Abstract
Background
Management of unstable pertrochanteric fractures remains a challenge with various implant choices. Intramedullary devices are usually preferred for the management of the unstable fractures. When nailing is unsuitable for the configuration of the fracture extra medullary procedures are preferred. PFLCP is a contact limited implant that allows multiple angularly stable fixations with preserving more bone stock after implantation as an extramedullary implant. There are only a few reports in the literature about the osteosynthesis of unstable trochanteric fractures with proximal femoral locking compression plates and their results are conflicting. In the present study we aimed to evaluate the functional and radiological outcomes of proksimal femoral locking compression plates in open reduction and internal fixation of AO/OTA 31A2-2 and 3 fractures.
Methods
Patients older than 18 years of age with a minimum follow-up time of 1 year matching the inclusion criteria retrospectively evaluated. Patients’ demographics, Singh index, intra and post-operative data, mobilization and union time gathered from the patients’ files. Baumgaertner modified criteria of fracture reduction was used to assess the post-operative reduction quality. Early and last follow-up radiographs were used to evaluate malunion and change in neck- shaft angle. Final clinical outcome was assessed using the Harris Hip scoring system.
Results
18 male and 13 female patients with the mean age of 74 (46–88) met the inclusion criteria. Reduction quality according to Baumgaertner modified criteria was good in 25 patients and acceptable in 6. Mean union time was 21.53 ± 4.18 weeks. There was neither non-union nor malunion. The mean neck-shaft angle change was −3.1° ± 2.16°. The mean HHS was 77.90 ± 4.84 and there was no significance in HHS according to reduction quality and change in neck-shaft angle (p = 0.385, p = 0.0059). HHS was negatively correlated with age, mobilization time and, longer union time (p < 0.05). There was no correlation between Singh index and reduction quality (p = 0.865). Singh index was only correlated with the patient’s age (p = 0.000, rho = −0.595). There were 2 infections and, 2 backing of the proximal screws.
Conclusion
Even though PFLCP is not the first choice in management of unstable pertrochanteric fractures, it must be kept in mind as an alternative to the other conventional plates and intramedullary implants with the properties of an increased stability by multiaxial screw locking and the results are satisfactory when appropriate settlement achieved.
Keywords: Unstable intertrochanteric fracture, Pertrochanteric fracture, Locking compression plate, Proximal femoral locking compression plate, Hip fractures
1. Introduction
Pertrochanteric fractures account for nearly 50% of all proximal femoral fractures with mortality rates ranging from 4.5% to 22%.1, 2 These fractures are associated with functional disability, loss of mobility and independence.3 While stable intertrochanteric fractures are usually managed with sliding hip screws (SHS), the unstable fractures remain a challenge with various implant choices and less clearly defined indications with mechanical complication rates reaching 20%.4, 5, 6, 7 Although unfavorable results have been shown with the use of SHS and the side plates, the 95° angle blade plates have better results.8 However, the 95° angle blade plates are technically difficult to implant and have higher failure and revision rates when compared to intramedullary nails. And also, 95° angle blade plates clinical outcome is similar to locking plates but they require a more extensile approach.6, 9 When unstable trochanteric fractures are managed by dynamic hip screws (DHS), shortening, medialisation of the distal fragment, implant cut–out, lateralization of proximal fragment and, varus collapse are common.4 Proximal femoral locking compression plates (PFLCP) offer certain advantages to address these complications of DHS.4 The intramedullary devices are usually preferred for the management of the unstable fractures because of biomechanical advantages.5, 6, 9, 12, 13, 14, 15 But, when nailing is difficult or unsuitable for difficult fracture patterns with comminution or when the medullary canal is narrow for the intramedullary implantation, extra medullary procedures are preferred.9, 16, 17 As an extra medullary implant PFLCP is a contact limited implant that allows multiple angularly stable fixations.2, 8 It preserves more bone stock after implantation and, it is also stronger and stiffer than the other angular stable implants especially in osteoporotic fractures.2, 8, 10, 11
The intact lateral trochanteric wall is an another key point of the stabilization of unstable trochanteric fractures and breakage of this wall causes collapse of the fixation.18 This complication has not been yet reported while fixing unstable trochanteric fractures via percutaneous plating.18 Locking plates with lateral wall buttress are also useful for maintaining reduction of unstable fractures.4, 17, 18
There are only a few reports in the literature about the osteosynthesis of unstable trochanteric fractures with proximal femoral locking compression plates and their results are still conflicting.1, 2, 6, 8, 10 Considering the issues mentioned above, we have aimed to report the clinical and radiological results of PFLCP in the management of unstable trochanteric fractures. We hypothesized that the functional results are independent in terms of the change in neck-shaft angles and reduction quality.
2. Materials and methods
The patients with unstable multifragmentary pertrochanteric fractures who were treated between 2009 and 2015 via proximal femoral locking compression plate (PFLCP) (PERI-LOC® PFP, Smith & Nephew, Inc., Memphis, USA) were enrolled in this retrospective study.
The inclusion criteria were; age older than 18 years old with a fracture of AO/OTA 31A2-2 or 31A2-3 multifragmentary pertrochanteric fracture, an American Society of Anesthesiologist (ASA) score of 1–4 and minimum follow-up time of 12 months. Polytrauma patients and patients with pathologic fractures and concomitant severe medical conditions (ASA 5) were excluded.
The operations were performed with the patients supine on the fracture table under fluoroscopic guidance. After closed reduction under fluoroscopic control, standard lateral approach over the trochanteric region was used to perform PFLCP. Minimally invasive approach was used whenever possible.
After the admission of the patient, anti-coagulative therapy with low molecular weight heparin was begun and continued for 3 post-operative weeks. All patients received single dose 1 gr. 1st generation cephalosporin prophylaxis prior to surgery. Patients received 4 more doses of cephalosporin after surgery.
Active and passive exercises for the ankle joint and quadriceps strengthening were begun under the supervision of the physiotherapists on the first postoperative day. All patients were mobilized with toe-touch using a walking frame on day 1 or 2.
Patients’ AO/OTA classification, preoperative Singh index, demographics, average time from injury to surgery, post-operative blood loss, the mean mobilization time, and length of hospital stay were noted from the file records. All patients were followed for over 12 months.
Routine follow-ups were done at 6th week, 3rd, 6th and 12th post-operative months. Partial weight bearing was allowed at the 6th post-operative week for all of the patients. Full weight bearing was encouraged if fracture healing was evident with callus seen on at least 3 cortices.
The quality of fracture reduction was assessed according to the modified criteria of Baumgaertner et al. 19 Time for union was assessed retrospectively from the patients’ files. Plain radiographs that were obtained at the early postoperative period and at the last follow-up visit were used to measure femoral neck-shaft angles. Change in the femoral neck-shaft angles (CNSA) and malunion were noted. At least 10° of varus in femoral neck −shaft angle accepted as malunion. Final clinical outcomes were assessed using the Harris Hip Scoring system (HHS) at the last follow-up.20
Statistical analyses were performed using SPSS software (v11.5; SPSS Inc. Chicago, IL, USA). Categorical variables were reported as frequencies (percent). The baseline characteristics compared for equality by means of an independent samples T-test for continuous variables, Mann-Whitney U test for two unpaired groups. Pearson’s rank correlation was used when looking for statistical dependence between two variables. A p value <0.05 is considered as statistically significant.
3. Results
31 patients with 31 fractures met inclusion criteria. Mean patient age was 74 (46–88) years old. 13 (41.9%) of the patients were female where as 18 (58.1%) were male. The mechanism of trauma was ground-level fall in 21, traffic accident in 6 and, high −level falls in 4 of the patients. Patients’ co-morbidities are outlined on Table 1. Patients’ demographics, fracture classification, preoperative Singh index, average time from injury to surgery, bleeding measured post-operatively in the hemovac drain, the mean mobilization time and, length of hospital stay are outlined on Table 2.
Table 1.
Medical co-morbidities of the patients.
| Co-morbidities | PF-LCP (n:14) |
|---|---|
| Hypertension | 3 |
| Chronic obstructive pulmonary disease | 2 |
| Chronic renal disease | 1 |
| Diabetes mellitus | – |
| Alzheimer | – |
| DM and Hypertension | 5 |
| DM and Alzheimer | 2 |
| DM and Parkinson | 1 |
Table 2.
Demographics’ of the patients.
bValues are expressed as means ± standard deviations.
| PATIENTS | PF-LCP | |
|---|---|---|
| Sex (F/M) | 13 F/18 M | |
| Agea | 74 (46–88) |
|
| Fracture side (n) | Right | 19 |
| Left | 12 | |
| Fracture classification (n) | OTA/AO | |
| 31 A2-2 | 17 | |
| ASAa | 2 (1–4) |
|
| Pre-op hospitalization time (days)b | 3.49 ± 1.52 | |
| Singh Index (n) | Grade 2 | 13 (41.9%) |
| Grade 3 | 12 (38.7%) | |
| Grade 4 | 6 (19.4%) | |
| Bleeding measured post-operatively in the hemovac drain b (units) | 1.03 ± 0.66 | |
| Surgical time (min.)b | 90.42 ± 15.14 | |
| Mobilization time (days)b | 2.87 ± 1.45 | |
| Length of stay (days)b | 10.71 ± 3.7 |
a Values are expressed as averages with minimum and maximum values in parentheses.
bValues are expressed as means ± standard deviations.
Postoperative reduction quality according to Baumgaertner criteria was good in 25 patients and was acceptable in 6 patients (Table 3). The mean HHS of the patients’ who had reduction qualities assessed as good was 78.24 ± 5.04 and, 76.20 ± 3.63 whom had reduction qualities assessed as acceptable. There was no statistically significance in HHS according to the Baumgaertner’s reduction quality (p = 0.385). Mean union time was 21.53 ± 4.18 weeks and there was neither non-union nor malunion. When the post-operative early mean neck-shaft angle compared with the mean neck-shaft angle assessed at the final follow-up there was change in neck- shaft angles with a mean angle of −3.1° ± 2.16° (Table 3). There was no correlation between HHS and CNSA Table 4. The mean early postoperative and last follow-up femur neck-shaft angle, mean CNSA, mean follow-up time, union time and, HHS at the last follow-up is outlined in Table 3.
Table 3.
Baumgaertner criteria of reduction, functional and radiological results.
| PF-LCP (n:31) |
||
|---|---|---|
| Baumgaertner criteria of reduction | Good | 25 (80.6%) |
| Acceptable | 6 (19.4%) | |
| Post-op femur neck-shaft anglea | 129.45°±3.10 | |
| Last follow-up femur neck-shaft anglea | 126.5°±3.71 | |
| Change in neck −shaft anglea (degrees) | −3.1 ± 2.16 | |
| HHSa | 77.90 ± 4.84 | |
| Union timea (weeks) | 21.53 ± 4.18 | |
| Total Follow- upa (weeks) | 24.19 ± 6.47 |
Values are expressed as mean ± standard deviations.
Table 4.
Correlations between HHS and mobilization time, Singh index, change neck-shaft angle, length of stay, follow-up time, union time and patients’ age.
| HARRİS |
||
|---|---|---|
| r | p* | |
| Post-op mobilization | −0.523 | 0.003# |
| Singh index | 0.090 | 0.637 |
| Change in neck-shaft angle | 0.349 | 0.059 |
| Lenght of stay | −0.236 | 0.209 |
| Follow-up time | 0.134 | 0.481 |
| Union time | −0.571 | 0.001# |
| Age | −0.504 | 0.005# |
Spearman/Pearson’s correlation coefficient.
p value is <0.05 and statistically significant.
The HHS was negatively correlated with age, mobilization time and union time (Table 4).
There was no statistically significance between Singh index and, Baumgaertner’s reduction quality (p = 0.865). The Singh index was found positively correlated with a statistically significance only with the patients’ age (rho = −0.593, p = 0,000) Table 5.
Table 5.
Correlations between Singh index and, mobilization time, change in neck-shaft angle, length of stay, follow-up time, union time and patients’ age.
#p value is <0.05 and statistically significant.
| SINGH Index |
||
|---|---|---|
| r | p* | |
| Change in neck-shaft angle | 0.141 | 0.458 |
| Union time | 0.031 | 0.872 |
| Age | −0.593 | 0.000# |
*Spearman/Pearson’s correlation coefficient.
#p value is <0.05 and statistically significant.
There were 2 (6.45%) infections. One of them was superficial and managed with IV antibioteraphy for 2 weeks. The second patient was an 88 years old male with AO/OTA 31A2-3 fracture. Infection was diagnosed four weeks after the initial surgery and implants had to be removed. After the treatment of the infection via IV antibioteraphy for 6 weeks, he did not accept further surgery.
There was no implant failure, cutout of the screws and, secondary varus displacement. Backing out of the proximal locking screws occurred in 2 (6.45%) patients 4 and 6 months after surgery respectively. The fracture union had already occurred when this was detected and patients were symptom free. No intervention was deemed necessary.
4. Discussion
In the present study, management of unstable pertrochanteric fractures with PFLCP yielded good results. Infection and backing out of the screws were the only complications. There was no correlation found between CNSA, reduction quality and functional results as hypothesized. And, it was seen that patient’s age, mobilization time and, union time directly affecting the functional results, where as there was no correlation between osteoporosis (according to Singh index) and functional results and, reduction quality.
Even though the results of the management of pertrochanteric fractures with PFLCP are conflicting, agreement has been achieved on the restoring stability and early mobilization.1, 2, 8, 17, 21, 22 Where as the intramedullary implants has many complications such as cut-out, Z-effect, reverse Z-effect and, femoral shaft fractures, management of pertrochanteric fractures with PFLCP stated as lowering these complications by three-dimensional and angular stable fixation along the study of 110 patients.2 Collinge et al. associated the excellent results of Zha et al.2 to the usage of PFLCP only in selected cases that are unsuitable to perform intramedullary options.23
According to Oh et al., the 6 locking screw holes at the proximal part of the plate which they had used was the reason for avoiding implant failure and nonunion in their series.21 Similarly, the implant, which we used also, had 6 proximal locking screw holes and this may have led to increased stiffness in the neck and the head of the femur especially in osteoporotic fractures as stated (Fig. 1). Failure rates were stated as fewer with the implant that we used compared to other implants that had 3 proximal holes.23 On the other hand, Hu et al. reported a series consisted of AO 31-A3 or 31-A2.3 fractures with a union of 43 in 45 fractures even though the plate that they had used had only 3 proximal locking screw holes.17 According to their study the reason of failure was early weight bearing (before 8 weeks).17 Saini et al. also reported similar gratifying results in their study with delaying of weight bearing of 6 six weeks.22 Delayed weight bearing must be the accepted post-operative protocol when these implants are used in unstable pertrochanteric fractures.23 Our findings are the same as Collinge et al.’s23 and delaying weight bearing is necessary to avoid complications such as malunion or nonunion in management by PFLCP because of the biomechanics of the construct.
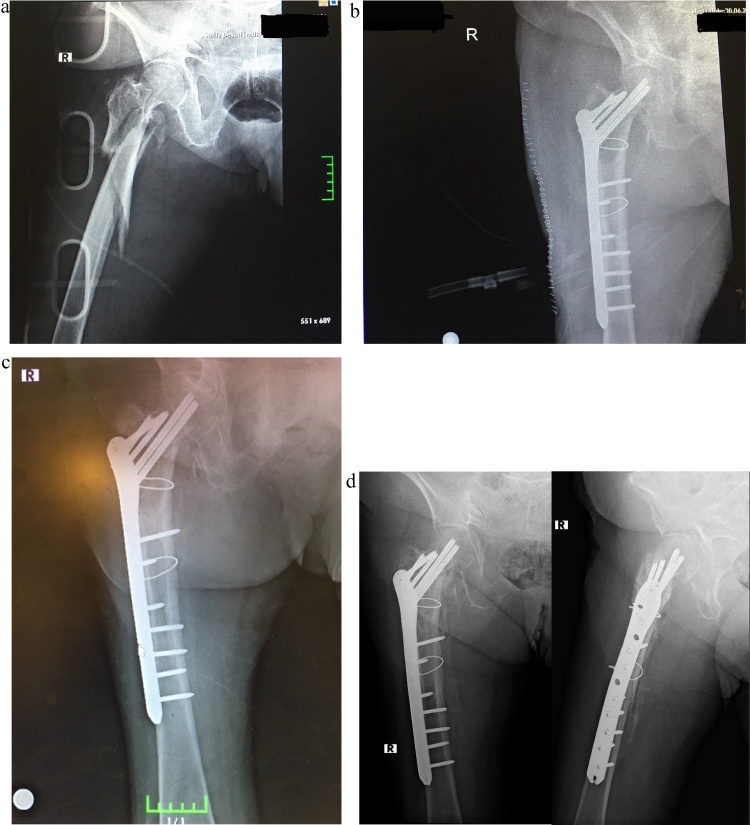
Fig. 1.
a and b: Pre-operative and early post-operative radiographs of an 83 years old patient sustaining OTA/AO 31A2-3 fracture. c Post-operative 3th month radiography. d Post-operative 12th month AP and lateral radiographs.
Not all of the studies on PFLCP are promising.1, 6, 8 Wirtz et al. reported 19 patients with trochanteric fractures with high rates of varus collapse, cut-out of proximal screws and screw brakeage.1 The re-operation rate was 52.6% in the study group and, the main reason was loss of posteromedial buttress.1, 24, 25 These results point to the importance of accurate medial buttressing in order to reduce the risk of failure while managing pertrochanteric fractures.1 On the contrary, Streubel et al. reported that the rate of failure was not lowered when the medial buttress was reduced appropriately.8 While the compression along the long axis of the femur by the plate in simple fractures is advantageous, its significance in unstable fractures is unclear.8 In the study of Wirtz et al., patients were allowed partial weight bearing immediately for 6 weeks and they have stated that the size and the number of proximal screws were small to provide stable fixation at the proximal part, so they recommended using screws with larger diameter and polyaxial orientation.1 Similarly, Streubel et al. reported a failure rate of 33% in a year and related this to the strength of the proximal construct with small number of proximal screws rather than the plate strength.8 Glassner and Tejwani reported a failure rate of 7 out of 10 in their series.10 Considering this study10 patients were not homogenous in primary diagnosis and they were encouraged early weight bearing. Either heterogeneity of primary diagnosis and early weight bearing or both of these seem to be the reason of failures.10 According to Saini et al. the failures in the study of Glassner and Tejwani’s10 were related to the patients and surgical technique rather than the weakness of the construct.22 Improper placement of the PFLCP usually results in breakage or backing out of the screws.6 Its importance was stated in a case series with a failure rate of 41.4%.6 Inadequate reduction also leads progressive loosening of locking screws.24 It is demonstrated that the failure was associated with loosening in younger patients where as it was associated with screw cutout in elderly.8 It was also emphasized that 2° of off-axis of the proximal screws leads to failure and failure was associated to the surgical technique rather than the weakness of the construct.16 Although there is no improper placement of the plate and inadequate reduction, we had screw backing out in 2 patients without malposition. We thought that improper locking of the screws could have caused this complication.
In osteoporotic fractures subsidence in the femoral neck and head can occur even though PFLCP does not allow controlled collapse.4, 24, 26 The resulting compressive forces may aid fracture healing or may lead to varus collapse.4 In the present study, in most cases 6 screws with a diameter of 6.3 mm were used at the proximal part of the fracture and partial weight bearing delayed till postoperative 6th week. Even though there was no malposition, there was a significant change in neck- shaft angles regardless of the age and follow-up time. Even though this issue stated by Kumar et al. with an average varus collapse of lower than 10°, the correlation of this change with the functional results and osteoporosis was not mentioned.26 But when the master chart of this study-Kumar et al.26 is scrutinized it can be easily seen that osteoporosis and varus collapses do not correlate consistent with the present study. Streubel et al. and Wirtz et al. also have not found an association between failure rates and patient age, the only difference was in types of failures related to the ages.1, 8 On the contrary, Johnson et al. reported that the failure rate was higher in elderly, especially in women.6 Even though the cause of higher failure rates in the elderly females was not pointed out in that study6, the reason might be osteoporosis. In the present study, we found no correlation between osteoporosis and the neck- shaft angle changes by the time and, also these changings were not affecting the HHS. The mean HHS of 77.90 ± 4.84 in our series was consistent with the written literature.21, 22, 27 In other series importance of neck shaft angle change in functional outcome was not stated out.4, 24 Nonetheless, Wirtz et al. stated out the importance of osteoporosis without statistical significance in small number of patients, osteoporosis and old age were not suggested as predisposing factors for loss of reduction.1
The retrospective design and relatively small patient sample are the limitations of the present study. The main reason for this is that we have aimed to report the results of certain subtypes of pertrochanteric fractures (AO/OTA 31 A2-2 and A2-3) that are regarded as multifragmentary and unstable. Further prospective studies with a larger, homogenous patient size are needed to make any certain comment.
5. Conclusion
As a conclusion, in the light of the literature and, according to the findings of this study PFLCP technique is not the first choice in unstable pertrochanteric fractures. But it must be kept in mind as an alternative to the other conventional plates with the properties of an increased stability by multiaxial screw locking and, possibility of minimally invasive application when the fracture configuration is hard to manage with aforementioned implants. And additionally the functional results of unstable pertrochanteric fractures are seem highly associated with the patient’s age, mobilization time and union time.
Conflict of interest
None.
Contributions of the authors
Emrah Kovalak: Planning the study, archive research, evaluating the results and writing the manuscript. Cenk Ermutlu: Archive research, evaluating the results and writing the manuscript. Tolga Atay: Evaluating the results and writing the manuscript. Özgür Başal: Archive research, evaluating the results.
Footnotes
This study is carried on Süleyman Demirel University and İstanbul Education and Research Hospital Departments of Orthopedics and Traumatology.
References
- 1.Wirtz C., Abbassi F., Evangelopoulos D.S. High failure rate of trochanteric fracture osteosynthesis with proximal femoral locking compression plate. Injury. 2013;44:751–756. doi: 10.1016/j.injury.2013.02.020. [DOI] [PubMed] [Google Scholar]
- 2.Zha G.C., Chen Z.I., Qi X.B., Sun J.Y. Treatment of pertrochanteric fractures with a proximal femur locking compression plate. Injury. 2011;42:1294–1299. doi: 10.1016/j.injury.2011.01.030. [DOI] [PubMed] [Google Scholar]
- 3.Eberle S., Gerber C., von Oldenburg G. Type of hip fracture determines load share in intramedullary osteosynthesis. Clin Orthop Relat Res. 2009;467:1972–1980. doi: 10.1007/s11999-009-0800-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dhamangaonkar A.C., Joshi D., Goregaonkar A.B., Tawari A.A. Proximal femoral locking plate versus dynamic hip screw for unstable intertrochanteric femoral fractures. J Orthop Surg. 2013;21:317–322. doi: 10.1177/230949901302100311. [DOI] [PubMed] [Google Scholar]
- 5.Fogagnolo F., Kfuri M., Jr., Paccola C.A. Intramedullary fixation of pertrochanteric hip fractures with the short AO-ASIF proximal femoral nail. Arch Orthop Trauma Surg. 2004;124:31–37. doi: 10.1007/s00402-003-0586-9. [DOI] [PubMed] [Google Scholar]
- 6.Johnson B.J., Stevenson J., Chamma R. Short-term follow-up of pertrochanteric fractures treated using the proximal femoral locking plate. J Orthop Trauma. 2014;28:283–287. doi: 10.1097/01.bot.0000435629.86640.6f. [DOI] [PubMed] [Google Scholar]
- 7.Knobe M., Drescher W., Heussen N. Is helical blade nailing superior to locked minimally invasive plating in unstable pertrochanteric fractures. Clin Orthop Relat Res. 2012;470:2302–2312. doi: 10.1007/s11999-012-2268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Streubel P.N., Moustoukas M.J., Obremskey W.T. Mechanical failure after locking plate fixation of unstable intertrochanteric femur fractures. J Orthop Trauma. 2013;27:22–28. doi: 10.1097/BOT.0b013e318251930d. [DOI] [PubMed] [Google Scholar]
- 9.Ma C.H., Tu Y.K., Yu S.W. Reverse LISS plates for unstable proximal femoral fractures. Injury. 2010;41:827–833. doi: 10.1016/j.injury.2010.03.028. [DOI] [PubMed] [Google Scholar]
- 10.Glassner P.J., Tejwani N.C. Filure of proximal femoral locking compression plate: a case series. J Orthop Trauma. 2011;25:76–83. doi: 10.1097/BOT.0b013e3181e31ccc. [DOI] [PubMed] [Google Scholar]
- 11.Miller D.L., Goswami T. A review of locking compression plate biomechanics and their advantages as internal fixators in fracture healing. Clin Biomech. 2007;22:1049–1062. doi: 10.1016/j.clinbiomech.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Gadegone W.M., Salphale Y.S. Proximal femoral nail–an analysis of 100 cases of proximal femoral fractures with an average follow up of 1 year. Int Orthop. 2007;408:403–408. doi: 10.1007/s00264-006-0170-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang X., Leung F., Xiang Z. Proximal femoral nail versus dynamic hip screw fixation for trochanteric fractures: a meta-Analysis of randomized controlled trials. Sci World J. 2013 doi: 10.1155/2013/805805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tao R., Lu Y., Xu H. Internal fixation of intertrochanteric hip fractures: a clinical comparison of two implant designs. Sci World J. 2013;2013:834825. doi: 10.1155/2013/834825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tylliananakais M., Panagopoulos A., Papadopoulos A. Treatment of extracapsular hip fractures with the proximal femoral nail (PFN): Long term results in 45 patients. Acta Orthop Belg. 2004;70:444–454. [PubMed] [Google Scholar]
- 16.Schneider K., Oh J.K., Zderic I. What is the underlying mechanism for the failure mode observed in the proximal femoral locking compression plate. A biomechanical study. Injury. 2015;46:1483–1490. doi: 10.1016/j.injury.2015.05.034. [DOI] [PubMed] [Google Scholar]
- 17.Hu S.J., Zhang S.M., Yu G.R. Treatment of femoral subtrochanteric fractures with proximal lateral femur locking plates. Acta Ortop Bras. 2012;20:329–333. doi: 10.1590/S1413-78522012000600003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gotfried Y. The lateral trochanteric wall: a key element in the reconstruction of unstable pertrochanteric hip fractures. Clin Orthop Relat Res. 2004;425:82–86. [PubMed] [Google Scholar]
- 19.Baumgaertner M.R., Curtin S.L., Linskog D.M., Keggi J.M. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Harris W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 21.Oh C.W., Kim J.J., Byun Y.S. Minimally invasive plate osteosynthesis of subtrochanteric femur fractures with a locking plate: a prospective series of 20 fractures. Arch Orthop Trauma Surg. 2009;129:1659–1665. doi: 10.1007/s00402-009-0815-y. [DOI] [PubMed] [Google Scholar]
- 22.Saini P., Kumar R., Shekhawat V. Biological fixation of comminuted subtrochanteric fractures with proximal femur locking plate. Injury. 2013;44:226–231. doi: 10.1016/j.injury.2012.10.037. [DOI] [PubMed] [Google Scholar]
- 23.Collinge C.A., Hymes R., Archdeacon M. Unstable proximal femur fractures treated with proximal femoral locking plates: a retrospective, multicenter study of 111 cases. J Orthop Trauma. 2016;30:489–495. doi: 10.1097/BOT.0000000000000602. [DOI] [PubMed] [Google Scholar]
- 24.Lee W.T., Murphy D., Kagda F.H., Thambiah J. Proximal femoral locking compression plate for proximal femoral fractures. J Orthop Surg. 2014;22:287–293. doi: 10.1177/230949901402200304. [DOI] [PubMed] [Google Scholar]
- 25.Wieser K., Babst R. Fixation failure of the LCP proximal femoral Plate 4.5/5.0 in patients with missing posteromedial support in unstable per-, inter-, and subtrochanteric fractures of the proximal femur. Arch Orthop Trauma Surg. 2010;130:1281–1287. doi: 10.1007/s00402-010-1074-7. [DOI] [PubMed] [Google Scholar]
- 26.Kumar N., Kataria H., Gadagoli B. Evaluation of proximal femoral locking plate in unstable extracapsular proximal femoral fractures: surgical technique and mid term follow up results. J Clin Orthop Trauma. 2014;5:137–145. doi: 10.1016/j.jcot.2014.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Azboy I., Demirtas A., Gem M., Çakır I.A. A comparison of proximal femoral locking plate versus 95- degree angled blade plate in the treatment of reverse intertrochanteric fractures. Joint Dis Related Surg. 2014;25:15–20. doi: 10.5606/ehc.2014.04. [DOI] [PubMed] [Google Scholar]