Abstract
Tension pneumomediastinum is a rare and life-threatening complication of mediastinal emphysema which can occur with mechanical ventilation. We present a case of tension mediastinum associated with mechanical ventilation in a patient with Acute Respiratory Distress Syndrome due to Pneumocystis jirovecii pneumonia. We discuss the mechanism and pathophysiology of tension pneumomediastinum, the potential association with Pneumocystis jirovecii pneumonia and recruitment manouvres, and its definitive emergency treatment.
Keywords: Pneumomediastinum, Pneumocystic jirovecii pneumonia, recruitment manoeuvres, pneumatocele
Case description
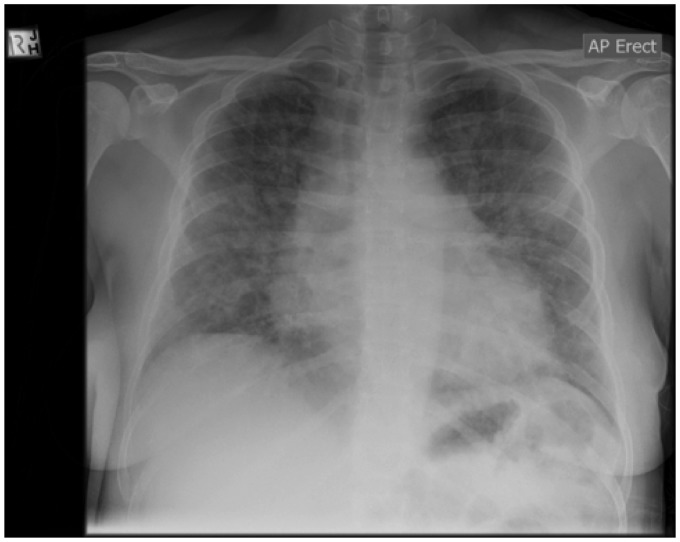
A 38 year-old female presented to the Emergency Department with respiratory distress, coryzal symptoms and a non-productive cough. She had a history of a previous renal transplant subsequent to bilateral nephrectomy for polycystic kidney disease. She was compliant with her immunosuppressive regimen, and was not receiving prophylactic trimethoprim/sulphamethoxazole. She was admitted to the Intensive Care Unit (ICU) due to severe hypoxaemia and worsening respiratory distress, requiring high levels of oxygen therapy delivered by high-flow nasal cannulae. Her initial chest X-ray demonstrated four quadrant opacification (Figure 1). She was treated presumptively with trimethoprim/sulphamethoxazole and intravenous hydrocortisone due to a high suspicion of PJP, along with ceftriaxone and azithromycin. The diagnosis of PJP was confirmed by polymerase chain reaction (PCR) from a sputum specimen. Her treatment was changed from trimethoprim/sulphamethoxazole to primaquine because of worsening renal function, then back to a renally adjusted dose of trimethoprim/sulphamethoxazole because of primaquine-induced methaemoglobinaemia.
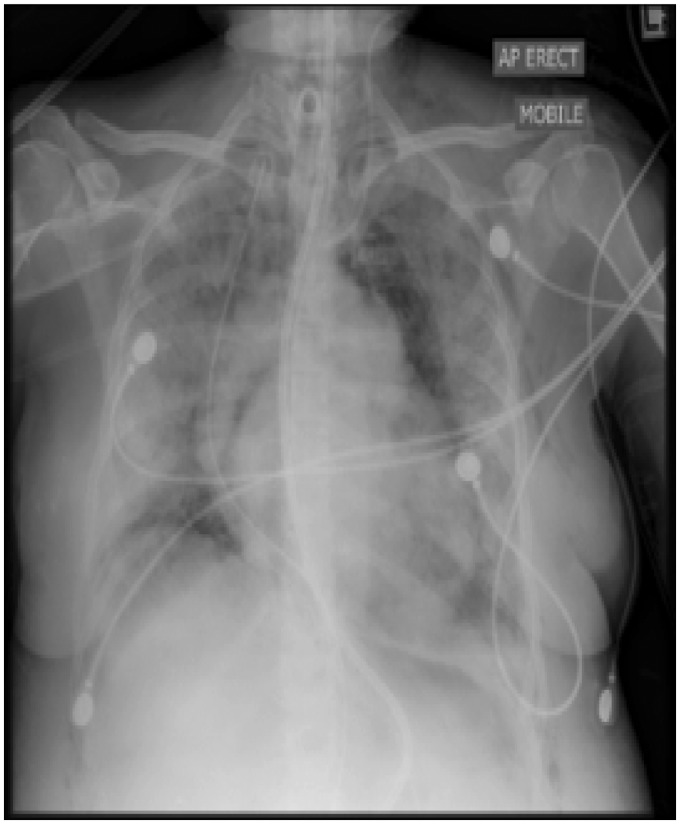
Figure 1.
Initial CXR showing bilateral patchy shadowing associated with peribronchial thickening.
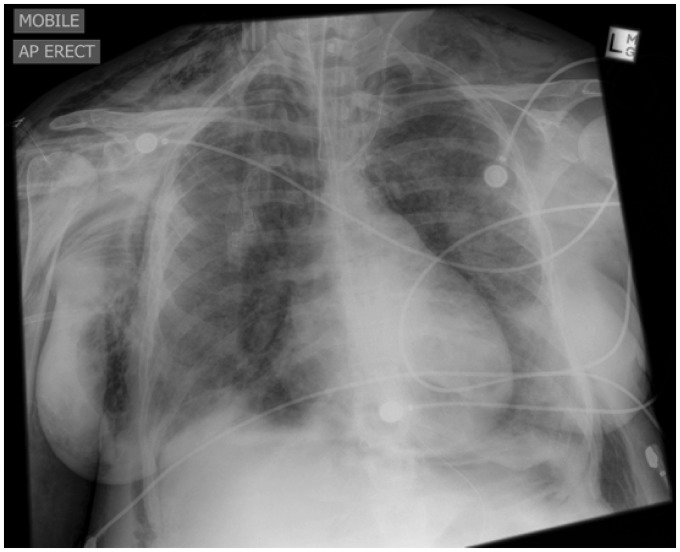
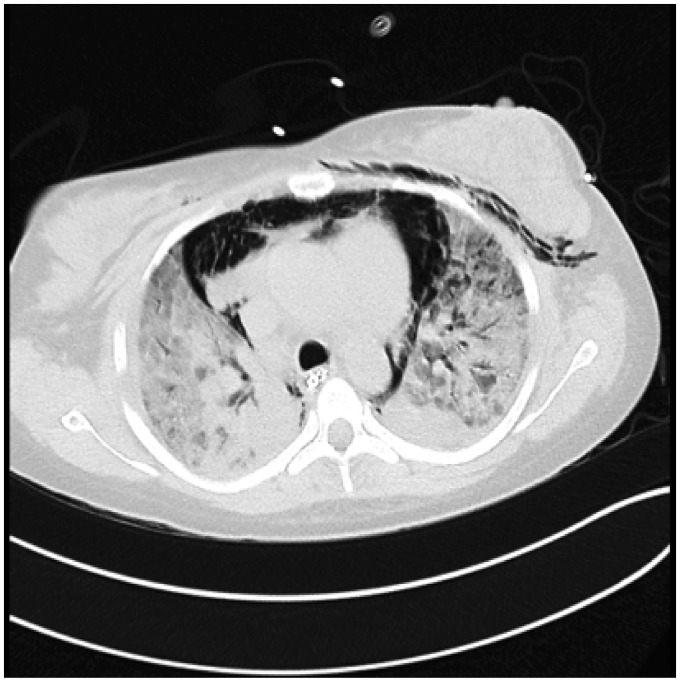
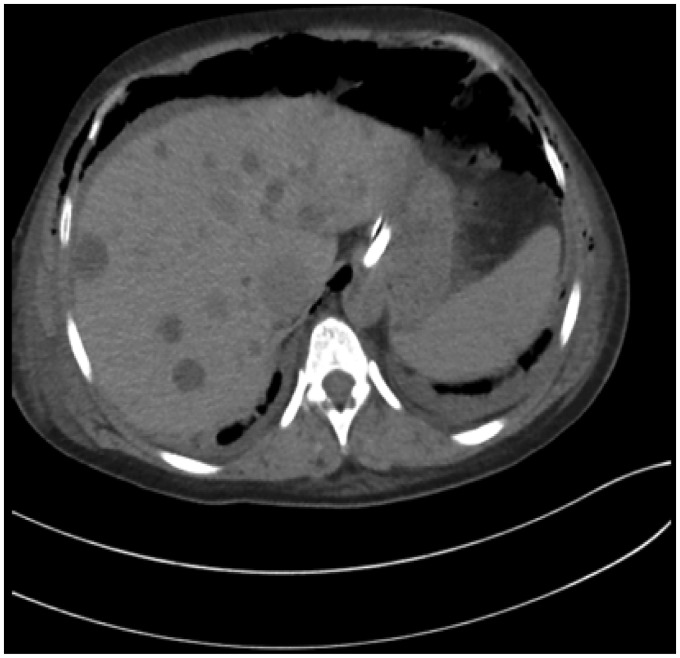
She was intubated on day 3 of her admission due to worsening hypoxic respiratory failure and fatigue, and required rescue therapy with high frequency oscillation ventilation (HFOV) from day 9. On day 15 whilst still receiving HFOV her hypoxaemia improved, allowing a return to conventional ventilation. At this stage, her pulmonary compliance was poor with tidal volume of only 200 ml at a plateau pressure of 35 cm H2O. On day 16, a pulmonary recruitment manouvre was performed due to recurrent hypoxaemia, which led to the development of widespread subcutaneous emphysema and an increase in her pulse-pressure variation as monitored by the arterial line. Subsequently, she developed hypotension and chest X-ray confirmed extensive pneumomediastium with a right pneumothorax (Figure 2). Given the worsening haemodynamics, a clinical diagnosis of tension pneumothorax was made. Needle decompression and the insertion of an intercostal catheter in the right pleural space did not improve the hypotension, and therefore a CT chest was done to further differentiate the air collections. Based on the CT (Figures 3 to 5) and the failure pleural decompression to resolve the hypotension, a diagnosis of tension pneumomedistinum was made. A subxiphoid mediastinal drain was placed by a thoracic surgeon (Figure 6), with resolution of the hypotension and pneumomediastinum. Although her progress was slow, she was ultimately liberated from the ventilator and was later discharged home, and returned to her previous level of independent function.
Figure 2.
Extensive pneumomediastinum and subcutaneous emphysema. There is a deep sulcus sign on right side consistent with a pneumothorax.
Figure 3.
Coronal section on CT—large pneumomediastinum, with significantly consolidated tissue bilaterally.
Figure 4.
Transverse CT section—pneumomediastinum causing cardiac compression and compression of large vessels.
Figure 5.
Transverse CT section showing air through peritoneal space. There are also hepatic cysts in a patient with background of polycystic kidney disease.
Figure 6.
CXR post mediastinal drain insertion with improvement of hypotension and resolution of the pneumomediastinum.
Within the next two months, we encountered a second case of tension pneumediastinum, also in a patient with ARDS due to Pneumocystis jirovecii pneumonia (PJP). However, we were unable to gain consent to allow publication in this manuscript.
Discussion
Tension pneumomediastinum is a rare but life threatening event in the critically ill. It was first described by a French physician Laennecc1 in 1827. Trapping of air in the mediastinum with a resulting increase in pressure causes compression of the great vessels, and leads to decreased venous return and cardiovascular compromise. Pneumomediastinum is historically associated with pulmonary tissue necrosis in tuberculosis; however, more recently it has been associated with barotrauma in patients with severe asthma requiring intubation and positive pressure ventilation. It can also occur from tracheobronchial injury due to either penetrating or blunt trauma, including percutaneous dilatational tracheostomy insertion.
The theory of the pathophysiological mechanism was first described by Macklin and Macklin2 in 1944. Leakage of air from the alveolus occurs due to a pressure gradient between the alveolus and the perivascular sheaths (i.e. from overinflation). If the pressure gradient is maintained, the air tracks along the vascular sheaths to the mediastinum, and may also track peripherally to the sub-pleural space. From the mediastinum, the air can escape to the pleural spaces, the head and trunk (manifested as subcutaneous emphysema), or to the retroperitoneal space which practically acts as a release valve. However, if the pressure in the mediastinum continues to rise, physiological effects similar to pericardial tamponade occur, causing compression of the great vessels and compromising right heart filling, leading to hypotension and ultimately cardiac arrest. The early signs can manifest clinically as pulses paradoxus and electrical alternans. It is more usual for air to collect in the anterior mediastinum; however, a posterior pneumomediastinum (retro-pneumomediastinum3) can rarely occur. This retro-pneumomediastinum3 can be difficult to diagnose on routine AP X-ray films; however, one potential radiological clue is the earth-heart sign, where the cardiac silhouette resembles the shape of an oblate sphere. This is due to an increase in the transverse cardiac diameter, and decrease in the vertical cardiac diameter, due to collapse and restricted filling of the cardiac chambers.4
Interstitial lung diseases and infections such as Tuberculosis and pertussis may make the patient susceptible to barotrauma from pressure gradients across the alveolus and perivascular sheath. PJP is an opportunistic infection that may result in such damage to the alveolar tissue and create large subpleural cysts. PJP requiring positive pressure ventilation is associated with pneumothoraces in 5–10% of cases,5 so the potential to cause pneumomediastinum is well described. However, these figures were from a study that assessed patients with HIV-associated PJP and only 13.4% of the study cohort received positive pressure ventilation. Therefore, it would be intuitive to suspect that the incidence would be higher in mechanically ventilated patients, and the study demonstrated this with over 50% of the patients who received mechanical ventilation developing a pneumothorax.
There are many documented contraindications to pulmonary recruitment manouvres such as shock; barotrauma with the presence of pneumothoraces, pneumomediastinum, pneumatoceles, or subcutaneous air; unilateral or focal lung disease; necrotizing lung disease; and presence of bullous lung disease, although clinicians may argue that in some of these contexts, it is a question of clinical prioritirization as to whether a recruitment manouvre is deployed. However, during our literature search, we could not find a protocol or manuscript that contraindicated a recruitment manouvre on the basis of PJP as the underlying pathology. As we discussed earlier, the risk of developing complications with mechanical ventilation is significant, and this is because the incidence of the development of pneumatoceles associated with PJP may be as high as 37%.6
The current ANZICS CTG PHAR-LAP trial (NCT01667146 – clinical trials.gov) is investigating the use of an open lung strategy with staircase recruitment, titrated PEEP and targeted low airway pressures in patients with ARDS. In the trial description, there is a discussion of which patients are contraindicated to enrollment, and this does include the presence of pneumatoceles. However, this diagnosis is usually made on CT imaging of the chest, and many patients with severe ARDS would be deemed unsuitable for transfer, and since it would be unliklely that the imaging would change current management, the actual presence of pneumatoceles is unlikely to be known.
There was only one other case of tension pneumomediastinum associated with PJP found during our review of the literature, and this was neither associated with mechanical ventilation, nor a recruitment manouvre.7 Given this known susceptibility in PJP, the decision to use a recruitment maneuver in this clinical context should still not be undertaken lightly. Whilst it is not disputed that pulmonary recruitment procedures have their place in the Intensivist’s armamatarium, ARDS is not a homogeneous process. In the case of PJP-associated ARDS, it may be appropriate to consider the use of a pulmonary recruitment manouvres only when other options are exhausted.
The initial management of tension pneumomediastinum includes reduction of airway pressures in order to reduce the potential for a pressure gradient; and allowing permissive hypercapnoea and 100% oxygen to denitrogenate the mediastinal space. Mediastinal decompression can be performed via various techniques, and is indicated in cases where there is cardiorespiratory embarrassment. Shenib and Barkun suggest an incision in the suprasternal notch with blunt finger-dissection.1,8 This is also common route of entry used for mediastinoscopy. Kiefer et al.9 describe the Gills technique in a patient with cardiac arrest secondary to tension pneumomediastinum resulting in ROSC and successful decompression. This technique comprises of bilateral supraclavicular incisions through the fascia. Both of these measures may be considered in patients in extremis from tension pneumomediastinum. A further method utilizes the oesophageal hiatus to access the mediastinum via a mini-laparotomy.10 In our patient, a subxiphoid approach was used, based largely on the clinical experience of the thoracic surgeon. The incision was made lateral to the xiphersternum with blunt dissection through the diaphragm. The drain was directed anteriorly. Note that the compression of significant vascular structures retrosternally reduces the risk of injury, which is also the case if the approach to decompression was via an anterior mediastinotomy using the left parasternal second intercostal space. The authors also note that chest drains can also be placed using the seldinger technique. This can be aided with ultrasound or fluoroscopy as been previously reported in the neonatal population.11 However, subcutaneous air may create significant artifact with ultrasound, making CT suitable to guide the insertion of a percutaneous drainage. Failure to resolve the tension with the above measures may warrant a sternotomy.
Conclusion
Pneumomediastinum can occur as a result of an excessive pressure gradient between the alveolus and perivascular sheaths. Patients may be susceptible to these pressure gradients due to damage of the pulmonary tissue from infections such as Pneumocystis jirovecii. PJP as a causative agent for ARDS predisposes patients to an increased risk of barotrauma and therefore pneumomediastinum, and the use of a pulmonary recruitment manouvres should not be undertaken lightly. Whilst pneumomediastinum generally has a benign course, if the pressure continues to rise it can cause tension pneumomediastinum, with subsequent cardiovascular instability from mechanism similar to classic cardiac tamponade. If this occurs, immediate decompression is required and the technique used will vary depending on the expertise available.
Consent
Published with the written consent of the patient.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.McNicholl B. Pneumomediastinum and subcutaneous emphysema in status asthmaticus requiring surgical decompression. Arch Dis Child 1967; 114: 42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Macklin M, Macklin C. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: interpretation of the clinical literature in the light of laboratory experiment. Medicine 1944; 23: 281–358. [Google Scholar]
- 3.Kyle A, Veldtman G, Stanton M. Barotrauma-associated posterior tension pneumomediastinum, a rare cause of cardiac tamponade in a ventilated neonate: a case report and review of the literature. Acta Paediatric 2012; 101: e142–e144. [DOI] [PubMed] [Google Scholar]
- 4.Obesa Carillo GA. Tension pneumomedistinum: the earth-heart sign. Radiopedia.org, http://radiopaedia.org/cases/tension-pneumomediastinum-earth-heart-sign Radhi S and Alexander T. Outcome of HIV-associated Pneumocystis pneumonia in hospitalized patients from 2000 to 2003. BMC Infect Dis 2008; 8: 119. [DOI] [PMC free article] [PubMed]
- 5.Chow C, Templeton PA, White CS. Lung cysts associated with Pneumocystis carinii pneumonia: radiographic characteristics, natural history, and complications. Am J Roentgenol 1993; 161: 527–531. [DOI] [PubMed] [Google Scholar]
- 6.Carillo G, Caballero G. The Earth-Heart sign: a new diagnostic finding in a patient with tension pneumomediastinum. Lancet 2014; 383: 486. [DOI] [PubMed] [Google Scholar]
- 7.Shennib H, Barkun A. Surgical decompression of a tension pneumomediastinum. Chest 1988; 93: 1301–1302. [DOI] [PubMed] [Google Scholar]
- 8.Kiefer M, Feeney C. Management of subcutaneous emphysema with “gills”: case report and review of the literature. J Emerg Med 2013; 45: 666–669. [DOI] [PubMed] [Google Scholar]
- 9.Paluszkiewicz P, Bartosinski J. Cardiac Arrest caused by tension pneumomediastinum in a Boerhaave syndrome patient. Ann Thoracic Surg 2009; 87: 1257–1258. [DOI] [PubMed] [Google Scholar]
- 10.Mohamed IS, Lee YH. Ultrasound guided percutaneous relief of tension pneumomediastinum in a 1-day-old newborn. Chinese J Contemporary Paediatr 2008; 10: 675–676. [Google Scholar]
- 11.Dondeliner RF, Coulon M, Kurdziel JC. Tension Mediastinal emphysema: emergency percutaneous drainage with CT guidance. Eur J Radiol 1992; 15: 7–10. [DOI] [PubMed] [Google Scholar]