Abstract
Objectives:
To assess the visibility of the mandibular canal (MC) morphology in different jaw dental segments (JDSs) in relation to morphometric and densitometric parameters on digital panoramic radiographs (DPRs).
Methods:
32 DPRs (155 JDSs) were selected randomly after retrieval. MC visibility in conjunction with superior and inferior border visibility was scored on a 5-point scale in four places on the JDS—that is, for the medial, distal, superior and inferior MC parts. Morphometric and densitometric analyses were made horizontally and vertically in the JDS region. Descriptive statistics, Fisher's exact test, Mann–Whitney U test and additional tests were performed.
Results:
There was no significant difference in MC visibility for the superior, inferior, medial and distal parts of the JDSs. Statistically significant (p < 0.05) differences were identified between particular visibility scores of the superior and inferior MC borders. In 22.0–24.7% of JDSs, the superior MC border was not visible, more than twice as often as the inferior MC border was not visible (9.1–10.2%). The visibility of superior and inferior MC borders in JDSs was not related to the morphometric or densitometric assessment parameters, or to age, gender, JDS location, condition or the visibility of neighbouring MC parts or contralateral JDSs.
Conclusions:
DPRs failed to provide MC visibility based on a single factor. Particular differences were identified between the levels of visibility of the superior and inferior MC borders. More advanced radiological investigation methods could be required for the evaluation of about 25% of JDSs when superior MC border identification is obligatory.
Keywords: mandible; alveolar nerve, inferior; radiography, panoramic; densitometry; dental implants
Introduction
Dental implant surgery is a widely accepted and increasingly frequent treatment method in dentistry, but it can involve many complications. Injury to the inferior alveolar nerve (IAN) is one of the most serious complications in implant dentistry. IAN injury is a predominantly iatrogenic complication with reported incidence of up to 40%.1 Furthermore, IAN is the most commonly injured peripheral branch of the trigeminal nerve (64.4%).2 Intraoperative pain, bleeding and temporary or permanent post-operative anaesthesia, paraesthesia, hypaesthesia or dysaesthesia can follow such an injury. Pre-operative radiological planning is obligatory for interventions in the posterior mandible to minimize the IAN injury rate.
Opinion leaders and responsible organizations worldwide periodically provide guidelines for the application of diagnostic imaging in implant dentistry.3–6 The guidelines have been adapted many times in particular countries or regions based on particular scientific data and laws. The authors of the present study operated according to guidelines set forth by the European Commission and European Association for Osseointegration.3,5
Panoramic imaging has a wide range of applications and is accepted for the evaluation of mandibular canal (MC) visibility despite the existence of more accurate investigation methods (e.g. CBCT).7 Panoramic imaging lacks three-dimensional visualization and suffers from vertical and horizontal magnification.8 A previous panoramic radiography quality evaluation study9 discusses possible positioning, image taking and processing errors as well as errors due to anatomical abnormalities, but these images commonly have normal or higher level quality9 and are recommended for examination in implant dentistry. Despite the possible shortcomings of panoramic imaging, accurate endosseous dental implant planning by means of panoramic radiographs reduces the risk for IAN injury and subsequent function impairment to a non-significant level.10,11 Treatment planning is exclusively unique because MC location and course are individual. MC visibility on panoramic radiographs changes from the mandibular foramen to the mental foramen.12 The identification of fine anatomical structures on radiographs in the implant site is a delicate task for dental professionals. Juodzbalys and Raustia13 proposed to use the term “jaw dental segment” (JDS) for more accurate jaw segment identification and related investigations.
The use of digital panoramic imaging is becoming widespread due to improvements to image quality and after the introduction of dedicated software for image manipulation.14 Although MC visibility changes throughout the course of the MC, the more precise evaluation of JDS by means of dedicated digital panoramic radiographs (DPRs) could provide more details with regard to possibilities for MC visibility. Manufacturers even provide tools for densitometric analysis of bone density on panoramic radiographs. The clinician hopes to benefit from these technologies. Unfortunately, we could not find in the literature even one source for comprehensive MC region assessment with DPR using vertical morphometric measurements of the MC and surrounding bone nor a source using vertical or horizontal densitometric measurements of the MC and neighbouring regions to allow identification of the acquired parameters' relationship to MC visibility. Therefore, the present study was initiated to assess whether the morphometric measurements of the MC and surrounding bone and specific patterns of densitometric value changes could be the guide for detecting the MC and its walls, even in cases of poor visibility.
The aim of the present study was to assess the visibility of the MC morphology in different JDSs in relation to morphometric and densitometric parameters on DPRs.
Methods and materials
Patient selection
Caucasian patients were selected randomly for the study at the Department of Oral and Maxillofacial Surgery (Lithuanian University of Health Sciences, Kaunas, Lithuania) from among patients needing panoramic imaging for pre-operative planning of surgery. Patients were asked for medical and dental history to reveal any unsuitability for the study. All subjects had permanent dentition, were systematically healthy or with mild systemic diseases (American Society of Anaesthesiologists I or II) and had no history of mandibular traumas or surgical interventions in the regions of the evaluated JDSs (e.g. lateralization of IAN; the exception was removal of a tooth). Exclusion criteria were active periodontal diseases, current periodontal or orthodontic treatment, and inability to sign the informed consent. Ethical approval (number BE-2-76) was retrieved from the Kaunas Regional Biomedical Research Ethics Committee (Lithuania). Permission for personal data management (number 2R-4170) was obtained from the ethical State Data Protection Inspectorate. Written permissions to participate in the study were obtained from randomly selected subjects.
Panoramic radiographs
All radiographs in this study were taken with a Kodak 9000® Extraoral Imaging System (Kodak Dental Systems, Carestream Health Inc., Rochester, NY). According to the manufacturer's manual, 68–73 kV, 10–12 mA and 6 mA were set, and the exposure time was 13.5–14.4 s. Patients were positioned in a standardized manner according to the manufacturer's recommendations to reduce positional errors. Kodak Dental Imaging Software v. 6.12.18.1 (Carestream Health Inc) was used for image analysis. Evaluation was performed by one trained and calibrated oral surgeon on a 29.9-inch display (Coronis Fusion 4MP; Barco N.V, Kortrijk, Belgium) at a distance of 60 cm from the screen in dimmed room conditions. DPR inclusion criteria were based on image quality analysis; images considered optimal and adequate for diagnosis were suitable for further evaluation.9 The main errors were positioning (e.g., patient movement or patient positioning asymmetry in any direction) and image taking or processing errors such as the image not being at the optimal contrast or density. If the DPR did not satisfy the mentioned quality requirements or had errors due to anatomical abnormalities, such as an unidentified mental foramen or a bifid MC, it was rejected from further evaluation.
Mandibular canal visibility and jaw dental segment evaluation protocol
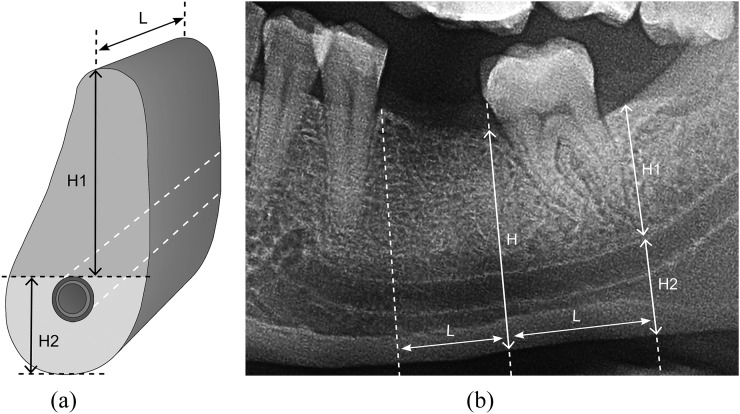
MC visibility assessment in relation to morphometric and densitometric parameters of the jaw bone on DPRs were made based on the JDS pattern.13 This is defined as a vertically cut jaw segment including tooth, alveolar bone and basal bone (Figure 1). The location of bone suitable for implantation is identical with the former location of a tooth in the jaw. The number of the JDS describing the position of a planned implant in the jaw can be shown. If the JDS is edentulous, the term “edentulous jaw segment” is used. On DPR, it is possible to assess only two-dimensional JDS parameters: height and length. The height of JDS is defined as the distance between the alveolar crest and inferior border of the mandible (Figure 1). The medial and distal borders of the JDS are vertical dividing lines between the evaluated JDS and the medially and distally located JDS borders, respectively.
Figure 1.
Jaw dental segment. (a) Drawing and (b) digital panoramic radiograph showing jaw dental segment (JDS). H, the height of the JDS: the distance between the crest of alveolar ridge and inferior ridge of the mandible; H1, the alveolar bone: the distance from the crest of alveolar ridge to the superior border of the mandibular canal (MC); H2, the basal bone: the distance from the superior border of the MC to the inferior ridge of the mandible; L, the length of the JDS: the distance between vertical lines that divides medial and distal borders of the JDS between the evaluated JDS and the medially and distally located JDSs borders, respectively.
JDS inclusion criteria were left and right mandibular first and second premolar (PM1 and PM2) and first and second molar (M1 and M2) jaw segments in which the MC was in an independent form condition that was dentate or edentulous. JDS exclusion criteria were the presence of mental foramen; impacted tooth or wisdom tooth; dental implant; overlapping JDSs; teeth with <1.0 mm distance between the lamina dura of neighbouring roots or <2.0 mm distance between the root apex and the MC; artefacts or bone pathology (e.g. cysts, inflammation-induced osteosclerosis) presented in any region of the JDS; less than 6 months since tooth extraction; longitudinal tooth axis and mandibular inferior ridge formed at an angle of <60°; and mediodistal length of the edentulous JDS that did not correspond to the mediodistal length of the contralateral tooth crown (if the contralateral JDS was edentulous, then the average of the mediodistal crown values was used).15
Mandibular canal visibility analysis
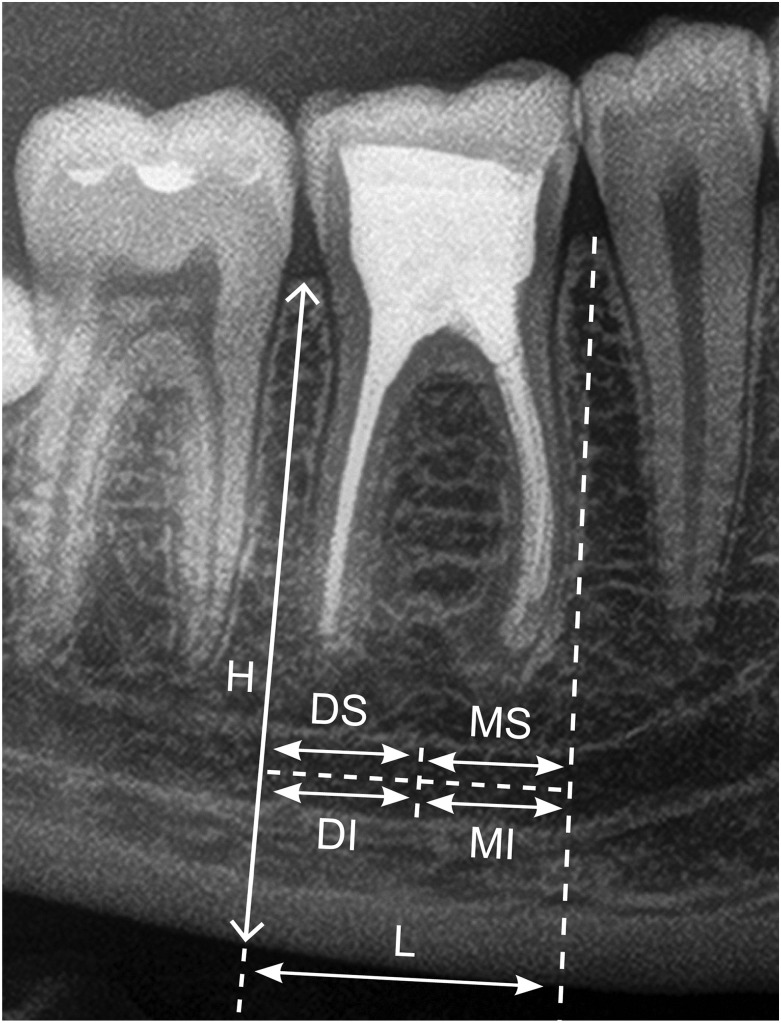
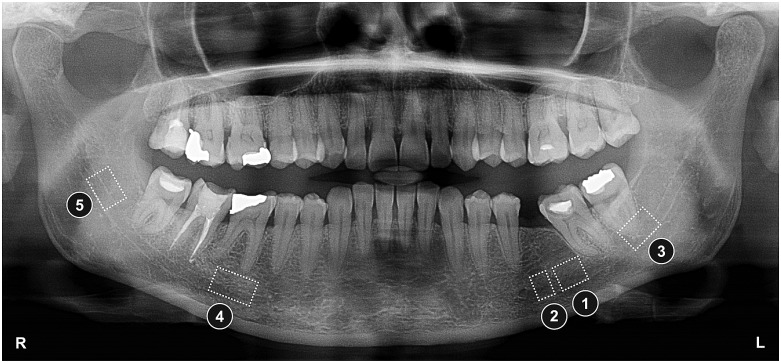
The radiographic image of the MC on DPR is defined as a dark ribbon between two white lines—the bony walls (borders) of the MC.12 MC visibility was scored in a multifunction window (the “measurements” tool was selected without additional settings) for each JDS in the four parts: medial superior, medial inferior, distal superior and distal inferior (Figure 2). Since many anatomical variations can alter the common pattern of MC detection through the course, the visibility scores of the MC part for each JDS were characterized (Figure 3) as 5 (good), 4 (moderate), 3 (poor), 2 (MC border is not visible, but visibility of the dark ribbon is good) or 1 (MC border is not visible, but visibility of the dark ribbon is moderate). A MC part with an identified MC border was scored as 5 or 4, whereas a detectable MC part with unidentified borders was scored as 2 or 1. An unidentified MC part was scored as 3.
Figure 2.
Jaw dental segment (JDS) with mandibular canal parts for visibility evaluation. DI, distal inferior part; DS, distal superior part; H, the height of the JDS; L, the length of the JDS; MI, medial inferior part; MS, medial superior part.
Figure 3.
Digital panoramic radiograph showing samples of the visibility scores of mandibular canal (MC) parts: 5, good; 4, moderate; 3, poor; 2, MC border is not visible, but visibility of the dark ribbon is good; 1, MC border is not visible, but visibility of the dark ribbon is moderate.
Morphometric analysis
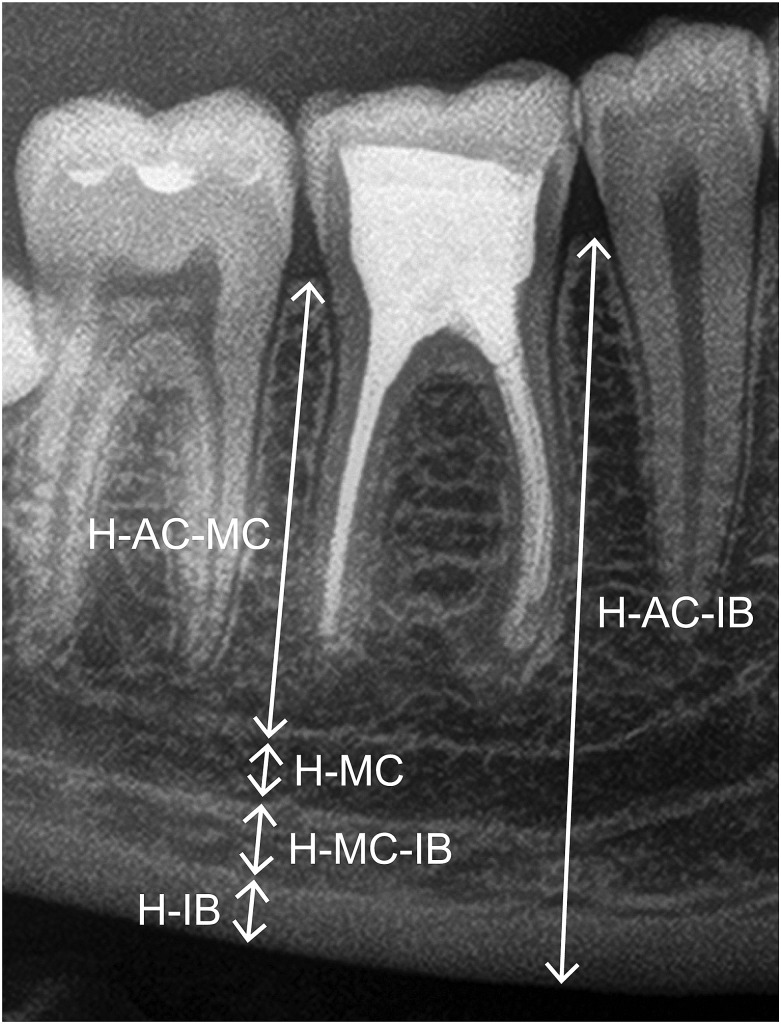
Vertical JDS evaluation was performed using the “measurements” tool without additional adjustments in the medial and distal parts of the segment perpendicular to the inferior mandibular ridge. The centre of the JDS could not be evaluated properly according to the investigation protocol because dentate JDS contains root(s). Figure 4 shows the vertical measurements that were assessed medially and distally for each JDS: (a) the height (H) from the alveolar crest (AC) to the MC dark ribbon (H-AC-MC), including the superior MC border; (b) the height of the MC (H-MC), corresponding to the MC dark ribbon height; (c) the height from the lowest point of the MC dark ribbon to the superior border of the inferior cortical bone (IB) (H-MC-IB); (d) the height of the inferior cortical bone (H-IB); and (e) the height of the mandible (H-AC-IB). Accepted measurement error was ±0.1 mm.
Figure 4.
Morphometric measurements. H-AC-MC, the height from the alveolar crest to the mandibular canal (MC) dark ribbon, including superior MC border; H-MC, the height of the MC, corresponding to the MC dark ribbon height; H-MC-IB, the height from the lowest point of the MC dark ribbon to the superior border of the inferior cortical bone; H-IB, the height of the inferior cortical bone; H-AC-IB, the height of the mandible.
Densitometric analysis
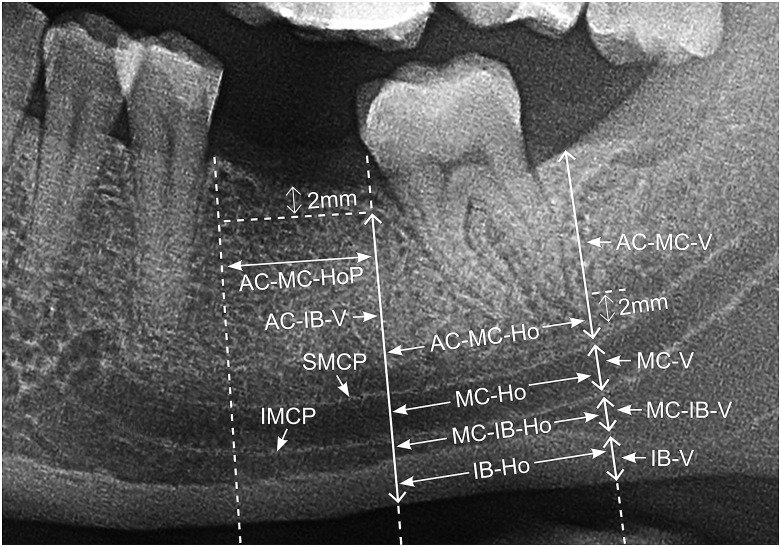
The analysis was made in a multifunction window with the “densitometric analysis” tool selected. The “sharp enhancement” tool was activated for standardization of measurements, and no additional adjustments were used. Figure 5 shows vertical and horizontal measurements in the region of the JDS. The following vertical (V) measurements were made medially and distally: (a) from the alveolar crest in the trabecular bone to the bone 2.0 mm over the MC (AC-MC-V); (b) in the MC region (MC-V); (c) from the trabecular bone below the MC to the superior border of the inferior cortical bone (MC-IB-V); (d) in the inferior cortical bone region (IB-V); (e) from the alveolar crest in the trabecular bone to the end of the inferior cortical bone (AC-IB-V); and (f) at two bone density peaks, the superior MC peak (SMCP) and the inferior MC peak (IMCP), corresponding to the borders of the MC. Horizontal (Ho) densitometric measurements (Figure 5) within JDS mediodistal length were (a) 2.0 mm above the MC (AC-MC-Ho) (the measurement was not taken if the visibility of the superior MC border was poor (the border was not visible)); (b) the MC region (MC-Ho); (c) the trabecular bone below the MC (MC-IB-Ho); (d) the inferior cortical bone region (IB-Ho); (e) 2.0 mm below the superior cortical bone of the edentulous JDS (or the mathematical average of horizontal measurements in the medial and distal parts of the dentate JDS trabecular bone 2.0 mm below the superior cortical bone) when visibility of the MC superior border was poor (AC-MC-HoP). The vertical densitometric analysis line could not have an angle of >30° and must be without overlapping lamina dura or tooth root when artefacts or anatomical structures were present in the region of measurement. Accepted measurement error was ±5 relative measurement units.
Figure 5.
Densitometric measurements. Vertical densitometric measurements: AC-MC-V, from the alveolar crest in the trabecular bone to the bone 2.0 mm over the mandibular canal (MC); MC-V, in the MC region; MC-IB-V, from the trabecular bone below the MC to the superior border of the inferior cortical bone; IB-V, in the inferior cortical bone region; AC-IB-V, from the alveolar crest in the trabecular bone to the end of the inferior cortical bone; SMCP, at the superior MC peak corresponding to the border of the MC; IMCP, at the inferior MC peak corresponding to the border of the MC. Horizontal densitometric measurements: AC-MC-Ho, 2.0 mm above the MC; MC-Ho, the MC region; MC-IB-Ho, the trabecular bone below the MC; IB-Ho, the inferior cortical bone region; AC-MC-HoP, 2.0 mm below the superior cortical bone of the edentulous jaw dental segment (JDS) (or mathematical average of horizontal measurements in medial and distal parts of the dentate JDS trabecular bone 2.0 mm below the superior cortical bone) when visibility of the MC superior border is poor.
MC visibility and densitometric and morphometric analysis results were assessed additionally for possible significant differences between patients' age, gender, JDS condition, side of the mandible or number.
Data and statistical analysis
Statistical analysis was performed by means of IBM SPSS® v. 20.0 for Windows (IBM Corp., New York, NY; formerly SPSS Inc., Chicago, IL). A Kolmogorov–Smirnov test was used for data (distribution of patients according to age) normality evaluation. The sample size was selected randomly using the criteria α = 0.05 (confidence level) and β = 0.8 (power of the study). The sample size was calculated by means of a sample size calculator in the survey software (Creative Research System, Sebastopol, CA). The three-sigma rule was applied for data inclusion before further analyses. The data are presented as mean ± standard error (SE) in millimetres.
Repeated MC visibility evaluations were tested for agreement using Cohen's kappa coefficient. Investigation was simplified for intraobserver agreement evaluation: if an MC part was identified (previous scale grades of 5, 4, 2 or 1), then the visibility score was 1 (logical); if MC visibility was poor (previous scale grade of 3), then the score was 0 (logical).
Descriptive statistics was applied for the morphometric, densitometric and MC visibility analysis. Fisher's exact test served for the MC border parts with the same visibility score comparison. A Pearson χ2 test was used to compare samples of categorical variables. Differences between the two independent samples were calculated using the Mann–Whitney U test.
Statistical significance was considered for p-values <0.05.
Results
The primary sample consisted of 101 patients of Caucasian race. 69 DPRs (68.3%) were scored less than “adequate for diagnosis”9 and were excluded from subsequent evaluation. 32 panoramic radiographs (31.7%) met the requirements of the investigation (mean age of the patient in years 43.7 ± 2.0, range 17–64 years). A total of 155 JDSs were evaluated from the 32 DPRs.
The Kolmogorov–Smirnov test showed normally distributed data (d = 0.09, p > 0.05) of the sample (distribution of patients by age). Distribution of patients of both genders by age was homogeneous. No statistically significant differences (p > 0.05) were identified between JDS condition (edentulous or dentate) and JDS number.
Mandibular canal visibility analysis results
Intraobserver agreement (Cohen's kappa coefficient) for the MC visibility evaluation was almost perfect (Table 1).
Table 1.
Cohen's kappa coefficients (κ) for the visibility of the mandibular canal (MC) parts
| MC part in JDS | κ | CI |
|---|---|---|
| Medial superior | 0.96a | 0.91–1.01 |
| Medial inferior | 0.97a | 0.92–1.01 |
| Distal superior | 0.97a | 0.92–1.01 |
| Distal inferior | 0.88a | 0.80–0.97 |
CI, confidence interval by 95%; JDS, jaw dental segment.
Almost perfect agreement = 0.81–0.99.
Table 2 shows the distribution of MC visibility scores according to the MC border part evaluation. The predominant MC visibility score was 4, with a mathematical average of 40.7%. The most frequent superior MC border visibility value was 4 (42.6–43.0%), and the most common inferior MC visibility value was 5 (43.9–49.5%). The most uncommon MC visibility value was 2 (1.0–7.0%). The medial inferior MC part had no visibility value of 2. In 22.0–24.7% of JDSs, the superior MC border was not visible, more than twice as often as the inferior MC border was not visible (9.1–10.2%). The superior MC border was not visible in 22.0% of the medial parts and 24.7% of the distal parts in all evaluated JDSs. Statistically non-significant differences were identified between the visibility scores for the medial and distal superior and the medial and distal inferior MC border parts (Fisher's exact test, p > 0.05). Statistically significant differences were identified between particular MC visibility scores for the medial superior and medial inferior MC border parts (Fisher's exact test, p < 0.01), as well as between the distal superior and distal inferior MC border parts (Fisher's exact test, p < 0.01) (Table 2).
Table 2.
Mandibular canal (MC) visibility analysis results
| Visibility scores | MC part in JDS |
|||
|---|---|---|---|---|
| Medial superior (I) | Medial inferior (II) | Distal superior (III) | Distal inferior (IV) | |
| 1 | 21.0% | 7.1% | 21.8% | 2.0% |
| I vs II p < 0.001 | II vs III p < 0.001 | III vs IV p < 0.001 | I vs IV p < 0.001 | |
| 2 | 7.0% | – | 3.0% | 1.0% |
| III vs IV p = 0.16 | I vs IV p < 0.001 | |||
| 3 | 22.0% | 10.2% | 24.7% | 9.1% |
| I vs II p < 0.01 | II vs III p < 0.03 | III vs IV p < 0.002 | I vs IV p < 0.006 | |
| 4 | 43.0% | 38.8% | 42.6% | 38.4% |
| I vs II p = 0.24 | II vs III p = 0.23 | III vs IV p = 0.23 | I vs IV p = 0.22 | |
| 5 | 7.0% | 43.9% | 7.9% | 49.5% |
| I vs II p < 0.001 | II vs III p < 0.001 | III vs IV p < 0.001 | I vs IV p < 0.001 | |
JDS, jaw dental segment.
Data are provided as a percentage (%) of the sum of visibility scores of the particular MC border part from all visibility scores of the particular border. Fisher's exact test results (p-value) between the indicated groups are provided below the percentage line.
Statistically non-significant differences were identified between groups I vs III and II vs IV (p > 0.05) and were not provided in the table.
No significant differences were identified between gender and MC visibility score (p > 0.05) or JDS number and MC visibility score (p > 0.05) in any MC visibility evaluation part. There were no differences in MC superior border visibility across ages (p > 0.05). Significant differences were identified between mean age and visibility scores of 4 and 5 for the medial inferior border (p = 0.02). The visibility of the MC medial and distal superior border (p > 0.05) and distal inferior border (p > 0.05) was independent of JDS condition. MC medial inferior border visibility evaluation scores 5 and 3 were dependent on the JDS condition (edentulous or dentate), i.e. statistically significant differences were identified (Fisher's exact test, p = 0.04, odds ratio = 5.67, 95% confidence interval = 4.05–7.94, p-value two-tailed = 0.02). No differences were revealed between the corresponding MC parts of the JDSs in the visibility evaluation of PM1 and PM2 (p > 0.05); PM2 and M1 (p > 0.05); or M1 and M2 (p > 0.05).
MC visibility of particular JDSs did not reveal differences in the MC visibility of corresponding JDSs in the contralateral mandible side (p > 0.05).
Morphometric analysis results and relations to mandibular canal visibility scoring
Table 3 provides morphometric measurement data. The highest SE values were found for the anatomically most-variable measurements: H-AC-MC and H-AC-IB. The lowest values of SE were achieved for MC height as well as for inferior cortical bone height evaluation.
Table 3.
Jaw dental segment (JDS) morphometric analysis results
| Measurement location | Measurement | Mean | SE |
|---|---|---|---|
| Medially | H-AC-MC | 15.6 | 0.4 |
| H-MC | 2.4 | 0.1 | |
| H-MC-IB | 3.8 | 0.1 | |
| H-IB | 3.2 | 0.1 | |
| H-AC-IB | 25.4 | 0.4 | |
| Distally | H-AC-MC | 14.1 | 0.5 |
| H-MC | 2.3 | 0.1 | |
| H-MC-IB | 4.1 | 0.2 | |
| H-IB | 2.8 | 0.1 | |
| H-AC-IB | 23.3 | 0.4 |
SE, standard error.
Measurement location, JDS measurement location medially and distally; H-AC-MC, the height from the alveolar crest to the MC dark ribbon, including superior MC border; H-MC, the height of MC, corresponding to the MC dark ribbon height; H-MC-IB, the height from the lowest point of the MC dark ribbon to the superior border of the inferior cortical bone; H-IB, the height of the inferior cortical bone; H-AC-IB, the height of the mandible.
The data are presented as mean, SE in millimetres.
Morphometric analysis relations to mandibular canal visibility scoring
Analysis of the results revealed statistically non-significant differences between the visibility of the medial superior (p > 0.05) as well as the medial inferior MC (p > 0.05) part and the morphometric analysis results in the medial part of JDS.
MC visibility revealed significant differences in particular morphometric analysis results (Table 4).
Table 4.
Morphometric analysis relations to mandibular canal (MC) visibility scoring
| MC part for visibility evaluation | JDS part for morphometric analysis |
||
|---|---|---|---|
| H-AC-MC | H-MC | H-AC-IB | |
| Distal superior | 1 [12.8 (0.9)] and 4 [15.2 (0.6)] (p = 0.01), 3 [10.2 (0.4)] and 4 [15.2 (0.6)] (p = 0.04) |
1 [2.4 (0.1)] and 3 [1.7(0.1)] (p = 0.04), 3 [1.7 (0.1)] and 4 [2.4 (0.1)] (p = 0.04) |
1 [22.2 (0.7)] and 4 [24.2 (0.6)] (p = 0.04) |
| Distal inferior | 4 [13.3 (1.0)] and 5 [14.6 (0.6)] (p = 0.04) | –a | –a |
JDS, jaw dental segment.
MC part for visibility evaluation: JDS MC visibility evaluation in distal superior and distal inferior part (in visibility scores: 1, 2, 3, 4, 5); JDS part for morphometric analysis: JDS measurement part for morphometric analysis {measurement values are presented as mean [standard error (SE)] in millimetres}: H-AC-MC, the height from the alveolar crest to the MC dark ribbon; H-MC, the height of the MC; H-AC-IB, the height of the mandible.
Statistically significant differences are presented: “visibility score [morphometric analysis value (SE)]” and “visibility score [morphometric analysis value (SE)]” “(p-value)”.
“–” indicates no statistically significant difference (p > 0.05).
Densitometric analysis results in relation to mandibular canal visibility scoring
Densitometric analysis results are provided in Table 5. Significant differences were identified (p < 0.05) between the corresponding results of medial and distal densitometric analyses in the vertical direction of JDS.
Table 5.
Jaw dental segment (JDS) densitometric analysis results in vertical and horizontal directions
| Measurement location | Measurement direction | Measurement | Mean | SE |
|---|---|---|---|---|
| Medially | Vertically | AC-MC-V | 106.0 | 2.4 |
| MC-V | 89.2 | 2.8 | ||
| MC-IB-V | 89.2 | 2.8 | ||
| IB-V | 97.7 | 2.7 | ||
| AC-IB-V | 100.4 | 2.3 | ||
| SMCP | 108.1 | 3.1 | ||
| IMCP | 105.2 | 2.6 | ||
| Distally | AC-MC-V | 122.7 | 2.5 | |
| MC-V | 103.1 | 2.8 | ||
| MC-IB-V | 97.4 | 2.5 | ||
| IB-V | 100.4 | 2.1 | ||
| AC-IB-V | 109.8 | 2.0 | ||
| SMCP | 117.8 | 3.1 | ||
| IMCP | 114.1 | 2.6 | ||
| Horizontally | AC-MC-Ho | 108.4 | 3.1 | |
| MC-Ho | 93.1 | 2.4 | ||
| MC-IB-Ho | 92.3 | 2.6 | ||
| IB-Ho | 101.5 | 2.2 | ||
| AC-MC-HoP | 111.2 | 4.4 |
SE, standard error.
Measurement location, JDS measurement location medially and distally; Measurement direction, vertically and horizontally; Measurement: AC-MC-V, from the alveolar crest in the trabecular bone to the bone 2.0 mm over the MC; MC-V, in the MC region; MC-IB-V, from the trabecular bone below the MC to the superior border of the inferior cortical bone; IB-V, in the inferior cortical bone region; AC-IB-V, from the alveolar crest in the trabecular bone to the end of the inferior cortical bone; SMCP, at the superior MC peak corresponding to the border of the MC; IMCP, at the inferior MC peak corresponding to the border of the MC; AC-MC-Ho, 2.0 mm above the MC; MC-Ho, the MC region; MC-IB-Ho, the trabecular bone below the MC; IB-Ho, the inferior cortical bone region; AC-MC-HoP, 2.0 mm below the superior cortical bone of the edentulous JDS (or mathematical average of horizontal measurements in medial and distal parts of the dentate JDS trabecular bone 2.0 mm below the superior cortical bone) when visibility of the MC superior border is poor.
Measurement values are presented as mean, SE (standard error) in relative measurement units.
Vertical densitometric analysis in relation to mandibular canal visibility scoring
Non-significant differences were found between the visibility analysis results of the medial superior MC and the densitometric analysis results of the vertical medial part (p > 0.05). The results provided no statistically significant differences between the distally evaluated visibility of the inferior MC part and vertical densitometric analysis results in the distal part of the JDS (p > 0.05). Statistically significant differences between the MC visibility scores and the vertical densitometric analysis results are provided in Table 6.
Table 6.
Vertical densitometric analysis in relation to mandibular canal (MC) visibility scoring
| MC part for visibility evaluation | JDS part for vertical densitometric analysis |
||||||
|---|---|---|---|---|---|---|---|
| AC-MC-V | MC-V | MC-IB-V | IB-V | AC-IB-V | SMCP | IMCP | |
| Medial inferior | –a | 4 [97.1 (4.2)] and 5 [81.5 (3.9)] (p = 0.01) | –a | 1 [111.4 (5.6)] and 5 [89.6 (4.3)] (p = 0.03), 3 [121.2 (4.2)] and 4 [98.6 (4.2)] (p = 0.02), 3 [121.2 (4.2)] and 5 [89.6 (4.3)] (p = 0.01) |
3 [115.7 (7.0)] and 5 [95.1 (3.5)] (p = 0.04) | 1 [122.4 (7.5)] and 5 [99.3 (4.8)] (p = 0.04), 4 [114.3 (4.1)] and 5 [99.3 (4.8)] (p = 0.02) |
–a |
| Distal superior | 4 [119.7 (3.5)] and 5 [142.0 (8.5)] (p = 0.03) | –a | 4 [91.7 (3.7)] and 5 [110 (7.6)] (p = 0.04) | 4 [95.3 (3.2)] and 5 [111.5 (2.2)] (p = 0.04) | 1 [107.0 (4.5)] and 5 [124.6 (5.4)] (p = 0.04), 4 [106.9 (2.6)] and 5 [124.6 (5.4)] (p = 0.01) |
–a | 4 [110.3 (3.4)] and 5 (127.4 (6.8)] (p = 0.04) |
JDS, jaw dental segment; SE, standard error.
MC part for visibility evaluation, JDS MC visibility evaluation in medial inferior and distal superior parts (in visibility scores: 1, 2, 3, 4, 5); JDS part for vertical densitometric analysis: JDS measurement part for vertical densitometric analysis [measurement values are presented as mean (SE) in relative measurement units]: AC-MC-V, from the alveolar crest in the trabecular bone to the bone 2.0 mm over the MC; MC-V, in the MC region; MC-IB-V, from the trabecular bone below the MC to the superior border of the inferior cortical bone; IB-V, in the inferior cortical bone region; AC-IB-V, from the alveolar crest in the trabecular bone to the end of the inferior cortical bone; SMCP, at superior MC peak corresponding to the border of MC; IMCP, at inferior MC peak corresponding to the border of MC.
Statistically significant results are presented: “visibility score [vertical densitometric analysis value (SE)]” and “visibility score [vertical densitometric analysis value (SE)]” “(p-value)”.
“–” indicates no statistically significant difference.
Horizontal densitometric analysis in relation to mandibular canal visibility scoring
The results provided statistically non-significant differences between the visibility of the medial superior (p > 0.05) as well as distal inferior MC parts (p > 0.05) and the horizontal densitometric analysis results of the JDS.
MC visibility evaluation results were significantly different from particular horizontal densitometric analysis results (p < 0.05) (Table 7).
Table 7.
Horizontal densitometric analysis in relation to mandibular canal (MC) visibility scoring
| MC part for visibility evaluation | JDS part for horizontal densitometric analysis |
||
|---|---|---|---|
| MC-IB-Ho | IB-Ho | AC-MC-HoP | |
| Medial inferior | –a | 1 [113.9 (6.5)] and 5 [94.5 (3.6)] (p = 0.04), 3 [112.2 (5.0)] and 5 [94.5 (3.6)] (p = 0.02) |
1 [133.9 (12.0)] and 4 [96.0 (7.2)] (p = 0.03) |
| Distal superior | 4 [85.6 (3.6)] and 5 [108.2 (9.0)] (p = 0.02) | 3 [106.7 (3.9)] and 4 [96.4 (3.1)] (p = 0.04) | –a |
JDS, jaw dental segment.
MC part for visibility evaluation, JDS mandibular canal visibility evaluation in medial inferior and distal superior parts [visibility scores (1, 2, 3, 4, 5) in pairs]; JDS part for horizontal densitometric analysis, JDS measurement part for horizontal densitometric analysis: MC-IB-Ho, the trabecular bone below the MC; IB-Ho, the inferior cortical bone region; AC-MC-HoP, 2.0 mm below the superior cortical bone of the edentulous JDS (or mathematical average of horizontal measurements in medial and distal parts of the dentate JDS trabecular bone 2.0 mm below the superior cortical bone) when visibility of the MC superior border is poor {measurement values are presented as mean [standard error (SE)] in relative measurement units}.
Statistically significant results are presented: “visibility score [horizontal densitometric analysis value (SE)]” and “visibility score [horizontal densitometric analysis value (SE)]” “(p-value)”.
“–” indicates no statistically significant difference.
Discussion
The “as low as reasonably achievable” principle is of high importance for widespread dental implant surgery. The clinician can choose from several radiographic investigation methods to evaluate the alveolar ridge height and width for prosthetic implant placement. In many cases, a treatment plan cannot be composed without panoramic radiograph evaluation, even for an edentulous JDS in the region of MC, because the H-AC-MC distance must be measured.15 Precise investigation requires more advanced investigation methods, such as CBCT. Otherwise, there is still discussion about the application of panoramic radiography in clinical practice to facilitate treatment planning. Digital technologies are rapidly replacing analogue imaging techniques in dentistry. Updates to devices and software are periodically available. The software contains linear measurement tools, including a densitometric analysis tool. We noted the absence of investigations on the possibility of evaluating MC visibility using DPRs. Hence, we aimed to evaluate MC and the visibility of its walls by means of dedicated software (linear and densitometric analysis tools).
It is difficult to achieve optimal- or high-quality panoramic radiographs. Quality requirements were met in only 31.7% of the DPRs in our study. Similarly, Rumberg et al16 found 33% of their panoramic radiographs to be of acceptable quality. The percentage of the JDSs evaluated in the regions of PM1, PM2, M1 and M2 cannot be the same because of the study protocol requirements for inclusion. JDSs were not included in the study if they contained the mental foramen. A common horizontal position of the mental foramen (for Caucasian individuals) can be found in the premolar region.17
Detailed MC evaluation was introduced due to variability of visibility through the course of the MC. The 5-point scale (Figure 3) was suggested during the present study for the comprehensive evaluation of MC visibility for the medial, distal, inferior and superior parts of each JDS. Various 3-, 4- and 5-point MC visibility rating scales have been proposed by investigators.7,18,19 Oliveira-Santos et al12 used two scores for the evaluation of separate MC regions, whereas the overall MC visibility score was the sum of the six evaluated regions. MC depiction in another study was classified into three types for each implant site: visible in the superior and inferior walls; visible in the inferior walls and invisible in the superior walls; or invisible in the superior and inferior walls.20
Agreement between observers' repeated MC visibility evaluations of one investigator's findings (Table 1) was almost perfect (a reflection of consistent measurements throughout the study) and coincided with the results of other investigators' data.12
The different visibility of the MC borders in the mediodistal and vertical directions was confirmed by the current study (Table 2). The most uncommon MC visibility score was two for the evaluation of the inferior and superior MC borders, and the MC tended to have better visibility when the borders were present. This tendency agrees with other investigations, showing the importance of the MC border for MC visibility.12,21,22 The superior medial and superior distal parts of the MC border had visibility score 3 in 22.0% and 24.7% of the sample, respectively, which is similar to data from investigation of Jung and Cho.23 Naitoh et al20 found the MC superior wall to be invisible in 31.7% of designed implant sites, whereas the investigation of Klinge et al24 with specimen cadavers demonstrated an invisible MC in 36.1% (the superior and inferior borders of MC were not distinguished). Therefore, it could be concluded from our study that the three-dimensional evaluation of JDSs should be recommended for further analysis of MC in about 25% of JDSs if the identification of the superior MC border is obligatory. In comparison, the MC was not visible in 0.2% of the third molar (M3) regions, 5.7% of the M2 regions and 8.2% of the M1 regions in the CBCT images. Of more importance for this study was that the superior MC border could be identified in 75.3% of distal parts and 78.0% of medial parts. We could not get data from the literature to make a clinical comparison with our results for the medial and distal parts of the MC superior border.
It is interesting to know that anatomically trabeculated MC walls tend to be denser in the upper part than the lower part, but MC visibility does not have a similar tendency, according to our study and to that of Wadu et al.21 The last-mentioned sources supplement the statement that radiographic identification of the superior MC border cannot directly relate to MC border density and cannot have a prognostic value for MC damage during implant surgery. Furthermore, the multiple accessory canals directed toward root apices while leaving the MC could have a negative influence on trabeculation and the radiographic visibility of the superior MC border. However, our study results did not confirm the statement that superior or inferior MC border visibility is related to JDS condition in partially dentate lower jaws (with one exception between scores 5 and 3 for the visibility evaluation of the medial and inferior parts of the MC border) and coincide with the CBCT study results.12
The present study results confirmed (Table 2) that the superior MC border has lower visibility scores more often than the inferior MC border. Non-significant differences were identified between numbers of moderate visibility scores for both MC borders. Conversely, the superior border received the score 4 more than twice as often as the inferior border. These data tend to use the inferior MC border as a reference point for the identification of the imagined superior MC border in implant planning, whereas the diameter of the MC can be measured using other parts of the panoramic radiograph or by means of MC height (e.g. from our study). Indeed, this idea should be avoided because of the unreliable data. Wadu et al21 recognized and demonstrated a tendency to identify fine or non-existent structures. Furthermore, worldwide studies provide different mean MC diameters from 2 to about 5 mm with probable relation to race.25 Even bifid MC can be identified in 0.08–65% of radiographs, depending on the investigation method.25 The position of the mental foramen varies in horizontal and vertical planes and is related to race. The accessory mental foramen can be identified in 1.4–10% in patients of different populations.17 Misidentification of these structures may lead to serious complications during implant surgery.
It is important to mention that the current study provides data with no difference between the visibility scores for the medial and distal superior MC borders and the medial and distal inferior MC borders (Table 2). It was considered that the clinician should not expect to observe differences in the visibility of corresponding MC parts of particular JDSs or even between neighbouring or other JDSs—that is, MC visibility did not change through the course, contrary to other investigators' results.12,21,23 This statement could not be applied to MC visibility in the mandibular ramus, the M3 JDS region or the mental canal region, as these regions were not included in our study protocol. There were no differences between any pair of corresponding bilateral JDSs in any of the four visibility evaluations of the MC parts. Similarly, researchers found no difference between MC visibility on the left and right sides.12,23
Our results revealed that MC visibility was not related to the subject's gender or age. Significant differences were only identified between the means of age groups with visibility scores of 4 and 5 for the medial inferior MC border part, but this does not reflect a general tendency. This can be explained by the fact that patients included in the study were systematically healthy or had mild systemic diseases. The bone anatomy and endocrine system function could have influenced MC visibility.26
It is interesting to know that we could not find any analogous studies confirming MC border visibility in relation to the region of each JDS and related regions.
A morphometric analysis of separate JDS parts (Figure 4) was necessary before evaluating the relations between the morphometric analysis and the MC visibility scoring. Our measurements of MC height were within the range demonstrated in the summary that Juodzbalys et al25 provided of MC vertical linear evaluations made by various authors. We found that the mean distance from the alveolar crest to the MC was similar to the review results25 and was the most variable linear height measurement (SE was 0.4–0.5 mm) in the present study. It confirms a widely known requirement for individual implant length planning while alveolar ridge height is variable.
It is important to consider that the morphometric measurements did not correlate with MC visibility in our study (Table 4). For example, no significant differences were identified between the medially evaluated morphometric parameters of JDS and the corresponding MC visibility scores. By contrast, some differences were identified in the distally evaluated morphometric parameters of JDS.
The analysis of MC densitometric assessment data and visible MC depiction revealed controversial results. The corresponding vertical (Table 6) and horizontal (Table 7) densitometry did not provide statistically significant differences from the visibility analysis results in the medial superior parts of the MC, but some differences were found in the distal superior parts. We expected to identify similar differences for the inferior MC border in the mediodistal direction, but the results were the opposite: some significant differences were identified for the inferior medial parts of JDS, whereas no significant differences were identified for the distal parts. The results might have differed for the superior and inferior MC borders due to significant differences in densitometric analysis results for medial and distal JDS parts in the vertical direction. However, this would not explain the same differences when a comparison was made between MC visibility and horizontal densitometric analysis data. Based on these results, we concluded that the success in visually identifying MC borders did not correlate with the densitometric depiction of the MC borders (peaks).
Our investigation provides results indicating the limited accuracy of the densitometric tool for the possible improvement of radiographic MC identification. Naitoh et al20 found relations between MC depiction in DPRs and bone density in the alveolar region, but they evaluated bone density by multislice CT in HUs. HUs give the relative density of tissue according to a calibrated scale. HUs were found to be stable after quality phantom scanning with an multislice CT scanner.27 To our knowledge, there is no data in the literature regarding the investigation of the densitometric analysis tool used. The region of interest could not be modified (one standard line could be drawn without entering the desirable area). We found this to be a drawback, as a bigger and standardized region of interest should provide more stable results in the investigated region, especially in the region of MC with variable visibility. The densitometric analysis tool was tested with several enhancements that were provided prior to the investigation. The results varied and depended on the chosen enhancement tool. “Sharp enhancement” was chosen to standardize the measurements. We recommend conducting additional investigations for the validation of the densitometric tool with the inclusion of a quality control phantom. If the results are positive, a new investigation with a bigger sample is recommended.
In conclusion, evaluation of the visibility of the MC superior and inferior borders on DPRs depends on multiple factors without priority of gender, age, JDS location and condition, particular mandibular height parameter measurements or anatomically specific area evaluation with the dedicated densitometric analysis tool. The MC visibility of particular JDSs does not change significantly from the MC visibility of medially and distally located neighbouring JDSs. Particular differences between the visibility of the superior and inferior MC borders were identified to produce a clinically more important conclusion: the superior MC border was not visible more than twice as often as the inferior MC border.
Contributor Information
Marius Kubilius, Email: mariuskubilius@yahoo.com.
Gintaras Juodžbalys, Email: gintaras@stilusoptimus.lt.
References
- 1.Juodzbalys G, Wang HL, Sabalys G. Injury of the inferior alveolar nerve during implant placement: a literature review. J Oral Maxillofac Res 2011; 2: e1. doi: http://dx.doi.org/10.5037/jomr.2011.2101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tay AB, Zuniga JR. Clinical characteristics of trigeminal nerve injury referrals to a university centre. Int J Oral Maxillofac Surg 2007; 36: 922–7. doi: http://dx.doi.org/10.1016/j.ijom.2007.03.012 [DOI] [PubMed] [Google Scholar]
- 3.SEDENTEXCT Project. Radiation protection: cone beam CT for dental and maxillofacial radiology. Evidence Based Guidelines. Radiation protection no. 172. Luxembourg: European Commission; 2012 [cited 17 May 2016]. Available from: http://www.sedentexct.eu/files/radiation_protection_172.pdf
- 4.Tyndall DA, Price JB, Tetradis S, Ganz SD, Hildebolt C, Scarfe WC, et al. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 113: 817–26. doi: http://dx.doi.org/10.1016/j.oooo.2012.03.005 [DOI] [PubMed] [Google Scholar]
- 5.Harris D, Horner K, Gröndahl K, Jacobs R, Helmrot E, Benic GI, et al. E.A.O. guidelines for the use of diagnostic imaging in implant dentistry 2011. A consensus workshop organized by the European Association for Osseointegration at the Medical University of Warsaw. Clin Oral Implants Res 2012; 23: 1243–53. doi: http://dx.doi.org/10.1111/j.1600-0501.2012.02441.x [DOI] [PubMed] [Google Scholar]
- 6.Bornstein MM, Scarfe WC, Vaughn VM, Jacobs R. Cone beam computed tomography in implant dentistry: a systematic review focusing on guidelines, indications, and radiation dose risks. Int J Oral Maxillofac Implants 2014; 29: 55–77. doi: http://dx.doi.org/10.11607/jomi.2014suppl.g1.4 [DOI] [PubMed] [Google Scholar]
- 7.Jacobs R, Mraiwa N, Van Steenberghe D, Sanderink G, Quirynen M. Appearance of the mandibular incisive canal on panoramic radiographs. Surg Radiol Anat 2004; 26: 329–33. doi: http://dx.doi.org/10.1007/s00276-004-0242-2 [DOI] [PubMed] [Google Scholar]
- 8.Devlin H, Yuan J. Object position and image magnification in dental panoramic radiography: a theoretical analysis. Dentomaxillofac Radiol 2013; 42: 29951683. doi: http://dx.doi.org/10.1259/dmfr/29951683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi BR, Choi DH, Huh KH, Yi WJ, Heo MS, Choi SC, et al. Clinical image quality evaluation for panoramic radiography in Korean dental clinics. Imaging Sci Dent 2012; 42: 183–90. doi: http://dx.doi.org/10.5624/isd.2012.42.3.183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bartling R, Freeman K, Kraut RA. The incidence of altered sensation of the mental nerve after mandibular implant placement. J Oral Maxillofac Surg 1999; 57: 1408–12. doi: http://dx.doi.org/10.1016/S0278-2391(99)90720-6 [DOI] [PubMed] [Google Scholar]
- 11.Mehra A, Pai KM. Evaluation of dimensional accuracy of panoramic cross-sectional tomography, its ability to identify the inferior alveolar canal, and its impact on estimation of appropriate implant dimensions in the mandibular posterior region. Clin Implant Dent Relat Res 2012; 14: 100–11. doi: http://dx.doi.org/10.1111/j.1708-8208.2009.00226.x [DOI] [PubMed] [Google Scholar]
- 12.Oliveira-Santos C, Capelozza AL, Dezzoti MS, Fischer CM, Poleti ML, Rubira-Bullen IR. Visibility of the mandibular canal on CBCT cross-sectional images. J Appl Oral Sci 2011; 19: 240–3. doi: http://dx.doi.org/10.1590/S1678-77572011000300011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Juodzbalys G, Raustia AM. Accuracy of clinical and radiological classification of the jawbone anatomy for implantation—a survey of 374 patients. J Oral Implantol 2004; 30: 30–9. doi: http://dx.doi.org/10.1563/1548-1336(2004)030<0030:AOCARC>2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- 14.Gijbels F, De Meyer AM, Bou Serhal C, Van den Bossche C, Declerck J, Persoons M, et al. The subjective image quality of direct digital and conventional panoramic radiography. Clin Oral Investig 2000; 4: 162–7. doi: http://dx.doi.org/10.1007/s007840000059 [DOI] [PubMed] [Google Scholar]
- 15.Angelopoulos C, Thomas SL, Hechler S, Parissis N, Hlavacek M. Comparison between digital panoramic radiography and cone-beam computed tomography for the identification of the mandibular canal as part of presurgical dental implant assessment. J Oral Maxillofac Surg 2008; 66: 2130–5. doi: http://dx.doi.org/10.1016/j.joms.2008.06.021 [DOI] [PubMed] [Google Scholar]
- 16.Rumberg H, Hollender L, Oda D. Assessing the quality of radiographs accompanying biopsy specimens. J Am Dent Assoc 1996; 127: 363–8. doi: http://dx.doi.org/10.14219/jada.archive.1996.0207 [DOI] [PubMed] [Google Scholar]
- 17.Juodzbalys G, Wang HL, Sabalys G. Anatomy of mandibular vital structures. Part II: mandibular incisive canal, mental foramen and associated neurovascular bundles in relation with dental implantology. J Oral Maxillofac Res 2010; 1: e3. doi: http://dx.doi.org/10.5037/jomr.2010.1103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lindh C, Petersson A, Klinge B. Visualisation of the mandibular canal by different radiographic techniques. Clin Oral Implants Res 1992; 3: 90–7. doi: http://dx.doi.org/10.1034/j.1600-0501.1992.030207.x [DOI] [PubMed] [Google Scholar]
- 19.Yasar F, Yesilova E, Apaydin B. The effects of compression on the image quality of digital panoramic radiographs. Clin Oral Investig 2012; 16: 719–26. doi: http://dx.doi.org/10.1007/s00784-011-0587-y [DOI] [PubMed] [Google Scholar]
- 20.Naitoh M, Katsumata A, Kubota Y, Hayashi M, Ariji E. Relationship between cancellous bone density and mandibular canal depiction. Implant Dent 2009; 18: 112–18. doi: http://dx.doi.org/10.1097/ID.0b013e318198da7e [DOI] [PubMed] [Google Scholar]
- 21.Wadu SG, Penhall B, Townsend GC. Morphological variability of the human inferior alveolar nerve. Clin Anat 1997; 10: 82–7. doi: http://dx.doi.org/10.1002/(SICI)1098-2353(1997)10:2<82::AID-CA2>3.0.CO;2-V [DOI] [PubMed] [Google Scholar]
- 22.Naitoh M, Yoshida K, Nakahara K, Gotoh K, Ariji E. Demonstration of the accessory mental foramen using rotational panoramic radiography compared with cone-beam computed tomography. Clin Oral Implants Res 2011; 22: 1415–19. doi: http://dx.doi.org/10.1111/j.1600-0501.2010.02116.x [DOI] [PubMed] [Google Scholar]
- 23.Jung YH, Cho BH. Radiographic evaluation of the course and visibility of the mandibular canal. Imaging Sci Dent 2014; 44: 273–8. doi: http://dx.doi.org/10.5624/isd.2014.44.4.273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Klinge B, Petersson A, Maly P. Location of the mandibular canal: comparison of macroscopic findings, conventional radiography, and computed tomography. Int J Oral Maxillofac Implants 1989; 4: 327–32. [PubMed] [Google Scholar]
- 25.Juodzbalys G, Wang HL, Sabalys G. Anatomy of mandibular vital structures. Part I: mandibular canal and inferior alveolar neurovascular bundle in relation with dental implantology. J Oral Maxillofac Res 2010; 1: e2. doi: http://dx.doi.org/10.5037/jomr.2010.1102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mirza F, Canalis E. Management of endocrine disease: secondary osteoporosis: pathophysiology and management. Eur J Endocrinol 2015; 173: R131–51. doi: http://dx.doi.org/10.1530/EJE-15-0118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nackaerts O, Maes F, Yan H, Couto Souza P, Pauwels R, Jacobs R. Analysis of intensity variability in multislice and cone beam computed tomography. Clin Oral Implants Res 2011; 22: 873–9. doi: http://dx.doi.org/10.1111/j.1600-0501.2010.02076.x [DOI] [PubMed] [Google Scholar]