Abstract
Background
Individuals involved in antisocial behavior often engage in excessive reward-driven behavior even in the face of severe punishments including incarceration. However, the neural mechanisms of reward processing in antisocial behavior have not been examined while considering the heterogeneity of antisocial behavior and specific phases of reward and loss processing. In this study, we investigate the relationship between antisocial behavior, callous-unemotional traits, and neural activity during the anticipation and receipt of rewards and losses.
Methods
A community sample of 144 low income, racially diverse, urban males at risk for antisocial behavior completed self-report measures, a clinical interview, and an fMRI scan at age 20. Neural response during the anticipation and receipt of monetary rewards and losses was linked to antisocial behavior and callous-unemotional traits using a priori ventral striatum region of interest analyses and exploratory whole brain analyses.
Results
Antisocial behavior, but not callous-unemotional traits, was related to less ventral striatum response during reward anticipation. There were no significant relationships between neural reactivity and antisocial behavior or callous-unemotional traits during reward or loss outcomes. Antisocial behavior was also related to less ventrolateral prefrontal cortex reactivity during reward and loss anticipation.
Conclusions
These findings support a hypo-reactivity model of reward and loss anticipation in antisocial behavior. Lower striatal reactivity to cues of reward and lower prefrontal-regulatory recruitment during reward and loss anticipation may contribute to maladaptive reward-related behavior found in antisocial behavior.
Keywords: Reward, Loss, fMRI, Antisocial Behavior, Ventral Striatum, Callous-Unemotional
Introduction
Antisocial behavior (AB), which includes aggression and rule breaking, is the cornerstone of the diagnoses of Conduct Disorder (CD) in youth and Antisocial Personality Disorder (APD) in adults (1). AB is an important public health concern because of the large financial and emotional costs to perpetrators, victims, and society (2). Recently, neuroimaging research has focused on connecting emotional deficits seen in AB, such as abnormal fear processing, to altered function in limbic and prefrontal neurocircuitry (3, 4). However, individuals high on AB also show marked behavioral differences in response to reward (5). For example, they perseverate on previously rewarded, but now punished behaviors, engage in greater risk taking, and are less sensitive to punishments and losses (5–9). Improved understanding of the neural bases of these behavioral deficits is key to understanding the etiology of AB and informing biologically-based assessment and treatment.
Reward Processing in AB
The few studies investigating reward-related neural activity in relation to AB focus on the ventral striatum (VS), a region active during reward evaluation, anticipation, and receipt (10). These studies have yielded conflicting results: Two studies have linked AB to greater reward-related VS reactivity in youth (11) and healthy adults (12), consistent with studies of substance abusers who show neural hyper-sensitivity to highly valued rewards (i.e., drug cues)(13–15). These studies suggest that individuals high on externalizing/AB may be hyper-sensitive to rewards leading to reward dominant behavior. Conversely, two other studies have linked AB to less reward reactivity in youth with persistent disruptive behavior disorders (16) and in undergraduates (17). This pattern of hyporeactivity to rewards parallels the lower VS reactivity found in those with ADHD (18, 19) and in substance users when responding to non-drug rewards. This pattern is hypothesized to drive maladaptive reward seeking behavior via attempts to “normalize” reward-related neural reactivity by pursuing progressively more intense rewards (20–22). Based on the conflicting findings for AB, research is needed to identify the extent to which those engaged in AB may be better characterized by hyper- versus hypo-sensitivity to highly valued cues (i.e., monetary reward).
One potential explanation for the heterogeneity of findings of reward-related neural functioning in AB may be the failure of previous studies to discriminate between phases of reward and loss processing. Human and animal research demonstrates that reward anticipation and receipt have dissociable neural networks (14, 23), and may be differentially implicated in AB and externalizing disorders (11, 12, 16). Thus, neuroimaging studies of AB are needed that discriminate between anticipation and receipt of reward.
Beyond reward-related reactivity in the VS, a broader literature on decision-making and learning suggests that AB is linked to dysfunction in prefrontal regions during tasks that tap emotion regulation, affective decision-making, and learning (i.e., OFC/vmPFC; 24, 25–28), as well as affective responses to reward (i.e., vlPFC; 29, 30). In Blair’s model of AB, impairment in prefrontal functioning that leads to deficits in cognitive control and reward-dominant behavior is central to the etiology of broad disinhibited externalizing behaviors including AB, ADHD, and substance use (31). These studies and theoretical models suggest that beyond the VS, reward-related processing is likely to elicit AB-related differences in medial and lateral prefrontal cortex (32).
Dimensions of AB
Beyond the need to separately examine phases of reward, little existing research has examined whether reward-related neural activity may differentiate different types of AB (12, 17). Research examining dimensions of AB and the CU traits prominent in adult psychopaths and youth diagnosed with the DSM-5 “limited prosocial emotions” specifier to CD (1), has demonstrated divergent relationships between AB, CU traits, and emotion-related amygdala reactivity (33, 34). These studies suggest that dimensions of AB and CU traits should be examined separately in relation to neural reactivity. In one of the few studies parsing AB versus CU trait dimensions in relation to reward-related neural reactivity, we have shown that antisocial, but not callous-unemotional, components of psychopathy were associated with reduced reward-related VS reactivity (17). However, this study used a sample of healthy college students, highlighting the need for studies of those with a greater range of AB.
Current Study
The current study aims to elucidate the reward-related neural underpinnings of AB in a diverse community sample enriched for AB by sampling young men who were raised in low-income, urban environments. We examine the impact of the phase of reward (i.e., anticipation versus receipt/outcome) on the association between neural reactivity and AB, while leveraging multi-method assessment of AB through self-report, diagnostic interview, and official report, as well as self-reports of CU traits. Finally, we examine these questions at the transition to adulthood when serious AB peaks, and when youth transition to more independence and the adult legal system.
Based on previous findings (5), we hypothesized that AB would be related to greater VS reactivity during reward anticipation, but not reward outcome. Because of the lack of concern about performance that often characterizes individuals high on CU traits (1), we hypothesized that CU traits would be related to decreased VS reactivity during reward outcome, reflecting reduced sensitivity to the receipt of rewards.
Methods and Materials
Participants
Participants are part of the Pitt Mother & Child Project, an ongoing longitudinal study of 310 low-income boys and their families recruited in 1991 and 1992 from Allegheny County Women, Infant and Children Nutritional Supplement Clinics when boys were between 6 and 17 months old (35). This community sample is at high sociodemographic risk for AB based on being male, urban, and primarily low-income (at initial recruitment, per capita income was $241 per month). The sample is also racially diverse (e.g., 53.5% European-American, 36% African-American of those included at age 20). Target children and their mothers were seen almost yearly from age 1.5–20 in the laboratory and/or home with assessments that included questionnaires, a psychiatric interview, and at age 20, an fMRI scan. Participants were reimbursed after each assessment and all procedures were approved by the University of Pittsburgh IRB. Retention rates are high at each time point, with behavioral and fMRI data on 186 participants at age 20 (35, 36). After excluding for motion, task and signal-related error, 144 men had usable fMRI data (Supplemental Table S1).
Measures
Self-Report Measures
AB was assessed using the 53-item Self-Report of Antisocial Behavior Questionnaire (37). Items probing alcohol and drug use were removed to reduce the possibility that substance use could explain any potential findings. The remaining 41 items were summed to form a dimensional measure of AB (α=0.84). CU traits were measured using a sum of 5 items from the CU factor of the Antisocial Process Screening Device (38) as described previously in this sample (α=0.58) (39).
Interview Measures
Antisocial Personality Disorder (APD) was assessed by trained interviewers using the Structured Clinical Interview for DSM-IV for Axis II personality disorders (40). Cases approaching diagnosis were reviewed by a licensed clinical psychologist (39). As reported previously, at age 17, 35 of 250 participants (14%) met diagnostic criteria for CD, and at age 20, 34 of 254 participants (13%) met criteria for APD (39). In the current sample, 8% (n=11) met criteria for APD. Thus rates of diagnosis were above national prevelance estimates (i.e., APD rate is 5.5% in males)(41), but below forensic/clinical samples, consistent with an at-risk community sample (42). Based on research emphasizing the dimensional nature of AB (43, 44), for the present analyses, APD symptoms were summed to create a dimensional measure of AB. For covariates, we used the Structured Clinical Interview for DSM-IV (SCID)(45) to assess for lifetime symptom counts of major depressive episode (MDE), generalized anxiety disorder (GAD), and substance use disorders (SUD).
Court records
Records of adult violent charges (e.g., homicide, arson, sexual assault) were collected using the Pennsylvania state public court records website. These records were last checked in February, 2014 when almost all men were at least 21 years old (and up to 24 years old; average age=23.3). Age at time of record review was unrelated to number of violent charges (p=0.57). Of the full cohort that was searched, 91 young men (29%) had at least one adult arrest (39). The number of violent charges was summed for each participant, creating a dimensional measure (10% of the sample had at least 1 violence charge).
Neuroimaging Procedures
The fMRI paradigm was a slow event-related card-guessing game that evaluates neural response to the anticipation and receipt of monetary rewards and losses (46, 47). During each trial, participants guessed via button press whether the value of a visually presented card, with a possible value of 1–9, was higher or lower than 5 (4s), learned the trial type (possible-win, possible-loss) to anticipate (6s), and received feedback (win, lose, or no change; 1s plus 9s inter-trial interval)(47). Participants were told that their performance would determine a monetary reward after the scan, with $1 for each win and $0.50 deducted for each loss. Trials were presented in pseudorandom order with predetermined outcomes. Earnings totaled $6. Trials were presented in an 8-minute, 24-trial run, and a balanced number of trial types. This task has been shown previously to differentiate phases of reward and loss processing and to have large task-based effect sizes in the VS and prefrontal regions (46–50).
Bold fMRI acquisition parameters
As described previously (36), participants were scanned with a research-dedicated Siemens 3-T Trio scanner. Blood oxygenation level–dependent (BOLD) functional images were acquired with a gradient-echo echoplanar imaging sequence (repetition time/echo time=2000/29 milliseconds, field of view=200x200mm, matrix=64x64), that covered 34 interleaved axial slices (3mm slice thickness) aligned with the AC-PC plane and encompassing the entire cerebrum and most of the cerebellum to maximize limbic structure coverage.
Image processing
Image analyses were completed using the general linear model of SPM8 (http://www.fil.ion.ucl.ac.uk/spm/). Images for each participant were grey matter segmented, realigned to the first volume in the time series, unwarped to correct for head motion, co-registered to high resolution structural scans (MPRAGE), spatially normalized into a standard stereotactic space (MNI template) using a 12-parameter affine model, and smoothed to minimize noise and residual difference in gyral anatomy with a 6mm FWHM Gaussian filter. Voxelwise signal intensities were ratio-normalized to the whole-brain global mean. After preprocessing, Artifact detection Tools (ART) software (http://www.nitrc.org/projects/artifact_detect/) was used to address any possible influence of spiking or high-movement volumes by detecting global mean intensity and translation or rotational motion outliers (>4.5 SD from the mean global brain activation, >2mm movement, or 2o translation in any direction) within each participant’s data by creating a regressor within each participant’s first-level analysis that accounted for the possible confounding effects of volumes with large motion deflections or intensity spikes. Because of the potential for signal loss in limbic regions, particularly our main region of interest (ROI), single-subject BOLD fMRI data were only included in subsequent analyses if there was a minimum of 85% VS coverage using our bilateral VS ROI (51, 52). Participants with <80% task responding were excluded from analysis (n=24)(51, 53). These thresholds were chosen to balance sample/power considerations with coverage and task engagement (51–54). Participants excluded versus included due to task performance did not differ on measures of AB, CU traits, other psychopathology, race, or SES.
BOLD fMRI data analysis
Linear contrasts employing canonical hemodynamic response functions were used to estimate condition-specific BOLD activation for each individual. These individual contrast images were then used in second-level random effects models to determine mean reward-related reactivity using one-sample t-tests on the following contrasts: 1) reward anticipation>baseline, 2) loss anticipation>baseline, 3) reward outcome>baseline, and 4) loss outcome>baseline. Baseline was defined as the last 3 seconds of the 9-second inter-trial interval as previously described in this task/dataset (47, 50, 51, 53, 54). See Supplemental Table S2 for the main effects of the task.
We examined all results within the VS ROI, while masking for main effects of the task. The VS ROI was constructed using the Talairach Daemon option of the WFU PickAtlas Tool v2.4. Two spheres of 10mm radius were created around MNI coordinates x=+/−12, y=12, z= 10 to encompass the right and left VS. To examine whether reward-related differences may be present in other brain areas such as the PFC (55), we conducted whole-brain analyses in regions showing a main effect of task. We used 3DClustSim which uses a Monte Carlo simulation to correct for multiple comparisons across the whole brain or ROI at p<.05. Within 3DClustSim, we used a voxel-level threshold of p<.05, resulting in whole-brain cluster thresholds of k=505–742 (4040-5936mm3), and k=23–72 (184–756mm3) within the VS ROI (Supplemental Table S3).
For each contrast we used the following series of multiple regressions to examine our aims: 1) We examined the relationship between neural activity and self-reported AB or CU traits (each measure separately); 2) if self-reported AB was related to neural reactivity in a contrast, we examined whether results extended across other measures of AB (i.e., APD symptoms and/or violent charges); 3) in addition to assessing zero-order correlations, we also probed for suppression and confounding effects by controlling for the overlap between AB and CU traits, and 4) examined whether the results remained when adding psychiatric covariates (e.g., MDE, GAD, SUD). These analyses aimed to address recent studies showing a suppressor effect wherein only dimensional models that parse the overlapping variance separately between CU traits and AB predict neural reactivity (56–58) and to confirm that results were not due to general psychiatric symptoms. Finally, to address potential confounding by IQ or ADHD symptoms, we examined these variables as covariates (Supplemental Table S4).
Results
Reward Anticipation
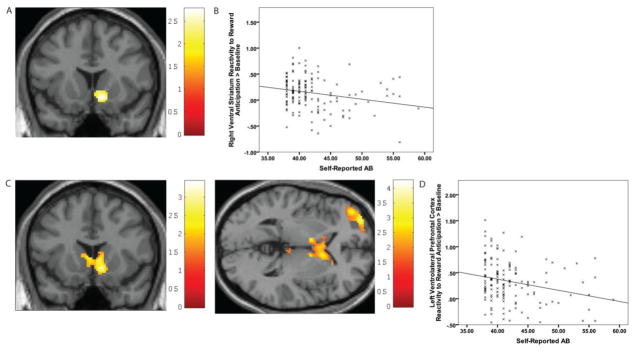
Self-reported AB was associated with decreased right VS reactivity during reward anticipation (t=3.06, k=148; x=10, y=14, z=−6). This finding remained significant when controlling for CU traits and psychiatric symptoms (t=2.73, k=164; x=10, y=14, z=−8) (Figure 1a/b). Moreover, APD symptoms and violent charges were also related to decreased bilateral VS reactivity (Table 1).
Figure 1. Self-reported antisocial behavior (AB) predicts less ventral striatum and vlPFC reactivity during the anticipation of rewards.
(A) Self-reported AB is negatively correlated with ventral striatum reactivity in the right ventral striatum region of interest (centered at the peak voxel, MNI: 10, 14, -6, t=−2.73, k=164). This finding emerges across multiple measures of AB and when controlling for CU traits and other psychiatric diagnoses. (B) Scatterplot of Self-Reported AB and ventral striatum reactivity during anticipation of rewards. (C) Self-reported AB is negatively correlated with activity in the left middle frontal gyrus (ventrolateral prefrontal cortex) and activity in a cluster extending from the right VS into the broader caudate during anticipation of rewards (centered at the second peak voxel, MNI: 10 14 −6; t = 3.06, k=625). The VS/caudate cluster remains (and demonstrated suppression effects) when controlling for CU traits and other psychiatric diagnoses. The left middle frontal gyrus cluster was only significant when partialling out variance of CU traits and other psychiatric diagnoses (centered at the peak voxel, MNI: −32, 60, −2; t = −3.36, k =601). (D) Scatterplot of Self-Reported AB and middle frontal gyrus (ventrolateral prefrontal cortex) reactivity during anticipation of rewards
Table 1.
Neural Reactivity Correlates of the Anticipation and Outcome of Rewards and Losses in Dimensions of Antisocial Behavior
| T | Cluster size | MNI coordinates | Analysis | Brain Region | |
|---|---|---|---|---|---|
| Reward Anticipation > Baseline | |||||
| Antisocial Behavior | −3.06 | 148 | 10 14 −6 | ROI | Right Ventral Striatum |
| −3.43 | 625 | 6 26 6 | Whole Brain | Right Ventral Striatum & Caudate | |
| Antisocial Behavior when controlling for Callous- Unemotional traits and psychiatric symptoms | −2.73 | 164 | 10 14 −8 | ROI | Right Ventral Striatum |
| −3.36 | 601 | −32 60 −2 | Whole Brain | Left Middle frontal gyrus | |
| −4.25 | 1052 | 4 12 −2 | Whole Brain | Right Ventral Striatum & Caudate | |
| Adult Violent Charges | −3.04 | 124 | 4 12 −2 | ROI | Right Ventral Striatum |
| −2.31 | 81 | −8 8 −2 | ROI | Left Ventral Striatum | |
| −3.96 | 804 | 34 60 8 | Whole Brain | Right Middle Frontal Gyrus | |
| Antisocial Personality Disorder Symptoms | −3.08 | 91 | −14 14 −8 | ROI | Left Ventral Striatum |
| −3.28 | 77 | 16 18 −6 | ROI | Right Ventral Striatum | |
| −3.93 | 706 | 2 −26 8 | Whole Brain | Right Ventral Striatum & Caudate | |
| Callous- Unemotional Traits | −3.77 | 760 | 34 56 6 | Whole Brain | Right Middle Frontal Gyrus |
| −3.62 | 2134 | −42 −56 6 | Whole Brain | Left Middle Occipital Gyrus | |
| Callous- Unemotional Traits when controlling for Antisocial Behavior and psychiatric symptoms | −3.41 | 1434 | −22 −82 22 | Whole Brain | Left Middle Occipital Gyrus |
| Loss Anticipation > Baseline | |||||
| Antisocial Behavior | −3.32 | 531 | −42 48 2 | Whole Brain | Left Middle Frontal Gyrus |
| Antisocial Behavior when controlling for Callous- Unemotional traits and psychiatric symptoms | −3.72 | 793 | −32 58 2 | Whole Brain | Left Middle Frontal Gyrus |
| −3.58 | 1514 | −48 −60 42 | Whole Brain | Left Inferior Parietal Lobe | |
| Adult Violent Charges | 3.32 | 696 | 34 −48 −8 | Whole Brain | Occipital Lobe |
All ROI analyses were for the bilateral Ventral Striatum. Psychiatric symptoms include major depressive episode, generalized anxiety disorder and substance use disorders.
In whole-brain analyses, self-reported AB was associated with decreased reactivity in a cluster that extended from the right VS into the broader caudate (t=3.43, k=625, x=6, y=26, z=6) (Figure 1c). Consistent with past findings of suppression effects, this effect strengthened when controlling for CU traits and psychiatric symptoms (t=4.25, k=1052, x=4, y=24, z=8). Self-reported AB was also associated with decreased left ventrolateral PFC (vlPFC) reactivity, but only when partialling out the variance of CU traits and psychiatric symptoms (t=3.36, k=601; x=−32, y=60, z=−2) (Figure 1c/d). Violent charges were related to decreased right vlPFC reactivity and APD was related to decreased right VS/caudate reactivity.
CU traits were not related to VS reactivity during reward anticipation, but were related to decreased right vlPFC reactivity (t=3.77, k=760; x=34, y=56, z=6) (Supplemental Figure S1). However, this finding was not unique to CU traits, as the result was no longer significant when controlling for self-reported AB. Unexpectedly, CU traits were related to decreased middle occipital gyrus reactivity (t=3.62, k=2134, x=−42, y=−56, z=6).
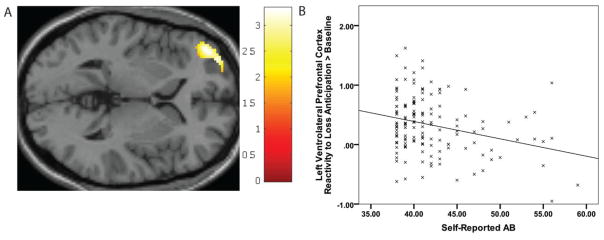
Loss Anticipation
During the anticipation of potential losses, AB was not related to VS reactivity, but was related to decreased left vlPFC reactivity (t=3.32, k=531; x=−42, y=48, z=2) (Figure 2a/b) and this relationship strengthened (i.e., suppression effects) when controlling for CU traits and other psychiatric symptoms (t=3.72, k=793; x=−32, y=58, z=2). Unexpectedly, when controlling for CU traits and other psychiatric symptoms, AB was also related to decreased inferior parietal lobe reactivity (t=3.58, k=1514, x=−48, y=−60, z=42). Violent charges were also related to decreased occipital lobe reactivity. CU traits and APD symptoms were not related to neural reactivity to loss anticipation.
Figure 2. Self-reported antisocial behavior (AB) predicts less middle frontal gyrus reactivity during loss anticipation (versus baseline).
(A) Self-report AB is negatively correlated with left middle frontal gyrus (lateral prefrontal cortex) reactivity (centered at the peak voxel, MNI: −42, 48, 2, t=−3.32, k=531) during anticipation of loss. This cluster remains (and demonstrated suppression effects) when controlling for CU traits and other psychiatric diagnoses. (B) Scatterplot of Self-Reported AB and middle frontal gyrus (ventrolateral prefrontal cortex) reactivity during anticipation of loss.
Reward Outcome
Neither AB nor CU traits were related to neural reactivity to reward receipt.
Loss Outcome
Neither AB nor CU traits were related to neural reactivity to loss receipt.
Potential Confounds
Though no measures of ADHD or IQ were collected concurrently with fMRI scanning, exploratory analyses with ADHD symptoms at earlier age periods (collected at age 15 and age 17, n=134) and IQ (collected at age 11, n=114) indicated that most results remained significant or were near significance (i.e., p<0.1) when these potential confounding characteristics were included, despite the reductions in power due to a reduced sample size (Supplemental Table S4).
Discussion
In a large, racially-diverse and at-risk sample of young men, the current study identified neural hypo-reactivity to reward and loss in the VS and vlPFC as a potential biomarker for AB. We found that AB was related to lower VS reactivity during the anticipation, but not receipt of rewards. We also found that CU traits were related to decreased vlPFC reactivity during reward anticipation, although this effect did not remain when controlling for AB. AB was also related to decreased vlPFC reactivity during the anticipation, but not receipt, of losses. These results demonstrate hypoactivity in the VS and vlPFC during anticipation of rewards and losses may be a neural “biomarker” of broad AB (and not of CU traits). These findings may inform the search for biomarkers related to AB (59, 60), inform our understanding of the etiology AB, and eventually inform prevention and treatment programs that seek to address the reward-dominant behavior seen in AB. Furthermore, these results also highlight the appreciable complexity when considering the role of reward-related neural reactivity and AB, and the need for high-risk community samples where AB and CU traits can be examined dimensionally with tasks that parse phases of reward.
Although previous literature has been mixed regarding the direction of reward processing deficits in AB, our findings suggest that AB is linked to a hyposensitive neural reward system (16, 17). Importantly, the negative relationship between AB and VS activity to cues of reward was quite robust as it was present across multiple measures of AB, in ROI and whole-brain analyses, and persisted after controlling for CU traits and other psychopathology. These findings suggest that AB is linked to lower levels of reward-related reactivity when considering potential rewards which could cause individuals with AB to seek more risky behaviors to achieve an “optimal” level of anticipation-related neural activity.
AB was also related to lower vlPFC activity during reward and loss anticipation. Interestingly, for reward anticipation, associations between AB and prefrontal neural activity showed suppression effects wherein the relationship was only significant when controlling for CU traits. These results support Blair’s model suggesting that prefrontal neural differences in response to reward, decision making, and cognitive control are markers of broad externalizing/disinhibitory behaviors and unrelated to the level of CU traits (32, 61). Indeed, in the current study it appears that only the variance related uniquely to AB (and not overlapping with CU traits) is related to this blunted left vlPFC reactivity to reward.
Research suggests that activity in the vlPFC is important generally during response inhibition (62), representation of punishment information (63), and reappraisal of affective stimuli (54, 67, 68), as well as response conflict and response reversal in those high on AB (64–66). Moreover, left vlPFC activity during reward processing is associated with impulsive sensation seeking (69). Although reward-related processing is complex and may engage multiple and different cognitive processes, reduced reward-related vlPFC activity during reward and loss anticipation in this study could help to explain reward-related behavioral deficits seen in AB. That is, lower reward-related reactivity in the VS and vlPFC may help to explain why individuals high on AB seek increasingly risky rewards and then have difficulty changing their behavior in response to unfavorable outcomes due to deficits in inhibition, representing changing contingencies, or reappraising stimuli (70). This combination of neurobehavioral deficits may make it difficult to refrain from engaging in rewarding but risky behaviors, and may help explain why individuals with AB continue to engage in such behaviors despite harmful consequences.
In the current study, CU traits were related to lower right vlPFC activity during reward anticipation, but this finding did not remain after accounting for AB. Thus, CU traits showed little unique association with reward-related neural activity. Although this result is consistent with Blair's model of the role of reward-related neural activity in AB versus CU traits, as this measure of CU traits has failed to predict some expected outcomes in this sample (i.e., future AB, amygdala reactivity; 36, 39), CU traits may manifest differently in these young men who were reared in urban, low-income contexts fraught with acute and chronic adversities (e.g., exposure to deviance and violence). Additionally, previously documented psychometric issues with the measure of CU (71), including the small number of items and low internal consistency (α=0.58) in this sample may have underestimated the true effect of CU traits on reward processing, particularly in comparison to our more reliable measures of AB (36, 39). A more comprehensive and age-appropriate measure of psychopathy (36) will be important for future studies in confirming that CU/psychopathic traits are unrelated to reward-related neural reactivity.
Although the current study has many strengths including a large, racially-diverse, high-risk sample, use of multi-method dimensional measures of AB and CU traits, and assessment of anticipation and outcome phases of reward processing, the results should be interpreted with some caution based on several potential limitations. First, while research on reward-related neural processing in AB is limited, our findings do conflict with a previous report linking AB to greater VS activity in a healthy community sample (12). However, our study’s sample was different than most based on the high-risk status of participants and the inclusion of only males, which could explain the difference in findings. It is also possible that the link between reward-related brain function and AB/CU traits could be curvilinear or vary by AB severity (i.e., findings may diverge between clinical, at-risk, and community samples) and this hypothesis (61) should be tested. Additionally, our task used relatively small monetary rewards (total=$6). As differences in neural responding may only manifest for larger rewards, it is possible that the larger rewards in this previous study (12), may moderate findings. Second, the fMRI task was relatively short and did not include a jitter between trials. Third, because concurrent ADHD was not assessed and some of our findings when controlling for earlier ADHD did not meet stringent correction for multiple comparisons, it is possible that ADHD could be accounting for some of the results. Although parsing AB from ADHD may be difficult based on the high comorbidity between these constructs (72), given findings linking ADHD to reward-related neural differences in frontostriatal brain activity (19, 29), future studies should parse the unique contributions of reward-related neural functioning between ADHD and AB. Fourth, despite the at-risk nature of our sample, the rates of AB were relatively low compared to clinical/forensic samples. A small percentage of participants were incarcerated during data collection and did not complete the MRI scan, further lowering the rate of severe AB in the sample. Replicating the current findings in a clinical/forensic sample will be important in determining whether these effects exist linearly across a wide range of AB (19). Nevertheless, the high-risk focus of this study is a strength because it allows for dimensional analyses of the relationship between AB and reward-related neural response with a range from little AB to those with extensive legal records and APD diagnoses. Finally, our findings should be interpreted with caution in generalizing to other populations, particularly women and men not living in low-income, urban environments. Participants in this sample have been exposed to a high level of acute and chronic stressors, which may affect their frontostriatal reactivity during reward processing (73, 74). Thus, follow-up studies are needed to examine how individual differences in life experiences may lead to individual differences in reward-related neural reactivity.
The current study is one of the first to use a large at-risk community sample of low-income, racially-diverse males to link distinct components of AB to neurobiological differences in specific phases of reward processing. To address the increasingly important conceptualization of psychopathology as dimensional (75, 76), we used dimensional measures from multiple sources to assess AB and CU traits. We found evidence that AB was related to less VS reactivity during the anticipation of rewards and less vlPFC reactivity during anticipation of rewards and losses. These results suggest that AB is linked to dysfunction in neural regions that are important in the learning and updating of reward-related behavioral responses to help guide appropriate decision making and suggest neural mechanisms underlying why individuals with AB persist in delinquent behavior despite continued negative consequences.
Supplementary Material
Table 2.
Zero-order correlations of main study behavioral variables
| Socioeco nomic Status |
Self- repo rted AB |
Adul t Viol ent Char ges |
APD sympt oms |
CU Trai ts |
Depre ssion |
G A D |
Dru g Ab use |
Drug Depen dence |
Alco hol Abu se |
Alcoho l Depen dence |
IQ | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | 23.5 | 4.07 | 0.19 | 0.5 | 3.52 | 0.29 | 0.15 | 0.29 | 0.62 | 0.19 | 0.38 | 96.30 |
| Range | 6–57 | 0–21 | 0–4 | 0–7 | 0–9 | 0–6 | 0–5 | 0–4 | 0–6 | 0–3 | 0–7 | 59-138 |
| Standard Deviation | 9.05 | 4.62 | 0.65 | 1.12 | 1.70 | 1.15 | 0.77 | 0.66 | 1.27 | 0.60 | 1.08 | 17.52 |
| Self- reportedd AB | .044 | |||||||||||
| Adult Violent Charges | .022 | .070 | ||||||||||
| APD symptoms | −.084 | .437** | .019 | |||||||||
| CU traits | −.180* | .286** | .103 | .092 | ||||||||
| Depression | −.040 | .286** | −.058 | .041 | .118 | |||||||
| GAD | .090 | .051 | − .057 | −.047 | .042 | .142 | ||||||
| Drug Abuse | .089 | .376** | .063 | .281** | .116 | .053 | .109 | |||||
| Drug Dependence | .037 | .409** | .029 | .275** | .156 | .103 | .056 | .631** | ||||
| Alcohol Abuse | .220** | .209* | −.044 | .084 | .072 | .029 | −.063 | .337** | .124 | |||
| Alcohol Dependence | .193* | .338** | −.107 | .125 | .073 | .107 | .068 | .484** | .465** | .342** | ||
| IQ (age11) | .206* | −.140 | −.181 | −.132 | −.255** | −.064 | .177 | −.116 | −.142 | .113 | .088 |
Note:
p< .05;
p < .01.
AB = Antisocial Behavior. APD = Antisocial Personality Disorder. CU = Callous-Unemotional. GAD = Generalized Anxiety Disorder Symptoms. Depression = Major Depressive Episode symptoms. All alcohol and drug measures were symptom counts within each diagnosis. Hollingshead socioeconomic status was measured at age 1.5, and IQ was collected at age 11. All other measures were collected at age 20.
Acknowledgments
We are grateful to the work of the staff of the Pitt Mother & Child Project for their many years of service, and to our study families for sharing their lives with us and making the research possible
The research reported in this article was supported by grants to D.S.S. (R01 MH50907, R01 MH01666, and K05 DA25630), D.S.S. and E.E.F (R01 DA026222), and L.W.H. (L40 DA036468 & L40 MH108392) from the National Institutes of Health
Footnotes
Financial Disclosures
The authors report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 2.Foster EM, Jones DE. The high costs of aggression: public expenditures resulting from conduct disorder. Am J Public Health. 2005;95:1767–1772. doi: 10.2105/AJPH.2004.061424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hyde LW, Shaw DS, Hariri AR. Understanding Youth Antisocial Behavior Using Neuroscience through a Developmental Psychopathology Lens: Review, Integration, and Directions for Research. Dev Rev. 2013:33. doi: 10.1016/j.dr.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Viding E, McCrory EJ. Genetic and neurocognitive contributions to the development of psychopathy. Dev Psychopathol. 2012;24:969–983. doi: 10.1017/S095457941200048X. [DOI] [PubMed] [Google Scholar]
- 5.Byrd AL, Loeber R, Pardini DA. Antisocial behavior, psychopathic features and abnormalities in reward and punishment processing in youth. Clin Child Fam Psychol Rev. 2014;17:125–156. doi: 10.1007/s10567-013-0159-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Budhani S, Blair RJR. Response reversal and children with psychopathic tendencies: success is a function of salience of contingency change. Journal of Child Psychology and Psychiatry. 2005;46:972–981. doi: 10.1111/j.1469-7610.2004.00398.x. [DOI] [PubMed] [Google Scholar]
- 7.De Brito SA, Viding E, Kumari V, Blackwood N, Hodgins S. Cool and hot executive function impairments in violent offenders with antisocial personality disorder with and without psychopathy. PLoS One. 2013;8:e65566. doi: 10.1371/journal.pone.0065566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fairchild G, van Goozen SH, Stollery SJ, Aitken MR, Savage J, Moore SC, et al. Decision making and executive function in male adolescents with early-onset or adolescence-onset conduct disorder and control subjects. Biol Psychiatry. 2009;66:162–168. doi: 10.1016/j.biopsych.2009.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luman M, Tripp G, Scheres A. Identifying the neurobiology of altered reinforcement sensitivity in ADHD: a review and research agenda. Neurosci Biobehav Rev. 2010;34:744–754. doi: 10.1016/j.neubiorev.2009.11.021. [DOI] [PubMed] [Google Scholar]
- 10.Heekeren HR, Wartenburger I, Marschner A, Mell T, Villringer A, Reischies FM. Role of ventral striatum in reward-based decision making. Neuroreport. 2007;18:951–955. doi: 10.1097/WNR.0b013e3281532bd7. [DOI] [PubMed] [Google Scholar]
- 11.Bjork JM, Chen G, Smith AR, Hommer DW. Incentive-elicited mesolimbic activation and externalizing symptomatology in adolescents. J Child Psychol Psychiatry. 2010;51:827–837. doi: 10.1111/j.1469-7610.2009.02201.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buckholtz JW, Treadway MT, Cowan RL, Woodward ND, Benning SD, Li R, et al. Mesolimbic dopamine reward system hypersensitivity in individuals with psychopathic traits. Nat Neurosci. 2010;13:419–421. doi: 10.1038/nn.2510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robinson TE, Berridge KC. Incentive-sensitization and addiction. Addiction. 2001;96:103–114. doi: 10.1046/j.1360-0443.2001.9611038.x. [DOI] [PubMed] [Google Scholar]
- 14.Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain research reviews. 1993;18:247–291. doi: 10.1016/0165-0173(93)90013-p. [DOI] [PubMed] [Google Scholar]
- 15.Robinson TE, Berridge KC. The incentive sensitization theory of addiction: some current issues. Philosophical Transactions of the Royal Society of London B: Biological Sciences. 2008;363:3137–3146. doi: 10.1098/rstb.2008.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohn MD, Veltman DJ, Pape LE, van Lith K, Vermeiren RR, van den Brink W, et al. Incentive Processing in Persistent Disruptive Behavior and Psychopathic Traits: A Functional Magnetic Resonance Imaging Study in Adolescents. Biol Psychiatry. 2014 doi: 10.1016/j.biopsych.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 17.Carre JM, Hyde LW, Neumann CS, Viding E, Hariri AR. The neural signatures of distinct psychopathic traits. Soc Neurosci. 2013;8:122–135. doi: 10.1080/17470919.2012.703623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klein RG, Abikoff H. Behavior therapy and methylphenidate in the treatment of children with ADHD. Journal of Attention Disorders. 1997;2:89–114. [Google Scholar]
- 19.Plichta MM, Scheres A. Ventral–striatal responsiveness during reward anticipation in ADHD and its relation to trait impulsivity in the healthy population: A meta-analytic review of the fMRI literature. Neurosci Biobehav Rev. 2014;38:125–134. doi: 10.1016/j.neubiorev.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beck A, Schlagenhauf F, Wüstenberg T, Hein J, Kienast T, Kahnt T, et al. Ventral striatal activation during reward anticipation correlates with impulsivity in alcoholics. Biol Psychiatry. 2009;66:734–742. doi: 10.1016/j.biopsych.2009.04.035. [DOI] [PubMed] [Google Scholar]
- 21.Wrase J, Schlagenhauf F, Kienast T, Wüstenberg T, Bermpohl F, Kahnt T, et al. Dysfunction of reward processing correlates with alcohol craving in detoxified alcoholics. Neuroimage. 2007;35:787–794. doi: 10.1016/j.neuroimage.2006.11.043. [DOI] [PubMed] [Google Scholar]
- 22.Ahmed SH, Koob GF. Transition to drug addiction: a negative reinforcement model based on an allostatic decrease in reward function. Psychopharmacology (Berl) 2005;180:473–490. doi: 10.1007/s00213-005-2180-z. [DOI] [PubMed] [Google Scholar]
- 23.Tindell AJ, Berridge KC, Zhang J, Pecina S, Aldridge JW. Ventral pallidal neurons code incentive motivation: amplification by mesolimbic sensitization and amphetamine. Eur J Neurosci. 2005;22:2617–2634. doi: 10.1111/j.1460-9568.2005.04411.x. [DOI] [PubMed] [Google Scholar]
- 24.White SF, Pope K, Sinclair S, Fowler KA, Brislin SJ, Williams WC, et al. Disrupted expected value and prediction error signaling in youths with disruptive behavior disorders during a passive avoidance task. Am J Psychiatry. 2013 doi: 10.1176/appi.ajp.2012.12060840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Banich MT, Crowley TJ, Thompson LL, Jacobson BL, Liu X, Raymond KM, et al. Brain activation during the Stroop task in adolescents with severe substance and conduct problems: A pilot study. Drug Alcohol Depend. 2007;90:175–182. doi: 10.1016/j.drugalcdep.2007.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crowley TJ, Dalwani MS, Mikulich-Gilbertson SK, Du YP, Lejuez CW, Raymond KM, et al. Risky decisions and their consequences: neural processing by boys with antisocial substance disorder. PLoS One. 2010;5:e12835. doi: 10.1371/journal.pone.0012835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Finger EC, Marsh AA, Blair KS, Reid ME, Sims C, Ng P, et al. Disrupted reinforcement signaling in the orbitofrontal cortex and caudate in youths with conduct disorder or oppositional defiant disorder and a high level of psychopathic traits. Am J Psychiatry. 2011 doi: 10.1176/appi.ajp.2010.10010129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rubia K, Smith AB, Halari R, Matsukura F, Mohammad M, Taylor E, et al. Disorder-specific dissociation of orbitofrontal dysfunction in boys with pure conduct disorder during reward and ventrolateral prefrontal dysfunction in boys with pure ADHD during sustained attention. Am J Psychiatry. 2009;166:83–94. doi: 10.1176/appi.ajp.2008.08020212. [DOI] [PubMed] [Google Scholar]
- 29.Rubia K, Halari R, Cubillo A, Mohammad A-M, Brammer M, Taylor E. Methylphenidate normalises activation and functional connectivity deficits in attention and motivation networks in medication-naive children with ADHD during a rewarded continuous performance task. Neuropharmacology. 2009;57:640–652. doi: 10.1016/j.neuropharm.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 30.Fuster JM. The prefrontal cortex—an update: time is of the essence. Neuron. 2001;30:319–333. doi: 10.1016/s0896-6273(01)00285-9. [DOI] [PubMed] [Google Scholar]
- 31.Blair RJR, Leibenluft E, Pine DS. Conduct disorder and callous–unemotional traits in youth. N Engl J Med. 2014;371:2207–2216. doi: 10.1056/NEJMra1315612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zucker RA, Heitzeg MM, Nigg JT. Parsing the undercontrol–disinhibition pathway to substance use disorders: A multilevel developmental problem. Child Development Perspectives. 2011;5:248–255. doi: 10.1111/j.1750-8606.2011.00172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hyde LW, Byrd AL, Votruba-Drzal E, Hariri AR, Manuck SB. Amygdala reactivity and negative emotionality: divergent correlates of antisocial personality and psychopathy traits in a community sample. J Abnorm Psychol. 2014;123:214–224. doi: 10.1037/a0035467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sebastian CL, McCrory EJ, Cecil CA, Lockwood PL, De Brito SA, Fontaine NM, et al. Neural responses to affective and cognitive theory of mind in children with conduct problems and varying levels of callous-unemotional traits. Arch Gen Psychiatry. 2012;69:814–822. doi: 10.1001/archgenpsychiatry.2011.2070. [DOI] [PubMed] [Google Scholar]
- 35.Shaw DS, Hyde LW, Brennan LM. Early predictors of boys' antisocial trajectories. Dev Psychopathol. 2012;24:871–888. doi: 10.1017/S0954579412000429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hyde LW, Shaw DS, Murray L, Gard A, Hariri AR, Forbes EE. Dissecting the Role of Amygdala Reactivity in Antisocial Behavior in a Sample of Young, Low-Income, Urban Men. Clinical Psychological Science. 2015 doi: 10.1177/2167702615614511. 2167702615614511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elliott D, Huizinga D, Ageton S. Explaining delinquency and drug use. Beverly Hills, CA: Sage Publications; 1985. [Google Scholar]
- 38.Frick PJ, Bodin SD, Barry CT. Psychopathic traits and conduct problems in community and clinic-referred samples of children: further development of the psychopathy screening device. Psychol Assess. 2000;12:382. [PubMed] [Google Scholar]
- 39.Hyde LW, Burt SA, Shaw DS, Donnellan MB, Forbes EE. Early starting, aggressive, and/or callous-unemotional? Examining the overlap and predictive utility of antisocial behavior subtypes. J Abnorm Psychol. 2015;124:329–342. doi: 10.1037/abn0000029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.First MB, Gibbon M. User's guide for the structured clinical interview for DSM-IV axis II personality disorders: SCID-II. American Psychiatric Pub; 1997. [Google Scholar]
- 41.Grant BF, Hasin DS, Stinson FS, Dawson DA, Chou SP, Ruan WJ, et al. Prevalence, correlates, and disability of personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of clinical psychiatry. 2004;65:948–958. doi: 10.4088/jcp.v65n0711. [DOI] [PubMed] [Google Scholar]
- 42.Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. The Journal of clinical psychiatry. 2005;66:1,478–685. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- 43.Blonigen DM, Hicks BM, Krueger RF, Patrick CJ, Iacono WG. Continuity and change in psychopathic traits as measured via normal-range personality: a longitudinal-biometric study. J Abnorm Psychol. 2006;115:85. doi: 10.1037/0021-843X.115.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: an integrative quantitative model of the adult externalizing spectrum. J Abnorm Psychol. 2007;116:645. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.First M, Spitzer R, Gibbon M, Williams . Structured Clinical Interview for DSM-IV Axis I Disorders Research Version (SCID-I) J New York: New York State Psychiatric Institute; 1996. [Google Scholar]
- 46.Forbes EE, Hariri AR, Martin SL, Silk JS, Moyles DL, Fisher PM, et al. Altered striatal activation predicting real-world positive affect in adolescent major depressive disorder. Am J Psychiatry. 2009;166:64–73. doi: 10.1176/appi.ajp.2008.07081336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nusslock R, Almeida JR, Forbes EE, Versace A, Frank E, Labarbara EJ, et al. Waiting to win: elevated striatal and orbitofrontal cortical activity during reward anticipation in euthymic bipolar disorder adults. Bipolar Disord. 2012;14:249–260. doi: 10.1111/j.1399-5618.2012.01012.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Forbes EE, Shaw DS, Dahl RE. Alterations in reward-related decision making in boys with recent and future depression. Biol Psychiatry. 2007;61:633–639. doi: 10.1016/j.biopsych.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 49.Hasler BP, Dahl RE, Holm SM, Jakubcak JL, Ryan ND, Silk JS, et al. Weekend–weekday advances in sleep timing are associated with altered reward-related brain function in healthy adolescents. Biol Psychol. 2012;91:334–341. doi: 10.1016/j.biopsycho.2012.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morgan JK, Shaw DS, Olino TM, Musselman SC, Kurapati NT, Forbes EE. History of Depression and Frontostriatal Connectivity During Reward Processing in Late Adolescent Boys. J Clin Child Adolesc Psychol. 2015:1–10. doi: 10.1080/15374416.2015.1030753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Casement MD, Guyer AE, Hipwell AE, McAloon RL, Hoffmann AM, Keenan KE, et al. Girls’ challenging social experiences in early adolescence predict neural response to rewards and depressive symptoms. Dev Cogn Neurosci. 2014;8:18–27. doi: 10.1016/j.dcn.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Morgan JK, Shaw DS, Forbes EE. Maternal depression and warmth during childhood predict age 20 neural response to reward. J Am Acad Child Adolesc Psychiatry. 2014;53:108–117. e101. doi: 10.1016/j.jaac.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hasler BP, Sitnick SL, Shaw DS, Forbes EE. An altered neural response to reward may contribute to alcohol problems among late adolescents with an evening chronotype. Psychiatry Research: Neuroimaging. 2013;214:357–364. doi: 10.1016/j.pscychresns.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chase HW, Nusslock R, Almeida JR, Forbes EE, LaBarbara EJ, Phillips ML. Dissociable patterns of abnormal frontal cortical activation during anticipation of an uncertain reward or loss in bipolar versus major depression. Bipolar disorders. 2013;15:839–854. doi: 10.1111/bdi.12132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.O'Doherty J, Kringelbach ML, Rolls ET, Hornak J, Andrews C. Abstract reward and punishment representations in the human orbitofrontal cortex. Nat Neurosci. 2001;4:95–102. doi: 10.1038/82959. [DOI] [PubMed] [Google Scholar]
- 56.Viding E, Sebastian CL, Dadds MR, Lockwood PL, Cecil CAM, De Brito SA, et al. Amygdala Response to Preattentive Masked Fear in Children With Conduct Problems: The Role of Callous-Unemotional Traits. Am J Psychiatry. 2012;169:1109–1116. doi: 10.1176/appi.ajp.2012.12020191. [DOI] [PubMed] [Google Scholar]
- 57.Lozier LM, Cardinale EM, VanMeter JW, Marsh AA. Mediation of the relationship between callous-unemotional traits and proactive aggression by amygdala response to fear among children with conduct problems. JAMA psychiatry. 2014;71:627–636. doi: 10.1001/jamapsychiatry.2013.4540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hyde LW, Byrd AL, Votruba-Drzal E, Hariri AR, Manuck SB. Antisocial behavior and amygdala reactivity: Divergent correlates of antisocial personality and psychopathy traits in a community sample. J Abnorm Psychol. 2014;123:214–224. doi: 10.1037/a0035467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Insel TR. The NIMH research domain criteria (RDoC) project: precision medicine for psychiatry. Am J Psychiatry. 2014 doi: 10.1176/appi.ajp.2014.14020138. [DOI] [PubMed] [Google Scholar]
- 60.White SF, Briggs-Gowan MJ, Voss JL, Petitclerc A, McCarthy K, Blair RRJ, et al. Can the fear recognition deficits associated with callous-unemotional traits be identified in early childhood? J Clin Exp Neuropsychol. 2016;38:672–684. doi: 10.1080/13803395.2016.1149154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Blair RJR. Reward Processing, Functional Connectivity, Psychopathy, and Research Domain Criteria. Biol Psychiatry. 2015;78:592–593. doi: 10.1016/j.biopsych.2015.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sakagami M, Pan X. Functional role of the ventrolateral prefrontal cortex in decision making. Curr Opin Neurobiol. 2007;17:228–233. doi: 10.1016/j.conb.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 63.Kringelbach ML, Rolls ET. The functional neuroanatomy of the human orbitofrontal cortex: evidence from neuroimaging and neuropsychology. Prog Neurobiol. 2004;72:341–372. doi: 10.1016/j.pneurobio.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 64.Budhani S, Richell RA, Blair RJR. Impaired reversal but intact acquisition: probabilistic response reversal deficits in adult individuals with psychopathy. J Abnorm Psychol. 2006;115:552. doi: 10.1037/0021-843X.115.3.552. [DOI] [PubMed] [Google Scholar]
- 65.Budhani S, Marsh A, Pine D, Blair R. Neural correlates of response reversal: considering acquisition. Neuroimage. 2007;34:1754–1765. doi: 10.1016/j.neuroimage.2006.08.060. [DOI] [PubMed] [Google Scholar]
- 66.Blair R. Dysfunctions of medial and lateral orbitofrontal cortex in psychopathy. Ann N Y Acad Sci. 2007;1121:461–479. doi: 10.1196/annals.1401.017. [DOI] [PubMed] [Google Scholar]
- 67.Johnstone T, van Reekum CM, Urry HL, Kalin NH, Davidson RJ. Failure to regulate: counterproductive recruitment of top-down prefrontal–subcortical circuitry in major depression. The Journal of neuroscience. 2007;27:8877–8884. doi: 10.1523/JNEUROSCI.2063-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vink M, Derks JM, Hoogendam JM, Hillegers M, Kahn RS. Functional differences in emotion processing during adolescence and early adulthood. Neuroimage. 2014;91:70–76. doi: 10.1016/j.neuroimage.2014.01.035. [DOI] [PubMed] [Google Scholar]
- 69.Phillips ML, Swartz HA. A critical appraisal of neuroimaging studies of bipolar disorder: toward a new conceptualization of underlying neural circuitry and a road map for future research. Am J Psychiatry. 2014 doi: 10.1176/appi.ajp.2014.13081008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Blair RJR. Psychopathic traits from an RDoC perspective. Curr Opin Neurobiol. 2015;30:79–84. doi: 10.1016/j.conb.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 71.Dillard CL, Salekin RT, Barker ED, Grimes RD. Psychopathy in adolescent offenders: An item response theory study of the antisocial process screening device–self report and the Psychopathy Checklist: Youth Version. Personality Disorders: Theory, Research, and Treatment. 2013;4:101. doi: 10.1037/a0028439. [DOI] [PubMed] [Google Scholar]
- 72.Fehon DC, Becker DF, Grilo CM, Walker ML, Levy KN, Edell WS, et al. Diagnostic comorbidity in hospitalized adolescents with conduct disorder. Compr Psychiatry. 1997;38:141–145. doi: 10.1016/s0010-440x(97)90066-3. [DOI] [PubMed] [Google Scholar]
- 73.Ohira H, Matsunaga M, Kimura K, Murakami H, Osumi T, Isowa T, et al. Chronic stress modulates neural and cardiovascular responses during reversal learning. Neuroscience. 2011;193:193–204. doi: 10.1016/j.neuroscience.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 74.Romens SE, Casement MD, McAloon R, Keenan K, Hipwell AE, Guyer AE, et al. Adolescent girls’ neural response to reward mediates the relation between childhood financial disadvantage and depression. Journal of Child Psychology and Psychiatry. 2015 doi: 10.1111/jcpp.12410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Krueger RF, Markon KE. A dimensional-spectrum model of psychopathology: progress and opportunities. Arch Gen Psychiatry. 2011;68:10–11. doi: 10.1001/archgenpsychiatry.2010.188. [DOI] [PubMed] [Google Scholar]
- 76.Markon KE, Krueger RF. Categorical and continuous models of liability to externalizing disorders: a direct comparison in NESARC. Arch Gen Psychiatry. 2005;62:1352–1359. doi: 10.1001/archpsyc.62.12.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.