79–84. doi: 10.1016/j.parkreldis.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 210.Visanji NP, Brooks PL, Hazrati LN, Lang AE. The prion hypothesis in Parkinson’s disease: Braak to the future. Acta Neuropathol Commun. 2013;1:2. doi: 10.1186/2051-5960-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Braak H, Rub U, Gai WP, Del Tredici K. Idiopathic Parkinson’s disease: possible routes by which vulnerable neuronal types may be subject to neuroinvasion by an unknown pathogen. J Neural Transm. 2003;110:517–536. doi: 10.1007/s00702-002-0808-2. [DOI] [PubMed] [Google Scholar]
- 212.Zheng LF, et al. The role of the vagal pathway and gastric dopamine in the gastroparesis of rats after a 6-hydroxydopamine microinjection in the substantia nigra. Acta Physiol (Oxf) 2014;211:434–446. doi: 10.1111/apha.12229. [DOI] [PubMed] [Google Scholar]
- 213.Braak H, et al. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging. 2003;24:197–211. doi: 10.1016/s0197-4580(02)00065-9. [DOI] [PubMed] [Google Scholar]
- 214.Greene JG. Causes and consequences of degeneration of the dorsal motor nucleus of the vagus nerve in Parkinson’s disease. Antioxid Redox Signal. 2014;21:649–667. doi: 10.1089/ars.2014.5859. [DOI] [PubMed] [Google Scholar]
- 215.Burke RE, Dauer WT, Vonsattel JP. A critical evaluation of the Braak staging scheme for Parkinson’s disease. Ann Neurol. 2008;64:485–491. doi: 10.1002/ana.21541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Kalaitzakis ME, Graeber MB, Gentleman SM, Pearce RK. The dorsal motor nucleus of the vagus is not an obligatory trigger site of Parkinson’s disease: a critical analysis of α-synuclein staging. Neuropathol Appl Neurobiol. 2008;34:284–295. doi: 10.1111/j.1365-2990.2007.00923.x. [DOI] [PubMed] [Google Scholar]
- 217.Brettschneider J, Del TK, Lee VM, Trojanowski JQ. Spreading of pathology in neurodegenerative diseases: a focus on human studies. Nat Rev Neurosci. 2015;16:109–120. doi: 10.1038/nrn3887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Hawkes CH, Del TK, Braak H. Parkinson’s disease: the dual hit theory revisited. Ann NY Acad Sci. 2009;1170:615–622. doi: 10.1111/j.1749-6632.2009.04365.x. [DOI] [PubMed] [Google Scholar]
- 219.Buckinx R, Adriaensen D, Nassauw LV, Timmermans JP. Corticotrophin-releasing factor, related peptides, and receptors in the normal and inflamed gastrointestinal tract. Front Neurosci. 2011;5:54. doi: 10.3389/fnins.2011.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Bale TL, Vale WW. CRF and CRF receptors: role in stress responsivity and other behaviors. Annu Rev Pharmacol Toxicol. 2004;44:525–557. doi: 10.1146/annurev.pharmtox.44.101802.121410. [DOI] [PubMed] [Google Scholar]
- 221.Valentino RJ, Pavcovich LA, Hirata H. Evidence for corticotropin-releasing hormone projections from Barrington’s nucleus to the periaqueductal gray and dorsal motor nucleus of the vagus in the rat. J Comp Neurol. 1995;363:402–422. doi: 10.1002/cne.903630306. [DOI] [PubMed] [Google Scholar]
- 222.Tache Y, Bonaz B. Corticotropin-releasing factor receptors and stress-related alterations of gut motor function. J Clin Invest. 2007;117:33–40. doi: 10.1172/JCI30085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Lenz HJ, Raedler A, Greten H, Vale WW, Rivier JE. Stress-induced gastrointestinal secretory and motor responses in rats are mediated by endogenous corticotropin-releasing factor. Gastroenterology. 1988;95:1510–1517. doi: 10.1016/s0016-5085(88)80070-2. [DOI] [PubMed] [Google Scholar]
- 224.Martinez V, Rivier J, Wang L, Tache Y. Central injecton of a new corticotropin-releasing factor (CRF) antagonist, astressin, blocks CRF- and stress-related alterations of gastric and colonic motor function. J Pharmacol Exp Ther. 1997;280:754–760. [PubMed] [Google Scholar]
- 225.Li JY, et al. Lewy bodies in grafted neurons in subjects with Parkinson’s disease suggest host-to-graft disease propagation. Nat Med. 2008;14:501–503. doi: 10.1038/nm1746. [DOI] [PubMed] [Google Scholar]
- 226.Goedert M, Falcon B, Clavaguera F, Tolnay M. Prion-like mechanisms in the pathogenesis of tauopathies and synucleinopathies. Curr Neurol Neurosci Rep. 2014;14:495. doi: 10.1007/s11910-014-0495-z. [DOI] [PubMed] [Google Scholar]
- 227.Goedert M. Alzheimer’s and Parkinson’s diseases: the prion concept in relation to assembled Aβ, tau, and α-synuclein. Science. 2015;349:1255555. doi: 10.1126/science.1255555. [DOI] [PubMed] [Google Scholar]
- 228.Desplats P, et al. Inclusion formation and neuronal cell death through neuron-to-neuron transmission of α-synuclein. Proc Natl Acad Sci USA. 2009;106:13010–13015. doi: 10.1073/pnas.0903691106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Olanow CW, Brundin P. Parkinson’s disease and alpha synuclein: is Parkinson’s disease a prion-like disorder? Mov Disord. 2013;28:31–40. doi: 10.1002/mds.25373. [DOI] [PubMed] [Google Scholar]
- 230.Hansen C, et al. α-synuclein propagates from mouse brain to grafted dopaminergic neurons and seeds aggregation in cultured human cells. J Clin Invest. 2011;121:715–725. doi: 10.1172/JCI43366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Lee HJ, et al. Direct transfer of α-synuclein from neuron to astroglia causes inflammatory responses in synucleinopathies. J Biol Chem. 2010;285:9262–9272. doi: 10.1074/jbc.M109.081125. [DOI] [PMC free article] [PubMed] [Google Scholar]