Abstract
Several integrated models of psychosis have implicated adverse, stressful contexts and experiences, and affective and cognitive processes in the onset of psychosis. In these models, the effects of stress are posited to contribute to the development of psychotic experiences via pathways through affective disturbance, cognitive biases, and anomalous experiences. However, attempts to systematically test comprehensive models of these pathways remain sparse. Using the Experience Sampling Method in 51 individuals with first-episode psychosis (FEP), 46 individuals with an at-risk mental state (ARMS) for psychosis, and 53 controls, we investigated how stress, enhanced threat anticipation, and experiences of aberrant salience combine to increase the intensity of psychotic experiences. We fitted multilevel moderated mediation models to investigate indirect effects across these groups. We found that the effects of stress on psychotic experiences were mediated via pathways through affective disturbance in all 3 groups. The effect of stress on psychotic experiences was mediated by threat anticipation in FEP individuals and controls but not in ARMS individuals. There was only weak evidence of mediation via aberrant salience. However, aberrant salience retained a substantial direct effect on psychotic experiences, independently of stress, in all 3 groups. Our findings provide novel insights on the role of affective disturbance and threat anticipation in pathways through which stress impacts on the formation of psychotic experiences across different stages of early psychosis in daily life.
Keywords: stress sensitivity, aberrant salience, threat anticipation, experience sampling method, first-episode psychosis, at-risk mental state
Introduction
There is now strong evidence that subclinical psychotic experiences are prevalent in the general population and phenomenologically and temporally continuous with clinical symptoms in psychotic disorders.1,2 A number of psychological mechanisms have been implicated in the development of psychotic experiences (PE) across different stages of subclinical and clinical psychosis. Several integrated models of psychosis implicate adverse, stressful contexts and experiences, as well as affective and cognitive processes in the onset of psychosis.3–7 These models propose that, in individuals with an increased premorbid vulnerability of biopsychosocial origin,4 the effects of stress on the development of PE are (in part) mediated through affective disturbances, cognitive biases, and anomalous experiences.3–5 Unravelling the complex interplay between stress, affective and cognitive processes as basis for targeting these at an early stage, with the goal of preventing onset and achieving better outcomes of psychosis, is of public health importance.8–12
Recently, the interplay between affective disturbances and stressful contexts and experiences in daily life (including stressful events, activities, and social situations) that may be underlying the development of PE has received much attention.12–16 It has been repeatedly suggested that emotional reactivity to such routine daily hassles and minor socioenvironmental stressors may be an important mechanism.5,13 Previous studies have found elevated emotional reactivity to minor stressors in individuals with psychotic disorder and increased familial or psychometric risk (ie, a high score of sub-clinical PE).12–16 Similarly, a recent study reported elevated emotional reactivity in response to minor stressors in individuals with an at-risk mental state (ARMS).17 Previous research further suggest some degree of specificity, for example, of elevated emotional reactivity to social but not event-related stress as a putative mechanism underlying the association between childhood trauma and psychosis.18 Affective disturbances, more generally, have been shown to be linked to PE across different stages along the psychosis continuum.19–25
Cognitive models of psychosis provide a detailed specification of the cognitive processes associated with emotional responses to stress and consider cognitive biases, such as a hypervigilance for threat, to be involved in stress reactivity.4,26 First, stressful experiences per se may alter cognitive interpretation and bias individuals toward hypervigilance for threat.3,12 Further, cognitive models ascribe a prominent role to (stress-induced) affective disturbances, such as symptoms of anxiety, which are considered to drive individuals into enhanced anticipation of threat;23,27 enhanced threat anticipation, in turn, has been shown to be linked to the formation of PE.4,5,21,23
Stress-induced emotional and cognitive changes may result in anomalous experiences such as experiences of aberrant novelty and salience in vulnerable individuals.4,28 Cognitive models further posit, based on neurobiological approaches, that these experiences are closely linked to a sensitized dopaminergic system (secondary to variant genes, early neurological insults, and exposure to social adversity),3,4,29 which in the event of further stressful experiences, even if minor, will be followed by dysregulated dopamine release, leading to the aberrant assignment of salience to otherwise irrelevant stimuli. As individuals seek to explain these experiences, biased cognitive processes (such as enhanced threat anticipation) then result in the appraisal of anomalous experiences as uncontrollable, threatening, externally caused or attributable, which, ultimately, lead to abnormal beliefs and hallucinations becoming symptomatic.3,4 In this regard, PE may be seen as an attempt to make sense of these aberrant salient stimuli.3,29
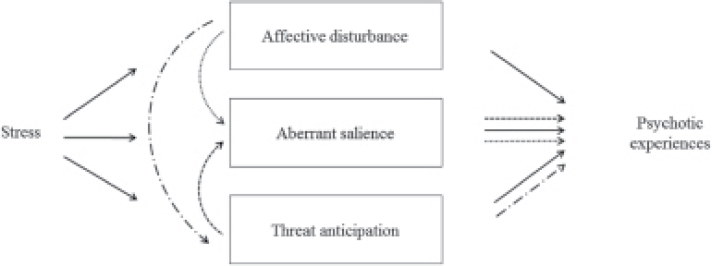
From the above, it becomes apparent that much attention has been paid to the association between stress and PE across different stages of psychosis. Several models have proposed that the formation of PE is complex and likely to be the result of the interplay between stress, cognitive, and affective processes. However, only a small number of studies have directly tested these specific pathways. Also, no study that we are aware of has tested these pathways in individuals’ daily lives. However, in order to elucidate the multi-factorial nature of psychotic disorders further, the pathways to psychosis, as proposed by prior work, should be tested in one comprehensive model. The primary aim of the current study therefore was to examine how stressful contexts and experiences (event-related, activity-related, and social stress), affective disturbance (ie, negative affect), cognitive bias (ie, enhanced threat anticipation), and anomalous experiences (ie, aberrant salience) combine to increase the intensity of PE in daily life. We used the Experience Sampling Method (ESM),30 a structured diary technique, in a sample of individuals with a first-episode psychosis (FEP), individuals with ARMS, and controls to test the following hypotheses (figure 1): within each group, (1) stressful contexts and experiences in daily life increase the intensity of PE via pathways through affective disturbance, enhanced threat anticipation, and aberrant salience; (2) affective disturbance increases the intensity of PE through enhanced threat anticipation and aberrant salience; and (3) enhanced threat anticipation increases intensity of PE through experiences of aberrant salience. We furthermore hypothesized that the indirect effects of stressful contexts and experiences on PE through affective disturbance, anomalous experiences, and cognitive bias are greater in FEP than in controls, ARMS than in controls, and FEP than in ARMS.
Fig. 1.
Schematic representation of pathways tested within each group: the following hypotheses were tested within each group: (1) stressful contexts and experiences in daily life increase the intensity of psychotic experiences through their impact on affective disturbance, enhanced threat anticipation, and aberrant salience ( ); (2) affective disturbance increases the intensity of psychotic experiences through enhanced threat anticipation (
); (2) affective disturbance increases the intensity of psychotic experiences through enhanced threat anticipation ( ) and aberrant salience (
) and aberrant salience ( ); and (3) enhanced threat anticipation increases intensity of psychotic experiences through their impact on experiences of aberrant salience (
); and (3) enhanced threat anticipation increases intensity of psychotic experiences through their impact on experiences of aberrant salience ( ), while controlling for age, gender, ethnicity, level of education, employment status, area-related stress, and outsider status as potential confounders.
), while controlling for age, gender, ethnicity, level of education, employment status, area-related stress, and outsider status as potential confounders.
Methods
Sample
A sample of FEP individuals, ARMS individuals, and controls with no history of psychosis was recruited as part of the Childhood Adversity and Psychosis study and EU-GEI.31 FEP individuals were recruited from mental health services in South-East London, UK. Inclusion criteria were: aged 18–64; resident in defined catchment area; diagnosis of FEP (ICD-10, F20-F29, F30-F33)32; command of the English language. Exclusion criteria were: transient psychotic symptoms resulting from intoxication; psychotic symptoms precipitated by an organic cause. Individuals with an ARMS were recruited from Outreach and Support in South London,33 the West London Mental Health NHS Trust, and a community survey of General Practitioner (GP) practices. Inclusion criteria were: aged 18–35; presence of an ARMS as assessed with the CAARMS;31,34 command of the English language. Exclusion criteria were: prior experience of a psychotic episode for more than 1 week as determined by the CAARMS and Structured Clinical Interview for DSM Disorders;35 previous treatment with an antipsychotic for a psychotic episode; IQ <60 measured with an adapted version of the WAIS.31,36 Controls were recruited through GP lists and the national postal address file. Inclusion criteria were: aged 18–64; resident within the same areas as FEP individuals, command of the English language. Exclusion criteria were: personal/family history of psychosis, presence of PE as measured with the Psychosis Screening Questionnaire; and presence of an ARMS based on the CAARMS or the Schizophrenia Proneness Instrument–Adult version.
Data Collection
Basic Sample Characteristics
Data on basic sample characteristics were collected with the modified MRC sociodemographic schedule. ICD-10 diagnosis of FEP was determined using the OPCRIT system. Presence of an ARMS was based on the CAARMS and the SCID.
ESM Measures
We used the ESM, a structured diary technique, to collect data on stress, negative affect, aberrant salience, threat anticipation, and PE. Using a time-based design with stratified random sampling, this method allows for assessing moment-to-moment fluctuations in daily life. Feasibility, reliability, and validity of this method in individuals with a FEP and individuals with an ARMS has been demonstrated recently.16,17,30 Further information on the ESM procedure and variables are presented in table 1.
Table 1.
ESM Procedurea and Measures of Stress, Negative Affect, Aberrant Salience, Threat Anticipation, and Psychotic Experiences
| Domain | ESM Measures |
|---|---|
| Stress | |
| Event-related | Event-related stress was assessed with 1 item in which participants rated the most important event since the last beep on a 7-point Likert scale (−3 = “very unpleasant” to 3 = “very pleasant). The item was reverse coded with higher ratings indicating higher levels of stress (a rating of −3 coded as 7 and a rating of 3 coded as 1). |
| Activity- related | The activity-related stress scale consisted of 3 items (“This activity is difficult for me,” “I would prefer doing something else,” “This is a pleasant activity” [reversed]) rated on a 7-point Likert (1 = “not at all” to 7 = “very much”). |
| Social | Social stress was measured with a mean of 2 items. The first item asked participants to indicate “Who am I with?” (eg, partner, family, friends, colleagues, acquaintances, strangers, others, nobody). The second item asked participants to rate their current social context on a 7-point Likert scale (1 = “not at all” to 7 = “very much”) with 2 questions: 1) “I would prefer to be alone [if with someone]/I would prefer to have company [if alone]”; 2) “I find being with these people pleasant [if with someone]/it pleasant to be alone [if alone]” (reversed). |
| Negative affect | The negative affect scale consisted of 5 items asking participants to rate the extent to which they felt down, lonely, anxious, insecure, and annoyed on a 7-point Likert scale (1 = “not at all” to 7 = “very much”). |
| Aberrant salience | Aberrant salience was assessed with 3 items (“Everything grabs my attention right now,” “Everything seems to have meaning right now,” and “I notice things that I haven’t noticed before.”) that were rated on a 7-point Likert scale (1 = “not at all” to 7 = “very much”). |
| Threat anticipation | Threat anticipation was measured by asking participants to think about what might happen in the next few hours and rate the item “I think that something unpleasant will happen” on a 7-point Likert scale (1 = “not at all” to 7 = “very much”). |
| Psychotic experiences | We used the ESM psychosis measure by Myin-Germeys et al, which consists of 8 items covering different aspects of mental states that are directly associated with psychotic experiences (“I feel paranoid,” “I feel unreal,” “I hear things that aren’t really there,” “I see things that aren’t really there,” “I can’t get these thoughts out of my head,” “My thoughts are influenced by others,” “It’s hard to express my thoughts in words,” and “I feel like I am losing control”). Participants were asked to rate the intensity of psychotic experiences on a 7-point Likert scale (1 = “not at all” to 7 = “very much”). These items have been reported to show high levels of internal consistency in previous studies (Cronbach’s alpha = 0.80)37 as well as in the current study (Cronbach’s α = 0.90).18 They have been further shown to have good convergent validity with interviewer-rated measures of psychosis (r = .45, P < .001) the PANSS (r = .45; P < .001)37 as well as good concurrent validity with negative affect (r = .68, P < .001).18 |
a ESM procedure: Over a period of 6 consecutive days, participants were prompted by the PsyMate “beep” signal to complete the ESM questionnaire 10 times a day at random moments within set blocks of time. Participants were provided with detailed instructions and a practice session as training in the use of the PsyMate during an initial briefing period. Participants were explained to stop their activity and respond to the above items when prompted by the beep signal as part of a comprehensive diary questionnaire assessing activities, feelings, thoughts, behaviors, social situations, and neighborhood surroundings in daily life. The assessment period started on any day of the week as selected by the participant, and the ESM questionnaire was available up to 10 minutes after the beep signal. In order to maximize the number of observations per participant, participants were contacted at least once during the assessment period to assess instruction adherence, identify any concerns associated with the method, and help participants with any problems in completing the ESM questionnaire. The participants’ reactivity to and compliance with the method was assessed in a debriefing session at the end of the assessment period. In order to be included in the analysis, participants had to provide valid responses to at least one-third of the beep signals.
Statistical Analysis
Multilevel moderated mediation models were fitted in MPlus, Version 7,38 with multiple observations (level 1) being treated as nested within subjects (level 2). A detailed description of these models is included in the online supplementary methods. The total effect of each stress variable (event-related, activity-related, and social stress) in daily life (level 1) on intensity of PE (level 1) was apportioned into direct and indirect (or, synonymously, mediating) effects through negative affect, aberrant salience, and enhanced threat anticipation (level 1) using the product of coefficients strategy. Group (FEP, ARMS, controls) was used as the moderator variable (level 2) of direct and conditional indirect which allowed us to test whether conditional indirect effects were greater in (1) FEP than in controls, (2) ARMS than in controls, and (3) FEP than in ARMS.39–41 We first fitted separate simple moderated multilevel mediation models: (1) with one independent variable for event-related stress, activity-related stress, or social stress, one mediator variable for negative affect, threat anticipation or aberrant salience, and one outcome variable for PE; (2) with one independent variable for negative affect, one mediator variable for threat anticipation or aberrant salience, and one outcome variable for PE; and (3) with enhanced threat anticipation as independent variable, aberrant salience as mediator variable, and PE as outcome variable. Based on evidence of mediation in these models, we next fitted a multiple multilevel moderated mediation model to examine the relative contribution of direct effects and specific indirect effects via these pathways simultaneously.42 All analyses were adjusted for age, gender, ethnicity, level of education, employment status as potential confounders.
Results
Basic Sample Characteristics
ESM data were collected for 165 participants (59 FEP, 51 ARMS, 55 controls). Fifteen participants were excluded from the analysis due to an insufficient number of valid responses (<19), resulting in a sample of 150 participants (51 FEP, 46 ARMS, 53 controls). The control group was slightly older and included more women than the FEP group (supplementary table 1). ARMS and FEP individuals showed higher levels of stress, negative affect, aberrant salience, threat anticipation, and PE compared to controls (supplementary table 2). The magnitude of correlations between stress, negative affect, aberrant salience, threat anticipation, and PE was moderate to small (supplementary table 3).
Simple Moderated Mediation Models
To examine pathways from stress to PE via negative affect, aberrant salience, and threat anticipation, we first fitted simple multilevel moderated mediation models (table 2). Indirect effects of all markers of stress on intensity of PE via negative affect were significant at conventional levels (P < .05) in all groups. This indicated that an increase of stress was associated with higher levels of negative affect, which, in turn, was associated with more intense PE. The indirect effect of event- and activity-related stress was greater in ARMS than in controls (P < .05).
Table 2.
Total, Direct, and Conditional Indirect Effects of Best Fitting (Simple) Multilevel Moderated Mediation Models of Stress, Negative Affect, Threat Anticipation, Aberrant Salience, and Psychotic Experiencesa
| FEP | ARMS | Controls | ||||
|---|---|---|---|---|---|---|
| Adj. B (95% CI) | P | Adj. B (95% CI) | P | Adj. B (95% CI) | P | |
| Pathways via affective disturbance | ||||||
| Event-related stress, negative affect, psychotic experiences | ||||||
| Direct effect (event-related stress → psychotic experiences) | 0.007 (−0.018 to 0.033) | .558 | −0.002 (−0.037 to 0.032) | .900 | 0.002 (−0.013 to 0.018) | .789 |
| Indirect effectb (event-related stress → negative affect → psychotic experiences) | 0.035 (0.011 to 0.065) | .011 | 0.053 (0.035 to 0.074) | <.001 | 0.026 (0.015 to 0.039) | <.001 |
| Total effect | 0.042 (0.002 to 0.083) | .040 | 0.050 (0.016 to 0.085) | .005 | 0.028 (0.005 to 0.050) | .016 |
| Activity-related stress, negative affect, and psychotic experiences | ||||||
| Direct effect (activity-related stress → psychotic experiences) | 0.053 (0.027 to 0.079) | <.001 | 0.061 (0.028 to 0.093) | <.001 | 0.015 (−0.008 to 0.037) | .198 |
| Indirect effectb (activity-related stress → negative affect → psychotic experiences) | 0.085 (0.055 to 0.122) | <.001 | 0.100 (0.066 to 0.138) | <.001 | 0.055 (0.037 to 0.077) | <.001 |
| Total effect | 0.138 (0.097 to 0.180) | <.001 | 0.161 (0.116 to 0.206) | <.001 | 0.070 (0.034 to 0.106) | <.001 |
| Social stress, negative affect, and psychotic experiences | ||||||
| Direct effect (social stress → psychotic experiences) | −0.017 (−0.046 to 0.013) | .262 | 0.024 (0.001 to 0.046) | .039 | 0.012 (−0.005 to 0.029) | .155 |
| Indirect effectb (social stress → negative affect → psychotic experiences) | 0.052 (0.029 to 0.079) | <.001 | 0.070 (0.044 to 0.100) | <.001 | 0.048 (0.031 to 0.068) | <.001 |
| Total effect | 0.035 (−0.009 to 0.078) | .115 | 0.094 (0.060 to 0.127) | <.001 | 0.060 (0.030 to 0.089) | <.001 |
| Pathways via aberrant salience | ||||||
| Event-related stress, aberrant salience, psychotic experiences | ||||||
| Direct effect (event-related stress → psychotic experiences) | 0.058 (0.020 to 0.095) | .003 | 0.055 (0.023 to 0.087) | <.001 | 0.030 (0.007 to 0.053) | .010 |
| Indirect effectb (event-related stress → aberrant salience → psychotic experiences) | −0.015 (−0.027 to −0.004) | .011 | −0.005 (−0.017 to 0.004) | .363 | −0.002 (−0.006 to 0.002) | .363 |
| Total effect | 0.043 (0.002 to 0.083) | .038 | 0.050 (0.015 to 0.085) | .005 | 0.028 (0.005 to 0.050) | .015 |
| Activity-related stress, aberrant salience, psychotic experiencesc | — | — | — | |||
| Social stress, aberrant salience, psychotic experiences | ||||||
| Direct effect (social stress → psychotic experiences) | 0.038 (−0.004 to 0.080) | .075 | 0.094 (0.064 to 0.124) | <.001 | 0.061 (0.033 to 0.088) | <.001 |
| Indirect effectb (social stress → aberrant salience → psychotic experiences) | −0.003 (−0.015 to 0.008) | .541 | −0.001 (−0.011 to 0.013) | .891 | −0.001 (−0.005 to 0.006) | .793 |
| Total effect | 0.035 (−0.009 to 0.078) | .115 | 0.094 (0.060 to 0.127) | <.001 | 0.060 (0.030 to 0.089) | <.001 |
| Negative affect, aberrant salience, psychotic experiences | ||||||
| Direct effect (negative affect → psychotic experiences) | ||||||
| Indirect effectb (negative affect→ aberrant salience → psychotic experiences) | 0.026 (−0.001 to 0.046) | .095 | 0.017 (−0.012 to 0.049) | .443 | 0.017 (−0.004 to 0.030) | .220 |
| Total effect | 0.187 (0.114 to 0.346) | <.001 | 0.237 (0.128 to 0.346) | <.001 | 0.173 (0.096 to 0.251) | <.001 |
| Threat anticipation, aberrant salience, psychotic experiences | ||||||
| Direct effect (threat anticipation → psychotic experiences) | 0.144 (0.092 to 0.196) | <.001 | 0.117 (0.073 to 0.161) | <.001 | 0.091 (0.058 to 0.124) | <.001 |
| Indirect effectb (threat anticipation → aberrant salience → psychotic experiences) | 0.004 (−0.008 to 0.022) | .563 | 0.002 (−0.009 to 0.017) | .813 | 0.008 (0.000 to 0.021) | .124 |
| Total effect | 0.148 (0.089 to 0.208) | <.001 | 0.119 (0.070 to 0.167) | <.001 | 0.099 (0.062 to 0.137) | <.001 |
| Pathways via threat anticipation | ||||||
| Event-related stress, threat anticipation, psychotic experiences | ||||||
| Direct effect (event-related stress → psychotic experiences) | 0.029 (−0.005 to 0.064) | .093 | 0.034 (0.002 to 0.066) | .036 | 0.020 (0.000 to 0.039) | .047 |
| Indirect effectb (event-related stress → threat anticipation → psychotic experiences) | 0.013 (0.003 to 0.027) | .034 | 0.016 (0.007 to 0.027) | .003 | 0.008 (0.003 to 0.015) | .008 |
| Total effect | 0.042 (0.002 to 0.083) | .038 | 0.050 (0.015 to 0.084) | .005 | 0.028 (0.005 to 0.050) | .015 |
| Activity-related stress, threat anticipation, psychotic experiences | ||||||
| Direct effect (activity-related stress → psychotic experiences) | 0.113 (0.078 to 0.148) | <.001 | 0.136 (0.098 to 0.175) | <.001 | 0.055 (0.025 to 0.085) | <.001 |
| Indirect effectb (activity-related stress → threat anticipation → psychotic experiences) | 0.025 (0.011 to 0.043) | .003 | 0.024 (0.011 to 0.039) | <.001 | 0.015 (0.007 to 0.024) | <.001 |
| Total effect | 0.138 (0.078 to 0.148) | <.001 | 0.160 (0.098 to 0.175) | <.001 | 0.070 (0.025 to 0.085) | <.001 |
| Social stress, threat anticipation, psychotic experiences | ||||||
| Direct effect (social stress → psychotic experiences) | 0.020 (−0.019 to 0.059) | .320 | 0.075 (0.045 to 0.104) | <.001 | 0.050 (0.026 to 0.075) | <.001 |
| Indirect effectb (social stress → threat anticipation → psychotic experiences) | 0.015 (0.003 to 0.031) | .043 | 0.018 (0.008 to 0.031) | .001 | 0.009 (0.003 to 0.017) | .008 |
| Total effect | 0.034 (−0.009 to 0.078) | .118 | 0.093 (0.059 to 0.127) | <.001 | 0.059 (0.030 to 0.089) | <.001 |
| Negative affect, threat anticipation, psychotic experiences | ||||||
| Direct effect (negative affect → psychotic experiences) | 0.315 (0.239 to 0.391) | .000 | 0.324 (0.235 to 0.412) | .000 | 0.252 (0.188 to 0.316) | .000 |
| Indirect effectb (negative affect → threat anticipation → psychotic experiences) | 0.030 (0.014 to 0.053) | .002 | 0.015 (−0.001 to 0.033) | .072 | 0.019 (0.009 to 0.031) | .001 |
| Total effect | 0.345 (0.257 to 0.433) | .000 | 0.339 (0.250 to 0.428) | .000 | 0.271 (0.199 to 0.343) | .000 |
Note: FEP, first-episode psychosis; ARMS, at-risk mental state for psychosis; SD, standard deviation; df, degrees of freedom; CI, confidence interval; significant indirect paths (P < .05) are presented in bold.
aAdjusted for age, gender, ethnicity, level of education, employment status, area-related stress and outsider status.
bDifference in indirect effects across groups (Δ indirect effects).
cModel estimation did not terminate normally.
| ARMS vs Controls | FEP vs Controls | FEP vs ARMS | ||||
|---|---|---|---|---|---|---|
| Adj. B (95% CI) | P | Adj. B (95% CI) | P | Adj. B (95% CI) | P | |
| Δ Indirect effects | ||||||
| Event-related stress → negative affect → psychotic experiences | 0.009 (−0.003 to 0.020) | .129 | 0.004 (−0.009 to 0.018) | .582 | −0.005 (−0.020 to 0.012) | .520 |
| Event-related stress → aberrant salience → psychotic experiences | −0.004 (−0.020 to 0.008) | .404 | −0.011 (−0.021 to −0.001) | .037 | −0.006 (−0.021 to −0.001) | .370 |
| Event-related stress → negative affect → threat anticipation → psychotic experiences | 0.000 (−0.000 to 0.000) | .824 | 0.000 (−0.000 to 0.001) | .301 | 0.000 (−0.000 to 0.001) | .431 |
| Activity-related stress → negative affect → psychotic experiences | 0.018 (0.001 to 0.036) | .039 | 0.017 (−0.001 to 0.037) | .072 | −0.001 (−0.022 to 0.021) | .928 |
| Activity-related stress → threat anticipation → psychotic experiences | −0.001 (−0.008 to 0.006) | .848 | 0.006 (−0.001 to 0.013) | .084 | 0.007 (−0.002 to 0.015) | .126 |
| Activity-related stress → negative affect → threat anticipation → psychotic experiences | 0.000 (−0.001 to 0.001) | .994 | 0.001 (0.000 to 0.002) | .062 | 0.001 (−0.000 to 0.003) | .109 |
| Social stress → negative affect → psychotic experiences | −0.004 (−0.018 to 0.012) | .642 | −0.004 (−0.017 to 0.009) | .534 | −0.001 (−0.017 to 0.015) | .950 |
| Social stress → negative affect → threat anticipation → psychotic experiences | 0.000 (−0.001 to 0.000) | .379 | 0.000 (−0.000 to 0.001) | .446 | 0.000 (−0.000 to 0.001) | .141 |
| Negative affect → threat anticipation → psychotic experiences | −0.001 (−0.006 to 0.004) | .659 | 0.005 (−0.001 to 0.011) | .115 | 0.006 (−0.000 to 0.014) | .090 |
Models including pathways from stress to PE via threat anticipation showed that, in all 3 groups, the effects of event-related, activity-related, and social stress on PE were mediated via enhanced threat anticipation, with a similar magnitude of indirect effects across groups (table 2).
When we examined models of stress, aberrant salience, and PE, there was a negative indirect effect of event-related stress on PE via aberrant salience in FEP individuals (B = −0.015, P = .011). When we inspected individual paths of this negative indirect effect, this indicated that higher levels of event-related stress were associated with less intense experiences of aberrant salience (B = −0.079, P = .010), which was, in turn, associated with less intense PE (B = 0.190, P < .001) in FEP individuals.
Turning to models of affective disturbance, threat anticipation, and PE (table 2), some of the effects of affective disturbance on more intense PE were mediated via enhanced threat anticipation, independently of stress, in FEP individuals, controls and, at trend level, ARMS individuals. There was no evidence of an indirect effect of affective disturbance on PE via aberrant salience in any of the groups.
Inspecting, finally, the model of threat anticipation, aberrant salience, and PE, the indirect effects of threat anticipation on PE via aberrant salience fell short of statistical significance in all 3 groups (table 2).
Final Multiple Moderated Mediation Model
When we probed findings from simple moderated mediation models further, and examined indirect effects of stress, affective disturbance, threat anticipation, and aberrant salience in the multiple multilevel moderated mediation model, there was evidence that the indirect effects of all markers of stress on PE via more intense negative affect remained significant in all (all P < .049; table 3, supplementary figure 1). The relative contribution of this indirect effect, from stress to PE through negative affect, was larger than the contribution of other indirect pathways. This was especially apparent in pathways from activity-related stress to PE, in which the total and total indirect effects were mostly accounted for by indirect effects through negative affect. The specific indirect effect from activity-related stress to PE via negative affect was significantly greater in ARMS than controls (B = 0.018, P = .039) and, at trend level, in FEP individuals than controls (B = 0.017, P = .072).
Table 3.
Total, Direct, and Conditional Indirect Effects of Multiple Multilevel Moderated Mediation Models of Stress on Psychotic Experiences Via Negative Affect, Threat Anticipation and Aberrant Saliencea
| FEP | ARMS | Controls | ||||
|---|---|---|---|---|---|---|
| Adj. B (95% CI) | P | Adj. B (95% CI) | P | Adj. B (95% CI) | P | |
| Event-related stress | ||||||
| Direct effect (event-related stress → psychotic experiences) | 0.015 (−0.008 to 0.038) | .192 | −0.005 (−0.030 to 0.021) | .731 | 0.000 (−0.013 to 0.013) | .965 |
| Total indirect effect (event-related stress) | 0.005 (−0.010 to 0.021) | .574 | 0.012 (−0.005 to 0.027) | .124 | 0.008 (0.001 to 0.016) | .030 |
| Specific indirect effectsb | ||||||
| Event-related stress → negative affect → psychotic experiences | 0.012 (0.001 to 0.025) | .049 | 0.017 (0.007 to 0.027) | .001 | 0.008 (0.033 to 0.014) | .002 |
| Event-related stress → aberrant salience → psychotic experiences | −0.012 (−0.023 to −0.004) | .009 | −0.006 (−0.017 to 0.002) | .207 | −0.002 (−0.006 to 0.001) | .278 |
| Event-related stress → threat anticipation → psychotic experiences | 0.005 (−0.000 to 0.010) | .072 | 0.001 (−0.001– 0.004) | .236 | 0.002 (−0.000 to 0.003) | .073 |
| Event-related stress → negative affect → threat anticipation → psychotic experiences | 0.000 (−0.000 to 0.001) | .092 | 0.000 (−0.000 to 0.001) | .222 | 0.000 (0.000 to 0.000) | .036 |
| Total effect (event-related stress) | 0.020 (−0.010 to 0.050) | .194 | 0.008 (−0.021 to 0.037) | .602 | 0.008 (−0.007 to 0.023) | .312 |
| Activity-related stress | ||||||
| Direct effect (activity-related stress → psychotic experiences) | 0.051 (0.021 to 0.081) | .001 | 0.034 (0.007 to 0.060) | .014 | 0.004 (−0.015 to 0.022) | .708 |
| Total indirect effect (activity-related stress) | 0.058 (0.037 to 0.081) | .000 | 0.061 (0.040 to 0.084) | .000 | 0.034 (0.022 to 0.048) | .000 |
| Specific indirect effectsb | ||||||
| Activity-related stress → negative affect → psychotic experiences | 0.046 (0.030 to 0.064) | <.001 | 0.047 (0.033 to 0.062) | <.001 | 0.029 (0.020 to 0.039) | <.001 |
| Activity-related stress → aberrant salience → psychotic experiences | −0.001 (−0.010 to 0.010) | .896 | 0.009 (−0.004 to 0.025) | .219 | 0.000 (−0.004 to 0.005) | .949 |
| Activity-related stress → threat anticipation → psychotic experiences | 0.011 (0.005 to 0.017) | <.001 | 0.004 (−0.002 to 0.010) | .191 | 0.005 (0.002 to 0.008) | .004 |
| Activity-related stress → negative affect → threat anticipation → psychotic experiences | 0.002 (0.001 to 0.003) | .003 | 0.001 (−0.000 to 0.001) | .201 | 0.001 (0.000 to 0.001) | .007 |
| Total effect (activity-related stress) | 0.109 (0.075 to 0.142) | .000 | 0.094 (0.061 to 0.128) | .000 | 0.038 (0.012 to 0.063) | .003 |
| Social stress | ||||||
| Direct effect (social stress → psychotic experiences) | −0.029 (−0.058 to −0.001) | .044 | 0.001 (−0.021 to 0.022) | .962 | −0.001 (−0.014 to 0.012) | .844 |
| Total indirect effect (social stress) | 0.018 (0.004 to 0.031) | .010 | 0.013 (−0.004 to 0.031) | .136 | 0.019 (0.009 to 0.030) | .000 |
| Specific indirect effectsb | ||||||
| Social stress → negative affect → psychotic experiences | 0.017 (0.008 to 0.028) | .001 | 0.018 (0.006 to 0.032) | .006 | 0.021 (0.013 to 0.031) | <.001 |
| Social stress → aberrant salience → psychotic experiences | −0.003 (−0.014 to 0.005) | .466 | −0.006 (−0.016 to 0.004) | .239 | −0.004 (−0.009 to 0.001) | .129 |
| Social stress → threat anticipation → psychotic experiences | 0.003 (−0.002 to 0.008) | .220 | 0.001 (−0.000 to 0.004) | .285 | 0.001 (−0.000 to 0.002) | .326 |
| Social stress → negative affect → threat anticipation → psychotic experiences | 0.001 (0.000 to 0.001) | .009 | 0.000 (−0.000 to 0.001) | .201 | 0.000 (0.000 to 0.001) | .013 |
| Total effect (social stress) | −0.012 (−0.044 to 0.021) | .481 | 0.014 (−0.013 to 0.041) | .318 | 0.018 (0.003 to 0.032) | .017 |
| Negative affect | ||||||
| Direct effect | 0.255 (0.197 to 0.314) | .000 | 0.260 (0.192 to 0.327) | .000 | 0.220 (0.173 to 0.267) | .000 |
| Total indirect effect | ||||||
| Negative affect → threat anticipation → psychotic experiences | 0.009 (0.004 to 0.015) | .002 | 0.003 (−0.001 to 0.007) | .188 | 0.004 (0.002 to 0.007) | .002 |
| Total effect (negative affect) | 0.264 (0.203 to 0.325) | .000 | 0.263 (0.196 to 0.329) | .000 | 0.224 (0.176 to 0.271) | .000 |
| Threat anticipation | ||||||
| Direct effect (threat anticipation → psychotic experiences) | 0.075 (0.044 to 0.106) | .000 | 0.019 (−0.009 to 0.046) | .184 | 0.033 (0.014 to 0.052) | .001 |
| Aberrant salience | ||||||
| Direct effect (aberrant salience → psychotic experiences) | 0.156 (0.105 to 0.207) | .000 | 0.210 (0.142 to 0.278) | .000 | 0.134 (0.086 to 0.183) | .000 |
Note: FEP, first-episode psychosis; ARMS, at-risk mental state for psychosis; SD, standard deviation; df, degrees of freedom; CI, confidence interval; correlated mediators, r (negative affect, aberrant salience) = −.02, P = .667, r (aberrant salience, threat anticipation) = .34, P = .001; significant specific indirect paths (P < .05) are presented in bold. Overview of total, direct, and indirect effects of significant paths from simple moderated multilevel mediation models (table 2).
aAdjusted for age, gender, ethnicity, level of education, employment status, area-related stress, and outsider status.
bDifference in specific indirect effects across groups (Δ indirect effects):
| ARMS vs controls | FEP vs controls | FEP vs ARMS | ||||
|---|---|---|---|---|---|---|
| Adj. B (95% CI) | P | Adj. B (95% CI) | P | Adj. B (95% CI) | P | |
| Δ Indirect effects | ||||||
| Event-related stress → negative affect → psychotic experiences | 0.027 (0.004 to 0.050) | .023 | 0.009 (−0.017 to 0.041) | .536 | −0.018 (−0.049 to 0.018) | .295 |
| Activity-related stress → negative affect → psychotic experiences | 0.045 (0.005 to 0.086) | .030 | 0.030 (−0.007 to 0.070) | .125 | −0.015 (−0.063 to 0.033) | .544 |
| Social stress → negative affect → psychotic experiences | 0.022 (−0.011 to 0.057) | .195 | 0.004 (−0.026 to 0.036) | .801 | −0.018 (−0.056 to 0.019) | .335 |
| Event-related stress → threat anticipation → psychotic experiences | 0.007 (−0.011 to 0.018) | .212 | 0.005 (−0.008 to 0.028) | .468 | −0.002 (−0.025 to 0.006) | .757 |
| Activity-related stress → threat anticipation → psychotic experiences | 0.010 (−0.010 to 0.047) | .250 | 0.010 (−0.007 to 0.030) | .277 | 0.001 (−0.020 to 0.023) | .961 |
| Social stress → threat anticipation → psychotic experiences | 0.009 (−0.003 to 0.023 | .160 | 0.006 (−0.009 to 0.023) | .482 | −0.004 (−0.020 to 0.014) | .688 |
| Negative affect → threat anticipation → psychotic experiences | −0.004 (−0.024 to 0.017) | .721 | 0.011 (−0.009 to 0.036) | .307 | 0.015 (−0.009 to 0.036) | .240 |
Turning to pathways from stress via threat anticipation to more intense PE, the indirect effects of activity-related stress via enhanced threat anticipation remained significant in FEP individuals (B = 0.011, P < .001) and controls (B = 0.005, P = .004), independently of pathways via negative affect, but was attenuated and ceased to be statistically significant in ARMS individuals. Further, there was evidence in FEP individuals and controls that some of the effects of activity-related and social stress were mediated via threat anticipation followed by negative affect and, then, PE. While the indirect effect of event-related stress on PE via aberrant salience remained significant in FEP individuals (B = −0.012, P = .009), there was strong evidence of a direct effect of aberrant salience on more intense PE in all three groups (independent of all other direct and indirect effects).
The indirect effect of negative affect on PE via threat anticipation remained significant, independently of the effects of stress, in FEP individuals and controls in the multiple mediation model. However, we found no significant indirect effects of affective disturbance and threat anticipation via aberrant salience.
Discussion
Principal Findings
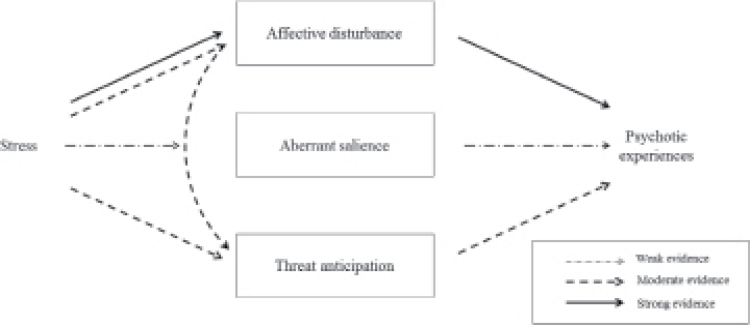
This study sought to move beyond previous experience sampling investigations of single psychological processes in daily life to investigate specific pathways derived from contemporary models of psychosis and examine how momentary stress, affective disturbance, threat anticipation, and aberrant salience combine in the development of PE (figure 2). We found strong and consistent evidence that momentary stress increases the intensity of PE via pathways through affective disturbance in FEP individuals, ARMS individuals, and controls, with only weak evidence of greater indirect effects in FEP and ARMS individuals than controls. There was further evidence that the effects of activity-related stress via threat anticipation remained significant, independently of pathways via affective disturbance, in FEP individuals and controls but not ARMS individuals. We also found some evidence of pathways from activity-related and social stress via affective disturbance followed by threat anticipation and, then, PE in FEP individuals and controls. A negative indirect effect was evident for the pathway of event-related stress on PE via aberrant salience in FEP individuals. We found no evidence of indirect effects of affective disturbance and threat anticipation via aberrant salience. The latter retained, however, a significant direct effect on PE.
Fig. 2.
Schematic representation of main findings across groups. This figure gives an overview of indirect effects of stress on psychotic experiences via pathways through affective disturbance, enhanced threat anticipation, and aberrant salience. Only findings with at least one significant indirect path in at least one group were considered in this representation. See supplementary figure 1 for a detailed breakdown of significant (P < .05) indirect effects for each group and marker of stress. For pathways through affective disturbance, strong and consistent evidence ( ) was observed across all 3 groups. For pathways through threat anticipation as well as through affective disturbance and threat anticipation (
) was observed across all 3 groups. For pathways through threat anticipation as well as through affective disturbance and threat anticipation ( ), the strength and consistency of evidence was, overall, moderate across the 3 groups. Overall, weak and inconsistent evidence was found for pathways through aberrant salience (
), the strength and consistency of evidence was, overall, moderate across the 3 groups. Overall, weak and inconsistent evidence was found for pathways through aberrant salience ( ).
).
Methodological Considerations
The current findings should be viewed in the light of potential limitations. First, we used cross-sectional and not time-lagged, multilevel moderated mediation models to investigate specific pathways due to sample size restrictions, providing insufficient power for fitting such computationally intensive models. This did not allow us to examine the temporal order of these variables as one important criterion for establishing causality. Hence, analyses using time-lagged models of larger samples are now needed to further elucidate the complex interplay of, and potential reciprocal associations between, psychological processes and momentary stress over time. However, the current study was the first to investigate and systematically test, in daily life, the indirect effects of stress on PE via pathways through affective disturbance, threat anticipation, aberrant salience and PE that have been repeatedly proposed in conceptual models of psychosis. Specifically, we tested a comprehensive, fully adjusted multiple multilevel moderated mediation model in a sample of controls, ARMS individuals, and FEP individuals, allowing us, at the same time, to minimize the potential impact of illness chronicity and other consequences of psychotic disorder. As such, this study advances previous research using network modeling of ESM data,43–46 which have not yet investigated indirect effects of stress, negative affect and other psychological mechanisms in the development of PE.
Second, ESM data collection is time-intensive and possibly associated with assessment burden for participants and, in turn, selection bias. However, previous research has shown that the ESM is a feasible, reliable, and valid assessment method in various populations.16,17,30,47 Applying this method enabled us to study the interplay of psychological processes in everyday life where these processes and their association with PE naturally occur.
Third, the magnitude of the indirect effects was, overall, small, with the greatest indirect effects being evident for pathways from stress to negative affect to PE. This was particularly evident for the longer indirect pathways via negative affect and threat anticipation. In mediation analyses using the product of coefficients strategy, longer indirect pathways are, by definition, of smaller magnitude, given their computation is based on the product of a higher number of individual path coefficients. In the current study, individual path coefficients (supplementary figure 1) were of similar magnitude to what has been observed in previous ESM studies. In ESM studies, effects of this magnitude may be considered important given they occur in the flow of daily life and, thereby, have a considerable cumulative impact on individuals over time.48 However, while total and total indirect effects of the indirect pathway with the largest magnitude from activity-related stress to PE were mostly accounted for by specific indirect effects through negative affect, even for this pathway a fair proportion of the total effect was still explained by the direct effect, suggesting evidence of partial mediation via this pathway. Hence, a number of other unmeasured factors and mechanisms may be operating on this and other pathways investigated that would need to be added before full mediation of the effects of stress on PE may be observed. Also, while indirect pathways of stress via affective disturbance were specifically related to intensity of PE as an outcome, differences in magnitude of indirect effects across the 3 groups were, overall, small, and most differences were not statistically significant at conventional levels, possibly due to limited statistical power to detect such small differences. However, it is noteworthy in this context that ARMS and FEP individuals reported, on average, higher levels of stress, negative affect, aberrant salience, threat anticipation, and PE than controls (supplementary table 2). This tentatively suggests that, even if the magnitude of differences in indirect effects across groups was small, the greater prevalence of stress in ARMS and FEP individuals may contribute to the development of PE via pathways through negative affect (and, in FEP individuals, higher levels of negative affect via threat anticipation and so forth).
Fourth, we investigated a number of a priori hypothesized, specific indirect effects of event-related, area-related and social stress via 3 distinct pathways (affective disturbance, aberrant salience, threat anticipation), which reflects the complexity of current models of the aetiology of psychosis. This may have, nonetheless, inflated type I error and resulted in over- or under-estimation of indirect effects. Therefore, careful replication in independent samples is required before firm conclusions can be drawn. However, pathways to psychosis have frequently been tested in isolation, thereby, ignoring the complexity involved and the potential impact of unmeasured impact or confounding by other pathways. All specific indirect effects reported in the final multiple moderated mediation model were included simultaneously to examine their relative contribution, which reflects a considerable advance over previous research, primarily testing pathways via affective disturbance, threat anticipation, and aberrant salience in isolation.
Comparison With Previous Research
Recently, a number of integrated models of psychosis have implicated stress, affective and cognitive processes in the onset of psychosis and specifically posited that, in individuals with heightened vulnerability of biopsychosocial origin, the effects of stress on PE are mediated via pathways through affective disturbances, anomalous experiences, and cognitive biases.3–7,13,22,23 While these models are now common ground and highly cited in psychosis research, attempts to systematically test comprehensive models of the complex interplay between psychological processes and stressful contexts and experiences in the origins of psychosis remain sparse.21,22
Elevated emotional reactivity to minor stressors has received great attention as a putative underlying mechanism in psychotic disorders.13,16,17 Individuals with increased familial and psychometric risk for psychosis have been found to experience an increased emotional reactivity to minor stressors in daily life.16,17,49,50 More generally, various models of psychosis have posited that the effects of stress are mediated via affective disturbance3–5 and may reflect what has previously been coined an affective pathway to psychosis.13 Our findings provide new evidence in support of this proposition, as this is the first ESM study to report that affective disturbance mediates the link from momentary stress to PE in daily life across different stages of early psychosis. In contrast to findings from previous research suggesting some degree of specificity for certain types of stressors for the formation of PE,18 we found evidence that the effects of all stress variables (ie, event-related, activity-related, and social stress) were mediated via pathways through affective disturbances. Further, while indirect effects of activity-related stress were greatest, there was no strong evidence of differences in magnitude of indirect effects via affective disturbance for different types of stressors.
Changes in the emotional response to stress have moreover been linked to cognitive biases such as enhanced anticipation of threat.23,27 It has been suggested that enhanced threat anticipation combines with affective disturbance in the development of PE.4,27 However, the precise nature of this pathway remained unclear. The current results point toward a link from stressful contexts and experiences to affective disturbance, followed by threat anticipation and, in turn, the formation of PE. This corroborates the prominent role ascribed to (stress-induced) affective disturbances such as symptoms of anxiety, which cognitive models of psychosis consider to be key in enhancing anticipation of threat and, in turn, intensity of PE.23,27 However, this pathway via enhanced threat anticipation was attenuated and ceased to be statistically significant in ARMS individuals, while controlling for pathways via affective disturbance in our final adjusted model. This finding may tentatively suggest a greater relevance of affective pathways rather than pathways via threat anticipation in the prodromal period of psychosis when a considerable proportion experience comorbid anxiety and depression.51
We did not find evidence in support of our hypotheses that aberrant salience mediated the effects of threat anticipation and negative affect on PE. What is more, event-related stress was associated with a slight decrease in aberrant salience, which, in turn, was associated with less intense PE in FEP individuals, who all (but one) received prior or ongoing treatment with antipsychotic medication. While tentative, the effects of antipsychotic medication may in part explain the finding of event-related stress on decreased aberrant salience in FEP individuals.28 More importantly, however, aberrant salience retained, independently of stress, a substantial direct effect on PE, which supports previous propositions by cognitive models and neurobiological approaches4,28 that experiences of aberrant salience occur as a result of dopamine release independent of cue and context due to hyperactivity of the mesolimbic dopaminergic system.28 In other words, augmented levels of aberrant salience may not be due to current contextual factors such as momentary stress, but primarily play a role in the formation of PE if genes, early neurological insults and adverse social environments impacted and sensitized the dopaminergic system at a developmentally earlier stage.3–5 Clinically, our findings suggest that the antipsychotic effects on dopamine dysregulation in FEP individuals may target one potential pathway, but not the pathways of stress via affective disturbance and threat anticipation on psychosis to the same extent.
Conclusions
This study provides evidence on the interplay between psychological processes and stress in the origins of psychosis and, thereby, contributes to improving our understanding of psychoses as disorders with very complex aetiologies. Our findings underscore the important role that affective disturbance, particularly emotional reactivity, and threat anticipation may play as putative mechanisms through which stress impacts on the formation of PE. Evidence on the psychological processes, and their interplay with stress, underlying the occurrence and persistence of PE in daily life is vital for gaining a better understanding of when and how to intervene to reduce intensity of PE. This, then, provides the basis for translational research using ecological interventionist causal models targeting these psychological processes in daily life through novel, personalized ecological momentary interventions that deliver treatment in the real-world and in real-time, tailored to what individuals need in a given moment and context through interactive delivery schemes.11,52 Developing and evaluating these interventions with the goal of promoting resilience to stress and achieving sustainable change in intended psychosis outcomes under real-world conditions is of considerable public health importance and an important next step toward preventing onset and improving long-term outcomes of psychosis.
Supplementary Material
Supplementary data are found at Schizophrenia Bulletin online.
Funding
This work was supported by a Postdoctoral Research Fellowship of the UK National Institute for Health Research (NIHR-PDF-201104065 to U.R.); a Veni grant from the Netherlands Organisation for Scientific Research (451-13-022 to U.R.); Wellcome Trust (WT087417 to C.M.); National Institute for Health Research (NIHR) Biomedical Research Centre for Mental Health at South London and Maudsley NHS Foundation Trust and King’s College London; and an ERC consolidator grant (ERC-2012-StG, project 309767—INTERACT to I.M.-G.). This work is an approved add-on study of the “The European Network of National Networks studying Gene-Environment Interactions in Schizophrenia” (EU-GEI), which is supported by funding from the European Union (European Community’s Seventh Framework Program [HEALTH-F2-2009–241909; Project EU-GEI]).
Supplementary Material
References
- 1. Linscott RJ, van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. 2013;43:1133–1149. [DOI] [PubMed] [Google Scholar]
- 2. van Os J, Linscott RJ. Introduction: the extended psychosis phenotype–relationship with schizophrenia and with ultrahigh risk status for psychosis. Schizophr Bull. 2012;38:227–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Howes OD, Murray RM. Schizophrenia: an integrated sociodevelopmental-cognitive model. Lancet. 2014;383:1677–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Garety PA, Bebbington P, Fowler D, Freeman D, Kuipers E. Implications for neurobiological research of cognitive models of psychosis: a theoretical paper. Psychol Med. 2007;37:1377–1391. [DOI] [PubMed] [Google Scholar]
- 5. Morgan C, Charalambides M, Hutchinson G, Murray RM. Migration, ethnicity, and psychosis: toward a sociodevelopmental model. Schizophr Bull. 2010;36:655–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Akdeniz C, Tost H, Meyer-Lindenberg A. The neurobiology of social environmental risk for schizophrenia: an evolving research field. Soc Psychiatry Psychiatr Epidemiol. 2014;49:507–517. [DOI] [PubMed] [Google Scholar]
- 7. Reininghaus U, Morgan C. Integrated models in psychiatry: the state of the art. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1–2. [DOI] [PubMed] [Google Scholar]
- 8. Garety PA, Fowler DG, Freeman D, Bebbington P, Dunn G, Kuipers E. Cognitive–behavioural therapy and family intervention for relapse prevention and symptom reduction in psychosis: randomised controlled trial. Br J Psychiatry. 2008;192:412–423. [DOI] [PubMed] [Google Scholar]
- 9. Malla A, Iyer S, McGorry P, et al. From early intervention in psychosis to youth mental health reform: a review of the evolution and transformation of mental health services for young people. Soc Psychiatry Psychiatr Epidemiol. 2016;51:319–326. [DOI] [PubMed] [Google Scholar]
- 10. McGorry PD, Nelson B, Goldstone S, Yung AR. Clinical staging: a heuristic and practical strategy for new research and better health and social outcomes for psychotic and related mood disorders. Can J Psychiatry. 2010;55:486–497. [DOI] [PubMed] [Google Scholar]
- 11. Reininghaus U, Depp CA, Myin-Germeys I. Ecological interventionist causal models in psychosis: targeting psychological mechanisms in daily life. Schizophr Bull. 2016;42:264–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Reininghaus U, Kempton MJ, Valmaggia L, et al. Stress sensitivity, aberrant salience, and threat anticipation in early psychosis: an experience sampling study. Schizophr Bull. 2016;42:712–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Myin-Germeys I, van Os J. Stress-reactivity in psychosis: evidence for an affective pathway to psychosis. Clin Psychol Rev. 2007;27:409–424. [DOI] [PubMed] [Google Scholar]
- 14. Collip D, Nicolson NA, Lardinois M, Lataster T, van Os J, Myin-Germeys I; G.R.O.U.P Daily cortisol, stress reactivity and psychotic experiences in individuals at above average genetic risk for psychosis. Psychol Med. 2011;41:2305–2315. [DOI] [PubMed] [Google Scholar]
- 15. Lataster T, Wichers M, Jacobs N, et al. Does reactivity to stress cosegregate with subclinical psychosis? A general population twin study. Acta Psychiatr Scand. 2009;119:45–53. [DOI] [PubMed] [Google Scholar]
- 16. Myin-Germeys I, van Os J, Schwartz JE, Stone AA, Delespaul PA. Emotional reactivity to daily life stress in psychosis. Arch Gen Psychiatry. 2001;58:1137–1144. [DOI] [PubMed] [Google Scholar]
- 17. Palmier-Claus JE, Dunn G, Lewis SW. Emotional and symptomatic reactivity to stress in individuals at ultra-high risk of developing psychosis. Psychol Med. 2012;42:1003–1012. [DOI] [PubMed] [Google Scholar]
- 18. Reininghaus U, Gayer-Anderson C, Valmaggia L, et al. Psychological processes underlying the association between childhood trauma and psychosis in daily life: an experience sampling study. Psychol Med. 2016;46:2799–2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Thewissen V, Bentall RP, Oorschot M, et al. Emotions, self-esteem, and paranoid episodes: an experience sampling study. Br J Clin Psychol. 2011;50:178–195. [DOI] [PubMed] [Google Scholar]
- 20. Varghese D, Scott J, Welham J, et al. Psychotic-like experiences in major depression and anxiety disorders: a population-based survey in young adults. Schizophr Bull. 2011;37:389–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bentall RP, Rowse G, Shryane N, et al. The cognitive and affective structure of paranoid delusions: a transdiagnostic investigation of patients with schizophrenia spectrum disorders and depression. Arch Gen Psychiatry. 2009;66:236–247. [DOI] [PubMed] [Google Scholar]
- 22. Fowler D, Hodgekins J, Garety P, et al. Negative cognition, depressed mood, and paranoia: a longitudinal pathway analysis using structural equation modeling. Schizophr Bull. 2012;38:1063–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington PE. A cognitive model of persecutory delusions. Br J Clin Psychol. 2002;41:331–347. [DOI] [PubMed] [Google Scholar]
- 24. Kramer I, Simons CJ, Wigman JT, et al. Time-lagged moment-to-moment interplay between negative affect and paranoia: new insights in the affective pathway to psychosis. Schizophr Bull. 2014;40:278–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wigman JT, van Nierop M, Vollebergh WA, et al. Evidence that psychotic symptoms are prevalent in disorders of anxiety and depression, impacting on illness onset, risk, and severity—implications for diagnosis and ultra-high risk research. Schizophr Bull. 2012;38:247–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Freeman D, Garety P. Advances in understanding and treating persecutory delusions: a review. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1179–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Freeman D, Dunn G, Fowler D, et al. Current paranoid thinking in patients with delusions: the presence of cognitive-affective biases. Schizophr Bull. 2013;39:1281–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kapur S. Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. Am J Psychiatry. 2003;160:13–23. [DOI] [PubMed] [Google Scholar]
- 29. Howes OD, Kapur S. The dopamine hypothesis of schizophrenia: version III–the final common pathway. Schizophr Bull. 2009;35:549–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Myin-Germeys I, Oorschot M, Collip D, Lataster J, Delespaul P, van Os J. Experience sampling research in psychopathology: opening the black box of daily life. Psychol Med. 2009;39:1533–1547. [DOI] [PubMed] [Google Scholar]
- 31. European Network of National Networks studying Gene-Environment Interactions in Schizophrenia (EU-GEI). Identifying gene–environment interactions in schizophrenia: contemporary challenges for integrated, large-scale investigations. Schizophr Bull. 2014;40:729–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 33. Fusar-Poli P, Byrne M, Badger S, Valmaggia LR, McGuire PK. Outreach and support in south London (OASIS), 2001–2011: ten years of early diagnosis and treatment for young individuals at high clinical risk for psychosis. Eur Psychiatry. 2013;28:315–326. [DOI] [PubMed] [Google Scholar]
- 34. Yung AR, Yuen HP, McGorry PD, et al. Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. Aust N Z J Psychiatry. 2005;39:964–971. [DOI] [PubMed] [Google Scholar]
- 35. First MB, Gibbon M. The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II). 2004. [Google Scholar]
- 36. Ryan JJ, Weilage ME, Spaulding WD. Accuracy of the seven subtest WAIS-R short form in chronic schizophrenia. Schizophr Res. 1999;39:79–83. [DOI] [PubMed] [Google Scholar]
- 37. Myin-Germeys I, Delespaul P, van Os J. Behavioural sensitization to daily life stress in psychosis. Psychol Med. 2005;35:733–741. [DOI] [PubMed] [Google Scholar]
- 38. Muthen LK, Muthen B. Mplus version 7. Los Angeles, CA: MPlus; 1998–2016. [Google Scholar]
- 39. Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: theory, methods, and prescriptions. Multivariate Behav Res. 2007;42:185–227. [DOI] [PubMed] [Google Scholar]
- 40. Bauer DJ, Preacher KJ, Gil KM. Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: new procedures and recommendations. Psychol Methods. 2006;11:142–163. [DOI] [PubMed] [Google Scholar]
- 41. Selig JP, Preacher KJ. Monte Carlo Method for Assessing Mediation: An Interactive Tool for Creating Confidence Intervals for Indirect Effects [Computer software]. http://quantpsy.org/.
- 42. Preacher KJ. Advances in mediation analysis: a survey and synthesis of new developments. Annu Rev Psychol. 2015;66:825–852. [DOI] [PubMed] [Google Scholar]
- 43. Wigman JT, van Os J, Borsboom D, et al. ; MERGE. Exploring the underlying structure of mental disorders: cross-diagnostic differences and similarities from a network perspective using both a top-down and a bottom-up approach. Psychol Med. 2015;45:2375–2387. [DOI] [PubMed] [Google Scholar]
- 44. Pe ML, Kircanski K, Thompson RJ, et al. Emotion-network density in major depressive disorder. Clin Psychol Sci. 2015;3:292–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bringmann LF, Vissers N, Wichers M, et al. A network approach to psychopathology: new insights into clinical longitudinal data. PLoS One. 2013;8:e60188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wichers M, Wigman J, Myin-Germeys I. Micro-level affect dynamics in psychopathology viewed from complex dynamical system theory. Emot Rev. 2015;7:362–367. [Google Scholar]
- 47. Edwards CJ, Cella M, Tarrier N, Wykes T. The optimisation of experience sampling protocols in people with schizophrenia. Psychiatry Res. 2016;244:289–293. [DOI] [PubMed] [Google Scholar]
- 48. Lardinois M, Lataster T, Mengelers R, Van Os J, Myin-Germeys I. Childhood trauma and increased stress sensitivity in psychosis. Acta Psychiatr Scand. 2011;123:28–35. [DOI] [PubMed] [Google Scholar]
- 49. Devylder JE, Ben-David S, Schobel SA, Kimhy D, Malaspina D, Corcoran CM. Temporal association of stress sensitivity and symptoms in individuals at clinical high risk for psychosis. Psychol Med. 2013;43:259–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Collip D, Myin-Germeys I, Van Os J. Does the concept of “sensitization” provide a plausible mechanism for the putative link between the environment and schizophrenia? Schizophr Bull. 2008;34:220–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Fusar-Poli P, Nelson B, Valmaggia L, Yung AR, McGuire PK. Comorbid depressive and anxiety disorders in 509 individuals with an at-risk mental state: impact on psychopathology and transition to psychosis. Schizophr Bull. 2014;40:120–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Steinhart H, Myin-Germeys I, Reininghaus U. Translating treatment of mental health problems to daily life: a guide to the development of ecological momentary interventions. In: Palmier-Claus JE, Haddock G, Varese F, eds. A Guide to Experiences Sampling in Mental Health Research and Practice. In press. [Google Scholar]
- 53. Preacher KJ, Selig JP. Advantages of Monte Carlo confidence intervals for indirect effects. Commun Methods Meas. 2012;6:77–98. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.