Abstract
Total knee arthroplasty is a traditional surgical procedure aimed to restore function and relief pain in patients with severe knee osteoarthritis. Recently, many medial pivot knee systems were deigned to replicate the normal knee kinematic: a highly congruent medial compartment and a less conforming lateral tibial plateau characterize these devices. A slightly asymmetric soft tissue balancing is mandatory using medial pivot designs to obtain a correct and physiological knee biomechanics leading good outcomes and long survival rates. This article describes a new surgical technique using a modern third generation TKA design combined with wireless load–sensor tibial trials to improve the correct knee load balancing with a minimal conformity of the polyethylene insert. The use of wireless load–sensing tibial trials has several benefits: it is an intraoperative, objective and dynamic tool allowing surgeons to optimize in real time soft tissue balancing. The meaning of a “truly balanced knee” is still a controversial issue in the current literature.
Keywords: Total knee arthroplasty, TKA, Ligament balance, Alignment, Intraoperative sensors, Knee, Instability
1. Introduction
Soft tissue imbalance in total knee arthroplasty (TKA) has been estimated to cause up to 35% of early TKA revisions in the United States.1 Soft tissue balancing, however, remains entirely subjective and extremely operator dependent. Historically, two surgical techniques have been utilized by surgeons to create the “perfectly balanced” TKA: a “measured resection technique” and a “gap balancing technique.”
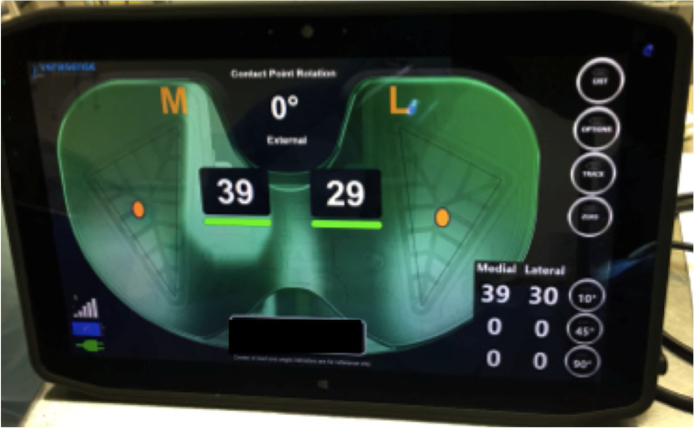
In the measured resection technique, the femoral component is rotated parallel to the surgical trans-epicondylar axis of the femur.2 In contrast, the determination of rotation using the gap balancing technique relies on the tension of the medial and lateral soft tissue sleeves with the knee at 90° of flexion.3 Independent of either technique used to determine proper femoral component rotation, manual stress testing, laminar spreaders, spacer blocks, and tensiometers are all used to assess intra-operative symmetry of the extension and flexion gaps.4 However, despite these tools, balancing the knee remains an inexact art with no standardized protocol to optimize tissue tension in TKA. The reason for this is bifactorial: it is extremely operator dependent and the relationship between soft tissue balance with regard to tibiofemoral contact stress during physiologic range of motion (ROM) remains unclear. Recent reports, including those from the author’s institution, have shown that the use of modern, third-generation TKA designs and instrumentation did not improve satisfaction rates in the TKA patient population.5, 6 Given this, studies show that using the minimum level of constraint to maintain stability has been related to a higher survivorship and patient satisfaction.7 Many surgeons, however, fearing mid-flexion instability as a cause for early revision,8 tend to over-constrain the knee resulting in loss of active ROM, point loading on the polyethylene insert, premature insert wear, and inferior implant survivorship.9 A more quantitative, and therefore more standardized, method of intra-operative detection of global soft tissue balancing and proper component alignment may help surgeons to optimize function and increase survivorship of TKA. Recently, intraoperative sensing technology (VERASENSE, Orthosensor, Dania, FL) (Fig. 1) has been presented as a way to give dynamic, real-time feedback regarding tibio-femoral position and quantitative pressure at peak contact points in the medial and lateral compartments during TKA trialing and final implant positioning. Using this sensor-derived data, the surgeon can intra-operatively track and evaluate inter-compartmental loading pressures during ROM and correct soft-tissue imbalance in real time. Using recently published literature measuring patient outcomes against sensor-derived data and existing biomechanical studies describing normal physiologic tibiofemoral loading in the native knee,10 there is now an objective means by which the operator can assess soft tissue balance in TKA.
Fig. 1.
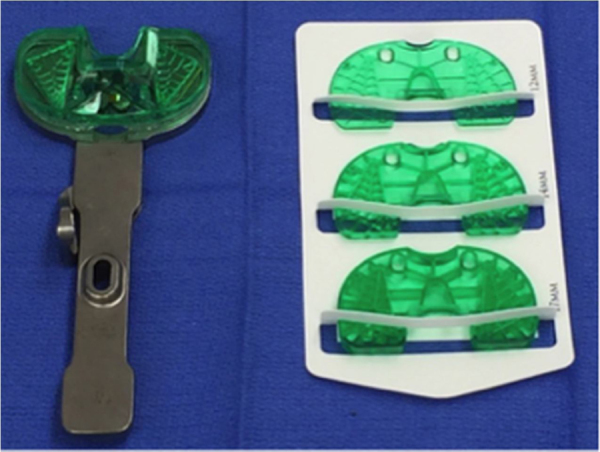
VERASENSE, Orthosensor, Dania, FL, USA. Four different thickness are available (10 mm, 12 mm, 14 mm, 17 mm) for TKA intraoperative load sensing testing.
The purpose of this technical note is to review the current literature on the use of intraoperative digital sensor technology and to propose a surgical technique, which might help surgeons in choosing the ideal level of polyethylene constraint in their primary TKAs.
1.1. Literature review
The use of a radiofrequency-based electronic load sensor for soft tissue balancing in primary TKA was first proposed by Gustke et al.11 in a multicenter study in 2014. The authors reported on 176 knees that received a PCL retaining or sacrificing Triathlon Knee System (Stryker, Mahwah, NJ) using the VERSASENSE sensor. Once the appropriate tibial size insert was determined with the trial components in place, the corresponding VERASENSE sensor was activated and implanted. Data was recorded with the knee in full-extension, mid-flexion and at 90° of flexion. All patients were evaluated 6 months postoperatively using two patient-reported outcomes measurement systems (PROMs): the American Knee Society Score (KSS)12 and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC).13 These authors demonstrated that balanced knees (87%/176), with an intraoperative mediolateral intercompartmental loading difference of ≤15 lbs measured with the sensor through ROM, showed greater improvements in KSS and WOMAC scores than in unbalanced knees (13%/176). It is important to note that this study had several limitations, including the lack of a control group, a significantly smaller “unbalanced” group with respect to the “balanced” group, eight different operating surgeons resulting in a lack of a homogeneous surgical technique, and the use of different levels of TKA constraint (PCL retaining versus PCL substituting).
Schnaser et al.14 reviewed the influence of the position of the patella on the sensor detected load distribution at the tibio-femoral compartment during gap assessment. The authors evaluated 57 patients (60 knees) who underwent primary posterior-stabilized (PS) TKA utilizing the Triathlon Knee System (Stryker, Mahwah, NJ). Intraoperatively, once the knee was considered well balanced with the trial components in, the sensor device was inserted and medial and lateral compartments loads were obtained during gravity assisted full extension, 45° of flexion, 90° of flexion, and gravity-assisted full flexion. Measurements were recorded with the patella relocated in the femoral groove with the medial retinaculum both open and closed, with the patella lateralized but not everted, and with the patella lateralized and everted. The authors of this study demonstrated that the dislocation of the patella, with and without eversion, alters the load distribution during sensor testing on the medial and lateral compartment of the knee. Mean loads registered in the medial compartment with the patella relocated in the femoral groove were 30 lbs in full extension, 17 lbs at 45°, and 15 lbs at 90°; the mean loads registered in the lateral compartment were 26 lbs in full extension, 21 lbs at 45°, and 16 lb at 90°. Of note, the medial and lateral compartments were found to exhibit a significantly different load pattern during ROM. A progressive shift of load from the medial to the lateral compartment was detected with progressive knee flexion regardless of the patellar position. This last finding contrasts with the physiologic greater lateral laxity and postero-lateral rollback of the knee during flexion demonstrated by many radiological and fluoroscopic studies.15, 16
Meere et al.17 conducted a multi-surgeon blinded cadaveric study to investigate differences in gapping of the medial and lateral compartments and to evaluate the medial and lateral compartment compressive forces through ROM using the same load-sensing technology while performing a PCL retaining TKA. This study showed significantly reduced medial, lateral, and total mediolateral gapping in sensor assisted TKA. Additionally, TKA performed without load-sensing technology resulted in greater lateral compartment compressive force in comparison to those performed with the sensor, which had greater medial compartment forces as the knee was flexed. Having slightly greater compressive forces in the medial compartment with greater lateral laxity during active ROM might reproduce the medial pivot and lateral femoral rollback characteristic of the normal knee.18 The “in vitro” results by Meere et al. reflect the “clinical” results reported by Liebs et al.19 in a study demonstrating that patients with a larger lateral extension gap in their replaced knee had significantly better WOMAC pain scores than patients with an increased medial gap. In another study, Meere et al.20 demonstrated that using wireless load-sensing tibial components allows surgeons to reproduce the normal21 medial-to-lateral force ratio when using PCL-retaining TKA implants via progressive, stepwise, surgical soft-tissue and bone corrections.
Recently, Meneghini et al.22 reviewed 189 consecutive TKAs (cruciate-retaining, posterior-stabilized, and high congruent) at a minimum of 4 months from surgery. All knees were intra-operatively balanced using tibial insert sensor trials (VERASENSE, Orthosensor, Dania, FL). The authors recorded intraoperative compartment forces and related those to the PROMs obtained at 4 months from surgery. This paper confirmed that mean medial compartment forces (70.7 lbs) were higher than mean lateral compartment forces (44.0 lbs) during trial sensor testing at 0°, 45° and 90° of flexion. Surprisingly, the authors demonstrated that PROM outcomes were unrelated to mediolateral balance of the knee as determined by medial and lateral compartment pressures.
1.2. Surgical technique for primary TKA using load sensors
At the author’s institution, we routinely use the Persona (Zimmer Biomet, Warsaw, USA) total knee system to treat advanced knee osteoarthritis. The proposed surgical technique, further described below, was implemented by the author beginning in 2015. It is targeted for patients with a mild, moderate, or severe varus alignment often requiring some amount of medial release. This TKA system has an extreme modularity allowing for an intraoperative shift between different levels of constraint: two femoral designs (PS – posterior stabilized and CR – cruciate retaining), one anatomic tibial baseplate, and four different polyethylene inserts (PS, CR, UC-Ultra Congruent and MC-Medially Congruent) are routinely available. The current authors advocate that the contemporary use of a modern and extremely modular total knee system, combined with a wireless load sensing device, provides a customized knee implant allowing for reduction in the level of constraint.
At the author’s institution, prior to TKA, all knees undergo standard antero-posterior, lateral, Merchant et al.23, and long leg alignment radiographic evaluation in order to detect the degree of deformity, bone loss, and the overall alignment. Intraoperatively, a median parapatellar approach is routinely used. Standard bone cuts are made using traditional instrumentation for the Persona knee system, including an extramedullary tibial jig for the tibial cut and intramedullary instrumentation for the distal femoral cut. The chosen surgical technique is a combination of the “balanced gaps technique”24 and the “measured resection technique.”25 First, a rectangular extension gap is created and checked using standard blocks. Then, the femoral sizing guide is oriented on the axial plane according to the surgical trans-epicondylar (sTEA) axis. Particular attention is paid to avoid excessive external rotation of the femoral component to prevent opening of the medial compartment in flexion. As such, 3° of external rotation of the femoral component is routinely, but not always, used in the varus knee. All implants are tentatively aligned in the coronal plane reproducing patient’s mechanical axis. Once the bony cuts are completed, the posterior cruciate ligament is resected and all osteophytes are removed. The extension gap is assessed one more time using a 10 mm bone block. The flexion gap is then re-evaluated using laminar spreaders. A soft tissue release is performed at this point, if needed, to reproduce a symmetrical rectangular space both in flexion and extension.
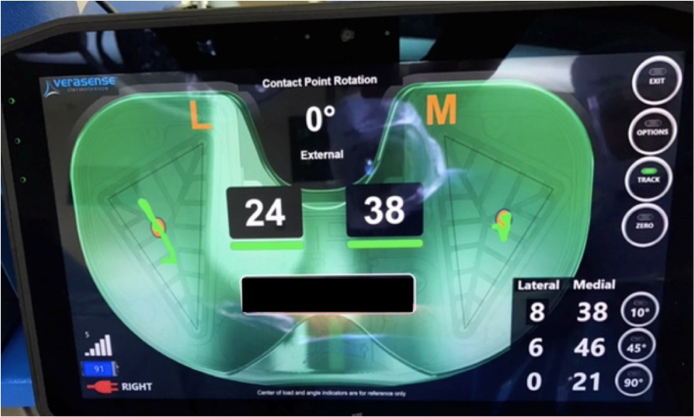
The trial for the Persona CR femoral component is fitted in the distal femur according to the bone cuts. Attention is then turned to the sizing and placement of the tibial component. The rotational alignment of the Persona anatomical tibial component is set according to the medial third of the tibial tubercle.26 When it is felt that both gaps are balanced using standard instrumentation and with the trial components in place, the CR VERASENSE tibial sensor is inserted (Fig. 2). Following the recommendations of multiple studies,14, 27 we routinely insert and then remove the trial so that it can be re-zeroed due to the small plastic deformation of the trial that occurs with initial implantation which may alter the load measurements. Care is taken not place excessive axial load on the knee in the fully extended position as this can over-load the sensors placing them out of calibration. The associated monitor displays warning if such event does occur, and the sensor is required to removed and re-zeroed before trialing again. With the patella relocated in the trochlear groove, load measurements are documented at 10° (Fig. 3), 45°, and 90° of flexion following a uniform data collection protocol. At this point, the distribution of compartment forces during intraoperative ROM drive the selection of the liner and, accordingly, the level of constraint. The ultimate goal is to intraoperatively replicate the physiological medial pivoting biomechanics of the natural knee28, 29 using the minimal level of intra-articular constraint.
Fig. 2.
Left total knee arthroplasty. Intraoperative use of the trial sensing insert.
Fig. 3.
Left knee. Loading forces at tibiofemoral interface. In this example, the knee in well balanced with 39 lbs in the medial compartment and 29 lbs in the lateral compartment: the intercompartimental load difference is 10 lbs.
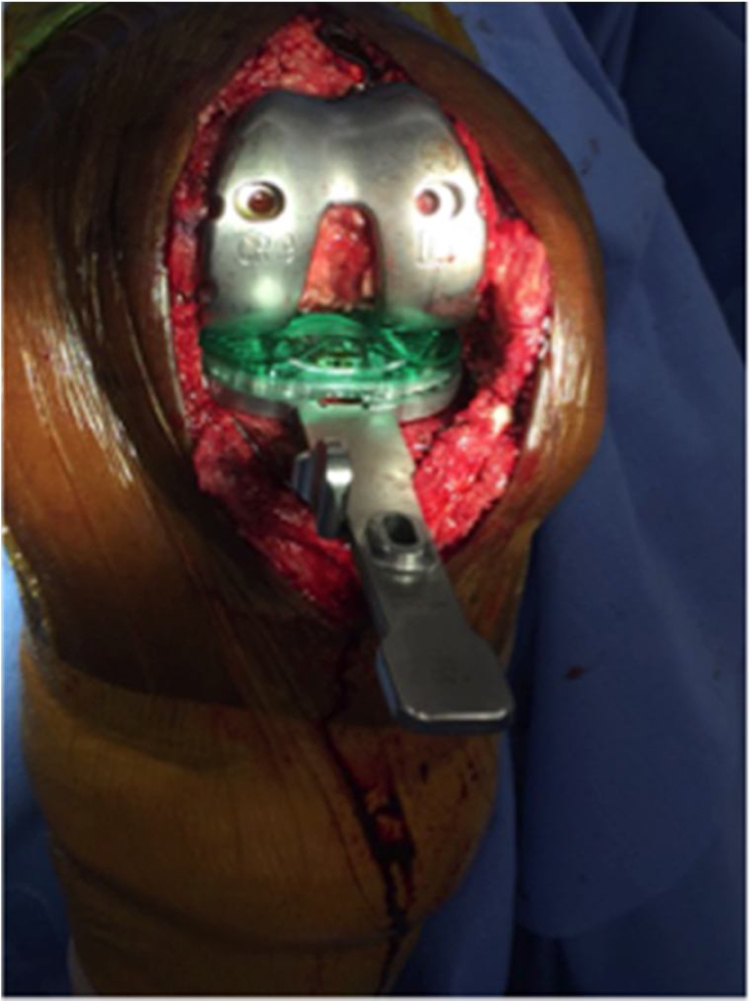
Following this objective, the authors aim to obtain a medial compartment slightly tighter than the lateral compartment, both in extension as well as flexion. Once the instrumented tibial trial is inserted, the authors check the magnitude of the contact forces, aiming to not exceed more than 70 lbs in any compartment. We consider stable knees as those with a pressure of 50 lbs ± 20 lbs on the medial compartment, 35 lbs ± 20 lbs on the lateral compartment, and mediolateral intercompartmental difference within 15 lbs ± 5 lbs. These values are comparable with those reported by Gustke et al.11 However, our technique suggests a different setting for the sagittal stability. Gustke et al.11 defines a sagittally stable implant as one having a contact point in the mid-third of the tibial plateau with minimal excursion and a stable end point during posterior drawer test. Our current surgical technique aims to restore the medial pivoting biomechanics of the knee using a Persona CR or MC tibial insert, obtaining a stable end point on the medial compartment and a physiologic postero-lateral roll back of the lateral femoral condyle. The contact point between tibial and femoral component can be analyzed during the passive ROM test showing a greater rolling from anterior to posterior on the lateral compartment (Fig. 4). Acknowledging that Meneghini et al.22 demonstrated that major differences in intercompartmental forces did not affect early clinical outcomes, a mediolateral intercompartmental difference of 15 lbs ± 5 lbs in favor of the medial compartment is the ideal value that drives our technique and provides the physiologic postero-lateral roll back of the lateral femoral condyle. When medial and lateral intercompartment loads are within the desired ranges, the current authors do not perform additional changes in neither bone resections nor soft tissue balancing. At this point, a final MC fixed bearing polyethylene insert is implanted.
Fig. 4.
Right knee. Verasense graphic user interface identifying a stable end point on the medial compartment and a postero lateral roll back during intraoperative passive ROM is noted.
When mean intercompartmental force differences are more than 15 + 5 lbs but less than 40 lbs, the authors decide to perform a soft tissue release addressing the tighter compartment and continue on to selecting a final MC fixed bearing polyethylene insert. The amount of soft tissue release, and what structures are to be released, depend upon wireless load assessment during flexion-extension evaluation. A medial collateral ligament (MCL) release is performed when the sensor demonstrates an excessive tightness on the medial compartment during passive ROM. If the knee is tighter in extension, a needle or #11 blade is used to release the posterior fibers of the MCL and eventually the pes anserine tibial insertion. If tightness is worse in flexion, the anterior fibers of the MCL and eventually the semi-membranosus insertion are released in conjunction with a release of the postero-medial capsule.
When values reported by the wireless tibial trial indicate a lateral tightness both in extension as well in flexion, a posterior lateral corner release is performed. This may additionally require a release of the arcuate ligament and the postero-lateral capsule. The iliotibial band is also released when intercompartmental force difference is still significant in extension. During this time, particular attention is paid to the presence of posterior condyle osteophytes, which can cause a mechanical obstacle to achievement of full extension.
When mean intercompartment force difference is more than 40 lbs, the authors prefer to increase the level of constraint in the polyethylene insert, shifting to use a PS design in attempt to address any residual instability. The tibial insert thickness is routinely increased if the total forces on the medial and lateral tibial condyles are too low. Schirm et al. demonstrated in a recent study that a 2 mm increase in tibial insert thickness has been shown to increase compressive forces by 54–131% with effects particularly noted PCL-retaining and mobile bearing prosthesis.30 Walker et al. showed that 2 mm in thickness difference results in a change in force sufficient to correct most imbalances.31 The current authors believe that instability requiring insertion of a polyethelene with thickness greater than 14 mm in order to achieve medial pivoting biomechanics is not indicated. Using a PS insert is recommended in such scenario.
A careful clinical examination is performed again at the end of the procedure. The correction of the preoperative axial deformity and the achievement of passive ROM from full extension to 130° of flexion is evaluated. Varus-valgus stress testing is performed at 10 and 45 ° with the capsule closed and patella relocated in the femoral groove. Finally, anterior and posterior drawer tests are evaluated at 90 ° of flexion with the hip in neutral rotation to test the AP stability of the final construct.
1.3. Conclusion
Proper balancing of soft tissues of the knee has become one of the primary goals while performing TKA. However, being an operator dependent entity with no accepted standard criteria with which it can be objectively measured, soft tissue balance remains more of an art than a science. Wireless load–sensing tibial components serve as an intraoperative tool that provides a surgeon with objective data by which they can optimize soft tissue balance. In the current literature, there seems to be no consensus as to the definition of a “truly balanced knee” and whether such knee results in improved functional outcomes. Few studies relate physiologic native knee biomechanics to the use of medial pivot or medially constrained TKA.32 This proposed surgical technique using wireless load–sensor tibial component facilitated the authors ability to reproduce physiologic knee biomechanics by providing objective and reproducible data. There are a number of limitations of this technique. First, the ideal target value for balancing the knee has been arbitrarily proposed by the authors, since the current literature is equivocal. A second limitation of our study is that the authors used a CR femoral component where typically an MC tibial insert is preferably used in combination with posterior cruciate ligament resection. Previous studies have shown that PCL tends to stretch out following primary CR-TKA leading to postoperative flexion instability.33 Lastly, during the technique outlined above the knee was not load-bearing during load-sensing testing. However, it has been shown that passive intraoperative force readings correlate with abnormal postoperative kinematics.34
Surgeons willing to follow this proposed surgical technique must keep in consideration to add about 500$ (estimated cost of the trial sensors in the USA) to the final cost of the TKA procedure.
The current authors consider that the use of a more objective measurement system can improve surgeon understanding of knee kinematics following primary total knee arthroplasty. Further study is warranted and should include clinical data following this technique to evaluate functional outcome.
Conflict of interest
The authors have none to declare.
References
- 1.Sharkey P.F., Hozack W.J., Rothman R.H. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002:7. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Dennis D.A., Komistek R.D., Kim R.H., Sharma A. Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res. 2010;468(1):102–107. doi: 10.1007/s11999-009-1112-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Griffin F.M., Insall J.N., Scuderi G.R. Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty. 2000;15(December (8)):970–973. doi: 10.1054/arth.2000.6503. [DOI] [PubMed] [Google Scholar]
- 4.Asano H., Hoshino A., Wilton T.J. Soft-tissue tension total knee arthroplasty. J Arthroplasty. 2004;19(August (5)) doi: 10.1016/j.arth.2004.01.003. 558–556. [DOI] [PubMed] [Google Scholar]
- 5.Indelli P.F., Pipino G., Graceffa A., Marcucci M. Posterior-stabilized (PS) total knee arthroplasty: a matched pair analysis of a classic and its evolutional design. Arthroplasty Today. 2016;2(4):193–198. doi: 10.1016/j.artd.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nunley R.M., Nam D., Berend K.R. New total knee arthroplasty designs: do young patients notice? Clin Orthop Relat Res. 2015;473(1):101–108. doi: 10.1007/s11999-014-3713-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Callahan C.M., Drake B.G., Heck D.A., Dittus R.S. Patient outcomes following tricompartmental total knee replacement. A meta-analysis. JAMA. 1994;271(17):1349–1357. [PubMed] [Google Scholar]
- 8.Vince K. Mid-flexion instability after total knee arthroplasty: woolly thinking or a real concern? Bone Joint J. 2016;98-B(1 Suppl. A):84–88. doi: 10.1302/0301-620X.98B1.36445. [DOI] [PubMed] [Google Scholar]
- 9.Atwood S.A., Currier J.H., Mayor M.B. Clinical wear measurement on low contact stress rotating platform knee bearings. J Arthroplasty. 2008;23(3):431–440. doi: 10.1016/j.arth.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 10.Morrison J.B. The mechanics of the knee joint in relation to normal walking. J Biomech. 1970;3(1):51–61. doi: 10.1016/0021-9290(70)90050-3. [DOI] [PubMed] [Google Scholar]
- 11.Gustke K.A., Golladay G.J., Roche M.W., Elson L.C., Anderson C.R. A new method for defining balance: promising short-term clinical outcomes of sensor-guided TKA. J Arthroplasty. 2014;29(5):955–960. doi: 10.1016/j.arth.2013.10.020. [DOI] [PubMed] [Google Scholar]
- 12.Insall J.N., Dorr L.D., Scott R.D., Scott W.N. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248(November):13–14. [PubMed] [Google Scholar]
- 13.Bellamy N., Buchanan W.W., Goldmith C.H. Validation study of WOMAC: a health status instrument ofr measuring clinically-imporant patient-relevant outcomes following total hip or knee arthroplasty in osteoarthritis. J Orthop Rhematol. 1988;1:95–108. [PubMed] [Google Scholar]
- 14.Schnaser E., Lee Y.Y., Boettner F., Gonzalez Della Valle A. The position of the patella and extensor mechanism affects intraoperative compartmental loads during total knee arthroplasty: a pilot study using intraoperative sensing to guide soft tissue balance. J Arthroplasty. 2015;30(August (8)):1348–1353. doi: 10.1016/j.arth.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 15.Okazaki K., Miura H., Matsuda S. Asymmetry of mediolateral laxity of the normal knee. J Orthop Sci. 2006;11(May (3)):264–266. doi: 10.1007/s00776-006-1009-x. [DOI] [PubMed] [Google Scholar]
- 16.Indelli P.F. Is normal knee biomechanics reproduced by modern TKA designs? The role of fluoroscopy. Osteol Rheumatol Open J. 2016;1(1):6–9. [Google Scholar]
- 17.Meere P., LaMont J., Baez J. Surgeon assessment of gapping versus kinetic load using intraoperative sensors during TKA. Reconstr Rev. 2017;5(3):29–34. [Google Scholar]
- 18.Iwaki H., Pinskerova V., Freeman M.A. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br. 2000;82(8):1189–1195. doi: 10.1302/0301-620x.82b8.10717. [DOI] [PubMed] [Google Scholar]
- 19.Liebs T.R., Kloos S.A., Herzberg W., Rüther W., Hassenpflug J. The significance of an asymmetric extension gap on routine radiographs after total knee replacement: a new sign and its clinical significance. Bone Joint J. 2013;95-B(4):472–477. doi: 10.1302/0301-620X.95B4.31080. [DOI] [PubMed] [Google Scholar]
- 20.Meere P.A., Schneider S.M., Walker P.S. Accuracy of balancing at total knee surgery using an instrumented tibial trial. J Arthroplasty. 2016;31(September (9)):1938–1942. doi: 10.1016/j.arth.2016.02.050. [DOI] [PubMed] [Google Scholar]
- 21.Heesterbeek P.J., Verdonschot N., Wymenga A.B. In vivo knee laxity in flexion and extension: a radiographic study in 30 older healthy subjects. Knee. 2008;15(1):45–49. doi: 10.1016/j.knee.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 22.Meneghini R.M., Ziemba-Davis M.M., Lovro L.R., Ireland P.H., Damer B.M. Can intraoperative sensors determine the target ligament balance? Early outcomes in total knee arthroplasty. J Arthroplasty. 2016;31(10):2181–2187. doi: 10.1016/j.arth.2016.03.046. [DOI] [PubMed] [Google Scholar]
- 23.Merchant A.C., Mercer R.L., Jacobsen R.H., Cool C.R. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391–1396. [PubMed] [Google Scholar]
- 24.Insall J.N., Scott W.N. 4th ed. Church Livingstone/Elsevier; Philadelphia: 2006. Insall & Scott surgery of the knee. [Google Scholar]
- 25.Lotke P.A., Lonner J.H. 3rd ed. Wolters Kluwer Health/Lippincott Williams & Wilkins; Philadelphia, PA: 2009. Knee arthroplasty. [Google Scholar]
- 26.Indelli P.F., Graceffa A., Payne B., Baldini A., Pipino G., Marcucci M. Relationship between tibial baseplate design and rotational alignment landmarks in primary total knee arthroplasty. Arthritis. 2015 doi: 10.1155/2015/189294. Open Access Article ID 189294. Published online 2015 Sep 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matsumoto T., Muratsu H., Tsumura N., Mizuno K., MD, Kurosaka M., Kuroda R. Soft tissue balance measurement in posterior-stabilized total knee arthroplasty with a navigation system. J Arthroplasty. 2009;24(3):358–364. doi: 10.1016/j.arth.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 28.Dennis D.A., Mahfouz M.R., Komistek R.D. In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech. 2005;38(2):241. doi: 10.1016/j.jbiomech.2004.02.042. [DOI] [PubMed] [Google Scholar]
- 29.Komistek R.D., Dennis D.A., Mahfouz M. In vivo fluoroscopic analysis of the normal human knee. Clin Orthop Relat Res. 2003;410:69. doi: 10.1097/01.blo.0000062384.79828.3b. [DOI] [PubMed] [Google Scholar]
- 30.Schrim A.C., Jeffcote B.O., Nicholls R.I. Sensitivity of knee soft-tissues to surgical technique in total knee arthroplasty. Knee. 2011;18:180. doi: 10.1016/j.knee.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 31.Walker P.S., Meere P.A., Bell C.P. Effect of surgical variables in balancing of total knee replacement using an instrumented tibial trial. Knee. 2014;21(1):156. doi: 10.1016/j.knee.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 32.Macheras G.A., Galanakos S.P., Lepetsos P., Anastasopoulos P.P., Papadakis S.A. A long term clinical outcome of the medial pivot knee arthroplasy system. Knee. 2017;24(March (2)):447–453. doi: 10.1016/j.knee.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 33.Victor J., Banks S., Bellemans J. Kinematics of posterior cruciate ligament retaining and -substituting total knee arthroplasty. A prospective randomized outcome study. J Bone Joint Surg Br. 2005;87(5):646–655. doi: 10.1302/0301-620X.87B5.15602. [DOI] [PubMed] [Google Scholar]
- 34.Wasielewski R.C., Galat D.D., Komistek R.D. Correlation of compartment pressure data from an intraoperative sensing device with postoperative fluoroscopic kinematics results in TKA patients. J Biomech. 2005;38:333. doi: 10.1016/j.jbiomech.2004.02.040. [DOI] [PubMed] [Google Scholar]