Abstract
Objective
A substantial percentage of children with congenital heart disease (CHD) fail to transfer to adult care, resulting in increased risk of morbidity and mortality. Transition planning discussions with a provider may increase rates of transfer, yet little is known about frequency and content of these discussions. We assessed prevalence and predictors of transition-related discussions between providers and parents of children with special healthcare needs (CSHCN) and heart problems, including CHD.
Design
Using parent-reported data on 12- to 17-year-olds from the 2009–2010 National Survey of CSHCN, we calculated adjusted prevalence ratios (aPR) for associations between demographic factors and provider discussions on shift to adult care, future insurance, and adult healthcare needs, weighted to generate population-based estimates.
Results
Of the 5.3% of adolescents with heart problems in our sample (n =724), 52.8% were female, 65.3% white, 62.2% privately insured, and 37.1% had medical homes. Less than 50% had parents who discussed with providers their child’s future health insurance (26.4%), shift to adult care (22.9%), and adult healthcare needs (49.0%). Transition planning did not differ between children with and without heart problems (aPR range: 1.0–1.1). Among parents of CSHCN with heart problems who did not have discussions, up to 66% desired one. Compared to 1-/13-year-olds, a larger percentage of 16-/17-year-olds had parents who discussed their shift to adult care (aPR 2.1, 95% confidence interval (CI) [1.1, 3.9]), and future insurance (aPR 1.8, 95% CI [1.1, 2.9]). Having a medical home was associated with discussing adult healthcare needs (aPR 1.5, 95% CI [1.2, 1.8]) and future insurance (aPR 1.8, 95% CI [1.3, 2.6]).
Conclusions
Nationally, less than half of adolescents with heart problems had parents who discussed their child’s transition with providers, which could be contributing to the large percentage of CHD patients who do not successfully transfer to adult care.
Keywords: Adolescent health services, cardiovascular disease, congenital heart defects, continuity of patient care, healthcare surveys, health services needs and demand
1 INTRODUCTION
Due to advances in medical diagnostics and treatment, 85%–90% of children with congenital heart disease (CHD) now survive to adulthood.1–3 However, individuals with CHD are never considered to be cured and require lifelong care for their condition, despite declines in morbidity and mortality.4 Continuity of care among patients with CHD has been a challenge as approximately 50% of adolescents with CHD fail to transfer to adult cardiac care and over 25% have no cardiac appointments after the age of 18 years.5 This observed lack of continuity of care into adulthood increases the risk of urgent cardiac intervention compared to those that remain in care.6 However, little information exists on the reasons why a large percentage of young adults with CHD or heart problems do not transfer to adult care.
Transition planning—the process by which healthcare providers give anticipatory guidance for the patient’s transfer to adult health care—is recommended by experts to improve rates of successful transfer to adult care.2,7–10 The few barriers to transfer that have been identified thus far include lack of knowledge regarding the importance of follow-up (even when feeling well), lack of insurability, and emotional attachment to the pediatric cardiologist;3,6,11 all concepts that providers should be addressing with their patients through transition planning.1,2,12–15 However, no studies have investigated the prevalence of transition planning among adolescents with CHD. Therefore, we used 2009–2010 National Survey for Children with Special Health Care Needs (NS-CSHCN) data to (1) examine national prevalence of transition planning among CSHCN ages 12–17 years with heart problems compared to CSHCN without and, (2) examine factors associated with transition planning for CSHCN with heart problems.
2 METHODS
2.1 National survey of children with special health care needs
We performed a cross-sectional study using data from the NS-CSHCN from July 2009 to March 2011. The NS-CSHCN is a population-based survey designed to estimate the prevalence of CSHCN and to describe their current care and medical service needs.16 Households with children under 18 years of age in all 50 states and the District of Columbia are identified by random-digit dial for the National Immunization Survey (NIS). To identify households eligible to participate in the NS-CSHCN, a parent or guardian of the household at least 18 years of age is asked immediately after the NIS, usually during the same phone call, a series of five questions about whether their child uses prescription medicine, has more healthcare encounters than other children their age, has limitations compared to other children their age, needs physical, occupational, or speech therapy, or has an emotional, developmental or behavioral problem in need of counseling or treatment. If the parent answers “yes” to one of the five questions above, then the parent is asked two additional questions on whether the specific health care need arises from a medical, behavioral, or other health condition and whether that condition has lasted or is expected to last 12 months or longer. If the parent answers “yes” to at least one of the five questions as well as the two additional questions, then the child is defined as having a special healthcare need and is eligible for inclusion in NS-CSHCN.
For each identified household with one or more CSHCN, a detailed computer-assisted telephone interview about one randomly selected CSHCN per household was completed by a parent or guardian knowledgeable about the child’s health and healthcare. Respondents were asked about their child’s health and functional status, coordination, access and utilization of care, and demographics. Sampling weights, which statistically account for sampling strategies, nonresponse, and noncoverage of households with age-eligible CSHCN, were applied to all survey responses, allowing for national estimates to be assessed from survey results. From July 2009 to March 2011, 196 309 households completed screening interviews (a weighted response rate of 64.3% for the screener among eligible identified households). Of screened households, 48 519 were identified as having at least one CSHCN and eligible for participation in NS-CSHCN. Of eligible households, 40 242 completed NS-CSHCN interviews (a weighted response rate of 80.8% for the interview among eligible identified households).10,16 Survey questions regarding transition planning were only asked of participating households with CSHCN between the ages of 12 and 17. Therefore, the study population for this analysis consisted of CSHCN between the ages of 12 and 17 with parents who completed a 2009–2010 NS-CSHCN interview. A more detailed description of the NS-CSHCN sampling and design can be found in the NS-CSHCN 2009–2010 Design and Operations Manual.16
2.2 Measures
CSHCN were considered to have heart problems if their parent answered “yes” to the following survey question: “Has a doctor or other healthcare provider ever told you that [CHILD] had a heart problem, including congenital heart disease?” The standard of transition planning has been broken down by the Maternal and Child Health Bureau (MCHB) into four components: “whether doctors had provided anticipatory guidance for the transition to adult healthcare” by discussing (1) the shift to adult providers if needed, (2) the child’s adult health care needs, and (3) the child’s health insurance as an adult, and (4) whether doctors usually or always encourage adolescents to take increasing responsibility for their care.10 The transition planning outcomes in this analysis were based on whether parents reported that these four MCHB components were met. To measure whether doctors provided anticipatory guidance, the following survey questions were asked of parents: (1) “Do any of [CHILD]’s doctors or other healthcare providers treat only children?” and if yes, “Have they talked with you about having [CHILD] eventually see doctors or other healthcare providers who treat adults?” (2) “Have [CHILD]’s doctors or other health-care providers talked with you about [his/her] healthcare needs as [he/she] becomes an adult?” and (3) “Has anyone discussed with you how to obtain or keep some type of health insurance coverage as [CHILD] becomes an adult?” To measure whether doctors were encouraging responsibility, the following survey questions was asked of parents: How often do [CHILD]’s doctors or other healthcare providers encourage [him/her] to take responsibility for [his/her] healthcare needs?” To assess the desire for anticipatory guidance noted in Questions 1–3 above, parents who responded “no” to any of these three questions were then asked: Would a discussion about [transition component 1, 2, or 3 accordingly] have been helpful for you?”
The child’s sex, age, race and ethnicity, federal poverty level, the impact of his or her special healthcare need on activities, number of comorbidities, health insurance, attendance at a well-child visit in the past 12 months, and having a medical home (“a source of ongoing, comprehensive, coordinated, family-centered care” measured in the survey using criteria specified by MCHB)10,17 were all assessed as potential predictors of having a transition-related discussion, based on literature review. Comorbidities were defined in this analysis as a parent reporting ever being told by a provider that their child has at least one of the following: attention deficit disorder or attention deficit hyperactivity disorder, depression, anxiety, behavioral or conduct problems, autism or an autism spectrum disorder, developmental delay, an intellectual disability or mental retardation, asthma, diabetes, epilepsy or seizure disorder, migraines or frequent headaches, blood problems, cystic fibrosis, cerebral palsy, muscular dystrophy, Down syndrome, arthritis or joint problems, allergies, and head injury, concussion or traumatic brain injury.
2.3 Data analysis
Weighted proportions were calculated for all sociodemographic and healthcare characteristics and transition-planning outcomes, stratified by heart problem status, and for parent’s desire for transition planning among CSHCN with heart problems. Chi-square tests were performed to examine all bivariate associations comparing individuals with and without heart problems. Multivariable logistic regression using the predicted marginal approach was performed to generate adjusted prevalence ratios (aPR).18 Two sets of multivariable models were used: the first set assessed associations between heart problem status and each transition-related outcome among all adolescent CSHCN, adjusting for all sociodemographic and healthcare characteristics; the second set assessed the associations between each sociodemographic or health-care variable and each transition-related outcome among adolescent CSHCN with heart problems, adjusting for all other sociodemographic and healthcare characteristics. The first model set was performed with and without stratification by age. All analyses were repeated excluding children with parent-report of Down syndrome; detailed results of these analyses are not reported.
All analyses were conducted using SAS-callable SUDAAN. Weights and design parameters were included to account for complex sampling and to produce nationally representative population-based estimates. Human subjects review was not required for this study since this was a secondary analysis of de-identified datasets.
3 RESULTS
There were 17 114 parents with CSHCN between 12 and 17 years of age who completed the 2009–2010 NS-CSHCN interview. Interviews with missing responses for pediatric heart problem status (n =15), any transition-related questions (n =494), or any of the potential predictors of transition-related discussions (n =1666) were excluded. A total of 14 939 (87%) parent-reported interviews were included in this analysis. Of these, 724 CSHCN with heart problems had parent-reported interviews, who were statistically weighted to represent approximately 210 000 CSHCN with heart problems nationally or 5.3% of all adolescent CSHCN in the United States.
Of included CSHCN with heart problems (hereafter referred to as “adolescents with heart problems”), 53% were female, 65.3% were non-Hispanic white, 21.1% were below 100% of the federal poverty level, and 37.8% had public insurance (Table 1). Compared to adolescents without heart problems, those with heart problems had more comorbidities but fewer special healthcare needs. Additionally, more adolescents with heart problems used prescription medicine for a lasting condition, had no medical home, and were seeing a provider that treats only children (P value for all <.05).
TABLE 1.
Characteristics of children with special healthcare needs ages 12–17 years with and without heart problems, National Survey for Children with Special Health Care Needs, United States, 2009–2010
| Parental report of a heart problem
|
P valuea | ||
|---|---|---|---|
| Yes N =724 Weighted %, 95% CI |
No N =14 215 Weighted %, 95% CI |
||
| Total | 5.3 (4.7, 6.1) | 94.7 (93.9, 95.3) | |
|
| |||
| Sex | .007 | ||
| Male | 47.2 (40.6, 53.9) | 57.0 (55.5, 58.5) | |
| Female | 52.8 (46.1, 59.4) | 43.1 (41.6, 44.5) | |
|
| |||
| Age (years) | .15 | ||
| 12–13 | 30.2 (24.5, 36.5) | 33.4 (32.0, 34.8) | |
| 14–15 | 29.1 (23.3, 35.6) | 32.7 (31.3, 34.1) | |
| 16–17 | 40.8 (34.3, 47.6) | 33.9 (32.5, 35.3) | |
|
| |||
| Race/ethnicity | .09 | ||
| White, NH | 65.3 (57.8, 72.0) | 66.3 (64.8, 67.8) | |
| Black, NH | 10.6 (7.3, 15.0) | 13.6 (12.6, 14.8) | |
| Hispanic | 19.5 (13.8, 27.6) | 13.0 (11.8, 14.3) | |
| Otherb | 4.7 (2.9, 7.7) | 7.1 (6.4, 7.8) | |
|
| |||
| Poverty statusc | .43 | ||
| <100% FPL | 21.1 (15.8, 27.6) | 18.3 (17.1, 19.5) | |
| 100%–199% FPL | 23.8 (17.8, 31.1) | 20.4 (19.2, 21.7) | |
| 200%–399% FPL | 26.1 (21.2, 31.8) | 29.6 (28.3, 30.9) | |
| ≥400% FPL | 29.0 (23.8, 34.8) | 31.8 (30.5, 33.1) | |
|
| |||
| Impact on activities | <.001 | ||
| None | 18.9 (14.7, 24.0) | 36.5 (35.1, 37.9) | |
| Moderate | 38.1 (31.9, 44.6) | 38.5 (37.1, 40.0) | |
| Great | 43.1 (36.4, 50.0) | 25.0 (23.7, 26.3) | |
|
| |||
| No. of comorbiditiesd | <.001 | ||
| 0 | 4.0 (2.6, 6.1) | 5.4 (4.8, 6.1) | |
| 1–2 | 32.6 (26.7, 39.2) | 47.4 (46.0, 48.9) | |
| 3 | 10.9 (8.1, 14.5) | 16.3 (15.2, 17.4) | |
| ≥4 | 52.5 (45.8, 59.1) | 30.9 (29.5, 32.3) | |
|
| |||
| Attended well-child visit in last 12 months | .97 | ||
| Yes | 90.0 (84.3, 93.8) | 89.9 (89.0, 90.7) | |
| No | 10.0 (6.3, 15.7) | 10.1 (9.3, 11.0) | |
|
| |||
| Medical homee | .03 | ||
| Yes | 37.1 (31.1, 43.4) | 44.5 (43.0, 45.9) | |
| No | 62.9 (56.6, 68.9) | 55.5 (54.1, 57.0) | |
|
| |||
| Insurance coverage | .15 | ||
| Any private | 62.2 (54.9, 69.0) | 67.8 (66.3, 69.2) | |
| Public | 37.8 (31.0, 45.1) | 32.2 (30.8, 33.7) | |
|
| |||
| Provider treats only children | .001 | ||
| Yes | 75.6 (69.3, 80.9) | 65.3 (63.9, 66.7) | |
| No/missing | 24.4 (19.1, 30.7) | 34.7 (33.3, 36.1) | |
|
| |||
| Special healthcare needsf | |||
| Needs medicine prescribed by a doctor | 84.1 (82.9, 85.2) | 77.2 (70.9, 82.5) | .03 |
| Needs more care than most children of same age | 44.0 (42.6, 45.5) | 63.2 (56.4, 69.5) | <.001 |
| Limited in ability to do things most children of same age do | 23.4 (22.1, 24.7) | 44.8 (38.1, 51.6) | <.001 |
| Needs special therapy | 14.9 (13.9, 16.0) | 25.9 (20.5, 32.1) | <.001 |
| Needs treatment or counseling | 36.1 (34.6, 37.5) | 40.4 (34.0, 47.2) | .21 |
|
| |||
| Number of special healthcare needs | <.001 | ||
| 1 | 46.0 (44.5, 47.4) | 30.2 (24.8, 36.3) | |
| 2 | 23.9 (22.6, 25.2) | 20.3 (15.0, 26.9) | |
| 3 | 16.0 (15.0, 17.1) | 24.6 (19.1, 31.0) | |
| 4 | 10.0 (9.1, 11.1) | 17.6 (12.9, 23.5) | |
| 5 | 4.1 (3.6, 4.7) | 7.4 (5.0, 10.8) | |
CI, confidence interval; CSHCN, children with special healthcare needs; FPL, federal poverty level; NH, non-Hispanic.
Chi square P value.
All other includes respondents identified as Asian, Alaskan Native, American Indian, Native Hawaiian, Pacific Islander, or mixed race.
Based on US Department of Health and Human Services poverty guidelines.
Comorbidities include attention deficit disorder or attention deficit hyperactivity disorder, depression, anxiety, behavioral or conduct problems, autism or an autism spectrum disorder, developmental delay, an intellectual disability or mental retardation, asthma, diabetes, epilepsy or seizure disorder, migraines or frequent headaches, blood problems, cystic fibrosis, cerebral palsy, muscular dystrophy, Down syndrome, arthritis or joint problems, allergies, and head injury, concussion or traumatic brain injury.
Meets Maternal and Child Health Bureau criteria for a medical home.
Special healthcare needs eligibility for the National Survey of Children with Special Health Care Needs is based on having one or more of the following five conditions: needing prescription medicine, having more healthcare encounters than other children their age, having limitations compared to other children their age, needing physical, occupational, or speech therapy, or having an emotional, developmental or behavioral problem in need of counseling or treatment. To be classified as special healthcare needs, these conditions must be related to a medical, behavioral, emotional, developmental, or other health condition that lasts or is expected to last 12 months or longer.
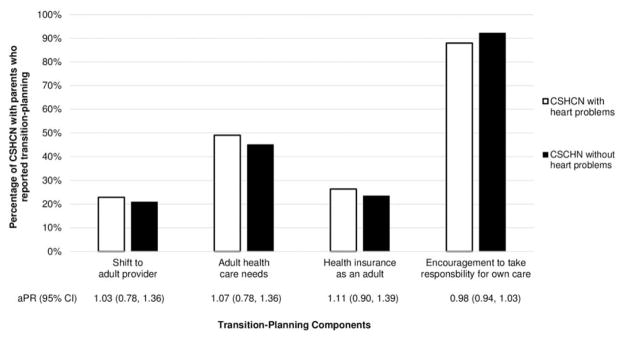
A quarter of adolescents with heart problems had parents who discussed with providers their child’s eventual need to shift to adult care and health insurance as an adult (Figure 1). Less than half of adolescents with heart problems had parents who discussed with providers their child’s healthcare needs as an adult. Less than 14% reported all three anticipatory guidance discussions. However, 88% of adolescents with heart problems had providers who encouraged them to take responsibility of their own healthcare. Both before and after adjusting for covariates, there were no statistically significant differences between prevalence estimates of transition-planning components for children with heart problems compared to those without heart problems. Observed associations did not change when stratified by age.
FIGURE 1.
Prevalence of transition planning among children with special healthcare needs (CSCHN), ages 12–17 years, with heart problems compared to those without heart problems, National Survey for Children with Special Health Care Needs, United States, 2009–2010. The prevalence of four transition-planning components among CSCHN ages 12–17 years stratified by presence of a heart problem and the respective adjusted prevalence ratios comparing children with special healthcare needs with heart problems to those without heart problems
Among adolescents with heart problems, factors associated independently with transition planning were age, having a medical home, and number of comorbidities (Table 2). About twice as many adolescents with heart problems in the oldest age group (16–17 years old) had parents who discussed their child’s shift to an adult healthcare provider (aPR =2.06, 95%CI [1.09, 3.89]) and future health insurance (aPR =1.80, 95% CI [1.14, 2.87]) compared to those in the youngest age group (12–13 years old). Among adolescents with heart problems, having a medical home was associated with a higher prevalence of discussions on adult healthcare needs (aPR =1.45, 95% CI [1.16, 1.81]) and health insurance as an adult (aPR =1.83, 95% CI [1.29, 2.59]). Compared to adolescents with heart problems but no comorbidities, adolescents with heart problems and one or two additional conditions were less likely to have parents who discussed shifting to an adult healthcare provider (aPR =0.38, 95% CI [0.20, 0.74]) and adult health care needs (aPR =0.73, 95% CI [0.55, 0.98]). Additionally, those with three comorbidities (aPR =0.59, 95% CI [0.40, 0.88]) and those with four or more comorbidities (aPR =0.62, 95% CI [0.45, 0.85]) were less likely to discuss adult healthcare needs compared to those with none. Discussions on health insurance as an adult were 1.79 (95% CI [1.08, 2.97]) times more prevalent among parents of non-Hispanic blacks than non-Hispanic whites. Discussions on adult healthcare needs were 1.44 (95%CI [1.01, 2.05]) times more prevalent among parents of adolescents with heart problems whose activities were greatly impacted by their special healthcare needs, compared to those with no impact. No other variables were associated with the four transition-planning components.
TABLE 2.
Associations between demographic characteristics and receipt of transition planning among children with special healthcare needs ages 12–17 years with heart problems, National Survey for Children with Special Health Care Needs, United States, 2009–2010
| Transition-planning discussions
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Discussed shift to adult providera
|
Discussed adult healthcare needs
|
Discussed health insurance as an adult
|
CSHCN usually/always encouraged to take responsibility
|
|||||
| Weighted %, 95% CI | aPR (CI) | Weighted %, 95% CI | aPR (CI) | Weighted %, 95% CI | aPR (CI) | Weighted %, 95% CI | aPR (CI) | |
| Sex | ||||||||
| Male | 22.3 (15.0, 31.8) | 1.0 | 54.0 (44.8, 63.0) | 1.0 | 28.3 (21.5, 36.2) | 1.0 | 92.4 (88.1, 95.3) | 1.0 |
| Female | 23.6 (16.1, 33.1) | 1.07 (0.68, 1.69) | 44.5 (35.2, 54.3) | 0.84 (0.65, 1.09) | 24.8 (17.1, 34.4) | 0.86 (0.59, 1.26) | 83.1 (71.4, 90.7) | 1.06 (0.97, 1.16) |
|
| ||||||||
| Age (years) | ||||||||
| 12–13 | 15.9 (9.1, 26.3) | 1.0 | 41.9 (31.2, 53.4) | 1.0 | 18.2 (11.5, 27.5) | 1.0 | 90.0 (82.8, 94.3) | 1.0 |
| 14–15 | 21.4 (12.0, 35.4) | 1.33 (0.66, 2.68) | 51.8 (39.2, 64.2) | 1.21 (0.87, 1.68) | 23.0 (15.2, 33.3) | 1.08 (0.61, 1.91) | 84.3 (65.5, 93.8) | 0.98 (0.90, 1.08) |
| 16–17 | 31.0 (21.4, 42.5) | 2.06 (1.09, 3.89) | 52.3 (41.6, 62.8) | 1.32 (0.97, 1.79) | 35.0 (25.4, 46.0) | 1.80 (1.14, 2.87) | 89.3 (81.7, 94.0) | 0.99 (0.91, 1.09) |
|
| ||||||||
| Race/ethnicity | ||||||||
| White, NH | 25.1 (18.7, 32.9) | 1.0 | 48.7 (41.6, 55.8) | 1.0 | 22.7 (17.8, 28.5) | 1.0 | 89.1 (84.3, 92.6) | 1.0 |
| Black, NH | 28.9 (12.2, 54.5) | 1.28 (0.57, 2.88) | 53.3 (35.1, 68.7) | 1.06 (0.70, 1.61) | 40.2 (23.6, 59.5) | 1.79 (1.08, 2.97) | 81.7 (64.5, 91.7) | 0.90 (0.73, 1.10) |
| Hispanic | 14.2 (5.6, 31.4) | 0.61 (0.22, 1.65) | 47.9 (27.8, 68.7) | 1.07 (0.69, 1.66) | 31.3 (15.4, 53.2) | 1.61 (0.95, 2.73) | 86.3 (52.2, 97.3) | 0.96 (0.83, 1.10) |
| Otherb | 14.7 (3.7, 43.4) | 0.58 (0.18, 1.82) | 48.4 (25.7, 71.8) | 1.14 (0.73, 1.79) | 27.6 (12.0, 51.7) | 1.35 (0.65, 2.87) | 94.7 (80.4, 98.7) | 1.08 (0.99, 1.17) |
|
| ||||||||
| Poverty status (%FPL)c | ||||||||
| <100 | 21.7 (10.3, 40.0) | 1.15 (0.40, 3.37) | 40.4 (26.4, 56.0) | 0.86 (0.51, 1.46) | 29.9 (17.9, 45.5) | 0.96 (0.46, 2.02) | 98.1 (95.9, 99.1) | 1.09 (1.00, 1.19) |
| 100–199 | 20.3 (10.9, 34.7) | 0.91 (0.42, 1.96) | 51.9 (35.2, 68.2) | 1.04 (0.72, 1.51) | 31.0 (17.8, 48.1) | 1.08 (0.53, 2.21) | 76.8 (56.2, 89.5) | 0.87 (0.74, 1.03) |
| 200–399 | 24.4 (14.9, 37.3) | 0.91 (0.42, 1.57) | 52.2 (41.3, 62.9) | 0.99 (0.75, 1.32) | 25.8 (17.8, 35.8) | 0.97 (0.63, 1.49) | 84.9 (75.1, 91.3) | 0.96 (0.86, 1.07) |
| ≥400 | 24.2 (15.2, 36.2) | 1.0 | 50.1 (39.8, 60.4) | 1.0 | 20.8 (14.5, 28.9) | 1.0 | 92.7 (86.4, 96.3) | 1.0 |
|
| ||||||||
| Impact on activities | ||||||||
| None | 19.3 (11.5, 30.6) | 1.0 | 44.8 (32.5, 57.7) | 1.0 | 22.2 (13.9, 33.5) | 1.0 | 94.6 (87.3, 97.8) | 1.0 |
| Moderate | 23.7 (15.0, 35.4) | 1.18 (0.65, 2.17) | 48.1 (38.0, 58.4) | 1.26 (0.89, 1.79) | 28.7 (19.8, 39.7) | 0.95 (0.57, 1.56) | 94.4 (86.4, 97.8) | 1.04 (0.95, 1.14) |
| Great | 23.6 (15.5, 34.2) | 1.42 (0.78, 2.56) | 51.7 (40.3, 62.9) | 1.44 (1.01, 2.05) | 26.3 (18.5, 36.0) | 0.87 (0.51, 1.48) | 79.5 (67.5, 87.9) | 0.91 (0.82, 1.01) |
|
| ||||||||
| No. of co-morbiditiesd | ||||||||
| 0 | 40.8 (21.7, 63.1) | 1.0 | 72.7 (51.8, 86.8) | 1.0 | 23.9 (10.6, 45.4) | 1.0 | 93.6 (73.0, 98.8) | 1.0 |
| 1–2 | 18.2 (10.2, 30.4) | 0.38 (0.20, 0.74) | 53.6 (41.8, 65.0) | 0.73 (0.55, 0.98) | 16.1 (10.3, 24.3) | 0.60 (0.26, 1.37) | 97.5 (91.5, 99.3) | 1.06 (0.94, 1.21) |
| 3 | 31.9 (18.6, 49.0) | 0.75 (0.37,1.50) | 44.9 (31.2, 59.4) | 0.59 (0.40, 0.88) | 34.7 (22.1, 49.9) | 1.59 (0.72, 3.51) | 80.6 (66.4, 89.7) | 0.87 (0.71, 1.05) |
| ≥4 | 22.6 (15.1, 32.6) | 0.56 (0.31, 1.02) | 45.3 (35.8, 55.2) | 0.62 (0.45, 0.85) | 31.3 (23.0, 41.1) | 1.43 (0.68, 3.01) | 83.3 (72.6, 90.4) | 0.92 (0.80, 1.06) |
|
| ||||||||
| Had well-child visite | ||||||||
| Yes | 22.2 (16.9, 28.7) | 0.74 (0.27, 2.03) | 49.3 (42.4, 56.3) | 1.16 (0.71, 1.88) | 26.8 (21.2, 33.3) | 1.06 (0.57, 2.01) | 88.0 (81.2, 92.5) | 1.06 (0.92, 1.22) |
| No | 29.8 (9.5, 63.2) | 1.0 | 46.3 (24.5, 69.7) | 1.0 | 23.2 (10.9, 42.8) | 1.0 | 88.5 (74.0, 95.4) | 1.0 |
|
| ||||||||
| Medical homef | ||||||||
| Yes | 28.9 (19.8, 40.1) | 1.46 (0.93, 2.30) | 60.0 (50.3, 69.0) | 1.45 (1.16, 1.81) | 31.4 (23.7, 40.3) | 1.83 (1.29, 2.59) | 91.3 (84.9, 95.1) | 1.02 (0.94, 1.11) |
| No | 19.4 (13.2, 27.6) | 1.0 | 42.6 (34.0, 51.5) | 1.0 | 23.5 (16.7, 32.0) | 1.0 | 86.1 (76.9, 92.1) | 1.0 |
|
| ||||||||
| Insurance coverage | ||||||||
| Any private | 24.8 (18.4, 32.6) | 1.0 | 51.0 (43.8, 58.1) | 1.0 | 22.6 (17.6, 28.4) | 1.0 | 88.5 (83.2, 92.3) | 1.0 |
| Public/none | 19.1 (10.6, 32.2) | 0.71 (0.30, 1.71) | 45.8 (33.3, 58.8) | 0.99 (0.68, 1.44) | 32.8 (22.0, 45.9) | 1.18 (0.68, 2.04) | 87.2 (71.4, 94.9) | 1.02 (0.92, 1.13) |
aPR: adjusted prevalence ratio, adjusted for sex, age, race/ethnicity, poverty status, impact on activities, number of comorbidities, attendance at a well-child visit in the last 12 months, having a medical home, and insurance coverage; CI, confidence interval; CSHCN, children with special healthcare needs; FPL, federal poverty level; NH, non-Hispanic.
Among CSHCN with heart problems whose providers do not also care for adults.
All other includes respondents identified as Asian, Alaskan Native, American Indian, Native Hawaiian, Pacific Islander, or mixed race.
Based on US Department of Health and Human Services poverty guidelines.
Comorbidities only include attention deficit disorder or attention deficit hyperactivity disorder, depression, anxiety, behavioral or conduct problems, autism or an autism spectrum disorder, developmental delay, an intellectual disability or mental retardation, asthma, diabetes, epilepsy or seizure disorder, migraines or frequent headaches, blood problems, cystic fibrosis, cerebral palsy, muscular dystrophy, Down syndrome, arthritis or joint problems, allergies, and head injury, concussion or traumatic brain injury.
Attended visit in last 12 months.
Meets Maternal and Child Health Bureau criteria for a medical home.
Among parents of adolescents with heart problems who did not discuss with a provider their child’s eventual shift to an adult care provider, adult healthcare needs, and/or health insurance as an adult, 42%, 64%, and 66% desired such a discussion, respectively. Results for all models did not change substantially after excluding from the analytic sample 140 CSHCN ages 12 to 17 with Down syndrome (62 with heart problems; 78 without heart problems).
4 DISCUSSION
Previous studies have confirmed that a large percentage of adolescents with CHD do not transfer to adult care. The results of our study suggest that failure to transfer might be secondary to inadequate transition planning and guidance from a provider. We found that up to 75% of adolescents with heart problems and their parents do not receive all four MCHB-established core components of transition planning, in spite of recent evidence that these discussions improve adolescents’ perceived readiness to transfer and perceived likelihood of transfer success19 and that CHD patients would prefer more information on longer-term implications of CHD and insurance prior to transition.20
Though no prior study has investigated the national prevalence of transition planning specifically among children with CHD or heart problems, studies based on the 2005–2006 and 2009–2010 NS-CSHCN reported similarly low prevalence of transition planning among all CSHCN ages 12–17 years.21,22 According to these analyses, approximately 40% of CSHCN met the core performance outcomes for transition, with 35% or less receiving discussions on upcoming changes in health insurance. Though not population based, a Canadian study assessing transition readiness among 82 adolescent CHD patients in a tertiary care setting found that 24% had not discussed transfer with a healthcare provider.23 In addition to the low prevalence of transition planning, and given recommendations for parental involvement in the transition process,1,13,24 the high percentage of CSHCN with parents desiring transition planning, ranging from 42% to 66% depending on the component, further emphasizes the need to prioritize transition planning within the routine healthcare of adolescents with CHD.
A primary goal of transition planning is to smooth the transfer from pediatric- to adult-oriented care, often from pediatricians to adult providers. Yet, among 69 pediatric cardiology centers in the United States and Europe, only one-third that transfer patients provide a structured preparation for patients and family.25 The American College of Cardiology/American Heart Association 2008 Guidelines for Adults with CHD recommends that a structured transition process should begin at the age of 12 years and that responsibility lies with the pediatric clinicians to ensure that young patients and their families are prepared for the transfer.2 It furthers states that important topics such as education on the cardiac defect, health maintenance and follow-up recommendations, vocational planning, and insurance information should be discussed in early childhood and repeatedly through adolescence and adulthood.2 By the age of 12 years, parents and their children should be introduced to a number of topics critical to the care, both present and future, of their defect. It may not be surprising that younger adolescents have not yet discussed all transition topics with their providers, given they might have just started the process. However, our results found that only a third to a half of parents of 16- to 17-year-olds reported discussing transition planning with their child’s provider, a group who should be nearing the end of the transition planning process. Additionally, a previous study found that almost 50% of children fell out of cardiac care before age 13 and another 60% by age 18.26 Therefore, discussing the transition process early and often, even with young adolescents, may help patients and their parents realize the need for continued care throughout adolescence and adulthood.2,26,27
By encouraging transition planning and preparation, the public health community attempts to prevent interrupted care and subsequent loss to follow up documented in young adult CHD survivors. Among a clinic-based cohort of CHD cases up to 22 years old in Quebec, 47% of those in care at the age of six years were lost to follow up after their 13th birthday, and 61% in care at 13 years old were lost to follow up after their 18th birthday.26 Other clinic-based studies in the United States of CHD patients 18 years and older have also observed that gaps in cardiac care are common.3,6 Gurvitz et al. estimated that 40% of their 922 study participants experienced more than a three year lapse of care, and the mean age at the beginning of lapse was 19.9 years old.3 Yeung et al. identified that 63% of their 158 participants experienced more than a two year lapse of care with the median duration of gap to be about 10 years. Those that experienced a lapse of care of at least two years were at higher risk of requiring urgent cardiac intervention compared to those without a lapse of care.6 Conversely, Mylotte et al. demonstrated that the referral and transfer of individuals with CHD into specialized adult CHD care is associated with a significant reduction in mortality.28 Given the importance of continued appropriate care for an individual’s specific healthcare needs and the substantial percentage of patients with CHD with interrupted care, improvement in the transition process, that is, discussing all four components of the MCHB transition planning guidance, and emphasis on regular follow-up throughout the lifespan are needed.
Current interventions are testing transition models or programs for transition planning in adolescent patient visits. Thus far, one Canadian study found that a brief nurse-led intervention improved cardiac knowledge and self-management of adolescents with CHD29; a similar study involving two sessions two months apart is underway.30 While the first CHD-specific trial and several other non-CHD trials31 found some improvement after implementing brief interventions, other studies have evaluated comprehensive transition programs that incorporate transition planning into the routine care of their patients throughout adolescence.32–34 Recommendations from transition interventions evaluated for other CSHCN include incorporating a structured multidisciplinary transition program, improving availability of resources, training, and staff, starting the transition process by ages 12–14, expanding the role in transition of nurse care managers, pediatricians, and adult clinicians, and offering incentives to providers for completing transition planning components.35–37 Our findings provide a baseline national estimate of the percentage of adolescents with CHD and their parents receiving transition planning by their provider, what subgroups of adolescents with CHD receive transition planning, and the desire by parents for transition planning for their children. As more centers implement successful transition planning interventions into their patient practice, these national estimates should be updated.
4.1 Limitations and strengths
There are some known limitations of this analysis. Missing data on completed surveys was minimal for the pediatric heart problems exposure (less than 1% missing) and the transition-planning outcomes (3% were missing at least one of the four transition questions), but a substantial number (10%) of interviews were missing data on a least one covariate. The data for this analysis were collected cross-sectionally, so these results cannot be used to assess causal relationships. Additionally, though the results are population based, they are only generalizable to children with heart problems who have special healthcare needs, rather than all children with heart problems. It should also be noted that the questions related to heart problems among children with special healthcare needs in the NS-CSHCN for 2009–2010 are not identical to those asked in the 2005–2006 or 2001 surveys and, therefore, the results of this study cannot be directly compared across the different data-collection time points.
The exposure for this study, pediatric heart problems, is heterogeneous (congenital, infectious, or trauma-related) and not specific to CHD type. Recommendations on the frequency and type of cardiac follow-up can vary by CHD severity.2 However, the majority of pediatric heart problems are likely congenital38 and the recommendations on transition process are universal across all types of CHD, regardless of whether they are transitioning to specialized adult CHD center or a general cardiologist.2 Additionally, we do not know if the child’s special healthcare need is related to his/her heart problem, one of the other 19 conditions defined as comorbidities in this analysis, or another condition not captured in the NSCSHCN.
Because these results are based on parent-reported data, it is possible that some parents may not recall a transition-related conversation or that some adolescents had transition discussions directly with their providers without a parent present. However, parents play an important role in the transition process,2,4,24 and parent report of their children’s medical care and history has frequently been reported as valid compared to provider documentation and medical records.39–44 The survey does not capture the type of provider(s) the child sees nor with whom the parents discussed transition-planning. However, any provider who sees children only should start discussing transition with the child’s parents early and often during adolescence. Our results suggest that gaps in transition planning exist regardless of what type and how many pediatric providers were visited. This study was able to examine transition planning discussions only and does not have information on whether the discussions increased rates of transfer for the individuals. Despite these limitations, this is one of the first population-based studies to examine the transitional experience in care for adolescents with heart problems. The results of these analyses only apply to adolescent CSHCN, but the population-based sampling frame and large sample size allow the estimates to be generalizable to adolescent CSHCN with heart problems nationally.
5 CONCLUSION
This analysis identified that, nationally, less than half of adolescents with heart problems had parents who discussed their child’s transition with providers, which could be contributing to the large percentage of CHD patients who do not successfully transfer to adult care. Health-care providers are encouraged to discuss transition planning with parents, and begin those discussions early, before lapses of care begin.1,45 Barriers to discussing transition may include time constraints in clinic, a lack of available or appropriate adult CHD resources for referral, or a lack of pediatric providers able to perform transition planning responsibilities. Research is needed to elucidate the barriers to transition planning and develop programs to overcome them.
Acknowledgments
Funding information
Internship/Research Participation Program
This project was supported in part by an appointment to the Intern-ship/Research Participation Program at the Centers for Disease Control, administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the US Department of Energy and EPA. We also thank Dr Ginnie Abarbanell for her review of the draft manuscript.
Footnotes
CONFLICTS OF INTERESTS
The authors have no conflicts of interest relevant to this article to disclose.
DISCLAIMER
The findings and conclusion in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
AUTHOR CONTRIBUTIONS
All authors read and approved the final version of the manuscript.
Conceptualized the study, carried out the initial analyses, drafted the manuscript: Downing
Conceptualized the study, critically reviewed and revised the manuscript: Oster
Conceptualized the study, refined the methods of analyses, contributed to the interpretation of the data, critically reviewed and revised the manuscript: Farr
References
- 1.Sable C, Foster E, Uzark K, et al. Best practices in managing transition to adulthood for adolescents with congenital heart disease: the transition process and medical and psychosocial issues: a scientific statement from the American Heart Association. Circulation. 2011;123(13):1454–1485. doi: 10.1161/CIR.0b013e3182107c56. [DOI] [PubMed] [Google Scholar]
- 2.Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American college of cardiology/American heart association task force on practice guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease) Circulation. 2008;118(23):e714–e833. doi: 10.1161/CIRCULATIONAHA.108.190690. [DOI] [PubMed] [Google Scholar]
- 3.Gurvitz M, Valente AM, Broberg C, et al. Prevalence and predictors of gaps in care among adult congenital heart disease patients: HEART-ACHD (The Health, Education, and Access Research Trial) J Am Coll Cardiol. 2013;61(21):2180–2184. doi: 10.1016/j.jacc.2013.02.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moceri P, Goossens E, Hascoet S, et al. From adolescents to adults with congenital heart disease: the role of transition. Eur J Pediatr. 2015;174(7):847–854. doi: 10.1007/s00431-015-2557-x. [DOI] [PubMed] [Google Scholar]
- 5.Goossens E, Stephani I, Hilderson D, et al. Transfer of adolescents with congenital heart disease from pediatric cardiology to adult health care: an analysis of transfer destinations. J Am Coll Cardiol. 2011;57(23):2368–2374. doi: 10.1016/j.jacc.2010.11.068. [DOI] [PubMed] [Google Scholar]
- 6.Yeung E, Kay J, Roosevelt GE, Brandon M, Yetman AT. Lapse of care as a predictor for morbidity in adults with congenital heart disease. Int J Cardiol. 2008;125(1):62–65. doi: 10.1016/j.ijcard.2007.02.023. [DOI] [PubMed] [Google Scholar]
- 7.Saidi A, Kovacs AH. Developing a transition program from pediatric-to adult-focused cardiology care: practical considerations. Congenit Heart Dis. 2009;4(4):204–215. doi: 10.1111/j.1747-0803.2009.00312.x. [DOI] [PubMed] [Google Scholar]
- 8.American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians-American Society of Internal Medicine. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110(6 Pt 2):1304–1306. [PubMed] [Google Scholar]
- 9.Foster E, Graham TP, Jr, Driscoll DJ, et al. Task force 2: special health care needs of adults with congenital heart disease. J Am Coll Cardiol. 2001;37(5):1176–1183. doi: 10.1016/s0735-1097(01)01277-3. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Department of Health and Human Services HRSA, Maternal and Child Health Bureau. The National Survey of Children with Special Health Care Needs Chartbook 2009–2010. Rockville, Maryland: U.S. Department of Health and Human Services; 2013. pp. 5–108. [Google Scholar]
- 11.Fernandes SM, Khairy P, Fishman L, et al. Referral patterns and perceived barriers to adult congenital heart disease care: results of a survey of U.S. pediatric cardiologists. J Am Coll Cardiol. 2012;60(23):2411–2418. doi: 10.1016/j.jacc.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 12.Jalkut MK, Allen PJ. Transition from pediatric to adult health care for adolescents with congenital heart disease: a review of the literature and clinical implications. Pediatr Nurs. 2009;35(6):381–387. [PubMed] [Google Scholar]
- 13.Higgins SS, Tong E. Transitioning adolescents with congenital heart disease into adult health care. Prog Cardiovasc Nurs. 2003;18(2):93–98. doi: 10.1111/j.1751-7117.2003.tb00310.x. [DOI] [PubMed] [Google Scholar]
- 14.Deanfield J, Thaulow E, Warnes C, et al. Management of grown up congenital heart disease. Eur Heart J. 2003;24(11):1035–1084. doi: 10.1016/s0195-668x(03)00131-3. [DOI] [PubMed] [Google Scholar]
- 15.Fernandes SM, Landzberg MJ. Transitioning the young adult with congenital heart disease for life-long medical care. Pediatr Clin North Am. 2004;51(6):1739–1748. doi: 10.1016/j.pcl.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 16.Bramlett MD, Blumberg SJ, Ormson AE, et al. Design and operation of the National Survey of Children with Special Health Care Needs, 2009–2010. National Center for Health Statistics. Vital Health Stat 1. 2014;(57):1–271. [PubMed] [Google Scholar]
- 17.U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. Child Health USA 2014. Rockville, Maryland: U.S. Department of Health and Human Services; 2015. pp. 93–4. Online at http://mchb.hrsa.gov/chusa14/ [Google Scholar]
- 18.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol. 2010;171(5):618–623. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- 19.Syverson EP, McCarter R, He J, D’angelo L, Tuchman LK. Adolescents’ perceptions of transition importance, readiness, and likelihood of future success: the role of anticipatory guidance. Clin Pediatr. 2016;55(11):1020–1025. doi: 10.1177/0009922816666882. [DOI] [PubMed] [Google Scholar]
- 20.Lopez KN, Karlsten M, Bonaduce De Nigris F, et al. Understanding Age-based Transition Needs: Perspectives from Adolescents and Adults with Congenital Heart Disease. Congenit Heart Dis. 2015;10(6):561–571. doi: 10.1111/chd.12283. [DOI] [PubMed] [Google Scholar]
- 21.Lotstein DS, Ghandour R, Cash A, McGuire E, Strickland B, Newacheck P. Planning for health care transitions: results from the 2005–2006 national survey of children with special health care needs. Pediatrics. 2009;123(1):e145–e52. doi: 10.1542/peds.2008-1298. [DOI] [PubMed] [Google Scholar]
- 22.McManus MA, Pollack LR, Cooley WC, et al. Current Status of Transition Preparation Among Youth With Special Needs in the United States. Pediatrics. 2013;131(6):1090–1097. doi: 10.1542/peds.2012-3050. [DOI] [PubMed] [Google Scholar]
- 23.Stewart KT, Chahal N, Kovacs AH, et al. Readiness for transition to adult health care for young adolescents with congenital heart disease. Pediatr Cardiol. 2017;38(4):778–786. doi: 10.1007/s00246-017-1580-2. [DOI] [PubMed] [Google Scholar]
- 24.McDonagh JE. Growing up and moving on: transition from pediatric to adult care. Pediatr Transplant. 2005;9(3):364–372. doi: 10.1111/j.1399-3046.2004.00287.x. [DOI] [PubMed] [Google Scholar]
- 25.Hilderson D, Saidi AS, Van Deyk K, et al. Attitude toward and current practice of transfer and transition of adolescents with congenital heart disease in the United States of America and Europe. Pediatr Cardiol. 2009;30(6):786–793. doi: 10.1007/s00246-009-9442-1. [DOI] [PubMed] [Google Scholar]
- 26.Mackie AS, Ionescu-Ittu R, Therrien J, Pilote L, Abrahamowicz M, Marelli AJ. Children and adults with congenital heart disease lost to follow-up: who and when? Circulation. 2009;120(4):302–309. doi: 10.1161/CIRCULATIONAHA.108.839464. [DOI] [PubMed] [Google Scholar]
- 27.Kovacs AH, McCrindle BW. So hard to say goodbye: transition from paediatric to adult cardiology care. Nat Rev Cardiol. 2014;11(1):51–62. doi: 10.1038/nrcardio.2013.172. [DOI] [PubMed] [Google Scholar]
- 28.Mylotte D, Pilote L, Ionescu-Ittu R, et al. Specialized adult congenital heart disease care: the impact of policy on mortality. Circulation. 2014;129(18):1804–1812. doi: 10.1161/CIRCULATIONAHA.113.005817. [DOI] [PubMed] [Google Scholar]
- 29.Mackie AS, Islam S, Magill-Evans J, et al. Healthcare transition for youth with heart disease: a clinical trial. Heart. 2014;100(14):1113–1118. doi: 10.1136/heartjnl-2014-305748. [DOI] [PubMed] [Google Scholar]
- 30.Mackie AS, Rempel GR, Kovacs AH, et al. A cluster randomized trial of a transition intervention for adolescents with congenital heart disease: rationale and design of the CHAPTER 2 study. BMC Cardiovasc Disord. 2016;16:127. doi: 10.1186/s12872-016-0307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Campbell F, Biggs K, Aldiss SK, et al. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst Rev. 2016;4:Cd009794. doi: 10.1002/14651858.CD009794.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grant C, Pan J. A comparison of five transition programmes for youth with chronic illness in Canada. Child Care Health Dev. 2011;37(6):815–820. doi: 10.1111/j.1365-2214.2011.01322.x. [DOI] [PubMed] [Google Scholar]
- 33.McManus M, White P, Barbour A, et al. Pediatric to adult transition: a quality improvement model for primary care. J Adolesc Health. 2015;56(1):73–78. doi: 10.1016/j.jadohealth.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 34.Ciccarelli MR, Brown MW, Gladstone EB, Woodward JF, Swigonski NL. Implementation and sustainability of statewide transition support services for youth with intellectual and physical disabilities. J Pediatr Rehabil Med. 2014;7(1):93–104. doi: 10.3233/PRM-140274. [DOI] [PubMed] [Google Scholar]
- 35.McManus M, White P, Pirtle R, Hancock C, Ablan M, Corona-Parra R. Incorporating the six core elements of health care transition into a Medicaid managed care plan: lessons learned from a pilot project. J Pediatr Nurs. 2015;30(5):700–713. doi: 10.1016/j.pedn.2015.05.029. [DOI] [PubMed] [Google Scholar]
- 36.Hergenroeder AC, Wiemann CM, Bowman VF. Lessons learned in building a hospital-wide transition program from pediatric to adult-based health care for youth with special health care needs (YSHCN) Int J Adolesc Med Health. 2016;28(4):455–458. doi: 10.1515/ijamh-2015-0048. [DOI] [PubMed] [Google Scholar]
- 37.Zhou H, Roberts P, Dhaliwal S, Della P. Transitioning adolescent and young adults with chronic disease and/or disabilities from paediatric to adult care services—an integrative review. J Clin Nurs. 2016;25(21–22):3113–3130. doi: 10.1111/jocn.13326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jacobs JP, Hess H. Pediatric and congenital heart disease. The Society of Thoracic Surgeons; 2012. [Accessed July 21, 2016]. Available at: http://www.sts.org/patient-information/what-pediatric-heart-disease. [Google Scholar]
- 39.Youngblade LM, Shenkman EA. Congruence between parents’ and adolescents’ reports of special health care needs in a Title XXI program. J Pediatr Psychol. 2003;28(6):393–401. doi: 10.1093/jpepsy/jsg029. [DOI] [PubMed] [Google Scholar]
- 40.Porter SC, Forbes P, Manzi S, Kalish LA. Patients providing the answers: narrowing the gap in data quality for emergency care. Qual Saf Health Care. 2010;19(5):e34. doi: 10.1136/qshc.2009.032540. [DOI] [PubMed] [Google Scholar]
- 41.Porter SC, Kohane IS, Goldmann DA. Parents as partners in obtaining the medication history. J Am Med Inform Assoc. 2005;12(3):299–305. doi: 10.1197/jamia.M1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Porter SC, Mandl KD. Data quality and the electronic medical record: a role for direct parental data entry. AMIA Annu Symp Proc. 1999:354–358. [PMC free article] [PubMed] [Google Scholar]
- 43.Porter SC, Silvia MT, Fleisher GR, Kohane IS, Homer CJ, Mandl KD. Parents as direct contributors to the medical record: validation of their electronic input. Ann Emerg Med. 2000;35(4):346–352. doi: 10.1016/s0196-0644(00)70052-7. [DOI] [PubMed] [Google Scholar]
- 44.Porter SC. Patients as experts: a collaborative performance support system. AMIA Annu Symp Proc. 2001:548–552. [PMC free article] [PubMed] [Google Scholar]
- 45.Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128(1):182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]