Abstract
Introduction
In performing surgery for fractures of the pelvis and acetabulum, various surgical approaches have been introduced with their own advantages and drawbacks. The extensile nature of ilioinguinal approach gives excellent exposure but was related to wound healing problems. Modified stoppa has a higher difficulty and poses a risk for neurovascular injury. In this study, we elaborate our experience using the Modified Stoppa approach with additional lateral window while adding few modifications to simplify the procedure and facilitate future implant removal.
Methods
A prospective-retrospective cohort involving 30 anterior pelvic ring and/or anterior column acetabulum fracture patients were conducted from 2012-2016. Fifteen cases were prospectively treated using the modified approach since 2014, while the remaining fifteen cases that were treated using Ilioinguinal approach were retrospectively reviewed. Intraoperative parameters such as blood loss, duration of surgery, quality of reduction (Matta) and postoperative functional outcome (Majeed and Hannover score) at 12 months period were recorded and evaluated by a blinded reviewer.
Result
There were no significant differences between the two groups in mean age, sex and fracture type. The mean blood loss in the MIPO group were 325 ± 225 mL versus 710.67 ± 384.51 mL in the control group (p = 0.002). Duration of surgery were 149.33 ± 91.92 minutes in MIPO group versus 235.71 ± 65.79 minutes in ilioinguinal group (p = 0.014). There were no significant differences noted between the two groups in the quality of reduction and postoperative functional outcome, either by using Majeed or Hannover pelvic score. No complications were found after a 12-months follow up period. Two modified cases already had their implant removed and during the procedure, fibrotic tissue were minimal making the implant removal was less complicated and easier.
Conclusions
Modified stoppa and lateral window technique can be used as a safe and effective alternative approach for anterior pelvic ring fracture and/or anterior column acetabulum fracture. This approach decreased the duration of surgery and blood loss without compromising the quality of reduction and functional outcome in patients.
Keywords: MIPO, Modified stoppa and lateral window, Pelvic fracture, Anterior column, Acetabular fracture
1. Introduction
Definitive surgical management of pelvic and acetabulum fracture has been revolutionized by Letournel in 1961. The introduction of Ilioinguinal approach has allowed surgeons to perform anatomical reduction with adequate visualization of the fracture fragments by exposing the inner surface of the pelvis from the anterior aspect of sacroiliac joint to the pubic symphisis.1, 2 The extensive exposure of ilioinguinal approach provides an excellent visualization of the fracture but is associated with several morbidities and wound healing problems. The need for detaching the anterior abdominal muscle groups and fascia from the ilium along the inguinal canal, may contribute to this problem as well. Related complications such as postoperative wound infections and inguinal hernia have been reported.1, 2, 3, 4 Dissections around the femoral and lymphatic vessels in the attempt to open the second window is also associated with some reported complications such as interruption of the lymphatic system causing limb edema, arterial thrombosis (femoral and inferior epigastric) and femoral nerve injury.4, 5, 6 Postoperative tissue fibrosis in the middle window is a major problem in implant removal, thus it is generally recommended that the plate be left insitu indefinitely.7 This may present a concern in several countries where cultural beliefs dictate that the implant should be removed.
Modifed Stoppa intrapelvic approach for acetabular fracture was introduced by Cole and Bofhofner in 1994. Despite being a less invasive approach, it provides a good visualization of the medial wall of the acetabulum, quadrilateral surface and sacroiliac joint.8, 9 Despite these advantages, this approach is technically more demanding and requires identification and ligation of corona mortis to prevent excessive bleeding intraoperatively. Neurovascular injuries such as obturator nerve palsy and superior gluteal artery injury have also been reported.10 Post operative fibrosis of the internal surface of the pelvis also hinders the possibility of implant removal using this approach.
In the past decade, several minimally invasive approaches have been proposed, either by modifying the Ilioinguinal approach or by adding a lateral window to the original modified Stoppa approach. In this paper, we would like to elaborate our personal experience using the Modified Stoppa approach with an additional lateral window in treating anterior pelvic ring injury and anterior column acetabular fracture, while adding a few modifications to simplify the procedure and facilitate future implant removal. The aim of this study was to evaluate the safety and efficacy of the minimally invasive plate osteosynthesis (MIPO) technique compared with the standard Ilioinguinal approach.
2. Methods
From January 2012 to January 2016, 30 patients (19 males; 11 females) with anterior pelvic ring injury and/or anterior column acetabular fracture were treated in our center. MIPO group were prospectively recruited from March 2014 up to January 2016 and ilioinguinal group were retrospectively analyzed from subjects that were operated during January 2012 and March 2014. Mean patient age was 33.58 ± 12.34 years. Twenty-four patients had anterior pelvic ring injury and six patients had anterior column acetabular fracture. Marvin Tile classification was used to describe the types of pelvic fracture based on the type of instability. Four cases were diagnosed as pelvic fracture Tile A, 11 cases were Tile B and the remaining 9 were Tile C.
Fifteen patients that were admitted prior to the early phase of our study (before March 2014) were operated through standard ilioinguinal approach. The remaining 15 patients were treated using the modified Stoppa and lateral window approach. All procedures were performed by one senior trauma consultant. The average age in the MIPO group was 35.13 ± 8.82 years and 32.13 ± 15.1 years in standard group.
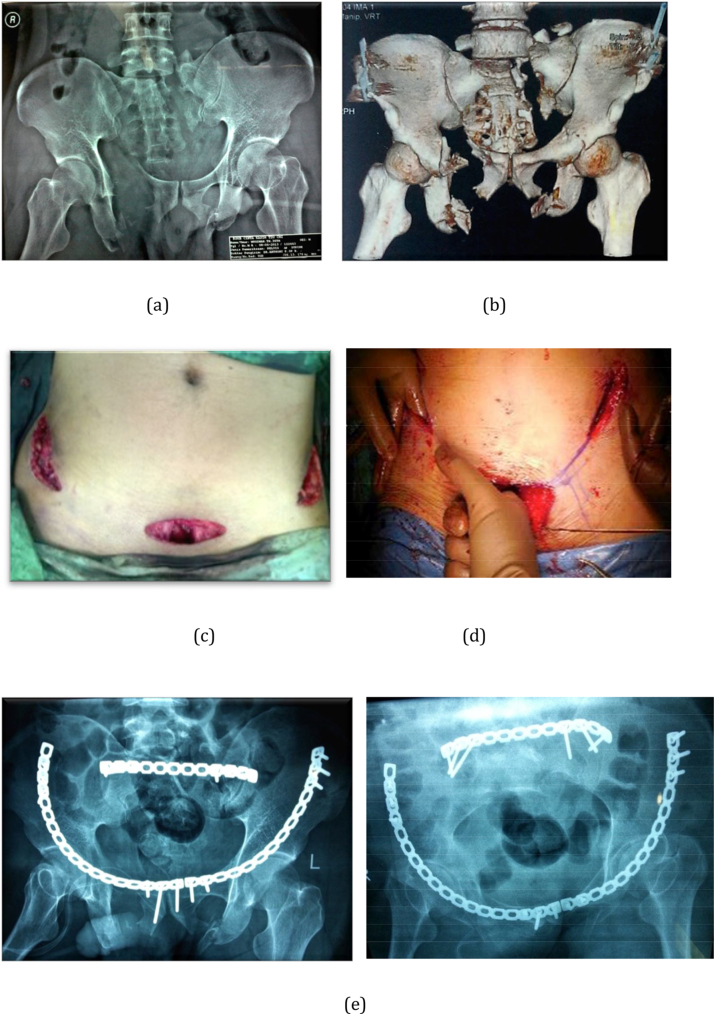
After general anaesthesia was induced, the patient was positioned supine in radiolucent operating Table Standard Letournel ilioinguinal approach was performed in 15 cases, with the pelvic/acetabulum in exposed in three surgical windows. The remaining 15 cases of those who came after March 2014 until January 2016 were treated using the minimally invasive plate osteosynthesis (MIPO) approach and were followed up prospectively. (Fig. 1C).
Fig. 1.
A 36 years old male with unstable pelvic fracture, MT C3 Type right anterior column (a) Preoperative anteroposterior pelvic radiograph showing fracture of right superior and inferior pubic rami, left anterior column acetabular fracture, left sacral fracture and vertical instability of left hemipelvis; (b) 3D reconstruction CT Scan showing clearer image of the fracture pattern. (c) Modified Stoppa and lateral ilioinguinal approach, showing the extent of incision while leaving the second (middle) window intact; (d) Blunt finger dissection subperiosteally connecting the tunnel from both incisions; (e) postoperative anteroposterior pelvic radiograph showing satisfactory reduction of pelvic fracture and anatomical reduction of left anterior acetabular column.
A transverse incision began at one to two finger-breath superior to ipsilateral pubic symphisis and was carried out laterally for about 4–5 cm. Sharp dissection was carried to the anterior rectus fascia and the subcutaneous fatty layer was elevated away from the rectus fascia. The rectus abdominis muscle was split along the linea alba and transversalis fascia was opened just superior to pubic symphisis to allow access to the retropubic space of Retzius. The bladder was mobilized bluntly from the anterior pelvic ring. The insertion of rectus abdominis muscle was left intact on the anterior aspect of pubic rami but was released on the superior part of pubic rami and symphisis. Periosteum of the pubic tubercle was opened and a subperiosteal plane was developed laterally by finger dissection along the surface of the superior ramus.
The lateral incision started at the junction of posterior and middle third of iliac crest and curved towards the anterior superior iliac spine and pubic symphisis for about 4–5 cm long. Lateral femoral cutaneous nerve should be identified and preserved. Origins of abdominal muscle and iliacus muscle at iliac crest were sharply elevated. Further elevation of the iliacus muscle from the inner table of the ilium was done by blunt subperiosteal dissection and continued medially along the surface of quadrilateral space to the superior ramus where the subperiosteal tunnel from both incisions connect. Flexing the hip was also helpful to relax to iliopsoas muscle when creating these tunnels. (Fig. 1D)
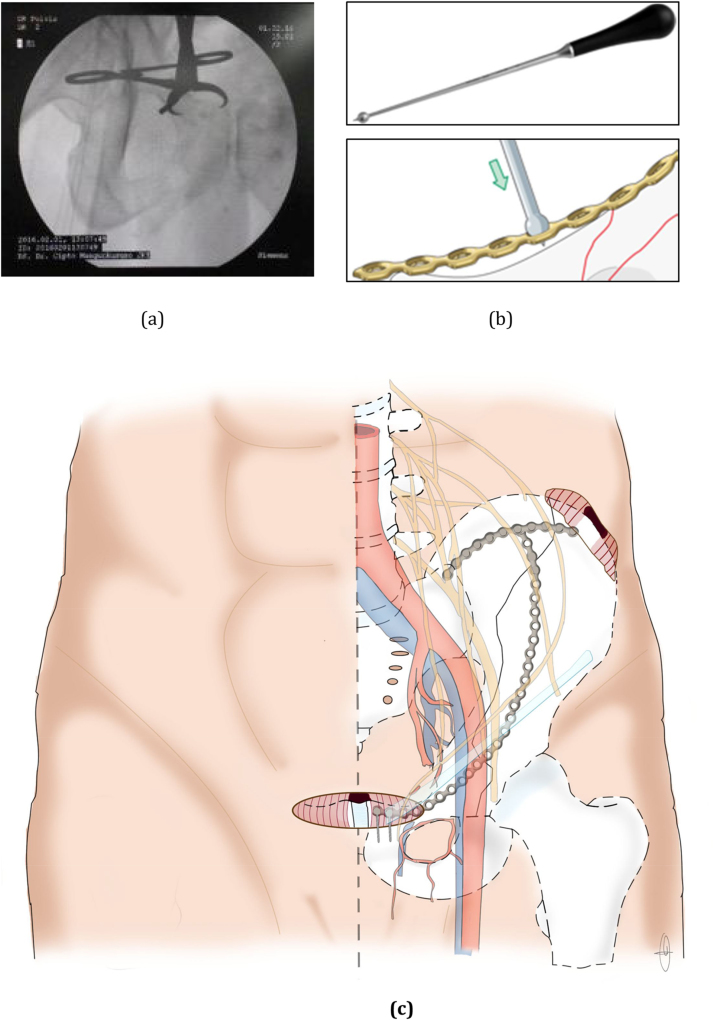
Since the second (middle) ilioinguinal window, in which most fracture site occurred at, was not opened, fracture reduction was evaluated using a C-arm fluoroscopy. Several reduction tools were also used in performing an indirect reduction of the fracture site, such as ball spike pusher or pelvic reduction forceps (Fig. 2). After achieving an acceptable reduction, the 3.5 mm 14–16 holes curved reconstruction plate was inserted to the subperiosteal tunnel from the modified Stoppa window. The plate was placed on the superior part of the ramus to enable screw placement towards the ischiopubic rami. Pre-bending the plate according to 3D CT reconstruction of the pelvis was recommended if possible. A minimum of two screws on each side was inserted into the superior pubic rami and the inner table of iliac wing at a neutral fashion as the function of the plate was only to bridge the fracture fragments. The positions of the plate and screws along with the reduction were verified using the C-arm fluoroscopy (Fig. 3, Fig. 4).
Fig. 2.
Indirect reduction using reduction tools. (a), Pelvic reduction clamp (b) ball and spike pusher (c) Post-fixation-illustration showing the modified Stoppa approach and final fixation of the reconstruction plate after indirect reduction.
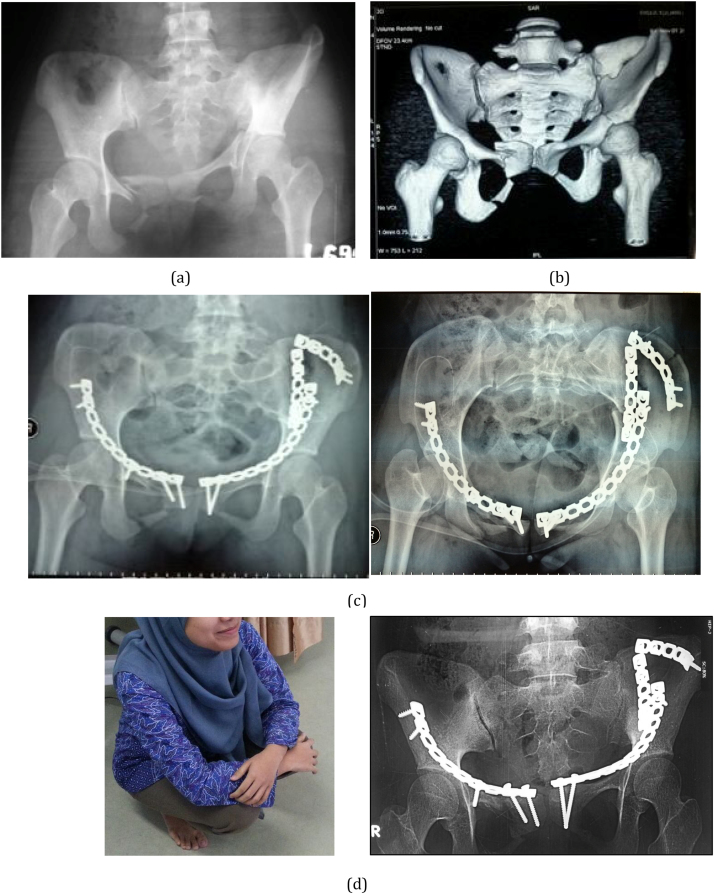
Fig. 3.
A 21 years old female with pelvic and acetabular fracture. (a) The anteroposterior radiograph showed that left acetabular anterior column fracture, superior and inferior right ramus pubis fracture, left iliac wing fracture. (b) Three dimensional CT reconstruction image shows the configuration of acetabular fracture and iliac wing more clearly; (c) Postoperative pelvis anteroposterior radiograph showing satisfactory reduction achieved in left acetabular fracture and satisfactory reduction on right superior pubic rami fracture using modified Stoppa and lateral window approach.
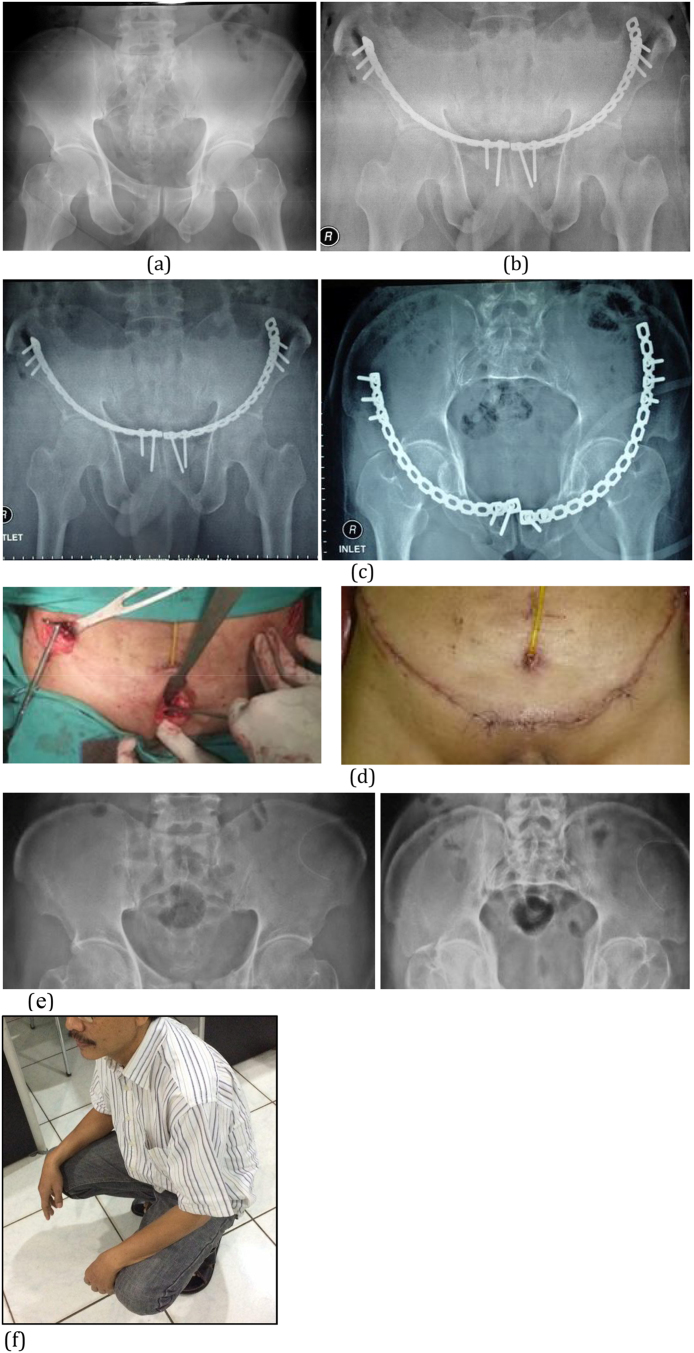
Fig. 4.
A 47 years old male with pelvic Tile A fracture and urethra rupture. (a) Pelvic anteroposterior radiograph showing fracture at bilateral superior and inferior pubic rami, (b) Postoperative pelvic anteroposterior radiograph showing anatomical reduction of the fracture and symphisiolysis using modified Stoppa and lateral window approach (c) Follow-up after 1 year, showing a complete union at both of his pubic ramus. (d) Removal of the implant, second window was necessary to be opened, no fibrosis was found. (e) Post removal x-ray.
Two drains were placed on both incisions and were removed after 3 days or when the blood output is less than 50 mL/24 h. Intravenous antibiotic was given to prevent infection until the drain is removed and was followed by oral antibiotic. Possible postoperative complications were closely monitored during the hospitalization, especially for wound infections and neurovascular injury.
Data on blood loss, duration of surgery, quality of reduction, and clinical functional outcome were collected and reviewed by a blinded reviewer. Intraoperative parameter and duration of surgery were collected from the anesthesia record. Duration of surgery was defined as the time from the first incision to the end of skin closure. Quality of fracture reduction was assessed using postoperative x-ray and then classified according to Matta reduction criteria.11 The criteria were anatomic (less than 2 mm of displacement), satisfactory (2–3 mm), and unsatisfactory (>3 mm). Average displacement on all projections −AP, inlet, outlet view for pelvic fracture and AP, iliac and obtutator oblique view for acetabular fracture − were measured by two blinded reviewers.
Clinical functional outcome were evaluated using the Majeed pelvic score12 and Hannover pelvic score13 at 12 months postoperative period. The patients were directly interviewed at the outpatient clinic or by evaluating the medical record. Numerical data such as blood loss, duration of surgery and Majeed pelvic score were presented as mean ± SD and compared using Mann Whitney (nonparametric test). Categorical data such as Hannover pelvic score and Matta reduction criterion were compared using chi-square analysis or Fischer exact test using SPSS version 23.0.
3. Results
3.1. Patient characteristic
Among the thirty-one anterior column acetabular/anterior pelvic ring injury patients underwent open reduction and internal fixation, 15 were treated through modified Stoppa and lateral window approach while the rest underwent standard ilioinguinal approach. Patient characteristics were summarized in Table 1. There were no significant differences in age, gender and type of fracture between the two treatment groups. We followed up these patients with a minimum of 12 months period.
Table 1.
Patient Demographic and Characteristic.
| Modified Stoppa and lateral window | Standard Ilioinguinal | p value | |
|---|---|---|---|
| Number of cases | 15 | 15 | |
| Age (Mean ± SD) | 35.13 ± 8.82 | 32.13 ± 15.09 | 0.384 |
| Sex (M/F) | 10/5 | 9/6 | 0.809 |
| Fracture type | |||
| Tile A | 3 | 1 | 0.702 |
| Tile B | 5 | 6 | |
| Tile C | 4 | 5 | |
| Anterior column acetabulum | 3 | 3 | |
3.2. Intraoperative record
Average intraoperative blood loss in modified Stoppa and lateral window group was 325.33 ± 225.0 mL compared with 710.67 ± 384.51 mL in standard Ilioinguinal group (p = 0.002). Duration of surgery in minimally invasive group averaged 149.33 ± 91.92 min compared with 229.81 ± 57.69 min in standard Ilioinguinal group (p = 0.014).
3.3. Quality of reduction
Postoperative quality of reduction were assessed based on methods described by Matta et al.11 In modified Stoppa and lateral window group, anatomic result were found in 6 cases and satisfactory results in 9 cases. Meanwhile in standard Ilioinguinal approach, 6 cases had anatomic results and 9 had satisfactory results. In both group, no unsatisfactory result were found. There were no significant differences between the two groups in terms of quality of reduction (p > 0.05).
3.4. Clinical functional outcome
All patients were followed up in outpatient clinic at least 12 months after surgery for clinical evaluation. The mean Majeed pelvic score was 81.73 ± 9.22 points and 78.8 ± 7.47 points for modified Stoppa lateral window approach and Ilioinguinal approach, respectively (p = 0.154). Hannover scoring system in modified Stoppa and lateral window group yielded 87% cases with a very good and good outcome in terms of clinical outcome and 47% cases with complete social reintegration. Meanwhile, in standard ilioinguinal group, 100% of the cases had a very good and good outcome clinically but only 40% had complete social reintegration the result of intra and post operative evaluation in both groups were summarised in (Table 2).
Table 2.
Intra and postoperative comparison between the 2 groups.
| Parameters | Modified Stoppa and lateral window | Standard Ilioinguinal | p value |
|---|---|---|---|
| Blood loss (mL) | 325.33 ± 225.0 mL | 710.67 ± 384.51 mL | 0.002 |
| Duration of surgery (minutes) | 149.33 ± 91.92 | 235.71 ± 65.79 | 0.014 |
| Quality of reduction | 1 | ||
| Anatomic | 6 | 6 | |
| Satisfactory | 9 | 9 | |
| Unsatisfactory | 0 | 0 | |
| Majeed pelvic score | 81.73 ± 9.22 | 78.8 ± 7.47 | 0.154 |
| Hannover clinical outcome (excellent – good percentage) | 87% | 100% | 0.981 |
| Hannover social reintegration (complete reintegration percentage) | 47% | 40% | 0.887 |
3.5. Complications
No intraoperative complications, such as neurovascular injury, were found in both groups. Possible postoperative complications were monitored closely during the hospital stay and in outpatient clinic. There were no signs of femoral nerve or vascular injury, limb edema, superficial or deep infection, as well as venous thrombosis in both groups.
4. Discussions
Minimally invasive modified Stoppa and lateral ilioinguinal window approach was used for selected patients that presented with anterior pelvic injury or anterior acetabular column fracture without involvement of posterior acetabulum that requires fixation. This minimally invasive approach used the modified Stoppa incisions to expose the medial window without detaching rectus abdominis insertion. Exposing the pubic tubercle and superior pubic rami at its anterosuperior part provided a decent space for plate placement and the use of reduction tools. Lateral window was made from iliac tubercle to anterior superior iliac spine and connected to the medial window through subperiosteal tunnel. Periosteal stripping at both sites of the incisions was necessary in creating this tunnel in order to prevent injury to neurovascular structures.
Some surgeons have reported their experience using the modified Stoppa approach and recommended that additional lateral window is necessary if the acetabular fracture line extends to the iliac wing.14 Modified Stoppa may provide an excellent visualization of the anterior and posterior column of acetabulum but it has a high level of difficulty.10, 14 In our series, we modified this approach only to exclusively expose the medial window without extending the dissection laterally. Therefore, direct visualization of corona mortis or iliopectineal fascia was not needed since the location of corona mortis is behind the pubic rami and about 33.4 mm (21.4–41 mm) away from the symphisis pubis.15
In this study, 15 cases with anterior pelvic ring injury or anterior acetabular column fracture were assigned to the minimally invasive group and 15 cases were put in standard ilioinguinal group whose surgery was performed in an earlier timeframe. In order to reduce the bias, all cases collected since the beginning of this study (March 2014) were consecutively put in the minimally invasive group.
Average duration of surgery for standard ilioinguinal approach from previous literature ranged from 175 to 275 min due to different composition of cases.4, 10, 16 Difference in surgeon’s experience and type or pattern of fractures may also affect the duration.17 In our study, duration of surgery was averaged at 235.71 ± 65.79 min in standard Ilioinguinal group which is comparable with previous studies. Average surgical time for modified Stoppa and lateral window group (149.33 ± 91.92 min) was significantly less than the standard ilioinguonal group (p = 0.0014). In our opinion, the reduction in the duration of surgery was not only associated with the time needed for exposing the second window, but also with wound closure which includes an inguinal canal repair.
Average blood loss in modified Stoppa and lateral window is significantly less than the standard Ilioinguinal group (325.33 ± 225.0 mL vs 710.67 ± 384.51 mL; p = 0.002). Previous studies recorded the blood loss with a standard ilioinguinal approach ranged from 732 to 1630 mL.17, 18, 19Blood loss in most cases is not associated with the approach but with the disruption of blood clot over the fracture site during cleaning and reduction.17, 20, 21 Decrease in the duration of surgery and the fracture pattern also affected the amount of intraoperative blood loss.
Quality of reduction, which is based on Matta reduction criteria,4is based on the amount of displacement of fracture fragments. There were no significant differences between minimally invasive and standard Ilioinguinal approach, indicating that the minimally invasive approach didn't affect the quality of reduction in this study. The advances of intraoperative imaging and the availability of indirect reduction tools had assisted the reduction and instrumentation in this study, without the need of exposing the fracture site. Similar to the previous parameter, no statistically significant differences were found between the 2 groups in both Majeed pelvic score and Hannover scoring system. Functional outcome is associated with the quality of reduction regardless of the fracture type.22
Previous studies have reported some complications related to the standard Ilioinguinal approach, such as wound breakdown due to superficial infection, femoral artery thrombosis,5 and thrombosis of epigastric inferior artery.6 There are also other potential complications such as meralgia, neurovascular injuries and asymmetric expansion of the abdomen when coughing.21 One of the limitations of our study was the small sample size and a limited follow up duration that, in our opinion, was the explanation why there was no complication found in both groups. Larger sample size and longer follow up period may reveal actual incidence of complications related to both approaches.
As mentioned earlier, in ilioinguinal approach, it is generally recommended that the plate is left in situ indefinitely, even after union is achieved, due to postoperative fibrosis that may hinder even a well-experienced surgeon in identifying the neurovascular structures.7 Despite the indications that favor implant removal are mostly relative nowadays, there are some potential indication for future implant removal such as stress riser that may resulting in peri-implant fracture or the future need for a joint replacement, although this reason is still up to debate.23 Patients request is the most common indication for plate removal due to various reasons.14, 23 In our series so far, two patients had achieved complete union and had their plate removed. Preservation of the second ilioinguinal window in the initial surgery had prevented the occurrence of postoperative fibrosis and made the implant removal less complicated and easier.
The indication for the modified Stoppa and lateral window approach is limited to the anterior pelvic ring injury, which includes superior pubic rami, anterior column of acetabulum, and some patterns of iliac wing fracture. If the posterior column of acetabulum is involved (transverse or both column), another posterior approach (eg. Kocher Langenbeck) should be combined with this modified approach.
The concept of minimal invasive plate osteosynthesis in pelvic fracture has been published in recent years. Yu24 (2013) introduced a minimal invasive plate osteosynthesis (MIPO) technique for treatment of pubic ramus fracture in 15 patients. In exposing the medial window, the ligaments and pyramidalis muscle were detached from pubic rami, which may cause hernia in long-term follow up. Zhu21 (2015) published a less invasive ilioinguinal approach for anterior ring fracture, in which the medial window is located on the transition zone of second and third (medial) window of standard ilioinguinal approach. Therefore, the fascia around iliopectineal and pectineal muscle should be separated which may also cause femoral/Cloquet’s hernia if the integrity of pectineal fascia is not restored.
Newly modified Stoppa approach described by Liu25 provided an access to both anterior and posterior column to the acetabulum by creating a procedure window between the rectus muscle and iliopsoas muscle, which is closer to the acetabulum and quadrilateral surface. Identification of the external iliac neurovascular bundle is not mandatory, however the corona mortis should be identified and ligated. Since the fracture site was exposed, the bleeding in their series ranged from 600 to 1800 mL, which is significantly higher than ours.
Yang17(2015) described a modified ilioinguinal approach to treat superior pubic rami or anterior column of acetabular fractures, which is quite similar with our series. By using medial and lateral window of standard ilioinguinal approach, blood loss and operation time can be reduced without compromising the quality of reduction. Medial window of ilioinguinal approach can also be an alternative to our modified Stoppa approach. But by minimizing the detachment of rectus abdominis insertion to the pubic symphisis as the rectus sheath is incised vertically in the modified Stoppa approach, rectus natural insertion may be preserved and the risk of iatrogenic abdominal hernia could be reduced. The proposed technical advantages of modified Stoppa and lateral window approach was easier and reproducible technique, diminished risk of abdominal hernia due to rectus insertion and inguinal ligament preservation, and minimal manipulation around neurovascular region. In our series, two patients already had their implant removed after union was achieved. Minimal soft tissue fibrosis eased the removal procedure. We also compared other minimal invasive approach and summarized them in Table 3.
Table 3.
Comparison of Minimal Invasive Plate Osteosynthesis Technique with previous publications.
| No | Author | Year | Journal | Approach | Fracture sample | Study design | NV Ident | Inguinal Canal | Rectus detached | Reduction | Complication |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Wolf26 | 2007 | Injury | Medial extraperitoneal window (vertical incision) and lateral window | Acet. | Case Series | None | Not Opened | No | Indirect | None reported |
| 2 | Hirvensalo27 | 2007 | Injury | Ilioanterior approach (similar with std. Modified Stoppa) | Both | Case Series | Corona mortis | Not Opened | No | Direct | loss of reduction |
| 3 | Farid28 | 2008 | J Orthop Trauma | Subinguinal Retroperitoneal (inferior inguinal canal) | Acet. | Case Series | Femoral vessel | Not Opened | Yes | Direct | Ext. iliac artery thrombosis |
| 4 | Jeffcoat29 | 2012 | J Orthop Trauma | Limited Ilioinguinal (Lateral two window) | Acet. | Retrospective Cohort | Femoral vessel | Partially Opened | No | Direct | Lateral femoral cutaneous palsy |
| 5 | Abo30 | 2014 | Int Orthop | Limited Ilioinguinal (Lateral one/two window) | Acet. | Historical-match-control | None | Partially Opened | No | Direct | None reported |
| 6 | Hagen31 | 2015 | J Orthop Trauma | Anterior Intrapelvic Modification of Ilioinguinal | Acet. | Technical Tips | Femoral vessel | Opened | No | Direct | None reported |
| 7 | Zhu21 | 2015 | BMC Musculoskelet Disord | Less Invasive ilioinguinal | Both + Sacrum | Case Series | None | Not Opened | Yes | Indirect | None reported |
| 8 | Yang17 | 2015 | Medicine | Modified Ilioinguinal (medial & lateral window) | Both | Retrospective Cohort | None | Partially Opened | Yes | Indirect | Fat liquefaction (1 case) |
| 9 | Liu25 | 2015 | Int Orthop | Newly modified Stoppa (medial − plane between rectus & iliopsoas) | Acet. | Case Series | Corona mortis | Partially Opened | No | Direct | None reported |
| 10 | Zhuang32 | 2017 | Int Orthop | Single Ilioinguinal approach (middle window) | Acet. | Case Series | Femoral vessel | Opened | No | Direct | Lateral femoral cutaneous palsy |
| 11 | Our Proposed Method | Newly Modified Stoppa and Lateral Window | Both | Prospective and Retrospective Cohort | None | Not Opened | No | Indirect | None Found | ||
There are some limitations in our study. First, as mentioned before, a small sample size and limited duration of follow up may mask the incidence of complications related to both approach. Second, the patient selection was based on a cut-off time (March 2014) where all patients presenting from that month were consecutively included in the modified Stoppa and lateral window group. Although only one surgeon performed all the surgeries, there is some debate about the learning curve whether the decreased blood loss and duration of surgery on the minimal invasive group was affected.
5. Conclusions
Modified Stoppa and lateral window technique can be used as a safe and effective alternative approach for anterior pelvic ring fracture and/or anterior column acetabulum fracture. This approach decreases the duration of surgery and blood loss without compromising the quality of reduction and functional outcome in patients.
Conflicts of interest
None.
Author contributions
All authors contributed in proposal preparation, data collection and analysis, and final manuscript preparation.
Acknowledgement
All authors don't have any financial or personal relationships with other people or organizations that could inappropriately influence our work. There are no other relationship/conditions/circumstances that present a potential conflict of interest.
This research is funded by our institution (Ciptomangunkusumo General Hospital) in their annual grant (2015).
Contributor Information
Hadisoebroto Dilogo Ismail, Email: ismailorthofkui@yahoo.co.id.
Yoshi Pratama Djaja, Email: oshipratamadjaja@yahoo.com.
Jessica Fiolin, Email: Jessica_fiolin@yahoo.co.uk.
References
- 1.Letournel E. Les fractures du cotyle. Etude d’une serie de 75 cas. J Chir. 1961;82:47–87. [PubMed] [Google Scholar]
- 2.Letournel E. The treatment of acetabular fractures through the Ilioinguinal approach. Clin Orthop. 1993;292:62–76. [PubMed] [Google Scholar]
- 3.Hoppenfeld S., deBoer P., Buckley R. 4th Edition. Lippincolt-Williams-Wilkins; Philadelphia: 2009. Surgical Exposures in Orthopaedics: The Anatomic Approach. [Google Scholar]
- 4.Matta J.M. Operative treatment of acetabular fractures through the Ilioinguinal approach. A 10-year perspective. Clin Orthop. 1994;305:10–19. [PubMed] [Google Scholar]
- 5.Gaheer R.S., Rysavy M., Al Khayarin M.M., Kumar K. Femoral artery intimal injury following open reduction of an acetabular fracture. Orthopedics. 2009;32(March (3)):212. [PubMed] [Google Scholar]
- 6.Heppert V., Holz F., Winkler H., Wentzensen A. [Necrosis of the rectus abdominis muscle: complication after ilioinguinal approach] Unfallchirurg. 1995;98(February (2)):98–101. [PubMed] [Google Scholar]
- 7.Mayo K., Oransky M., Rommens P., Sancieto C. 2007. Acetabulum – Anterior Wall Ilioinguinal Approach. AO Surgery reference. [ONLINE] Available at: https://www2.aofoundation.org/. [Accessed 27 August 2016] [Google Scholar]
- 8.Archdeacon M.T., Kazemi N., Guy P., Sagi H.C. The modified Stoppa approach for acetabular fracture. J Am Acad Orthop Surg. 2011;19(March (3)):170–175. doi: 10.5435/00124635-201103000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Cole J.D., Bolhofner B.R. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994;305(August):112–123. [PubMed] [Google Scholar]
- 10.Sagi C.H., Afsari A., Dziadosz D. The anterior intra-pelvic (modified rives-Stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010;24(5):263–270. doi: 10.1097/BOT.0b013e3181dd0b84. [DOI] [PubMed] [Google Scholar]
- 11.Matta J.M., Tornetta P., III Internal fixation of unstable pelvic ring injuries. Clin Orthop Relat Res. 1996;329:129–140. doi: 10.1097/00003086-199608000-00016. [DOI] [PubMed] [Google Scholar]
- 12.Majeed S.A. External fixation of the injured pelvis. The functional outcome. J Bone Joint Surg Br. 1990;72:612–614. doi: 10.1302/0301-620X.72B4.2380212. [DOI] [PubMed] [Google Scholar]
- 13.Grotz M.R., Allami M.K., Harwood P., Pape H.C., Krettek C., Giannoudis P.V. Open pelvic fractures: epidemiology, current concepts of management and outcome. Injury. 2005;36(1):1–13. doi: 10.1016/j.injury.2004.05.029. [DOI] [PubMed] [Google Scholar]
- 14.Khoury A., Weill Y., Mosheiff R. The Stoppa approach for acetabular fracture. Oper Orthop Traumatol. 2012;24(September (4–5)):439–448. doi: 10.1007/s00064-011-0093-z. [DOI] [PubMed] [Google Scholar]
- 15.Karakurt L., Karaca I., Yilmaz E. Corona mortis: incidence and location. Arch Orthop Trauma Surg. 2002;122:163–164. doi: 10.1007/s004020100341. [DOI] [PubMed] [Google Scholar]
- 16.Ochs B.G., Marintschev I., Hoyer H., Rolauffs B., Culemann U., Pohlemann T. Changes in the treatment of acetabular fractures over 15 years: analysis of 1266 cases treated by the German Pelvic Multicentre Study Group (DAO/DGU) Injury. 2010;41(August (8)):839–851. doi: 10.1016/j.injury.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 17.Yang Y., Li Q., Cui H. Modified ilioinguinal approach to treat pelvic or acetabular fractures: a retrospective study. Medicine (Baltimore) 2015;94(Septenber (37)):e1491. doi: 10.1097/MD.0000000000001491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mayo K. Open reduction and internal fixation of fractures of the acetabulum. Clin Orthop Relat Res. 1994;305:31–37. [PubMed] [Google Scholar]
- 19.Matta J.M. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks of the injury. J Bone Joint Surg Am. 1996;78:1632–1645. [PubMed] [Google Scholar]
- 20.Ruchholtz S., Buecking B., Delschen A. The two-incision, minimally invasive approach in the treatment of acetabular fractures. J Orthop Trauma. 2013;27:248–255. doi: 10.1097/BOT.0b013e3182690ccd. [DOI] [PubMed] [Google Scholar]
- 21.Zhu L., Wang L., Shen D., Ye T.W., Zhao L.Y., Chen A. Treatment of pelvic fractures through a less invasive ilioinguinal approach combined with a minimally invasive posterior approach. BMC Musculoskelet Disord. 2015;16:167. doi: 10.1186/s12891-015-0635-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mardanpour K., Rahbar M. The outcome of surgically treated traumatic unstable pelvic fractures by open reduction and internal fixation. J Inj Violence Res. 2013;5(June (2)):77–83. doi: 10.5249/jivr.v5i2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vos D.I., Verhofstad M.H. Indications for implant removal after fracture healing: a review of the literature. Eur J Trauma Emerg Surg. 2013;39(August (4)):327–337. doi: 10.1007/s00068-013-0283-5. [DOI] [PubMed] [Google Scholar]
- 24.Yu X., Tang M., Zhou Z., Peng X., Wu T., Sun Y. Minimally invasive treatment for pubic ramus fractures combined with a sacroiliac joint complex injury. Int Orthop. 2013;37(August (8)):1547–1554. doi: 10.1007/s00264-013-1954-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu Y., Yang H., Li X., Yang S.H., Lin J.H. Newly modified Stoppa approach for acetabular fractures. Int Orthop. 2013;37(July (7)):1347–1353. doi: 10.1007/s00264-013-1920-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wolf H., Wieland T., Pajenda G., Vecsei V., Mousavi M. Minimally invasive ilioinguinal approach to the acetabulum. Injury. 2007;38(10):1170–1176. doi: 10.1016/j.injury.2006.06.116. [DOI] [PubMed] [Google Scholar]
- 27.Hirvensalo E., Lindahl J., Kiljunen V. Modified and new approaches for pelvic and acetabular surgery. Injury. 2007;38(4):431–441. doi: 10.1016/j.injury.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 28.Farid Y.R. The subinguinal retroperitoneal approach for fractures of the acetabulum: a modified ilioinguinal approach. J Orthop Trauma. 2008;22(4):270–275. doi: 10.1097/BOT.0b013e3181673198. [DOI] [PubMed] [Google Scholar]
- 29.Jeffcoat D.M., Carroll E.A., Huber F.G. Operative treatment of acetabular fractures in an older population through a limited ilioinguinal approach. J Orthop Trauma. 2012;26(5):284–289. doi: 10.1097/BOT.0b013e31821e10a2. [DOI] [PubMed] [Google Scholar]
- 30.Abo-Elsoud M., Radwan Y.A., Gobba M., Sadek F. Short-segment fixation through a limited ilioinguinal approach for treating anterior acetabular fractures: a historical-control study. Int Orthop. 2014;38(7):1469–1475. doi: 10.1007/s00264-014-2354-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hagen J.E., Weatherford B.M., Nascone J.W., Sciadini M.F. Anterior intrapelvic modification to the ilioinguinal approach. J Orthop Trauma. 2015;29(Suppl. 2):S10–3. doi: 10.1097/BOT.0000000000000266. [DOI] [PubMed] [Google Scholar]
- 32.Zhuang Y., Zhang K., Wang H. A short buttress plate fixation of posterior column through single ilioinguinal approach for complex acetabular fractures. Int Orthop. 2017;41(1):165–171. doi: 10.1007/s00264-016-3225-0. [DOI] [PubMed] [Google Scholar]