Abstract
Background
To date, research on music for pain management has focused primarily on listening to pre-recorded music for acute pain. Research is needed on the impact of active music therapy interventions on chronic pain management.
Objective
The aim of this mixed methods research study was to determine feasibility and estimates of effect of vocal music therapy for chronic pain management.
Methods
Fifty-five inner city adults, predominantly African-Americans, with chronic pain were randomized to an 8-week vocal music therapy treatment group or waitlist control group. Consent and attrition rates, treatment compliance, and instrument appropriateness/burden were tracked. Physical functioning (pain interference and general activities), self-efficacy, emotional functioning, pain intensity, pain coping, and participant perception of change were measured at baseline, 4, 8, and 12 weeks. Focus groups were conducted at the 12-week follow-up.
Results
The consent rate was 77%. The attrition rate was 27% at follow-up. We established acceptability of the intervention. Large effect sizes were obtained for self-efficacy at weeks 8 and 12; a moderate effect size was found for pain interference at week 8; no improvements were found for general activities and emotional functioning. Moderate effect sizes were obtained for pain intensity and small effect sizes for coping, albeit not statistically significant. Qualitative findings suggested that the treatment resulted in enhanced self-management, motivation, empowerment, a sense of belonging, and reduced isolation.
Conclusions
This study suggests that vocal music therapy may be effective in building essential stepping stones for effective chronic pain management namely enhanced self-efficacy, motivation, empowerment, and social engagement.
Keywords: Chronic pain, music therapy, African Americans, mixed methods research
Introduction
Chronic pain affects approximately 43% of the United States (U.S.) population. It is the leading cause of disability in the U.S. and carries an estimated healthcare expense of over half a trillion dollars annually (Institute of Medicine, 2011). Billions of dollars are spent annually on traditional pain treatments such as opioids, non-steroidal anti-inflammatory agents, spine surgeries, and epidural injections, yet numerous meta-analyses have indicated that such treatments bring relief to only a small percentage of people and may even decrease a person’s quality of life because of side effects, addiction, and complications (Chou & Huffman, n.d.). Moreover, there has been an alarming increase in prescription opioids deaths in the U.S (Buckenmaier & Schoomaker, 2014). Between 1999 and 2008 there has been a threefold increase in deaths from drug overdose, with opioid prescription drugs (e.g., oxycodone and hydrocone) accounting for more overdose deaths than heroin and cocaine combined. This devastating fact coincides with a 300% surge in prescription pain medication from 1999 to 2008 (Centers for Disease Control and Prevention, 2011). Buckenmaier and Schoomaker (2014) have called for an urgent shift from an overreliance on “19th century opioid-based pain management” to therapies that treat people with chronic pain from a biopsychosocial perspective (Buckenmaier & Schoomaker, 2014, p. S8).
People with chronic pain, often after being disillusioned by traditional interventions, are increasingly seeking complementary pain treatments (Barnes, Bloom & Nahin, 2008). The use of music as a non-pharmacological pain treatment has received increasing attention during the past two decades. However, research on the use of music has focused primarily on ‘passive’ listening to pre-recorded music for acute pain management (Cepeda, Carr, Lau, & Alvarez, 2006). A Cochrane review of 51 studies found that listening to music reduced pain intensity levels and opioid requirements, but the magnitude of these benefits was small (Cepeda et al., 2006). While it is true that listening to music can function as a distractor or a relaxing agent, our clinical experience suggests that people’s active engagement in music therapy enlists added components of effective management of chronic pain.
We developed an 8-week vocal music therapy (VMT) treatment program that uses toning (i.e., singing of elongated vowels), deep breathing, group singing, vocal improvisations, as well as verbal processing of emotions and thoughts evoked by the music experiences. The intervention is guided by a biopsychosocial framework to chronic pain management. On a bioneurological level, music has been shown to activate opioid-rich midbrain nuclei that regulate descending inhibition of pain and influence activity in the medial prefrontal cortex and limbic/paralimbic brain structures involved in affective and cognitive modulation of pain (Brown, Martinez, & Parson, 2004; Koelsch, 2010). On a psychological level, participants are encouraged to reconnect with their body in a positive manner through toning and deep breathing. People with chronic pain often use body dissociation as a way to cope with physical pain. The negative impact of body dissociation on the well-being in people with chronic pain is well documented in the literature (Price & Thompson, 2007), making enhanced body awareness an important treatment target. As toning produces vibrations that are felt in our bodies, targeted toning aims to facilitate somatic awareness and address chronic patterns of tension. These embodied experiences help to develop a more caring and accepting attitude towards one’s body (Bullington, Nordemar, Nordemar, & Sjöström-Flanagan, 2003). Acceptance has been found to play an important role in adjustment to chronic pain (Kranz, Bollinger, & Nilges, 2010). Furthermore, singing songs that have a special meaning to the participants as well as vocal improvisations facilitate access to repressed emotions and create opportunities for expression, an important pathway to enhanced well-being and self-reliance (Keefe, Lumley, Anderson, Lunch, & Carson, 2001). Socially, the act of creating music together through vocal improvisations promotes a sense of belonging and social inclusion (Livesey, Morrison, Clift, & Camic, 2012). This is an important mechanism in chronic pain treatment as many people with chronic pain feel isolated and disconnected from the world (Bullington, 2009). Evolutionary theorists emphasize that a central function of music is to mobilize social cohesion (Boer & Abubakar, 2014). The act of making music with others also provides a strong sense of support and activates social engagement (Chanda & Levitin, 2013). This is evidenced by the use of songs by civil rights activists to unite gathering and inspire action (Sanger, 1997). Furthermore, singing inspirational songs in groups offers opportunities for collaboratively identifying sources of strength and motivation.
Our clinical experience indicates that VMT is particularly attractive to African-Americans for whom community music making is an integral part of their culture and an important source of strength, bonding, and celebration (Reagon, 1992). To date, research studies on psychological and complementary therapies for chronic pain management have suffered from under-representation of minority populations. Yet, data from large national health surveys indicate that African-Americans and Hispanics report higher pain intensity and pain-related disability than non-Hispanic Whites (Bolen et al., 2010). In addition, minority patients are less likely to go to treatment, less responsive to interventions, and leave treatment early (Hooten et al., 2012). Reasons for this include lack of cultural relevance of the interventions and mistrust of the medical community (Fisher, Burnet, Huang, Chin, & Cagney, 2007). Consequently, scholars have advocated for cultural leverage to be used as a framework for designing culturally appropriate treatment strategies, meaning that patients’ cultural practices and beliefs should form the bases for the development of interventions (Fisher et al., 2007). VMT asks patients to become active participants in creating the music. Interestingly, active music making maps onto several of the healing mechanisms hypothesized to be active in many African American Churches (McRae, Thompson, & Cooper, 1999): group singing to give voice to the suffering, singing to express joy, use of inspirational music, and active music making to build social supports. Furthermore, community music making is an important source of strength and inspiration for African- Americans as it has played a crucial role in their dealing with oppression and suffering throughout history (Maultsby, 2000). In this regard, VMT not only promotes skills that can contribute to chronic pain management, but uses strategies that may be particularly meaningful and relevant for African Americans.
The purpose of this mixed methods study was to: 1) determine the feasibility of the VMT treatment and research protocol with inner city African-Americans with chronic pain; 2) provide estimates of effect for core outcomes in chronic pain management; and 3) obtain qualitative data about feasibility and treatment benefits. Specifically, the following research questions were addressed through quantitative and qualitative data collection:
Feasibility: (a) What is the consent rate? (b) What is the attrition rate and what are the reasons for dropout? (c) What is the treatment compliance rate and what are the reasons for non-compliance? (d) Are the measurement tools appropriate for the targeted population? and (e) What suggestions do participants have for treatment improvement?
Treatment effect: (a) What are the estimates of treatment effect of an 8-week vocal music therapy treatment program on physical functioning, self-efficacy, pain intensity, pain coping, emotional functioning and patient perception of change in people with chronic pain, as measured by standardized outcome measures? (b) What treatment benefits/harms do participants describe in their own words? and (c) What are participants’ explanations for potentially discrepant quantitative results?
Methods
Design
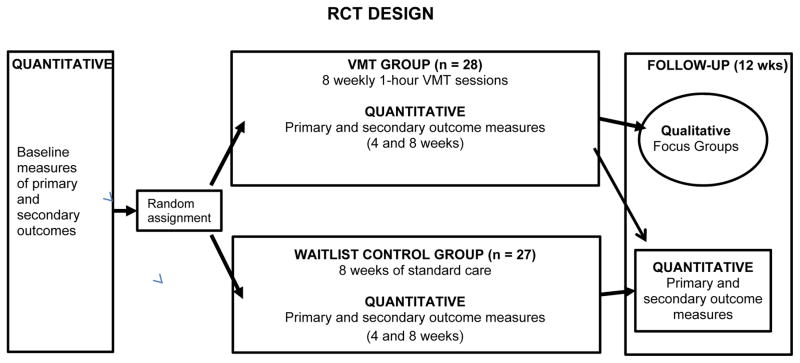
We employed a mixed methods intervention design (Creswell, 2015), in which qualitative data (i.e., focus groups) were embedded within a randomized controlled trial (RCT) (Figure 1). A list of random numbers was used for allocation to the VMT or wait-list control (WLC) group. The use of sequentially numbered, opaque, sealed envelopes ensured allocation concealment.
Figure 1.
Study Design
(Adapted from Plano Clark V. L., et al. (2013). Practices and tensions from embedding an interpretive qualitative approach within an RCT. Journal of Mixed Methods Research, 7(3), 219–242)
Study Participants
People with chronic pain were recruited from a nurse-managed health center that serves about 5,000 inner city adults, predominantly African-Americans. To be eligible, participants had to be 18 years of age or older and have a diagnosis of chronic benign pain (≥ 6 months). The exclusion criteria included: 1) having a mental health diagnosis that might prevent productive participation in group sessions, cognitive impairment, progressive neurological disorder, or moderate to profound hearing impairment; 2) being pregnant; or 3) being compensated or having any impending litigation for chronic pain related problems. We used self-report for eligibility screening. Because this was a feasibility study, no a priori sample size was computed. Instead, we aimed for a total sample size of 40 completed patients to enable examination of data trends. The study took place between September 1, 2012 and April 1, 2014 and was approved by an Institutional Review Board. Informed consent was obtained from all study participants.
Vocal Music Therapy Intervention
The VMT treatment program consisted of eight 60-minute weekly group therapy sessions (6–8 participants each group) administered by the lead investigator, a board-certified music therapist with expertise in chronic pain management. As this was a feasibility study, it was considered appropriate to have the lead investigator be the interventionist. This would allow for further refinement of the preliminary treatment manual that was developed for this study. Each session, as outlined in the treatment manual, followed the same basic structure and contained various essential treatment components. The therapist adhered to the treatment manual throughout the study period, however, formal evaluations of therapist treatment adherence were not conducted.
The VMT sessions consisted of the following essential components. First, music-guided deep breathing was used at the start of the session to allow participants to transition from prior activities and to help bring their focus to their body. After a brief verbal check-in, participants engaged in toning and humming experiences aimed at enhancing body awareness, releasing bodily tensions, and developing a caring attitude towards one’s body. This was followed by verbal processing of somatic experiences evoked by the toning exercises. Next, participants engaged in vocal improvisations. Vocal improvisations were initiated by the therapist or by the participants. For example, the music therapist could offer a brief vocal melodic phrase for the group to sing in a repetitive manner. The group was then encouraged to add harmonies and add additional vocal phrases. Percussion instruments or body percussion were typically added to provide rhythmic drive and energy. The music therapist also used circle songs for the vocal improvisation segment of the sessions. Singer songwriter Bobby McFerran used circle songs in his performances by engaging the audience in call-and-response type of interactions while creating various layers of vocal phrases, harmonies, and body percussion rhythms. In a similar fashion, the music therapist and the group members created layered group improvisations. These vocal improvisations resulted in energetic music making. At the same time, they provided opportunities for emotional expression and relating to others in creative and meaningful ways. The vocal improvisations typically evoked discussions about personal struggles and newly gained insights. Such discussions, at times, evolved in spontaneous call-and-response singing to affirm the main ideas of the group discussion.
Each session ended with singing an inspirational song selected by one of the group members. Songs can help validate and express feelings or thoughts that might be difficult to express (Clements-Cortés, 2004). As such, songs provided comfort, gave hope and encouragement.
All music making was recorded by the therapist during each session. In our clinic, we use Garageband with a high quality snowball microphone for recording of the live music. Every other week, the therapist created a new CD for the participants with music used during the music-guided deep breathing, vocal improvisations, songs learned in the sessions, and one or more of the inspirational songs selected by the participants. These songs were purchased at iTunes and copyright laws were observed. Each week, participants were offered instructions for how to use toning, humming and singing at home to help manage their pain. The CDs helped the VMT participants to recreate the session experiences at home, sing along with the CD, and experience the energy and joy created by the vocal improvisations.
Waitlist Control Group
Participants in the WLC group received care as usual at the health center. After completion of the follow-up measures (week 12), they participated in the 8-week VMT treatment program.
Outcome Measures
To determine feasibility, we tracked: a) consent rate; b) attrition rate; c) treatment compliance and acceptance; and d) appropriateness of the measurement tools. At the start of the study, participants filled out a participant information questionnaire with questions about demographics, clinical characteristics, their music background, and music preferences. Participants were also asked to rate their treatment expectancy on a 0–10 numeric rating scale (NRS).
We based our selection of outcome measures on recommendations for chronic pain trials as set forth by the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) (Dworkin et al., 2005). In people with chronic pain, pain intensity can often only be minimally reduced. Therefore, outcome success of a pain management program is typically evaluated by improvements in physical functioning and pain interference (Dworkin et al., 2005).
Physical functioning was measured by the Interference Scale (9 items) and General Activities Scale (18 items) of the Westhaven-Yale Multidimensional Pain Inventory (MPI) (Kerns et al., 1985). The Interference Scale asks participants to rate how much their pain is interfering with completing a given task (e.g. ability to work) and how much pain has changed their enjoyment of certain things (e.g. participating in social/recreational activities). The General Activities Scale asks participants to rate how often they engage in certain activities (e.g. visit relatives, prepare a meal). The MPI is a reliable and valid measure and has been studied with diverse chronic pain conditions (Dworkin et al., 2005). Researchers can use the complete inventory or opt to use select subscales (Kerns et al., 1985).
Self-efficacy was measured by the Pain Self-Efficacy Questionnaire (PSEQ) (Nicholas, 2007), a 10-item questionnaire which measures beliefs about one’s ability to accomplish certain tasks despite the pain. The total score ranges from 0 to 60, with higher scores reflecting greater self-efficacy. The PSEQ has been found to be responsive to detecting clinically important change in patients with chronic pain (Maughan & Lewis, 2010).
Participants rated their average pain intensity as well as average pain coping during the past week using an 11-point (0–10) numeric rating scale, as per IMMPACT recommendations (Dworking et al., 2005). In addition, VMT participants rated their present pain intensity before and after each VMT session.
Emotional functioning was assessed using the Hospital Anxiety and Depression Scale (HADS) (Zigmond & Snaith, 1983). The HADS contains two scales: an anxiety scale (7 items) and a depression scale (7 items). The scores for each scale ranges from 0 to 21. Its validity, reliability and responsiveness to change have been established (Zigmond & Snaith, 1983).
Finally, participants rated their perception of improvement using the Patient Global Impression of Change Scale (PGIC) (Guy, 1976). The PGIC consists of a single-item rating by participants of their improvement with treatment on a 7-point scale. PGIC data “provide a responsive and readily interpretable measure of participants’ assessments of the clinical importance of their improvement or worsening over the course of a clinical trial” (Dworkin et al., 2005, p.15).
It took participants 15–20 minutes to complete all assessments. Measurements were administered by an outcome assessor at baseline, 4, 8, and 12 weeks (follow-up). Outcome assessor blinding was frequently broken as participants talked to each other about their experiences during outcome assessment sessions.
Exit Focus Groups
At week 12, all participants were invited to partake in a 60–90 minute focus group administered by an independent focus group moderator. The focus group was aimed at exploring: 1) participants’ perception of treatment benefits/harms; 2) reasons for non-compliance; 3) instrument appropriateness; and 4) suggestions for treatment improvement. At the end of the focus group, additional questions were asked to help explain quantitative findings that seemed puzzling to the research team (e.g. improvement on the Interference Scale but little to no improvement on the General Activities Scale). In line with the mixed methods explanatory intent of this part the focus group, questions were formulated after the research team had reviewed the quantitative results.
Data Analysis
In line with our study aims, we used descriptive statistics to identify trends in the quantitative outcome data. Because of small sample sizes, feasibility, pilot and exploratory studies do not have the required statistical power to warrant hypothesis testing; the use of hypothesis testing in underpowered studies often results in failure to detect statistical significance for between-group differences on a given outcome, where, in reality, a true difference exists between the two groups. Therefore, it is recommended that, for these types of studies, effect sizes and associated confidence intervals are reported to communicate the size and the direction of the treatment effect (Lee, 2014; McGough & Faraone, 2009). We reported means, standard deviations (SD), effect sizes (i.e., standardized mean difference [SMD] also known as Cohen’s d) and associated 95% confidence intervals (CI). We used the guidelines by Cohen (1988) to interpret the magnitude of the effect sizes, namely small (0.2), moderate (0.5), and large (0.8). Besides magnitude of the treatment effect, the effect size also communicates the direction of the treatment effect. Conventionally, a positive value indicates that the intervention resulted in greater improvements than the control group; a negative value suggest that treatment group fared worse than the control group. In addition, the 95% CI provides information about the range of the treatment effect. Moreover, a CI that does not include a zero value (e.g. 95% CI 0.3 to 1.1) suggests that the treatment effect is statistically significant (McGough & Faraone, 2009). To compare sample baseline characteristics, we used Chi-Square or Fisher’s Exact test for categorical variables and a pooled two-sided t-test or Wilcoxon two-sample test for continuous variables.
The transcripts of the interviews were imported into MAXQDA 11 (MAXQDA, 1989–2014) and analyzed by two coders (JB, MN) using theoretical thematic analysis procedures (Braun & Clarke, 2006). Such analysis is aimed at identifying patterns driven by an a priori theoretical framework or research questions. We identified themes using a semantic approach in which themes are derived from “the explicit meaning of the data and the analyst is not looking for anything beyond what a participant has said” (Braun & Clarke, 2006, p. 84). The initial coding was guided by questions related to treatment benefit and harm: (a) What do participants report as VMT treatment benefits during and outside of the VMT session?; (b) What do participants report as harm or negative effects of treatment?; and (c) What specific aspects of the treatment were the most useful/beneficial to them?. After completion of this analysis, the transcripts were revisited to answer questions related to the treatment protocol as well as the measurement protocol. Coding was now guided by the following questions: (a) What recommendations do participants have for improvement of the treatment program?, (b) what were reasons for non-compliance with the treatment protocol, and (c) what did participants report related to the appropriateness of the measurement tools and potential measurement burden? Finally, the transcripts were coded for participants’ explanations of quantitative findings. We then compared the quantitative and qualitative data analyses to: 1) examine (dis)congruence of findings; 2) identify treatment benefits not measured by the standardized measures; and 3) enhance understanding of the quantitative outcomes.
Results
Participants
Table 1 summarizes participants’ socio-demographic and clinical characteristics at baseline. Eighty-nine percent of the participants were African American. No significant differences in demographic or clinical characteristics were found between the groups.
Table 1.
Socio-Demographic and Clinical Characteristics of Study Participants at Baseline (N = 55)
| Characteristic | Vocal music therapy (n = 28) | Waitlist control n = 27) | p-value |
|---|---|---|---|
| Age (years), mean (SD) | 54.5 (13) | 53 (12.8) | 0.66a |
| Gender, female | 23 (82.1%) | 26 (96.3%) | 0.19b |
| Ethnicity | 0.49b | ||
| Black | 24 (85.7%) | 25 (92.6%) | |
| Caucasian | 1 (3.6%) | 2 (7.4%) | |
| Other | 3 (10.7%) | 0 (0%) | |
| Employment | 0.22b | ||
| Employed | 6 (21.4%) | 2 (7.4%) | |
| Unemployed or on disability | 15 (53.5%) | 17 (63%) | |
| Retired | 7 (25%) | 8 (29.6%) | |
| Duration of pain (years), mean (SD) | 6.3 (5.4) | 6.7 (6.6) | 0.94c |
| Pain type | 0.27b | ||
| Back pain | 10 (35.7%) | 9 (33.3%) | |
| Arthritis | 7 (25%) | 8 (29.6%) | |
| Other musculoskeletal | 5 (17.9%) | 5 (18.6%) | |
| Neuropathic | 6 (21.4%) | 2 (7.4%) | |
| Other | 0 (0%) | 3 (11.1%) | |
| Medicine use for pain | 0.82d | ||
| Prescription medicine | 17 (60.7%) | 15 (57.7%) | |
| Over-the-counter medicine | 16 (57.1%) | 14 (53.9%) | |
| Treatment expectancy (NRSe), mean (SD) | 6.7 (1.9) | 6.0 (1.8) | 0.17a |
| Prior music performance experience | 18 (64.3%) | 13 (48.2%) |
Pooled two-sided t-test;
Fisher’s Exact Test;
Wilcoxon two-sample test;
Chi-Square Test;
NRS: 0–10 Numeric Rating Scale
Feasibility Results
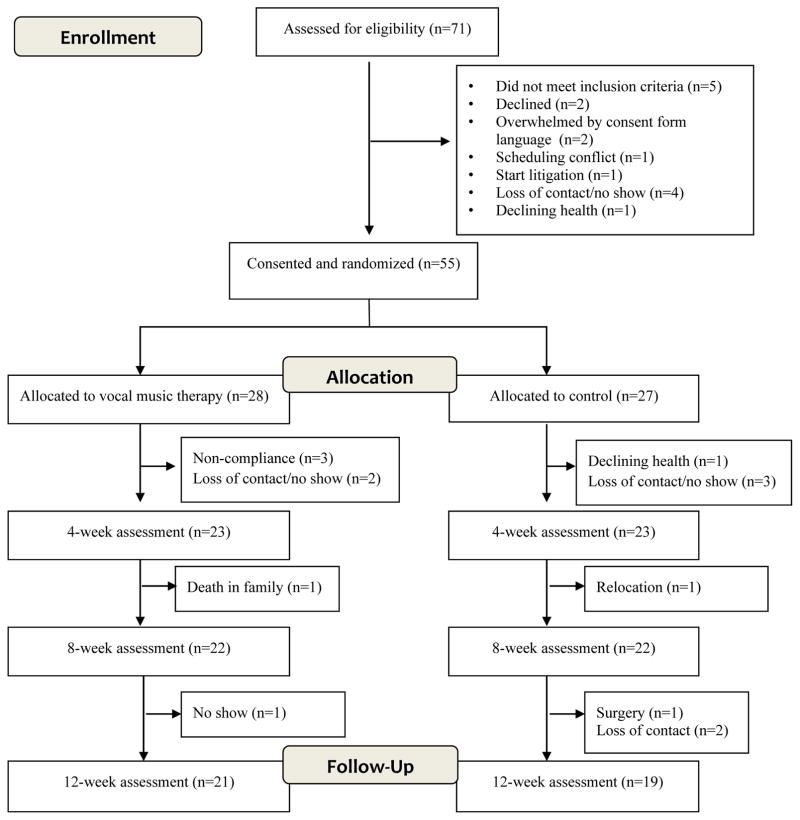
A total of 71 patients were referred to the study. Fifty-five individuals provided consent and were randomized to the either the VMT or WLC group resulting in a consent rate of 77%. In the VMT group, the largest attrition happened before the first VMT session. Measurement completion rates at follow up were 75% and 70% for the VMT and WLC groups, respectively. Failure to attend a session were mainly due to childcare issues, transportation issues, bad weather, and health issues.
Figure 2 details reasons for study participant drop-out. Of the 22 participants in the VMT treatment arm who completed the 8-week program, 19 (86%) attended 7 to 8 sessions, and three (14%) attended 4 to 5 sessions, suggesting that the treatment was well accepted. The main reasons for not attending sessions were: 1) transportation issues, 2) weather, 3) doctor appointments, and 4) family emergencies. Participants’ main recommendation for program improvement was an increase of program duration and session length.
Figure 2.
Participant Flow Chart
Participants’ focus group responses suggested that they did not feel burdened by the frequency of administration of the questionnaires. However, many expressed disappointment with the content of the questionnaires. They felt that many questions (e.g., MPI General Activities scale) were not relevant to what they personally gained from the VMT program. Participants wished that we would have inquired about the positive things they experienced in the sessions. One participant shared: “It wasn’t asking us anything we experienced going through the time that we spent as a group and the music and what it brought to us, and what we felt when it came out of us.” Finally, several participants expressed suspicion about the HADS wondering whether the researchers were “trying to find out if we are crazy.”
During the focus group participants were encouraged to provide feedback about the VMT program and offer suggestions for improvement. Participants expressed great satisfaction with the program. One participant recommended that more movement be integrated with the singing and improvisations. Many participants suggested that the treatment program should be at least 12 weeks long and that the session length should be increased to 90 minutes.
Treatment Benefits: Quantitative Results
Table 2 details the means and SDs for each group as well as the SMD and 95% CI at weeks 8 and 12. There was a moderate treatment effect of VMT on pain interference at the end of the treatment program (SMD = 0.6, 95% CI 0.01 to 1.22); however, by week 12, this effect had decreased to 0.23 (95% CI −0.39 to 0.86). VMT had a large effect on self-efficacy at week 8 (SMD = 1.09, 95% CI 0.45 to 1.73) and at follow-up (SMD = 0.77, 95% CI 0.13 to 1.42). VMT did not result in improvements in general activities or emotional functioning. Baseline levels for anxiety and depression were within the normal to mild range making it less likely for improvement to occur.
Table 2.
Means and Standardized Mean Differences at Baseline, Week 8 and Follow-Up
| Vocal Music therapy | Waitlist Control | ||||
|---|---|---|---|---|---|
|
|
|||||
| Outcomes | Mean, SD | Change score, SDa | Mean, SD | Change score, SD | SMD (95% CI)b |
| Pain interference (MPI)c | |||||
| Baseline d | 4.6 (1.3) | 4.3 (1.4) | |||
| Week 8 | 3.6 (1.6) | −1.0 (1.46) | 4.1 (1.4) | −0.2 (1.07) | 0.6 (0.01, 1.22) |
| Follow-up | 3.9 (1.2) | −0.7 (1.59) | 3.9 (1.6) | −0.4 (0.72) | 0.23 (−0.39, 0.86) |
| General activity (MPI) | |||||
| Baseline | 2.9 (1.1) | 3.3 (1.2) | |||
| Week 8 | 3.0 (1.2) | 0.1 (0.94) | 3.0 (1.2) | −0.3 (0.83) | 0.01 (−0.59, 0.6) |
| Follow-up | 2.9 (1.1) | 0 (1.26) | 2.9 (1.2) | −0.4 (1.38) | 0.3 (−0.33, 0.92) |
| Pain self-efficacy (PSEQ) | |||||
| Baseline | 28.6 (15.0) | 34.2 (13.6) | |||
| Week 8 | 32.5 (15.2) | 3.9 (10.69) | 27.7 (12.7) | −6.5 (7.82) | 1.09 (0.45, 1.73) |
| Follow-up | 32.5 (15.6) | 3.9 (10.64) | 30.4 (14.5) | −3.8 (8.75) | 0.77 (0.13, 1.42) |
| Anxiety (HADS) | |||||
| Baseline | 9.9 (5.3) | 9.3 (4.6) | |||
| Week 8 | 9.0 (4.8) | −0.9 (3.03) | 9.7 (5.2) | 0.4 (2.56) | 0.46 (−0.14, 1.05) |
| Follow-up | 10.4 (5.0) | 0.5 (2.35) | 8.8 (5.1) | −0.5 (2.73) | −0.39 (−1.01, 0.24) |
| Depression (HADS) | |||||
| Baseline | 7.3 (3.6) | 7.2 (3.7) | |||
| Week 8 | 7.1 (3.1) | −0.2 (2.64) | 8.0 (3.4) | 0.8 (2.37) | 0.39 (−0.21, 0.99) |
| Follow-up | 7.6 (3.7) | 0.3 (2.84) | 6.8 (4.0) | −0.4 (3.37) | −0.22 (−0.84, 0.40) |
| Average pain (NRS) | |||||
| Baseline | 8.3 (1.4) | 8.0 (1.8) | |||
| Week 8 | 6.8 (2.1) | −1.5 (1.94) | 7.6 (1.8) | −0.4 (1.68) | 0.6 (−0.01, 1.2) |
| Follow-up | 6.2 (2.7) | −2.1 (2.7) | 6.6 (2.9) | −1.4 (2.49) | 0.26 (−0.36, 0.89) |
| Average coping (NRS) | |||||
| Baseline | 5.0 (2.7) | 5.6 (2.7) | |||
| Week 8 | 5.5 (3.0) | 0.5 (2.82) | 6.1 (2.5) | 0.5 (3.19) | 0 (−0.50, 0.59) |
| Follow-up | 6.3 (2.7) | 1.3 (3.81) | 6.0 (2.9) | 0.4 (2.86) | 0.26 (−0.36, 0.88) |
Change scores are from baseline to week 8 and from baseline to follow-up
SMD (95% CI): the standardized mean difference was computed using the change score and the SD of the change score; 95% CI intervals that do not include the value zero suggest that the findings are statistically significant.
MPI = Westhaven-Yale Multidimensional Pain Inventory: range from 0 to 6 with higher scores representing greater pain interference; PSEQ = Pain Self-Efficacy Questionnaire: range from 0 – 60 with higher scores representing greater self-efficacy; HADS = Hospital Anxiety and Depression Scale: range from 0 – 21 with higher scores representing higher anxiety or higher depression
n at baseline: 28 for VMT, 27 for WLC; n at week 8: 22 for both groups, n at follow-up: 21 for VMT, 19 for WLC
As for pain, both VMT and WLC groups reported decreases in average weekly pain but pain reductions were greater in the VMT group than the control group at the end of treatment (SMD = 0.6, 95% CI −0.01 to 1.2). This difference between the group was smaller at follow-up (SMD = 0.26, 95% CI − 0.36 to 0.89). Participants in both groups improved their coping with pain with VMT participants reporting slightly greater improvements at follow-up (SMD = 0.26, 95% CI −0.36 to 0.88). We also examined the effect of VMT on weekly pre-session pain reports. The results suggest a decrease in pain intensity over the timespan of eight sessions (SDM = 0.54, 95% CI 0.15 to 2.34). Finally, ratings on the Patient Global Impression of Change scale at week 8 indicated that 63.7% of participants felt moderately to a great deal better since starting the VMT treatment program. At follow-up, 47.5% continued to feel that they had improved moderately to a great deal.
Treatment Benefits: Qualitative Results
A total of 23 participants attended the focus groups. The coding for treatment benefits or harms resulted in the identification of three themes (Table 3). First, participants reported that VMT had been beneficial for the management of their pain, stress, and emotions (Theme 1 Self-Management). The findings suggested further that skills learned in the sessions were transferred to non-clinical contexts. Specifically, participants reported using humming and toning, singing, and listening to the CDs for the management of pain and stress. Many expressed amazement at how they had never considered music for pain management: “You know, we always relate pain with a pill or something to rub on to ease the pain. I never thought of music to help ease pain until I took the music therapy sessions.” Participants also reported that the VMT sessions facilitated expression of feelings and alleviated depression. Participants expressed their emotions through music (e.g., spontaneous call-and-response style singing) or verbally shared feelings evoked by the music. Finally, several comments spoke to the fact that the VMT sessions had encouraged better self-care by creating some quiet time during the day and using music to nurture oneself.
Table 3.
Qualitative Findings: Treatment Benefits
| Theme and definition | Categories and definitions | Example quotes |
|---|---|---|
| Theme 1 Self-management: VMT promotes self-management of pain, stress, and mood through the use of music listening, singing, toning, and deep breathing techniques. It furthermore stimulates an attitude of self-care. | Pain: Participants discover music as a new way to help manage pain |
|
| Stress: Music helps to relax and elicits feelings of peace and safety |
|
|
| Emotions: Group music making enhances participants’ mood, gives “voice” to suppressed emotions, and enhances positive self-expression. |
|
|
| Self-care: VMT results in greater awareness of self and one’s needs, motivating participants to nurture and care for themselves. |
|
|
| Theme 2 Togetherness: The common experience of chronic pain coupled with creative engagement in group music making evoked a strong sense of belongings | Shared experience: Being with others affirms that one is not alone in the struggles with chronic pain. |
|
| Social support: Creating music together and verbally processing emotions provides support and reduces isolation. |
|
|
| Joy & happiness: Singing and improvising music with others brings joy and a sense of fulfillment |
|
|
| Theme 3 Transformation: VMT brings about a shift in how participants perceived themselves and their being-in-the-world. | Renewed sense of self: The VMT interventions increased participants’ awareness of and appreciation for their capable selves. |
|
| Empowerment: The act of creating music with one’s voice acts as a metaphor for having a voice and being heard in the world. |
|
|
| Repositioning oneself: Making music together enabled participants to experience a new way of being in the world. |
|
The second theme, Togetherness, identifies the importance of being with people who were also experiencing chronic pain. Participants felt understood and supported by other group members. One participant noted: “Everybody goes through different pain and my pain might not be your pain. You maybe can help me with my pain and I maybe can help you with your pain. So it was all a matter of meeting new people and listen to someone else… it’s not like you the only one having problems.”
Furthermore, creating music together resulted in a sense of unity and belonging. Participants noted that, in contrast to traditional support groups they had attended in the past, creating music together resulted in meaningful relating and much needed joy and motivation.
The third theme, Transformation, illustrates the role that the VMT intervention played in helping participants gain a new sense of self and experience a different way of being in the world. Numerous references were made to how the VMT sessions helped increase positive self-statements and elicit personal strengths that had been buried underneath the pain and suffering. A large number of comments spoke about the power of music to empower and motivate. For example: “Learning the different songs that are uplifting. Some of them are inspirational…it gives you a sense of you, a sense of being and makes you realize you have the key to your own destiny.” Participants also talked about how the VMT sessions transformed the way they related to others and the world. Many participants shared that they had been isolated and lonely and no longer had a desire to interact with others. In the VMT sessions, participants experienced the joy of being with others, the strength one gains from being together in creativity, and the personal benefits gained from positive connections with others.
Integration of Quantitative and Qualitative Findings
A side-by-side comparison of quantitative and qualitative findings (Table 4) shows congruency in the findings for self-efficacy, pain, coping, and patient perception of change. However, discrepancies were found for physical functioning and mood. For physical functioning, responses on the general activities subscale of the MPI showed no improvement. This subscale asks questions related to social activities (e.g., visit friends, go the the movies) and chores (e.g., do laundry). In contrast to the quantitative ratings, participants shared that since participating in the VMT treatment program they felt less isolated, had the desire to be around people again, and experienced joy when being with others. When asked about the discrepancy of these statements with their questionnaire scores, they provided three main explanations. First, they stated that many items on the scale did not capture the benefits they received from VMT. Second, they reported that they refrained from participating in several items listed on the scale (e.g., going to the movies, taking a trip) because of financial constraints, bringing the social validity of this scale into question for inner city, low-income African Americans. Third, participants explained that chronic pain had ruined their social relationships and that it would take more than 8 weeks to restore these.
Table 4.
Comparison of Quantitative and Qualitative Findings
| Outcome | Quantitative Results | Qualitative findings | Participants’ explanations of discrepancies |
|---|---|---|---|
| Physical functioning | Some improvement for pain interference; no change in general activities | Decreased isolation and desire to be around people again | MPI items lack relevance; lack of money for social activities; building relationships takes time |
| Self-efficacy | Moderate increase | Renewed sense of self, empowerment | N/A (congruent findings) |
| Average pain/coping | Small improvements | Better management of pain and stress | VMT interventions are effective, small improvements are important |
| Emotional functioning | Low anxiety and depression at BL; no improvement | VMT lifted mood, brought joy, and helped with depression | Distrust of HADS, pointing to stigmatizing association between chronic pain and mental illness Underreporting of anxiety and depression? |
| Perception of change | Significant improvement | Renewed sense of self, empowerment, and better self-management | N/A (congruent findings) |
| Other benefits | N/A | Social support, sense of belonging, emotional expression, joy, and self-care | Participants encourage inclusion of positive health outcomes in measurement protocol |
As for mood, participants reported experiencing great joy in the VMT sessions which, they noted, helped alleviate their depression. Their responses on the HADS indicated, on average, no to mild depression levels at baseline, yet many participants spoke during the VMT sessions about being lonely and depressed. Focus group statements, it should be noted, suggested feelings of distrust of the HADS This may have led to underreporting of anxiety and depression. Finally, the qualitative data suggested additional treatment benefits that were not included as outcomes in the current study, namely improved social engagement, emotional expression, self-care, happiness, empowerment, and motivation.
Discussion
The purpose of this study was to provide feasibility data as well as estimates of treatment effect of VMT for core outcomes in chronic pain management. The study achieved a consent rate of 77%, demonstrating acceptable recruitment feasibility. Of the 28 participants allocated to VMT, 24 started the first session and 22 completed the 8-week treatment protocol, suggesting excellent acceptability of the treatment. All but one VMT participant who completed the 8-week treatment period, returned for follow-up measures. In the WLC study group, most participants were lost between baseline and week 4 measurements and then prior to follow-up. Whereas an attrition rate of 20% (week 8) is compatible with reported attrition rates in interventions studies for chronic pain (Cheong, Smotra, & Williams, 2014), the attrition rate of 27% at follow-up was higher than expected. An important reason for dropout was our inability to maintain contact with several WLC participants due to disconnected phones, a common issue with patients served at our health center. As for feasibility of the outcome measures protocol, the participants were highly critical of the outcome measures related to physical functioning, particularly the MPI General Activities Subscale, and the HADS emotional functioning scale, as not capturing the treatment benefits they had experienced. Moreover, participants questioned the social validity of the MPI for a low-income population as several of the activities listed presumed availability of financial means. They strongly recommended measuring physical functioning through different means. Focus group comments about the HADS suggested distrust of the instrument pointing to the mental health taboo that surrounds societal, often stigmatizing, stereotypes about chronic pain (Kendall-Tackett, Marshall, & Ness, 2003). The HADS, however, has been successfully used in other chronic pain trials. As discussed earlier, minorities have been greatly underrepresented in chronic pain research. Given the high percentage of African-Americans in our study, we wonder whether this stigma may be more prominent for African-Americans. Finally, participants strongly recommended adding positive health outcome measures in future trials.
The focus groups provided supporting evidence of participant acceptability of the VMT program. Participants provided positive feedback about the intervention; only one suggestions for improvement of the VMT program content or process was offered, namely the inclusion of more movement in the sessions. However, many participants recommended that longer treatment sessions and increase of overall program duration.
In contrast to the WLC group, VMT participants’ self-efficacy improved significantly. Self-efficacy has been found to be a significant predictor of physical functioning in people with chronic pain (Strahl, Kleinknecht, & Dinnel, 2000), yet we did not find significant improvements in physical functioning at follow-up. This may have been due to the lack of social validity of the General Activities subscale of the MPI, as discussed above. However, post-intervention improvements in pain interference were also not sustained at the 12-week follow-up. It is possible that maintenance treatment may be needed to sustain long-term treatment effects.
Qualitative findings indicated that participants experienced a renewed sense of self and a desire to be with others. Chronic pain can have a devastating effect on relationships with family and friends. This collapse of one’s social world results in loss of interaction with people and engagement in activities that previously aided in coping with pain. Feeling connected with others has been identified as an important need of people with chronic pain (Skuladottir & Halldorsdottir, 2011). The qualitative data suggest that VMT helped to build renewed confidence that interaction with others can be joyful and motivating. The majority of participants reported that they had improved moderately to a great deal since starting the VMT treatment. This was supported by moderate effect sizes for average weekly pain intensity, but calls into question the small effect size that was found for average pain coping.
The integration of the quantitative and qualitative findings provides a more nuanced understanding of treatment benefits and points to additional benefits that were not captured by the outcome measure protocol of this study. First, participants discovered music as a resource for the self-management of pain and stress. Whereas music often functions as a backdrop against which activities take place, participants in the VMT program learned to use music more purposively to enhance breathing, release stress, and manage pain. Through its aesthetic qualities, music offers comfort and peace, lifts people’s spirit and improves their sense of well-being (Livesey et al., 2012). Similar findings were reported in a study exploring adult cancer patients’ use of music (O’Callaghan et al., 2014).
The qualitative findings also pointed to the importance of the participants’ active engagement in music making. Participants engaged in toning, singing of songs, and creative vocal improvisations that were characterized by beautiful harmonizing. It is important to note that most participants in this study belonged to African-American Churches. They felt quite comfortable singing, harmonizing, participating in call-and-response type singing, and improvising, as this was not unlike the music making in their Churches. For people with chronic pain, this active engagement is important for several reasons. First, it allowed the participants to “be heard” and “to have a voice” as stated by various participants. The experiences of chronic pain sufferers are often trivialized by doctors as well as family and friends who doubt the reality of their pain. And so, slowly but surely, their voices are muted by skepticism and mistrust (Werner, Widding Isaksen, & Materud, 2004). Second, the active and creative engagement in VMT stands in stark contrast to feeling victimized by the pain and passively receiving pharmacological treatments. Third, the active engagement resulted in strong feelings of empowerment and motivation. Whereas in many traditional treatment encounters patients learn ‘about’ the importance of self-motivation or are told that motivation is key to improvement, it appears that the act of creative music making with others was motivating in and of itself and, of more importance, it led to a shift from feeling victimized to a perception of a capable self. The literature has emphasized the primacy of motivation and patient engagement for successful management of chronic pain (Navratilova & Porreca, 2014).
This study has several limitations. As appropriate for a feasibility study, we used a small sample and the research was limited to one setting with a predominantly African American low income population. In addition, no active control group was used for this study. Therefore, we caution the reader against generalizing the results at this time. In addition, the VMT protocol was implemented by the lead investigator. Future studies will need to employ larger samples, include multiple therapists trained in the protocol, and include an attention control or active control group. The qualitative data suggest that refinement of the outcome assessment protocol will be needed for future trials through the addition of positive health outcomes. Furthermore, the outcomes measures used in this study should be reviewed for cultural relevance to inner city, low-income African-Americans and alternative measures may need to be considered.
The quantitative results of this study suggest that longer treatment periods or additional interventions may be needed for participants to translate improved self-efficacy into enhanced coping and functioning. Based on the integration of quantitative and qualitative findings, we conclude that VMT may be effective in building essential stepping stones for chronic pain management, namely developing: 1) a positive relationship with one’s self; 2) enhanced self-efficacy; 3) motivation and empowerment to take charge of one’s pain management; and 4) renewed social engagement. These components may lay important and necessary groundwork for patient engagement in subsequent interventions such as physical therapy and exercise.
Acknowledgments
Funding:
Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number R03NR013551. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors thank Dennis C. Turk, PhD, from the University of Washington for his valuable contributions to this study.
Contributor Information
Joke Bradt, Department of Creative Arts Therapies, College of Nursing and Health Professions, Drexel University, Philadelphia.
Marisol Norris, Department of Creative Arts Therapies, College of Nursing and Health Professions, Drexel University, Philadelphia.
Minjung Shim, Department of Creative Arts Therapies, College of Nursing and Health Professions, Drexel University, Philadelphia.
Edward J. Gracely, Department of Family, Community and Preventive Medicine, College of Medicine, Drexel University College of Medicine.
Patricia Gerrity, Department of Nursing, College of Nursing and Health Professions, Drexel University.
References
- Barnes PM, Bloom B, Nahin R. Complementary and alternative medicine use among adults and children: United States, 2007. National Health Statistics Reports. Vol. 12. Hyattsville, MD: National Center for Health Statistics; 2008. [PubMed] [Google Scholar]
- Boer D, Abubakar A. Music listening in families and peer groups: Benefits for young people’s social cohesion and emotional well-being across four cultures. Frontiers in Psychology. 2014;5:1–15. doi: 10.3389/fpsyg.2014.00392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolen J, Schieb L, Hootman J, Helmick C, Theis K, Murphy L, Langmaid G. Differences in the prevalence and severity of arthritis among racial/etnic groups in the United States. National Health Interview Surveys, 2002, 2003, and 2006. Preventing Chronic Disease. 2010;7(3):A64. [PMC free article] [PubMed] [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. [Google Scholar]
- Brown S, Martinze M, Parsons L. Passive music listening spontaneously engages limbic and paralimbic systems. Neuroreport. 2004;15(13):2033–2037. doi: 10.1097/00001756-200409150-00008. [DOI] [PubMed] [Google Scholar]
- Buckenmaier C, Schoomaker E. Patients’ use of active self-care complementary and integrative medicine in their management of chronic pain symptoms. Pain Medicine. 2014;15:S7–S8. doi: 10.1111/pme.12384. [DOI] [PubMed] [Google Scholar]
- Bullington J, Nordemar R, Nordemar K, Sjöström-Flanagan C. Meaning out of chaos: A way to understand chronic pain. Scandinavian Journal of Caring Sciences. 2003;17(4):325–331. doi: 10.1046/j.0283-9318.2003.00244.x. [DOI] [PubMed] [Google Scholar]
- Bullington J. Embodiment and chronic pain: Implications for rehabilitation practice. Health Care Analyrics. 2009;17:100–109. doi: 10.1007/s10728-008-0109-5. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Vital signs: Overdoses of prescription opioid pain relievers—United States, 1999–2008. Morbidity and Mortality Weekly Report. 2011;60:1–6. [PubMed] [Google Scholar]
- Cepeda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database of Systematic Reviews. 2006;2 doi: 10.1002/14651858.CD004843.pub2. [DOI] [PubMed] [Google Scholar]
- Chanda ML, Levitin DJ. The neurochemistry of music. Trends in Cognitive Sciences. 2013;17(4):179–193. doi: 10.1016/j.tics.2013.02.007. [DOI] [PubMed] [Google Scholar]
- Cheong YC, Smotra G, Williams AC. Non-surgical interventions for the management of chronic pelvic pain. Cochrane Database of Systematic Reviews. 2014;3 doi: 10.1002/14651858.CD008797.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou R, Huffman L. Guideline for the evaluation and management of low back pain: Evidence Review. Glenview, IL: n.d. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- Creswell JW. A concise introduction to mixed methods research. Thousand Oaks, CA: Sage; 2015. [Google Scholar]
- Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, … Witter J. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113(1–2):9–19. doi: 10.1016/j.pain.2004.09.012. [DOI] [PubMed] [Google Scholar]
- Fisher T, Burnet D, Huang E, Chin M, Cagney K. Cultural leverage: Interventions using culture to narrow racial disparities in health care. Medical Care Research and Review. 2007;64:243S–282S. doi: 10.1177/1077558707305414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy W. ECDEU assessment manual for psychopharmacology. Washington, DC: 1976. [Google Scholar]
- Institute of Medicine. Institute of Medicine Report. Washington, DC: Institute of Medicine; 2011. Relieving Pain in America: A blueprint for Transforming Prevention, Care, Education, and Research. [DOI] [PubMed] [Google Scholar]
- Keefe F, Lumley M, Anderson T, Lunch T, Carson K. Pain and emotion: New research directions. Journal of Clinical Psychology. 2001;57(4):587–607. doi: 10.1002/jclp.1030. [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett K, Marshall R, Ness K. Chronic pain syndromes and violence against women. Women & Therapy. 2003;26(1/2):45–56. [Google Scholar]
- Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory. Pain. 1985;23(4):345–356. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- Koelsch S. Towards a neural basis of music-evoked emotions. Trends in Cognitive Sciences. 2010;14(3):131–137. doi: 10.1016/j.tics.2010.01.002. [DOI] [PubMed] [Google Scholar]
- Kranz D, Bollinger A, Nilges P. Chronic pain acceptance and affective well-being: A coping perspective. European Journal of Pain. 2010;14(10):1021–1025. doi: 10.1016/j.ejpain.2010.03.010. [DOI] [PubMed] [Google Scholar]
- Lee EC, Whitehead AL, Jacques RM, Julious SA. The statistical interpretation of pilot trials: Should significance thresholds be reconsidered? BMC Medical Research Methodology. 2014;14:41. doi: 10.1186/1471-2288-14-41. http://www.biomedcentral.com/1471-2288/14/41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livesey L, Morrison I, Clift S, Camic P. Benefits of choral singing for social and mental wellbeing: Qualitative findings from a cross-national survey of choir members. Journal of Public Mental Health. 2012;11(1):10–26. [Google Scholar]
- Maughan EF, Lewis JS. Outcome measures in chronic low back pain. European Spine Journal. 2010;19(9):1484–1494. doi: 10.1007/s00586-010-1353-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maultsby P. Africanisms in African-American Music. In: Hayes FW, editor. A turbulent voyage: Readings in African American studies. Lanham, MD: Rowman & Littlefield Publishers; 2000. [Google Scholar]
- MAXQDA. Version 11. Berlin, Germany: VERBI Software - Consult - Sozialforschung; 1989–2014. [Google Scholar]
- McCough JJ, Faraone SV. Estimating the size of treatment effects: Moving beyond P values. Psychiatry. 2009;6(10):21–29. [PMC free article] [PubMed] [Google Scholar]
- McRae MB, Thompson DA, Cooper S. Black churches as therapeutic groups. Journal of Multicultural Counseling and Development. 1999;26(4):207–220. [Google Scholar]
- Navratilova E, Porreca F. Reward and motivation in pain and pain relief. Nature Neuroscience. 2014;17(10):1304–1312. doi: 10.1038/nn.3811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholas MK. The Pain Self-Efficacy Questionnaire: Taking pain into account. European Journal of Pain. 2007;11:153–163. doi: 10.1016/j.ejpain.2005.12.008. [DOI] [PubMed] [Google Scholar]
- O’Callaghan C, McDermott F, Michael N, Daveson B, Hudson P, Zalcberg J. “A quiet still voice that just touches”: Music’s relevance for adults living with life-threatening cancer diagnoses. Supportive Care in Cancer. 2014;22:1037–1047. doi: 10.1007/s00520-013-2059-1. [DOI] [PubMed] [Google Scholar]
- Price CJ, Thompson EA. Measuring dimensions of body connection: Body awareness and bodily dissociation. Journal of Alternative and Complementary Medicine. 2007;16(9):945–953. doi: 10.1089/acm.2007.0537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reagon BJ. Pioneering African American gospel composers. In: Reagon BJ, editor. We’ll understand it better by and by. Washington, D.C: Smithsonian Institution Press; 1992. pp. 3–18. [Google Scholar]
- Sanger KL. Functions of freedom songs in the civil rights movement. The Howard Journal of Communication. 1997;8:179–195. [Google Scholar]
- Skuladottir H, Halldorsdottir S. The quest for well-being: Self-identified needs of women in chronic pain. Scandinavian Journal of Caring Sciences. 2011;25(1):81–91. doi: 10.1111/j.1471-6712.2010.00793.x. [DOI] [PubMed] [Google Scholar]
- Strahl C, Kleinknecht RA, Dinnel DL. The role of pain anxiety, coping, and pain self-efficacy in rheumatoid arthritis patient functioning. Behaviour Research Therapy. 2000;38(9):863–873. doi: 10.1016/s0005-7967(99)00102-3. [DOI] [PubMed] [Google Scholar]
- Werner A, Widding Isaksen L, Materud K. ‘I am not the kind of woman who complains of everything’: Illness stories on self and shame in women with chronic pain. Social Science & Medicine. 2004;59:1035–1045. doi: 10.1016/j.socscimed.2003.12.001. [DOI] [PubMed] [Google Scholar]
- Zigmond A, Snaith R. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavia. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]