Abstract
Background
Individuals with certain communicable diseases may pose risks to the health of the traveling public; there has been documented transmission on commercial aircraft of tuberculosis (TB), measles, and severe acute respiratory syndrome (SARS). Federal public health travel restrictions (PHTR) prevent commercial air or international travel of persons with communicable diseases that pose a public health threat.
Methods
We described demographics and clinical characteristics of all cases considered for PHTR because of suspected or confirmed communicable disease from May 22, 2007, to December 31, 2015.
Results
We reviewed 682 requests for PHTR; 414 (61%) actions were completed to place 396 individuals on PHTR. The majority (>99%) had suspected (n = 27) or confirmed (n = 367) infectious pulmonary TB; 58 (16%) had multidrug-resistant-TB. There were 128 (85%) interceptions that prevented the initiation or continuation of travel. PHTR were removed for 310 (78%) individuals after attaining noninfectious status and 86 (22%) remained on PHTR at the end of the analysis period.
Conclusions
PHTR effectively prevent exposure during commercial air travel to persons with potentially infectious diseases. In addition, they are effective tools available to public health agencies to prevent commercial travel of individuals with certain communicable diseases and possibly reconnect them with public health authorities.
Keywords: Travel, Restrictions, Tuberculosis
1. Background
Although the overall likelihood appears low, there is documented evidence of transmission on commercial aircraft of communicable diseases such as tuberculosis (TB), measles, and severe acute respiratory syndrome (SARS) [1], [2], [3], [4], [5], [6], posing a risk to the health of the traveling public. The public health Do Not Board (DNB) list and Public Health Border Lookout (PHLO) record are mechanisms to prevent travel by an individual who is infectious with a communicable disease that poses a threat to public health and whose travel plans are under United States (U.S.) authorities.
The DNB list was developed in 2007 to prevent people who are infectious or likely infectious with a communicable disease that poses a public health threat from boarding commercial flights that have departures within, to, or from the U.S [7]. A PHLO is issued to complement the DNB, alerting the Department of Homeland Security (DHS) when a person who has been placed on these lists tries to enter the U.S. at any port of entry (seaport, airport, land border). These federal public health travel restrictions are managed by the Centers for Disease Control and Prevention (CDC) and implemented by DHS and its component agencies. Whenever a person is added to or removed from the DNB list, their record is added to or removed from the PHLO concurrently. A state or local health department typically initiates requests for travel restrictions; however, other agencies such as the U.S. Department of State or foreign public health authorities may also request travel restrictions.
In March 2015, CDC refined the criteria it considers when placing a person on federal travel restrictions [8]. Under the revised criteria, the individual must be known or believed to be infectious with, or exposed to, a communicable disease that would pose a public health threat should the individual travel, and additionally must meet at least one of the following three criteria: 1) be unable to be located, be unaware of diagnosis, be aware but noncompliant with public health requests, or have shown potential for noncompliance; 2) be at risk of traveling on a commercial flight or of traveling internationally by any means; or 3) need to be placed on the DNB list and issued a PHLO for effective response to an outbreak of a communicable disease or enforcement of a public health order [7]. The impetus for revising the criteria was to allow the DNB and PHLO to support a communicable disease outbreak. Revisions expanded the first criterion to allow travel restrictions to be considered for individuals with a known or believed exposure to a communicable, versus solely being confirmed or likely infectious with a communicable disease. An additional criterion was added allowing for placement on travel restrictions as part of a response to an outbreak of a communicable disease or a public health order for individuals who met the exposure criterion. The final revision was that individuals did not need to meet all listed criteria for placement, but rather meet the first criterion pertaining to known infectiousness or exposure plus only one of the other three criteria [8]. The sole criterion for removal from federal travel restrictions did not change: proof that the person is noninfectious or no longer at risk of becoming infectious, typically evidenced by laboratory documentation, lapse of the known period of infectiousness, or lapse of the incubation period without development of symptoms [8].
CDC confers with the requesting agency to gather information relevant to determining if the individual meets the criteria for placement on travel restrictions. Depending on the communicable disease of interest, CDC determines if the individual is infectious based on available clinical and laboratory data. For individuals with TB, CDC uses a detailed algorithm, developed by TB experts, to determine if an individual is infectious. If an individual is determined to meet criteria for placement and the requesting agency concurs with placement on travel restrictions, CDC coordinates actions for placement with DHS. Travel restrictions can be applied to any individual regardless of citizenship or country location.
To date, federal public health travel restrictions have been used primarily for TB, but they may be considered for other communicable diseases that pose a serious public health threat during travel, such as viral hemorrhagic fevers or measles [7], [8].
2. Methods
The objectives of our analysis were to describe the cohort of individuals placed under travel restrictions since inception and demonstrate the effectiveness of travel restrictions in preventing commercial air travel of individuals with communicable disease who are identified by health agencies and meet criteria for placement. For all individuals for whom travel restrictions are requested, CDC maintains case records in its Quarantine Activity Reporting System (QARS), a secure, restricted-access database [9]. Demographic and clinical information is obtained from the requesting agency, typically local and state health departments, as well as evidence that the addition and removal criteria are met, dates and times of significant events leading to addition or removal of federal travel restrictions, and outcomes following removal. We reviewed de-identified case data for all individuals considered for or placed on travel restrictions because of a suspected or confirmed communicable disease from May 22, 2007, to December 31, 2015; individuals considered for or placed on travel restriction related to an exposure to a communicable disease were not included in this analysis. CDC determined that this analysis did not meet the definition of research and was not subject to review by the CDC Institutional Review Board.
We summarized the number of requests for consideration of travel restrictions, the states, countries or agencies that made the request, and whether the request resulted in addition to the DNB and PHLO. Poisson regression was used to determine if the number of consultations for travel restrictions has significantly increased over time. Individuals could have multiple requests for consideration of travel restrictions and multiple DNB/PHLO actions.
For all individuals placed on travel restrictions, we examined demographics including country of citizenship, sex, age, and location at time of DNB and PHLO placement (i.e., within or outside the U.S.). We dichotomized status of individuals as either 1) U.S. citizens or U.S. lawful permanent residents (LPR) or 2) foreign nationals, i.e., individuals who held immigrant or non-immigrant visas, were visiting from a visa-waiver country, were undocumented, or had an unknown status.
We described the communicable diseases for which individuals were added to the DNB list and issued a PHLO. For those with suspected or confirmed TB, we described the final diagnosis based on laboratory confirmation of disease and categorized drug resistance as: 1) confirmed multidrug-resistant TB (MDR TB), defined as TB resistant to at least isoniazid and rifampin; 2) confirmed extensively drug-resistant TB (XDR TB), defined as TB resistant to isoniazid and rifampin plus any fluoroquinolone and at least one of the three injectable second-line drugs [10]; or 3) confirmed non-XDR TB or non-MDR TB, which included mono-resistance to isoniazid or rifampin. Since removal from the DNB and PHLO for individuals with TB requires follow-up and treatment until noninfectious, we calculated the time each person spent on the list, which reflected the amount of time before becoming noninfectious and subsequent removal from travel restriction status.
DHS notifies CDC when individuals listed on the DNB and PHLO try to travel; subsequently, individuals are often intercepted prior to or during travel. We examined interception events and dichotomized events as an individual attempting to obtain a boarding pass for a commercial flight departing within, to, or from the U.S. or as an interception occurring at a U.S. land border port of entry. We examined whether clinical follow up and referral to treatment were initiated after individuals on the DNB list and accompanying PHLO were intercepted before air travel or at a port of entry.
We also compared DNB/PHLO processing times before and after 2011, when CDC and DHS leveraged a secure, Web-based information-sharing platform managed by DHS [11], for sharing information including DNB/PHLO actions.
All analyses were performed in SAS version 9.3, and we assessed significance at p < 0.05.
3. Results
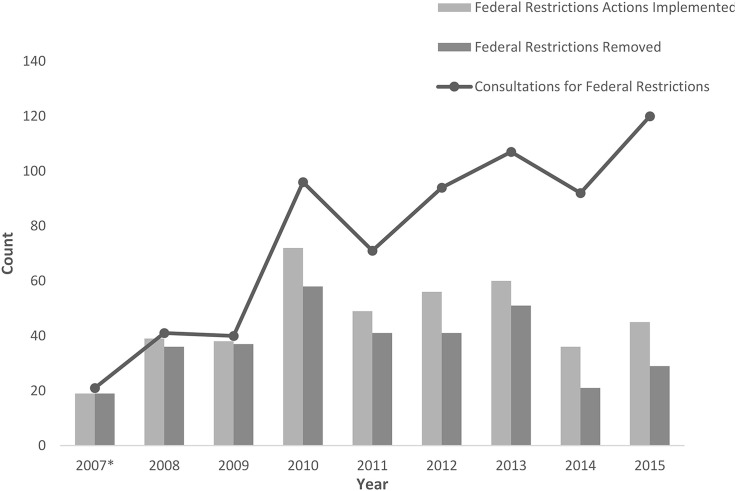
During the analysis period, state health departments, U.S. federal agencies and foreign ministries of health made 682 requests for federal public health travel restrictions. A total of 46 state health departments, as well as the health departments for the District of Columbia, Guam, Puerto Rico, made 621 (91%) of all requests for federal public health travel restrictions; the California and Texas state health departments made the most requests: 168 and 73, respectively. U.S. federal agencies only accounted for three (0.5%) placement requests, with one initiated by CDC and two by the U.S. Department of State. Nine foreign ministries of health made 58 (8.5%) requests; the majority of these requests (50) came from the public health authority in Canada. Requests for travel restriction consultations increased significantly each year since the inception of the DNB and PHLO (p < 0.0001) (Fig. 1 ), averaging 75 consultation requests per calendar year. Requests increased from 41 in 2008 to 120 in 2015.
Fig. 1.
Federal public health travel restriction consultations, actions implemented, and removals by year, 2007-2015.
After examining data accompanying requests and considering established criteria, 414 (61%) additions were initiated, representing 396 individuals; 17 (4%) individuals were added to the DNB and PHLO more than once. There were 328 removal actions, representing 310 (78%) individuals who had been removed from the DNB and PHLO by the end of the analysis period; 86 (21%) individuals, including five who had been placed multiple times, remained on the DNB list and with a PHLO at the end of the analysis period (Table 1 ). Of the 414 DNB/PHLO addition actions, 186 (45%) were for individuals who were within the U.S. at the time of placement; 195 (47%) were outside the U.S., and 33 (8%) had unknown whereabouts.
Table 1.
Characteristics of individuals placed on federal public health travel restrictions, 2007–2015 (N = 396).
| Variable | N (%) | |
|---|---|---|
| Age (average) | 45.5 | |
| Sex | Male | 266 (67) |
| Female | 130 (33) | |
| Citizenship | U.S. citizen/lawful permanent resident | 209 (53) |
| Non U.S. citizen/lawful permanent residenta | 146 (37) | |
| Unknown status | 41 (10) | |
| Country of citizenship | United States | 112 (28) |
| Mexico | 49 (12) | |
| India | 29 (7) | |
| China | 23 (6) | |
| Canada | 19 (5) | |
| Vietnam | 17 (4) | |
| Philippines | 13 (3) | |
| Pakistan | 10 (2.5) | |
| Otherb | 80 (20) | |
| Unknown | 44 (11) | |
| Location at time of placementc | Within the U.S. | 178 (45) |
| Outside the U.S. | 188 (47) | |
| Unknown | 30 (8) | |
| Communicable disease of interest | TB | 394 (99) |
| Measles | 2 (1) | |
| Number of placements on travel restrictions | One | 379 (96) |
| Two | 16 (4) | |
| Three | 1 (0.2) | |
| Attempted to travel while under travel restrictions |
Yes | 92 (23) |
| No | 304 (77) | |
| Travel restrictions statusd | Remain on travel restrictions | 86 (22) |
| Removed from travel restrictions | 310 (78) |
Includes individuals with immigration status of immigrant, non-immigrant visa holder, citizen of visa-waiver country, undocumented/illegal or other.
Countries where <10 individuals reported as citizenship country.
For individuals who were placed on travel restrictions multiple times, their location at time of placement is represented by their location at the time of their first placement on travel restrictions.
Individual status as of the end of analysis period: 2015 December 31.
Of the 396 individuals placed on the DNB and PHLO, the average age was 45.5 (range 9–89 years) and 67% were male. Of those, 209 (53%) were U.S. citizens or lawful permanent residents (LPR), 146 (37%) were non-U.S. citizens or did not have a LPR status and 41 (10%) had an unknown U.S. citizenship status. The most frequently reported countries of citizenship for the entire cohort were the U.S. (112, 28%), Mexico (49, 12%), India (29, 7%), China (11, 6%), Canada (19, 5%), Vietnam (17, 4%) and the Philippines (13, 3%); 44 (11%) individuals had an unknown country of citizenship (Table 1).
The majority (412, 99.5%) of the DNB/PHLO addition actions were for individuals with suspected or confirmed infectious pulmonary TB; two were for confirmed measles. The 412 additions for TB represented 394 individuals; 367 individuals (93%) had TB confirmed by culture or molecular diagnostic testing; three (0.8%) were diagnosed clinically and treated for infectious TB without laboratory confirmation; 12 (3%) had a final diagnosis of noninfectious or latent TB infection. Twelve (3%) individuals were placed on DNB/PHLO with a presumptive diagnosis of infectious TB but subsequently determined not to have TB; the final diagnoses for these individuals included nontuberculous mycobacterial infections, lung cancer, and other respiratory infections. Of those with a confirmed diagnosis of infectious TB (367), 58 (16%) had MDR TB and six (2%) had XDR TB. Of the 17 individuals added more than once, 16 had confirmed TB (six with MDR TB) and one had a clinical diagnosis of TB; 16 were added twice and one three times following a known lapse in treatment or after having been lost to follow-up with unknown treatment status and presumed infectiousness.
Of 384 restrictions placed for individuals with confirmed infectious TB, 298 (78%) were removed after these individuals met criteria adjudicating them as noninfectious; 86 (22%) remained under travel restrictions at the end of the analysis period. The removals were associated with initiation of or continued treatment (218, 73%), return to treatment following an interruption (33, 11%), or completion of treatment (9, 3%); treatment outcomes were not documented for 38 (13%) removal actions. Individuals added for suspected TB but subsequently determined not to have infectious TB were removed as soon as this determination was made, a median duration of 27 days (range 2–327 days). The two individuals with measles were removed on the fifth day after rash onset when no longer infectious. The median duration on the DNB/PHLO for those who had been removed by the end of the analysis period was 67 days, with a range of 23 h to 1538 days (approximately 4 years). The median duration for the 86 people who remained on the DNB and PHLO at the end of the analysis period was significantly longer (p < 0.0001) at 1065 days; 71 (82%) of these individuals were considered lost to follow up at the end of the analysis period.
CDC was notified of 150 attempts to travel while on federal travel restrictions, representing 92 individuals. There were 128 (85%) interceptions during attempted international travel; 27 (21%) of them prevented commercial air travel, and 96 (75%) occurred at a U.S. land-border port of entry. Five (4%) occurred after the individuals traveled by commercial aircraft despite DNB placement but were detected by DHS mid-itinerary or upon arrival. CDC staff were notified to facilitate public health interventions upon arrival. In 22 (15%) instances, individuals had confirmed travel reservations but did not try to travel. One person circumvented the DNB by taking a domestic flight without interception.
Of the 92 travelers who were intercepted because of the DNB or PHLO, 60 (65%) became noninfectious through treatment after a single interception and were removed from the DNB and PHLO status; 20 (22%) were removed after two or three interception events, and four (4%) were removed after four or more events. Only eight (9%) of the 86 people who remained on the DNB and PHLO at the end of the analysis period had been intercepted one or more times and did not result in DNB removal (Table 2 ).
Table 2.
Travel restriction status of individuals by number of interception events, 2007–2015 (n = 92).
|
Status of individual |
Interception count |
Total |
||
|---|---|---|---|---|
| 1 | 2–3 | ≥4 | N (%) | |
| Removed from Travel Restrictions | 60a | 20b | 4 | 84 (91) |
| Remain under Travel Restrictions | 6 | 1 | 1 | 8 (9) |
| Total N (%) |
66 (72) | 21 (23) | 5 (5) | 92 |
6 individuals were re-added to travel restrictions, 4 of whom were intercepted again before removal.
3 individuals were re-added to travel restrictions and were removed after achieving noninfectiousness.
In instances where one or more interceptions led to treatment and eventual removal from the DNB and PHLO (n = 76), those individuals who were denied an airline boarding pass met criteria for removal faster (n = 23, median = 62 days) than those intercepted at a U.S. land border (n = 46, median = 71 days), but the difference was not significant (p = 0.1327). Information on location of interception was not available for seven individuals.
After incorporating the secure, Web-based platform in December 2011 into the process for requesting and processing travel restrictions actions, analysis showed the median time for DNB and PHLO addition and removal processes decreased from 4.0 to 0.65 h (p < 0.0001) for placement and 4.43 to 0.62 h (p < 0.0001) for removal.
4. Conclusions
Since their inception in May 2007, federal public health travel restrictions have continued to be requested by domestic and foreign public health officials as a mechanism to prevent travel-related spread of communicable diseases. CDC periodically reviews epidemiologic data to assess transmission risk aboard commercial aircraft. These data along with level of morbidity and mortality are analyzed to decide whether threat justifies a travel restriction. As an example, based on data analyzed during an interstate outbreak of mumps, CDC concluded there was no evidence of transmission during air travel [3]. This along with its morbidity profile make it an unsuitable disease for a travel restriction.
An earlier report analyzing federal travel restrictions data reported that in the first year after the processes were implemented, there were 42 requests for placement, and 33 of those individuals (78%) met criteria and were placed on DNB and PHLO, representing an average of approximately three requests for placement and one actual addition per month [7]. Since the report was published in 2008, the average number of requests for travel restrictions has been increasing each year, and California and Texas have maintained the greatest number of requests. This increase in consultation requests may be due to increased awareness of federal travel restrictions because of outreach and training by CDC staff and experiences shared among state health departments.
A person may meet the infectiousness criterion for use of federal travel restrictions without laboratory confirmation if the state or local health department provides strong clinical evidence pointing to the suspicion that the individual has an active, infectious communicable disease, particularly TB, for which laboratory confirmation may be slow. Our review of data for people with suspected infectious TB who were placed on travel restrictions but later determined not to have infectious TB showed that, at time of DNB/PHLO placement, all were suspected of having infectious TB; final culture or molecular diagnostic testing results were unavailable or pending, so that a TB diagnosis could be not be confirmed or ruled out. The use of travel restrictions in approximately 6% of these patients who turn out not to have infectious TB appears reasonable when there is evidence that up to a fifth of patients with a clinical diagnosis of TB do not have bacteriologic evidence [12], [13]. Nonetheless, in the context of travel restrictions, these patients present a negligible risk of transmission.
The median time an individual was on travel restrictions was significantly shorter for those who had been removed than for those who remained on the list at the end of the analysis period, as the majority who remained on the list had been lost to follow up. CDC staff conduct regular case reviews and works with health departments to determine whether individuals are no longer infectious and can be removed from travel restrictions. Individuals on federal travel restrictions who are lost to follow up are maintained on the DNB and PHLO until they can be located, often through attempted travel, and can provide medical documentation to conclude that they are no longer infectious. Previous analyses have shown that those who are intercepted during travel across a land border are removed from the DNB/PHLO quicker than those who are not intercepted [14]. Our analysis also showed that the majority of travelers who were intercepted, either before boarding a commercial flight or at a land port of entry, achieved noninfectious status after a single interception event. This suggests that interception during travel provides a re-entry point to the public health system and an opportunity to reinitiate treatment and follow-up care by underscoring the importance of addressing their condition and protecting others.
CDC periodically reviews federal public health travel restriction processes and works with federal and state partners to address potential gaps. During the analysis period, six individuals were able to obtain boarding passes and fly on commercial aircraft despite being on the DNB list; all but one were detected during travel and intercepted at the arrival airport. Implementation of the Transportation Security Agency's (TSA) Secure Flight [15], an airline passenger prescreening program, in 2009 has resolved some issues identified in these instances. In addition, CDC works with state and local health departments to ensure all known aliases and identifiers are added to an individual's DNB and PHLO records to minimize the likelihood of evasion. When people have imminent travel scheduled while the DNB and PHLO additions are being processed, CDC and DHS staff work with state and local health departments to intercept them before flight departure even if they have already been issued a boarding pass or boarded an aircraft. Efforts to improve the travel restrictions process have also included the use of a secure, web-based platform to request DNB and PHLO actions. Since incorporation of this tool, administrative processing has been streamlined, improving data security and reducing the processing time for DNB/PHLO actions despite an increase in the number of requests and actions. Timely processing of DNB and PHLO actions ensures that travel is restricted only as long as necessary.
A limitation of this analysis was the inconsistent documentation in QARS of certain variables, specifically around treatment outcomes. The inconsistency was especially pronounced during the early years of the implementation of the DNB and PHLO tools, before a dedicated module was created in QARS to document these cases. CDC continues to address data quality and validity by refining the variables in the QARS database, by training staff to ensure accurate documentation of federal travel restrictions, and by evaluating the travel restrictions data collection and processes. In addition, the QARS cohort is limited to those cases of TB reported to CDC quarantine stations, generally by state and local health departments; thus the number of individuals prevented from traveling is small in comparison to the prevalence of TB both in the U.S. and globally [16].
Public health officials should be aware of the availability of federal public health travel restrictions and their advantages, such as finding individuals who need treatment for TB but have been lost to follow up and are suspected of traveling on commercial flights or crossing borders. For the cohort of individuals in our analysis who were placed on travel restrictions, any risk of transmission of infectious disease by these individuals during commercial air travel to the travel public was virtually eliminated (>99%); previous literature supports that infectious travelers have caused disease in other travelers [1], [2], [3], [4], [5], [6]. Similarly, travel restrictions may have saved federal and local resources used to conduct investigations of passengers with potential exposures when individuals fly while infectious with a communicable disease. More data needs to be collected and further analysis completed to determine the specific resource and cost savings and exact number of exposures prevented in the traveling public. CDC should continue to assess the use of federal travel restrictions, including evaluating the process and the impact these tools have on reducing communicable disease transmission.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
Acknowledgments
The authors would like to acknowledge Amy Jewett and Kirsten Buckley for their assistance in initial data management for this manuscript. The authors would also like to acknowledge the CDC Travel Restrictions and Interventions Activity, CDC Quarantine Station staff, and the Department of Homeland Security for their assistance and support of public health travel restriction actions.
Contributor Information
M. Robynne Jungerman, Email: Guk8@cdc.gov.
Laura A. Vonnahme, Email: kdy1@cdc.gov.
Faith Washburn, Email: Wlz5@cdc.gov.
Francisco Alvarado-Ramy, Email: Fba8@cdc.gov.
References
- 1.Mangili A., Gendreau M.A. Transmission of infectious diseases during commercial air travel. Lancet. 2005;365:989–996. doi: 10.1016/S0140-6736(05)71089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Driver C.R., Valway S.E., Morgan W., Onorato I.M., Castro K.G. TRansmission of mycobacterium tuberculosis associated with air travel. JAMA. 1994;272:1031–1035. doi: 10.1001/jama.1994.03520130069035. [DOI] [PubMed] [Google Scholar]
- 3.Nelson K., Marienau K., Schembri C., Redd S. Measles transmission during air travel, United States, December 1, 2008-December 31, 2011. Travel Med Infect Dis. 2013;11:81–89. doi: 10.1016/j.tmaid.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 4.Hagmann S.H.F., Christenson J.C. Measles and the risk posed by international travelers at the time of elimination or post-elimination. Travel Med Infect Dis. 2015;13:1–2. doi: 10.1016/j.tmaid.2014.12.017. [DOI] [PubMed] [Google Scholar]
- 5.Jost M., Luzi D., Metzler S., Miran B., Mutsch M. Measles associated with international travel in the region of the Americas, Australia and Europe, 2001–2013: a systematic review. Travel Med Infect Dis. 2015;13:10–18. doi: 10.1016/j.tmaid.2014.10.022. [DOI] [PubMed] [Google Scholar]
- 6.Huizer Y.L., Swaan C.M., Leitmeyer K.C., Timen A. Usefulness and applicability of infectious disease control measures in air travel: a review. Travel Med Infect Dis. 2015;13:19–30. doi: 10.1016/j.tmaid.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 7.Federal air travel restrictions for public health purposes - United States, june 2007-may 2008. Morb Mortal Wkly Rep. 2008;57:1009–1012. [PubMed] [Google Scholar]
- 8.CDC Criteria for requesting federal travel restrictions for public health purposes, including for viral hemorrhagic fevers. Fed Regist. 2015:16400–16402. 80 FR 1640. [Google Scholar]
- 9.Krishnamurthy R., Remis M., Brooke L., Miller C., Navin A., Guerra M. Quarantine activity reporting system (QARS) AMIA Annu Symp Proc. 2006;2006:990. [PMC free article] [PubMed] [Google Scholar]
- 10.CDC Drug-resistant TB. 2012. http://www.cdc.gov/tb/publications/factsheets/drtb/mdrtb.htm
- 11.Security D of H Homeland security information network (HSIN) 2013. 2014. http://hsin.dhs.gov
- 12.CDC Decrease in reported tuberculosis cases- United States, 2009. MMWR. 2010;59:289–294. [PubMed] [Google Scholar]
- 13.Dunlap N.E., Bass J., Fujiwara P., Hopewell P., Horsburgh C.R., Salfinger M. Diagnostic standards and classification of tuberculosis in adults and children. Am J Respir Crit Care Med. 2000;161:1376–1395. doi: 10.1164/ajrccm.161.4.16141. [DOI] [PubMed] [Google Scholar]
- 14.DeSisto C., Broussard K., Escobedo M., Borntrager D., Alvarado-Ramy F., Waterman S. Border Lookout: enhancing tuberculosis control on the United States–Mexico border. Am J Trop Med Hyg. 2015;93:747–751. doi: 10.4269/ajtmh.15-0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.TSA Secure flight program. 2014. https://www.tsa.gov/stakeholders/secure-flight-program 2014.
- 16.Glaziou P., Falzon D., Floyd K., Raviglione M. Global epidemiology of tuberculosis. Semin Respir Crit Care Med. 2013;34:3–16. doi: 10.1055/s-0032-1333467. [DOI] [PubMed] [Google Scholar]