Abstract
Objectives:
To detect and determine image error and artefact types in intraoral radiographs obtained with photostimulable phosphor (PSP) technology, place them in an appropriate classification and retrospectively analyze the PSP-specific image errors and artefacts. The causes and solutions of PSP-specific errors and artefacts have also been discussed.
Methods:
The radiographic database of Ondokuz Mayis University, Faculty of Dentistry, Department of Dentomaxillofacial Radiology, was used for this study. Different types of image errors and artefacts observed on intraoral radiographs during 2014–15 were detected and defined. A total of 2100 intraoral radiographs were individually evaluated for the distribution of PSP-specific image artefacts.
Results:
There were 34 image error and artefact types detected and classified into 4 groups according to the causative factors. The most common PSP-specific image artefacts were found in fading with a ratio of 44.1% for the ambient light-related group, peeling of the plate borders with a ratio of 53.4% for the PSP plate-related group and straight line with a ratio of 42.2% for the scanner-related group.
Conclusions:
The determination and definition of the image errors and artefacts with clarification of their causes and solutions are important for the improvement of radiographic quality and the reduction of the retake ratio.
Introduction
Photostimulable phosphor (PSP) plates are still widely used as receptors in intraoral radiography.These image receptors allow indirect digital image acquisition; more specifically, after the exposure, latent image occurs on the plate, it is then converted to a digital radiographic four image via a scanning device. Generally, PSP plate-based radiographic systems are named as “computed radiography” (CR) and the term “digital radiography” is preferred for the solid-state detector-based imaging. Advantages of CR include having cordless and flexible plates, having similar structural features to well-known conventional films, being easily manipulated, the option of changing image adjustments via software, lower dose requirements, a wide dose latitude, the elimination of chemical processes, an ease of storage, sharing and replication.1–5
The integration of these relatively new imaging technologies in dental radiographic practices has brought about innovations that have to be understood for a proper examination. Incorrect manipulations and technical errors during both acquisition and processing of the images may cause distinctive radiographic errors and artefacts. Thus, the optimal radiographic examination for an area of interest cannot be performed, which may lead to a misdiagnosis. Determining and clarifying the mechanisms of these mistakes is essential in overcoming these errors and artefacts.
The aim of this study was to detect and determine image error and artefact types in intraoral radiographs obtained with PSP technology, place them in an appropriate classification and retrospectively analyze the detected PSP-specific image artefacts. Evaluation includes a large number of PSP-based radiographs acquired in one university dental hospital. The causes and solutions of the errors and artefacts which are specific to PSP-based intraoral imaging have also been discussed.
Methods and materials
The study protocol was approved by the university institutional review board. The radiographic database of Ondokuz Mayıs University, Faculty of Dentistry, Department of Dentomaxillofacial Radiology, was used for this study.
Exposures were performed with two Sirona Heliodent Plus dental X-ray machines with parameters of 60 kVp and 7 mA (Sirona Dental Systems GmbH, Bensheim, Germany). All radiographs were obtained with the bisecting angle technique using VistaScan image plates and scanning procedures were performed with a VistaScan Combi scanner using a standard scanning mode that allowed for a 50-µm pixel size and a 10-lp/mm theoretical spatial resolution (Dürr Dental GmbH & Co. KG, Bietigheim-Bissingen, Germany). The images were transferred to the HBYS Hospital information management system computer program (Turcasoft Software Ltd., Samsun, Turkey) and evaluated on a 20.1-inch Dome GX2MP Plus monitor (NDS Surgical Imaging, LLC, San Jose, CA). The evaluation was performed in the reporting room that has semi-dark lighting condition.
This study consisted of two parts. In the first part, different types of image errors and artefacts observed on intraoral radiographs during 2014–15 were detected and defined. Possible causes and solutions of these errors and artefacts were determined through consideration of the materials and image acquisition process of faulty radiographs.
In the second part, 2100 intraoral radiographs were collected from the patient records in September 2015, which is the following month of major revision of the plates being used. These radiographs were individually evaluated for the absence or presence of all defined image errors and artefacts. All of the radiographs were evaluated by one observer. Selected 50 radiographs were revaluated after 2 weeks for the determination of intraobserver reliability.
Statistical analyses were performed with IBM SPSS® Statistics v. 21 (IBM Corp., New York, NY; formerly SPSS Inc., Chicago, IL), and the frequency and percentage of image errors and artefacts were determined. Intraobserver reliability was analyzed with kappa analyses.
Results
Image error and artefact types
There were 34 image error and artefact types detected and classified into 4 groups according to the causative factors. The four groups included: (1) operator- and patient-induced, (2) ambient light-induced, (3) PSP plate-induced and (4) scanner-induced errors and artefacts. The first group was formed with 11 errors that were well known already from long-existing techniques. The following 3 groups were formed with a total of 23 PSP-specific image artefacts and errors.
Operator- and patient-induced errors and artefacts
Well-known projection errors including cone cutting, crown cut-off, apices cut-off, incorrect dot position, non-parallel position to an occlusion, shortening, elongation, superimposition and movement errors may be observed with CR because these errors are independent of image receptor type. A mirror image occurs when the sheathed plate is incorrectly positioned in the mouth or the plate is inversely inserted into the sheath. Double exposure of the PSP plates without scanning or improper erasure of a previously acquired latent image is a cause of a double image.
Ambient light-induced artefacts and errors
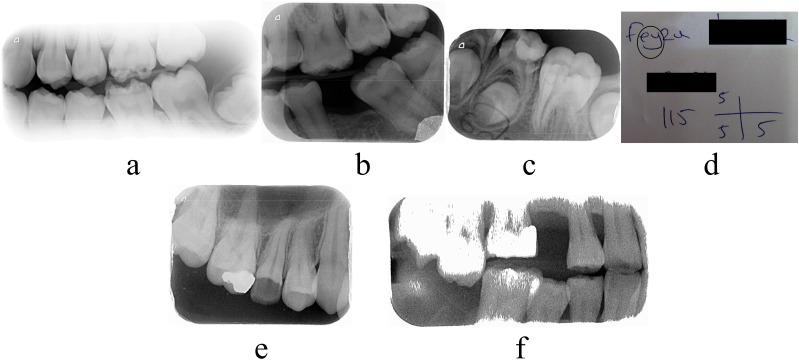
Table 1 shows the ambient light-induced artefacts and errors with their definitions, reasons and preventions. Mentioned artefacts and errors are shown in Figure 1.
Table 1.
Ambient light-induced artefacts and errors
| Error/artefact name | Definition | Reason | Prevention |
|---|---|---|---|
| Fading | Brighter radiographic image than usual, which is almost always correctable with image adjustment tools | Ambient light exposure of the unsheathed plate because of delayed scanning, tolerable spontaneous releasing of the electrons that form the latent image and reduced output signal that causes incorrect initial image density optimization | Plates should not be removed from their sheaths until just before the scanning procedure and unsheathed plates should not be overlapped with anything, advice from the manufacturers must be considered for the ambient light intensity and plates should be scanned as soon as possible after exposure |
| Non-uniform image density | Two or more radiographic areas on the image that exhibit different densities for same structures | Partial ambient light exposure of the plate generally because of the overlapped unsheathed plates and fading on the exposed area | |
| Text pattern | A readable text part on the radiographic image due to the density differences | Hanging on the exposed and unsheathed plate overlapped with the paper, on which patient information is written. Light transition on the unwritten part of paper and fading on the associated image area. Absorption and normal density on the written part | |
| Noisy image | Grainy image that exhibits random density variations for the same structural areas | Spontaneous releasing of electrons that creates uncorrectable changes to the latent image owing to delayed scanning and too much ambient light intensity and exposure | |
| Shining | Pure white areas generally formed at the centre of radiopaque structures and peripheral borders of the image | Total loss of the gained signal at the associated areas due to excessive spontaneous releasing |
Figure 1.
(a) Ambient light-related fading on the left bitewing radiograph; (b) non-uniform image density on the left bitewing radiograph; (c) text pattern on the mandibular left posterior periapical radiograph; (d) the circled area is indicating the associated writing part which has caused the text pattern artefact on the radiograph in (c); (e) fading and noisy image on the maxillary right posterior periapical radiograph; (f) significant noisy image and shining areas caused by total signal loss on the right bitewing radiograph.
Photostimulable phosphor plate-induced artefacts and errors
PSP plate-induced artefacts and errors basically have two main causative factors such as photostimulating luminescence layer damage and dirt on the plate. Table 2 and Figure 2 shows the photostimulating luminescence layer damage-related artefacts and errors. Table 3 and Figure 3 show dirt on the plate-related artefacts and errors.
Table 2.
Photostimulating luminescence layer damage-related photostimulable phosphor (PSP) plate-induced artefacts and errors
| Error/artefact name | Definition | Reason | Prevention |
|---|---|---|---|
| Cracking | Linear, irregular radiopaque line, mostly at the occlusion level of the bitewing radiographs. Generally, a polyester base of the plate is bent irreversibly on the associated area | Excessive bending and rough manipulation, which generate irreversible damage on the photostimulating luminescence layer and polyester base | Gentle manipulation of the plate by the operator at each step of the image acquisition and controlled biting of the bitewing and occlusal radiographs |
| Scratches | Small, smooth linear opacities anywhere on the image | Photostimulating luminescence layer damage without bending of the polyester base | |
| Peeling of the plate borders | Corruption and irregularity at the borders of radiographic image and plate | Peeling of the protective and photostimulating luminescence layer of the PSP plate borders as a result of friction when the plate is placed into the foil cassette (a special plate carrier of the VistaScan Combi Plus scanner) | |
| Bite-marks | Small multiple irregular radiopaque dots on the radiographic image and small pits on the plate surface | Pressure on the plate when the patient bites strongly | |
| Crescent-shaped bending | A crescent-shaped radiopacity on the image and a crescent-shaped bending at the corresponding area of the plate | Tension on the sheath and plate when patients bite the bite block improperly |
Figure 2.
(a, b) A mandibular right posterior periapical radiograph and the plate used for image acquisition of radiograph: the straight arrows are showing cracking, dashed arrows are showing scratches and dotted arrows are showing peeling of the plate border. In addition, adhesive contamination and associated image artefact is seen on the bottom right of the image and plate. (c) Biting-related multiple radiopaque dots on the maxillary occlusal radiograph. In (d), the arrow is showing the crescent-shaped bending on the left bitewing radiograph.
Table 3.
Dirt on the plate related photostimulable phosphor plate-induced artefacts and errors
| Error/artefact name | Definition | Reason | Prevention |
|---|---|---|---|
| Dust particles on the plate | Radiopaque dots anywhere on the image | Dust particles on the plate surface, which stay fixed during the scanning procedure | Careful manipulation by the operator and regular cleaning of the plates with appropriate materials |
| Glove powder contamination | Granular radiopaque clusters on the image | Accumulation of glove powder on the plate surface with the contribution of sweat and body oil | |
| Fingerprint | A radiopaque fingerprint appearance on the radiographic image | Body oil and dirt on the fingers of the operator | |
| Adhesive contamination | An irregular radiopaque area that is generally near the short edges of the plate | Adhesive contamination from the adhesive band of the sheath while sleeving the plate and dust accumulation over this adhesive area |
Figure 3.
(a) Dust particle-related multiple radiopaque dots on the maxillary right posterior periapical radiograph; (b) glove powder-related radiopaque clusters on the maxillary right posterior periapical radiograph; (c) a circled area of the maxillary anterior periapical radiograph indicating a radiopaque fingerprint appearance; (d, e) a maxillary anterior periapical radiograph and the plate used for image acquisition of radiograph. The accumulation of radiopaque dots superimposed over the left lateral incisor and dirt on the plate, which is related to adhesive contamination and dust accumulation, can be noticed.
Scanner-induced artefacts and errors
Definitions, reasons and prevention of the scanner-induced artefacts and errors are shown in Table 4. The images of mentioned artefacts and errors are shown in Figure 4.
Table 4.
Definitions, reasons and prevention of the scanner-induced artefacts and errors
| Error/artefact name | Definition | Reason | Prevention | |
|---|---|---|---|---|
| Lines parallel to the slow scan direction | Straight line | A radiopaque straight line on the radiographic image, which is parallel to the slow scan direction | Dust particles and dirt on the narrow scanning window of the scanner which stay fixed during scanning | Periodic control, cleaning and calibration of the scanning device, using appropriate foil cassette for each plate size, careful and gentle manipulation during scanning procedure |
| Zigzagged line | A radiopaque zigzagged line on the radiographic image, which is parallel to the slow scan direction | Dust particles and dirt on the narrow scanning window of the scanner which move slightly during scanning | ||
| Ridging | Multiple radiolucent lines with an increasing distance, which are seen parallel to the fast scan direction | Momentary changes of the stimulating laser light intensity, the loss of synchronization between fast scan cycles and image plate transition, which causes more or less stimulating laser light exposure | ||
| Skipped image part | A skipped image part, which is parallel to the fast scan direction | Synchronization failure between the stimulation of the laser beam on the fast scan direction and progression of the plate on the slow scan direction via rollers and a conveyor belt | ||
| Peeling of the conveyor belt | An irregular but well-defined mixed appearance usually seen at one corner of the image with different shapes | Peeling of the conveyor belt surface and positioning the peeled part between the plate and narrow scanning window | ||
| Erasure artefact | A double image, which has the same characteristics as an image acquired as a result of a double exposure | Improper erasure and reuse of the plate for another radiograph | ||
| Plate size determination errors | Combining | A large image that occurs with collection of the images from the separate plates of same scanning procedure the area between the plates is seen as white | Panoramic- or cephalometric-sized plate scanning determination of the scanner by mistake when multiple intraoral-sized plates are scanned | |
| Bisection | Two separate images from one plate scanning, which is the continuation of each other | Smaller plate size determination, faulty power supply or other malfunctions with the software | ||
| Incomplete scanning | Smaller radiographic image dimension when corresponding to its plate | Stopping the scanning procedure when the scanner reaches the excessive cone-cutting area | ||
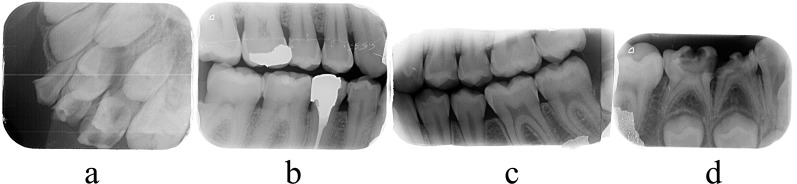
Figure 4.
(a) Horizontal radiopaque straight lines and vertical ridging pattern on the maxillary left posterior periapical radiograph; (b) a zigzagged radiopaque line on the right bitewing radiograph related to minimal movement of the blocking agent; (c) vertical skipped image part at the level of the third molars on the left bitewing radiograph; (d) well-defined mixed radiopacity at the bottom left corner of the right mandibular posterior periapical radiograph related to peeling of the conveyor belt.
Statistical analysis
Kappa values were found to be between 0.79 and 1 for various image artefacts. According to these values, a good/very good agreement was found for the intraobserver reliability.
Table 5 shows the frequency and percentage of the PSP-specific image artefacts. The most common image artefacts were found in fading with a ratio of 44.1% for the ambient light-induced group, peeling of the plate borders with a ratio of 53.4% for the PSP plate-induced group and straight line with a ratio of 42.2% for the scanner-induced group.
Table 5.
The classification, frequency and percentage of the photostimulable phosphor (PSP)-specific image artefacts
| Artefact group | Artefact type | Frequency |
||
|---|---|---|---|---|
| Absolute (n) | Relative (n) | |||
| Ambient light-induced artefacts and errors | Fading | 926 | 44.1 | |
| Non-uniform image density | 382 | 18.2 | ||
| Text pattern | 17 | 0.8 | ||
| Noisy image | 160 | 7.6 | ||
| Shining | 32 | 1.5 | ||
| PSP plate-induced artefacts and errors | Photostimulating luminescence layer damage | Cracking | 339 | 16.1 |
| Scratch | 871 | 41.5 | ||
| Bite marks | 22 | 1 | ||
| Peeling of the plate borders | 1121 | 53.4 | ||
| Crescent-shaped bending | 143 | 6.8 | ||
| Dirt on the plate | Dust particles on the plate | 737 | 35.1 | |
| Glove powder contamination | 195 | 9.3 | ||
| Fingerprint | 1 | 0.04 | ||
| Adhesive contamination | 164 | 7.8 | ||
| Scanner-induced artefacts and errors | Lines parallel to the slow scan direction | Straight line | 887 | 42.2 |
| Zigzagged line | 184 | 8.8 | ||
| Ridging | 4 | 0.2 | ||
| Skipped image part | 0 | 0 | ||
| Peeling of the conveyor belt | 31 | 1.5 | ||
| Erasure artefact | 0 | 0 | ||
| Plate size determination errors | Combining | 3 | 0.1 | |
| Bisection | 3 | 0.1 | ||
| Incomplete scanning | 11 | 0.5 | ||
Discussion
The intraoral radiographic errors and artefacts that form with film-based radiology are very well known. However, according to our knowledge, there are few studies that have determined and classified the image errors and artefacts specific to PSP technology,6–12 and only two of these are associated with dental practices.11,12 Therefore, we aimed to comprehensively determine and classify intraoral radiographic image errors and artefacts of PSP plates, which is a relatively new and popular imaging system.
The electrons that are captured via the F centres after exposure are metastable.1,13 This means that these captured electrons may spontaneously release from the F centres over time. High temperature and increased ambient light intensity and duration accelerate the release and have harmful effects on the latent image, especially on the underexposed PSP plates. Clinically, the most important reason of release is delayed scanning and ambient light exposure of the unsheathed plate. This behaviour of the PSP plates may cause a significant signal loss, which results in a decrease in the signal-to-noise ratio and an increase in the mean grey value.14,15 Image deterioration starts with fading or its partial forms like non-uniform image density or text pattern associated with the ambient conditions. Fluctuated signal loss creates a noisy image. However, darker image areas are affected more by the ambient light.15 Weak signals, which are generated by low-energy photons, are lost first as a result of excessive delayed scanning and ambient light exposure. These usually correspond with the radiopaque parts and periphery of the image. The shining artefact occurs on these specific areas together with a significantly noisy image. Shetty et al6 suggested that the intensity of the photons is decreased with the distance from the central beam. Therefore, recognizing the image loss first on the peripheral image is probably related to the lower intensity of the photons that exposes the periphery of the plate compared with the centre of the plate.
Although the manufacturer recommends an ambient light intensity of up to 1000 lux,16 a semi-dark room is recommended for scanning,1,2,14 and plate scanning delays should not be more than 10 min.15 The present study revealed a result of 44.1% for fading artefacts. However, these images are generally retrievable with the adjustment tools provided with the imaging software. The reason for this greater result is the removal of the plate from its sheath after the exposure to prevent contamination. In our department, a black cardboard that covers the imaging plate is routinely placed into all of the sheaths as an extra precaution to protect the PSP plate from both ambient light and mechanical stress.
Mechanical stress of the plate is a basic factor for photostimulating luminescence layer damage. Excessive bending, pressure, friction, biting, ageing and effects of the rollers have been reported as possible reasons for this damage.1,6 Handling of the plate during any image acquisition steps, especially during the scanning step, and wiping the plate have been considered as main causative factors for scratches.17,18 Kalathingal et al18 suggested handling of the plates with gloves in all steps and cleaning them with soft cloth instead of gauze only if a visible dirt is seen on the plate surface for the prevention of scratches. Chiu et al11 suggested that saliva contamination related to an inadequate sheath may have a peeling effect on the plate borders. The friction between the plate and foil cassette might be the main cause of this plate damage. The disinfectant solutions and skin oil combined with contaminants have been reported as possible permanent damage agents.1 However, in the present study, no permanent damage was observed on any plate associated with these agents.
Dirt on the plate blocks the stimulating laser light, which is necessary for phosphorescence and signal acquisition. The image from this area is seen as radiopaque because of no signal acquisition and takes the form of a blocking agent. Dirt on the black side does not produce an artefact; only the dirt on the active side of the plate creates the image artefact. Dust particles, glove powder contamination and body oil are the reported agents for dirt on the plate.1 The manufacturer recommends the use of image plate-cleaning wipes for cleaning and disinfection.19 These disposable wipes contain 4 g of isopropyl alcohol and the manufacturer recommends 15–30 s of application time for adequate effectiveness. Image plates must also be dried after cleaning.
Dust particles and dirt on the narrow scanning window of the scanner may block the stimulating laser light at the same place on every fast scan cycle. Also, acquired visible light from the constant part of every fast scan cycle, resulting from phosphorescence, may not reach the photomultiplier tube because of dust and dirt on the parabolic mirrors or light collector. These blockages cause a focal no-signal area and a loss of image acquisition. These always happen at the same focal area on the fast scan direction if the blocking agent is fixed. A repeat of this blockage during whole scanning procedures of the plate generates a radiopaque straight line on the radiographic image, which is parallel to the slow scan direction. The zigzagged line is probably related to minimal movement of the blocking agent because of scanner vibration during the process or the effect of plate movement elements. All of the images processed on the same scanning socket of the scanner show the same image artefact exactly at the same place, unless the blocking dust particles and dirt are cleaned or spontaneously moved. In addition, an air spray of the dental units may be used for removing dust particles and dirt on the narrow scanning window without removing the parts of the scanner.
The intensity and duration of the stimulating laser light determine the amount of phosphorescence and hence the amount of signal acquisition.13 If the stimulating laser light is applied to the image receptor erratically, a brighter radiographic image is seen on the longer exposed part of the plate.6 This is a possible reason for the ridging artefact. This artefact is not seen on subsequent scanning procedures.
Mismatch between foil cassette and plate size may be effective in occurring skipped image part. Using smaller sized foil cassettes and forcing the sliding button during the scanning procedure may have a pushing effect on the plate being scanned. In addition, software, conveyor belt or roller malfunctions during plate scanning may cause this artefact.
Plate size determination errors are rare artefacts. Combining error is almost always seen with multiple plate scanning including an occlusal-sized plate and may be related to sliding the occlusal plate with hand from the extra socket area instead of using the Size 4 foil cassette. The rarity and lack of repetition of certain errors and artefacts also bring about difficulty in explaining these mechanisms. Possible unforeseen software-associated malfunctions might be the main causative factors for these image errors and artefacts.
Conclusions
The wide usage of this imaging modality necessitates that the features of the PSP technology have to be understood well for successful radiographic imaging and eliminating image errors and artefacts.
The most common image errors and artefacts were peeling of the plate borders, fading, straight lines, scratches and dust particles on the plate. The determination and definition of the image errors and artefacts with the clarification of their causes and solutions are important for the improvement of radiographic quality and the reduction of the retake ratio.
Contributor Information
Armağan Çalışkan, Email: armagancaliskan@hotmail.com.
A Pinar Sumer, Email: psumer1970@yahoo.com.
References
- 1.Ludlow JB, Mol A. Digital imaging. In: White SC, Pharoah MJ, eds. Oral radiology: principles and interpretation. 7th edn. St Louis, MO: Mosby; 2014. pp. 41–62. [Google Scholar]
- 2.Wenzel A, Møystad A. Work flow with digital intraoral radiography: a systematic review. Acta Odontol Scand 2010; 68: 106–14. doi: https://doi.org/10.3109/00016350903514426 [DOI] [PubMed] [Google Scholar]
- 3.Berkhout E, Sanderink G, van der Stelt P. Digital intra-oral radiography in dentistry. Diagnostic efficacy and dose considerations. Oral Radiol 2003; 19: 1–13. doi: https://doi.org/10.1007/bf02493286 [Google Scholar]
- 4.Parks ET, Williamson GF. Digital radiography: an overview. J Contemp Dent Pract 2002; 3: 23–39. [PubMed] [Google Scholar]
- 5.Petrikowski CG. Introducing digital radiography in the dental office: an overview. J Can Dent Assoc 2005; 71: 651. [PubMed] [Google Scholar]
- 6.Shetty CM, Barthur A, Kambadakone A, Narayanan N, Kv R. Computed radiography image artifacts revisited. AJR Am J Roentgenol 2011; 196: W37–47. doi: https://doi.org/10.2214/AJR.10.5563 [DOI] [PubMed] [Google Scholar]
- 7.Solomon SL, Jost RG, Glazer HS, Sagel SS, Anderson DJ, Molina PL. Artifacts in computed radiography. AJR Am J Roentgenol 1991; 157: 181–5. doi: https://doi.org/10.2214/ajr.157.1.2048517 [DOI] [PubMed] [Google Scholar]
- 8.Cesar LJ, Schueler BA, Zink FE, Daly TR, Taubel JP, Jorgenson LL. Artefacts found in computed radiography. Br J Radiol 2001; 74: 195–202. doi: https://doi.org/10.1259/bjr.74.878.740195 [DOI] [PubMed] [Google Scholar]
- 9.Oestmann JW, Prokop M, Schaefer CM, Galanski M. Hardware and software artifacts in storage phosphor radiography. Radiographics 1991; 11: 795–805. doi: https://doi.org/10.1148/radiographics.11.5.1947316 [DOI] [PubMed] [Google Scholar]
- 10.Willis CE, Thompson SK, Shepard SJ. Artifacts and misadventures in digital radiography. Appl Radiol 2004; 33: 11–21. [Google Scholar]
- 11.Chiu HL, Lin SH, Chen CH, Wang WC, Chen JY, Chen YK, et al. Analysis of photostimulable phosphor plate image artifacts in an oral and maxillofacial radiology department. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106: 749–56. doi: https://doi.org/10.1016/j.tripleo.2008.01.003 [DOI] [PubMed] [Google Scholar]
- 12.Gulsahi A, Secgin CK. Assessment of intraoral image artifacts related to photostimulable phosphor plates in a dentomaxillofacial radiology department. Niger J Clin Pract 2016; 19: 248–53. doi: https://doi.org/10.4103/1119-3077.164338 [DOI] [PubMed] [Google Scholar]
- 13.Seibert JA, Bogucki TM, Ciona T, Huda W, Karellas A, Mercier JR, et al. Acceptance testing and quality control of photostimulable storage phosphor imaging systems. Report of AAPM task group 10. College Park, MD: American Association of Physicists in Medicine; 2006. [Google Scholar]
- 14.Ramamurthy R, Canning CF, Scheetz JP, Farman AG. Impact of ambient lighting intensity and duration on the signal-to-noise ratio of images from photostimulable phosphor plates processed using DenOptix and ScanX systems. Dentomaxillofac Radiol 2004; 33: 307–11. doi: https://doi.org/10.1259/dmfr/91373164 [DOI] [PubMed] [Google Scholar]
- 15.Akdeniz BG, Gröndahl HG, Kose T. Effect of delayed scanning of storage phosphor plates. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 99: 603–7. doi: https://doi.org/10.1016/j.tripleo.2004.10.021 [DOI] [PubMed] [Google Scholar]
- 16. Dürr digital diagnostic radiography. The time is right for a change in diagnostic radiography [Product brochure on the internet]. Bietigheim-Bissingen: Dürr Dental GmbH & Co. KG [updated 16 Jan 2012; cited 6 Aug 2014]. Available from: http://www.henryschein.nl/nl-nl/images/dentaal/vistascan_plus.pdf.
- 17.Bedard A, Davis TD, Angelopoulos C. Storage phosphor plates: how durable are they as a digital dental radiographic system? J Contemp Dent Pract 2004; 5: 57–69. [PubMed] [Google Scholar]
- 18.Kalathingal SM, Shrout MK, Comer C, Brady C. Rating the extent of surface scratches on photostimulable storage phosphor plates in a dental school environment. Dentomaxillofac Radiol 2010; 39: 179–83. doi: https://doi.org/10.1259/dmfr/28972644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Product information VistaScan image plate cleaning wipe [Product brochure on the internet]. Bietigheim-Bissingen: Dürr Dental AG; [updated 28 Feb 2014; cited 22 Feb 2015].