Abstract
We completed a meta-analysis to investigate the relationship between delusions in psychosis and 4 cognitive biases: “jumping to conclusions” (JTC), the “bias against disconfirmatory evidence” (BADE), the “bias against confirmatory evidence” (BACE), and “liberal acceptance” (LA). Building on recent meta-analyses we compared more narrowly defined groups. We identified 35 JTC, 8 BADE, 7 BACE, and 6 LA studies for inclusion. Groups with schizophrenia who were currently experiencing delusions demonstrated greater JTC, BADE, BACE, and LA than groups with schizophrenia who were not currently experiencing delusions, who in turn demonstrated no more JTC than healthy control groups. Hence JTC, BADE, BACE, and LA co-vary with delusions in cross-sectional samples of people with schizophrenia. Groups who were experiencing delusions due to other psychiatric illnesses also demonstrated greater JTC than healthy controls, and equivalent JTC to groups with schizophrenia currently experiencing delusions. Hence JTC is associated with delusions across a range of diagnoses. Groups with other, non-delusional psychiatric illnesses demonstrated less JTC, BADE, BACE, and LA than groups with schizophrenia currently experiencing delusions, less JTC than groups experiencing delusions due to other diagnoses, and no more JTC, BADE, BACE, or LA than healthy control groups. Hence JTC, BADE, BACE, and LA were not associated with psychiatric illnesses in general. Our results indicate all 4 biases are associated with delusions specifically rather than merely with a diagnosis of schizophrenia or with being psychiatrically ill, consistent with the possibility that they contribute to delusional severity.
Keywords: bias against disconfirmatory evidence, bias against confirmatory evidence, liberal acceptance, schizophrenia, delusional disorder, cognitive bias
Introduction
Two cognitive biases are reliably associated with delusions in schizophrenia. The first is the Jumping to Conclusions (JTC) bias, in which interpretations or judgments are made early and based on inadequate evidence.1 The second is the Bias Against Disconfirmatory Evidence (BADE), in which there is a failure to adequately re-evaluate an initial interpretation of events in the face of increasing evidence against that interpretation.2,3
The meaning of the association between JTC, BADE, and delusions in schizophrenia remains uncertain, however. It is plausible that JTC, BADE, and delusions arise independently as aspects of schizophrenia, and that JTC and BADE are merely spuriously related to delusions. Alternatively, such biases in perception and judgment may contribute to the formation and maintenance of delusions by affecting the manner in which evidence for ideas is weighted, accepted, or ignored.4 According to this hypothesis, JTC contributes to delusion formation through the early acceptance, with inadequate evidence, of incorrect hypotheses.5 BADE could contribute to the persistence and intractability of delusions by decreasing the likelihood that delusional beliefs will be re-evaluated when contrary evidence is provided.6
Despite the high face validity of the hypothesis that JTC and BADE contribute to delusion formation and maintenance, the evidence is mixed as to whether JTC and BADE are associated with delusions specifically (as a causal relationship would suggest), or merely with having schizophrenia (consistent with a spurious association). Two recent meta-analyses investigated the association of JTC with delusions. Dudley et al7 compared groups with mixed diagnoses (schizophrenia and delusional disorder) with healthy and psychiatric controls. Likewise, Ross et al8 assessed the relationship of JTC with delusions in mixed-diagnosis groups (schizophrenia, schizo-affective or bipolar disorder, major depression with delusions). However, by assessing JTC in mixed-diagnosis groups, neither meta-analysis clearly indicates whether JTC is associated with delusions in multiple diagnoses, or is only associated with delusions in schizophrenia. No BADE meta-analysis has previously been published. The present meta-analysis addresses these limitations, exploring whether JTC and BADE are together associated with current delusions in multiple diagnoses. The association of these biases with delusions in multiple diagnoses would demonstrate this relationship is not limited to schizophrenia, and would support a causal relationship.
JTC is most frequently measured by the beads task. Applying this task with people with schizophrenia, Huq et al9 showed participants 2 jars of colored beads. Each jar contained pink and green beads in an 85:15 ratio, with one jar containing mostly pink beads and the other mostly green beads. The jars were hidden from view and beads were drawn from one of the jars in a purportedly random but in fact pre-determined sequence. With each draw, participants were invited to indicate whether they had decided which jar (mostly pink or mostly green) beads were being drawn from. Huq et al9 found that participants with current delusions required fewer draws-to-decision (DTD) than those without current delusions, demonstrating a JTC bias. Variants of the beads task have utilized alternative stimuli, such as colored fish in lakes10,11 or emotionally-salient stimuli.12,13 Some versions of the task have incorporated an expanded instruction set to minimize potential miscomprehension regarding the nature of the task.14
To measure BADE, most studies have used the well-established procedure outlined by Woodward et al.15 Participants read a brief, ambiguous scenario and then rate and re-rate the plausibility of 4 interpretations as more evidence is provided. Two lure interpretations initially appear very plausible but become implausible as more evidence is provided; the true interpretation appears less plausible initially but, with more evidence, becomes the most plausible, and an “absurd” interpretation remains implausible throughout. Higher BADE is demonstrated when participants fail to adequately down-rate the plausibility of lure interpretations. Some earlier studies used successive pictures2 or fragmented pictures6 to present a disambiguating scenario. Typically 2 other biases are measured at the same time—a bias against confirmatory evidence (BACE), in which participants fail to adequately up-rate the plausibility of the true interpretation despite additional supporting evidence, and liberal acceptance (LA), where the plausibility of absurd interpretations is overrated.16 Principal Component Analysis has suggested BADE, BACE, and LA are nonindependent aspects of a single “evidence integration” cognitive process.2,3,17
While many studies have noted elevated JTC in schizophrenia samples, a much smaller number of studies have tested for a specific relationship with delusions by comparing schizophrenia samples with and without current delusions. In an early meta-analysis of 4 clinical studies, Fine et al18 found a significant relationship between JTC and delusions when comparing delusional vs non-delusional groups with schizophrenia, suggesting that JTC is specifically related to delusions rather than to schizophrenia generally. Some later studies have supported this finding,19–22 as did a recent systematic review1 (although many studies included in the review compared currently-deluded schizophrenia samples with non-delusional, non-schizophrenia samples, so that a schizophrenia diagnosis and the presence of delusions were confounded). JTC has also been associated with delusion-proneness in nonclinical samples,14,23,24 providing further tentative support for a causal relationship.
However, other studies comparing schizophrenia groups with vs without delusions have found no relationship between JTC and delusions beyond an association with schizophrenia itself,25,26 supporting a spurious explanation for the link between JTC and delusions. So et al27 tested whether JTC co-varied with delusional conviction over time in a year-long longitudinal study, but found no change in JTC even though delusional conviction decreased slightly. The change in delusional conviction over the duration of the study was small, however, and perhaps insufficient to be reflected in changes in bias.
With respect to BADE, the question of whether it is related to delusions specifically or merely with schizophrenia in general has not been investigated to the same depth as for JTC. Nevertheless, some studies found that BADE was related to delusional severity,3 and to delusions specifically rather than to a diagnosis of schizophrenia per se.2,17 In contrast, other studies have found no difference in BADE between schizophrenia samples with vs without current delusions.28,29
Overall the majority of studies support the possibility that JTC and BADE are meaningfully (and not merely spuriously) associated with delusions, however the literature is far from unanimous. As mentioned, 2 recent meta-analyses sought to address this problem. In their meta-analysis of between-groups and correlational studies, Dudley et al7 found a small difference in DTD between groups with schizophrenia who were and were not currently experiencing clinician-reported delusions, and a trend-level correlation between JTC and delusion severity in currently delusional samples with schizophrenia. This is consistent with a meaningful relationship, at least in the context of schizophrenia. However, when including other diagnoses with delusions as a symptom, such as delusional disorder, Dudley et al used a heterogeneous “psychosis” group, which included those with schizophrenia both with and without current delusions, plus those with delusional disorder. They compared this heterogeneous group with healthy and psychiatric controls, but it is unclear whether elevated JTC in this group was related to delusions only for those with schizophrenia, or for those with other diagnoses also. By considering such groups separately, our meta-analysis is able to assess whether JTC is associated with delusions in the context of multiple diagnoses, a key prediction of the hypothesis that JTC contributes to delusion severity.
Similarly, in a meta-analysis of correlational studies, Ross et al8 found a small correlation between JTC and self-reported delusional ideation in clinical and non-clinical samples, although it was not significant in the key current-delusions subgroup (probably due to the small number of studies that met their inclusion criteria). Again this finding is consistent with the possibility of a meaningful relationship between JTC and delusions. However Ross et al also used a heterogeneous clinical sample which included diagnoses of schizophrenia, schizo-affective or bipolar disorder, and major depression with delusions, and it is unclear whether JTC was associated with delusions across multiple diagnoses, or only associated with delusions in schizophrenia.
We build on the meta-analyses of Ross el al8 and Dudley et al7 by making comparisons between more narrowly-defined groups, allowing us to address in detail when and for whom cognitive biases are related to delusions. Specifically, we compared groups with schizophrenia with and without current delusions, groups with current delusions due to non-schizophrenia diagnoses, groups without delusions but with other psychiatric diagnoses, and healthy control groups.
The comparison of groups with schizophrenia with and without current delusions deserves additional consideration. One prediction of the causal hypothesis would be that cognitive biases co-vary with delusion severity over time. A meta-analysis of longitudinal studies would provide the ideal test of this, but few longitudinal studies are available. Nevertheless, cross-sectional data comparing groups with schizophrenia with and without current delusions may be used to approximate a longitudinal comparison, due to the high prevalence of delusions during psychotic episodes, and the alternation of psychotic episodes with periods of recovery or remission over the course of illness.30–32 Clinically significant delusions are a common symptom of schizophrenia, and may be experienced by over 70% of people during psychotic episodes,33 though rates as high as 97% were reported in one study.34 Yet psychotic symptoms may remit for a time in as many as 88% of people with schizophrenia within a 12-month period.35 Hence the majority of those with schizophrenia who are in remission and not currently experiencing delusions will have experienced a longitudinal decrease in delusional severity.
We made 3 key comparisons, as follows. (1) We compared groups with schizophrenia with and without current delusions (and compared the latter with healthy control groups), to determine whether the biases co-vary with delusions and illness severity, and might therefore causally contribute to delusions during acute phases. (2) We compared groups currently experiencing delusions due to non-schizophrenia diagnoses with other groups, to determine whether the biases are associated with delusions across multiple diagnoses, or perhaps spuriously associated with delusions only in the context of schizophrenia. (3) Finally, we compared groups that are psychiatrically ill but not experiencing delusions with other groups, to determine whether these biases could simply be associated with being psychiatrically ill. By estimating how JTC and BADE are differentially associated with schizophrenia, delusions, illness, and health, we inform the question of whether and how cognitive bias is related to delusions.
While JTC and BADE have both been associated with delusions, they are usually studied in isolation. They have not been investigated meta-analytically together, and indeed no BADE meta-analysis exists to date. By including BADE, BACE, and LA along with JTC in the current meta-analysis we hope to draw broader conclusions regarding their possible role in delusion formation and maintenance.
Method
Selection Criteria
JTC studies were included if they used the beads task or its variants (fish/lakes or emotionally-salient stimuli—JTC is observed at similar strength for both neutral and emotionally-salient tasks),36 and reported group mean DTD or the within-group correlation between DTD and delusion severity. Data from tasks of all ratios were accepted, as Ross et al8 found that bead ratio did not moderate the relationship between JTC and delusion strength. BADE studies which used either the ambiguous scenarios task15 or a similar task using ambiguous pictures2,6 were included.
For both JTC and BADE, studies were included only if they compared currently delusional and currently non-delusional groups with schizophrenia, or compared one of these groups with delusions not due to schizophrenia, non-delusional psychiatric, or healthy control groups. Groups with either delusional disorder or major depressive disorder with delusions22 were included as having current delusions not due to schizophrenia. Groups with current delusions and mixed diagnoses (schizophrenia and delusional disorder etc.) were included as having schizophrenia with current delusions if schizophrenia was the majority diagnosis.12,22,37,38 Similar to previous meta-analyses,7,8 no distinction was made among delusion subtypes.
Longitudinal JTC data were included when participants who were currently experiencing delusions at baseline were no longer experiencing delusions at follow-up.38,39 Only baseline data were used from longitudinal studies in which participants were still experiencing delusions at follow-up.40,41 There were no BADE longitudinal studies.
Search Strategy
JTC studies and unpublished data meeting our selection criteria were identified from the recent comprehensive literature search completed by Dudley et al,7 from Garety and Freeman,1 and from a search of the Pubmed and PsycINFO databases using the search terms delusions, schizophrenia, psychosis, or paranoia, in combination with jump(ing) to conclusions or JTC.
BADE studies were identified from a search of the Pubmed and PsycINFO databases, using the search terms delusions, schizophrenia, psychosis, or paranoia, in combination with bias against disconfirmatory evidence, bias against confirmatory evidence, BADE, BACE, or evidence integration. Additional data were requested from the authors of BADE studies that appeared to meet the inclusion criteria but did not report adequate descriptive statistics. Data from included JTC and BADE studies were coded by the lead author.
Statistical Methods
JTC was operationalized as the mean DTD,7 when available, for both neutral and emotionally-salient stimuli. BADE was calculated as the mean change in plausibility rating of lure interpretations between the first and last piece of evidence,15 BACE as the change in plausibility rating of true interpretations between the first and last piece of evidence, and LA as the average plausibility rating of absurd interpretations. Several studies have alternatively operationalized LA as the willingness to make a decision for a plausible option based on lower-than-average confidence.42–44 While informative, these studies were not included in our meta-analysis because of fundamental differences in the way in which LA was measured.
Cohen’s d effect size was calculated for each cognitive bias contrast using the between-groups method45 for both between-groups and repeated-measures studies, and arithmetically averaged when multiple effect sizes were reported. Correlations (including Spearman’s ρ) were converted to Cohen’s d according to the method of Rosnow and Rosenthal,46 and group sizes of half the original group rounded down to the nearest whole number were recorded to account for dichotomization. Data from healthy delusion-prone and non-delusion-prone subgroups were recombined by weighted mean averaging and the pooling of standard deviations. All Cohen’s ds were then corrected to unbiased Hedges’ g.47
Hedges’ g were combined in a random-effects meta-analysis48 using the Exploratory Software for Confidence Intervals (ESCI) to determine an overall effect size for each comparison. In addition the likelihood of publication bias in the schizophrenia with current delusions vs healthy controls, and schizophrenia with and without current delusions comparisons was assessed by visual inspection of funnel-plot symmetry.
Results
Included Studies
Thirty-four of 54 JTC studies from Dudley et al7 met our inclusion criteria. One further study22 was identified for inclusion from Garety and Freeman,1 but no additional papers were identified via the Pubmed and PsycINFO databases on October 21, 2015. The 35 included JTC studies and their published contrasts are listed in table 1.
Table 1.
Included JTC Studies, Comparisons, and Effect-Size Measures
| Source | Comparisona | |||||||
|---|---|---|---|---|---|---|---|---|
| SD/HC | SD/SND | SND/HC | PD/HC | SD/PD | SD/PND | PD/PND | PND/HC | |
| Andreou et al49 | g b | |||||||
| Andreou et al50 | g | |||||||
| Baskak et al51 | g | |||||||
| Bentall et al21 | g | g | g | g | g | |||
| Buck et al52 | r | |||||||
| Colbert et al53 | g | g | g | |||||
| Conway et al54 | g | |||||||
| Corcoran et al22 | g | g | g | g | g | g | g | g |
| Dudley et al13 | g | g | g | |||||
| Dudley et al55 | g | g | g | |||||
| Dudley et al56 | g | |||||||
| Fear and Healy57 | g | g | g | |||||
| Fraser et al37 | g | g | g | |||||
| Garety et al58 | g | g | g | g | g | g | ||
| Huq et al9 | g | g | g | |||||
| Jacobsen et al36 | g | g | g | |||||
| Langdon et al59 | ρ | ρ | ||||||
| Langdon et al19 | r | |||||||
| Lim et al60 | r | |||||||
| Lincoln et al61 | g | g | g | |||||
| Menon et al25 | g | g | g | |||||
| Menon et al39,c | g | |||||||
| Menon et al26 | g | |||||||
| Moritz & Woodward62 | g | g | g | g | g | |||
| Mortimer et al63 | r | |||||||
| Peters & Garety38,c | g | g | g | g | g | |||
| Peters et al64 | g | |||||||
| Ross et al40 | g | |||||||
| So & Kwok65 | g | |||||||
| Startup et al66 | g | |||||||
| van der Gaag et al20 | r | |||||||
| Waller et al41 | r | |||||||
| Warman et al67 | g | |||||||
| Warman et al68 | r | |||||||
| Wittorf et al69 | r | g | ||||||
| Total participants (n) | 1131 | 834 | 385 | 152 | 86 | 409 | 123 | 558 |
| Total studies (k) | 21 | 20 | 7 | 4 | 2 | 10 | 3 | 12 |
| Heterogeneity variance (I2) | 58.2% | 0.0% | 47.3% | 0.0% | 0.0% | 0.0% | 15.7% | 22.1% |
| Heterogeneity significance (P) | .000 | .530 | .077 | .792 | .951 | .669 | .306 | .227 |
Note: JTC, jumping to conclusions.
aSD = schizophrenia with current delusions, HC = healthy controls, SND = schizophrenia without current delusions, PD = other psychiatric illnesses with current delusions, PND = other psychiatric illnesses without current delusions.
b g = Hedges’ g reported or calculated; r, ρ = correlation or Spearman’s correlation reported.
cLongitudinal data.
A search of the Pubmed and PsycINFO databases for BADE papers was completed on September 22, 2015, and identified 27 studies, of which 13 were selected for further review based on their abstracts. Of these, 8 studies met our inclusion criteria (table 2).
Table 2.
Included BADE, BACE, and LA Studies, Comparisons, and Effect-Size Measures
| Source | Comparisona | |||||||
|---|---|---|---|---|---|---|---|---|
| SD/HC | SD/SND | SND/HC | PD/HC | SD/PD | SD/PND | PD/PND | PND/HC | |
| Woodward et al15,c | g b | g | g | |||||
| Woodward et al2 | g | g | g | |||||
| Woodward et al28 | g | g | g | g | g | |||
| Veckenstedt et al70 | g | g | g | g | g | |||
| Riccaboni et al71,d | r | |||||||
| Eifler et al29 | g | g | g | |||||
| Sanford et al3 | g | g | g | g | g | |||
| Speechley et al17 | g | g | g | g | g | |||
| BADE | ||||||||
| Total participants (n) | 369 | 466 | 455 | 0 | 0 | 221 | 0 | 247 |
| Total studies (k) | 7 | 8 | 7 | 0 | 0 | 4 | 0 | 4 |
| Heterogeneity variance (I2) | 38% | 49.5% | 0.0% | 20.0% | 0.0% | |||
| Heterogeneity significance (P) | .139 | .054 | .689 | .290 | .801 | |||
| BACE | ||||||||
| Total participants (n) | 369 | 426 | 455 | 0 | 0 | 221 | 0 | 247 |
| Total studies (k) | 7 | 7 | 7 | 0 | 0 | 4 | 0 | 4 |
| Heterogeneity variance (I2) | 0.0% | 0.0% | 19.4% | 0.0% | 14.5% | |||
| Heterogeneity significance (P) | .487 | .549 | .282 | .468 | .319 | |||
| LA | ||||||||
| Total participants (n) | 338 | 383 | 409 | 0 | 0 | 221 | 0 | 247 |
| Total studies (k) | 6 | 6 | 6 | 0 | 0 | 4 | 0 | 4 |
| Heterogeneity variance (I2) | 50.6% | 8.9% | 48.6% | 0.0% | 32.5% | |||
| Heterogeneity significance (P) | .072 | .359 | .083 | .509 | .217 | |||
Note: BADE, bias against disconfirmatory evidence; BACE, bias against confirmatory evidence; LA, liberal acceptance.
aSD = schizophrenia with current delusions, HC = healthy controls, SND = schizophrenia without current delusions, PD = other psychiatric illnesses with current delusions, PND = other psychiatric illnesses without current delusions.
b g = Hedges’ g reported or calculated; r = correlation reported.
cBADE and BACE data only.
dBADE data only.
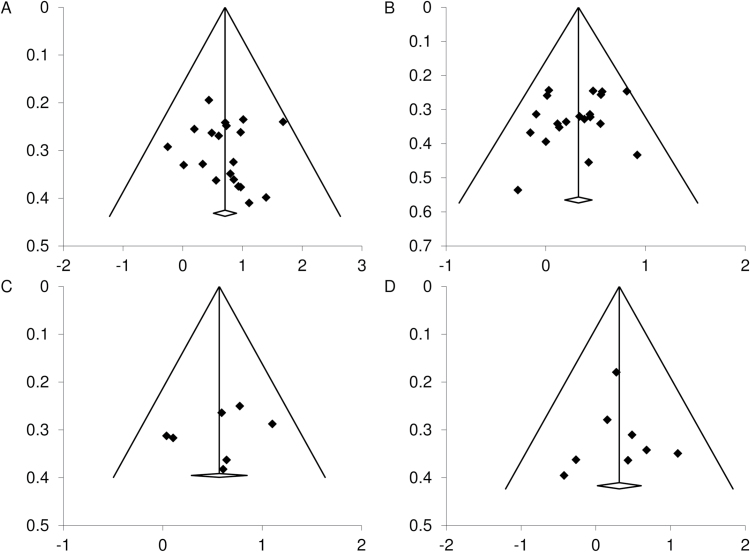
Publication Bias
Inspection of the funnel plots (figure 1) indicates a possible slight publication bias for the schizophrenia with current delusions vs healthy controls JTC comparison, but not the schizophrenia with vs without current delusions comparison. The funnel plots suggest little to no publication bias has influenced the BADE results.
Fig. 1.
Funnel plots showing standard error (y axis) against effect size (Hedges’ g, x axis) for the jumping to conclusions (JTC) comparison between (A) groups with schizophrenia with current delusions and healthy control groups, (B) groups with schizophrenia with and without current delusions, and the bias against disconfirmatory evidence (BADE) comparison between (C) groups with schizophrenia with current delusions and healthy control groups, (D) groups with schizophrenia with and without current delusions.
Preliminary Analyses
Subgroup analyses were performed where possible to determine whether studies using different methodologies could appropriately be combined. The core schizophrenia with vs without current delusions comparison was used for all subgroup analyses. There was no significant difference (Δg = 0.149 [−0.137, 0.434]) between studies that reported between-groups DTD (g = 0.275 [0.106, 0.444]) and those reporting the correlation between DTD and delusion strength (g = 0.424 [0.194, 0.654]), confirming the validity of converting correlational data to Hedges’ g and combining with the between-groups studies.
There was a small difference in effect sizes between longitudinal and between-groups JTC studies (Δg = 0.177 [0.056, 0.463]), and hence some caution in interpretation is suggested. Specifically, the longitudinal subgroup demonstrated a small but nonsignificant effect (g = 0.167 [−0.273, 0.608]), with poor precision due to the inclusion of only 2 studies. The cross-sectional subgroup demonstrated a small effect with much greater precision (g = 0.344 [0.201, 0.487]). Despite the small difference in effect sizes, inclusion of the 2 longitudinal studies in the meta-analysis increased overall precision, and we consider the combined between-groups and longitudinal data to be valid.
Analysis of Heterogeneity
Significant heterogeneity was observed for the schizophrenia with current delusions vs healthy controls JTC meta-analysis (table 1). When an unusually high-67 and low-effect53 study were removed from the analysis, heterogeneity was no longer significant, while effect size remained consistent. No obvious methodological differences were noted for either study which might account for extreme results, and they were included in subsequent analyses. No significant heterogeneity was observed for any other JTC, BADE, BACE, or LA comparisons (tables 1 and 2).
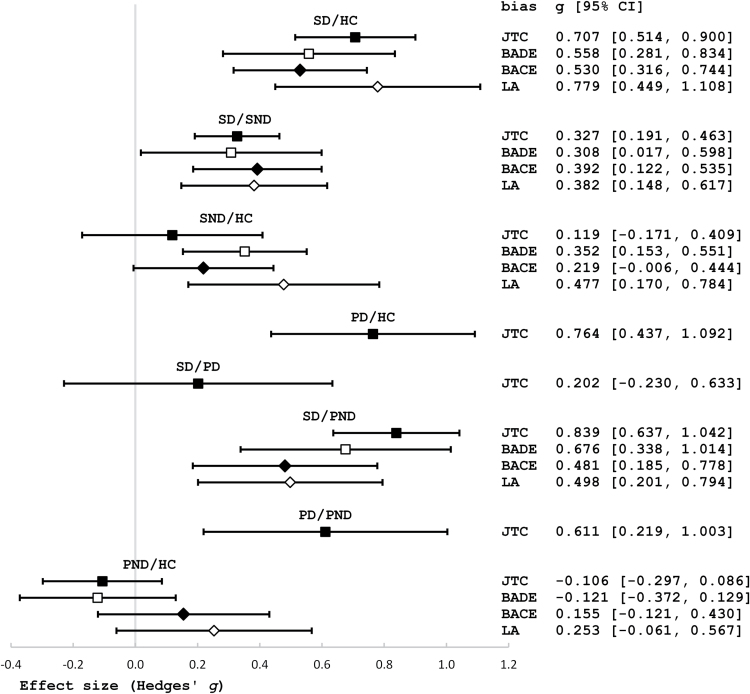
Replication of the Basic Relationship
The majority of studies and 2 recent meta-analyses7,8 attest that there is a relationship, whether direct or spurious, between cognitive bias and delusions in schizophrenia. As a prerequisite to further investigations we also tested this relationship, and found that groups with schizophrenia and current delusions showed greater JTC, BADE, BACE, and LA than healthy control groups, with a medium effect size (figure 2). Forest plots for all meta-analyses are included in the supplementary material. Our results replicate Dudley et al7 and Ross et al8 by confirming a relationship between having schizophrenia with delusions and elevated JTC, and additionally confirms this same relationship for the BADE, BACE, and LA biases also.
Fig. 2.
Plot and values of Hedges’ g effect size and 95% CI for group differences in jumping to conclusions (JTC), bias against disconfirmatory evidence (BADE), bias against confirmatory evidence (BACE), and liberal acceptance (LA). SD = schizophrenia with current delusions, HC = healthy controls, SND = schizophrenia without current delusions, PD = other psychiatric illnesses with current delusions, PND = other psychiatric illnesses without current delusions.
Key Comparisons Results
Groups with schizophrenia and current delusions demonstrated greater JTC, BADE, BACE, and LA than groups with schizophrenia who were not currently experiencing delusions, with a small effect size (see figure 2 for all key comparisons). In fact, schizophrenia groups without current delusions demonstrated no more JTC than healthy control groups, although they demonstrated more BADE with a small effect, a small trend towards more BACE, and more LA with small to medium effect.
Groups who were experiencing delusions due to psychiatric disorders other than schizophrenia also demonstrated greater JTC than healthy control groups, with a medium effect size (no BADE, BACE, or LA data were available for this comparison). These groups demonstrated equivalent levels of JTC to groups with schizophrenia who were currently experiencing delusions.
Groups with other psychiatric illnesses who were not experiencing delusions demonstrated less JTC and BADE with a large effect size, and less BACE and LA with a small to medium effect size than groups experiencing delusions due to schizophrenia. Groups with other psychiatric illnesses who were not experiencing delusions also demonstrated less JTC, with a medium effect size, than groups experiencing delusions owing to other diagnoses (no BADE, BACE, or LA data was available), and demonstrated no more JTC, BADE, BACE, or LA than healthy control groups.
Discussion
This meta-analysis compared narrowly-defined groups across the JTC, BADE, BACE, and LA spectrum of cognitive biases, in order to determine (1) whether these biases co-vary with delusions, consistent with the possibility they contribute causally to delusions, (2) whether these biases are associated with delusions in illnesses other than schizophrenia, to demonstrate whether the association is with a diagnosis of schizophrenia or with delusions in particular, and (3) whether these biases could merely be associated with being psychiatrically ill.
Do Biases Co-vary With Delusions Over Time?
The co-variability of biases with delusions over time would ideally be tested using longitudinal data, but only 2 longitudinal studies met the inclusion criteria and a separate analysis was of limited value owing to imprecision. Combined with the minimal longitudinal data available, we took the alternative approach of approximating longitudinal information using cross-sectional data. Groups with schizophrenia and current delusions demonstrated greater JTC (consistent with Dudley et al7), BADE, BACE, and LA than groups with schizophrenia who were not currently experiencing delusions, although the difference was small. Further, for the first time in a meta-analysis, we have shown that groups with schizophrenia without current delusions demonstrated no more JTC than healthy control groups (though they showed more BADE and LA than healthy control groups with small effect, and a trend towards more BACE). The medium JTC effect found by Dudley et al7 for their psychosis group vs healthy controls comparison (g=−0.53 [−0.69, −0.36]) lies between our results for schizophrenia groups with current delusions vs healthy controls, and for schizophrenia groups without current delusions vs healthy controls, as might be expected considering the mixed delusional status of their psychosis group. Together, our results suggest that JTC, BADE, BACE and LA are not simply stable features of schizophrenia. They appear elevated during times of worse delusions, and appear lower (BADE, BACE, LA) or comparable to normal levels (JTC) as delusions abate. This is consistent with the possibility that these biases contribute causally to delusions during acute phases of illness. Additionally, the presence of some biases (at reduced levels) in non-delusional groups suggests people with schizophrenia may also have a trait vulnerability to biases, which could be targeted by interventions during all phases of illness.
A significant limitation of this meta-analysis however is that it included longitudinal data from only 2 studies, and while longitudinal information was approximated using cross-sectional data, questions remain about the validity of this approach. It is possible that the schizophrenia groups without current delusions included participants for whom delusions were never a prominent feature of their schizophrenia, and that perhaps delusional severity is relatively stable over time.72 If this were the case, cross-sectional data from groups with and without current delusions would not reflect changes in delusion severity, but stable individual differences in symptomatology. As such, our results would demonstrate an association between biases and individual differences in the development of delusions, suggesting cognitive bias might be a risk factor for delusions in psychosis. Only longitudinal data can unequivocally show whether the biases truly co-vary over time with delusions in schizophrenia, and hence whether they may act as causal agents or risk factors for worse delusions.
Are Biases Associated With Delusions Across Multiple Diagnoses?
JTC was equally elevated in delusional groups with schizophrenia and other illnesses, suggesting that JTC is not spuriously related to delusions merely owing to their co-occurrence in schizophrenia. Rather, the finding that JTC was associated with delusions across diagnoses is consistent with the possibility that JTC contributes to the development of delusions, and suggests the association could be strong enough that JTC might even be a necessary (though not sufficient) factor for the development of delusions. Unfortunately no relevant BADE, BACE or LA data were available, but would make a worthy focus for future research. It is also possible that biases contribute to certain types of delusions and not others. For example, Garety et al73 found that JTC was more strongly associated with grandiose delusions than with persecutory delusions. Understanding whether the biases feature differently in different subtypes of delusions would be another worthy focus for future research, potentially leading to more targeted and effective cognitive therapies.
Are Biases Simply Elevated in Psychiatric Illnesses?
An association of biases with delusions in both schizophrenia and other delusional disorders could nevertheless occur if these biases were simply a consequence of having a psychiatric illness more generally. If this were the case, the biases should be elevated in groups with psychiatric diagnoses which are not associated with delusions also. However, groups with psychiatric illnesses not associated with delusions demonstrated less JTC, BADE, BACE, and LA than groups experiencing delusions, whether the delusions were due to schizophrenia (all biases) or other diagnoses (only JTC data available). Additionally, groups with psychiatric illnesses who were not experiencing delusions demonstrated no more JTC, BADE, BACE or LA than healthy control groups. As these biases are not elevated in psychiatric illnesses more generally, merely having a psychiatric illness cannot account for cognitive bias in those experiencing delusions.
General Discussion
Our results are consistent with the hypothesis that cognitive biases play a causal role in delusions. The hypothesis finds indirect support in treatment studies also. Metacognitive Training, a cognitive therapy that focuses on reducing JTC and BADE, has been shown by meta-analysis to weaken delusional severity in people with schizophrenia.74,75
The similar pattern of occurrence of the BADE, BACE, and LA biases supports their interpretation as parts of a unified evidence integration construct.3,17 That JTC also demonstrates a similar pattern of occurrence to the evidence integration biases suggests they may share a common underlying cognitive mechanism, while remaining independent constructs.76 One mechanism proposed to underlie JTC and BADE is the hypersalience of evidence which matches a hypothesis.11,17,23,77 Hypersalient evidence-hypothesis matches could lead to reduced data-gathering and premature decision-making (JTC), or strengthen a weak hypothesis against counter-evidence (BADE). Though not discussed in the literature, perhaps BACE arises when the hypersalience of evidence-hypothesis matches renders evidence for new alternative (and perhaps true) hypotheses comparatively less salient. The theory could even explain LA, as the hypersalience of positive evidence for an absurd hypothesis might overwhelm the nonspecific common-sense evidence most people presumably draw upon to discount very unlikely scenarios.
Conclusion
Our meta-analysis demonstrates that JTC, BADE, BACE, and LA are associated with delusions across multiple diagnoses, and not merely with having a schizophrenia diagnosis nor with having a psychiatric illness more generally. The association of these biases with delusions specifically is consistent with the possibility these biases contribute to delusions. Additionally our meta-analysis implies that these biases could co-vary with delusions over time, increasing in strength and contributing to the development and maintenance of delusions during acute phases of illness. The suggestion that cognitive biases play a role in the development and maintenance of delusions in a range of psychiatric illnesses has high apparent validity, and remains a parsimonious and convincing explanation for the close association of JTC and BADE with delusions.
Funding
This work was supported by Flinders University, South Australia.
Supplementary Material
Acknowledgments
We thank Todd Woodward who, together with Balzan several years ago suggested the need for a meta-analysis of cognitive bias studies which strategically compared groups differing on diagnosis and delusional status. We would also like to thank the following authors for providing unpublished BADE data and additional information: Todd Woodward, Steffen Moritz, Ruth Veckenstedt, and Sarah Eisenacher (nee Eifler). We are additionally grateful to the 2 anonymous reviewers for their constructive input. R.P.B. has conducted Metacognitive Training (MCT) and undertaken studies on MCT, JTC, and BADE, for which he has received funding from Flinders University and the Trevor Prescott Freemasons Memorial Scholarship. B.F.M. has conducted Metacognitive Training (MCT) for which he has been paid as a Research Assistant. J.K.M. declares she has no conflicts of interest in relation to the subject of this study. B.F.M.: Conception and design of the review methodology, undertaking of literature searches, data extraction and analysis, results interpretation, writing of manuscript drafts, critical revision and final approval of manuscript. J.K.M.: Conception and design of the review methodology, results interpretation, critical revision and final approval of manuscript. R.P.B.: Conception and design of the review methodology, results interpretation, critical revision and final approval of manuscript.
References
- 1. Garety PA, Freeman D. The past and future of delusions research: from the inexplicable to the treatable. Br J Psychiatry. 2013;203:327–333. [DOI] [PubMed] [Google Scholar]
- 2. Woodward TS, Moritz S, Cuttler C, Whitman JC. The contribution of a cognitive bias against disconfirmatory evidence (BADE) to delusions in schizophrenia. J Clin Exp Neuropsychol. 2006;28:605–617. [DOI] [PubMed] [Google Scholar]
- 3. Sanford N, Veckenstedt R, Moritz S, Balzan RP, Woodward TS. Impaired integration of disambiguating evidence in delusional schizophrenia patients. Psychol Med. 2014;44:2729–2738. [DOI] [PubMed] [Google Scholar]
- 4. Garety P, Hemsley D. Delusions: Investigations Into the Psychology of Delusional Reasoning. Oxford, UK: Oxford University Press; 1994. [Google Scholar]
- 5. Freeman D, Garety P. Worry, worry processes and dimensions of delusions: an exploratory investigation of a role for anxiety processes in the maintenance of delusional distress. Behav Cogn Psychother. 1999;27:47–62. [Google Scholar]
- 6. Moritz S, Woodward TS. A generalized bias against disconfirmatory evidence in schizophrenia. Psychiatry Res. 2006;142:157–165. [DOI] [PubMed] [Google Scholar]
- 7. Dudley R, Taylor P, Wickham S, Hutton P. Psychosis, delusions and the “Jumping to Conclusions” reasoning bias: a systematic review and meta-analysis. Schizophr Bull. 2016;42:652–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ross R, McKay R, Coltheart M, Langdon R. Jumping to conclusions about the beads task? A meta-analysis of delusional ideation and data-gathering. Schizophr Bull. 2015;41:1183–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Huq SF, Garety PA, Hemsley DR. Probabilistic judgements in deluded and non-deluded subjects. Q J Exp Psychol A. 1988;40:801–812. [DOI] [PubMed] [Google Scholar]
- 10. Woodward TS, Munz M, LeClerc C, Lecomte T. Change in delusions is associated with change in “jumping to conclusions”. Psychiatry Res. 2009;170:124–127. [DOI] [PubMed] [Google Scholar]
- 11. Speechley WJ, Whitman JC, Woodward TS. The contribution of hypersalience to the “jumping to conclusions” bias associated with delusions in schizophrenia. J Psychiatry Neurosci. 2010;35:7–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Young HF, Bentall RP. Probabilistic reasoning in deluded, depressed and normal subjects: effects of task difficulty and meaningful versus non-meaningful material. Psychol Med. 1997;27:455–465. [DOI] [PubMed] [Google Scholar]
- 13. Dudley RE, John CH, Young AW, Over DE. The effect of self-referent material on the reasoning of people with delusions. Br J Clin Psychol. 1997;36:575–584. [DOI] [PubMed] [Google Scholar]
- 14. Balzan RP, Delfabbro PH, Galletly CA, Woodward TS. Over-adjustment or miscomprehension? A re-examination of the jumping to conclusions bias. Aust N Z J Psychiatry. 2012;46:532–540. [DOI] [PubMed] [Google Scholar]
- 15. Woodward TS, Moritz S, Chen EY. The contribution of a cognitive bias against disconfirmatory evidence (BADE) to delusions: a study in an Asian sample with first episode schizophrenia spectrum disorders. Schizophr Res. 2006;83:297–298. [DOI] [PubMed] [Google Scholar]
- 16. Moritz S, Woodward TS. Plausibility judgment in schizophrenic patients: evidence for a liberal acceptance bias. German J Psychiatry. 2004;7:66–74. [Google Scholar]
- 17. Speechley W, Moritz S, Ngan E, Woodward T. Impaired evidence integration and delusions in schizophrenia. J Exp Psychopathol. 2012;3:688–701. [Google Scholar]
- 18. Fine C, Gardner M, Craigie J, Gold I. Hopping, skipping or jumping to conclusions? Clarifying the role of the JTC bias in delusions. Cogn Neuropsychiatry. 2007;12:46–77. [DOI] [PubMed] [Google Scholar]
- 19. Langdon R, Still M, Connors MH, Ward PB, Catts SV. Jumping to delusions in early psychosis. Cogn Neuropsychiatry. 2014;19:241–256. [DOI] [PubMed] [Google Scholar]
- 20. van der Gaag M, Schütz C, Ten Napel A, et al. Development of the Davos assessment of cognitive biases scale (DACOBS). Schizophr Res. 2013;144:63–71. [DOI] [PubMed] [Google Scholar]
- 21. Bentall RP, Rowse G, Shryane N, et al. The cognitive and affective structure of paranoid delusions: a transdiagnostic investigation of patients with schizophrenia spectrum disorders and depression. Arch Gen Psychiatry. 2009;66:236–247. [DOI] [PubMed] [Google Scholar]
- 22. Corcoran R, Rowse G, Moore R, et al. A transdiagnostic investigation of ‘theory of mind’ and ‘jumping to conclusions’ in patients with persecutory delusions. Psychol Med. 2008;38:1577–1583. [DOI] [PubMed] [Google Scholar]
- 23. Balzan R, Delfabbro P, Galletly C, Woodward T. Reasoning heuristics across the psychosis continuum: the contribution of hypersalient evidence-hypothesis matches. Cogn Neuropsychiatry. 2012;17:431–450. [DOI] [PubMed] [Google Scholar]
- 24. Colbert SM, Peters ER. Need for closure and jumping-to-conclusions in delusion-prone individuals. J Nerv Ment Dis. 2002;190:27–31. [DOI] [PubMed] [Google Scholar]
- 25. Menon M, Pomarol-Clotet E, McKenna PJ, McCarthy RA. Probabilistic reasoning in schizophrenia: a comparison of the performance of deluded and nondeluded schizophrenic patients and exploration of possible cognitive underpinnings. Cogn Neuropsychiatry. 2006;11:521–536. [DOI] [PubMed] [Google Scholar]
- 26. Menon M, Addington J, Remington G. Examining cognitive biases in patients with delusions of reference. Eur Psychiatry. 2013;28:71–73. [DOI] [PubMed] [Google Scholar]
- 27. So SH, Freeman D, Dunn G, et al. Jumping to conclusions, a lack of belief flexibility and delusional conviction in psychosis: a longitudinal investigation of the structure, frequency, and relatedness of reasoning biases. J Abnorm Psychol. 2012;121:129–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Woodward TS, Moritz S, Menon M, Klinge R. Belief inflexibility in schizophrenia. Cogn Neuropsychiatry. 2008;13:267–277. [DOI] [PubMed] [Google Scholar]
- 29. Eifler S, Rausch F, Schirmbeck F, et al. Neurocognitive capabilities modulate the integration of evidence in schizophrenia. Psychiatry Res. 2014;219:72–78. [DOI] [PubMed] [Google Scholar]
- 30. Marengo JT, Harrow M. Schizophrenic thought disorder at follow-up. A persistent or episodic course? Arch Gen Psychiatry. 1987;44:651–659. [DOI] [PubMed] [Google Scholar]
- 31. Robinson DG, Woerner MG, McMeniman M, Mendelowitz A, Bilder RM. Symptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry. 2004;161:473–479. [DOI] [PubMed] [Google Scholar]
- 32. Jobe TH, Harrow M. Long-term outcome of patients with schizophrenia: a review. Can J Psychiatry. 2005;50:892–900. [DOI] [PubMed] [Google Scholar]
- 33. Lewis S, Escalona P, Keith S. Phenomenology of Schizophrenia. In: Sadock B, Sadock V, Ruiz P, eds. Kaplan and Sadock′s Comprehensive Textbook of Psychiatry. Vol 1 9th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2009:1433–1451. [Google Scholar]
- 34. Gourzis P, Katrivanou A, Beratis S. Symptomatology of the initial prodromal phase in schizophrenia. Schizophr Bull. 2002;28:415–429. [DOI] [PubMed] [Google Scholar]
- 35. Nuechterlein KH, Miklowitz DJ, Ventura J, Gitlin MJ, Stoddard M, Lukoff D. Classifying episodes in schizophrenia and bipolar disorder: criteria for relapse and remission applied to recent-onset samples. Psychiatry Res. 2006;144:153–166. [DOI] [PubMed] [Google Scholar]
- 36. Jacobsen P, Freeman D, Salkovskis P. Reasoning bias and belief conviction in obsessive-compulsive disorder and delusions: jumping to conclusions across disorders? Br J Clin Psychol. 2012;51:84–99. [DOI] [PubMed] [Google Scholar]
- 37. Fraser J, Morrison A, Wells A. Cognitive processes, reasoning biases and persecutory delusions: a comparative study. Behav Cogn Psychother. 2006;34:421–435. [Google Scholar]
- 38. Peters E, Garety P. Cognitive functioning in delusions: a longitudinal analysis. Behav Res Ther. 2006;44:481–514. [DOI] [PubMed] [Google Scholar]
- 39. Menon M, Mizrahi R, Kapur S. ‘Jumping to conclusions’ and delusions in psychosis: relationship and response to treatment. Schizophr Res. 2008;98:225–231. [DOI] [PubMed] [Google Scholar]
- 40. Ross K, Freeman D, Dunn G, Garety P. A randomized experimental investigation of reasoning training for people with delusions. Schizophr Bull. 2011;37:324–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Waller H, Freeman D, Jolley S, Dunn G, Garety P. Targeting reasoning biases in delusions: a pilot study of the Maudsley Review Training Programme for individuals with persistent, high conviction delusions. J Behav Ther Exp Psychiatry. 2011;42:414–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Moritz S, Woodward TS, Hausmann D. Incautious reasoning as a pathogenetic factor for the development of psychotic symptoms in schizophrenia. Schizophrenia Bulletin. 2006;32:327–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Moritz S, Woodward T, Jelinek L, Klinge R. Memory and metamemory in schizophrenia: a liberal acceptance account of psychosis. Psychol Med. 2008;38:825–832. [DOI] [PubMed] [Google Scholar]
- 44. Moritz S, Woodward TS, Lambert M. Under what circumstances do patients with schizophrenia jump to conclusions? A liberal acceptance account. Brit J Clin Psychol. 2007;46:127–137. [DOI] [PubMed] [Google Scholar]
- 45. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 46. Rosnow RL, Rosenthal R. Computing contrasts, effect sizes, and counternulls on other people’s published data: general procedures for research consumers. Psychol Methods. 1996;1:331. [Google Scholar]
- 47. Hedges LV. Distribution theory for Glass’s estimator of effect size and related estimators. J Educ Behav Stat. 1981;6:107–128. [Google Scholar]
- 48. Cumming G. Understanding the New Statistics: Effect Sizes, Confidence Intervals, and Meta-analysis. New York, NL: Routledge; 2013. [Google Scholar]
- 49. Andreou C, Roesch-Ely D, Veckenstedt R, et al. Predictors of early stable symptomatic remission after an exacerbation of schizophrenia: the significance of symptoms, neuropsychological performance and cognitive biases. Psychiatry Res. 2013;210:729–734. [DOI] [PubMed] [Google Scholar]
- 50.Andreou C, Schneider BC, Balzan R, Luedecke D, Roesch-Ely D, Moritz S. Neurocognitive deficits are relevant for the jumping-to-conclusions bias, but not for delusions: A longitudinal study. Schizophr Res Cogn. 2015;2:8–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Baskak B, Baran Z, Ozguven HD, et al. Prefrontal activity measured by functional near infrared spectroscopy during probabilistic inference in subjects with persecutory delusions. Schizophr Res. 2015;161:237–243. [DOI] [PubMed] [Google Scholar]
- 52. Buck KD, Warman DM, Huddy V, Lysaker PH. The relationship of metacognition with jumping to conclusions among persons with schizophrenia spectrum disorders. Psychopathology. 2012;45:271–275. [DOI] [PubMed] [Google Scholar]
- 53. Colbert SM, Peters E, Garety P. Jumping to conclusions and perceptions in early psychosis: relationship with delusional beliefs. Cogn Neuropsychiatry. 2010;15:422–440. [DOI] [PubMed] [Google Scholar]
- 54. Conway CR, Bollini AM, Graham BG, Keefe RS, Schiffman SS, McEvoy JP. Sensory acuity and reasoning in delusional disorder. Compr Psychiatry. 2002;43:175–178. [DOI] [PubMed] [Google Scholar]
- 55. Dudley RE, John CH, Young AW, Over DE. Normal and abnormal reasoning in people with delusions. Br J Clin Psychol. 1997;36:243–258. [DOI] [PubMed] [Google Scholar]
- 56. Dudley R, Shaftoe D, Cavanagh K, et al. ‘Jumping to conclusions’ in first-episode psychosis. Early Interv Psychiatry. 2011;5:50–56. [DOI] [PubMed] [Google Scholar]
- 57. Fear CF, Healy D. Probabilistic reasoning in obsessive-compulsive and delusional disorders. Psychol Med. 1997;27:199–208. [DOI] [PubMed] [Google Scholar]
- 58. Garety P. Reasoning and delusions. Br J Psychiatry Suppl. 1991;14:14–18. [PubMed] [Google Scholar]
- 59. Langdon R, Ward PB, Coltheart M. Reasoning anomalies associated with delusions in schizophrenia. Schizophr Bull. 2010;36:321–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lim MH, Gleeson JF, Jackson HJ. The jumping-to-conclusions bias in new religious movements. J Nerv Ment Dis. 2012;200:868–875. [DOI] [PubMed] [Google Scholar]
- 61. Lincoln TM, Ziegler M, Mehl S, Rief W. The jumping to conclusions bias in delusions: specificity and changeability. J Abnorm Psychol. 2010;119:40–49. [DOI] [PubMed] [Google Scholar]
- 62. Moritz S, Woodward TS. Jumping to conclusions in delusional and non-delusional schizophrenic patients. Br J Clin Psychol. 2005;44:193–207. [DOI] [PubMed] [Google Scholar]
- 63. Mortimer A, Bentham P, McKay A, et al. Delusions in schizophrenia: a phenomenological and psychological exploration. Cogn Neuropsychiatry. 1996;1:289–304. [DOI] [PubMed] [Google Scholar]
- 64. Peters ER, Thornton P, Siksou L, Linney Y, MacCabe JH. Specificity of the jump-to-conclusions bias in deluded patients. Br J Clin Psychol. 2008;47:239–244. [DOI] [PubMed] [Google Scholar]
- 65. So SH-w, Kwok NT-k. Jumping to conclusions style along the continuum of delusions: delusion-prone individuals are not hastier in decision making than healthy individuals. PloS One. 2015;1:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Startup H, Freeman D, Garety PA. Jumping to conclusions and persecutory delusions. Eur Psychiatry. 2008;23:457–459. [DOI] [PubMed] [Google Scholar]
- 67. Warman DM, Lysaker PH, Martin JM, Davis L, Haudenschield SL. Jumping to conclusions and the continuum of delusional beliefs. Behav Res Ther. 2007;45:1255–1269. [DOI] [PubMed] [Google Scholar]
- 68. Warman DM, Martin JM, Lysaker P. Jumping to conclusions and delusions: the impact of discussion of the bias on the bias. Schizophr Res. 2013;150:575–579. [DOI] [PubMed] [Google Scholar]
- 69. Wittorf A, Giel KE, Hautzinger M, et al. Specificity of jumping to conclusions and attributional biases: a comparison between patients with schizophrenia, depression, and anorexia nervosa. Cogn Neuropsychiatry. 2012;17:262–286. [DOI] [PubMed] [Google Scholar]
- 70. Veckenstedt R, Randjbar S, Vitzthum F, Hottenrott B, Woodward TS, Moritz S. Incorrigibility, jumping to conclusions, and decision threshold in schizophrenia. Cogn Neuropsychiatry. 2011;16:174–192. [DOI] [PubMed] [Google Scholar]
- 71. Riccaboni R, Fresi F, Bosia M, et al. Patterns of evidence integration in schizophrenia and delusion. Psychiatry Res. 2012;200:108–114. [DOI] [PubMed] [Google Scholar]
- 72. Marengo J, Harrow M, Herbener ES, Sands J. A prospective longitudinal 10-year study of schizophrenia’s three major factors and depression. Psychiatry Res. 2000;97:61–77. [DOI] [PubMed] [Google Scholar]
- 73. Garety PA, Gittins M, Jolley S, et al. Differences in cognitive and emotional processes between persecutory and grandiose delusions. Schizophr Bull. 2012;39:629–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Eichner C, Berna F. Acceptance and efficacy of metacognitive training (MCT) on positive symptoms and delusions in patients with schizophrenia: a meta-analysis taking into account important moderators [published online ahead of print January 8, 2016]. Schizophr Bull. 2016. doi:10.1093/schbul/sbv225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Eichner C. Can Metacognitive Training (MCT) Reduce Positive Symptoms and Delusions in Patients with Schizophrenia? A Meta-Analysis Taking into Account Important Moderators. Hamburg, Germany: Department of Psychology, University of Hamburg; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Moritz S, Veckenstedt R, Hottenrott B, Woodward TS, Randjbar S, Lincoln TM. Different sides of the same coin? Intercorrelations of cognitive biases in schizophrenia. Cogn Neuropsychiatry. 2010;15:406–421. [DOI] [PubMed] [Google Scholar]
- 77. Balzan R, Delfabbro P, Galletly C, Woodward T. Confirmation biases across the psychosis continuum: the contribution of hypersalient evidence-hypothesis matches. Br J Clin Psychol. 2013;52:53–69. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.