Abstract
Objectives:
To evaluate the effect of orthodontic stainless steel brackets and two different types of archwires on the diagnostic quality of 3-T MR images.
Methods:
This prospective, case-control study was conducted following Strengthening the Reporting of Observational Studies in Epidemiology guidelines. The recruitment was conducted among orthodontic patients. 80 subjects, requiring MRI for the presence of temporomandibular disorders, were enrolled and divided into four groups: 20 patients using aligners (control group); 20 patients with stainless steel brackets without archwires; 20 patients with stainless steel brackets and nickel–titanium archwires; and 20 patients with stainless steel brackets and stainless steel archwires. Two experts in neuroradiology evaluated the images to determine the amount of distortion in 6 regions and 48 districts. A score was subjectively assigned according to a modified receiver operating characteristic method of distortion classification. Any disagreement was resolved through consensus seeking; when this was not possible, a third neuroradiologist was consulted. The following statistical methods were used: descriptive statistics, Cohen's kappa coefficient (k), Kruskal–Wallis test, pairwise comparisons using the Dunn–Bonferroni approach. The significance was set at p ≤ 0.05.
Results:
The presence of stainless steel brackets with or without archwires negatively influenced MRI of the cervical region, paranasal sinuses, head and neck region, and cervical vertebrae but did not influence MRI of brain and temporomandibular joint regions.
Conclusions:
Patients with a stainless steel multibracket orthodontic appliance should remove it before cervical vertebrae, cervical region, paranasal sinuses, and head and neck MRI scans. The brain and temporomandibular joint region MRI should not require the removal of such appliances.
Keywords: MRI, orthodontics, artefacts, orthodontic brackets, orthodontic wires
Introduction
MRI is an essential diagnostic tool in both medicine and dentistry and, given its distinct advantages over conventional techniques, high-field MRI at 3 T or even higher is becoming increasingly common in daily practice.1–3
However, despite these advantages, MRI is only useful as a tool if the images that it produces are easy to interpret. Distortion in MRI signal intensity with no identifiable anatomical source can produce what is termed an “artefact” in the resultant image.4 These artefacts may be due to patient movement, to changes in the chemical bonding of molecules under a strong magnetic field (chemical artefacts), or they may result from blood flow (saturation artefacts).4 The presence of metals such as palladium–cobalt–nickel (Ni) and tin–cobalt alloys, so common in dentistry, also cause image distortion due to the susceptibility of these metals to become magnetized.4,5 When a material is placed in an external magnetic field, it may affect inhomogeneity in the magnetic field with subsequent changes in the magnetic field gradient.6 The capacity of an object to induce such changes is referred to as magnetic susceptibility which could be classified as diamagnetic, paramagnetic, superparamagnetic and ferromagnetic, according to the magnitude.6 However, metallic property should not be misunderstood as ferromagnetic property, indeed not all metals cause signal loss and image distortion. Usually, precious metals (gold, platinum, silver, iridium and palladium) which are more conductive cause less heterogeneity of radiofrequency (RF) field and signal loss, and encoding distortion happen locally at the distance very close to them.7 Otherwise, chromium (Cr)–cobalt and Ni-Cr alloys are less conductive, but render the undiagnostic image and significant heterogeneity in the magnetic field.8 Given the prevalence of ferromagnetic materials in dentistry, metal artefacts are one of the most important features of MRI.9–11 Although titanium (Ti) produces fewer artefacts than ferromagnetic alloys, it is nevertheless impossible to obtain precise anatomical information in the immediate area of Ti.12 Orthodontic appliances are employed in large regions in the upper and lower jaws and comprise stainless steel composed of Ni (8–12%), Cr (17–22%) and variable amounts of others metals.13 Ni and Cr are ferromagnetic metals; consequently, they determine a distortion on the local magnetic field, causing large artefacts which can make image interpretation impossible.14
The purpose of the present study is to subjectively evaluate the effect of orthodontic metallic braces and archwires on the diagnostic quality of 3-T MR images of six craniofacial and cervical regions.
The differences in the diagnostic quality of images between patients with no stainless steel brackets and those with stainless steel brackets without archwires are the primary outcome, and as a secondary outcome, patients with stainless steel brackets but with two different types of archwires (stainless steel and Ni-Ti) are also evaluated. The working hypothesis is that artefacts created by fixed orthodontic appliances were negligible; therefore, removal of this orthodontic product before the MRI scans of the head and neck area would not be recommended.
Methods and materials
Study design and sample
This prospective, case-control study was conducted at the Department of Radiology, “Sapienza”, University of Rome, Rome, Italy. The Strengthening the Reporting of Observational Studies in Epidemiology guidelines for prospective case-control studies were followed. This clinical investigation was conducted in accordance with the ethical principles of the World Medical Association Declaration of Helsinki and was undertaken after informing the patient of the content, risks and benefits of the study. Written consent was obtained from each participant. The investigation was reviewed and approved by the local ethics committee. The recruitment was conducted at the Department of Oral and Maxillo-Facial Sciences of the “Sapienza”, University of Rome, between November 2013 and July 2016, among patients in fixed orthodontic treatment using stainless steel brackets (in the upper and lower jaws, from the first molar to the first molar) (Victory Series™ Metal Brackets 0.022; 3M Unitek Orthodontic Products, Monrovia, CA) and Ni-Ti archwires (NiTi wires) (0.017 × 0.025-inches, 3M Unitek Orthodontic Products) or stainless steel archwires (SS wires, 0.017 × 0.025-inches; 3M Unitek Orthodontic Products) and among patients in removable orthodontic treatment using clear aligners (control group).
In total, 80 patients were included in the study, 59 females and 21 males with ages ranging from 20 to 29 years (22.65 ± 2.74 years), providing 80 MRI images.
The subjects were enrolled using the following criteria: Caucasian subjects, over 18 years of age, requiring MRI for the presence of the temporomandibular disorders of either gender but excluding pregnant females; the absence of MRI contraindications (e.g. medical devices such as aneursymal clips, pacemakers etc); no metal dental fillings, metal-containing crowns or dental implants.
The 80 selected patients were divided into four groups:1 20 patients using aligners (control group);2 20 patients with stainless steel brackets without archwires;3 20 patients with stainless steel brackets and Ni-Ti archwires;4 and 20 patients with stainless steel brackets and stainless steel archwires. The control subjects were paired in age and sex with the studied groups.
Blinding
Information about the type of orthodontic appliance of each study subject was blinded to the radiologists (responsible for MRI evaluation) and statistician. Only an external study collaborator, whose duty was to record the code indicating to which group each patient had been assigned until the conclusion of the study, was aware of the relative assignations.
MRI acquisition protocol
The scout view was initially obtained following which the imaging protocol for the brain evaluation consisted of axial fluid attenuated inversion recovery sequences with the following parameters: repetition time (TR) 9010 ms, echo time (TE) 114 ms, field of view (FOV) 240 × 240 mm, with sections of 5 mm thickness, intergap 0.5 mm, matrix 320 × 320; then the axial oblique double echo proton density and weighted/turbo spin echo (TSE) T2 weighted (T2w) sequences were acquired (TR 5600 ms, TE 114/7 ms, FOV 240 × 240 mm, with sections of 5 mm thickness, intergap 0.5 mm, matrix 320 × 320). For the cervical spine evaluation, sagittal TSE T2w with the following parameters: TR 6700 ms, TE 83 ms, FOV 240 × 240 mm, with sections of 4 mm thickness, intergap 0.5 mm, matrix 320 × 320; sagittal TSE T1 with the parameters: TR 400 ms, TE 20 ms, FOV 240 × 240 mm, with sections of 4 mm thickness, intergap 0.5 mm, matrix 320 × 320 and, finally, axial T2* gradient echo sequences were employed: TR 816 ms, TE 11 ms, FOV 240 × 240 mm, with sections of 3 mm thickness, intergap 0.5 mm, matrix 320 × 320. Axial and coronal TSE T2w images for the head and neck structures were also acquired (TR 5600 ms, TE 114/7 ms, FOV 240 × 240 mm, with sections of 5 mm, thickness, intergap 0.5 mm, matrix 320 × 320). For the temporomandibular joint sagittal, axial and coronal proton density and TSE T2 weighted sequences were employed (TR 5653 ms, TE 13 and 102 ms, FOV 160 × 160 mm, with sections of 2 mm thickness, intergap 0.2 mm, matrix 256 × 256).
MRI evaluation
Two radiologists, experts in neuroradiology, evaluated the images to determine the amount of distortion in 6 regions and 48 districts. In terms of the quality of images, a score was assigned for each region according to a modified receiver operating characteristic method of distortion classification: (1) no distortion/artefact; (2) minimal distortion/artefact; (3) moderate distortion/artefact; (4) severe distortion; (5) complete obliteration.15 The images with Scores 1 and 2 were considered diagnostic; the images with Score 3 were considered moderately diagnostic; and the images with Scores 4 and 5 were considered non-diagnostic. Any disagreement was resolved through consensus seeking; when this was not possible, a third neuroradiologist was consulted. The following were the anatomical regions and districts evaluated: brain (frontal lobe, occipital lobe, temporal lobe, parietal lobe, basal ganglia, substantia nigra, cerebellum, cerebellar vermis, brain hemispheres, meninges, mastoid cells and pituitary gland), paranasal sinuses (infratemporal fossa, frontal sinus, maxillary sinuses, sphenoidal sinus, nasal turbinates, nasal septum and orbits), head and neck (major salivary glands, rhinopharynx lymphatic tissue, body of the tongue, palatine tonsil, body of the mandible, and condyle of the mandible), cervical region (trachea, root of the tongue, pre-epiglottic fat tissue, epiglottic vallecola, pyriform sinuses, corde vocali false, glossoepiglottic folds, vocal folds, thyroid cartilage, cricoid cartilage, arytenoid cartilage, middle pharyngeal constrictor muscle, inferior pharyngeal constrictor muscle), cervical vertebrae (vertebral body, vertebral arch, interapophyseal joints, intersomatic disk, paravertebral muscles and medulla) and temporomandibular joint (disc, condyle, articular tubercle and retrodiscal space).
A Barco diagnostic display (Barco, Kortrijk, Belgium) was used during image evaluation [resolution: 4 MP (2560 × 1600); pixel pitch: 0.256 mm; bit depth: 30 bit; maximum luminance (panel typical): 1050 cd m−2].
Statistical analysis
The required sample size was calculated using statistics software (GPower v. 3.1.9.2; Heinrich-Heine-Universität, Düsseldorf, Germany). A power analysis using the one-way, fixed-effects ANOVA model with an α-level of 0.05 showed that 20 subjects for each group would be adequate to obtain 95% power in detecting a statistical difference between groups in scores on the image quality. The power calculation was based on the quality of image scores in a previous pilot study involving five patients for each groups: 2.33 ± 0.93 [mean ± standard deviation (SD)] for the first group 3.29 ± 1.74; (mean ± SD) for the second group; 3.39 ± 1.63 (mean ± SD) for the third group; and 3.55 ± 1.42 (mean ± SD) for the fourth group. In the same pilot study, Cohen's kappa coefficient (k) was used to calculate the intraobserver reliability in the evaluation of MRI distortions. The determined intraobserver reliability was: k = 0.809 (p < 0.0001). The MRI distortion data were illustrated using mean and SD, and box plots. The Kruskal–Wallis test was used to evaluate the influence of different orthodontic appliances on MRI distortion. Pairwise comparisons, using the Dunn–Bonferroni approach, were used for post hoc testing. Data were evaluated using standard statistical analysis software (SPSS® v. 20.0; IBM Corp., New York, NY; formerly SPSS Inc., Chicago, IL). In each test, the cut-off for statistical significance was p ≤ 0.05.
Results
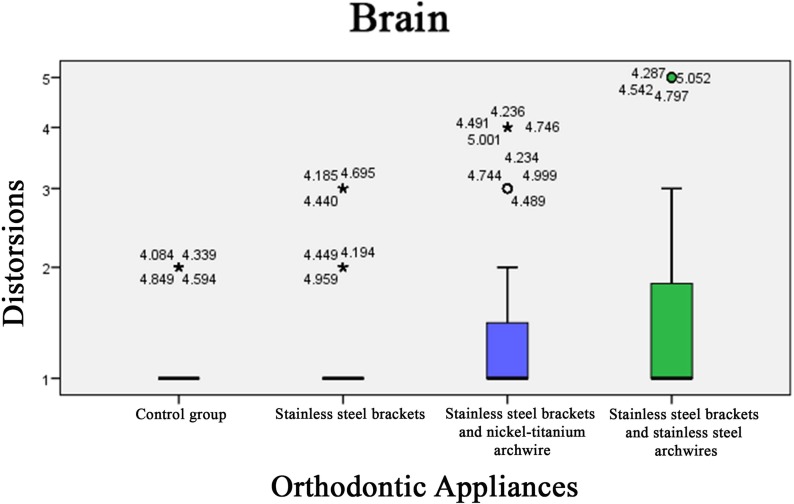
Brain region
In the control group (i.e. patients using aligners), MRI was diagnostic in each district. In patients with stainless steel brackets, without archwires, MRI was diagnostic in 91.6% of districts evaluated and moderate diagnostic in the remaining 8.4%. In patients with stainless steel brackets and Ni-Ti archwires, MRI was diagnostic in 83.3% of districts evaluated, moderate diagnostic in 10.2% and non-diagnostic in 6.5%. In patients with stainless steel brackets and stainless steel archwires, MRI was diagnostic in 75% of districts evaluated, moderate diagnostic in 16.7% and non-diagnostic in 8.3%. There were statistically significant differences between the mean distortion scores in the four groups (p < 0.0001).
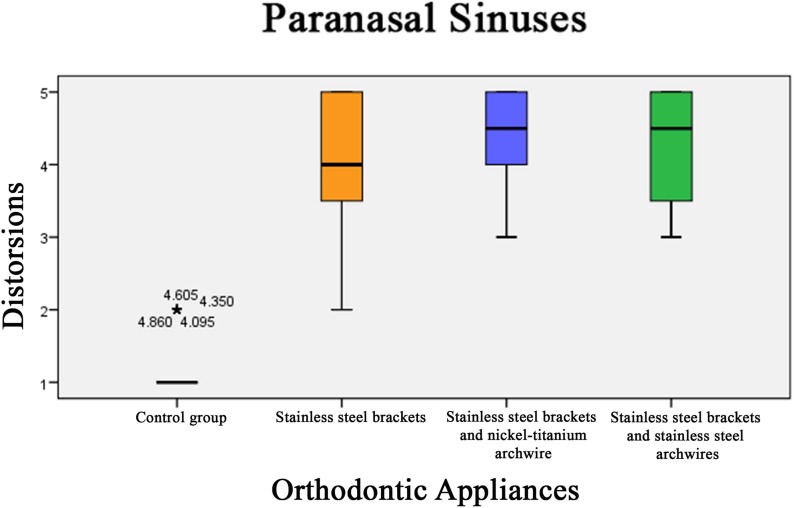
Paranasal sinuses region
In the control group, MRI was diagnostic in each district. In patients with stainless steel brackets, without archwires, the MRI was diagnostic in 12.3% of districts evaluated, moderate diagnostic in 12.7% and non-diagnostic in 75%. In patients with stainless steel brackets and Ni-Ti archwires, MRI was moderate diagnostic in 12.5% of districts evaluated and non-diagnostic in the remaining 87.5%. In patients with stainless steel brackets and stainless steel archwires, MRI was moderate diagnostic in 23.7% of districts evaluated and non-diagnostic in 76.3%. There were statistically significant differences between the mean distortion scores in the four groups (p < 0.0001).
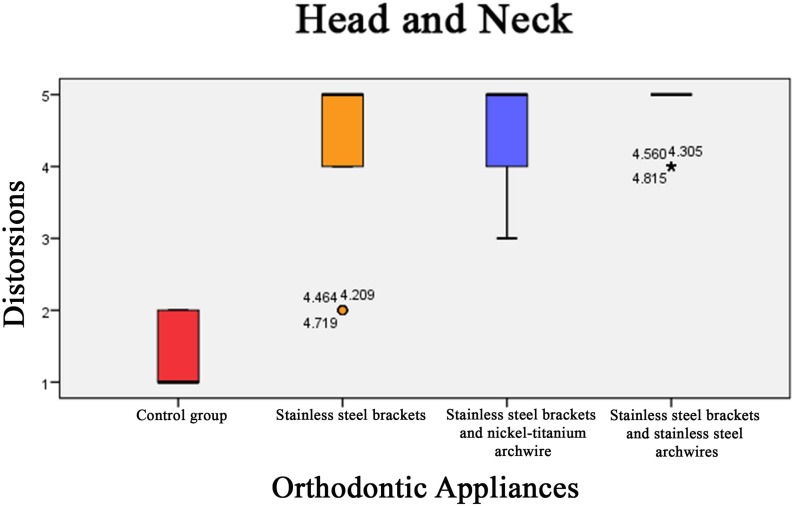
Head and neck
In the control group, MRI was diagnostic in each district. In patients with stainless steel brackets, without archwires, MRI was diagnostic in 7.1% of districts evaluated, moderate diagnostic in 8.2% and non-diagnostic in 84.7%. In patients with stainless steel brackets and Ni-Ti archwires, MRI was moderate diagnostic in 14.3% of districts evaluated and non-diagnostic in the remaining 85.7%. In patients with stainless steel brackets and stainless steel archwires, MRI was non-diagnostic in 100% of districts evaluated. There were statistically significant differences between the mean distortion scores in the four groups (p < 0.0001).
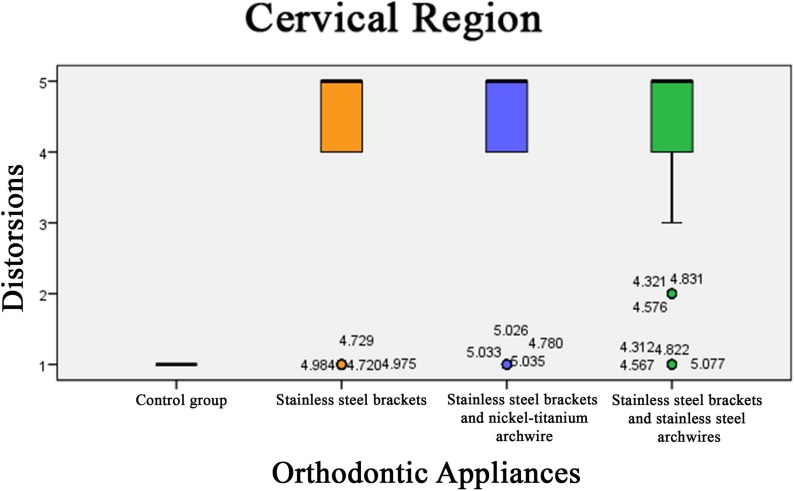
Cervical region
In the control group, MRI was diagnostic in each district. In patients with stainless steel brackets without archwires, MRI was diagnostic in 15.4% of districts evaluated and non-diagnostic in 84.6%. In patients with stainless steel brackets and Ni-Ti archwires, MRI was diagnostic in 11.3% of districts evaluated, moderate diagnostic in 11.8% and non-diagnostic in 76.9%. In patients with stainless steel brackets and stainless steel archwires, MRI was diagnostic in 7.7% of districts evaluated, moderate diagnostic in 9.8% and non-diagnostic in 82.5%. There were statistically significant differences between the mean distortion scores in the four groups (p < 0.0001).
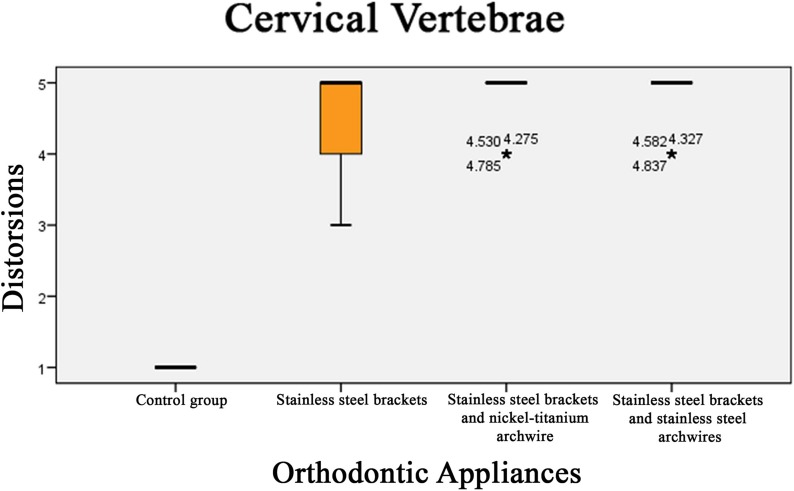
Cervical vertebrae region
In the control group, MRI was diagnostic in each district. In patients with stainless steel brackets, without archwires, MRI was moderate diagnostic in 13.7% of districts evaluated and non-diagnostic in 86.3%. In patients with stainless steel brackets and Ni-Ti archwires and with stainless steel brackets and stainless steel archwires, MRI was non-diagnostic in 100% of districts evaluated. There was a statistically significant difference between the mean distortion scores in the four groups (p < 0.0001).
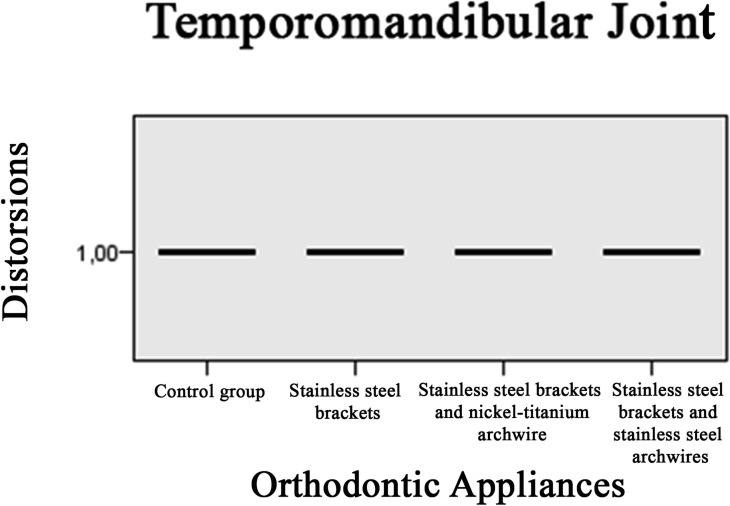
Temporomandibular joint
In the temporomandibular joint region, MRI was diagnostic in each district of the four groups. Indeed, no difference was found between the mean distortion scores in the four groups (p = 1.000).
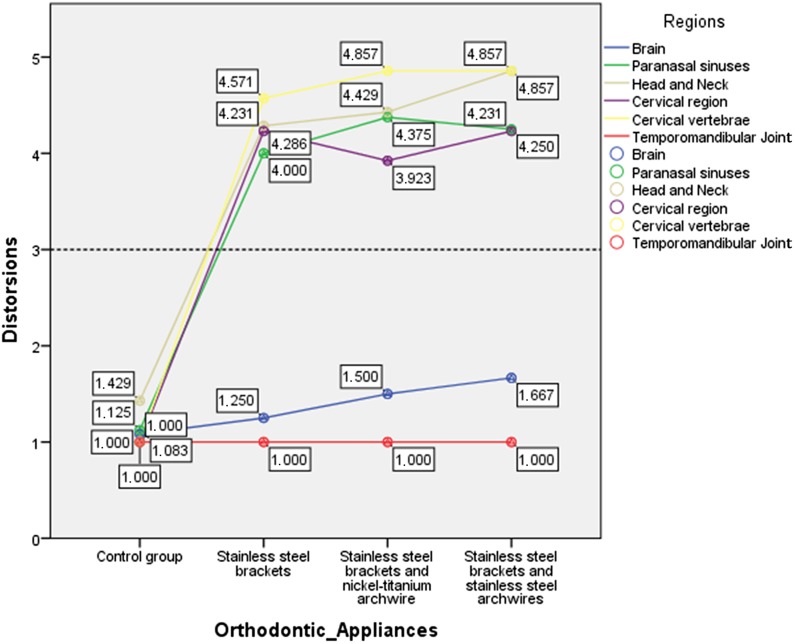
The results of MRI evaluation according to orthodontics appliance are summarized in Figures 1–7 and in Table 1; post hoc analysis results are shown in Table 2.
Figure 1.
Mean distortion scores of MRI according to orthodontic appliance. The linear graph showed a mean score > of 3 (nondiagnostic line) in each group with different orthodontic appliances. Only two regions (brain and temporomandibular joint) were considered always diagnostic.
Figure 7.
Box-and-whisker plots related to the distortion scores in the four groups according to orthodontics appliance in the temporomandibular joint region.
Table 1.
Number and percentages of images with artefacts by type of orthodontic appliances and anatomical area
| craniofacial and cervical regions | Group 1 | Group 2 | Group 3 | Group 4 | Total |
|---|---|---|---|---|---|
| Brain | |||||
| No distortion (%) | 220 (28.2) | 200 (25.6) | 180 (23.1) | 180 (23.1) | 780 (100) |
| Minimal distortion (%) | 20 (33.3) | 20 (33.3) | 20 (33.3) | 0 | 60 (100) |
| Moderate distortion (%) | 0 | 20 (25) | 20 (25) | 40 (50) | 80 (100) |
| Severe distortion (%) | 0 | 0 | 20 (100) | 0 | 20 (100) |
| Complete obliteration | 0 | 0 | 0 | 20 (100) | 20 (100) |
| Paranasal sinuses | |||||
| No distortion (%) | 140 (100) | 0 | 0 | 0 | 140 (100) |
| Minimal distortion (%) | 20 (50) | 20 (50) | 0 | 0 | 40 (100) |
| Moderate Distortion (%) | 0 | 20 (25) | 20 (25) | 40 (50) | 80 (100) |
| Severe distortion (%) | 0 | 60 (37.5) | 60 (37.5) | 40 (25) | 160 (100) |
| Complete obliteration | 0 | 60 (27.3) | 80 (36.4) | 80 (36.4) | 220 (100) |
| Head and neck | |||||
| No distortion (%) | 80 (100) | 0 | 0 | 0 | 80 (100) |
| Minimal distortion (%) | 60 (75) | 20 (25) | 0 | 0 | 80 (100) |
| Moderate distortion (%) | 0 | 0 | 20 (100) | 0 | 20 (100) |
| Severe distortion (%) | 0 | 40 (40) | 40 (40) | 20 (20) | 100 (100) |
| Complete obliteration | 0 | 80 (28.6) | 80 (28.6) | 120 (42.9) | 280 (100) |
| Cervical region | |||||
| No distortion (%) | 260 (68.4) | 40 (10.5) | 60 (15.8) | 20 (5.3) | 380 (100) |
| Minimal distortion (%) | 0 | 0 | 0 | 20 (100) | 20 (100) |
| Moderate distortion (%) | 0 | 0 | 0 | 20 (100) | 20 (100) |
| Severe distortion (%) | 0 | 40 (40) | 40 (40 ) | 20 (20) | 100 (100) |
| Complete obliteration | 0 | 180 (34.6) | 160 (30.8) | 180 (34.6) | 520 (100) |
| Cervical vertebrae | |||||
| No distortion (%) | 140 (100) | 0 | 0 | 0 | 140 (100) |
| Minimal distortion (%) | 0 | 0 | 0 | 0 | 0 |
| Moderate distortion (%) | 0 | 20 (100) | 0 | 0 | 20 (100) |
| Severe distortion (%) | 0 | 20 (33.3) | 20 (33.3) | 20 (33.3) | 60 (100) |
| Complete obliteration | 0 | 100 (29.4) | 120 (35.3) | 120 (35.5) | 340 (100) |
| Temporomandibular joint | |||||
| No distortion (%) | 80 (25) | 80 (25) | 80 (25) | 80 (25) | 320 (100) |
| Minimal distortion (%) | 0 | 0 | 0 | 0 | 0 |
| Moderate distortion (%) | 0 | 0 | 0 | 0 | 0 |
| Severe distortion (%) | 0 | 0 | 0 | 0 | 0 |
| Complete obliteration | 0 | 0 | 0 | 0 | 0 |
Table 2.
Pairs comparison using the Dunn–Bonferroni approach was used for post hoc testing, to evaluate the statistical differences of distortion in MRI evaluation between the four groups
| craniofacial and cervical regions | Test statistic | Std. error | Std. test statistic | Sig. | Adj. sig. |
|---|---|---|---|---|---|
| Brain | |||||
| Group 1 vs Group 2 | −40.833 | 17.219 | −2371 | 0.018 | 0.106 |
| Group 1 vs Group 3 | −86.833 | 17.219 | −4985 | 0.000 | 0.000a |
| Group 1 vs Group 4 | −93.333 | 17.219 | −5420 | 0.000 | 0.000a |
| Group 2 vs Group 3 | −45.000 | 17.219 | −2613 | 0.009 | 0.054 |
| Group 2 vs Group 4 | −52.500 | 17.219 | −3049 | 0.002 | 0.014a |
| Group 3 vs Group 4 | −7500 | 17.219 | −0.436 | 0.663 | 1000 |
| Paranasal sinuses | |||||
| Group 1 vs Group 2 | −292.500 | 19.947 | −14.664 | 0.000 | 0.000a |
| Group 1 vs Group 3 | −323.750 | 19.947 | −16.230 | 0.000 | 0.000a |
| Group 1 vs Group 4 | −338.750 | 19.947 | −16.982 | 0.000 | 0.000a |
| Group 2 vs Group 3 | −31.250 | 19.947 | −1567 | 0.117 | 0.703 |
| Group 2 vs Group 4 | −46.250 | 19.947 | −2319 | 0.020 | 0.122 |
| Group 3 vs Group 4 | 15.000 | 19.947 | 0.752 | 0.452 | 1000 |
| Head and neck | |||||
| Group 1 vs Group 2 | −248.571 | 17.970 | −13.833 | 0.000 | 0.000a |
| Group 1 vs Group 3 | −255.714 | 17.970 | −14.230 | 0.000 | 0.000a |
| Group 1 vs Group 4 | −318.571 | 17.970 | −17.728 | 0.000 | 0.000a |
| Group 2 vs Group 3 | −7143 | 17.970 | −0.397 | 0.691 | 1000 |
| Group 2 vs Group 4 | −70.000 | 17.970 | −3895 | 0.000 | 0.001a |
| Group 3 vs Group 4 | −62.867 | 17.970 | −3498 | 0.000 | 0.003a |
| Cervical region | |||||
| Group 1 vs Group 2 | −406.154 | 23.933 | −16.971 | 0.000 | 0.000a |
| Group 1 vs Group 3 | −451.538 | 23.933 | −18.867 | 0.000 | 0.000a |
| Group 1 vs Group 4 | −462.308 | 23.933 | −19.317 | 0.000 | 0.000a |
| Group 2 vs Group 3 | 45.385 | 23.933 | 1896 | 0.058 | 0.347 |
| Group 2 vs Group 4 | −56.154 | 23.933 | −2346 | 0.019 | 0.114 |
| Group 3 vs Group 4 | −10.769 | 23.933 | −0.450 | 0.653 | 1000 |
| Cervical vertebrae | |||||
| Group 1 vs Group 2 | −257.143 | 16.852 | −15.259 | 0.000 | 0.000a |
| Group 1 vs Group 3 | −291.429 | 16.852 | −17.294 | 0.000 | 0.000a |
| Group 1 vs Group 4 | −291.429 | 16.852 | −17.294 | 0.000 | 0.000a |
| Group 2 vs Group 3 | −34.286 | 16.852 | −2035 | 0.042 | 0.251 |
| Group 2 vs Group 4 | −34.286 | 16.852 | −2035 | 0.042 | 0.251 |
| Group 3 vs Group 4 | 0.000 | 16.852 | 0.000 | 1000 | 1000 |
adj., adjusted; Group 1, control group; Group 2, stainless steel brackets without archwires; Group 3, stainless steel brackets and nickel-titanium archwires; Group 4, stainless steel brackets and stainless steel archwires; sig., significance; std., standard.
Each row tests the null hypothesis that the two group distributions are the same.
Asymptotic significances (two-sided tests) are displayed.
The significance level is 0.05.
Figure 2.
Box-and-whisker plots related to the distortion scores in the four groups according to orthodontics appliance in the brain region. The dark line in the middle of the boxes is the median. The box represents the interquartile (IQ) range which contains the middle 50% of the records. The whiskers are lines that extend from the upper and lower edges of the box to the highest and lowest values which are no greater than 1.5 times the IQ range. The circles are outliers. These are defined as values that do not fall within the whiskers. The asterisks or stars are extreme outliers. These represent cases that have values more than three times the height of the boxes.
Figure 3.
Box-and-whisker plots related to the distortion scores in the four groups according to orthodontics appliance in the paranasal sinuses region.
Figure 4.
Box-and-whisker plots related to the distortion scores in the four groups according to orthodontics appliance in the head and neck region.
Figure 5.
Box-and-whisker plots related to the distortion scores in the four groups according to orthodontics appliance in the cervical region.
Figure 6.
Box-and-whisker plots related to the distortion scores in the four groups according to orthodontics appliance in the cervical vertebrae region.
Discussion
The present study evaluated the effects of common stainless steel orthodontic brackets and archwires (stainless steel and Ni-Ti), on the diagnostic quality of 3-T MRI of six craniofacial and cervical regions.
The following hypotheses of the study were partially confirmed:
– It is appropriate to remove stainless steel orthodontic brackets in patients who require MRI in the cervical region, paranasal sinuses, head and neck region and cervical vertebrae.
– The presence of stainless steel or Ni-Ti archwires negatively influences MRI of the cervical region, paranasal sinuses, head and neck region and cervical vertebrae to such an extent that it makes the images unusable for diagnostic purposes although it does not influence MRI of the brain and temporomandibular joint regions.
The effects of archwires also affected the clarity of image in the present study, therefore the recommendation is that they be removed before an MRI examination.
In terms of the study's limitations, the present study focused solely on bonded stainless steel orthodontic bracket appliances for which removal procedures are time-consuming, uncomfortable for the patient, costly and that which could potentially damage enamel. Plastic, ceramic and Ti brackets were not evaluated given that previous studies have shown the uncommon occurrence of artefacts.15 Considering the other limitations of the present study, the heating of the orthodontic metallic braces with different wires in a 3-T MRI environment was not evaluated. This issue was not evaluated based on the findings of a recent in vitro study reporting the absence of excessive heating (highest temperature change: <3.04 °C), of fixed metallic orthodontic appliances with different wires and ligaments in a 3-T MRI environment.16 The temperature changes of the specimens were considered to be within acceptable ranges.16 These results confirmed the findings of a previous in vitro study conducted to estimate the risk of injury from RF heating of metallic dental devices in use during 3.0-T MRI. In this study, when the fixed metallic orthodontic appliances were considered, the assessed RF heating was +2.61 °C.17
In terms of new knowledge originating from the present study, its in vivo design more closely resembles the clinical scenario in terms of materials used and anatomical areas investigated than previously published studies. In addition, several anatomical areas of the head and neck were individually evaluated, and the image diagnostic quality of the MRI cervical spine examination, never before evaluated, was also determined. The study was undertaken using a 3-T MRI scanner (Discovery MR750; General Electric, Milwaukee, WI) since a magnetic field of this strength is now increasingly used in clinical radiology, whereas in all previous studies, a magnetic field of lower strength was employed. The sequence used were representative for the pathologies usually investigated in the head and neck area. No contrast media was used. In the present study, evaluation was based on clinical criteria (diagnostic or non-diagnostic) unlike other studies that have measured the size of the artefact18 or pixel density.19
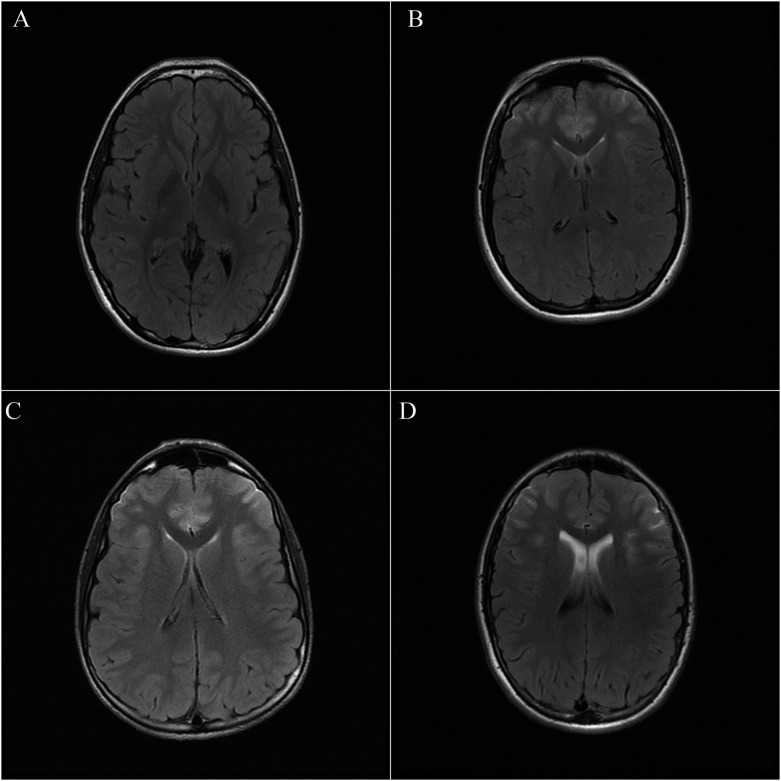
Based on the present study's results, stainless steel orthodontic appliances should be removed before MRI focused on the cervical region, cervical vertebrae, paranasal sinuses, and head and neck region because they often cause distortion in the resultant MRI. Concerning brain imaging in the patient group with stainless steel brackets, without archwires, the main artefact was the hyperattenuation of the subarachnoid spaces in the fluid attenuated inversion recovery images at the level of the frontal lobe, mainly in the straight gyra and the orbital gyra (Figure 8). This artefact could mimic pathology or interfere with the diagnosis of subarachnoid haemorrhage, meningitis and leptomeningeal carcinomatosis. In the group with stainless steel brackets and Ni-Ti archwires, the artefacts involve the frontal horn of the lateral ventricles. Lastly, in the group of patients with stainless steel brackets and stainless steel archwires, there was a complete loss of signal of the frontal lobe, making it impossible to evaluate the area for pathological or normal findings. The various regions of the brain parenchyma, aside from the frontal lobe, were almost always well displayed for diagnostic use. For the cervical and head and neck evaluation, the quality of the images was poor in all the groups with metallic orthodontic appliances. In particular, the paranasal sinus was completely non-visible (Figure 9) because, in this area, the metal artefact added to the issue of the loss of signal due to the natural presence of air. The cervical region displayed artefacts at the level of the spinal cord that appeared hyperintense in the T2 images, mimicking pathology. The artefacts were also severe on the bone marrow of the spine, whereas the effect on the hypointense spinal disc was not as great. On the basis of this observation, the examination of the spine was not diagnostic for the majority of patients (Figure 10). Head and neck structures in all three groups with metallic orthodontic appliances nearby resulted in images which were either wholly or partially indecipherable. Given that a great number of head and neck studies are performed due to lumps in the area generally caused by tumours or infections, a result which does not allow for a thorough evaluation should be considered diagnostically unacceptable (Figure 9). The only results which were diagnostically valid were those of the temporomandibular joint; the results could be due to the posterior and lateral position of the joint to the orthodontic appliance and may also be due to the high contrast signal between the articular components of the disc, bone and ligament (Figure 11). Though minor, the MR scan distortion recorded in the present study compromises the integrity of the scan and could make diagnosis of a particular condition difficult or impossible (i.e. epilepsy, searching for metastases etc). A compromised scan cannot be used for diagnosis and must be repeated.
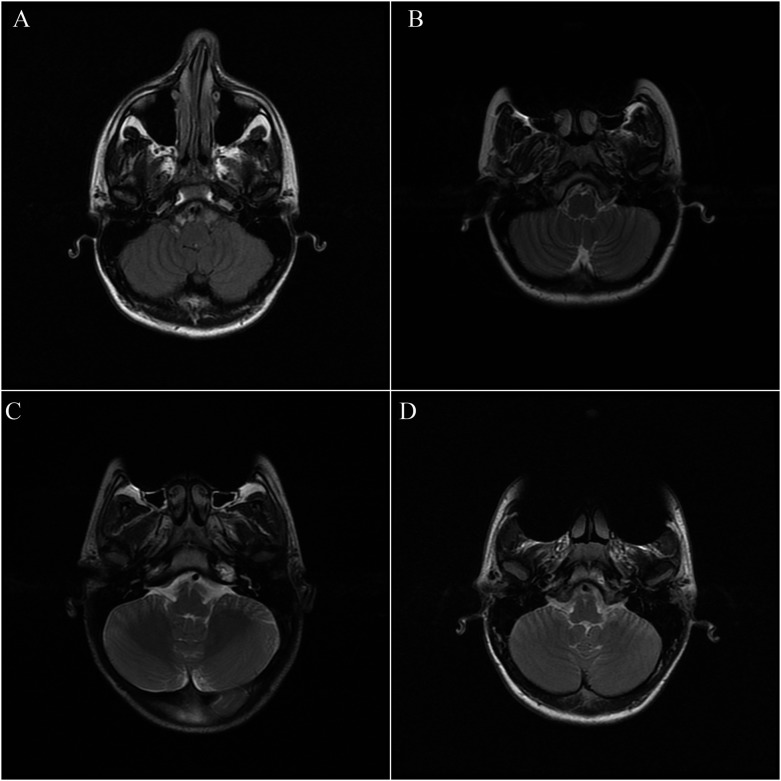
Figure 8.
Axial fluid attenuated inversion recovery (FLAIR) MR images of three groups with orthodontic appliances (b–d) showed artefacts caused by stainless steel brackets and archwires corresponding to hyperattenuation of the subarachnoid spaces in the FLAIR images at the level of the frontal lobe, mainly in the straight gyra and the orbital gyra. No artefacts were reported in the control group (a).
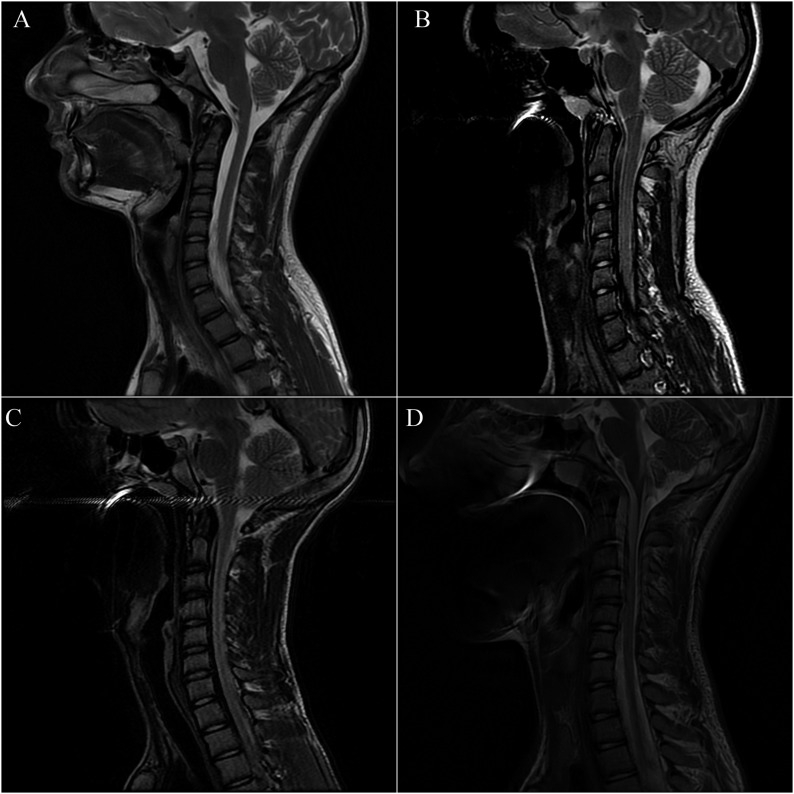
Figure 9.
Axial oblique double echo proton density and weighted/turbo spin echo T2 weighted MR images of three groups with orthodontic appliances (b–d) showed severe artefacts caused by stainless steel brackets and archwires corresponding to a complete or partial obliteration of the cervical area, paranasal sinuses and head and neck regions. No artefacts were reported in the control group (a).
Figure 10.
Sagittal turbo spin echo T2 weighted MR images of three groups with orthodontic appliances (b–d) showed severe artefacts caused by stainless steel brackets and archwires corresponding to an hyperintense signal of the spinal cord in the T2 images and a severe distortion on the bone marrow of the spine. No artefacts were reported in the control group (a).
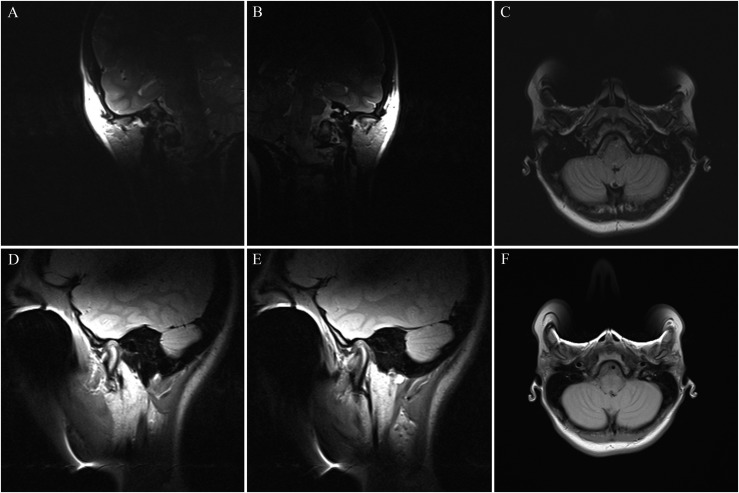
Figure 11.
Sagittal, axial and coronal double echo proton density (a–c) and weighted/turbo spin echo T2 weighted (d–f) sequences performed in a 23-year-old female patient with stainless steel brackets and stainless steel archwires, obtained at closed-mouthed position, showed diagnostic MR images of the temporomandibular joint region with a high quality. The contours of the articular disc, mandibular condyle, articular eminence, lateral pterygoid muscle and cortical bone are better displayed.
To minimize the likelihood of such distortions in MRI, one consideration is that materials used in dentistry could be selected based on whether they generate artefacts in MRI, and likewise, metals that cause MRI distortion should only be used in dentistry if they are removable and not fixed. Indeed, this consideration may be valid beyond the realm of dentistry, whereas one study reported that orthodontic braces had little effect on MRI of the brain and spinal cord, the oral region was significantly distorted,20 another study reported that 78% of the artefacts in brain MRI were caused by orthodontic metallic appliances.14
In a retrospective study aimed to identify the main metal dental objects that produce artefacts on brain MRIs, 1200 MRI scans performed for the investigation of epilepsy were assessed.14 Artefacts were observed in 6% of scans. Metallic orthodontic appliances produced 78% of the imaging artefacts (55 images), dental implants produced 18% (13 images) and dental gold crowns produced 4% (2 images). Orthodontic appliances were responsible for the largest number of misinterpretations of the MRI results, followed by dental implants (nine scans). All scans with artefacts caused by dental crowns presented acceptable diagnostic quality. The results of this study demonstrate that the most likely origin of dental artefacts is metallic orthodontic appliances leading to large areas of artefacts, making image interpretation difficult. These findings have been confirmed in the present study. Indeed, the presence of stainless steel orthodontic brackets and stainless steel or Ni-Ti archwires often cause distortion, negatively influencing MRI of the cervical region, paranasal sinuses, head and neck region, and cervical vertebrae.
In the study conducted by Sadowsky et al,21 the mouth and facial regions were affected by significant artefacts produced by fixed orthodontic appliances, and in most cases, the maxillary sinuses were not clearly visible. The lobes of the brain most affected by artefacts were the frontal and temporal lobes, but the degree of artefact varied from patient to patient. The artefacts were not considered severe enough to significantly alter the diagnostic quality of the scans in any of these cases. In this study,21 the temporomandibular joints were well visualized. The temporomandibular joint discs were well evaluated in both open and closed mouth positions. Disc displacement and recapture, when present, was adequately visualized, as well as the condyle heads. The degree of artefacts varied from patient to patient but were most obvious closer to the orthodontic appliances. These results agree with the results of the present study and highlight the absence of artefacts in MRI of the temporomandibular joint.
A previous study aimed to evaluate cranial MRI distortion caused by various orthodontic brackets (plastic, ceramic, Ti and stainless steel brackets), showed a statistically significant difference between the mean distortion scores of stainless steel brackets and the mean distortion scores of the other experimental MR scans.15 The plastic, ceramic and Ti brackets caused minimal distortion of cranial MRI (similar to the control group), whereas stainless steel brackets cause significant distortion, rendering non-diagnostic images of several cranial regions.15 The areas with the most distortion were the body of the mandible, hard palate, base of the tongue, globes, nasopharynx and frontal lobes.15 In general, the closer the stainless steel appliance was to a specific anatomical region, the greater the distortion of MRI.15 For ceramic, plastic and Ti brackets, all anatomical regions had an average distortion score within the limit of the diagnostic score.15 Stainless steel bracket material consistently had averages for each anatomical region in the non-diagnostic area of the grading scale.15 Only the brain stem received a distortion scale score that was within the range of a diagnostic score, but this score (2.69) was close to non-diagnostic.15 These results indicate that it might be appropriate to use ceramic, Ti or plastic brackets for patients who require MRI.15 To reduce the risk of removing stainless steel brackets, it is clearly important to improve our initial assessment of the probability that a patient will require cranial MRI and to avoid stainless steel brackets in those likely to require MRI scans. The results of this study were confirmed by the present study, although a magnetic field with higher strength was used.
A recent study22 aimed to find the exact indications for removal of various fixed attachments when imaging four specific areas of the head and neck (maxillary sinus, oral cavity, temporomandibular joints and posterior cerebral fossa) evaluated four different types of fixed attachments (stainless steel brackets, Ti brackets, ceramic brackets with metal slots and stainless steel retainers). Archwires were not investigated, as they are easily removed before a scan.22 Stainless steel brackets always caused non-interpretability of all anatomical areas (100%).22 Ti brackets, ceramic brackets with metal slots and stainless steel retainers caused artefacts in the oral cavity only.22 The presence of artefacts in the temporomandibular joint region, caused by stainless steel brackets, is in contrast with the results of the present study.
Considering the production of metal artefacts by multibracket devices while performing MRI of brackets having different arch wires, Dalili Kajan et al23 stated that stainless steel archwires (SS wires) had a considerable capacity to interfere with magnetic field gradients, inducing more metal artefacts. These results are in line with the present study results, confirming that nickel-Ti archwires (NiTi wires) induce smaller artefacts than SS wires.
The magnitude of susceptibility artefacts is also related to the type of imaging sequence used; some sequences are more sensitive to susceptibility artefacts.24 A more severe artefact is produced in images with a long TE because small differences in precession frequency have more time to increase a large phase error.24 Artefacts are most severe in gradient echo sequences owing to the absence of the 180° refocusing pulse.25 Therefore, the best sequence to reduce the severity of the susceptibility artefact would be a spin echo sequence with a short TE.26,27 However, in the study of Costa et al,14 the short TE was not sufficient to reduce the susceptibility artefact.
In conclusion, the radiologist should be aware of the effects of orthodontic appliances on the cervical region, cervical vertebrae, paranasal sinuses, and head and neck MRI scans affecting the diagnostic quality of these scans. Patients with a stainless steel multibracket orthodontic appliance should remove it before the scan. MRI of the brain and temporomandibular joint regions should not require the removal of such appliances.
Contributor Information
Michele Cassetta, Email: michele.cassetta@uniroma1.it.
Nicola Pranno, Email: nicola.pranno@uniroma1.it.
Alessandro Stasolla, Email: Alestaso@tiscali.it.
Nicola Orsogna, Email: nicola.orsogna@libero.it.
Davide Fierro, Email: fierrodavide852@hotmail.com.
Costanza Cavallini, Email: costanza.cavallini@uniroma1.it.
Vito Cantisani, Email: Vito.cantisani@uniroma1.it.
References
- 1.Cassetta M, Pranno N, Barchetti F, Sorrentino V, Lo Mele L. 3.0 Tesla MRI in the early evaluation of inferior alveolar nerve neurological complications after mandibular third molar extraction: a prospective study. Dentomaxillofac Radiol 2014; 43: 20140152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cassetta M, Pranno N, Pompa V, Barchetti F, Pompa G. High resolution 3-T MR imaging in the evaluation of the trigeminal nerve course. Eur Rev Med Pharmacol Sci 2014; 18: 257–64. [PubMed] [Google Scholar]
- 3.Mazza D, Marini M, Impara L, Cassetta M, Scarpato P, Barchetti F, et al. Anatomic examination of the upper head of the lateral pterygoid muscle using magnetic resonance imaging and clinical data. J Craniofac Surg 2009; 20: 1508–11. doi: https://doi.org/10.1097/scs.0b013e3181b09c32 [DOI] [PubMed] [Google Scholar]
- 4.Hargreaves BA, Worters PW, Pauly KB, Pauly JM, Koch KM, Gold GE. Metal-induced artifacts in MRI. AJR Am J Roentgenol 2011; 197: 547–55. doi: https://doi.org/10.2214/ajr.11.7364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matsumi S, Arita M, Morikawa M, Toyoda S. Effect of dental metals on magnetic resonance imaging (MRI). J Oral Rehabil 1993; 20: 97–106. [DOI] [PubMed] [Google Scholar]
- 6.Poorsattar-Bejeh Mir A, Rahmati-Kamel M. Should the orthodontic brackets always be removed prior to magnetic resonance imaging (MRI)? J Oral Biol Craniofac Res 2016; 6: 142–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Starčuk Z, Bartušek K, Hubálková H, Bachorec T, Starčuková J, Krupa P. Evaluation of MRI artifacts caused by metallic dental implants and classification of the dental materials in use. Meas Sci Rev 2006; 6: 24–7. [Google Scholar]
- 8.Gunzinger JM, Delso G, Boss A. Metal artifact reduction in patients with dental implants using multispectral three dimensional data acquisition for hybrid PET/MRI. EJNMMI Phys 2014; 1: 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beuf O, Lissac M, Cremillieux Y, Briguet A. Correlation between magnetic resonance imaging disturbances and the magnetic susceptibility of dental materials. Dent Mater 1994; 10: 265–8. doi: https://doi.org/10.1016/0109-5641(94)90072-8 [DOI] [PubMed] [Google Scholar]
- 10.Cassetta M, Di Carlo S, Pranno N, Stagnitti A, Pompa V, Pompa G. The use of high resolution magnetic resonance on 3.0-T system in the diagnosis and surgical planning of intraosseous lesions of the jaws: preliminary results of a retrospective study. Eur Rev Med Pharmacol Sci 2012; 16: 2021–8. [PubMed] [Google Scholar]
- 11.Cassetta M, Barchetti F, Pranno N, Marini M. Comparing proton density and turbo spin echo T2 weighted static sequences with dynamic half-Fourier single-shot TSE pulse sequence at 3.0 T in diagnosis of temporomandibular joint disorders: a prospective study. Dentomaxillofac Radiol 2014; 43: 20130387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wichmann W, Von Ammon K, Fink U, Weik T, Yasargil GM. Aneurysm clips made of titanium: magnetic characteristics and artifacts in MR. AJNR Am J Neuroradiol 1997; 18: 939–44. [PMC free article] [PubMed] [Google Scholar]
- 13.Leite L, Bell R. Adverse hypersensitivity reactions in orthodontics. Semin Orthod 2004; 10: 240–3. doi: https://doi.org/10.1053/j.sodo.2004.09.002 [Google Scholar]
- 14.Costa AL, Appenzeller S, Yasuda CL, Pereira FR, Zanardi VA, Cendes F. Artifacts in brain magnetic resonance imaging due to metallic dental objects. Med Oral Patol Oral Cir Bucal 2009; 14: E278–82. [PubMed] [Google Scholar]
- 15.Elison JM, Leggitt VL, Thomson M, Oyoyo U, Wycliffe ND. Influence of common orthodontic appliances on the diagnostic quality of cranial magnetic resonance images. Am J Orthod Dentofacial Orthop 2008; 134: 563–72. doi: https://doi.org/10.1016/j.ajodo.2006.10.038 [DOI] [PubMed] [Google Scholar]
- 16.Görgülü S, Ayyildiz S, Kamburoglu K, Gökçe S, Ozen T. Effect of orthodontic brackets and different wires on radiofrequency heating and magnetic field interactions during 3-T MRI. Dentomaxillofac Radiol 2014; 43: 20130356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hasegawa M, Miyata K, Abe Y, Ishigami T. Radiofrequency heating of metallic dental devices during 3.0 T MRI. Dentomaxillofac Radiol 2013; 42: 20120234. doi: https://doi.org/10.1259/dmfr.20120234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abbaszadeh K, Heffez LB, Mafee MF. Effect of interference of metallic objects on interpretation of T1-weighted magnetic resonance images in the maxillofacial region. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 89: 759–65. doi: https://doi.org/10.1067/moe.2000.105942 [DOI] [PubMed] [Google Scholar]
- 19.Shafiei F, Honda E, Takahashi H, Sasaki T. Artifacts from dental casting alloys in magnetic resonance imaging. J Dent Res 2003; 82: 602–6. doi: https://doi.org/10.1177/154405910308200806 [DOI] [PubMed] [Google Scholar]
- 20.Hinshaw DB, Holshouser BA, Engstrom HI, Tjan AH, Christiansen EL, Catelli WF. Dental material artifacts on MR images. Radiology 1988; 166: 777–9. doi: https://doi.org/10.1148/radiology.166.3.3340777 [DOI] [PubMed] [Google Scholar]
- 21.Sadowsky PL, Bernreuter W, Lakshminarayanan AV, Kenney P. Orthodontic appliances and magnetic resonance imaging of the brain and temporomandibular joint. Angle Orthod 1988; 58: 9–20. [DOI] [PubMed] [Google Scholar]
- 22.Beau A, Bossard D, Gebeile-Chauty S. Magnetic resonance imaging artefacts and fixed orthodontic attachments. Eur J Orthod 2015; 37: 105–10. doi: https://doi.org/10.1093/ejo/cju020 [DOI] [PubMed] [Google Scholar]
- 23.Dalili Kajan Z, Khademi J, Alizadeh A, Babaei Hemmaty Y, Atrkar Roushan Z. A comparative study of metal artifacts from common metal orthodontic brackets in magnetic resonance imaging. Imaging Sci Dent 2015; 45: 159–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harris CA, White LM. Metal artifact reduction in musculoskeletal magnetic resonance imaging. Orthop Clin North Am 2006; 37: 349–59. doi: https://doi.org/10.1016/j.ocl.2006.04.001 [DOI] [PubMed] [Google Scholar]
- 25.Brown MA, Semelka RC. MR imaging abbreviations, definitions, and descriptions: a review. Radiology 1999; 213: 647–62. doi: https://doi.org/10.1148/radiology.213.3.r99dc18647 [DOI] [PubMed] [Google Scholar]
- 26.Tartaglino LM, Flanders AE, Vinitski S, Friedman DP. Metallic artifacts on MR images of the postoperative spine: reduction with fast spin-echo techniques. Radiology 1994; 190: 565–9. doi: https://doi.org/10.1148/radiology.190.2.8284417 [DOI] [PubMed] [Google Scholar]
- 27.Arena L, Morehouse HT, Safi RJ. MR imaging artifacts that simulate disease: how to recognize and eliminate them. Radiographics 1995; 15: 1373–94. doi: https://doi.org/10.1148/radiographics.15.6.8577963 [DOI] [PubMed] [Google Scholar]