Abstract
Background
Pseudoaneurysms as result of orthopaedic injuries are a known clinical entity. But with increase in operative interventions and use of implants, its incidence is bound to increase. It is important to detect this complication at the earliest to avoid any limb or life threatening problems. Selective angiography is a minimally invasive technique to pin point the diagnosis and at the same time allow for therapeutic embolization/stenting of the pseudo aneurysm.
Methods
A retrospective review of inpatients from January 2007 to January 2013 requiring transarterial embolization/stenting for pseudoaneurysm in the limbs. All patients had evidence of pseudoaneurysm as proved by radiological findings. Angiographic intervention in a cath lab was performed, following which patients were monitored for morbidity and mortality benefits on short and long term follow up.
Results
Out of the total 13 patients; 7 adults and 1 child underwent embolisation with polyvinyl alcohol particle/soft metal coil, whereas the remaining 5 adults underwent revascularisation with covered stent. The mean age of patients in our case series was 41.92 ± 18.89 years. The mean follow up period of the group was 14.61 ± 12.21 months. All but one patients showed significant clinical improvement with endovascular management with no procedure related mortality.
Conclusion
Endovascular management is the modality of choice in comparison to other procedures for traumatic pseudoaneurysms in both paediatric and adult patients.
Keywords: Traumatic Pseudoaneurysms, Endovascular coiling, Stents, Outcome
1. Introduction
Pseudoaneurysm as a result of orthopaedic injuries1 and their management is a well known entity with pseudoaneurysms being documented after all spectrum of musculoskeletal injuries varying from sprains, closed reductions, interlock nailing,2 plating, arthroscopies3 and joint replacements.4 These aneurysms are the result of a tangential injury in an arterial wall through which blood continues to flow.5 This continues gradually and the aneurysm continues to grow and encroach upon the surrounding tissues. It may at times rupture causing massive haemorrhage which can be life or limb threatening. Once the diagnosis of a pseudoaneurysm has been made, it is imperative to intervene surgically to prevent the growth and the complications of these aneurysms.
The conventional approach in the management of these aneurysms has been a direct approach to the lesion followed by ligation or resection with a venous graft. This technique is demanding, costly in terms of prolonged hospital stay and patient morbidity. Selective angiography and therapeutic embolization for the treatment of pseudoaneurysms is a technique which aids in diagnosing the exact site and size of the aneurysm. The embolization can be done with a variety of materials and is a minimally invasive method to diagnose and treat pseudoaneurysms.
Taking into consideration the complications associated with the conventional open surgical methods and the advantages of arterial angiography and embolization, seven patients with a pseudoaneurysm as a result of orthopaedic surgical intervention were diagnosed and managed by selective arterial angiography and simultaneous therapeutic selective embolisation.
In the present study, we audited our experience with the use of endovascular management in a catheterisation laboratory for traumatic pseudoaneurysm to address various important issues of limb survival benefit, morbidity and mortality on short to long term follow up.
2. Material and methods
A retrospective review of hospital record of inpatients from January 2007 to January 2013 was performed after approval from Ethics Committee in a tertiary care hospital. Data was collected on patients who underwent Arterial Embolisation which included demographics, injury specific data, physical findings, X-ray findings, operative intervention,length of hospital stay and final outcome at discharge.
A high index of suspicion of pseudoaneurysm was kept in patients presenting to emergency and outpatient department who presented with either a pulsatile swelling, uncontrollable bleeding or non responding pain following an Orthopaedic injury with the use of metal work. Indications to perform angiography were determined after active extravasation of contrast on CT scan. Angiography/Angioraphic embolization was performed after taking informed consent from patient/patient’s relative as per protocol.
Angiography and embolization/stenting was performed in a cath lab with angiographic Philips Allura Integris System (Philips Medical Systems, Best, The Netherlands). Arterial access was obtained via the femoral artery in the lower limbs and brachial artery in the upper limbs using the Seldinger technique. A 5–8, 10 French Cordis sheath was then placed to secure the arterial access and different diagnostic catheters (3French Cook’s microcatheter, 5–7 French Judkin catheter, 6–7 French crossover sheath, 0.014 PTCA guidewire of Abott and 0.35” Teurner guide to cross the lesion) were then used to access the culprit vessels and diagnostic arteriograms were performed. The arteriograms of culprit vessels either demonstrated active contrast extravasations, pseudoaneurysms and were selectively embolised/stented resulting in stasis of blood flow.
In cases where pseudoaneurysm was found to be arising from a small artery, of less importance which could be sacrificed, it was embolised with help of poly vinyl particles/coils or thrombin injection; and where it was arising from large artery it was isolated with help of an expandable stent graft of appropriate size, using front and back technique.
3. Results
During the 6 year period, out of 15,786 trauma patients presenting to Orthopaedics and trauma department, thirteen patients were taken up for arterial angiographic embolization/stenting in the catheterisation laboratory and were evaluated. Demographics showed that 62% were men and 38% were 0045">During the 6 year period, out of 15,786 trauma patients presenting to Orthopaedics and trauma department, thirteen patients were taken up for arterial angiographic embolization/stenting in the catheterisation laboratory and were evaluated. Demographics showed that 62% were men and 38% were women. The mean age of patients was 41.92 (range 10–71 years). Mechanism of injury was due to road traffic accidents in 8 (61.5%) and accidental/domestic fall in 4 (30.8%). 6 (46%) patients had post traumatic vascular injury, while 7 (54%) had injury following operative intervention Fig. 1 out of which 6 (46%) were following use of metal work and one had following central venous cannulation. 7 (54%) patients presented early (within 15 days of trauma/intervention), while 6 (46%) presented late (3 weeks-9 months following trauma). None of the late presenting cases was infected in our series.
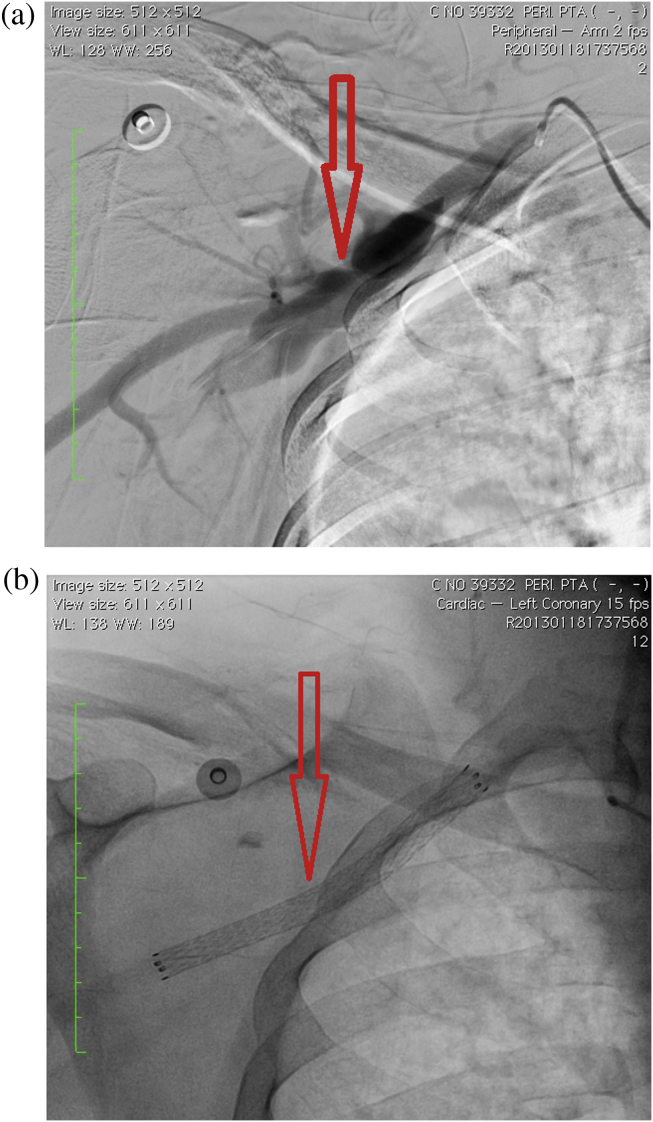
Fig 1.
(a): Case 2: Pseudoaneurysm in branch of Profunda Femoris following Dyanmic Hip Screw Removal. (b): No leakage following embolisation with PV particles.
Arterial injuries was confirmed by MDCT scan in 100% of the series. 8 (61.5%) patients had pseudoaneurysm in artery of lower limb, while upper limb was involved in 5 (38.5%). Embolisation was done in 7 (53.8%) patients. Polyvinyl alcohol (PVA) particles ranging from 350 to 750 μm and soft metal coils made from Teflon O35 wire were used for embolization.(Fig. 2) In 5 (38.5%) patients covered stent (WARD) was used to bypass the pseudoaneurysm.(Fig. 3)In one patient (Case No. 13), additional thrombin injection was used, as following stenting there was filling of pseudoaneurysm from the surrounding vessels and good end result was obtained.
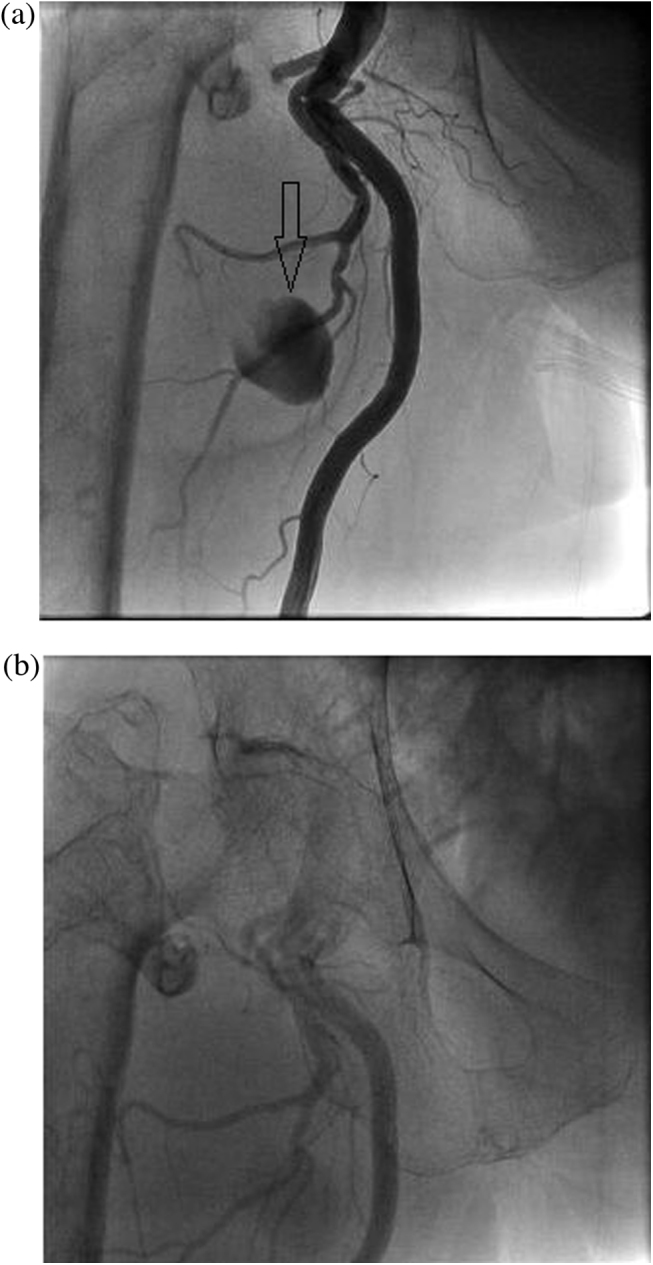
Fig. 2.
(a): Case 3: Pseudoaneurysm in Posterior Tibial Artery, due to schanz pin impingement. (b): Embolisation with PV particles.
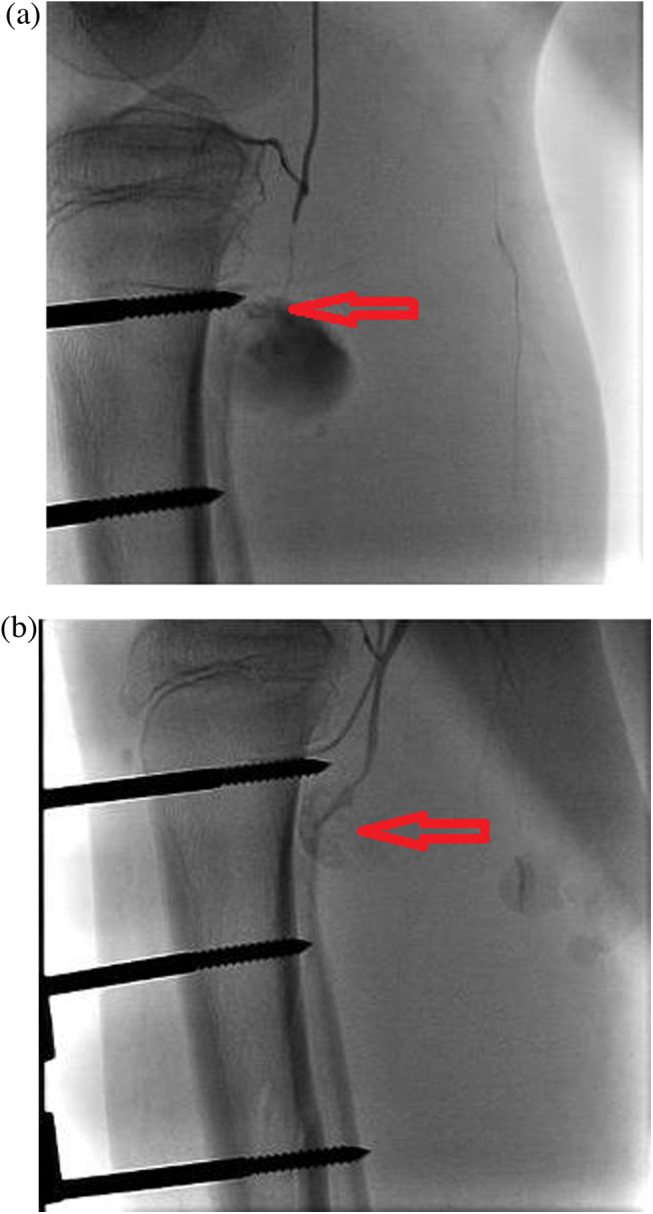
Fig. 3.
(a): Case 4: Pseudoaneurysm in branch of Superficial Femoral Artery following Dyanmic Hip Screw insertion. (b) Stenting with covered stent done.
All patients underwent successful angiographic embolization/stenting and there was no procedure related mortality in the group. One patient had angiography related local complications, a pseudoaneurysm in brachial artery which was managed with thrombin injection. In all cases the involved limb was salvaged following the procedure. In Case No. 12, on MDCT there was injury in the axillary artery with complete cutoff and plan was kept for surgery, but following embolization, brachial artery was found to be filling from collaterals, so no further intervention was done
All patients were followed up till June 2013 (range 12–36 months) and no rebleed or necrosis of the limb was reported.
4. Discussion
False aneurysms in the vicinity of a fracture and orthopaedic implants are a well recognized entity. The diagnosis and early treatment of pseudoaneurysms is important owing to the fact that any complication attributed to them can severely compromise the function of a limb and possibly lead to an amputation.
Traumatic pseudoaneurysms follow incomplete disruption of an artery and result in leakage of blood into the surrounding tissues.6 The uninjured portion of the arterial wall prevents the vessel from contracting leading to unbridled extravasation, which in due course organises and develops a fibrous capsule.7 However, turbulent blood flow continues in the central region. False aneurysms are distinguished from true aneurysms by a wall composed of fibrous tissue rather than components of the normal arterial wall.8
The various vessel traumas that lead to pseudoaneurysms include blunt injury,9 direct trauma and branch avulsion. Penetration by a drill bit, excessive screw length, sharp bone fragment or placement of the retractor too deep during surgery are documented as the causes of pseudoaneurysm formation.10, 11 In our series six out of thirteen cases developed pseudoaneurysm postoperatively.Apart from surgical injury, certain patient factors may predispose to pseudoaneurysm formation for example atherosclerotic peripheral vascular disease can lead to formation of collateral vessels and hence larger than expected vessels in unexpected positions that may not tamponade as expected. In another predisposed group, patients receiving anticoagulants, take longer to seal traumatized vessels, and are more likely to experience prolonged bleeding. This group includes patients with recently discontinued warfarin and with subcutaneous heparin. Similar is the case in patients with congenital bleeding diatheses.
In our series, nearly half of these cases were caused by use of metal work. So, it can be concluded that pseudoaneurysms caused due to use of metal work are not that uncommon as it was thought to be previously. To prevent this complication we recommend the use of meticuluous surgical dissection and techniques, achieving good haemostasis, choosing proper screw lengths and appropriate size of schanz pins for external fixators.
The classical presentation of psudeoaneurysm is that of an enlarging pulsatile swelling. A systolic bruit may be audible and a thrill may be present. Distal pulsations are usually present.Classic signs of arterial injury such as pulse deficit, bruit, arterial bleeding and expanding or pulsatile haematoma may be absent despite significant damage to the arterial wall. Aneurysms may mimic soft-tissue masses including abscesses, neoplasms or ganglions. The inflammation that results subsequent to organisation of the haematoma may masquerade as an infection because local heat and tenderness are usually present. In our series Case No. 3, 4, 5 and 8 presented only with dull ache in the concerned region, without the classical features of pseudoaneurysm. So in cases presenting with dull pain after operative intervention or following trauma, which is not getting relieved after trial of analgesics, a possibility of pseudoaneurysm should be kept.
The interval between injury and the appearance of the clinical presentation of the pseudo aneurysm may vary from less than one week up to years.12 In our series, seven patients presented to us within fifteen days following injury. Late presentation was of Case No. 4, who presented to us nine months following initial trauma. There was no infection related to the formation of pseudoaneurysms in our case series.
The initial diagnosis depends on a high degree of clinical suspicion and usually followed by an ultrasound doppler. Various other modalities have been reported to establish the diagnosis of these aneurysms, but angiography remains the gold standard.
Although some pseudoaneurysms can thrombose spontaneously, they usually need treatment, as there is a risk of continued expansion leading to rupture, adjacent structure compression, infection, or embolization.4
Multiple management strategies can be applied to pseudoaneurysms; options range from ultrasound compression13, 14 to thrombin injection,15 radiologic intervention and surgery. The management of arterial pseudoaneurysms depends on their location and size and the presence or absence of infection. Some pseudoaneurysms may simply be observed if they are less than 10 mm in size, are asymptomatic, and involve arteries of minor importance. Larger aneurysms, those that become symptomatic, or those that involve major arteries in which occlusion would threaten severe ischaemic effects generally require intervention.
Ultrasound compression is limited by position deep within muscle compartments, late presentations, and large pseudoaneurysm neck size making its use in orthopaedic cases limited. Thrombin injection again is dependent on access and on appropriate pseudoaneurysm neck length,thus limiting its use.
Many surgical techniques have been reported like resection, ligation and vein grafting. The most appropriate technique depends on the site and size of the lesion. The conventional treatment has been to directly approach the aneurysm followed by ligation of the artery proximal and distal to the lesion. If need arises a venous graft may have to be put in order to establish the blood flow in case the aneurysm is present in an artery which cannot be sacrificed. Open surgical repair can be difficult because of large haematoma and risk of active bleeding, which can further reduce the accessibility to the artery.Most of the times the approach to an aneurysm may require considerable soft tissue dissection which may further compromise the safety of the surrounding neurovascular structures. Another concern is the increased chance of infection as a result of soft tissue damage during an open approach.
Selective angiography is a minimally invasive technique which helps to exactly localize the site of the aneurysm and at the same time the aneurysm can be treated in the form of embolization or bypass. This is very cost-effective, reduces patient’s hospital stay and also does not increase the chance of infection to the affected limb. It offers the advantage of minimally invasive approach with no surgical incision. Proper patient selection and timely diagnosis are the two most important factors which determine the successful outcome of the use of this technique for managing pseudo aneurysms.
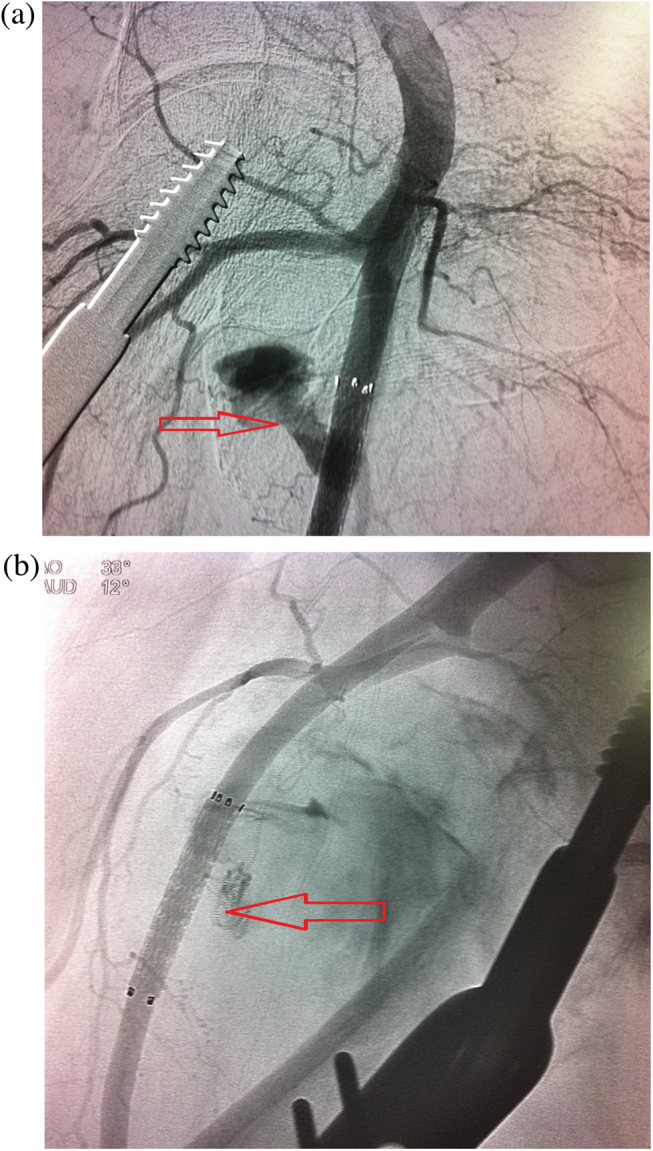
In our series all the thirteen cases were effectively managed by selective angiography. In the present series eight pseudoaneurysm were managed in the lower limb vessels, while five were present in the upper limb vessels. So, selective angiography is an effective tool for management of pseudoaneurysms both in the upper as well as lower limb. In cases where the artery in which pseudoaneurysm had formed was found to be of a small calibre and had good collateral circulation, in those cases it was sacrificed, and embolization was done. In cases where pseudoaneurysm was seen to be arising from a major vessel, there it was bypassed with a covered stent as in Case No: 4, 8, 9, 10, 11(Fig.4) and 13. There is risk of stent fracture of about 10%, but still in patients where vessel supplying the limb is a major vessel which couldn’t be sacrificed, stenting is preferred over embolization and patients are put on long term antiplatelet therapy(single anti platelet for at least 6 months).
Fig. 4.
(a) Case 11: Pseudoaneurysm in subclavian artery following fracture clavicle. (b): Bypass done with a covered stent.
At the mean followup of 14.61 ± 12.21 months, all the patients were doing well, with no signs of ischemia or bleed.
Our case series strongly puts forth the view that pseudoaneurysms following injury are an important cause of concern for the clinicians which needs to be tackled with immaculate radiological evaluation followed by prompt clinical endovascular management. But one should be careful of endoleak in large vessels and filling of pseudoaneurysm from collateral vessels.
5. Conclusion
High degree of suspicion and timely embolization/stenting can not only save the limb, but also avoids surgery which has high mortality and morbidity. In brief,the comprehensive management of traumatic pseudoaneurysms in our cathlab involving a team approach of orthopaedic surgeon, interventionist, anesthesist, and intensive care physician adjudicates the use of embolization/stenting as the gold standard treatment in all age group of patients. The results with regular follow up till date points out to our strategy being thoroughly effective with nil mortality rate. To conclude, angiographic embolization/stenting should be concomitantly used in all age groups following early or late pseudoaneurysm formation for a successful outcome.
Conflict of interest
The authors have none to declare.
Contributor Information
Bishav Mohan, Email: bishav_68@yahoo.co.in.
Shekhar Singal, Email: shekharsingla@gmail.com.
Akshdeep Singh Bawa, Email: bawa.akshdeep@gmail.com.
Pankaj Mahindra, Email: pmahindra@hotmail.com.
Mohammad Yamin, Email: drmyamin@gmail.com.
References
- 1.Gantz E.D., Sweet M.B., Jakim I. False aneurysm mimicking an aggressive soft-tissue tumor. A case report. J Bone Joint Surg Am. 1988;70:1090–1092. [PubMed] [Google Scholar]
- 2.Dickson J.W. False aneurysm after intramedullary nailing of the femur. J Bone Joint Surg Br. 1968;50:144–145. [PubMed] [Google Scholar]
- 3.Vincent G.M., Stanish W.D. False aneurysm after arthroscopic meniscectomy: a report of two cases. J Bone Joint Surg Am. 1990;72:770–772. [PubMed] [Google Scholar]
- 4.Umar S., Jagjeeth N., Verma P. Endovascular management of pseudoaneurysms following lower limb orthopedic surgery. Am J Orthop. 2008;37(5):E99–E102. [PubMed] [Google Scholar]
- 5.Spencer F.C., Imparato A.M. Peripheral arterial disease. In: Schwartz S.I., Lillehei R.C., Shires G.T., Spencer F.C., Storer E.H., editors. Principles of Surgery. 2nd ed. McGraw Hill; New York: 1969. pp. 900–901. [Google Scholar]
- 6.Dhal A., Chadha M., Lal H., Singh T., Tyagi S. Encounters with pseudoaneurysms in orthopedic practice. Injury. 2001;32(10):771–778. doi: 10.1016/s0020-1383(01)00094-8. [DOI] [PubMed] [Google Scholar]
- 7.Zitsman J.L. Pseudoaneurysm after penetrating trauma in children and adolescents. J Pediatr Surg. 1998;33(10):1574–1577. doi: 10.1016/s0022-3468(98)90504-8. [DOI] [PubMed] [Google Scholar]
- 8.Inamdar D., Alagappan M., Shayam L., Devadoss S., devadoss A. Pseudoaneurysm of the anterior tibial artery following tibial nailing: a case report. J Orth Surg. 2005;13(2):186–189. doi: 10.1177/230949900501300216. [DOI] [PubMed] [Google Scholar]
- 9.Atta H.M., Tagoe A., Walker M.L. Delayed presentation of popliteal artery pseudoaneurysm following blunt trauma. Am Surg. 1997;63(6):496–499. [PubMed] [Google Scholar]
- 10.Fordyce A. False aneurysm of the profunda femoris artery following nail and plate fixation of an intertrochanteric fracture. J Bone Joint Surg. 1968;50B:141–143. [PubMed] [Google Scholar]
- 11.Yang K.H., Park M.W., Park S.J. Pseudoaneurysm of the superficial femoral artery after closed hip nailing with a Gamma nail. J Orthop Trauma. 2002;16:124–127. doi: 10.1097/00005131-200202000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Laohapoonrungsee A. Y sirirungruangsarn. J Med Assoc Thail. 2005;88(11):1703–1706. [PubMed] [Google Scholar]
- 13.Paschalidis M., Theiss W., Kolling K., Busch R., Schomig A. Randomised comparison of manual compression repair versus ultrasound guided compression repair of postcatheterisation femoral pseudoaneurysms. Heart. 2006;92(2):251–252. doi: 10.1136/hrt.2004.053793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Danzi G.B., Sesana M., Capuano C. Compression repair versus lowdose thrombin injection for the treatment of iatrogenic femoral pseudoaneurysm: a retrospective case–control study. Ital Heart J. 2005;6(5):384–389. [PubMed] [Google Scholar]
- 15.Olsen D.M., Rodriguez J.A., Vranic M., Ramaiah V., Ravi R., Diethrich E.B. A prospective study of ultrasound scan–guided thrombin injection of femoral pseudoaneurysm: a trend toward minimal medication. J Vasc Surg. 2002;36(4):779–782. [PubMed] [Google Scholar]