Abstract
Purpose
Medial close wedge Coventry type osteotomy is commonly performed procedure for adoloscent Genu valgum. However this osteotomy has some inherent problems, a wedge resection causes shortening of affected site. An additional plate for stabilization causes increase in soft tissue dissection and surgical time. A cheveron osteotomy is an alternative procedure, not requiring any internal fixation due to its inherent stability. We started this study with aim to analyze the results of Cheveron osteotomy, to see if the osteotomy was stable enough without implants, time required for healing of osteotomy, post-operative range of motion, limb length discrepancy and to evaluate any other complication.
Methods
This study was conducted to evaluate the efficacy of cheveron osteotomy in cases with genu valgum in our department from 2005 to 2012. 75 children with 115 knee deformities were included in the study. Patients were followed upto minimum 3 years post surgery. Clinical and radiological assessment was done on all subsequent visits.
Results
Preoperative mean valgus angle was 21° (12–30°) and mean inter malleolar distance was 12.3 cm(11–21 cm). The mean post-operative angle was 6.5° and mean intermalleolar distance was 5.6 cm. The difference was statistically significant. The mean tourniquet time was 26 min and mean surgical time including plaster cast application was 38 min. Mean blood loss was 75 ml. The mean time to union was 10.3 weeks.
Conclusion
Supracondylar cheveron osteotomy is simple, stable, low cost osteotomy for surgical correction of genu valgum. The osteotomy provides excellent clinical, radiological and functional results in short surgical time and has an added advantage of omitting the need of second surgery.
Keywords: Genu valgum, Osteotomy, Rickets, Cheveron
1. Introduction
Knock-knees or genu valgum is one of the most common lower limb deformities to present in an orthopedic outpatient clinic. These deformities, in general, are benign and most children achieve the adult valgus alignment of 5–7° by age of 6 years. However in few children the valgus may persist and surgical intervention may be required in cases of frequent falls due to knock knees, anterior knee pain due to malalignment, patellofemoral problems owing to increased Q-angle, gross asymmetry on both sides or concern of cosmesis.1
Treatment of genu valgum aims to correct the mechanical axis of lower limb. This requires an osteotomy around the center of rotation of angulation, which mostly lies in distal femur. Numerous techniques have been described for correction of such deformities. It includes lateral opening wedge osteotomy, medial closing wedge osteotomy, dome osteotomy and Illizarov’s distraction method. Each procedure has its advantages and disadvantages. Medial close wedge Coventry type osteotomy is commonly performed procedure.2, 3 However this osteotomy has some inherent problems, a wedge resection causes shortening of affected site. The contact area of bone after resection is small which requires an additional plate for stabilization causing increase in soft tissue dissection and surgical time. Opening wedge osteotomy on the other hand leads to lengthening apart from problems related to graft site morbidity and incorporation of bone grafts.4 Ring distraction has been used successfully however cost and problems related to external fixation including pin site care, pin site infections and bulky hardware visible outside makes it a less attractive alternative.5 Additional procedure may be required for hardware removal other than inherent problems of hardware itself. Dome osteotomy has a disadvantage to violate anterior quadriceps muscle and secondly it forms a dome near anterior supracondylar area near to trochlea and may cause trochleo-patellar problems.6 Guided growth is not feasible with minimal growth left in patients after 12 years. Agelietti et al. have described a simple and stable supracondylar ‘V’ osteotomy that does not require any fixation other than K-wires.7 However their method has not been thoroughly researched in literature and mostly forgotten. Only a few reports about the procedure with small patients sample are presented.8, 9 We started this study with aim to analyze the results of the osteotomy, to see if the osteotomy was stable enough without implants, time required for healing of osteotomy, post-operative range of motion, limb length discrepancy and to evaluate any other complication.
We here present our experience of supracondylar cheveron osteotomy in 115 knees In 75 children treated at our institute in last 8 years with a minimum follow-up of 3 years.
2. Materials and methods
This study was conducted to evaluate the efficacy of cheveron osteotomy in cases with genu valgum in our department of Orthopedics from 2005 to 2012. The inclusion criterion for the surgery was a symptomatic genu valgum patient with intermalleolar distance of more than 10 cm, tibio-femoral angle more than 12° after the age of 12 years.6 Children less than 12 years were preferred for guided growth owing to sufficient growth remaining. Concern for cosmesis, knee pain due to mal-alignment, patella-femoral instability, difficulty in running or climbing stairs and frequent falls were considered symptoms due to genu valgum for purpose of our study. Cases of traumatic and dysplasia were excluded from the study.
A thorough history regarding onset and progression of deformity was sought. Clinical tibiofemoral angles and inter malleolar distances were noted in all patients initially and after 3 months interval as described below. On standing position with patella facing outwards, anterior superior iliac spine (ASIS), center of patella and center of ankle (point between midpoint of medial and lateral malleoli) were marked. Anterior superior iliac spine and center of patella were joined and center of patella and center of ankle were joined by 2 lines. By using goniometer, tibiofemoral angle was measured using the above lines.10 Intermalleolar distance were also noted in standing patient. These clinical measurements were measured on all subsequent visits by same personnel and recorded by different person to omit any bias.
Laboratory investigations included all routine investigations including serum calcium, phosphorus and alkaline phosphatase (ALP). An initial scanogram was done for all patients. The underlying cause for genu valgum was sought and medical treatment when necessary was carried out before surgical procedure.
3. Surgical approach
All surgeries were carried out under general or regional anesthesia as per discretion of anesthesiologist. Surgery was done in supine position. Tourniquet was used in all cases and was kept 100 mm of mercury over systolic blood pressure. A 3–4 cm longitudinal incision was given proximally from adductor tubercle. Belly of vastus medialis was elevated from the inter-muscular septum. A leash of physeal vessals was always seen traversing transversely in the surgical field. The osteotomy was carried out 3–5 mm proximal to this site. A small incision is given in the periosteum and it is elevated. A ‘v’ is then marked with apex at adductor tubercle and two limbs at 80–90° angle. The posterior limb was kept short to lessen the pull of gastrocnemius muscle. The osteotomy was completed with saw or osteotome and lateral cortex was left intact. The limb was then corrected applying the varus stress and plastically deforming the lateral cortex. The apex, at times, was needed to be nibbled. (Fig. 1a–e) The correction was checked using the radio-opaque lead of electro-cautery with one end placed at center of hip and other end placed at center of ankle and this should pass through center of knee. It was checked under C-arm. The stability of osteotomy was assessed and if in doubt it was fixed using 2 K-wires. A cylindrical cast was given after closure under a drain.
Fig. 1.
(a) Calinical photograph showing the incision. (b) clinical photograph after elevating vastus medialis, there is a leash of vessels visible. Site of osteotomy is just proximal to this site. (c) A ‘V’ osteotomy marked by drill holes. (d) Osteotomy made in shape of ‘V’. note angle is less than 90° and anterior limb is kept bigger. (e) After correction of deformity. Apex is nibbled just a little and the proximal part gets impacted medially.
Suture removal and change of cast was done at 2 weeks and patient was allowed walker assisted partial weight bearing mobilization. The second cast was removed at 3 weeks and range of motion exercises were begun. Full weight bearing was allowed after complete union of bone. A scanogram was taken at bone union to assess for limb alignment.
The patients were thereafter followed at 6 months interval and assessed for any complications. Limb length measurements were carried out on all subsequent visits.
All quantitative variables were expressed in mean ± standard deviation. Pre-operative range of motion and deformities were compared to post-operative value using student’s t-test. A value of <0.05 was considered significant. All data was analyzed using spss software version 21
4. Results
75 children with ages 12–18 (mean-14.6 years) were treated surgically at our institute from 2005 to 2012. 28 patients were male and 47 females. 40 cases had bilateral correction and 35 had unilateral correction. The mean follow up was 3.1 years. Most common etiology for genu valgum was post rachitic.
Preoperative mean valgus angle was 21° (12–30°) and mean inter malleolar distance was 12.3 cm(11–21 cm). The mean post-operative angle was 6.5° and mean intermalleolar distance was 5.6 cm. The difference was statistically significant (<0.05). The mean range of motion preoperatively was 0–132° and mean range post operatively was 0–135° at 6 months and it was not statistically significant. (p = 0.92). Table 1. The mean tourniquet time was 26 min and mean surgical time including plaster cast application was 38 min. Mean blood loss was 75 ml. (Fig. 2, Fig. 3) The mean time to union was 10.3 weeks.
Table 1.
pre and postoperative variables in patients undergoing cheveron osteotomy.
| Pre-operative | Post operative at 6 months | P- value (paired t-test) |
|
|---|---|---|---|
| Genu valgum | 21 (12–30°) | 6.5 (5–9°) | 0.002 |
| Intermalleolar angle | 12.3 (11–21 cm) | 5.6 (3–7 cm) | 0.000 |
| Range of motion | 0−132 | 0−135 | 0.92 |
| Lysholm score | 78 | 92 | 0.021 |
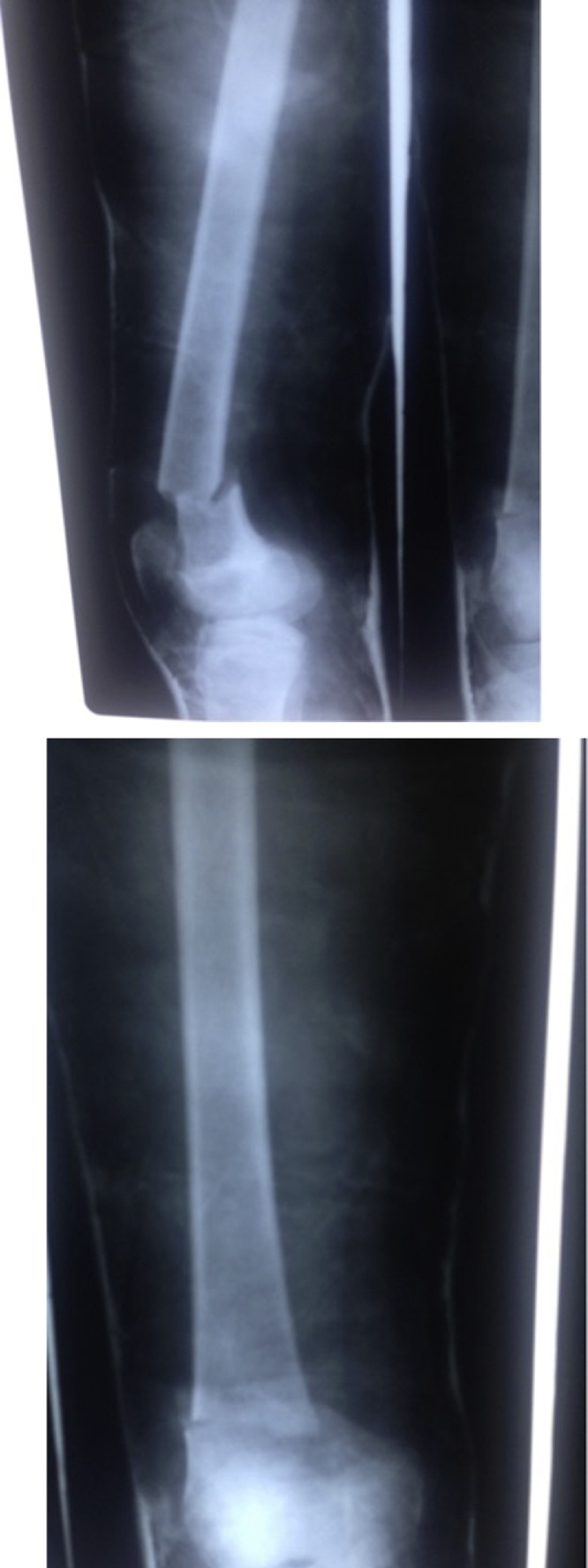
Fig. 2.
(a) Scanogram showing 25.1° of genu valgum on left side. (b) and (c) AP and Lateral Xrays after 3 weeks of cheveron osteotomy.
Fig. 3.
(a) Scanogram showing right sided genuvalgum in 14 year old child. (b) immediate post-operative photograph. No internal fixation device is required. (c) Scanogram after 18 months showing no limb length discrepancy with complete union.
In order to find out if age had any effect on the prognosis after osteotomy, we divided our results in 3 groups depending on the age. The results were analyzed using Analysis of Variance (ANOVA) test. The results are detailed in Table 2. The union time was found to increase with age Another important finding was that none of the cases had limb length discrepancy in 12–14 years, one in 14–16 years and 2 in 16–18 years. We believe this is due to the larger remodeling and growth potential remaining in a younger child which may compensate for mild errors in osteotomy. Other than this, there were no significant difference among each group in terms of studied variables. None of the groups showed any recurrence of deformity after osteotomy in followed up period probably because our patients were mostly rachitic and we corrected all biochemical parameters before planning the osteotomy. We believe that rachitic deformities would not recur if the deficiency is met.
Table 2.
Age wise distribution of results.
| 12–14 years | 14–16 years | 16–18 years | P value | |
|---|---|---|---|---|
| Number of patients | 27 | 29 | 19 | |
| Unilateral/bilateral | 6/21 | 17/12 | 12/7 | |
| Male/female | 10/17 | 7/22 | 11/8 | |
| Pre-correction valgus | 24 (16–30°) | 20.1 (12–28°) | 22.1(18–26°) | 0.65 |
| Pre correction intermalleolar angle | 14.4 (12–21 cm) | 12.1 (11–20 cm) | 12.1 (11–18 cm) | 0.74 |
| Pre surgery lyslohm score | 78 | 76 | 80 | 0.59 |
| Post-correction valgus | 6.6 (5–8°) | 6.1 (5–9°) | 6.9 (6–9°) | 0.34 |
| Post correction intermalleolar angle | 5.1 (3–7 cm) | 5.6 (3–7 cm) | 5.8 (3–6 cm) | 0.28 |
| Post surgery lyslohm score | 90 | 93 | 92 | 0.59 |
| Union time | 9.8 weeks | 10.5 weeks | 12.1 weeks | 0.04 |
| Infection | 2 | 1 | 2 | 0.23 |
| Loss of correction | 1 | 0 | 1 | 0.12 |
| Limb length discrepency | 0 | 1 | 2 | 0.00 |
The functional scoring was done using Lysholm knee score. The pre-operative score was 78 and post-operative score was 92 at 6 months and difference was statistically significant (p < 0.05) (Fig. 4).
Fig. 4.
clinical photograph at 6 months from surgery showing complete range of motion.
There were 5 cases of superficial infection and all cases were in patients in whom K-wires were used. This was in earlier half of our study and in later half we did not use any K-wires. In order to find out if K-wires provided any extra stability, we compared the results of these two groups using independent t-test (Table 3). We found no significant difference in two groups in terms of pre-operative variables as well as post-operative results. Hence authors recommend that plaster of paris cast is sufficient to hold the osteotomy site until union without need of any other fixation if the osteotomy angle was kept less than 90°. 3 cases had limb length discrepancy in our series, which was actually a technical error due to posterior tilt of distal fragment not recognized during surgery (Fig. 5). Following this a true AP and Lateral view was taken in routinely after plaster cast application. 2 cases had loss of reduction in plaster of paris cast and it was due to more obtuse angle formed by limbs of osteotomy (Fig. 6). Whenever the limbs made an angle of 90 or less, the osteotomy was very stable and no loss of reduction was seen. There was one case of non union and it was because the fact that osteotomy was made little proximal in diaphyseal area.
Table 3.
comparison of results of patients with and without K-wires undergone Cheveron Osteotomy.
| With K-wire | Without K-wire | P value | |
|---|---|---|---|
| Number of patients | 32 | 43 | |
| Unilateral/bilateral | 10/22 | 25/18 | |
| Male/female | 13/19 | 15/28 | |
| Pre-correction valgus | 24.1 (14–30°) | 23.5 (12–28°) | 0.38 |
| Pre correction intermalleolar angle | 12.1 (11–20 cm) | 13.2 (12–21 cm) | 0.65 |
| Pre surgery lyslohm score | 76 | 80 | 0.21 |
| Post-correction valgus | 6.1 (5–9°) | 6.0 (5–9°) | 0.19 |
| Post correction intermalleolar angle | 5.5 cm 3–7 cm) | 5.6 (3–7 cm) | 0.11 |
| Post surgery lyslohm score | 92 | 94 | 0.64 |
| Union time | 10.3 weeks | 10.2 weeks | 0.12 |
| Infection | 0 | 5 | 0.000 |
| Loss of correction | 1 | 1 | 0.23 |
| Limb length discrepency | 1 | 2 | 0.11 |
Fig. 5.
lateral X-ray showing posterior tilt, which was cause of 1.5 cm shortening in this patient.
Fig. 6.
AP and Lateral X-ray showing loss of reduction. Note the angle of osteotomy is little obtuse.
5. Discussion
Salenius and Vankka in 1975 described normal clinical tibiofemoral angles in 1279 children. They showed mean varus alignment of 15° was attained at neonatal period and decreased to approximately 10° of varus by the age 1 year. At the age of 18–20 months it becomes neutral and maximum valgus of approximately 12° was reached by 3–4 years of age. By age 7 years normal valgus of 8° in women, 7° in men is achieved. Most studies have shown that valgum angle of 12° is never physiological after 7 years [11]. We gave some time for natural correction of deformity in younger patient and any patient with genu valgum over 12° after 12 years with symptoms that can be attributed to genu valgum were taken as indication for surgical correction.10, 11, 12
Various treatment options for genu valgum in adolescents have been described. With open physis, temporary hemiepiphysiodesis has been described. Figure of 8 plates or staples have been used with good success.13, 14, 15 However these procedures have their own problems. Correction is slow and not predictable.16 Risk of problems related to implant including infection, screw breakage etc. are always present.17 Rebound growth after implant removal is always a risk.18, 19 More importantly, we believed that figure of 8 plates may not work well after 12 years. Period of second growth spurt is usually over in this age and only minimal growth is left. Literature shows that rate of correction dramatically decreases with age. Balal et al. showed rate of correction after 10 years is 0.6° a month compared to 1.4°/month in patients in less than 10 years.20 The rate would be further less in patients older than 12 years. These were the reasons why we preferred osteotomy rather than guided growth in over 12 years of age. Further a second surgery is always required for plate removal and it is not un-common in developing country like ours for patients not to follow up in time causing deformity in reverse side due to keeping of plate for prolonged time.
Closing wedge osteotomy on other hand is better suited where little follow up is required after surgery. Correction is instantaneous and there are no risks of rebound growth. However a second surgery for implant removal is required. The osteotomy is inherently not stable enough and has to be stabilized through plate. This increases surgical time, soft tissue dissection and blood loss. Also as a wedge is to be resected from medial side, it invariably results in some shortening.2, 3, 4, 5, 21
Open wedge osteotomy has been described for valgus correction using a fixed implant bone construct like locking plate or blade plates. But these include several risks including include potential hardware irritation, a high rate of plate removal, malunion, or nonunion with the possible need for bone grafting, malcorrection, contracture, intra-articular fracture, breach of medial cortex, and neurovascular injury.4
In order to overcome problems of wedge osteotomy like length discrepancy, a mismatch of fragment ends created by osteotomy and the need for translation of the distal fragment, circular bone cuts – Dome osteotomy was introduced. However it is technically difficult to obtain a perfect dome, the dome is created in anterior supracondylar region resulting in probable trochleo- patellar problems and lastly quadriceps muscle is violated anteriorly.6
Illizarov distraction histogenesis has been tries in correction of genu valgum. However it’s a high risk procedure and includes Major complications like nerve palsy, joint contracture necessitating lengthening of the tendon, premature or delayed osseous consolidation, and permanent stiffness of the joint. Typical minor complications include pin tract infection, oedema, and transient paresthesia (an impermanent tingling sensation in the skin).5
Cheveron osteotomy provides distinct advantages compared to closing wedge osteotomy. No wedge resection is required which omits any influence of osteotomy on limb length discrepancy. Inherent stable osteotomy requires no plate and this decreases blood loss, surgical time and tourniquet time. Average tourniquet time in our series was 26 min. This also decreases the surgical cost as no plate is required, a very important factor in developing country. Further this osteotomy gives a chance to re-align the axis in case of any error during first surgery. The correction can be re-assessed and rectified at 2 weeks during change of cast. Lastly important advantage of the osteotomy is its ‘V’ shape that avoids the supra-patellar area and prevents any patella-femoral problems.7, 8, 9
The author found this method to be highly effective in correcting genu-valgum up till 18 years of age with no implant fixation. This is one of the largest series on Agelietti procedure.
However our study is not a comparative or randomized study, a comparison between different methods would be able to provide statistical difference in different procedures. Secondly it is a single center trial and method can be best established if carried out in different regions by different surgeons. However despite these shortcomings it is an encouraging procedure, especially in developing country, where both cost and regular follow up is a problem.
6. Conclusion
Supracondylar cheveron osteotomy is simple, stable, low cost osteotomy for surgical correction of genu valgum. The osteotomy provides excellent clinical, radiological and functional results in short surgical time and has an added advantage of omitting the need of second surgery.
Conflict of interests
The authors have none to declare.
Funding
None.
References
- 1.Mooney J.F., 3rd. Lower extremity rotational and angular issues in children. Pediatr Clin North Am. 2014;61(6):1175–1183. doi: 10.1016/j.pcl.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Coventry M.B. Osteotomy about the knee for degenerative and rheumatoid arthritis: indications, operative technique, and results. J Bone Joint Surg. 1973;55-A:23. [PubMed] [Google Scholar]
- 3.Coventry M.B., Finerman G.A., Riley L.H., Turner R.H., Upshaw J.E. A new geometric knee for total knee arthroplasty. Clin Orthop. 1972;83:157. doi: 10.1097/00003086-197203000-00030. [DOI] [PubMed] [Google Scholar]
- 4.O’Malley M.P., Pareek A., Reardon P.J., Stuart M.J., Krych A.J. Distal femoral osteotomy: lateral opening wedge technique. Arthroscopy Techniques. 2016;5(4):e725–e730. doi: 10.1016/j.eats.2016.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Velazquez R.J. Complications of use of the Ilizarov technique in the correction of limb deformities in children. J Bone Joint Surg. 1993;75(8):1148–1156. doi: 10.2106/00004623-199308000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Gautam V.K., Kumar R., Mishra P. Focal dome osteotomy for correction of genu valgum. Indian J Orthop. 2002;36:6. [Google Scholar]
- 7.Aglietti P., Stringa G., Buzzi R. Correction of valgus knee deformity with a supracondylar V osteotomy. Clin Orthop. 1987;217:214. [PubMed] [Google Scholar]
- 8.Agarwal Sharat. Modified Aglietti procedure (supracondylar femoral osteotomy) for correction of the post-rachitic valgus deformity of the knee in adolescents –a short case series. J Orthop. 2013;10(December (4)):196–199. doi: 10.1016/j.jor.2013.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta V., Kamra G., Singh D., Pandey K., Arora S.W. Wedgeless ‘V' shaped distal femoral osteotomy with internal fixation for genu valgum in adolescents and young adults. Acta Orthop Belg. 2014;80(June (2)):234–240. [PubMed] [Google Scholar]
- 10.Mathew S.E., Madhuri V. Clinical tibiofemoral angle in south Indian children. Bone Joint Res. 2013;2(August (8)):155–161. doi: 10.1302/2046-3758.28.2000157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salenius P., Vankka E. The development of the tibiofemoral angle in children. J Bone Joint Surg Am. 1975;57(March (2)):259–261. [PubMed] [Google Scholar]
- 12.Vankka E., Salenius P. Spontaneous correction of severe tibiofemoral deformity in growing children. Acta Orthop Scand. 1982;53(August (4)):567–570. doi: 10.3109/17453678208992259. [DOI] [PubMed] [Google Scholar]
- 13.Zuege R.C., Kempken T.G. Blount WP: Epiphyseal stapling for angular deformity at the knee. J Bone Joint Surg Am. 1979;61:320–329. [PubMed] [Google Scholar]
- 14.Frantz C.H. Epiphyseal stapling (1971) a comprehensive review. Clin Orthop Relat Res. 2017;77:149–157. [PubMed] [Google Scholar]
- 15.PM;1 Stevens. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 2007;27:253–259. doi: 10.1097/BPO.0b013e31803433a1. [DOI] [PubMed] [Google Scholar]
- 16.Masse P., Zreik H. Can one determine the age at which epiphysiodesis should be performed in the treatment of genu valgum in the adolescent? Rev Chir Orthop Reparatrice Appar Mot. 1985;71:319–325. [PubMed] [Google Scholar]
- 17.Burghardt R.D., Specht S.C., Herzenberg J.E. Mechanical failures of eight-plateguided growth system for temporary hemiepiphysiodesis. J Pediatr Orthop. 2010;30:594–597. doi: 10.1097/BPO.0b013e3181e4f591. [DOI] [PubMed] [Google Scholar]
- 18.Burghardt R.D., Herzenberg J.E., Standard S.C., Paley D. Temporary hemiepiphyseal arrest using a screw and plate device to treat knee and ankle deformities in children: a preliminary report. J Child Orthop. 2008;2:187–197. doi: 10.1007/s11832-008-0096-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kulkarni Ruta M., Ilyas Rushnaiwala Faizaan M., Kulkarni G.S., Negandhi Rajiv, Kulkarni Milind G., Kulkarni Sunil G. Correction of coronal plane deformities around the knee using a tension band plate in children younger than 10 years. Indian J Orthop. 2015;49(March-April (2)):208–218. doi: 10.4103/0019-5413.152484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ballal M.S., Bruce C.E., Nayagam S. Correcting genu varum and genu valgum in children by guided growth: temporary hemiepiphysiodesis using tension band plates. J Bone Joint Surg Br. 2010;92(February (2)):273–276. doi: 10.1302/0301-620X.92B2.22937. [DOI] [PubMed] [Google Scholar]
- 21.Mycoskie P. Complication of osteotomies about the knee in children. Orthopedics. 1981;4:1005–1015. doi: 10.3928/0147-7447-19810901-04. [DOI] [PubMed] [Google Scholar]