Abstract
Vital to the prevention of work-related ill-health (WRIH) is the availability of good quality data regarding WRIH burden and risks. Physician-based surveillance systems such as The Health and Occupation Research (THOR) network in the UK are often established in response to limitations of statutory, compensation-based systems for addressing certain epidemiological aspects of disease surveillance. However, to fulfil their purpose, THOR and others need to have methodologic rigor in capturing and ascertaining cases. This article describes how data collected by THOR and analogous systems can inform WRIH incidence, trends, and other determinants. An overview of the different strands of THOR research is provided, including methodologic advancements facilitated by increased data quantity/quality over time and the value of the research outputs for informing Government and other policy makers. In doing so, the utility of data collected by systems such as THOR to address a wide range of research questions, both in relation to WRIH and to wider issues of public and social health, is demonstrated.
Keywords: incidence, interventions, methodology, occupational, surveillance
1. Introduction
The prevention of ill health associated with work, as well as the promotion of health at work and the maintenance of work ability need to be informed by good quality data regarding the burden and risks of ill health. Such data are key to preventing work-related ill health (WRIH) as enshrined in regulatory guidance, be it through the preparation of suitable and sufficient risk assessments to managing occupational health risks through information, instruction, and training of workers and employers.
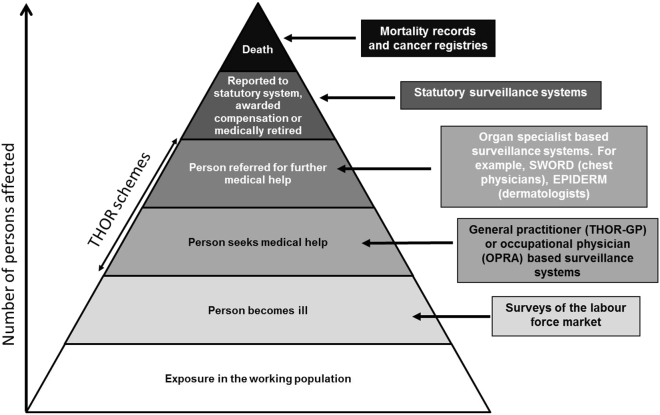
On a national scale, data sources include statutory reporting systems (often linked to compensation), mortality records, cancer registries, and other routine data sources such as labor market surveys. Many countries, including the UK, may also have one or more surveillance systems based on voluntary physician reporting [1]. These systems are often established in response to limitations of statutory based systems for addressing certain epidemiological aspects of disease surveillance, typically capturing cases at a much broader level (than statutory systems) and therefore representing a complementary picture of the burden of disease. However, to fulfil their purpose these systems need to have methodologic rigor in capturing and ascertaining cases. They have to characterize the numerator cases by demography, industry, occupation, and exposures (including tasks and psychological health hazards as well as physical, chemical, and biological ones) and to relate them to a defined denominator. The systems also need to recognize and take steps to mitigate, or at least understand, biases for example from fatigue in data collection or reporting or from different sampling strategies.
The Health and Occupation Research (THOR) network is hosted by the Centre for Occupational and Environmental Health (COEH) in the Faculty of Biological, Medical and Health Sciences at the University of Manchester, Manchester, UK and collects data on WRIH and its determinants throughout the UK and (since 2005) the Republic of Ireland (ROI) [2]. THOR is (partially) funded by the two regulators of health and safety: the Health and Safety Executive (HSE) in the UK and the Health and Safety Authority (HSA) in the ROI. The evolution of the network has been gradual. The network initiated as Occupational Disease Intelligence Network (ODIN) with schemes set up (at various time points) to enable system-specific specialists (e.g., chest physicians) and occupational physicians to report throughout the UK (Table 1). THOR developed from ODIN in a number of important ways including explicitly the development of new methods such as to study trends, and to obtain better estimates of incidence and by extending the scope of the research beyond occupational disease to include other aspects of health and occupation research such as sickness absence and rehabilitation following WRIH (Table 2). THOR also extended the data collection and surveillance both beyond specialists, that is further down the surveillance pyramid by launching a general practitioner (GP)-based network [3] and beyond the UK by launching sister schemes in the ROI [4]. By becoming a leading founding member in the international MODERNET (monitoring trends in occupational diseases and tracing new and emerging risks in a network) consortium, THOR also influences WRIH research on a much wider scale [5]. Other important developments include the implementation of electronic reporting (which has been mandatory for new surveillance schemes since 2005 and encouraged for the extant legacy schemes) and innovation in research-led teaching by using the research database as a platform from which to launch the THOR-related educational initiative, Electronic Experiential Learning Audit & Benchmarking (EELAB) [6].
Table 1.
The Health and Occupation Research network
| Name of scheme | Reporting specialists | Related organization | Period of data collection |
|---|---|---|---|
| SWORD – Surveillance of Work-related & Occupational Respiratory Disease | Consultant chest physicians | British Thoracic Society & Society of Occupational Medicine | 1989–current |
| EPIDERM – Surveillance of Work-related Skin Disease | Consultant dermatologists | British Contact Dermatitis Group, British Association of Dermatologists, Society of Occupational Medicine | 1993–current |
| OPRA – Occupational Physicians Reporting Activity | Occupational physicians | Society of Occupational Medicine, Faculty of Occupational Medicine | 1996–current |
| SIDAW – Surveillance of Infectious Diseases at Work | Consultants in communicable diseases | Public Health Medicine Environmental Group, Communicable Disease Surveillance Centre, Public Health Laboratory Service | 1996–current |
| OSSA – Occupational Surveillance Scheme for Audiological Physicians | Consultant audiologists | British Association of Audiological Physicians | 1997–2006 |
| MOSS – Musculoskeletal Occupational Surveillance Scheme | Consultant rheumatologists | British Society for Rheumatology | 1999–2009 |
| SOSMI – Surveillance of Occupational Stress & Mental Illness | Consultant psychiatrists | Royal College of Psychiatrists | 1999–2009 |
| THOR-GP – THOR in General Practice | General practitioners | Royal College of General Practitioners | 2005–current |
Table 2.
Summary of organizational, methodological, and other developments implemented by The Health and Occupation Research (THOR)
| Topic | Development implemented by THOR |
|---|---|
| THOR & its coverage |
|
| Physician participation & motivation |
|
| Estimates of disease incidence |
|
| Estimates of trends in disease incidence |
|
| Other THOR research developments |
|
The blend of surveillance schemes has changed with time (the first scheme, SWORD, is still going strong [7]), and new ones have been launched replacing others partly to ensure the most effective approach, and partly to achieve efficiencies because of limitations in the funding resources. Thus, data on musculoskeletal and mental disorders which from 1999 to 2009 were collected from MOSS and SOSMI by rheumatologists and psychiatrists, respectively, are now collected from the GP as well as the occupational physician schemes [3], [8]. As of January 2016, in excess of 1,000 physicians were enrolled in THOR with approximately 1,700 case notifications during 2015.
As with the evolution of the network itself, the research outputs generated by THOR have also evolved over time, both in response to the increase in data but also in response to increased sophistication in the methods employed to analyze the data. Since 2002, there have been 60+ peer reviewed articles addressing different aspects of THOR research, from simplistic overviews of the burden of disease to more sophisticated analyses such as methodological refinements to estimating disease incidence and trends in incidence. The aim of this review is to bring together the different strands of THOR research into one concise article therefore providing a single useful resource describing how data collected by voluntary surveillance systems such as THOR can be used to determine occupational and work-related disease incidence, trends, and other related determinants. The value of these research outputs in terms of informing Government and other policy makers is our ultimate goal and will also be discussed as will the methods employed to ensure physician motivation and engagement.
2. Disease incidence
Data collected by surveillance systems such as THOR are invaluable for determining disease incidence. Although under-reporting is likely to be an issue for THOR, it is probably more of a concern for statutory systems (where reporting may also exclude certain diseases, for example, mental ill-health). By contrast, systems based on self-reports (e.g., labor market surveys) may over-estimate disease incidence. At the simplest level, the cases, or numerator data, collected by THOR provide an overview of the burden of disease including how this might vary by factors such as geography, age and sex, causal agent, and occupation. Such descriptive overviews are a useful starting point, particularly during the initial data collection period of a surveillance scheme when the quantity of data may not suffice to undertake more sophisticated analyses and most research outputs will include at least an element of such descriptive analyses. However, whilst descriptive overviews of the reported cases are of interest, a key objective of surveillance systems such as THOR is to determine nationally representative and statistically robust estimates of disease incidence. To do so (and to compare disease incidence meaningfully between different locations, jobs, industries, etc.), it is necessary to take into account differences in the underlying populations (denominators) from which the cases are drawn. This has led to a number of methodological challenges, some of which are specific to estimating incidence for certain groups of physicians, whilst others are more general.
Issues that have been addressed by THOR include allowing for the likelihood that not all cases of WRIH are captured by voluntary surveillance systems such as THOR (a physician may not participate in the scheme or if they do, they may not report everything they see) [9], addressing biases in the populations covered by a reporting system (e.g., towards specific industries as exemplified by occupational physician reporting to Occupational Physicians Reporting Activity) [10], or biases arising from participating physicians being possibly different to physicians in general (e.g., ∼1% of GPs in Britain participate in THOR-GP, and, unlike GPs in general, they have a diploma in occupational medicine) [11]. THOR researchers have also addressed important issues such as incidence calculations for long latency diseases (whereby denominators may need to be lagged by several decades) and the impact of physician sampling frequency (e.g., monthly vs. annual reporting) on disease incidence [12]. Recently, work has focused on estimating the proportion of false zeros and the resulting impact on disease incidence reported to THOR. When a physician does not see any cases during their reporting month they are asked to respond with “I have nothing to report”. It is hypothesized that some of these zero returns may in fact be false, that is, the physician did see reportable cases but due to time constraints, for example, it was easier to respond with a zero return.
To illustrate with an example, UK incidence rates for chest physicians reporting to SWORD were initially calculated by applying the UK working population (obtained from the labor force survey) as the denominator [7]. With the development of THOR, these rates were subsequently refined to take into account cases not captured by SWORD due to non-participation and nonresponse [9] and then refined further still to take into account the likely presence of false zeros. Whilst some of the assumptions behind these adjustments are still to be fully resolved (and therefore the true incidence likely lies somewhere in between these estimates), addressing issues such as these, which is ongoing within THOR, has ensured the validity, reliability, and therefore utility of THOR data for determining disease incidence. The calculation of incidence rates using data collected from GPs has presented further challenges. The participating GPs have a UK-wide distribution; however, the population captured by the THOR-GPs (the employed patients registered with each participating practice) may have a different employment distribution than the national population. Therefore, using Labour Force Survey data as a denominator is likely to lead to inaccuracies when calculating incidence rates. Methods have been developed to characterize the THOR-GP population denominator by linking practice postcode information to census data. A further strength of having a network with multiple sources of data such as THOR is the ability to compare or triangulate incidence rates arising from different groups of physicians [13]. THOR data can also be compared with incidence rates derived from other, external data sources—for example, the self-reported work-related illness surveys [14]. Triangulations such as these help validate the individual data sources and enable a more complete picture of WRIH in the UK to be constructed (Fig. 1).
Fig. 1.
Disease severity pyramid.
EPIDERM, Occupational Skin Surveillance; OPRA, Occupational Physicians Reporting Activity; SWORD, Surveillance of Work-related and Occupational Respiratory Disease; THOR-GP, The Health and Occupation Research in General Practice.
Although significant methodological advances within THOR have been made over the years in relation to determining disease absolute incidence rates by factors such as type of disease, age and sex, determining disease incidence rates in relation to specific exposures is more problematic, primarily because it is difficult to quantify the denominator (population exposed). Whilst for some agents (e.g., coal or flour) it may be easier to quantify the (occupationally) exposed population, for others (e.g., soaps and detergents) it may be more problematic. One way THOR researchers have addressed this has been to analyze relative rather than absolute trends in incidence. Thus in some circumstances it is not necessarily important that the denominator is quantified, so long as it remains fairly stable over time.
3. Trends in incidence and a new methodology
Whilst plotting reported cases over time can provide an indication of temporal trends, this approach does not necessarily take into account factors that might unduly influence the true trend. One of the most significant methodological advances implemented by THOR in recent times has been the use of multilevel models (MLMs) to investigate the change in disease incidence over time [15]. This approach enables (among other things) factors such as variation in the number of physicians reporting to THOR, seasonal patterns in reporting, or a decrease in reporting over time because of reporter fatigue to be taken into account. The issue of reporter fatigue (and its potential impact on WRIH trends) has attracted considerable research within THOR: as membership time within a scheme such as THOR increases, might a reporter become less committed to active participation but still retain membership? How such fatigue manifests itself and whether this can cause bias in time trend estimation has been a major methodological concern. Approaches taken to address this have included modelling change in reporters’ response over time (e.g., has there been an increase in zero-returns or nonresponse) and investigations of false zeros.
This MLM method was first used to estimate change in incidence of WRIH relative to 1999 for the HSE as part of their Revitalising Health and Safety Strategy, and continues to be used on an annual basis to provide the HSE with estimates of trends in WRIH [16]. In addition to looking at overall trends, this method has more recently been applied to investigate trends in WRIH within specific industries [17], attributed to specific agents [18], [19], [20] or most notably, to evaluate specific interventions aimed at decreasing disease incidence [21], [22], [23], [24], [25]. In doing so it has become apparent that whilst the overall incidence of work-related diseases such as asthma and contact dermatitis may be decreasing (and in some cases these reductions may be attributed to specific interventions by the HSE and others), for certain groups—for example, asthma in bakers attributed to flour, allergic contact dermatitis in nail technicians attributed to acrylates, and irritant contact dermatitis in healthcare workers attributed to hand washing—incidence in these situations may be increasing.
In addition to investigating WRIH trends in the UK, this MLM methodology has recently been applied to investigate WRIH trends in other European countries, primarily as a result of THOR’s participation in MODERNET. Approximately 20 European countries participate in MODERNET with the aim of facilitating the exchange of information and knowledge by collaboration on a European scale. Analysis of trends of specific occupational diseases/disease groups across 10 MODERNET countries observed similar trends for asthma and contact dermatitis (generally declining) but more variable trends (both within and between countries) for the other groups studied (noise-induced hearing loss, carpal tunnel syndrome, and upper limb musculoskeletal disorders) [26].
4. Other research areas
Although the primary aim of THOR data collection is to estimate incidence trends in WRIH, the quantity and quality of the data collected plus the methodological and other developments implemented by THOR have enabled a wide range of additional research questions to be addressed. For example, studies have been implemented within THOR to examine physicians’ diagnostic preferences regarding WRIH. From these it was concluded that, when presented with the same information, there was no systematic difference in the diagnostic labelling of work-related mental ill health by (THOR) occupational physicians, psychiatrists, and GPs or of asthma by (THOR) occupational physicians and chest physicians [27], [28]. Research by THOR is not limited to WRIH determinants. Other research areas include the length of sickness absence and how this may vary by diagnosis, job, sex, and other factors, the impact of the introduction of the Fit Note, and the role of GP–patient negotiations in sickness absence certification [29], [30], [31]. THOR-GP data have also enabled the investigation of factors influencing whether, and to whom, a secondary referral is made. Another recent and innovative area of THOR research is the use of SWORD data in conjunction with techniques such as Quantitative Structure Activity Relationships (QSAR) in order to help identify and even predict novel asthmagens [32]. Work in this area is currently being extended to the feasibility of applying QSAR to identify novel agents for other THOR data, for example, contact dermatitis.
THOR data can often also be applied to investigate new or emerging areas of broader social and public health interests such as the impact of an ageing population or of widening social inequalities. For example, increased life expectancy and pensionable age, and an increasing dependency ratio necessitate a need to keep older workers in employment and encourage those who have left to return to work. However, research is needed to address questions such as whether older workers with existing comorbidities have an increased susceptibility to occupational injuries or other WRIH. Similarly, social inequalities in health have long been described as showing an inverse relationship between social class and mortality and morbidity. However, incidence rates for work-related mental-ill health by socioeconomic group based on reports to THOR-GP suggest a different pattern; rates were highest in lower management and intermediate occupations. Thus, THOR data are currently being used to examine the psychosocial risk factors affecting different socioeconomic and demographic groups. Another current topic of interest is the application of data collected by occupational surveillance systems such as THOR to act as an early warning system for the wider (nonoccupational) environment, the rationale being that health risks often occur first in the workplace where the same environmental contaminants are present at concentrations or intensities which are orders of magnitude greater than in the general environment.
5. Collaborative research
Although all research carried out within THOR is collaborative, physician-based networks such as THOR also provide the opportunity for external collaboration between academic (THOR) researchers and the physicians participating in the schemes. For example, the latter may identify a new cause or emerging trend during their clinical practice that they want to corroborate further by interrogating THOR data. To this end, research led by key dermatologists participating in EPIDERM has investigated trends in contact dermatitis attributed to agents such as isothiazolinones, rubber accelerators, and acrylates [19], [20], [33]. Since COEH also undertakes postgraduate teaching in occupational medicine, there is also the opportunity for collaboration between THOR researchers and COEH students (physicians and hygienists). Recent examples that have resulted in joint peer reviewed publications include a comparison of work-place injury data as reported by occupational physicians and GPs [34] and an investigation of work-related neoplasia associated with solar radiation [35]. On a wider scale, there are the aforementioned opportunities for collaborative research arising from THOR’s participation in networks such as MODERNET [26], [36].
6. Physician motivation and engagement
Critical to the success of THOR (and analogous schemes) is the ongoing participation, truly voluntary, of the physicians. To this end, emphasis is placed on keeping the reporting process as simple as possible and not overburdening the reporting physician. For most schemes, the initial approach (ODIN) was for physicians to participate either monthly or for one randomly selected month per year by returning a postal report card containing details of the cases seen. When ODIN evolved into THOR, other options were introduced. Physicians can now delegate the task to another member of their clinical team such as a specialist registrar or clinical nurse specialist—so long as the physician accepts responsibility for the diagnostic standard of the cases—and we also have different methods of reporting, for example, via a web form. A survey of THOR participants in 2011 suggested that it takes 2–5 minutes to report a case to THOR, with a general consensus that the benefits obtained from participating in THOR far outweighed the time spent reporting. The benefits comprise the other important component of ensuring physician participation and regular feedback in the form of quarterly and annual reports [6]. Participants can also make use of the THOR ad hoc enquiry service whereby the THOR database (currently containing in excess of 100,000 case reports) can be interrogated to answer specific questions [37] on possible occupational health risks. Other benefits include attendance at meetings (where participants can learn about recent research within their specialty and also inform and influence the future of the surveillance system) and collaboration with colleagues and with THOR researchers to publish work based on collected data.
7. How THOR informs policy
THOR has been assessed by the UK Statistics Authority to meet the required standard to be classified as national statistics and remains one of the main sources of statistical information with which the HSE (and other agencies) determine their priorities and work programs on occupational health. A search for THOR on the HSE’s website will yield hundreds of documents which make substantial reference to THOR, and > 50 tables of THOR data. In addition to their routine use in presenting annual statistical data on WRIH, THOR data are also used regularly by the HSE to check anecdotal suspicions against a wider range of evidence, thus helping prioritize and provide an evidence base for their campaigns and interventions. For the period 2002–2014, the HSE submitted approximately 200 enquiries to THOR requesting information on cases reported in the respective areas of interest [37].
THOR data also provide an input to informing Parliament, for example, evidence to Select Committees, and parliamentary questions directed at government ministers, with data solicited by various public bodies, such as the Industrial Injuries Advisory Council and the HSE’s Asthma Partnership Board, to help inform their decisions. A key example is the aforementioned Revitalising Health and Safety Strategy. This was a 10-year strategy to improve health and safety at work, which aimed to reduce the impact of health and safety failures by 30% over this period [38]. THOR played an important part in measuring this target alongside HSE’s other data sources, including RIDDOR and the Labour Force Survey. In particular, THOR was the main data source used to report the statistically significant decrease in both work-related asthma and contact dermatitis between 1999–2000 and 2009–2010. A major advance regarding the utility of THOR data for policymakers has been the aforementioned development of MLMs to investigate overall trends and, more specifically, the impact of interventions. Applying this method, THOR data have not only been able to show beneficial reductions in incidence against government (HSE) strategic targets but also in response to interventions such as the EU Directive resulting in reduction of exposure to chromate in cement [25].
THOR also contributes to raising awareness among other sectors of society regarding the risks to health from work. Approximately 11% of the 631 enquiries to THOR in the period 2002–2014 were from industry and other bodies (excluding HSE, participating physicians, or research institutions) [38]. A recent HSE consultation on changes to the RIDDOR statute asked respondents to say what sources of data they used—including for “benchmarking of own performance against sector and for setting targets”—and 31% of the 558 responders had used one or more of the THOR data sets, compared with 25% using the government’s self-reported work-related illness surveys [39].
8. Summary and conclusions
In conclusion, this article shows that data collected by voluntary occupational surveillance systems such as THOR can be used to address a wide range of research questions, not only those limited to disease incidence and trends in incidence, but also to other determinants of WRIH and to wider issues of public and social health. It has shown how the research outputs have evolved over time, partly in response to an increase in data but also in response to increased sophistication in the methods used to analyze the data. Finally, it illustrates the importance of data such as the data used for informing Government policies aimed at reducing occupational disease incidence. This is an ongoing process, and as data collection continues, refinement of the methods used to analyze these data will also continue, thus providing us with even better quality occupational health information and hence enabling further important research questions to be addressed.
Conflicts of interest
All authors have no conflicts of interest to declare.
Acknowledgments
The authors are grateful to all physicians who report to the THOR schemes in the UK and ROI. This work was supported by the HSE in the UK (contract number PRJ500) and the Health and Safety Authority in ROI (contract number R101774). The study sponsors were not involved in the preparation, conducting, writing, or submitting of this manuscript.
References
- 1.Carder M., Bensefa-Colas L., Mattioli S., Noone P., Stikova E., Valenty M., Telle-Lamberton M. A review of occupational disease surveillance systems in Modernet countries. Occup Med (Lond) 2015;65:615–625. doi: 10.1093/occmed/kqv081. [DOI] [PubMed] [Google Scholar]
- 2.The Health and Occupation Research (THOR) network [Internet]. Manchester: the University of Manchester [cited 2016 Jun 30]. Available from: http://www.coeh.man.ac.uk/thor.
- 3.Hussey L.J., Turner S., Thorley K.J., McNamee R., Agius R. Work-related ill health in general practice, as reported to a UK-wide surveillance scheme. Br J Gen Pract. 2008;58:637–640. doi: 10.3399/bjgp08X330753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Money A., Carder M., Noone P., Hayes J., Bourke J., Turner S., Agius R. Work-related ill-health: Republic of Ireland, Northern Ireland, Great Britain 2005-2012. Occup Med (Lond) 2015;65:15–21. doi: 10.1093/occmed/kqu137. [DOI] [PubMed] [Google Scholar]
- 5.The MODERNET (monitoring trends in occupational diseases and tracing new and emerging risks in a network) website [Internet]. Leuven: MODERNET [cited 2016 Jun 30]. Available from: http://www.modernet.org/.
- 6.Electronic Experiential Learning Audit & Benchmarking – EELAB - a novel resource for education and continuing professional development in occupational health [Internet]. Manchester: the University of Manchester [cited 2016 Jun 30]. Available from: http://www.population-health.manchester.ac.uk/epidemiology/COEH/eelab.
- 7.Meredith S.K., Taylor V.M., McDonald J.C. Occupational respiratory disease in the United Kingdom 1989: a report to the British Thoracic Society and the Society of Occupational Medicine by the SWORD project group. Br J Ind Med. 1991;48:292–298. doi: 10.1136/oem.48.5.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cherry N.M., Meyer J.D., Holt D.L., Chen Y., McDonald J.C. Surveillance of work-related diseases by occupational physicians in the UK: OPRA 1996-1999. Occup Med. 2000;50:496–503. doi: 10.1093/occmed/50.7.496. [DOI] [PubMed] [Google Scholar]
- 9.Carder M., McNamee R., Turner S., Hussey L., Money A., Agius R. Improving estimates of incidence of specialist diagnosed, work-related respiratory and skin disease in Great Britain. Occup Med (Lond) 2011;61:33–39. doi: 10.1093/occmed/kqq164. [DOI] [PubMed] [Google Scholar]
- 10.Carder M., Money A., Turner S., Agius R. Workforce coverage by GB occupational physicians and disease incidence rates. Occup Med (Lond) 2014;64:271–278. doi: 10.1093/occmed/kqu042. [DOI] [PubMed] [Google Scholar]
- 11.Health and Safety Executive (HSE). Background quality report: Work-related ill-health statistics based on reports by general practitioners to THOR-GP [Internet]. Health and Safety Executive. 2015. 12 p. [cited 2016 Jun 30]. Available from: http://www.hse.gov.uk/statistics/pdf/thorgp-background-quality-report.pdf.
- 12.McNamee R., Chen Y., Hussey L., Agius R. Randomised controlled trial comparing time-sampled versus continuous time reporting for measuring incidence. Epidemiology. 2010;21:376–378. doi: 10.1097/EDE.0b013e3181d5c03f. [DOI] [PubMed] [Google Scholar]
- 13.Hussey L., Carder M., Money A., Turner S., Agius R. Comparison of work-related ill-health data from different GB sources. Occup Med (Lond) 2013;63:30–37. doi: 10.1093/occmed/kqs181. [DOI] [PubMed] [Google Scholar]
- 14.Self-reported work-related illness (SWI) and workplace injuries (LFS) [Internet]. Health and Safety Executive. [cited 2016 Jun 30]. Available from: http://www.hse.gov.uk/statistics/publications/swi.htm.
- 15.McNamee R., Carder M., Chen Y., Agius R. Measurement of trends in incidence of work-related skin and respiratory diseases, UK 1996–2005. Occup Environ Med. 2008;65:808–814. doi: 10.1136/oem.2007.036731. [DOI] [PubMed] [Google Scholar]
- 16.Carder M, McNamee R, Hussey L, Money A and Agius R. Time trends in the incidence of work-related disease in the UK, 1996-2014: estimation from THOR surveillance data [Internet]. Health and Safety Executive. 2015. 118 p. [cited 2016 Jun 30]. Available from: http://www.hse.gov.uk/statistics/pdf/thortrends15.pdf.
- 17.Carder M., McNamee R., Turner S., Hodgson J., Holland F., Agius R. Time trends in the incidence of work-related mental ill-health and musculoskeletal disorders in the UK. Occup Environ Med. 2013;70:317–324. doi: 10.1136/oemed-2012-100904. [DOI] [PubMed] [Google Scholar]
- 18.Stocks S.J., Jones K., Piney M., Agius R.M. Isocyanate exposure and asthma in the UK vehicle repair industry. Occup Med (Lond) 2015;65:713–718. doi: 10.1093/occmed/kqv108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Urwin R., Warburton K., Carder M., Turner S., Agius R., Wilkinson S.M. Methylchloroisothiazolinone and methylisothiazolinone contact allergy: an occupational perspective. Contact Dermatitis. 2015;72:381–386. doi: 10.1111/cod.12379. [DOI] [PubMed] [Google Scholar]
- 20.Warburton K.L., Urwin R., Carder M., Turner S., Agius R., Wilkinson S.M. UK rates of occupational skin disease attributed to rubber accelerators, 1996-2012. Contact Dermatitis. 2015;72:305–311. doi: 10.1111/cod.12356. [DOI] [PubMed] [Google Scholar]
- 21.Stocks S.J., McNamee R., Turner S., Carder M., Agius R.M. The impact of national level interventions to improve hygiene on the incidence of irritant contact dermatitis in healthcare workers: changes in incidence from 1996-2012 and interrupted times series analysis. Br J Dermatol. 2015;173:165–171. doi: 10.1111/bjd.13719. [DOI] [PubMed] [Google Scholar]
- 22.Stocks S.J., McNamee R., Turner S., Carder M., Agius R.M. Assessing the impact of national level interventions on workplace respiratory disease in the UK: part 1—changes in workplace exposure legislation and market forces. Occup Environ Med. 2013;70:476–482. doi: 10.1136/oemed-2012-101123. [DOI] [PubMed] [Google Scholar]
- 23.Stocks S.J., McNamee R., Turner S., Carder M., Agius R.M. Assessing the impact of national level interventions on workplace respiratory disease in the UK: part 2—regulatory activity by the Health and Safety Executive. Occup Environ Med. 2013;70:483–490. doi: 10.1136/oemed-2012-101124. [DOI] [PubMed] [Google Scholar]
- 24.Turner S., McNamee R., Agius R., Wilkinson S.M., Carder M., Stocks S.J. Evaluating interventions aimed at reducing occupational exposure to latex and rubber glove allergens. Occup Environ Med. 2012;69:925–931. doi: 10.1136/oemed-2012-100754. [DOI] [PubMed] [Google Scholar]
- 25.Stocks S.J., McNamee R., Turner S., Carder M., Agius R. Has European Union legislation to reduce exposure to chromate in cement been effective in reducing the incidence of allergic contact dermatitis attributed to chromate in the UK? Occup Environ Med. 2012;69:150–152. doi: 10.1136/oemed-2011-100220. [DOI] [PubMed] [Google Scholar]
- 26.Stock S.J., McNamee R., van der Molen H.F., Paris C., Urban P., Campo G., Sauni R., Martínez Jarreta B., Valenty M., Godderis L., Miedinger D., Jacquetin P., Gravseth H.M., Bonneterre V., Telle-Lamberton M., Bensefa-Colas L., Faye S., Mylle G., Wannag A., Samant Y., Pal T., Scholz-Odermatt S., Papale A., Schouteden M., Colosio C., Mattioli S., Agius R., Working Group 2; Cost Action IS1002—Monitoring trends in Occupational Diseases and tracing new and Emerging Risks in a NETwork (MODERNET) Trends in incidence of occupational asthma, contact dermatitis, noise-induced hearing loss, carpal tunnel syndrome and upper limb musculoskeletal disorders in European countries from 2000 to 2012. Occup Environ Med. 2015;72:294–303. doi: 10.1136/oemed-2014-102534. [DOI] [PubMed] [Google Scholar]
- 27.O'Neill E., McNamee R., Agius R., Gittins M., Hussey L.J., Turner S. The validity and reliability of diagnoses of work-related mental ill-health. Occup Environ Med. 2008;65:726–731. doi: 10.1136/oem.2008.039008. [DOI] [PubMed] [Google Scholar]
- 28.Turner S., McNamee R., Roberts C., Bradshaw L., Curran A., Francis M., Fishwick D., Agius R. Agreement in diagnosing occupational asthma by occupational and respiratory physicians who report to surveillance schemes for work-related ill-health. Occup Environ Med. 2010;67:471–478. doi: 10.1136/oem.2008.044560. [DOI] [PubMed] [Google Scholar]
- 29.Hussey L., Turner S., Thorley K., McNamee R., Agius R.M. Work-related sickness absence as reported by general practitioners in the UK. Occup Med (Lond) 2012;62:105–111. doi: 10.1093/occmed/kqr205. [DOI] [PubMed] [Google Scholar]
- 30.Hussey L., Money A., Gittins M., Agius R. Has the fit note reduced general practice sickness certification rates? Occup Med (Lond) 2015;65:182–189. doi: 10.1093/occmed/kqu207. [DOI] [PubMed] [Google Scholar]
- 31.Money A., Hussey L., Thorley K., Turner S., Agius R. Work-related sickness absence negotiations: general practitioners' qualitative perspective. Br J Gen Pract. 2010;60:721–728. doi: 10.3399/bjgp10X532350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jarvis J., Seed M.J., Elton R., Sawyer L., Agius R. Relationship between chemical structure and the occupational asthma hazard of low molecular weight organic compounds. Occup Environ Med. 2005;62:243–250. doi: 10.1136/oem.2004.016402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kwok C., Money A., Carder M., Turner S., Agius R., Orton D., Wilkinson M. Occupational disease in Beauticians reported to The Health and Occupation Research (THOR) network from 1996 to 2011. Clin Exp Dermatol. 2014;39:590–595. doi: 10.1111/ced.12367. [DOI] [PubMed] [Google Scholar]
- 34.Jabbour R., Turner S., Hussey L., Page F., Agius R. Workplace injury data reported by occupational physicians and general practitioners. Occup Med (Lond) 2015;65:296–302. doi: 10.1093/occmed/kqv014. [DOI] [PubMed] [Google Scholar]
- 35.Turner S., Forman S.D., McNamee R., Wilkinson S.M., Agius R. Investigating work-related neoplasia associated with solar radiation. Occup Med (Lond) 2015;65:22–28. doi: 10.1093/occmed/kqu156. [DOI] [PubMed] [Google Scholar]
- 36.Van der Molen H.F., Stocks S.J., Frings-Dresen M.H.W. Exploring study designs for evaluation of interventions aimed to reduce occupational diseases and injuries. Saf Health Work. 2016;7:83–85. doi: 10.1016/j.shaw.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Money A., Carder M., Hussey L., Agius R.M. The utility of information collected by occupational disease monitoring systems. Occup Med (Lond) 2015;65:626–631. doi: 10.1093/occmed/kqv138. [DOI] [PubMed] [Google Scholar]
- 38.Health and Safety Executive. Statistical assessment of progress towards the Revitalising Health and Safety targets [Internet]. Health and Safety Executive. 2011. 9 p. [cited 2016 Jun 30]. Available from: http://www.hse.gov.uk/aboutus/meetings/hseboard/2011/230211/pfebb1113.pdf.
- 39.Health and Safety Executive. HSE statistics consultation response [Internet]. Health and Safety Executive. 2011. [cited 2016 Jun 30]. Available from: http://www.hse.gov.uk/statistics/about/engagement/consultation-response.pdf.