Abstract
Objective
Salmonella osteomyelitis in immunocompromised individuals with sickle cell anaemia is well documented. Its occurrence in immunocompetent children is rare.
Methods
All pus culture positive cases of salmonella typhi between the period 2009 to 2014 were reviewed and only those children without sickle cell disease or trait were considered further.
Results
Eighty five patients had positive cultures. Of these only three children had culture positive Salmonella septic arthritis in the absence of sickle cell disease. Two children had shoulder septic arthritis while one had hip septic arthritis.
Conclusion
Our case series highlights the possibility of salmonella typhi osteomyelitis in immunocompetent individuals. Clinicians should be aware of this presentation which is usually delayed due to the atypical organism and lack of clinical response in the initial stages, as disastrous sequelae of septic arthritis may result if prompt treatment is not initiated in time.
Keywords: Salmonella, Osteomyelitis, Septic arthritis, Child, Immunocompetent
1. Introduction
Septic arthritis can occur in any joint, but if not diagnosed early can lead to devastating complications. The most common organism causing septic arthritis in infants and children less than 3 years is Staphylococcus aureus.1 Osteomyelitis caused by atypical organisms are often termed atypical osteomyelitis.1 Salmonella is commonly considered in the differential diagnosis of osteomyelitis in children with sickle cell anaemia but Salmonella osteomyelitis and septic arthritis are rare in immunocompetent children who do not have sickle cell disease or trait.2,3
Salmonella is an encapsulated, motile, facultative anaerobic bacilli, gram negative, coliform group bacteria belonging to the family of enterobacteraciae.4 The reported incidence of Salmonella osteomyelitis is 0.45% in normal population and it is 70% in children with sickle cell disease.4, 5 Salmonella typhi is a human pathogen whereas non typhi group of organisms including typhimurium is transmitted from animals.6, 7
Most common cause of Salmonella septic arthritis is Non Typhoidal Salmonellae (NTS).8 S choleraesius and S typhimurium are the most common pathogens known to be isolated from the cases with septic arthritis due to Salmonella species.9
We present our experience with management of osteomyelitis with concurrent septic arthritis caused by Salmonella species in immunocompetent children.
2. Materials and methods
A retrospective review of microbiological data base for pus culture positive Salmonella infections reported in our institute from 2009 January to 2014 February was undertaken. The search retrieved 85 cases reported as Salmonella positive. Among these cases, 14 patients were in paediatric (<18 years) age group and five out of fourteen had culture positive Salmonella septic arthritis. This study was approved by the institutional review board. Inclusion criteria included children <18 years age, normal health condition without immunosuppression, no sickle cell disease or trait.
Two of the five children had sickle cell disease and were not included in this report. We elaborate the clinical features of the three children who were immunocompetent and did not have sickle cell disease.
3. Results
3.1. Case 1
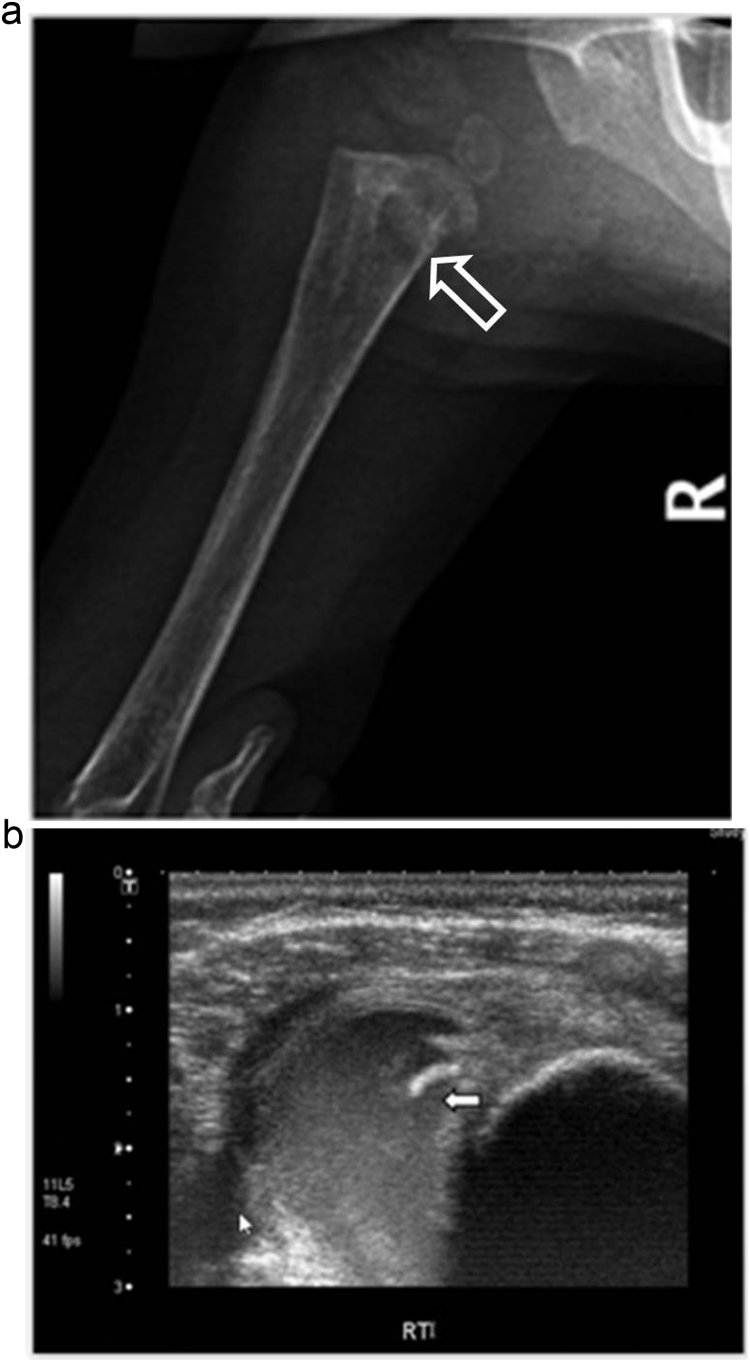
A nine month old male infant presented with complaints of paucity of movements of right upper limb for ten days and fever for three days. There was no history suggestive of any antecedent respiratory or skin infection. Clinical examination revealed warmth and tenderness in the proximal aspect of right arm. Radiographs of the right shoulder revealed a metaphyseal lytic lesion in the proximal humerus with cortical erosion of the medial cortex (Fig. 1a,b). He underwent arthrotomy and decompression of the right shoulder and proximal humerus. The pus culture grew Salmonella enterica subspecies enterica serotype typhimurium. The child was started on ceftazidime and ciprofloxacin following the antibiotic sensitivity report. She was on empirical antibiotics initially. Histopathological examination of tissue from proximal humerus was reported as acute osteomyelitis. On second post-operative day, the infant developed hypotensive shock, and underwent resuscitation with saline boluses (totally 40 ml/kg) and dopamine in paediatric ICU and eventually stabilized. Haemoglobin was low with low mean corpuscular volume, low serum iron and high total iron binding capacity attributed to iron deficiency anaemia for which oral iron supplementation was started. Antibiotics were continued for a total of four weeks. The child had recovered completely at six month follow-up with remodelling of the proximal humerus on the radiograph.
Fig. 1.
a) Radiograph showing metaphyseal lytic lesion in the proximal humerus with erosion of medial cortex (open white arrow). Demonstrating the concurrent shoulder septic arthritis and osteomyelitis. (b) Ultrasound of shoulder shows hypoechoic sub-periosteal abscess (white arrow) in the proximal humerus.
3.2. Case 2
An 18 month old girl child presented with swelling and pain in the right shoulder for 10 days. There was history of associated high grade fever. The child had been treated with oral antibiotics for ten days before referral to our centre. At presentation, there was swelling of the shoulder with tenderness and restriction of movements of the shoulder joint. Ultrasonogram revealed joint effusion and radiographs showed periosteal reaction in the proximal humerus (Fig. 2) The child underwent right shoulder arthrotomy. She was empirically started on crystalline penicillin, cloxacillin and gentamicin and later changed to injection ceftriaxone from the fourth post-operative day as the culture grew Salmonella enterica subspecies enterica serotype typhi. 2 weeks of IV ceftriaxone and 4 weeks of oral cefuroxime. At 10 weeks follow up, the child was asymptomatic and had full range of motion of the right shoulder joint.
Fig. 2.
Radiograph of the right proximal humerus showing the periosteal reaction.
3.3. Case 3
An eleven year old boy presented with persistent pain around the left groin, limiting his hip movements for two weeks. He had been diagnosed elsewhere with typhoid fever and received treatment for the same. Examination revealed tenderness over left hip joint and restriction of movements. His hip radiographs revealed apparent abduction deformity and widened medial joint space (Fig. 3). Left hip aspiration revealed 15 ml of thick yellowish pus. He underwent left hip arthrotomy and washout. Culture grew Salmonella enterica subspecies enterica serotype typhi species. He was empirically treated with crystalline penicillin, cloxacillin and gentamicin initially and shifted to ciprofloxacin and ceftriaxone based on sensitivity. He was discharged on oral ciprofloxacin and cefixime for 4 weeks. (Table 1, Table 2)
Fig. 3.
Radiograph of the pelvis with hip showing the medial joint space widening in the left hip with apparent abduction deformity.
Table 1.
Pus culture reports of three children showing isolated organisms, antibiotic sensitivity and blood picture.
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Organism | Salmonella enterica subspecies enterica serotype Typhimurium | Salmonella enterica subspecies enterica serotype Typhi | Salmonella enterica subspecies enterica serotype Typhi species |
| Susceptible to | Nalidixic Acid, Co-Trimoxazole, Ampicillin Chloramphenicol, Ciprofloxacin |
Ampicillin, Ceftriaxone, Cotrimoxazole-Chloramphenicol | Ampicillin,Ceftriaxone, Cotrimoxazole, Chloramphenicol |
| Ciprofloxacin resistance | Cipro MIC* not done | Cipro MIC* – 0.25 μ/ml-intermediate. | Cipro MIC*- 0.38 μg/ml – intermediate |
| ESR | 80 mm/hr | 58 mm/hr | 94 mm/hr |
| Total count | 18900/mm3 | 14,400/mm3 | 9400/mm3 |
| Hb | 8.7 gm% | 9.4 gm% | 10.2 gm% |
MIC: Minimum inhibitory concentration.
Table 2.
Decreasing serial CRP (C reactive protein) values following antibiotic therapy.
| CRP Case 1 | Case 2 | Case 3 | |||
|---|---|---|---|---|---|
| Day 1 | 85.2 | Day 1 | 48.1 | Day 1 | 62.9 |
| Day 5 | 17.3 | Day 5 | 45.5 | Day 5 | 125 |
| Day 12 | <3.08 | Day 9 | 4.69 | Day 12 | 13.1 |
4. Discussion
Osteomyelitis and concurrent septic arthritis due to salmonella species in immunocompetent children is a rare entity.10 Presence of transphyseal capillaries in the hip, shoulder, elbow and ankle enable seeding of infection across the physis. Mahajan et al. in their article had speculated that this entity was either under-recognised or that it was a new emerging pathogen.11 Most of the case reports have been from India and this is not surprising as enteric fever is endemic in India.6, 11, 12 Agnihotri et al., 5 reported a case of septic arthritis of the hip, Naithani et al.,12 reported its existence in a immunocompromised neutropenic child. Govendhar et al., 13 reported cases from South Africa mostly comprising adults and Adeyokunnu et al. had only one immunocompetent child in their series of sixty three children from Nigeria, who presented with multifocal osteomyelitis, rest having sickle cell disease, sickle cell trait or were carriers.2 Our series highlights that Salmonella might be considered as a possible pathogen even in immunocompetent children who fail to respond to the standard treatment regimen. These children may present late as osteomyelitis with septic arthritis, which is difficult to recognize early in atypical cases, as they usually do not respond to conventional treatment in the initial stages. These patients however, make a complete recovery if prompt surgical drainage is carried out and appropriate antibiotics are started. An inordinate delay in treatment of septic arthritis places a child at risk for a poor result.1 It is not possible to clinically differentiate Salmonella septic arthritis from other unusual pathogens as we have to rely on the culture reports. However, those who fail to respond to standard antibiotics for the common pathogens encountered should be investigated for other rare ones as shown in this report. All three cases in our series failed to drop the CRP until the appropriate antibiotic was started. We evaluated all these patients with the immunodeficiency panel for any predisposition to Salmonella infection. All of them had normal findings in the immunodeficiency workup, which included IgA, IgG, IgM, CD4+ count, CD4+:CD8+ ratio and total protein. None of the children had history of recurrent infections, weight loss, positive viral markers or low leucocyte count to suggest the same. Differential diagnosis of acute rheumatic fever/JIA/Ewing’s were considered as these children presented late and CRP failed to decrease after starting the routine flucloxacillin for presumed staphylococcus aureus sepsis before cultures were available. Sensitive intravenous antibiotics were administered until CRP showed a downward trend with clinical improvement, following which they were shifted to oral antibiotics (Table 4).
Table 4.
Algorithm for treatment of Septic arthritis with Salmonella.
 |
Salmonella osteoarticular infection is common in children with underlying disorders like sickle cell disease, immunocompromised conditions like connective tissue disorders, chronic steroid intake, diabetes mellitus, lymphoma, liver diseases, previous surgery or trauma and those at extremes of age.12 To the best of our knowledge, there have been no reports of shoulder septic arthritis due to salmonella in an immunocompetent child (Table 3).
Table 3.
Published English literature on Salmonella septic arthritis in immunocompetent children.
| Year | Author | Joint | Age (years) |
|---|---|---|---|
| 1983 | Horesh Z (Hebrew) | Knee | NA |
| 1990 | Govender S | Hip (4), knee (2) | 12,13,14,15,15,16 |
| 1993 | Siam AR | Sacroilitis | 13 |
| 1993 | Menon KP | Sacrolilits | 17 |
| 1994 | Fule RP | Elbow | 4 |
| 1995 | Osman | NA | 15 |
| 1997 | Alsoub H | Sacroiliac joint | 13 |
| 2001 | Chiu S | Hip | Child |
| 2005 | Agnihotri N | Hip | 7 |
| 2010 | Faseela T S | Hip | 16 |
| 2012 | Mahajan RK | Hip | 3, 5, 6 |
| 2014 | Pocock JM | Hip | 12 |
| 2015 | Current study | Shoulder, hip | 9months,18months, 11 years |
Osteomyelitis occurs in 0.8% of cases with typhoid fever.13, 14 Blood culture was negative in all our cases indicating that occult bacteraemia was present in our cases. In our patients, all Salmonella typhi cultures had intermediate resistance to ciprofloxacin. As has been recently reported in literature, there is an emerging resistance to ciprofloxacin which was evident in our series too. This was reportedly due to mutations in DNA gyrase and topoisomerase IV gene (gyrA &parC).15 Emergence of antibiotic resistance was noted among both the Salmonella typhi cases in our series. Blood culture was negative in our patients and literature has shown that the reported incidence of the blood culture positivity is only 25–30%.16
In our report, the NTS organism was sensitive to all common antibiotics against Salmonella. The child responded well to ceftazidime and ciprofloxacin. Though there are no definite guidelines for the choice of antibiotics it is advisable to follow the local sensitivity pattern based on microbiology reports. As a protocol, we start antibiotics only after collecting the specimen for culture in all cases of uncomplicated septic arthritis. Hyperbaric oxygen has also been reported in literature since the NTS are facultative anaerobes; however, we have no experience with this modality.17 Osteomyelitis due to NTS usually is monoarticular, but can involve rare sites like pelvis, spine, tarsals, sacroiliac joint, skull, radius and ulna. These organisms have been reported to exhibit resistance to ampicillin and cotrimoxazole at the rate of 30% and 3.6% respectively.18 On the contrary, the isolate in our report was sensitive to ampicillin and cotrimoxazole also indicating the variable pattern of sensitivity of antibiotics to Non Typhoidal Salmonellae (NTS) in our setting.
Galanakis et al. had postulated that children less than one year of age are especially prone to NTS infections.17 NTS bacteraemia is predisposed in children with malnutrition, anaemia and malaria. All our three patients had haemoglobin levels below the threshold level for anaemia for their corresponding age group as defined by WHO.19 Chronic anaemia may be a predisposing factor for susceptibility to uncommon pathogens like Salmonellae as described by Adeyokunnu in the Nigerian children.2 However it has been shown by Nathani et al. that Salmonella can cause serious infection based on its virulence alone.12 Two of our three children (case two and three) presented late after ten and fourteen days of treatment elsewhere with antibiotics but prompt surgical drainage and appropriate antibiotic therapy resulted in complete recovery without disastrous complications such as dislocation, growth arrest, chronic osteomyelitis or limb length discrepancy. It may be that these infections are being picked up with better microbiological culture methods or these hitherto non-pathogenic organisms have acquired virulence over time as hypothesised by Mahajan et al.14 Our study underscores the importance of prompt surgical management of Salmonella infection with appropriate antibiotic resulting in complete recovery without any long term sequel. Diagnosis of septic arthritis in children is entirely clinical and a high index of suspicion is needed to successfully treat musculoskeletal infection caused by atypical organisms in children, as early recognition leads to better outcomes.
This study is not without limitations. Being a retrospective study, our study has the inherent limitations of all retrospective studies and inference needs to be drawn with caution.
5. Conclusion
Our report highlights the possibility of concurrent Salmonella typhi/NTS osteomyelitis and septic arthritis in immunocompetent children. It should be kept as one of the differentialdiagnosis for those who fail to respond to the usual regimen of antibiotics.
Patient declaration
Written informed consent to publish data and images was obtained from the patients/guardians concerned.
Authors contribution
BB was involved in conceiving the idea, data collection and drafting the article, SG was involved in data collection, collaborating with authors from other departments, NP was involved in data collection and revision, SK was involved with conceptualisation and revision, JAJ was involved with conceptualisation and revision, TP was involved with conceiving, drafting and revision of the study
Acknowledgements
The authors would like to acknowledge the secretarial assistance….Details to be added later (*in line with the journal policy not to reveal any author identity). The authors would like to acknowledge the secretarial assistance Mrs Malathy, Secretary, Paediatric Orthopaedic unit, Paul Brand Building, CMC Vellore, Tamil Nadu, India, rendered during the writing up of this article.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors declare that there is no conflict of interest
Contributor Information
Balasubramaniam Balakumar, Email: dr.b.balakumar@gmail.com.
Sangeet Gangadharan, Email: drsangeetgangadharan@gmail.com.
Nithya Ponmudi, Email: nannu.ponmudi@gmail.com.
Satish Kumar, Email: satishkumar@cmcvellore.ac.in.
John Jude Prakash, Email: prakjaj@cmcvellore.ac.in.
Thomas Palocaren, Email: thomaspalox@cmcvellore.ac.in.
References
- 1.Mckarthy J.J., Dormans J.P., Kozin S.H., Pizzutillo P.D. Musculoskeletal infections in children. J Bone Joint Surg Am. 2004;86:850–863. [Google Scholar]
- 2.Adeyokunnu A.A., Hendrickse R.G. Salmonella osteomyelitis in childhood. A report of 63 cases seen in Nigerian children of whom 57 had sickle cell anaemia. Arch Dis Child. 1980;55:175–184. doi: 10.1136/adc.55.3.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhan M.K., Bahl R., Bhatnagar S. Typhoid and paratyphoid fever. Lancet. 2005;366:749–762. doi: 10.1016/S0140-6736(05)67181-4. [DOI] [PubMed] [Google Scholar]
- 4.Rayan F., Mukundan C., Shukla D.D. A case of relapsing Salmonella osteomyelitis in a thalassaemia trait patient. J Orthop Traumatol Off J Ital Soc Orthop Traumatol. 2009;10:31–33. doi: 10.1007/s10195-008-0033-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thanni L. Bacterial osteomyelitis in major sickling haemoglobinopathies: geographic difference in pathogen prevalence. Afr Health Sci. 2006;6:236–239. doi: 10.5555/afhs.2006.6.4.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agnihotri N., Dhingra M.S., Gautam V., Gupta V., Kaushal R., Mehta D. Salmonella typhi septic arthritis of hip–a case report. Jpn J Infect Dis. 2005;58:29–30. [PubMed] [Google Scholar]
- 7.Huang D.B., DuPont H.L. Problem pathogens: extra-intestinal complications of Salmonella enterica serotype Typhi infection. Lancet Infect Dis. 2005;5:341–348. doi: 10.1016/S1473-3099(05)70138-9. [DOI] [PubMed] [Google Scholar]
- 8.Haeusler G.M., Curtis N. Non-typhoidal Salmonella in children: microbiology, epidemiology and treatment. Adv Exp Med Biol. 2013;764:13–26. doi: 10.1007/978-1-4614-4726-9_2. [DOI] [PubMed] [Google Scholar]
- 9.Sarguna P., Lakshmi V. Neonatal septic arthritis due to Salmonella typhimurium. Indian J Med Microbiol. 2005;23:66–67. doi: 10.4103/0255-0857.13880. [DOI] [PubMed] [Google Scholar]
- 10.Pezone I., Penna M.R.D., Flamini S., Nigro G. Non-typhoidal Salmonella septic arthritis in an immunocompetent child with a pharyngeal streptococcal infection. Int J Infect Dis IJID Off Publ Int Soc Infect Dis. 2009;13:e35–36. doi: 10.1016/j.ijid.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Mahajan R.K., Chaudhary J., Chaskar P., Arya R.K., Duggal N., Hans C. Septic arthritis due to Salmonella Typhi in children—a case series. J Biosci Med [Internet 2012] 2014 http://www.jbscience.org/index.php?journal=jbscience&page=article&op=download&path%5B%5D=117&path%5B%5D=pdf [Google Scholar]
- 12.Naithani R., Rai S., Choudhry V.P. Septic arthritis of hip in a neutropenic child caused by Salmonella typhi. J Pediatr Hematol Oncol. 2008;30:182–184. doi: 10.1097/MPH.0b013e318161aa67. [DOI] [PubMed] [Google Scholar]
- 13.Govender S., Chotai P.R. Salmonella osteitis and septic arthritis. J Bone Joint Surg Br. 1990;72:504–506. doi: 10.1302/0301-620X.72B3.2341457. [DOI] [PubMed] [Google Scholar]
- 14.Mathuram A., Rijn R.V., Varghese G.M. Salmonella typhi Rib osteomyelitis with abscess mimicking a cold abscess. J Glob Infect Dis. 2013;5:80–81. doi: 10.4103/0974-777X.112271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson G., Prabhu N., Easow J.M., Mukhopadhyay C. Ciprofloxacin-resistant Salmonella enterica serotype typhi in a patient with osteomyelitis of the rib. Med J Malaysia. 2005;60:667–669. [PubMed] [Google Scholar]
- 16.Dizbay M., Sezer B.E., Arman D. Salmonella osteomyelitis and soft tissue abscess secondary to corticosteroid treatment. Gazi Med J. 2014 [Internet] 2007 cited 2014 4:18. medicaljournal.gazi.edu.tr/index.php/GMJ/article/download/168/166. [Google Scholar]
- 17.Lima A.L., Oliveira P.R., Carvalho V.C. Recommendations for the treatment of osteomyelitis. Braz J Infect Dis. 2014;18:526–534. doi: 10.1016/j.bjid.2013.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galanakis E., Bitsori M., Maraki S., Giannakopoulou C., Samonis G., Tselentis Y. Invasive non-typhoidal salmonellosis in immunocompetent infants and children. Int J Infect Dis IJID Off Publ Int Soc Infect Dis. 2007;11:36–39. doi: 10.1016/j.ijid.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Beutler E., Waalen J. The definition of anemia: what is the lower limit of normal of the blood hemoglobin concentration? Blood. 2006;107:1747–1750. doi: 10.1182/blood-2005-07-3046. [DOI] [PMC free article] [PubMed] [Google Scholar]