Abstract
Background: incidence of cardiovascular diseases in Saudi Arabia is growing and more patients are expected to have cardiac revascularization surgery. Optimal pharmacotherapy management with Guideline Directed Medical Therapy (GDMT) post coronary artery bypass grafting (CABG) plays an important role in the prevention of adverse cardiovascular outcomes. The objective of this study was to assess the utilization of GDMT for secondary prevention in CABG patients and determine whether specific patients' characteristics can influence GDMT utilization. Method: A retrospective chart review of patients discharged from the hospital after CABG surgery from April 2015 to April 2016. The primary outcome was the utilization of secondary prevention GDMT after CABG surgery - aspirin, B-blockers, statin and angiotensin-converting enzyme inhibitors (ACEI) (or angiotensin receptor blockers (ARB) in ACEI-intolerant patients). The proportions of eligible and ideal patients who received treatment were calculated, and mixed-effects logistic regression was used to estimate odds ratios (OR) for the association of age, gender or patient nationality with the use of GDMT. Results: A total number of 119 patients included in the analysis. The median age of the cohort was 57.3 ± 11 years, and 83% were male (83.2%). Nearly 69.7% of patients had diabetes, and 82% had a previous diagnosis of hypertension. Nearly 91% received aspirin therapy and the rate was lower for B-blocker and statin. The rate of GDMT utilization did not change with the change in patient’s age, gender or nationality. Conclusion: Despite adjustments for contraindications to GDMT, the rate of GDMT utilization was suboptimal.
Keywords: Guideline Directed Medical Therapy (GDMT), Coronary artery bypass grafting (CABG), Secondary prevention, Pharmacotherapy
1. Introduction
Coronary artery bypass grafting (CABG) is a recognized surgical procedure that improves survival in patients with significant left main coronary artery stenosis (>70% diameter) and in patients with multiple vessel disease (Hillis et al., 2012). Nearly, 400,000 patient undergo coronary artery revascularization surgeries each year in the United States (Writing Group Members et al., 2016, Hillis et al., 2012). Our center annually performs close to 400 open-heart procedures a year. Isolated CABG makes 50% of the caseload, CABG combined with other valve procedures 15%, valve repairs/replacements 30%, and 5% for other procedures such as aortic dissection and adult congenital.
However, coronary artery revascularization surgery restores the oxygen supply and the blood flow to the myocardium tissues as a result of bypassing the occluded arteries, and patients who have undergone CABG remain at risk for subsequent cardiovascular ischemic events. (Smith et al., 2011) Subsequent ischemic events can result from native coronary artery disease (CAD) progression and the development of vein graft atherosclerosis (Farooq et al., 2012, Smith et al., 2011). Thus, international guidelines recommend guideline directed medical therapy (GDMT) as the mainstay of pharmacological therapy for CABG patients to improve survival and reduce subsequent cardiovascular events in the absence of any contraindications or intolerance (Kolh et al., 2014, Kulik et al., 2015). GDMT for CABG patients includes antiplatelet therapy, high-intensity statin, beta-blockers (BB) and angiotensin-converting enzyme inhibitors (ACEI) (or angiotensin receptor blockers (ARB) in ACEI-intolerant patients) (Kolh et al., 2014, Kulik et al., 2015). Secondary prevention with GDMT plays a key role in the maintenance of native and graft vessel patency and in the prevention of adverse cardiovascular outcomes (The MACB Study Group, 1995, Knatterud et al., 2000, Oosterga et al., 2001, Mangano, 2002, Warnica et al., 2002). Studies reported 69% improvement in 2-year survival in patients taking half or more of indicated GDMT following discharge compared to patients taking 50% or less half of indicated GDMT in CABG patients (Post Coronary Artery Bypass Graft Trial Investigators, 1997, Goyal et al., 2007, Kulik et al., 2015).
Despite the strong evidence for secondary prevention in CABG patients, many studies have reported suboptimal use of GDMT following CABG (Bi et al., 2009, Goyal et al., 2007). In the United States, the use of antiplatelet agents and statins was high at discharge and at 1 year, but the use of beta-blockers and ACEi or ARBs was suboptimal (Goyal et al., 2007). In China, the utilization GDMT was reported (above 90% for aspirin, 70% for beta-blockers and ACEI, and 80% for statin) at the time of hospital discharge but decreased during follow-up (Bi et al., 2009). Despite the high incidence of CAD, and subsequent mortality and morbidity in Saudi Arabia, the utilization of GDMT after CABG for secondary prevention is unknown (Al-Nozha et al., 2004).
The aim of this study was to evaluate the utilization of GDMT for secondary prevention in CABG patients in Saudi Arabia. Furthermore, it will determine the association between patients' demographic data such as age, gender and nationality and the use of GDMT to provide clinicians with evidence to better guide management of CABG patients.
2. Method
2.1. Study population
After ethical approval from the office of institutional review board, we screened all patients discharged from the hospital after CABG surgery from April 2015 to April 2016. We excluded patients with any conditions in which the GDMT after CABG is contraindicated (due to complications from surgery or extended length of stay at the intensive care unit >9 days), or they had any missing data.
2.2. Outcome and data collection
In this study, data from the medical reports of the eligible patients were reviewed. The primary outcome was the utilization of secondary prevention GDMT after CABG surgery. We reviewed discharge prescriptions for each patient included in the study. GDMT was defined based on 2015 American Heart Association (AHA) secondary prevention after CABG guidelines published in 10 March 2015 and includes the following (Kulik et al., 2015):
-
•
Aspirin for all patients unless they are intolerant of or allergic to aspirin.
-
•
B-Blockers for all patients unless they have of the following bradycardia or severe reactive airway disease.
-
•
High-intensity statin therapy for all patients unless contraindicated.
-
•
ACEi or ARBs for patients with one or more of the following conditions: left ventricular ejection fraction < 40%, Diabetes Mellitus (DM), recent myocardial infarction, and/or chronic kidney disease unless the patients have hypotension, hyperkalemia, and worsening renal function.
The following data were reviewed in each patient’s medical report and the following data were collected including demographic information and past medical history (e.g., hypertension, diabetes mellitus, chronic kidney disease, left ventricle dysfunction and myocardial infarction). Date of the CABG surgery and discharge medications prescribed after CABG (e.g., Antiplatelet drug, statins, B-blockers ACEI and others) were also collected.
2.3. Analytical methods
We used descriptive statistics to describe demographic and clinical characteristics of the patients. Percentages and frequencies were used for the categorical variables, while means and standard deviations were calculated for the continuous variables. We used mixed-effects logistic regression to estimate odds ratios (OR) for the association of age, gender or patient nationality with the use of GDMT. The SPSS (version 22.0; SPSS Inc., Chicago, Illinois) was used for all analyses.
3. Results
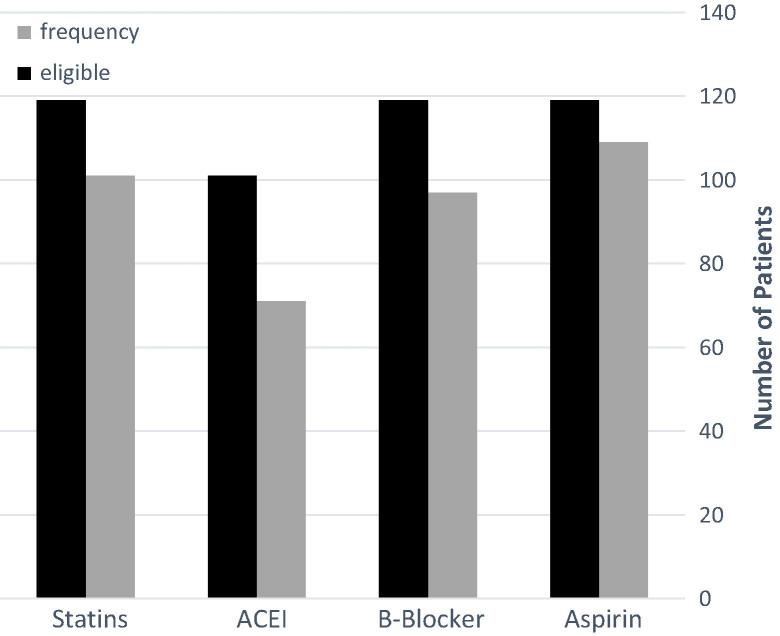
Of the 184 patients screened for the study, 119 (64%) patients met the inclusion criteria and included in the final assessment, and 65 patients were excluded (60% complications including prolonged intubation, infections and bleeding, 20% extended duration of stay and 20% different surgical procedures). The average age of the patients was 57.3 ± 11 years, most patients were male (83.2%) and the mean length of stay after the surgery was 9 days (Table 1). Approximately 69.7% of patients had diabetes, and nearly 82% had a previous diagnosis of hypertension. All patients included in the final assessment were eligible to receive aspirin, BB and statin after the surgery. Nearly 85% of the patients were eligible to receive ACE inhibitor or ARBs. At hospital discharge, rates of secondary prevention GDMT for use for candidate patients were suboptimal. The use of aspirin was 91%, β-blockers use was 81%, and statin therapy use was 84%. Notably, among eligible patients for ACE inhibitors or ARBs for mortality benefit (n = 101), the rate of use was low (70%; Fig. 1).
Table 1.
Characteristics of discharges of patients following heart revascularization surgery.
| Characteristics | (n = 119) |
|---|---|
| Age-Years | 57.3 (11) |
| Female Gender | 20 (16.8) |
| Nationality | |
| Saudi | 48 (40.3%) |
| Non-Saudi | 70 (59.6%) |
| Body Mass Index (kg/m2) | 27.4 (3) |
| Comorbidities: | |
| Diabetes | 83 (69.7%) |
| Hypertension | 98 (82.4%) |
| Hyperlipidemia | 89 (74.8) |
| Atrial Fibrillation | 24 (20%) |
| Prior Myocardial Infarction | 19 (16%) |
| Left Ventricular Ejection Fraction < 40% | 23 (19%) |
| Chronic Obstructive Pulmonary Disease | 12 (10.1%) |
| Tobacco Use | 36 (30.3%) |
| Chronic Kidney Disease | 36 (30.3%) |
| Exam/Laboratory Valuesa | |
| Blood Pressure (mmHg) | 132 (28) |
| Heart Rate (bpm) | 84 (18) |
| BUN (mg/dL) | 23 (16) |
| Creatinine Clearance (mL/min) | 82.8 (29.2) |
| Sodium (mEq/L) | 138 (5) |
| Potassium (mEq/L) | 4.1 (0.5) |
| Alanine Aminotransferase-ALT (U/L) | 47.2 (23.5) |
| Aspartate Aminotransferase-AST (U/L) | 34.7 (25.3) |
| Miscellaneous | |
| Post-op Stay – Days | 8 (6) |
| Intensive Care Time-Hours | 44.3 (31.5) |
Continuous variables are reported as mean (SD), and constant variables are reported as number (percentage).
Value reported at the day of discharge, or lowest value after the cardiac revascularization surgery.
Figure 1.
Rate of guidelines-directed medical therapy utilization after cardiac revascularization surgery.
In the multivariate regression model the rate of GDMT use for secondary prevention in CABG patients did not differ with change in patient’s demographics. The difference in the rate of aspirin use was not significant with age, gender nor nationality (p-value = 0.2, 0.3 and 0.9, respectively). Similarly, the difference in the rate of β-blockers, statin and ACE inhibitors or ARBs use was not significant with age, gender nor nationality. (Table 2).
Table 2.
Multivariate regression model the rate of GDMT use for secondary prevention in CABG.
| Factor | GDMT | OR | [95% CI] | p-value |
|---|---|---|---|---|
| Age | Aspirin | 0.97 | 0.25–3.65 | 0.2 |
| β-blockers | 0.97 | 0.71–5.52 | 0.2 | |
| Statin | 0.96 | 0.91–1.01 | 0.1 | |
| ACEI/ARBs | 1.01 | 0.97–1.04 | 0.9 | |
| Gender | Aspirin | 1.98 | 0.45–1.02 | 0.3 |
| β-blockers | 1.36 | 0.42–4.41 | 0.6 | |
| Statin | 1.79 | 0.54–5.98 | 0.3 | |
| ACEI/ARBs | 1.65 | 0.61–4.41 | 0.3 | |
| Nationality | Aspirin | 0.95 | 0.25–3.65 | 0.9 |
| β-blockers | 1.97 | 0.71–5.52 | 0.1 | |
| Statin | 1.21 | 0.88–3.41 | 0.6 | |
| ACEI/ARBs | 0.77 | 0.36–1.64 | 0.5 | |
4. Discussion
This is the first study in Saudi Arabia described the utilization of GDMT for secondary prevention in patients after coronary artery revascularization surgery. Moreover, it assessed the predictive factors of GDMT underutilization in CABG patients. Our findings showed that patients who underwent cardiac revascularization surgery are sub-optimally discharged on GDMT; for instance, 9% of CABG patients did not receive aspirin therapy, 19% did not receive B-blocker and 16% did not receive statin therapy. Additionally, among patients whom ACE inhibitors or ARBs are recommended (those with left ventricular ejection fraction < 40%, diabetes mellitus, recent myocardial infarction, and/or chronic kidney disease), only 70% have received the medication at discharge. Our findings failed to highlight any predictors of GDMT underutilization in CABG patients. Notably, advanced age did not significantly reduce the rate of GDMT use in CABG patients. Similarly, the rate of GDMT use was not associated with either patients’ gender or nationality.
Our study further reinforces current evidence for GDMT use by assessing a diverse cohort of patients commonly seen in practice. In addition, our study population has a large representation of Non-Saudi patient, and more male patients. Our findings regarding the rate of GDMT utilization in CABG patients for secondary prevention are concerning and show a significant group of patients did not receive the appropriate secondary prevention. The reasons for this underutilization are not known, as the rate of GDMT use did not change with different demographic characteristics, ruling out disparity in patient care based on age, gender or nationality. Our findings are similar with the data reported in a bigger registry of 2970 patients undergoing CABG surgery in the PREVENT IV trial (Goyal et al., 2007). At hospital discharge the rates of antiplatelet use were 95.59%, rate of b-blockers use was 88.8%, and lipid-lowering agents use was 83.9% (Goyal et al., 2007). Moreover, in the study only 46% of patients received ACE inhibitors or ARBs when recommended at discharge (Goyal et al., 2007).
As the incidence of cardiovascular diseases in Saudi Arabia is growing more patients are expected to have cardiac revascularization surgery. Optimal secondary prevention in patients undergoing cardiac revascularization surgery is an emerging area of interest and optimal pharmacotherapy management during hospital stay and after discharge remains yet to be challenging for healthcare providers. This study assessed utilization of GDMT practices can be the first step in targeting future interventions to improve the rate of utilization. As such, prospective national studies are needed to determine the national practice following heart surgery and to establish a ‘get with the guidelines’ initiatives to improve patient’s outcome and optimize pharmacotherapy secondary prevention.
This study has several limitations that should be addressed. First, the retrospective observational design limits the ability to determine cause and effect. Therefore, it is mostly hypothesis generating for further national studies. Second, the data obtained from a single center only therefore, the rate of pharmacotherapy secondary prevention utilization cannot be generalized to all patients following cardiac revascularization surgery.
5. Conclusion
The current practice of GDMT utilization for secondary prevention post cardiac revascularization surgery is suboptimal. No association was found between GDMT utilization and age, gender and nationality. Awareness of healthcare providers to the GDMT for secondary prevention in CABG patients is necessary to optimize the patients’ outcomes.
Acknowledgments
This project was supported by College of Pharmacy Research Centre, Deanship of Scientific Research, King Saud University.
Footnotes
Peer review under responsibility of King Saud University.
References
- Al-Nozha M.M. Coronary artery disease in Saudi Arabia. Saudi Med. J. 2004;25(9):1165–1171. [PubMed] [Google Scholar]
- Bi Y., Gao R., Patel A. Evidence-based medication use among Chinese patients with acute coronary syndromes at the time of hospital discharge and 1 year after hospitalization: results from the Clinical Pathways for Acute Coronary Syndromes in China (CPACS) study. Am. Heart J. 2009;157 doi: 10.1016/j.ahj.2008.09.026. 509,516.e1. [DOI] [PubMed] [Google Scholar]
- Farooq V., Serruys P.W., Bourantas C. Incidence and multivariable correlates of long-term mortality in patients treated with surgical or percutaneous revascularization in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial. Eur. Heart J. 2012;33:3105–3113. doi: 10.1093/eurheartj/ehs367. [DOI] [PubMed] [Google Scholar]
- Goyal A., Alexander J.H., Hafley G.E. Outcomes associated with the use of secondary prevention medications after coronary artery bypass graft surgery. Ann. Thorac. Surg. 2007;83:993–1001. doi: 10.1016/j.athoracsur.2006.10.046. [DOI] [PubMed] [Google Scholar]
- Hillis L.D., Smith P.K., Anderson J.L. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Thorac. Cardiovasc. Surg. 2012;143:4–34. doi: 10.1016/j.jtcvs.2011.10.015. [DOI] [PubMed] [Google Scholar]
- Kolh P., Windecker S., Alfonso F. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Eur. J. Cardiothorac. Surg. 2014;46:517–592. doi: 10.1093/ejcts/ezu366. [DOI] [PubMed] [Google Scholar]
- Kulik A., Ruel M., Jneid H. Secondary prevention after coronary artery bypass graft surgery: a scientific statement from the American Heart Association. Circulation. 2015;131:927–964. doi: 10.1161/CIR.0000000000000182. [DOI] [PubMed] [Google Scholar]
- Knatterud G.L., Rosenberg Y., Campeau L. Long-term effects on clinical outcomes of aggressive lowering of low-density lipoprotein cholesterol levels and low-dose anticoagulation in the post coronary artery bypass graft trial. Post CABG Investigat. Circulat. 2000;102:157–165. doi: 10.1161/01.cir.102.2.157. [DOI] [PubMed] [Google Scholar]
- Mangano D.T. Multicenter study of perioperative Ischemia Research group. Aspirin and mortality from coronary bypass surgery. N. Engl. J. Med. 2002;347:1309–1317. doi: 10.1056/NEJMoa020798. [DOI] [PubMed] [Google Scholar]
- Oosterga M., Voors A.A., Pinto Y.M. Effects of quinapril on clinical outcome after coronary artery bypass grafting (The QUO VADIS Study). QUinapril on Vascular Ace and Determinants of Ischemia. Am. J. Cardiol. 2001;87:542–546. doi: 10.1016/s0002-9149(00)01428-4. [DOI] [PubMed] [Google Scholar]
- Post Coronary Artery Bypass Graft Trial Investigators The effect of aggressive lowering of low-density lipoprotein cholesterol levels and low-dose anticoagulation on obstructive changes in saphenous-vein coronary-artery bypass grafts. N. Engl. J. Med. 1997;336:153–162. doi: 10.1056/NEJM199701163360301. [DOI] [PubMed] [Google Scholar]
- Smith S.C., Jr, Benjamin E.J., Bonow R.O. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J. Am. Coll. Cardiol. 2011;58:2432–2446. doi: 10.1016/j.jacc.2011.10.824. [DOI] [PubMed] [Google Scholar]
- The MACB Study Group Effect of metoprolol on death and cardiac events during a 2-year period after coronary artery bypass grafting. Eur. Heart J. 1995;16:1825–1832. [PubMed] [Google Scholar]
- Warnica J.W., Gilst W.V., Baillot R. Ischemia Management with Accupril post bypass Graft via Inhibition of angiotensin converting enzyme (IMAGINE): a multicentre randomized trial – design and rationale. Can. J. Cardiol. 2002;18:1191–1200. [PubMed] [Google Scholar]
- Writing Group Members, Mozaffarian D., Benjamin E.J. Executive summary: heart disease and stroke statistics – 2016 update: a report from the American heart association. Circulation. 2016;133:447–454. doi: 10.1161/CIR.0000000000000366. [DOI] [PubMed] [Google Scholar]