Abstract
OBJECTIVE
To assess participant-level results from the first 4 years of implementation of the National Diabetes Prevention Program (National DPP), a national effort to prevent type 2 diabetes in those at risk through structured lifestyle change programs.
RESEARCH DESIGN AND METHODS
Descriptive analysis was performed on data from 14,747 adults enrolled in year-long type 2 diabetes prevention programs during the period February 2012 through January 2016. Data on attendance, weight, and physical activity minutes were summarized and predictors of weight loss were examined using a mixed linear model. All analyses were performed using SAS 9.3.
RESULTS
Participants attended a median of 14 sessions over an average of 172 days in the program (median 134 days). Overall, 35.5% achieved the 5% weight loss goal (average weight loss 4.2%, median 3.1%). Participants reported a weekly average of 152 min of physical activity (median 128 min), with 41.8% meeting the physical activity goal of 150 min per week. For every additional session attended and every 30 min of activity reported, participants lost 0.3% of body weight (P < 0.0001).
CONCLUSIONS
During the first 4 years, the National DPP has achieved widespread implementation of the lifestyle change program to prevent type 2 diabetes, with promising early results. Greater duration and intensity of session attendance resulted in a higher percent of body weight loss overall and for subgroups. Focusing on retention may reduce disparities and improve overall program results. Further program expansion and investigation is needed to continue lowering the burden of type 2 diabetes nationally.
Introduction
Diabetes takes a significant toll on the public’s health and on our nation’s health care systems and payers. In addition to the 29 million people in the U.S. population with diabetes, the Centers for Disease Control and Prevention (CDC) estimates that 86 million adults aged 20 years or older have prediabetes (1) according to the American Diabetes Association (ADA) definition (2). People with prediabetes have blood glucose levels that are higher than normal but not high enough to be considered diabetes (1). Prediabetes increases the risk for type 2 diabetes, heart disease, and stroke (1). The Diabetes Prevention Program (DPP) randomized controlled trial and its follow-up translation studies have demonstrated that in many cases, type 2 diabetes can be prevented or delayed for those at high risk (3,4) through a structured intervention that can be delivered cost effectively in real-world settings (5,6). These interventions are year-long lifestyle change programs that focus on achievement of modest weight loss (5–7%) and moderate increases in physical activity (7–12). However, several challenges related to resourcing, delivery, and engagement have had to be addressed to achieve large-scale implementation of these evidence-based lifestyle change programs.
To accomplish widespread implementation of the 2002 DPP study results, Congress authorized CDC to establish and manage the National DPP. The National DPP is a comprehensive approach that is establishing a system to link the community and clinical sectors in order to scale the lifestyle intervention for type 2 diabetes prevention to achieve a population health impact. CDC, in collaboration with nongovernmental partners, developed an evidence-based curriculum with training guide for lifestyle coaches to deliver the year-long lifestyle change program (4) to people with diagnosed prediabetes or who are at high risk for developing type 2 diabetes. The CDC evidence-based curriculum and all supplemental materials are available in English and Spanish. The program consists of 16 hourly sessions held at approximately weekly intervals during the first 6 months, followed by a minimum of six sessions held at approximately monthly intervals during months 7–12. The second 6 months is intended to reinforce and build on content delivered in the first half of the program. The 1-year duration and minimum of 22 sessions (i.e., intensity) are key to program success. The format of program delivery is customizable by stakeholders as long as key criteria are met, including the use of a CDC-approved curriculum that focuses on lifestyle change and the importance of at least moderate physical activity of 150 min or more each week, healthy eating, and weight loss of 5–7% over a 1-year period of time. Organizations must also meet program eligibility requirements of minimally 50% of a participant cohort entering with a qualifying blood test or history of gestational diabetes mellitus (GDM). These key criteria are outlined in a set of evidence-based standards and operating procedures (13).
In March 2016, the Centers for Medicare and Medicaid Services (CMS) certified that the National DPP model was both cost saving and able to improve the quality of patient care. The Department of Health and Human Services then declared it the first-ever preventive service model certified for expansion from the CMS Innovation Center. CMS has proposed expanding the DPP to benefit more Medicare beneficiaries beginning 1 January 2018 (14).
To ensure quality and fidelity of type 2 diabetes prevention programs nationally, CDC established the Diabetes Prevention Recognition Program (DPRP) to monitor and support the delivery of National DPP lifestyle change programs grounded in an evidence-based set of evaluation standards. CDC recognition is granted to organizations that have applied to the DPRP and have been approved based on factors that include using a CDC-approved curriculum and agreeing to the specified intensity and duration requirements. Through maintenance of an ongoing registry of programs and the monitoring of participant weight loss and behavioral responses to the National DPP, the DPRP is designed to ensure broad use of effective type 2 diabetes prevention lifestyle interventions in the U.S. Here, we report the first 4 years of experience (February 2012 to January 2016) of participants enrolled in CDC-recognized diabetes prevention programs in the National DPP (including organizations in both pending and full recognition status), including their adherence, weight loss, and physical activity in response to the intervention and variation according to their characteristics.
Research Design and Methods
Population
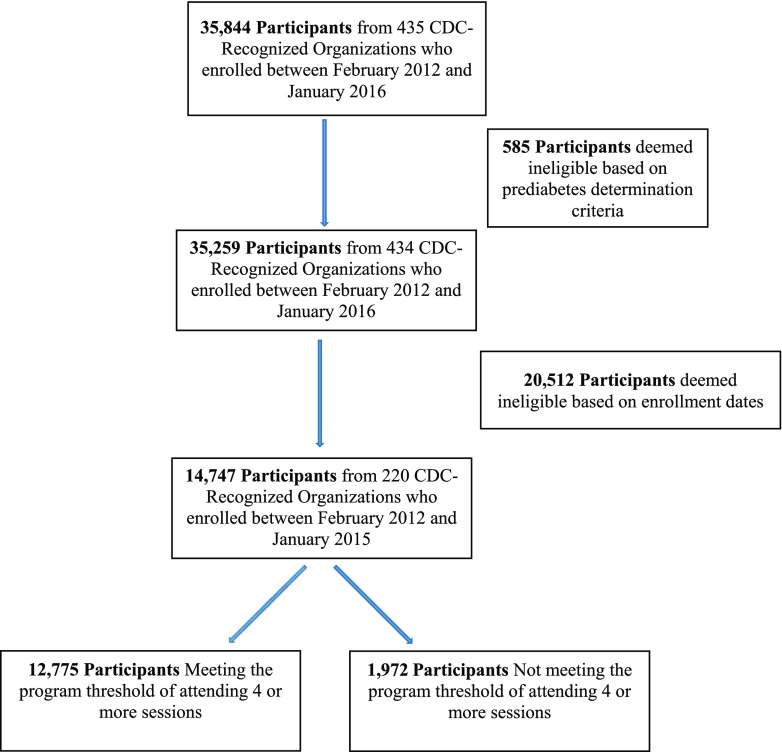
These analyses are based on registry data collected on all 35,844 adults aged 18 years and older received from 435 CDC-recognized organizations that had at least 12 months of submitted data. These are participants who were enrolled in a program (i.e., attended at least one class) between February 2012 and January 2016. Counted among these organizations are those that have subsequently voluntarily withdrawn from the program (n = 24), as well as those that have had their recognition revoked (n = 53) due to factors that include not making required data submissions or not meeting specific program requirements. Although the DPRP allows virtual programs, the first such program began in February 2015 and therefore did not have 1-year data to submit within the study period. Because the program is designed for adults at high risk for type 2 diabetes, a participant’s eligibility was based on the results of a blood-based test (A1C, fasting blood glucose [FBG], or oral glucose tolerance test [OGTT]), a history of GDM, or their score on the CDC’s or the ADA’s prediabetes risk test. Of the 35,844 adults with data submitted to the registry, 585 (1.6%) were excluded because they did not meet this participant eligibility criterion, leaving a total of 35,259 eligible participants. Of the 35,259 eligible participants, only 14,747 are included in the primary analysis. These are participants who were enrolled in a program between February 2012 and January 2015 with sessions delivered for at least 12 months after their enrollment (Fig. 1 provides a schematic of the inclusion/exclusion of participants).
Figure 1.
Flowchart of study inclusion/exclusion criteria.
Variables
The National DPP lifestyle change program consists of a series of sessions in which trained lifestyle coaches provide information based on an approved curriculum, suggest at-home activities that augment session content, and offer feedback to participants in stages to optimize behavioral change. Program attendance for each participant is the total number of sessions the person attended during the 12-month program. The primary threshold was set a priori as four sessions, as defined in the DPRP standards (13). The DPRP considers this to be the minimum dose to begin seeing lifestyle/weight change that can impact the prevention or delay of type 2 diabetes. By using this threshold, there is the possibility of three weight loss points in the analysis, which the program believes is enough to see some forward progression on that measure. However, results were also assessed by number of sessions attended to better describe the effect of participation intensity.
Number of months in the program was calculated as the number of days from first session attended to last session attended, divided by 30.4, and rounded. A person attending only one session is said to have attended only month 1 of the program.
Body weight was recorded at each session attended, and a goal of 5–7% weight loss was encouraged. Percent weight change was calculated for those with at least two documented body weights. This analysis uses the first (baseline) and last recorded weights (up to 12 months after baseline) to calculate the percent of body weight lost.
It was also recommended that participants engage in moderate to vigorous physical activity for at least 150 min per week (15). The DPRP requires participants to report the number of minutes of physical activity that were performed in the week prior to each session (valid entries ranged from 0 to 997 min). The average reported physical activity minutes were calculated for each participant as the total number of minutes reported divided by the number of sessions in which minutes were reported.
Additional information collected on each participant included demographic information (self-reported sex, age, race, and ethnicity) as well as dates of the sessions attended. The data used in this report have been checked against a series of validations for incorrect formatting and coding. The distributions of weight change and physical activity minutes over all participants are used in conjunction with the number of sessions attended and the number of days that participants remained in the program (defined as the time lapsed from the first session attended to the last session attended, up to 12 months) to determine the effectiveness of the delivery of the intervention. All analyses were conducted using SAS 9.3.
Data Analysis
All measures were stratified on sex, age category at enrollment (18–44, 45–64, and 65+ years), race/ethnicity (Hispanic, non-Hispanic white only, non-Hispanic black only, and other), eligibility category (entered the program based on a blood test result or history of GDM, or entered the program based on a risk test only), and baseline BMI category (normal: <25 kg/m2, overweight: 25–29 kg/m2, and obese: ≥30 kg/m2). The “other” group for race/ethnicity primarily included participants who identified themselves as being multiracial or Asian but also those who did not respond to the ethnicity or race questions.
We compared characteristics of participants who attended less than four sessions with those of participants who attended at least four sessions (i.e., participants meeting the threshold). A Pearson χ2 test was used to determine whether the distribution of each categorical demographic variable was different among participants meeting the threshold and participants not meeting the threshold. A two-sample Student t test was used to test for differences between these two groups for the two continuous variables (baseline weight and number of days in the program), as well as for the average weight loss at the end of the 12-month intervention period. Bivariate analysis was used to determine the significance of odds ratios associated with achieving the 150 min per week physical activity goal within subgroups. P values <0.05 were considered statistically significant for all analyses.
A mixed linear regression model (PROC MIXED in SAS 9.3) was used to analyze the association between both the number of sessions attended and average reported physical activity minutes (independent variables) on percent weight loss (dependent variable). Twelve months was the maximum period for which participant session data could be included for analysis; the period could be shorter depending on how long a participant remained in the program. The model considered the organization in which a participant enrolled as a random effect. Modeled estimates of weight loss were adjusted for a participant’s sex, age category, race/ethnicity, and BMI category. Participant eligibility category was initially included in the model, but it was not found to be significant so it was removed.
Results
Across 220 organizations delivering diabetes prevention programs in 40 states and the District of Columbia, 14,747 participants had been associated with a program for 12 months. Table 1 displays the characteristics of participants within demographic subgroups, by program completion status. Of the 14,747 participants included in these analyses, 80.3% were female. Approximately half of participants (56.0%) were aged 45–64 years, 19.9% were aged 18–44 years, and 24.2% were aged 65+ years; average age was 55.1 years. Participants were ethnically and racially diverse, with 44.9% non-Hispanic white only, 10.0% Hispanic, 13.8% non-Hispanic black only, and 31.3% reporting another race/ethnicity or combination (other). Three-fourths of the participants were found to have obesity, and 22.5% were overweight. Approximately 63.7% had a blood-based test to determine prediabetes status or history of GDM, whereas the remaining 36.3% entered the program on the basis of a risk test alone.
Table 1.
| All eligible participants, n = 14,747 | Participants not meeting the threshold, n = 1,972 (13.4%)‡ | Participants meeting the threshold, n = 12,775 (86.6%)§ | P value (meeting the threshold vs. not meeting the threshold)‖ | |
|---|---|---|---|---|
| Sex | <0.9674 | |||
| Male | 19.7% | 19.7% | 19.7% | |
| Female | 80.3% | 80.3% | 80.3% | |
| Age-group (years) | <0.0001 | |||
| 18–44 | 19.9% | 28.1% | 18.6% | |
| 45–64 | 56.0% | 55.3% | 56.1% | |
| 65+ | 24.2% | 16.6% | 25.3% | |
| Average age (years) | 55.1 | 52.0 | 55.6 | |
| Race/ethnicity | <0.0001 | |||
| Hispanic | 10.0% | 17.3% | 8.9% | |
| Non-Hispanic white only | 44.9% | 26.4% | 47.7% | |
| Non-Hispanic black only | 13.8% | 16.2% | 13.4% | |
| Other | 31.3% | 40.1% | 30.0% | |
| Baseline BMI (kg/m2) | 0.7831 | |||
| <25 (normal) | 2.8% | 2.7% | 2.8% | |
| 25–29 (overweight) | 22.5% | 22.9% | 22.4% | |
| ≥30 (obese) | 74.8% | 74.4% | 74.8% | |
| Eligibility category | 0.0170 | |||
| Entered program with blood test or history of GDM | 63.7% | 66.1% | 63.4% | |
| Entered program with risk test only | 36.3% | 33.9% | 36.6% | |
| Average initial weight (kg)** | 96.8 | 96.5 | 96.8 | 0.5217 |
| Average number of days in the program†† | 172 | 12 | 197 | <0.0001 |
*A participant’s eligibility was based on the results of a blood-based test (A1C, FBG, or OGTT), their score on the CDC’s or the ADA’s prediabetes risk test, or a history of GDM.
†Participants must have been enrolled between February 2012 and January 2015 in a program that held sessions for at least 12 months after their enrollment and attended at least one session.
‡Participants who attended less than four sessions.
§Participants who attended four or more sessions.
‖Results are based on Pearson χ2 test for categorical variables and two-sample Student t test for continuous variables.
**Median initial weights were 93.4 kg overall, 92.9 kg for those not meeting the threshold, and 93.4 kg for those meeting the threshold.
††Median number of days in the program was 134 overall, 7 for those not meeting the threshold, and 182 for those meeting the threshold.
Approximately 86.6% (12,775) of participants met the threshold of attending four or more sessions. The age distribution was different for these participants compared with those not meeting the threshold, with participants attending four or more sessions older than those not meeting this threshold (P < 0.0001). There were also important differences by race/ethnicity (P < 0.0001), although not by sex, BMI category, or initial weight (P > 0.5 for each) (Table 1).
The overall average baseline weight was 96.8 kg. Among the 12,775 participants meeting the threshold, Hispanic participants had the lowest average baseline weight: 88.9 kg compared with 97.4 kg among non-Hispanic white participants, 100.4 kg among non-Hispanic black participants, and 96.6 kg among participants of other race/ethnicity (data not shown).
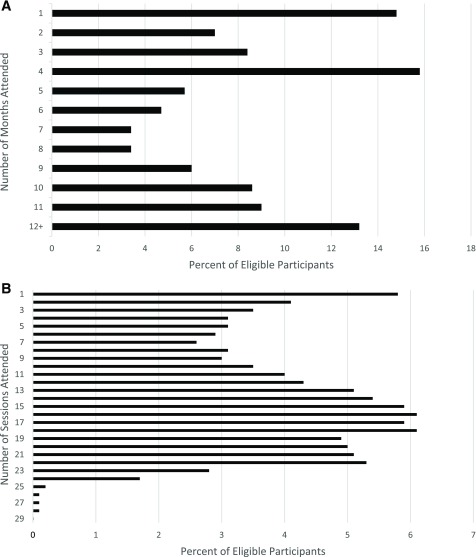
The average number of days in the program for all eligible participants was 172 with a median of 134. Figure 2A translates the number of days each participant attended sessions into months attended. The most common duration was 4 months (15.8%) followed by 1 month (14.8%) and 12+ months (13.2%). Nearly half (48.3%) of participants remained in the program for at least 6 months. The median number of sessions attended was 14, with most of these within the first 6 months of the program (Fig. 2B and Table 2). The most common numbers of sessions attended were 16 and 18 (each with 6.1%), 15 and 17 (each with 5.9%), and 1 (5.8%) (Fig. 2B); 10.4% of eligible participants attended at least the full 22-session program.
Figure 2.
A: Number of eligible participants enrolled in the lifestyle change program, by number of months in the program. Median number of months attended was 5. B: Number of eligible participants enrolled in the lifestyle change program, by number of sessions attended. Median number of sessions attended was 14. A participant’s eligibility was based on the results of a blood-based test (A1C, FBG, or OGTT), their score on the CDC’s or the ADA’s prediabetes risk test, or a history of GDM. Participants must have been enrolled between February 2012 and January 2015 in a program that held sessions for at least 12 months after their enrollment and attended at least one session. Number of months in the program is calculated as the number of days from first session attended to last session attended, divided by 365, multiplied by 12, and rounded. A person attending only the first session offered is said to have attended only month 1 of the program.
Table 2.
Participants’ attendance and percent body weight lost (unadjusted) by number of sessions attended among eligible* participants enrolled† in the lifestyle change program
| Percent of body weight lost from first to last session attended among those reporting at least 2 weights (94.2% of 14,747) |
Percent achieving weight loss goal of ≥5%, n = 13,893§ | Odds ratios for meeting 5% goal | P value# | ||||
|---|---|---|---|---|---|---|---|
| Sessions attended, n = 14,747‡ |
All eligible participants, n = 13,893§ |
Participants not meeting the threshold, n = 1,118‖ |
Participants meeting the threshold, n = 12,775¶ |
||||
| Median (25th, 75th) | Median (25th, 75th) | Median (25th, 75th) | Median (25th, 75th) | ||||
| Total | 14 (7, 19) | 3.1 (0.8, 6.7) | 0.4 (+0.3, 1.2) | 3.6 (1.1, 7.1) | 35.5 | ||
| Sex | |||||||
| Male** | 14 (8, 19) | 3.8 (1.1, 7.4) | 0.4 (+0.2, 1.4) | 4.1 (1.4, 7.7) | 40.0 | — | — |
| Female | 14 (7, 19) | 3.0 (0.7, 6.5) | 0.4 (+0.3, 1.2) | 3.4 (1.0, 6.9) | 34.5 | 0.788 | <0.0001 |
| Age group (years) | |||||||
| 18–44** | 12 (5, 16) | 2.2 (0.3, 5.4) | 0.3 (+0.5, 1.1) | 2.7 (0.5, 5.9) | 27.5 | — | — |
| 45–64 | 14 (7, 18) | 3.1 (0.8, 6.7) | 0.4 (+0.1, 1.3) | 3.5 (1.1, 7.0) | 35.0 | 1.422 | 0.8756 |
| 65+ | 16 (10, 20) | 4.1 (1.4, 7.6) | 0.4 (+0.2, 1.1) | 4.4 (1.8, 7.9) | 43.1 | 1.999 | <0.0001 |
| Race/ethnicity | |||||||
| Hispanic | 11 (4, 16) | 2.5 (0.5, 5.9) | 0.4 (+0.4, 1.3) | 3.0 (0.9, 6.5) | 30.8 | 0.583 | 0.1352 |
| Non-Hispanic/white only** | 16 (10, 20) | 4.1 (1.4, 7.8) | 0.5 (+0.3, 1.3) | 4.4 (1.7, 8.0) | 43.2 | — | — |
| Non-Hispanic/black only | 13 (7, 18) | 2.2 (0.3, 5.3) | 0.4 (0.0, 1.3) | 2.6 (0.5, 5.7) | 27.1 | 0.489 | <0.0001 |
| Other | 12 (6, 16) | 2.6 (0.4, 5.7) | 0.4 (+0.2, 1.1) | 3.0 (0.8, 6.3) | 29.1 | 0.540 | <0.0001 |
| Baseline BMI (kg/m2) | |||||||
| <25** | 14 (7, 19) | 2.8 (0.8, 6.0) | 0.9 (0.0, 1.4) | 3.2 (0.9, 6.1) | 30.8 | — | — |
| 25–29 | 14 (8, 19) | 3.4 (0.9, 6.8) | 0.5 (0.0, 1.2) | 3.8 (1.2, 7.1) | 37.2 | 1.352 | 0.0115 |
| ≥30 | 14 (8, 19) | 3.1 (0.8, 6.8) | 0.4 (+0.3, 1.2) | 3.6 (1.1, 7.2) | 35.9 | 1.289 | 0.1030 |
| Eligibility category | |||||||
| Entered program with blood test/history of GDM** | 14 (7, 19) | 3.2 (0.8, 6.8) | 0.4 (+0.2, 1.3) | 3.7 (1.2, 7.1) | 36.1 | — | — |
| Entered program on risk test only | 14 (8, 18) | 3.0 (0.7, 6.6) | 0.3 (+0.3, 1.1) | 3.4 (1.0, 7.0) | 34.6 | 0.938 | 0.0834 |
*A participant’s eligibility was based on the results of a blood-based test (A1C, FBG, or OGTT), their score on the CDC’s or the ADA’s prediabetes risk test, or a history of GDM.
†Participants must have been enrolled between February 2012 and January 2015 in a program that held sessions for at least 12 months after their enrollment and attended at least one session.
‡Among all eligible participants who attended at least one session.
§Among all eligible participants who reported at least two weights.
‖Participants who attended less than four sessions.
¶Participants who attended four or more sessions.
#Results are based on Pearson χ2 test for categorical variables and two-sample Student t test for continuous variables.
**Reference group for bivariate analysis.
Table 2 displays the medians and quartiles for percent body weight lost among the 13,893 participants (94.2%) reporting at least two weights. The overall average weight lost was 4.2% (median 3.1%), with 35.5% of participants achieving the ≥5% weight loss goal. Median weight lost among participants meeting the four-session threshold was 3.6% compared with 0.4% for those not meeting it. The odds of meeting the 5% weight loss goal were significantly lower among females than males, younger participants than older ones, and non-Hispanic black and participants in the other race/ethnicity category compared with non-Hispanic white participants (all P < 0.0001).
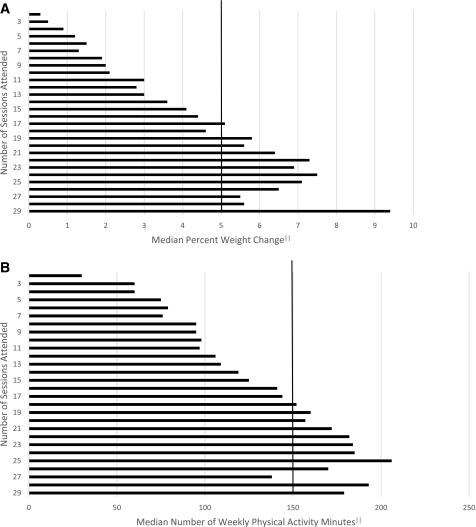
Median percent body weight loss generally increased as the number of sessions attended increased, up to ∼24 sessions (Fig. 3A). Median weight loss of ≥5% was generally achieved by participants who attended at least 17 sessions (viewed as participants who completed the initial weekly phase of the program and had attended at least one session of the monthly phase of the program). Percent body weight lost by duration and intensity of participation are examined more closely in Table 3. Median weight loss among participants attending at least 17 sessions and remaining in the program for 7–12 months was 6.0%, compared with 1.9% among those attending 2–16 sessions and remaining in the program 1–6 months. These results were consistent across all demographic, BMI, and eligibility categories; weight loss ranged from 4.9 to 6.6% among participants with high duration and intensity of participation, and 1.1 to 2.4% among those with low duration and intensity.
Figure 3.
A: Median percent weight change (among participants with at least two recorded weights [94.2%]) by number of sessions attended for eligible participants enrolled in a lifestyle change program. B: Median number of weekly physical activity minutes (among participants who reported physical activity minutes [87.7%]) by number of sessions attended for eligible participants enrolled in a lifestyle change program. A participant’s eligibility was based on the results of a blood-based test (A1C, FBG, or OGTT), their score on the CDC’s or the ADA’s prediabetes risk test, or a history of GDM. Participants must have been enrolled between February 2012 and January 2015 in a program that held sessions for at least 12 months after their enrollment and attended at least one session. ‖, the vertical reference line indicates the 5% weight loss goal (A) and 150-min physical activity goal (B).
Table 3.
Percent body weight lost (unadjusted), by program attendance, as reported by eligible* participants enrolled† in the lifestyle change program
| Percent of body weight lost from first to last session attended among those reporting at least 2 weights, n = 13,893 |
||||
|---|---|---|---|---|
| 1–6 months in the program, n = 7,585 |
7–12 months in the program, n = 6,308 |
|||
| 2–16 sessions attended, n = 7,290 |
17+ sessions attended, n = 295 |
2–16 sessions attended, n = 1,500 |
17+ sessions attended, n = 4,808 |
|
| Median (25th, 75th) | Median (25th, 75th) | Median (25th, 75th) | Median (25th, 75th) | |
| Total | 1.9 (0.3, 4.2) | 5.7 (3.1, 8.8) | 3.2 (0.8, 6.5) | 6.0 (2.7, 10.1) |
| Sex | ||||
| Male | 2.4 (0.5, 4.9) | 6.3 (4.0, 10.6) | 3.5 (0.7, 6.9) | 6.6 (3.3, 10.6) |
| Female | 1.8 (0.2, 4.1) | 5.6 (2.8, 8.4) | 3.1 (0.8, 6.3) | 5.9 (2.6, 9.9) |
| Age-group (years) | ||||
| 18–44 | 1.4 (0.0, 3.6) | 3.7 (1.9, 7.4) | 2.6 (0.0, 6.1) | 5.3 (2.0, 9.7) |
| 45–64 | 1.9 (0.4, 4.2) | 5.8 (3.3, 9.0) | 3.1 (0.7, 6.5) | 5.9 (2.5, 10.1) |
| 65+ | 2.4 (0.6, 4.7) | 6.1 (3.1, 9.5) | 3.5 (1.1, 6.9) | 6.4 (3.3, 10.1) |
| Race/ethnicity | ||||
| Hispanic | 1.5 (0.3, 4.1) | 6.1 (4.9, 7.7) | 2.8 (0.6, 7.2) | 5.5 (2.4, 9.7) |
| Non-Hispanic/white only | 2.3 (0.6, 4.7) | 5.5 (2.7, 8.8) | 3.5 (1.0, 7.0) | 6.6 (3.3, 11.0) |
| Non-Hispanic/black only | 1.1 (0.0, 3.0) | 4.7 (1.6, 6.7) | 2.7 (0.6, 5.5) | 4.9 (1.8, 8.3) |
| Other | 1.8 (0.2, 4.1) | 6.1 (3.1, 10.2) | 3.0 (0.6, 5.9) | 5.3 (1.8, 9.0) |
| Baseline BMI (kg/m2) | ||||
| <25 | 1.9 (0.0, 4.2) | 4.3 (1.5, 5.7) | 2.2 (0.7, 5.3) | 5.0 (2.1, 7.9) |
| 25–29 | 2.0 (0.4, 4.5) | 5.7 (2.8, 8.4) | 3.4 (0.6, 6.6) | 5.9 (2.9, 9.4) |
| ≥30 | 1.9 (0.3, 4.2) | 5.8 (3.1, 8.9) | 3.1 (0.8, 6.5) | 6.2 (2.7, 10.4) |
| Eligibility category | ||||
| Entered program with blood test/history of GDM | 1.9 (0.4, 4.3) | 5.7 (2.9, 8.8) | 3.2 (0.9, 6.7) | 6.1 (2.8, 9.9) |
| Entered program on risk test only | 1.9 (0.2, 4.1) | 5.8 (3.4, 8.7) | 3.1 (0.6, 6.2) | 6.0 (2.5, 10.4) |
*A participant’s eligibility was based on the results of a blood-based test (A1C, FBG, or OGTT), their score on the CDC’s or the ADA’s prediabetes risk test, or a history of GDM.
†Participants must have been enrolled between February 2012 and January 2015 in a program that held sessions for at least 12 months after their enrollment and attended at least one session.
Table 4 displays participants’ average weekly physical activity minutes. Valid activity minutes were reported by 87.7% of the participants analyzed (n = 12,929). Overall, participants reported an average 152 (median 128) weekly minutes of physical activity, and 41.8% of participants achieved the physical activity goal of 150 min per week. Females showed significantly lower odds of achieving the goal than males (P < 0.0001). Participants aged 45–64 and 65+ years were more likely to achieve the goal than those 18–44 years (P < 0.05). Hispanics and those in the other race/ethnicity category showed a lower odds than non-Hispanic whites (P < 0.0001), and participants with obesity had a significantly lower odds than those of normal weight (P < 0.0001). Figure 3B shows that median physical activity minutes increased with number of sessions attended, up to 25 sessions. Those attending 18 or more sessions generally achieved the goal of 150 min per week. A total of 12,900 participants reported physical activity minutes during the first 6 months of the program, and 3,368 participants reported minutes during the second 6 months. Overall, and in all subgroups, the median average weekly physical activity minutes reported was lower in the first 6 months (phase 1) than the second 6 months (phase 2). However, among the 3,339 participants who reported physical activity minutes in both program phases, the median decreased from 166 to 150 min.
Table 4.
Weekly physical activity minutes, overall and by program phase, as reported by eligible* participants enrolled† in the lifestyle change program
| Weekly physical activity minutes, n = 12,929‡ | Weekly physical activity minutes recorded during months 1–6, n = 12,900§ | Weekly physical activity minutes recorded during months 7–12, n = 3,368‖ | Percent achieving physical activity goal of 150 min/week, n = 12,929‡ | Odds ratios¶ | P value# | |
|---|---|---|---|---|---|---|
| Median (25th, 75th) | Median (25th, 75th) | Median (25th, 75th) | ||||
| Total | 128 (66, 203) | 128 (65, 203) | 150 (71, 240) | 41.8 | ||
| Sex | ||||||
| Male** | 154 (84, 244) | 153 (84, 244) | 165 (86, 297) | 52.3 | — | — |
| Female | 123 (63, 195) | 122 (62, 194) | 150 (70, 232) | 39.2 | 0.589 | <0.0001 |
| Age-group (years) | ||||||
| 18–44** | 113 (55, 177) | 113 (55, 175) | 145 (73, 211) | 34.3 | — | — |
| 45–64 | 124 (62, 200) | 123 (61, 199) | 150 (69, 240) | 40.2 | 1.284 | 0.0127 |
| 65+ | 150 (86, 229) | 150 (86, 230) | 150 (75, 253) | 50.9 | 1.979 | <0.0001 |
| Race/ethnicity | ||||||
| Hispanic | 144 (77, 209) | 144 (77, 211) | 149 (68, 240) | 47.3 | 0.952 | <0.0001 |
| Non-Hispanic/white only** | 146 (88, 220) | 147 (87, 220) | 150 (85, 240) | 48.6 | — | — |
| Non-Hispanic/black only | 122 (63, 205) | 119 (60, 196) | 173 (109, 329) | 39.9 | 0.703 | 0.1256 |
| Other | 98 (42, 168) | 99 (42, 170) | 60 (0, 172) | 30.7 | 0.469 | <0.0001 |
| Baseline BMI (kg/m2) | ||||||
| <25** | 161 (93, 271) | 158 (93, 259) | 183 (130, 360) | 54.8 | — | — |
| 25–29 | 142 (76, 218) | 141 (75, 218) | 150 (60, 248) | 46.6 | 0.721 | 0.7132 |
| ≥30 | 123 (62, 197) | 123 (61, 196) | 150 (73, 232) | 39.8 | 0.546 | <0.0001 |
| Eligibility category | ||||||
| Entered program with blood test/history of GDM** | 130 (68, 205) | 129 (67, 204) | 150 (75, 240) | 42.2 | — | — |
| Entered program on risk test only | 127 (63, 200) | 128 (62, 200) | 150 (68, 240) | 41.0 | 0.949 | 0.1611 |
*A participant’s eligibility was based on the results of a blood-based test (A1C, FBG, or OGTT), their score on the CDC’s or the ADA’s prediabetes risk test, or a history of GDM.
†Participants must have been enrolled between February 2012 and January 2015 in a program that held sessions for at least 12 months after their enrollment and attended at least one session.
‡Among all eligible participants who reported physical activity minutes at one or more sessions.
§Among all eligible participants who reported physical activity minutes at one or more sessions in months
1–6.
‖Among all eligible participants who reported physical activity minutes at one or more sessions in months
7–12.
¶Odds of achieving average weekly physical activity minutes of 150.
#Results are based on Pearson χ2 test for categorical variables and two-sample Student t test for continuous variables.
**Reference group for bivariate analysis.
Results of regression analysis indicate a positive relationship between the number of sessions attended and percent weight loss; for every additional session attended, participants lost 0.31% of body weight (P < 0.0001). Average reported physical activity minutes also had a positive relationship with percent weight loss, resulting in a loss of 0.3% (P < 0.0001) for every 30 additional weekly minutes of physical activity reported.
Adjusted percent weight loss was 3.7% among those aged 18–44 years, 4.0% among those 45–64, and 4.2% among those 65+ (P < 0.05 for each age-group comparison). Non-Hispanic white participants had higher adjusted percent weight loss (4.6%) when compared with all other race/ethnicity groups (P < 0.01), whereas non-Hispanic black participants had the lowest adjusted percent weight loss (3.2%) when compared with all other race/ethnicity groups (P < 0.0001). The difference between males (4.1%) and females (3.9%) was small but statistically significant (P < 0.05). All comparisons between BMI categories were significant, with participants in the highest BMI category (>30 kg/m2) having the highest adjusted percent weight loss of 4.5% compared with those with a BMI of 25–29 kg/m2 (4.1%) and those with BMI <25 kg/m2 (3.3%) (P < 0.01).
Conclusions
The 2002 DPP research study showed that a mean weight loss of 5–7% among high-risk adults contributes to a 58% reduction in progression to type 2 diabetes in those aged 18 years and over and a 71% reduction in those aged 60 years and over (8). Our findings show that although only a little over one-third were successful in reaching the 5% weight loss goal, many more were close to reaching it, resulting in a mean weight loss of 4.2%. Nearly half of the participants reporting physical activity achieved the physical activity goal of 150 min per week.
Perhaps more importantly, we found that those who remained in the program were successful. For every additional session attended, participants lost an average of 0.31% of their body weight. Among those with high duration (7–12 months) and intensity (17 or more sessions) of participation, median weight loss was 6% and every subgroup successfully achieved, or nearly achieved, the 5% weight loss goal. However, most participants are not participating fully during the maintenance portion of the program. Whereas nearly 87% attended at least 4 sessions, only 43% completed 16 sessions, compared with 95% in the original DPP trial (16), and nearly all of the sessions attended took place during the first 6 months. Further exploration into organizational metrics and interviews with participants may elucidate whether this attrition is a result of poor or waning infrastructure or whether participants are losing interest in the program or are unable to attend 12 months of programming. Regardless, these findings suggest that differences in success may be attributable to variable participation duration and intensity, and that disparities may be reduced and overall results improved by focusing on retention.
More than 35,000 people at high risk for type 2 diabetes participated in the National DPP during the program’s first 4 years, making it one of the largest nationwide community-based diabetes prevention lifestyle change programs. Eighty-seven percent of participants attended at least 4 sessions, and more than half attended at least 14 sessions; however, just 1 in 10 participants completed the full 22-session program. Therefore, although completion rates for the entire program are not high, nearly half (48.3%) did attend the program for at least 6 months, completing the training portion of the program.
Several other studies have examined behavioral interventions among adults at high risk for type 2 diabetes. The original DPP trial achieved 7.2% average weight loss at year 1 (17), higher than the 4.2% found in this current study. A meta-analysis of 28 U.S.-based studies found a mean weight loss of 3.99% (3). In addition, the meta-analysis showed that for each additional session attended in the first 24 weeks of the program, an additional weight loss of 0.26% was achieved, generally consistent with the 0.31% found in our study. The average age in the current study was the same as in the meta-analysis; however, the National DPP had a higher proportion of females (80.3% vs. 69.9%). The National DPP was also more racially and ethnically diverse, with only 44.9% non-Hispanic white compared with 70.9% in the meta-analysis, suggesting that the organizations participating in the National DPP serve more diverse populations. In Finland in 2003–2008, the National Program for the Prevention of Type 2 Diabetes (FIN-D2D) was implemented in five hospital districts (18). More than 10,000 people were identified as being at high risk for developing type 2 diabetes. Interventions focusing on weight, diet, physical activity, alcohol use, and smoking were held as individual or group sessions. At the end of a 1-year follow-up, 17.5% of participants had lost at least 5% of their body weight, substantially less than the 35.5% of National DPP participants.
In 2015, the Community Preventive Services Task Force published a review of 53 studies that described 66 diet and physical activity promotion programs for the prevention of type 2 diabetes (19). The median number of sessions offered by these programs was 16 versus the minimum 22 sessions required in the National DPP. The median average age across participants in the programs was 53.6 years, similar to our average age of 55.1 years. Of the 66 programs reviewed, 27 were based on the DPP or Diabetes Prevention Study (19). Average weight loss across the programs was 3.0%. Based on this level, the Task Force concluded that there was strong evidence of effectiveness for participation in combined diet and physical activity promotion programs, such as the National DPP, for people at increased risk of type 2 diabetes in reducing new-onset type 2 diabetes (19).
Our study is subject to limitations, some of which may overestimate program benefits. First, because the program is relatively new, our analyses were limited to fewer than half of the total National DPP participants, as the remaining participants had not yet had the opportunity to participate in the program for a year prior to our study. Second, organizations within the DPRP are responsible for collecting and reporting their own data. Lifestyle coaches are asked to use the same scale at each session for recording body weight to ensure consistency. Physical activity minutes are reported by the participants to their lifestyle coaches; information on how these data are being measured or recorded is not provided. Also, as in previous studies (16), analysis of weight loss was based on participants with at least two weight measurements. If those with only one weight measurement (5%) were assumed to have no weight loss, the mean weight loss drops from 4.2 to 4.0%. Finally, the ultimate goal of the National DPP is to prevent or delay onset of type 2 diabetes. Because we do not collect information on glycemic markers, progression to type 2 diabetes may take many years, and the National DPP is relatively young, we are not yet able to directly evaluate this end-level outcome. However, evidence from the DPP trial strongly supports the benefits of weight loss and physical activity resulting from the lifestyle change program used in the National DPP.
Since its inception in 2012, the National DPP has seen promising results among its participants. Organizations from 46 states and the District of Columbia are offering classes to tens of thousands of adults in a variety of venues that include community health centers, hospitals, local health departments, and universities. New organizations are continuously joining the program, and the Department of Health and Human Services has pronounced that Medicare expansion of the National DPP would be a “significant step forward in building a health care system that works better, spends dollars smarter, and keeps people healthy” (20). Since February 2015, the intervention is also being delivered virtually in order to reach those who do not have access to brick-and-mortar programs or do not wish to participate in an in-person group format. As data from these virtual programs and the growing number of in-person programs become available, they will offer a rich opportunity for ongoing program evaluation and improvement. Additionally, efforts are underway to better understand outcomes. The National DPP is examining the causes for participant attrition as well as other key variables in a subset of >100 sites, in an effort to glean lessons learned and to document successful program implementation strategies. Enrollment drivers, participant engagement activities, and retention and maintenance strategies are being studied. There are an increasing number of insurance companies that are providing coverage for the National DPP. Over 70 commercial health plans provide some coverage, three million state employees are covered through their state employee health plans, several state plans cover Medicaid participants in certain networks, and CMS plans to begin national coverage in January 2018.
In summary, these results show encouraging success in the implementation of community-based lifestyle change programs to prevent type 2 diabetes across a large number of delivery organizations nationwide. Attainment of program goals appears to hinge on intensity and duration of participation. Challenges remain in identifying, engaging, and retaining those at risk, and further expansion, investigation, and refinement of the program are needed to continue to lower the burden of type 2 diabetes nationally.
Article Information
Acknowledgments. The authors thank the members of the National DPP team who contributed to the validation and aggregation of the data used in this study. In addition, the authors acknowledge the contributions of the CDC-recognized organizations that collected and submitted the data used in this study.
Funding. The National DPP is funded by the CDC. M.K.A. was partially supported by the Georgia Center for Diabetes Translation Research (P30-DK-111024) funded by the National Institute of Diabetes and Digestive and Kidney Diseases.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. E.K.E. contributed to the study concept and design, conducted the statistical analysis, contributed to the interpretation of data, drafted the manuscript, contributed to the discussion, and reviewed and edited the manuscript and approved the final version. S.M.G., E.W.G., M.K.A., D.B.R., and A.L.A. contributed to the study concept and design, contributed to the interpretation of data, drafted the manuscript, contributed to the discussion, and reviewed and edited the manuscript and approved the final version. E.T.L. contributed to the interpretation of data, drafted the manuscript, contributed to the discussion, and reviewed and edited the manuscript and approved the final version. K.N. conducted the statistical analysis, contributed to the interpretation of data, drafted the manuscript, contributed to the discussion, and reviewed and edited the manuscript and approved the final version. E.K.E. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
This article is featured in a podcast available at http://www.diabetesjournals.org/content/diabetes-core-update-podcasts.
References
- 1.Centers for Disease Control and Prevention Diabetes Report Card 2014. Atlanta, GA, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, 2015 [Google Scholar]
- 2.American Diabetes Association Standards of Medical Care in Diabetes—2016. Diabetes Care 2016;39(Suppl. 1):S1–S106 [DOI] [PubMed] [Google Scholar]
- 3.Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health Aff (Millwood) 2012;31:67–75 [DOI] [PubMed] [Google Scholar]
- 4.Albright AL, Gregg EW. Preventing type 2 diabetes in communities across the U.S.: the National Diabetes Prevention Program. Am J Prev Med 2013;44(Suppl. 4):S346–S351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pronk NP, Remington PL; Community Preventive Services Task Force . Combined diet and physical activity promotion programs for prevention of diabetes: Community Preventive Services Task Force recommendation statement. Ann Intern Med 2015;163:465–468 [DOI] [PubMed] [Google Scholar]
- 6.Li R, Qu S, Zhang P, et al. Economic evaluation of combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the community preventive services task force. Ann Intern Med 2015;163:452–460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crandall JP, Knowler WC, Kahn SE, et al.; Diabetes Prevention Program Research Group . The prevention of type 2 diabetes. Nat Clin Pract Endocrinol Metab 2008;4:382–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Knowler WC, Barrett-Connor E, Fowler SE, et al.; Diabetes Prevention Program Research Group . Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoerger TJ, Hicks KA, Sorensen SW, et al. Cost-effectiveness of screening for pre-diabetes among overweight and obese U.S. adults. Diabetes Care 2007;30:2874–2879 [DOI] [PubMed] [Google Scholar]
- 10.Lindström J, Ilanne-Parikka P, Peltonen M, et al.; Finnish Diabetes Prevention Study Group . Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet 2006;368:1673–1679 [DOI] [PubMed] [Google Scholar]
- 11.Tuomilehto J, Lindström J, Eriksson JG, et al.; Finnish Diabetes Prevention Study Group . Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001;344:1343–1350 [DOI] [PubMed] [Google Scholar]
- 12.Zhuo X, Zhang P, Gregg EW, et al. A nationwide community-based lifestyle program could delay or prevent type 2 diabetes cases and save $5.7 billion in 25 years. Health Aff (Millwood) 2012;31:50–60 [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Centers for Disease Control and Prevention Diabetes Prevention Recognition Program standards and operating procedures [Internet], 2015. Available from http://www.cdc.gov/diabetes/prevention/pdf/dprp-standards.pdf. Accessed 1 March 2016
- 14.Centers for Medicare and Medicaid Services. Medicare Diabetes Prevention Program expansion. Available from https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2016-Fact-sheets-items/2016-07-07.html. Accessed 21 July 2016
- 15.Sigal RJ, Kenny GP, Wasserman DH, Castaneda-Sceppa C. Physical activity/exercise and type 2 diabetes. Diabetes Care 2004;27:2518–2539 [DOI] [PubMed] [Google Scholar]
- 16.Wing RR, Hamman RF, Bray GA, et al.; Diabetes Prevention Program Research Group . Achieving weight and activity goals among Diabetes Prevention Program lifestyle participants. Obes Res 2004;12:1426–1434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hamman RF, Wing RR, Edelstein SL, et al. ; Diabetes Prevention Program Research Group. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care 2006;29:2102–2107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saaristo T, Moilanen L, Korpi-Hyövälti E, et al. Lifestyle intervention for prevention of type 2 diabetes in primary health care: one-year follow-up of the Finnish National Diabetes Prevention Program (FIN-D2D). Diabetes Care 2010;33:2146–2151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Balk EM, Earley A, Raman G, Avendano EA, Pittas AG, Remington PL. Combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the Community Preventive Services Task Force. Ann Intern Med 2015;163:437–451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.U.S. Department of Health & Human Services. Independent experts confirm that diabetes prevention model supported by the Affordable Care Act saves money and improves health. Available from http://www.hhs.gov/about/news/2016/03/23/independent-experts-confirm-diabetes-prevention-model-supported-affordable-care-act-saves-money.html. Accessed 21 July 2016