Abstract
In Korea, herbal remedies have been widely used to treat polycystic ovarian syndrome (PCOS). We report the case of a woman with obese-type PCOS who was successfully treated with Korean herbal medicine (KHM) and lifestyle management. A 23-year-old female patient was first examined at our clinic in April 2015. She had amenorrhea for the previous 9 months and presented with obesity and abnormal reproductive hormone levels. She was treated using KHM and lifestyle management. We observed her menstrual cycles and re-evaluated her hormonal levels during the treatment. After KHM therapy, her body weight decreased from 88.2 kg to 66.7 kg. Her menstrual cycles resumed regularly, and the serum levels of the hormones had normalized. No adverse effects on liver and renal functions were observed. This study indicates that KHM might be considered an option for treating women with obese-type PCOS. Further large-scale trials are needed.
Keywords: Korean herbal medicine, menstruation, obesity, ovulation, polycystic ovarian syndrome
1. Introduction
Polycystic ovarian syndrome (PCOS) is diagnosed on the basis of oligo-ovulation or anovulation, hyperandrogenism (HA; either clinical or biochemical), and the presence of polycystic ovaries.1 The prevalence of PCOS is as high as 15% when the Rotterdam criteria are applied.2 In PCOS, fertility is adversely affected by an individual being overweight, having HA, and having an elevated serum concentration of luteinizing hormone (LH).3
Obesity causes relative hyperandrogenemia, characterized by reduced levels of sex hormone binding globulin and increased bioavailable androgens delivered to the target tissues. Moreover, obesity increases the risk of metabolic syndromes such as diabetes mellitus, dyslipidemia, and insulin resistance (IR).4, 5 Therefore, weight loss [in women with a body mass index (BMI) of >25 kg/m2 (overweight)] and prevention of weight gain [in women with a BMI <25 kg/m2 (lean)] are the responsibility of all health professionals who care for women with PCOS.3
PCOS has been treated with herbal remedies and lifestyle management in Korean medicine clinics. Although the evidence was limited by small sample size and low quality of methodologies, herbal medicines have a similar efficacy as Western antiobesity drugs but with fewer reported adverse effects.6 However, there have been few published studies in which these treatments were evaluated using key hormone levels for the obese type of PCOS. Herein, we report the case of a woman with obese-type PCOS, in which the patient’s menstrual cycle and reproductive hormone levels normalized with Korean herbal medicine (KHM) therapy and lifestyle management.
2. Case Report
A 23-year-old woman was followed-up in the Conmaul hospital of Korean medicine from April 2015 to December 2016. Written informed consent was obtained from the patient. She was obese and had been trying to reduce her body weight by self-management including low-calorie diet and exercises, but was unsuccessful. Her BMI was 33.9 kg/m2 (body weight, 88.2 kg; height, 161.4 cm) at the first visit and, and she was having amenorrhea since August 2014. A polycystic ovarian morphology was confirmed on transvaginal ultrasonography by an experienced obstetric and gynecologist. She had high levels of LH, testosterone, dehydroepiandrosterone sulfate, and hemoglobin A1c. She had not undergone any previous surgery. She was diagnosed with PCOS (Table 1).
Table 1.
Body weight and serum hormone levels throughout the treatment course.
| Variable | April 2015 | May 2016 | October 2016 |
|---|---|---|---|
| Body weight (kg) | 88.2 | 67.0 | 66.0 |
| BMI (kg/m2) | 33.9 | 25.7 | 25.3 |
| FSH (mIU/mL) | 5.67 | 4.53 | 4.33 |
| LH (mIU/mL) | 14.61 | 2.74 | 3.09 |
| E2 (pg/mL) | 28.15 | 33.15 | 8.13 |
| Testosterone (ng/mL) | 1.43 | 1.01 | 0.81 |
| DHEA-S (μg/dL) | 1024.4 | 736.2 | 542.9 |
| SHBG (nmol/L) | 10 | 21.1 | 30.8 |
| AMH (ng/mL) | 5.91 | 5.56 | 3.77 |
| Total cholesterol (mg/dL) | 159 | 128 | 143 |
| HDL cholesterol (mg/dL) | 53 | 54 | 60 |
| LDL cholesterol (mg/dL) | 89 | 67 | 75 |
| AST (IU/L) | 24 | 18 | 13 |
| ALT (IU/L) | 22 | 8 | 8 |
| Creatinine (mg/dL) | 0.9 | 0.8 | 0.8 |
AMH, antimullerian hormone; ALT, alanine transminase; AST, asparte transminase; BMI, body mass index; DHEA-S, dehydroepiandrosterone sulfate; E2, estradiol; FSH, follicular stimulating hormone; HDL, high-density lipoprotein; LDL, low-density lipoprotein; LH, luteinizing hormone; SHBG, sex hormone binding globulin.
2.1. Therapeutic intervention
2.1.1. KHM therapy
Considering the long period of amenorrhea, she received progesterone for withdrawal bleeding, prior to KHM therapy. She received two courses of KHM therapy, of 5 months and 2 months duration, respectively. The daily dose and components of KHM are presented in Table 2. Each plant material was mixed and decocted with purified water. This KHM was administered three times a day, prior to each meal. The patient did not receive any conventional treatment while receiving KHM therapy.
Table 2.
Composition and daily dose of Korean herbal medicine.
| Medicinal plants (Chinese word) | Dosages (g) |
|---|---|
Coicis Semen ( ) ) |
46 |
Rehmanniae Radix ( ) ) |
33 |
Radix Angelicae ( ) ) |
12 |
Ephedrae Herba ( ) ) |
12 |
Astragali Radix ( ) ) |
9 |
Dioscoreae Rhizoma ( ) ) |
9 |
Cnidii Rhizoma ( ) ) |
7 |
Citri Unshius Pericarpium ( ) ) |
7 |
Poria ( ) ) |
7 |
Acanthopanacis Cortex ( ) ) |
7 |
Magnoliae Cortex ( ) ) |
6 |
Coptidis Rhizoma ( ) ) |
4 |
Gardeniae Fructus ( ) ) |
4 |
Cyperi Rhizoma ( ) ) |
4 |
Foeniculi Fructus ( ) ) |
4 |
Glycyrrhizae Radix et Rhizoma ( ) ) |
4 |
| Total | 175 |
2.1.2. Lifestyle management
She was educated to take a low-calorie diet, including low glycemic index and protein rich foods (800–1000 kcal/d). In addition, she was recommended resistance or weight-bearing exercise in combination with aerobic exercise twice per week. She received in-person counseling sessions with a trained interventionist (JL), who provided encouragement, goal setting, and problem-solving instructions every week during two courses of KHM therapy.
2.2. Follow-up and outcomes
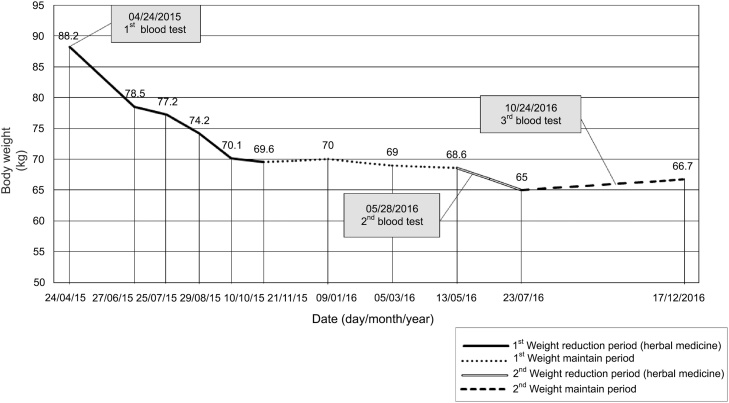
After 13 months and 18 months of treatment, a second and third blood test including reproductive hormones, lipid profiles, and liver function tests of the patient were conducted. The levels of LH, testosterone, dehydroepiandrosterone sulfate, AMH decreased, whereas the levels of sex hormone binding globulin increased. The results of blood testing prior to and after KHM therapy are shown in Table 1. After the treatment, body weight reduced from 88.2 kg to 66.7 kg. The changes in body weight during the treatment are shown in Fig. 1. In addition, the patient’s menstrual cycles gradually became regular (once a month) from November 2015 to the present date. A normal ovarian morphology was confirmed on transvaginal ultrasonography by an experienced obstetric and gynecologist. No adverse effects on liver and renal function were observed during the treatment.
Fig. 1.
Body weight changes throughout the treatment course.
3. Discussion
We report a case of a woman with obese-type PCOS, in which the patient’s menstrual cycles and reproductive hormone levels normalized with KHM therapy and lifestyle management. After the treatment, her body weight reduced from 88.2 kg to 66.7 kg. Moreover, she was able to maintain her body weight at 65 kg until now (June 2017). No adverse effects on liver and renal function were observed during the course of KHM treatment.
Currently, dietary interventions involving caloric restriction are recommended to treat both reproductive and metabolic abnormalities in obese women with PCOS.7 Modest reductions in energy intake (500–1000 kcal/d) and weight (5–10%) have been shown to normalize gonadotropin secretion, reduce clinical and biochemical HA, and improve insulin sensitivity in this population.8 However, for obese women with PCOS, weight loss is not easy to achieve because the management of established obesity is challenging. Therefore, encouraging women to reduce weight and engage in regular self-monitoring of weight can help women overcome obesity and recognize even small increments in weight.9
Regular, moderate-intensity aerobic exercise over a short period improves reproductive outcomes, including ovulation and menstrual cycle regulation, in addition to reducing weight and IR, in overweight women with PCOS.10 Exercise alone also improves clinical outcomes without significant weight change, and therefore, goals for exercise must focus on overall health benefits and not on weight loss alone.9
The herbal remedy that was prescribed to the patient is known to be effective in reducing weight in Korean medicine clinics.11, 12 A study of the herbal medicine in rats has shown that the reduction in weight was attributable to decreased energy intake and increased energy expenditure and fat oxidation.12 The improvement in energy homeostasis was associated with the enhancement of the hypothalamic leptin signaling pathway.12 The water extracts of Coicis Semen, one of the major ingredients of KHM prescribed, decreased food intake and body weight in rats with diet-induced obesity and reduced leptin and tumor necrosis factor α messenger RNA expression in the white adipose tissues.13 The herbal medicine including Ephedrae Herba was effective in decreasing visceral adiposity and IR in obese women with impaired glucose tolerance.14
There are several limitations to our study. First, our study included only one case; thus, more cases are needed to confirm the effect of KHM therapy. Second, it is possible to argue that the weight reduction was simply the result of caloric restriction. However, it is not easy to reduce weight by as much as 21.5 kg through caloric restriction alone. The goal of KHM treatment is to support the weight reduction efficiently and safely; therefore, our case report could add to the available evidence that KHM therapy might be a reasonable option for obese women in clinical practice.
Despite these limitations, we believe that our results are noteworthy, because this case was evaluated for key related hormones, lipid profiles, and liver function, and was followed for 1.5 years. The results of the present study demonstrate the clinical potency of treatment of obese-type PCOS with KHM therapy. Further large-scale randomized controlled trials with elaborate designs should be performed to verify the clinical efficacy of KHM for obese-type PCOS.
Conflicts of interest
All authors have no conflicts of interest to declare.
References
- 1.Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81:19–25. doi: 10.1016/j.fertnstert.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 2.Fauser B.C., Tarlatzis B.C., Rebar R.W., Legro R.S., Balen A.H., Lobo R. Consensus on women’s health aspects of polycystic ovary syndrome (PCOS): the Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop Group. Fertil Steril. 2012;97:28–38.e25. doi: 10.1016/j.fertnstert.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 3.Balen A.H., Morley L.C., Misso M., Franks S., Legro R.S., Wijeyarante C.N. The management of anovulatory infertility in women with polycystic ovary syndrome: an analysis of the evidence to support the development of global WHO guidance. Hum Reprod Update. 2016;22:687–708. doi: 10.1093/humupd/dmw025. [DOI] [PubMed] [Google Scholar]
- 4.Pasquali R., Gambineri A., Pagotto U. The impact of obesity on reproduction in women with polycystic ovary syndrome. BJOG. 2006;113:1148–1159. doi: 10.1111/j.1471-0528.2006.00990.x. [DOI] [PubMed] [Google Scholar]
- 5.Pasquali R. Obesity and androgens: facts and perspectives. Fertil Steril. 2006;85:1319–1340. doi: 10.1016/j.fertnstert.2005.10.054. [DOI] [PubMed] [Google Scholar]
- 6.Sui Y., Zhao H.L., Wong V.C., Brown N., Li X.L., Kwan A.K. A systematic review on use of Chinese medicine and acupuncture for treatment of obesity. Obes Rev. 2012;13:409–430. doi: 10.1111/j.1467-789X.2011.00979.x. [DOI] [PubMed] [Google Scholar]
- 7.Jarrett B.Y., Lujan M.E. Impact of hypocaloric dietary intervention on ovulation in obese women with PCOS. Reproduction. 2017;153:R15–R27. doi: 10.1530/REP-16-0385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moran L.J., Hutchison S.K., Norman R.J., Teede H.J. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2011 doi: 10.1002/14651858.CD007506.pub2. Cd007506. [DOI] [PubMed] [Google Scholar]
- 9.Joham A.E., Palomba S., Hart R. Polycystic ovary syndrome, obesity, and pregnancy. Semin Reprod Med. 2016;34:93–101. doi: 10.1055/s-0035-1571195. [DOI] [PubMed] [Google Scholar]
- 10.Harrison C.L., Lombard C.B., Moran L.J., Teede H.J. Exercise therapy in polycystic ovary syndrome: a systematic review. Hum Reprod Update. 2011;17:171–183. doi: 10.1093/humupd/dmq045. [DOI] [PubMed] [Google Scholar]
- 11.Kim S.M., Kim K.S. Effect of Chegamuiyiin-tang and electro-lipolysis acupuncture on the reduction of body fat. J Korean Med Obes Res. 2002;2:13–23. [Google Scholar]
- 12.Park S., Lee J.B., Daily J.W. Anti-obesity effects of Chang-Chul-Eui-Ee-In-Tang [see text] in female rats with diet-induced obesity. Chin J Integr Med. 2011;17:925–932. doi: 10.1007/s11655-011-0936-3. [DOI] [PubMed] [Google Scholar]
- 13.Kim S.O., Yun S.J., Jung B., Lee E.H., Hahm D.H., Shim I. Hypolipidemic effects of crude extract of adlay seed (Coix lachrymajobi var. mayuen) in obesity rat fed high fat diet: relations of TNF-alpha and leptin mRNA expressions and serum lipid levels. Life Sci. 2004;75:1391–1404. doi: 10.1016/j.lfs.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 14.Hioki C., Yoshimoto K., Yoshida T. Efficacy of bofu-tsusho-san, an oriental herbal medicine, in obese Japanese women with impaired glucose tolerance. Clin Exp Pharmacol Physiol. 2004;31:614–619. doi: 10.1111/j.1440-1681.2004.04056.x. [DOI] [PubMed] [Google Scholar]