Abstract
The pharmacist’s role is expanding from medication dispensing to patient care. There are several newer horizons in which clinical pharmacists have a vital role to play such as diabetic care, handling asthma patients, pain management, anti-coagulation therapy and in hyperlipidemia. Among these, the disorder that is perceived to reach epidemic proportions globally is diabetes mellitus. In the Arab world, particularly in countries like Saudi Arabia, the number affected and the cost incurred in the management of diabetes are relatively high. Apart from adding to the economic burden, the complications arising due to a lag in identification and management are manifold. In developed countries, several practicing hospitals and clinics have inducted clinical pharmacists as vital members of the healthcare team. With profound knowledge about medications, clinical pharmacists are inclined to stay abreast with recent developments in research and latest guidelines, thus supporting physicians in evidence based practice. Clinical pharmacists through Medication Therapy Management can render services by guiding, identifying and monitoring drug related issues faced by the patients. This can contribute in reducing the prevalence of diabetes mellitus and improving the quality of life. To keep pace with the growing prevalence of diabetes in the kingdom, clinical pharmacists need to undergo specialized training in high risk areas. Health regulating bodies should be keen in adopting provisions of inducting them in discrete specialties which can also help in trimming heathcare expenditure.
1. Introduction
The world today has dynamically transformed from an agriculture based occupation into an industrialized work force resulting in tremendous rise in the per capita income. Dramatic improvement in the socioeconomic status has paved the way for torpid lifestyles and urbanized life experiences leading to environmental changes, stress and denouncement of native and healthy food habits. This has set an excellent backdrop for the emergence of metabolic disorders. Surprisingly, not just high income countries but low and middle income countries are also racing for a position on the scorecard with respect to the incidence of metabolic disorders. The most prominent disorder arising due to disruption of the metabolic machinery in the physiological system is diabetes mellitus (DM).
Improperly managed DM can induce major morbidities such as hypertension and dyslipidemia (Jouven et al., 2005). It can propel the occurrence of microvascular complications such as neuropathy, nephropathy and retinopathy. Inadequately controlled DM can induce vicious macrovascular complications such as coronary heart disease, ischemic stroke and peripheral vascular disease. In addition, lower leg amputation due to diabetic gangrene, diabetes associated blindness, kidney damage and periodontitis are the additional complications of DM. The risk of mortality due to cardiomyopathy and stroke is high in diabetics compared to non-diabetics (Geiss et al., 1995).
2. Global prevalence of diabetes mellitus & healthcare costs in Saudi Arabia
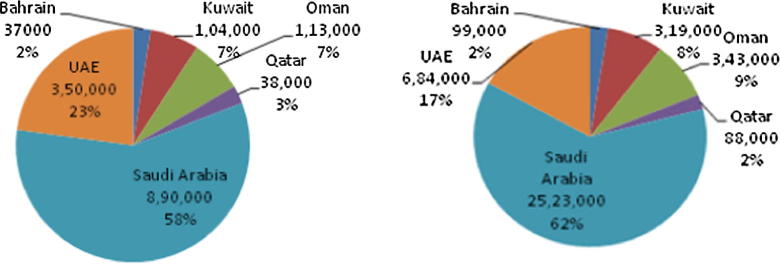
In 2011, the global prevalence of diabetes was 366 million people accounting for 6.3% of the adult population and predicted to exhibit an upward trend by 2030 (International Diabetes Federation, 2011). As per the American Diabetic association (ADA), one-third diabetics are prone to hospitalization two or more times per year (Jiang et al., 2003). The cost incurred in the management of DM is alarmingly high, with the US alone spending $92 billion in 2012 and is predicted to double by 2020. As per the WHO, the number of diabetic cases reported in the Kingdom of Saudi Arabia was significantly high compared to the rest of the Arab world. Nearly a million diabetic cases were reported in Saudi Arabia in year 2000 and are expected to rise to 2.5 million by 2030 (WHO, Diabetes Program) (Fig. 1). Prevalence of DM in Saudi Arabia was three times higher compared with the rest of the world (Al-Nozha et al., 2004, International Diabetes Federation, 2011). In a study conducted by Al-Daghri et al. (2011) on the Saudi population, it was found that type 2 diabetes mellitus (T2DM) was more rampant with a crude prevalence of 23.1%. The number of males having the disorder surpassed the females with an age-adjusted prevalence of 34.7% (Al-Daghri et al., 2011). Although diabetes in general is an age associated disorder, yet, this pattern is not replicated in the Saudi society. In addition, the rise in the aging population in Saudi Arabia can impact health outcomes and thereby enhance the chance of per capita disease rate (Khalid et al., 2011). By 2020, the estimated cost of managing diabetes would be $6.5 billion in Saudi Arabia requiring higher allocation of resources to meet the healthcare needs (Alhowaish, 2013). Expenditure incurred on health care in the kingdom was 9.3% in 2010 and perceived to escalate to 18.3% by 2030. Therefore, diabetes contributes significantly to the economic burden and also brings about a negative shift in productivity of the individual.
Figure 1.
Comparative assessment of the prevalence of diabetes mellitus in the year 2000 and 2030 in the Gulf region.
3. Role of clinical pharmacist-paradigm shift
Diabetes and associated complications need appropriate management; hence, the patient may be exposed to polypharmacy with medications being administered at different times and under different conditions. The patient might have to interact with multiple healthcare professionals to manage different complications of diabetes. Furthermore, diabetes being a crippling disorder, management with drugs alone cannot be the only solution but integration of multidisciplinary approaches such as modifying lifestyle, guidance pertaining to medication adherence and adverse effects monitoring need to be undertaken. Therefore, a concerted effort of the healthcare team will go a long way in managing diabetes. Unfortunately, this is easier said than done as patients have poor accessibility to the physician; lack knowledge of medications; and do not adhere to the course of therapy, further complicating the condition. Thus, the clinical pharmacist can serve as an excellent bridge between the physician and patients.
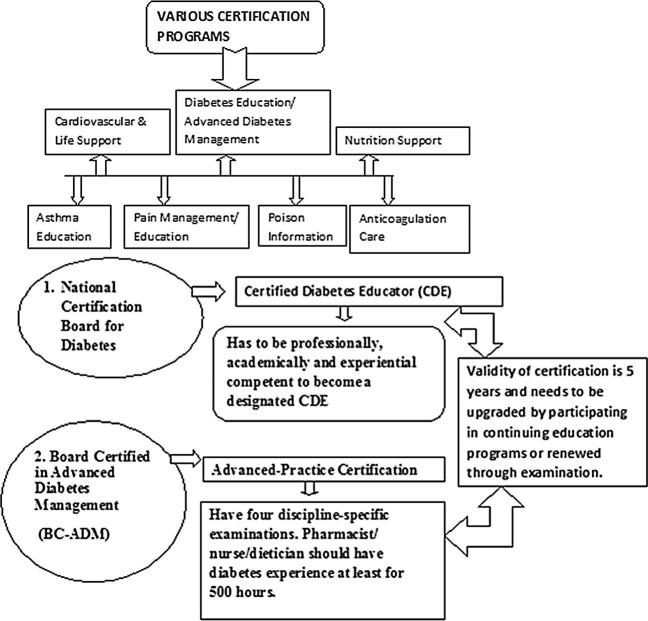
Traditionally, clinical pharmacists served more as medication dispensers; however, there is a paradigm shift in their role owing to their extensive clinical exposure. They are evolving as vital members of the healthcare team with additional professional training, education and certification in managing core primary care disorders such as diabetes, asthma, cardiovascular risk reduction, anti-coagulation therapy, osteoporosis, smoking cessation, pain management, and hyperlipidemia. During the course of specialized training in diabetic management, clinical pharmacist’s knowledge on diabetic disease advancement and its complications are revived (Fig. 2). Clinical pharmacists are trained to optimize lifestyles in diabetic patients as this is vital in foiling the progression of diabetes and the program tutelages them to educate patients in handling diabetes-related devices (Misita, 2013).
Figure 2.
Various certifications available for pharmacy professionals and types of diabetic certification.
4. Medication therapy management: clinical pharmacist as an asset
A wide array of medications are required to manage DM and its complications; thus, it requires Medication Therapy Management (MTM). MTM deals with the two R’s–the right dose and the right use of medications, in addition to, educating patients about side effects. Many boards regulating the profession of pharmacy the world over have approved Collaborative Drug Therapy Management (CDTM), wherein a clinical pharmacist enters into a collaborative practice agreement with the physician for providing appropriate patient care and delivering comprehensive medication management (CMM) to monitor and maximize medication benefits. The clinical pharmacist widens the purview of assessment by emphasizing on the entire regimen taken by the patient rather than focusing on a single medication. The American College of Clinical Pharmacy (ACCP) permits clinical pharmacists to make assessment and evaluation of medications required by the patient. In addition, the clinical pharmacist can modify or monitor the medication regimen (ACCP, 2013). Clinical pharmacists are readily accessible medication experts who through face time with the patient can comprehensively review various issues pertaining to the regimen and might personally or telephonically interact with the diabetic patients during the follow-up process. Thus clinical pharmacists with upgraded skills can play a pivotal role in emending clinical measures and patient outcomes thereby curtailing the progression of diabetes.
5. Managing medication related problems
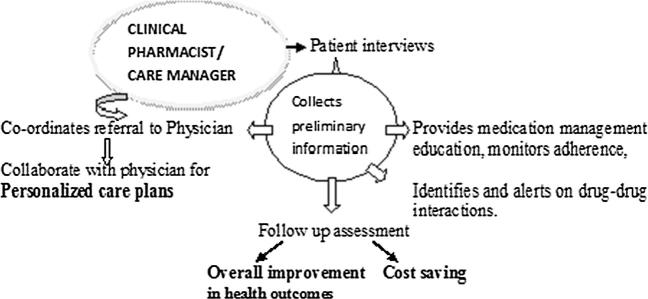
One area that needs to be viewed critically in diabetics is polypharmacy; wherein the clinical pharmacist can be of tremendous help. Multifarious medications can lead to Adverse Drug Reactions (ADRs) which favor discontinuation or non-adherence to medications and drug- drug interactions. Anon, 2005 has reported that patients with DM, hypertension and hypercholesteremia had twice the chance of being admitted to hospitals as they failed to conform to the medication pattern proposed by the physician (Anon, 2005). In some instances, patients cease to take medications against the advice given by the physician. This form of non-adherence ensues unintentionally due to lack of communication between patient and the physician. Patients may also defy the recommendations of the provider by taking medications at times not advised, missing out doses or taking more doses than actually required eventually non-conforming to the yardstick set forth by the physician. Often, there is scanty delivery of information to the patient as some physicians do not spend optimal time attending them or the lack of concordance between the physician and the patient could trigger non-adherence (Meichenbaum and Turk, 1987). Thus, errors occurring both during prescribing and by the end user of medications are on the rise. All these can exacerbate the diabetic condition, enhance the economic burden, produce a decline in quality of life, and most importantly risk frequent emergency hospital admission (Sullivan et al., 1990, Col et al., 1990). Thus with pronounced expertise and dedication, the clinical pharmacist can consolidate a position in diabetic clinics, interact with diabetic patients, monitor their drug regimen and thereby help in minimizing multiple problems. They can relate and coordinate with the physician thereby reducing their incidence. During follow-up visits, the pharmacist could track whether the patient’s attitude has transformed toward adherence and could schedule referrals to the physician if need be (Fig. 3).
Figure 3.
Key roles played by clinical pharmacists in diabetic clinics.
6. Ashville program-the beginning of an era
Several pilot scale-up programs have been set up by inducting clinical pharmacists into diabetic clinics and owing to improved patient outcomes they have been adopted on a larger scale. The initiative of assisting employees burdened with chronic diseases such as diabetes, hypertension, hyperlipidemia and asthma was undertaken in the 1990’s by two employers in city of Asheville, North Carolina- Municipal Government and Mission St. Joseph's Health System who inducted clinical pharmacist services for better patient care. Later on, the Asheville Project Diabetes Program was unveiled. Under the auspices of this program, employees would be assigned to a certified pharmacist care manager who would train and manage patients with diabetes. Employees utilizing the services of the clinical pharmacist recorded significant decline in the glycated hemoglobin values and lipid levels. Thus, the clinical pharmacist’s intervention in this program was acclaimed as it helped in restoring the productivity of individuals and reduced the cost of health care (Cranor et al., 2003). In 2009, University of North Carolina (UNC) Hospital’s endocrine clinic inducted the services of the clinical pharmacist to the extensive care team (Misita, 2013). Initially, the purpose of the clinical pharmacist was not clearly understood. Along with this, the physician felt that his autonomy could be threatened. However, clinical pharmacists undertook this responsibility with dedication spending 40 min sessions with each of these patients prior to their appointment with the physician. The competence they displayed in medication management has enabled them to be recognized as vital elements in the health care circuit. Clinical pharmacists have multifaceted role to play such as undertaking interim therapy visits wherein the clinical pharmacist interacts with patients several times in order to comprehend relevant modifications in the regimen in the best interests of the patient. These interactions also help in understanding patients’ perceptions of lifestyle modifications, patient practice toward therapy, and mode of monitoring blood glucose levels. The clinical pharmacist plays a pivotal role in encouraging adherence to medications by use of tools such as pill boxes and by streamlining schedules of drug dosing. Clinical pharmacists also educate patients about the importance of the daily dose of aspirin and help patients undergo testing for other vital issues related to diabetes least known to them such as low-density lipoproteins, microalbumin levels, eye and foot examination (Kiel and McCord, 2005, Scott et al., 2006). Clinical pharmacist along with other members of the healthcare team undertake several quality improvement initiatives as well as identify and ensure compliance with the pursuits laid down by the National Committee on Quality Assurance Diabetes Physician Recognition Program (Misita, 2013).
7. Scenario in Saudi Arabia
In Saudi hospitals, it was reported that pharmacists rendered services to patients by educating them on the use of medicines and counseled patients on high-risk medication or patients receiving a large number of medications (Al Asmary et al., 2013). However, an ASHP survey carried out in 2009 reflected that only 26% of patients had accessible drug monitoring services in Saudi Arabia (Pedersen et al., 2010, Alsultan et al., 2013). In terms of percentage, only 12% of integrated distributive-clinical pharmacists carried out drug monitoring activities in the kingdom which was relatively lower than the US. The prevalence of T2DM is perceived to soar in the Saudi population in the future requiring urgent primary prevention (Alqurashi et al., 2011). Precautionary and novel healthcare schemes need to be implemented and the services of the clinical pharmacist has to be focused to facilitate medication management, lifestyle coaching, dietary education, and conduct foot and eye care programs to prevent aggravation of T2DM.
8. Clinical pharmacist-an indispensible member: clinical evidence
It has been reinforced through several studies that clinical pharmacists are indispensible members of the healthcare team. A retrospective study examining the role of clinical pharmacists handling T2DM patients in diabetic care clinics found that their participation helped in achieving the desired treatment goals; in addition, they enabled early detection of DM in high risk population (Morello et al., 2006). Meta-analyses revealed that engaging clinical pharmacists in the healthcare setup had a favorable response with a 0.76% reduction in levels of glycated hemoglobin and an overall improvement in the quality of life (Chisholm-Burns et al., 2010). Randomized trial conducted in Canada delineated the services of clinical pharmacist in the primary care team. The results were beneficial with a significant reduction in co-morbidities such as hypertension in diabetic patients (Simpson et al., 2011). It has also been evidenced through another randomized controlled trial that clinical pharmacist’s intervention in outpatient diabetic clinics led to significant reduction in glycated hemoglobin levels in 6 months compared with patients in usual care (Jarab et al., 2012). In a recent randomized controlled trial conducted on a Malaysian population, it was found that the pharmacists’ intervention in the management of diabetic patients led to better quality of care with a decline in the HbA1c levels (Butt et al., 2016).
Apart from the medication management process, the clinical pharmacist can render educational programs for better self management of diabetes. Through this, the clinical pharmacists conduct motivational interviews enabling the respondent to set goals for disease management. Self management support has proved to provide promising results in reducing the complications of DM. With the advent and explosion of digital technology, the patient could upload essential information to obtain guidance from the pharmacist. Healthcare teams can telemonitor patients who find it difficult to reach the primary care setting. In addition, the clinical pharmacist can host educational programs which can be easily accessed by the patients.
9. Conclusion
In conclusion, DM has now become a medical and a national priority owing to the escalating numbers affected with it. With intimate knowledge about medications, the clinical pharmacist can make a comparative evaluation of medications based on current surveys, establish healthy interaction with physicians, extract valuable information from the patients and ensure protocol adherence. The multitasking of clinical pharmacists can ensure that they would be recognized and rewarded as vital members of the healthcare team. Extending diabetic services to ‘home based care’ could be another horizon for employment and recognition of clinical pharmacists. In countries imbibing the western structure of education and training like Saudi Arabia, the concept of inducting clinical pharmacists into specialized areas of practice such as in diabetic clinics can maximize therapeutic efficacy, better patient care and can serve as a useful measure to contain the national expenditure incurred in managing this disorder.
Footnotes
Peer review under responsibility of King Saud University.
References
- Al-Nozha M.M., Al-Maatouq M.A., Al-Mazrou Y.Y., Al-Harthi S.S., Arafah M.R., Khalil M.Z. Diabetes mellitus in Saudi Arabia. Saudi Med. J. 2004;25:1603–1610. [PubMed] [Google Scholar]
- Anon Poor medication adherence increases healthcare costs. PharmacoEcon. Outcomes News. 2005;480:5. [Google Scholar]
- Al-Daghri N.M., Al-Attas O.S., Alokail M.S., Alkharfy K.M., Yousef M., Sabico S.L., Chrousos G.P. Diabetes mellitus type 2 and other chronic non-communicable diseases in the central region, Saudi Arabia (Riyadh cohort 2): a decade of an epidemic. BMC Med. 2011;20(9):76. doi: 10.1186/1741-7015-9-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alqurashi K.A., Aljabri K.S., Bokhari S.A. Prevalence of diabetes mellitus in a Saudi community. Ann. Saudi Med. 2011;31(1):19–23. doi: 10.4103/0256-4947.75773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhowaish A.K. Economic costs of diabetes in Saudi Arabia. J. Family Commun. Med. 2013;20(1):1–7. doi: 10.4103/2230-8229.108174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Asmary S.M., Al-Harbi T., Tourkmani A.M., Al Khashan H.I., Al-Qahtani H., Mishriky A. Impact of integrated care program on glycemic control and cardiovascular risk in adult patients with type 2 diabetes. JCOM. 2013;20(8):356–363. [Google Scholar]
- Alsultan M.S., Mayet A.Y., Khurshid F., Al-jedai A.H. Hospital pharmacy practice in Saudi Arabia: drug monitoring and patient education in the Riyadh region. Saudi Pharm. J. 2013;21(4):361–370. doi: 10.1016/j.jsps.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College of Clinical Pharmacy (ACCP) Board of Regents commentary. Qualifications of pharmacists who provide direct patient care: perspectives on the need for residency training and board certification. Pharmacotherapy. 2013;33:888–891. doi: 10.1002/phar.1285. [DOI] [PubMed] [Google Scholar]
- Butt M., Ali A.M., Bakry M.M., Mustafa N. Impact of pharmacist led diabetes mellitus intervention on HbA1c, medication adherence and quality of life: a randomized control study. Saudi Pharm. J. 2016;24:40–48. doi: 10.1016/j.jsps.2015.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Col N., Fanale J.E., Kronholm P. The role of medication noncompliance and adverse drug reactions in hospitalizations of the elderly. Arch. Intern. Med. 1990;150(4):841–845. [PubMed] [Google Scholar]
- Cranor C.W., Bunting B.A., Christensen D.B. The Asheville Project: long-tem clinical and economic outcomes of a community pharmacy diabetes care program. J. Am. Pharm. Assoc. (Wash) 2003;43:173–184. doi: 10.1331/108658003321480713. [DOI] [PubMed] [Google Scholar]
- Chisholm-Burns M.A., Kim Lee J., Spivey C.A., Slack M., Herrier R.N., Hall-Lipsy E. U.S. pharmacists’ effect as team members on patient care: systematic review and meta-analyses. Med. Care. 2010;48:923–933. doi: 10.1097/MLR.0b013e3181e57962. [DOI] [PubMed] [Google Scholar]
- Geiss, L.S., Herman, W.H., Smith, P.J., 1995. Mortality in non-insulin-dependent diabetes. In: Harris, M.I., Cowie, C.C., Stern, M.P., et al. (Eds.), Diabetes in America, second ed. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD. pp. 233–257 (NIH publication 95-1468).
- Global burden of diabetes. International Diabetes Federation. Diabetic atlas, fifth ed. 2011, Brussels. Available at <http://www.idf.org/diabetes atlas> (accessed 5th September 2016).
- Jiang H.J., Stryer D., Friedman B., Andrews R. Multiple hospitalizations for patients with diabetes. Diabetes Care. 2003;26(5):1421–1426. doi: 10.2337/diacare.26.5.1421. [DOI] [PubMed] [Google Scholar]
- Jouven X., Lemaitre R.N., Rea T.D., Sotoodehnia N., Empana J.P., Siscovick D.S. Diabetes, glucose level, and risk of sudden cardiac death. Eur. Heart J. 2005;26(20):2142–2147. doi: 10.1093/eurheartj/ehi376. [DOI] [PubMed] [Google Scholar]
- Jarab A.S., Alqudah S.G., Mukattash T.L., Shattat G., Al-Qirim T. Randomized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in Jordan. J. Manage. Care Pharm. 2012;18(7):516–526. doi: 10.18553/jmcp.2012.18.7.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiel P.J., McCord A.D. Pharmacist impact on clinical outcomes in a diabetes disease management program via collaborative practice. Ann. Pharmacother. 2005;39(11):1828–1832. doi: 10.1345/aph.1G356. [DOI] [PubMed] [Google Scholar]
- Khalid A., Khalid S.A., Bokhari Samia A. Prevalence of diabetes mellitus in a Saudi community. Ann. Saudi Med. 2011;31(1):19–23. doi: 10.4103/0256-4947.75773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meichenbaum D., Turk D.C. Plenum Publishing Corp; New York: 1987. Facilitating Treatment Adherence: A Practitioner’s Guidebook. [Google Scholar]
- Morello C.M., Zadvorny E.B., Cording M.A., Suemoto R.T., Skog J., Harari A. Development and clinical outcomes of pharmacist-managed diabetes care clinics. Am. J. Health-Syst. Pharm. 2006;63(14):1325–1331. doi: 10.2146/ajhp050430. [DOI] [PubMed] [Google Scholar]
- Misita C.P. Clinical pharmacists in outpatient diabetes care: essential members of the multidisciplinary team. Clin. Diabetes. 2013;31(4):162–165. [Google Scholar]
- Pedersen C.A., Schneider P.J., Scheckelhoff D.J. ASHP national survey of pharmacy practice in hospital settings: monitoring and patient education–2009. Am. J. Health-Syst. Pharm. 2010;67:542–558. doi: 10.2146/ajhp090596. [DOI] [PubMed] [Google Scholar]
- Sullivan S., Kreling D., Hazlet T. Noncompliance with medication regimens and subsequent hospitalizations: a literature analysis and cost of hospitalization estimate. J. Res. Pharmaceut. Econ. 1990;2:19–33. [Google Scholar]
- Scott D.M., Boyd S.T., Stephan M., Augustine S.C., Reardon T.P. Outcomes of pharmacist-managed diabetes care services in a community health centre. Am. J. Health Syst. Pharm. 2006;63(21):2116–2122. doi: 10.2146/ajhp060040. [DOI] [PubMed] [Google Scholar]
- Simpson S.H., Majumdar S.R., Tsuyuki R.T., Lewanczuk R.Z., Spooner R., Johnson J.A. Effect of adding pharmacists to primary care teams on blood pressure control in patients with type 2 diabetes: a randomized controlled trial. Diabetes Care. 2011;34(1):20–26. doi: 10.2337/dc10-1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO report: diabetes programme: country and regional data on diabetes. <http://www.who.int/diabetes/facts/world_figures/en/index2.html> (accessed on 15-09-2016).