Sepsis can be associated with either hyperthermia or hypothermia, and various pharmacological and non-pharmacological methods are available in Intensive Care Units (ICUs) to manage extremes of temperature. Consensus is lacking regarding the optimal target temperatures of patients with sepsis. Observational data from national databases suggest a rise in mortality in patients with temperatures above 40°C and below 36.5°C1; mild hyperthermia may confer some benefit compared with normothermia.1,2
We recently distributed an online survey, via www.surveymonkey.com to UK intensive care consultants via the Critical Care Networks to explore current practice in temperature regulation in sepsis. We asked questions on individuals’ preferred methods of cooling and warming, their threshold temperatures for intervening and their degree of concern for a particular temperature. We received 45 responses from consultants working in a mix of general (43), Neuro (1) and burns ICUs (1). The majority work in medium sized (11–20 beds) units.
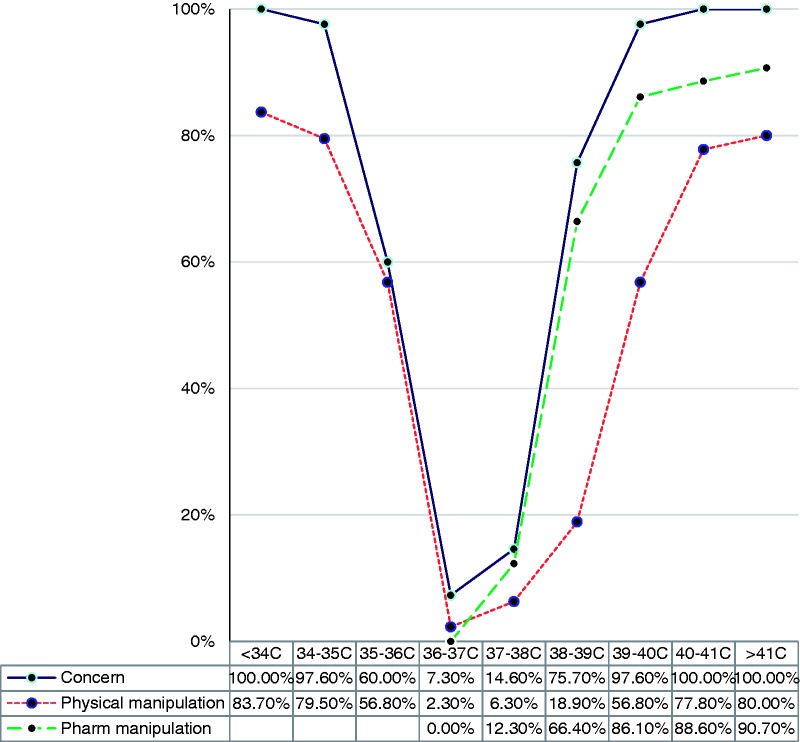
Figure 1.
Degree of concern and physical or pharmacological manipulations undertaken.
The results are shown in the graph below; 37°C caused the lowest level of concern, with concern rising rapidly with higher and lower temperatures. Mild pyrexia may be expected in sepsis; mortality is lower in patients with a temperature on admission to ICU of 38°C–39°C than 37°C,1 yet 75% of respondents would be concerned at this temperature, and greater than two-thirds of respondents would cool such a patient.
Eighty percent of consultants used physical cooling methods and 83% used physical means to warm a hypothermic septic patient; the threshold for starting temperature manipulation varied widely between less than 34°C and 37°C, and between 37°C and more than 41°C. Those not using physical cooling cited insufficient evidence base or lack of departmental guidelines.
Ninety percent of consultants reported using pharmacological agents (paracetamol or non-steroidal anti-inflammatory drugs) to cool the patient. The threshold for starting an antipyretic varied between 38°C and more than 41°C. Of colleagues who don’t use an antipyretic, the most commonly cited reason not to do so was insufficient evidence. A recent metanalysis has shown no mortality benefit from antipyretics3; other studies suggest a trend towards harm.4
Mortality appears to increase rapidly with hypothermia; patients with a temperature of 36°–36.4°C during the first 24 h in ICU have a 1.37 increase in mortality compared with 36.5°C–36.9°C, and a greater than three-fold increase in mortality below 36°C.1 However, very few respondents would be concerned at 36°C, and less than two-thirds would be concerned at 35°C.There still remains much uncertainty about the optimum temperature in sepsis, and the benefit or otherwise of manipulating the temperature. This is reflected in the wide variation in practice around the country. This survey suggests that we remain over-concerned at mild degrees of hyperthermia, but under-concerned with hypothermia. We look forward to further studies and further guidance soon.
References
- 1.Young PJ, Saxena M. Fever management in intensive care patients with infections. Critical Care 2014; 18: 206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Young PJ, Saxena M, Beasley R, et al. Early peak temperature and mortality in critically ill patients with or without infection. Intensive Care Med 2012; 38: 437–444. [DOI] [PubMed] [Google Scholar]
- 3.Lee BH, Inui D, Suh GY, et al. Association of body temperature and antipyretic treatments with mortality of critically ill patients with and without sepsis: multi-centred prospective observational study. Critical Care 2012; 16: R33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Niven DJ, Stelfox HT, Laupland KB. Antipyretic therapy in febrile critically ill adults: A systematic review and meta-analysis. J Crit Care 2013; 28: 303–310. [DOI] [PubMed] [Google Scholar]