Abstract
Introduction
Survivors of critical illness face many potential long-term sequelae. Prior studies showed that early rehabilitation in the intensive care unit (ICU) reduces physical impairment and decreases ICU and hospital length of stay (LOS). However, these studies are based on a single ICU or were conducted with a small subset of all ICU patients.
We examined the effect of an early rehabilitation program concurrently implemented in multiple ICUs on ICU and hospital LOS.
Methods
An early rehabilitation program was systematically implemented in five ICUs at the sites of two affiliated academic institutions. We retrospectively compared ICU and hospital LOS in the year before (1/2011–12/2011) and after (1/2012–12/2012) implementation.
Results
In the pre- and post-implementation periods, respectively, there were a total of 3945 and 4200 ICU admissions among the five ICUs. After implementation, there was a significant increase in the proportion of patients who received more rehabilitation treatments during their ICU stay (p < 0.001). The mean number of rehabilitation treatments per ICU patient-day increased from 0.16 to 0.72 (p < 0.001). In the post-implementation period, four of the five ICUs had a statistically significant decrease in mean ICU LOS among all patients. The overall decrease in mean ICU LOS across all five ICUs was 0.4 days (6.9%) (5.8 versus 5.4 days, p < 0.001). Across all five ICUs, there were 255 (6.5%) more admissions in the post-implementation period. The mean hospital LOS for patients from the five ICUs also decreased by 5.4% (14.7 vs. 13.9 days, p < 0.001).
Conclusions
A multi-ICU, coordinated implementation of an early rehabilitation program markedly increased rehabilitation treatments in the ICU and was associated with reduced ICU and hospital LOS as well as increased ICU admissions.
Keywords: Intensive care, rehabilitation, early ambulation, physical therapy, occupational therapy, length of stay
Introduction
Survivors of critical illness face many potential long-term sequelae, including neuromuscular dysfunction and cognitive impairment.1–6 Sedation, delirium and bed rest are considered important contributors to these complications.3,6–8 Early rehabilitation in the intensive care unit (ICU) focuses on minimizing sedation and providing early physical and occupational therapy (PT/OT) starting promptly after stabilization of major physiological derangements.9,10 In the USA, this approach sharply contrasts with a more traditional model of starting rehabilitation only after liberation from mechanical ventilation or after ICU discharge.11–15
Prior studies provide evidence for the benefits of early rehabilitation in ICUs, including reduced physical impairment and decreased ICU and hospital length of stay (LOS).10–13,16–24 However, these studies have often focused on a single medical ICU or were conducted with a relatively small subset of all ICU patients. Based on the encouraging results from these prior studies, an early rehabilitation program was implemented across five ICUs, encompassing medical, surgical and cardiac ICUs, at the sites of our two affiliated academic institutions. Our aim was to examine the effect of the coordinated implementation of this early rehabilitation program on our ICU and hospital LOS in this before/after quality improvement project. Some of the results of this study have been previously reported in the form of an abstract.25
Methods
Setting
An early rehabilitation program was simultaneously implemented beginning January 2012 in five ICUs (three medical, one cardiac, one surgical) across two affiliated academic institutions at two separate geographic sites in New York City: the New York-Presbyterian Hospital/Columbia University College of Physicians and Surgeons and the New York-Presbyterian Hospital/Weill Cornell Medical College. Both these sites are urban tertiary/quaternary referral academic medical centers that serve both the nearby local communities and referrals from the state of New York and the neighboring states.
Study design
To assess the effect of our early rehabilitation program, a retrospective analysis was performed on 8145 consecutive admissions to the five study ICUs comparing the 12-month period before versus after implementation of the early rehabilitation program (January 2011 to December 2011 versus January 2012 to December 2012). All admissions to the study ICUs were included. During this two-year study period, early rehabilitation was the only intervention implemented to reduce ICU LOS across the five ICUs. This retrospective study was approved by the Columbia University Institutional Review Board (IRB-AAAK7951). Waiver of consent was approved in accordance with our institutional review board guidelines.
The ICU early rehabilitation program
The ICU early rehabilitation program consisted of a multidisciplinary team of ICU clinicians (physicians, nurses, physician assistants and acute care nurse practitioners), physical therapists (PTs), occupational therapists (OTs), respiratory therapists and speech-language pathologists. The ICU clinicians together with the PTs and OTs evaluated all patients daily, from Monday to Saturday, for their suitability for participating in rehabilitation therapy. Guidelines for rehabilitation (Table 1), including contraindications and the range of activities undertaken, were adapted from the existing literature.16,19 Therapy could be deferred at the discretion of the treatment team based on their clinical judgment. On Sundays, therapy was performed on an ad hoc basis by the ICU clinicians.
Table 1.
Guidelines for ICU rehabilitation.
| Contraindications | Possible Rehabilitation Activities |
|
|---|---|---|
| Physical therapy | Occupational therapy | |
| Ongoing coronary ischemia Unstable arrhythmia Cardiac tamponade | Passive range of Motion | Feeding Grooming Dressing |
| Respiratory distress | ||
| Hypoxemia at rest (SpO2 <88%) | Exercises in bed | |
| Respiratory rate < 5 or > 40 per minute | Transfers | |
| Heart rate < 40 or > 130 beats per minute | (supine to sitting, | |
| Mean arterial pressure < 55 mmHg | sitting to standing, | |
| Systolic blood pressure > 200 mmHg | bed to chair) | |
| Unsecure airway | Ambulating in place | |
| Hypoglycemia (blood glucose < 50 mg/dL) | Ambulation | |
| Orthopedic contraindication | ||
| Unstable spinal cord injury | ||
| Intracranial hypertension | ||
| Morbid obesity (if unable to be managed safely) | ||
| Care focused on comfort measures only | ||
ICU: Intensive care unit.
The rehabilitation therapists determined the activities (possible activities listed in Table 1) for each therapy session. Physical therapy interventions included passive range of motion, transfers (including supine to sitting, sitting to standing, and bed to chair), ambulating in place and ambulation. Occupational therapy interventions included training with feeding, grooming, and dressing. Throughout all rehabilitation sessions, hemodynamic (heart rate, blood pressure) and respiratory statuses (respiratory rate and oxygen saturation) were closely monitored. Rehabilitation sessions involved one or more therapist, as well as a rehabilitation therapy assistant if extra assistance was required. For the mobilization of mechanically ventilated patients, a respiratory therapist was available upon request to transition the patient to a portable ventilator or to a bag-valve device for manually assisted ventilation. For patients on advanced circulatory support such as an extracorporeal membrane oxygenation device, additional staff members were available for assistance in mobility. The patient’s nurse and a nurse practitioner or a physician were also present in the ICU and aware of the therapy session in progress.
Prior to the implementation of the ICU early rehabilitation program, if any referral for physical and occupational therapy was made, it was typically done within one day of a patient being medically appropriate for transfer out of the ICU to a regular hospital ward. Physical therapy referral was rarely requested when a patient was endotracheally intubated.
Planning and education for implementation of the ICU early rehabilitation program took place from August 2011 to December 2011. There may have been heightened awareness of the benefits of early rehabilitation in the ICU during this educational period; however, there were no rehabilitation therapists dedicated to ICU patients. Implementation of the ICU early rehabilitation program in January 2012 involved 10 PTs and 4 OTs who focused their primary role on patients in the five participating ICUs (with a total of 80 beds). All PTs and OTs had prior experience of working with patients in the ICU, but not specifically in the context of an early ICU rehabilitation program. The PTs and OTs had an average of 6 years and 2.5 years of work experience in an acute care hospital, respectively. An additional five rehabilitation therapy assistants were hired specifically for the program. Depending on the number of patients in each ICU that were eligible for rehabilitation activities that day as determined on the morning meeting between the ICU clinicians and PTs and OTs, the ICU rehabilitation therapists were flexible to divide their time amongst the five ICUs. There were no fixed staffing ratios for number of rehabilitation therapists per ICU for each day.
As part of the ICU early rehabilitation program, there was no pre-specified sedation protocol mandated across the five ICUs. Individual ICUs were allowed to implement sedation minimization protocols. Only the Medical ICU at the Columbia campus implemented such a protocol. Otherwise, sedation practices in the pre- and post-implementation periods were at the discretion of the treating clinicians.
During the year of implementation in January to December 2012, while there were weekly multi-disciplinary staff meetings to discuss implementation progress, including monthly surveillance of rehabilitation treatments per ICU patient-day, there were no additional quality assessments to ensure that the ICU early rehabilitation program was implemented uniformly in all the study ICUs.
Data collection
All study data were obtained from a hospital-wide administrative database for all admissions to the five ICUs during the two-year period. Data included patient age, sex, and primary diagnosis (classified into medical or surgical diagnoses, with subcategories for the medical admissions). The proportion of patients on mechanical ventilation was not available. Primary outcomes were ICU and hospital LOS, with each midnight representing a one-day stay. Secondary outcomes included the number of PT and OT treatments performed in the ICU, hospital mortality and hospital discharge destination.
When available, patients’ baseline mobility and activity status prior to hospital admission were obtained from the electronic medical record. Baseline mobility and activity status was based on nursing intake documentation and presented as mobility and activity status scores. These scores each ranged from 0 to 3, with one point assigned if the patient was independent (i.e. not requiring assistance or assistive device) with each of three mobility tasks (bed mobility, bed-to-chair transfer, and ambulation) and activity tasks (dressing or grooming, feeding, and toileting or bathing). For example, a mobility score of 3 means the most independently mobile, while a score of 0 means minimally mobile (unable to even move in bed without assistance). Similarly, an activity score of 3 means the most independent in the activity tasks listed above, while a score of 0 means inability to perform any of the tasks listed above without assistance. Also if available, patients’ ambulation status in the ICU was obtained by tabulating cases where the physical therapist had checked the “patient ambulated” checkbox in their documentation.
Statistical analysis
We summarized data using standard descriptive statistics with unpaired t-tests used to compare continuous variables and Chi-squared tests to compare categorical variables. LOS data were expressed as mean with standard deviation (SD), as well as by percentiles. Due to its positively skewed distribution (skewness of 5.0 and 5.2 for ICU LOS, and 4.3 and 3.2 for hospital LOS in the pre- and post-implementation periods, respectively), p-values for the differences in LOS between the pre- versus post-implementation periods were calculated using Poisson’s regression, as done in previous ICU LOS analyses.26–28 The differences in the distribution of LOS data were also analyzed with the Mann–Whitney–Wilcoxon rank sum test. For all analyses, a two-sided p-value of less than 0.05 was considered statistically significant. In the small number of patient hospitalizations who had more than one ICU admission, we analyzed data from only their first ICU admission. Analyses were performed with Stata version 9.0 (College Station, TX, USA).
Results
Patient characteristics
In the pre- and post-implementation periods, respectively, there were a total of 3945 and 4200 ICU admissions among the five ICUs (with 89 and 96 hospitalizations having more than one ICU admission, respectively). Both pre- and post-implementation groups were remarkably similar in baseline characteristics (Table 2), with a mean (standard deviation (SD)) age of 63 (17) years, and 55% male, and 80% medical admissions. The subcategories of primary diagnosis for medical admissions were also similar between both groups. In the subset of patients with baseline mobility and activity data (approximately 33% and 46% of patients, respectively), scores were similar between the pre- and post-groups, with approximately 58% of ICU admissions in which the patient was fully independent for both activity and mobility and approximately 24% in which the patient was fully dependent (Table 3).
Table 2.
Baseline patient characteristics.
| Pre-implementation, 2011 (n = 3945) | Post-implementation, 2012 (n = 4200) | P-valuea | |
|---|---|---|---|
| Age in years, mean (SD) | 63.1 (17.1) | 63.0 (17.5) | 0.79 |
| Male, n (%) | 2152 (55) | 2370 (56) | 0.09 |
| Medical admission, n (%) | 3166 (80) | 3347 (80) | 0.53 |
| Primary diagnosis for medical admission, n (%)b | |||
| Cardiocerebrovascular disease | 1007 (32) | 1083 (32) | 0.149 |
| Sepsis/Infectious disease | 655 (21) | 772 (23) | |
| Toxic/Metabolic disease | 195 (6) | 209 (6) | |
| Gastrointestinal/Liver disease | 312 (10) | 296 (9) | |
| Pulmonary disease | 339 (11) | 342 (10) | |
| Neoplastic disease | 234 (7) | 218 (7) | |
| Renal disease | 99 (3) | 83 (2) | |
| Otherc | 325 (10) | 344 (10) |
Student’s T-test and Chi-squared tests were used to compare patient characteristics between the pre- and post- implementation periods.
Percentages do not add to 100% due to rounding.
“Other” includes: non-malignant hematological disease, rheumatological disease, non-vascular neurological disease.
Table 3.
Baseline mobility and activity status.a
| Scoreb | Pre-implementation, 2011 n (%)c | Post-implementation, 2012 n (%)c | P-valued |
|---|---|---|---|
| Mobility | 0.41 | ||
| 0 | 405 (31) | 605 (31) | |
| 1 | 61 (5) | 71 (4) | |
| 2 | 73 (6) | 93 (5) | |
| 3 | 782 (59) | 1171 (60) | |
| Activity | 0.07 | ||
| 0 | 318 (24) | 504 (26) | |
| 1 | 98 (7) | 117 (6) | |
| 2 | 57 (4) | 59 (3) | |
| 3 | 864 (65) | 1288 (65) | |
| Mobility and Activity | 0.68 | ||
| Fully independent | 732 (57) | 1110 (59) | |
| Fully dependent | 306 (23) | 481 (25) |
Status prior to hospital admission, assessed by nursing intake history from patient or family upon admission to the ICU. In the pre- and post-implementation periods, respectively, data are available as follows: mobility score – 1321 (33%) and 1943 (46%) patients, and activity score – 1337 (34%) and 1968 (47%).
These scores each ranged from 0 to 3, with 1 point assigned if the patient was independent (i.e. not requiring assistance or assistive device) with each of three mobility tasks (bed mobility, bed-to-chair transfer, and ambulation) and activity tasks (dressing or grooming, feeding, and toileting or bathing). For example, a mobility score of 3 means the most independently mobile, while a score of 0 means minimally mobile (unable to even move in bed without assistance). Similarly, an activity score of 3 means the most independent in the activity tasks listed above, while a score of 0 means inability to perform any of the tasks listed above without assistance.
Percentages do not add to 100% due to rounding.
Chi-squared tests were used to compare categorical differences between the pre- and post-implementation periods.
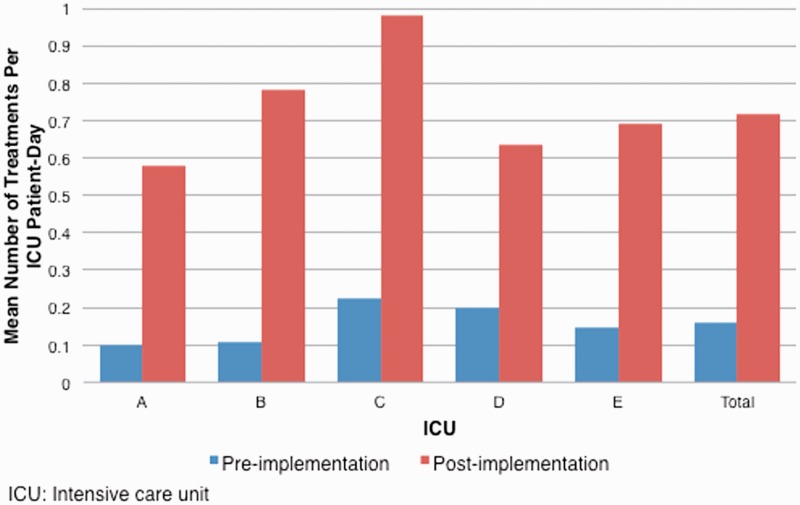
Rehabilitation treatments
Table 4 shows the distribution of patients by the number of ICU rehabilitation treatments received during their ICU stay in the pre- and post-implementation periods. There was a significant increase in the proportion of patients who received more rehabilitation treatments during their ICU stay in the post-implementation period (p < 0.001). In the pre- versus post-implementation periods, respectively, the mean number of rehabilitation (PT or OT) treatments was 0.16 versus 0.72 per ICU patient-day (p < 0.001, Figure 1). In the pre-implementation period, there was similarity in mean number of rehabilitation treatments per ICU patient-day across all five ICUs (range: 0.10–0.22) with a larger range during the post-implementation period (0.58–0.98). The mean number of rehabilitation treatments per ICU patient-day also increased from the pre- versus post-implementation period for all subgroups of patients who were fully independent, intermediate, and fully dependent for both baseline activity and mobility, from 0.11 to 0.63, 0.14 to 0.77, and 0.13 to 0.63, respectively. Finally, in the pre- versus post-implementation periods, patients ambulated with physical therapy at least once during their ICU stay in 15% versus 50% of ICU admissions (p < 0.001).
Table 4.
Distribution of patients by the number of ICU rehabilitation treatments received during their ICU stay.
| Rehabilitation treatments received (n) | Pre-implementation, 2011 |
Post-implementation, 2012 |
P-valueb |
|---|---|---|---|
| %a | %a | ||
| 0 | 69 | 21 | <0.001 |
| 1 | 15 | 21 | |
| 2 | 7 | 16 | |
| 3 | 3 | 10 | |
| 4 | 2 | 8 | |
| 5–10 | 4 | 16 | |
| >10 | 1 | 8 |
ICU: intensive care unit.
Percentages do not add to 100% due to rounding.
A Chi-squared test was used to compare the distribution of patients between the pre- and post-implementation periods.
Figure 1.
The mean number of rehabilitation treatments per intensive care unit patient-day in the pre- versus post-implementation period.
Outcomes
Four out of five ICUs had a significantly decreased mean ICU LOS in the post-implementation period, ranging from a decrease of 0.4 days (6.7% of pre-implementation LOS) to 0.6 days (10.3%). The overall average ICU LOS across all five ICUs was 5.8 versus 5.4 days (p < 0.001) in the pre- versus post-implementation period (Table 5), with a mean decrease of 0.4 days (95% confidence interval (CI) 0.3–0.5). Across all five ICUs, the number of ICU admissions in the post-implementation period increased by 255 (6.5% of pre-implementation value).
Table 5.
Length of stay outcomes.a
| ICU |
||||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | Overall | |
| Number of ICU admissions, n | ||||||
| Pre, 2011 | 587 | 594 | 779 | 1011 | 974 | 3945 |
| Post, 2012 | 687 | 608 | 853 | 1022 | 1030 | 4200 |
| % Change | +17.0 | +2.4 | +9.5 | +1.1 | +5.7 | +6.5 |
| Mean (SD) ICU LOS, days | ||||||
| Pre, 2011 | 5.8 (5.9) | 5.7 (5.9) | 5.0 (9.6) | 6.2 (7.7) | 6.0 (7.6) | 5.8 (7.6) |
| Post, 2012 | 5.2 (6.3) | 5.9 (7.3) | 4.6 (7.4) | 5.7 (7.3) | 5.6 (6.4) | 5.4 (7.0) |
| Change in Mean ICU LOS, days | −0.6 | 0.2 | −0.4 | −0.5 | −0.4 | −0.4 |
| % Change | −10.0 | +3.5 | −8.0 | −8.1 | −6.7 | −6.9 |
| P-value | <0.001 | 0.124 | <0.001 | <0.001 | 0.001 | <0.001 |
| Mean (SD) Hospital LOS, days | ||||||
| Pre, 2011 | 17.5 (20.0) | 16.2 (20.7) | 14.3 (13.7) | 11.2 (12.8) | 16.3 (17.0) | 14.7 (16.7) |
| Post, 2012 | 15.1 (15.2) | 15.9 (15.7) | 14.1 (15.5) | 10.4 (12.4) | 15.5 (18.1) | 13.9 (15.6) |
| Decrease in Mean Hospital LOS, days | −2.4 | −0.3 | −0.2 | −0.8 | −0.8 | −0.8 |
| Change (%) | −13.7 | −1.9 | −1.4 | −7.1 | −4.9 | −5.4 |
| P-value | <0.001 | 0.187 | 0.406 | <0.001 | <0.001 | <0.001 |
ICU: Intensive care unit; SD: standard deviation; LOS: length of stay.
ICUs A, B and E are purely medical ICUs, while ICU D is a non-surgical cardiac ICU, and ICU C is the surgical ICU.
In the pre- versus post-implementation period, mean hospital LOS for admissions from all five ICUs was 14.7 vs. 13.9 days, representing a significant mean decrease of 0.8 days (95% CI 0.6 - 0.9 days, p < 0.001), representing a 5.4% decrease from pre-implementation LOS. Across each of the five ICUs, there was a decrease in hospital LOS with a range of 0.2 days (1.4%) to 2.4 days (13.7%) (Table 5). The reduction of ICU LOS accounted for half of the reduction in hospital LOS. The mean decrease in hospital LOS spent outside of the ICU in the pre- and post-implementation periods was 0.4 days (p < 0.001).
Table 6 shows the distribution of LOS outcomes by percentiles in the pre- and post-implementation periods. The change in ICU LOS distribution had a p-value of 0.06. The change in hospital LOS distribution had a p-value of 0.005. The reductions in ICU and hospital LOS were in the highest quartile of the LOS distribution.
Table 6.
Distribution of length of stay outcomes.
| Pre, 2011 |
Post, 2012 |
P valuea |
|
|---|---|---|---|
| Percentiles, % | ICU LOS, Days | 0.06 | |
| 1st | 1 | 1 | |
| 5th | 1 | 1 | |
| 10th | 1 | 1 | |
| 25th | 2 | 2 | |
| Median, 50th | 3 | 3 | |
| 75th | 7 | 6 | |
| 90th | 13 | 12 | |
| 95th | 19 | 17 | |
| 99th | 37 | 34.5 | |
|
Percentiles, %
|
Hospital LOS, Days
|
0.005 | |
| 1st | 1 | 1 | |
| 5th | 2 | 2 | |
| 10th | 3 | 3 | |
| 25th | 5 | 5 | |
| Median, 50th | 9 | 9 | |
| 75th | 18 | 17 | |
| 90th | 32 | 31 | |
| 95th | 44 | 44 | |
| 99th | 82 | 76 | |
ICU: Intensive care unit; LOS: length of stay.
Mann–Whitney–Wilcoxon rank sum test was used to compare the distribution of ICU and hospital LOS between the pre- and post-implementation periods.
There was no change in pre- and post-implementation ICU LOS in the subgroups of patients who were fully independent, intermediate, or fully dependent in their pre-admission activity and mobility.
The distribution of hospital mortality and discharge destinations were the same in the pre- versus post-implementation periods (Table 7), with 17% dying, 59% discharged home, and 20% discharged to a health care facility (e.g. rehabilitation or other facility).
Table 7.
Hospital mortality and discharge destination.
| ICU |
||||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | Overall | |
| Died, n (%) | ||||||
| Pre, 2011 | 126 (22) | 142 (25) | 54 (7) | 104 (10) | 234 (24) | 660 (17) |
| Post, 2012 | 153 (24) | 131 (23) | 53 (6) | 104 (10) | 261 (25) | 702 (17) |
| Survived – Home, n (%) | ||||||
| Pre, 2011 | 276 (49) | 288 (51) | 571 (75) | 701 (70) | 433 (45) | 2269 (59) |
| Post, 2012 | 288 (44) | 290 (50) | 608 (73) | 735 (72) | 496 (48) | 2417 (59) |
| Survived – Facilitya, n (%) | ||||||
| Pre, 2011 | 136 (24) | 118 (21) | 127 (17) | 165 (17) | 212 (22) | 758 (20) |
| Post, 2012 | 170 (26) | 135 (23) | 164 (20) | 135 (13) | 190 (19) | 794 (19) |
| Survived – Otherb, n (%) | ||||||
| Pre, 2011 | 31 (5) | 21 (4) | 9 (1) | 29 (3) | 79 (8) | 169 (4) |
| Post, 2012 | 40 (6) | 25 (4) | 9 (1) | 40 (4) | 77 (8) | 191 (5) |
| P-value | 0.52 | 0.61 | 0.47 | 0.14 | 0.19 | 0.94 |
ICU: intensive care unit.
“Facility” included: long-term acute care facility, intermediate care facility, sub-acute nursing facility, long term care facility, and inpatient rehabilitation facility.
“Other” included patients who were discharged to: law enforcement, psychiatric hospital, left against medical advice, home hospice, and a hospice facility.
Discussion
In this retrospective pre-post study of 8145 ICU admissions, a multi-ICU coordinated implementation of an early rehabilitation program, across two hospital sites, resulted in a significant increase in the proportion of patients who received more rehabilitation treatments during their ICU stay and a significant increase in the mean number of rehabilitation treatments per ICU patient-day. These improvements were associated with a significantly reduced mean ICU LOS and hospital LOS, as well as an increase in ICU admissions.
Our study demonstrates that implementation of a multi-disciplinary early rehabilitation program across different types of ICUs (medical, cardiac, surgical) across two campuses of a large academic hospital system was able to increase rehabilitation therapy in the ICUs. At the time of implementation planning, guidelines for ICU rehabilitation activities were available and adapted from the existing literature.16,19 In addition to education for the multidisciplinary ICU staff regarding the plan for the early ICU rehabilitation program, the assignment of specific physical and occupational therapists to primarily work in the five ICUs and the hiring of additional rehabilitation assistants were central parts of this large implementation effort. In the post-implementation year, the mean number of rehabilitation treatments per ICU patient-day increased more than 4-fold from 0.16 to 0.72 per ICU patient-day. This is consistent with prior pre-post projects evaluating early ICU rehabilitation, where mean treatments per day increased three-fold from 0.33 to 0.83,19 the number of patients receiving PT in the ICU increased by 60%,24 or physical therapy billable units per day of PT doubled.29 To our knowledge, our multisite study is among the largest of published reports of early rehabilitation of critically ill patients and adds to the growing number of academic institutions reporting experiences with implementation of early ICU rehabilitation programs.10–13,16–19,23,24,29
In our study, after implementation of the early ICU rehabilitation program, mean ICU LOS decreased by 0.4 days (95% CI 0.3–0.5, p < 0.001) and mean hospital LOS decreased by 0.8 days (95% CI 0.6–0.9, p < 0.001). This finding reinforces earlier studies demonstrating that implementation of early rehabilitation in the ICU can contribute to a reduction in LOS,10–13,16–24 though our LOS reduction is modest relative to prior studies. The ICU LOS reduction from prior retrospective and prospective studies ranged from 1.4 to 2.1 days (20–33% reduction), while the hospital LOS reduction ranged from 2 to 3.3 days (14–23% reduction).11–12,19,24,29 These LOS reduction ranges come from studies of different types of ICUs, with different eligibility (for example, patients on mechanical ventilation versus all-comers), and so precludes direct comparison to the LOS changes observed in our study of all-comers to five ICUs. Since we do not have detailed patient-level information such as those on mechanical ventilation or those specifically with acute lung injury, we were unable to examine LOS differences in these subgroups that might have had additional benefit from early ICU rehabilitation. A meta-analysis21 of other prospectively controlled studies that included surgical and medical ICU patients found a modest but statistically significant pooled effect size for both ICU (n = 597, Hedge’s g −0.34 [−0.51 to −0.18], p < 0.01) and hospital LOS (n = 441, Hedge’s g −0.34 [−0.53 to −0.15], p < 0.01). There was variability in the amount that our ICU early rehabilitation program increased rehabilitation treatments per ICU-patient day among the five ICUs. The range of ICU and hospital LOS in the post-implementation period could reflect a difference in adherence to implementation of the program or a different patient response to the same program depending on the type of ICU (e.g. surgical versus medical). Further exploration is needed in other large-sized multi-ICU studies that involve different types of ICUs.
The distribution of ICU and hospital LOS by percentiles also changed between the pre- and post-implementation periods. In particular, we found that the reductions in ICU and hospital LOS were in the highest quartile of the LOS distribution. The early ICU rehabilitation program may have had the highest impact on patients in highest quartile of LOS because they were exposed to the program longest or that these patients were the most likely to benefit from the program. Since the benefits were concentrated in the highest quartile, the median LOSs did not show a reduction. For example, even if every patient in the highest quartile had their LOS reduced by half, the median would still not change.
To further explore why our LOS reductions are modest relative to prior reports,11,19,23–24 we examined a subgroup of our study population where more detailed baseline information was available. In our study, as assessed by history at ICU admission, there were 25% of ICU admissions where the patient was completely dependent for both baseline activity and mobility prior to their ICU admission and critical illness. These fully dependent patients are likely from long-term care facilities or those with advanced illnesses requiring complete care at home or at long-term nursing facilities. As evidenced by the similar increase in mean number of rehabilitation treatments per ICU patient day for the fully dependent, the intermediate, and the fully independent subgroups from 0.13 to 0.63 versus 0.14 to 0.77 versus 0.11 to 0.63, respectively), the severely debilitated candidates were not excluded from participating in early rehabilitation in the ICU. There was no significant difference in ICU LOS between pre- and post-implementation periods for the fully dependent, the intermediate, or fully independent groups. There are two possibilities for these findings – either that the subgroups have inadequate power to detect a statistically significant difference in ICU LOS between the pre- and post-implementation periods, or that the overall ICU LOS reduction was driven by the group that did not have baseline activity and mobility scores available for subgroup analysis. The baseline activity and mobility scores were only available for a 30–40% subset of the total 8145 ICU admissions in the study, so we cannot better describe the baseline status of the group of patients that drove the decrease in overall ICU and hospital LOS. This highlights the need for future studies to help better define candidates who may benefit from the early rehabilitation efforts while in the ICU.
There was no difference in the discharge distribution between our pre- and post-implementation periods. Existing literature has a variety of findings regarding this outcome, with Morris et al.11 reporting no difference in discharge disposition, Schweickert et al.12 reporting a non-significant trend in increased discharges to home, and Engel et al.24 reporting an increase in the number of patients who received PT in the ICU being discharged home. With only limited data available regarding discharge destination within the existing administrative data used for this analysis, we are constrained in our ability to more comprehensively evaluate patients’ physical functional status upon discharge in the pre- versus post-implementation periods.
The ICU LOS reduction associated with implementation of an early ICU rehabilitation program may have costs and savings implications. Lord et al.23 applied financial models based on LOS data from an ICU early rehabilitation program and estimated that the projected net cost of implementation was modest compared to improvement in patient outcomes. For the implementation program in our study, the complete profit and loss assessment data was not made available to the investigators. However, the hospital has indicated that there was a positive return on investment based on the new resources committed and the calculated savings due to the consequent decreases in LOS.
There are several potential limitations of our study. First, this was a retrospective observational study using hospital-wide administrative data limiting cause–effect inferences from being drawn and having potential bias from unmeasured confounders such as severity of illness and need for mechanical ventilation. Moreover, we could not control for temporal changes between the pre- and post-implementation periods. However, there were no other systematic interventions implemented to reduce ICU LOS during the study period, no systematic changes in our institution’s ICU referral patterns, and the baseline characteristics (Table 2) and mortality rate (Table 7) of our pre- and post-intervention groups were remarkably similar. Furthermore, our findings of decreased ICU LOS were consistent with multiple prior studies.10–13,16–24 Second, pre-admission baseline mobility and functional scores were available for only a subset of patients, which limits inferences that can be made from these data. Third, the retrospective design precluded having detailed and standardized data on rehabilitation activities performed in the pre- versus post-implementation periods. In future evaluations, the integration of a reliable and feasible ICU mobility scale would be helpful to better address this issue.30 Lastly, the generalizability of our findings is tempered since this was a single hospital system. However, given that the study was conducted in five ICUs (including medical, surgical and cardiac ICU) at two locations, and that our results are consistent with prior literature, this weakness may be limited.
Conclusion
A large, multi-ICU, early rehabilitation program was concurrently implemented in two sites of our hospital system. In this retrospective before/after comparison, we found that the ICU early rehabilitation program increased the proportion of patients who received more rehabilitation treatments during their ICU stay and increased the average number of rehabilitation treatments per ICU patient-day. After implementation of the program, we also observed a significantly reduced ICU and hospital length of stay, as well as an increase in ICU admissions.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Outside the work under consideration for publication, Dr Brodie reports receiving research support and previously provided research consulting for Maquet Cardiovascular. All compensation is paid to Columbia University. He is a member of the Medical Advisory Board for ALung Technologies. All compensation is paid to Columbia University. Outside the work under consideration for publication, Dr Needham reports receiving grant support from NIH, AHRQ, and Moore Foundation.
Authors’ contributions
RW, NY, SC, DMN, and DB contributed to literature search, figures, study design, data collection, data analysis, data interpretation, and writing. MN and KHP contributed to data collection, data analysis, data interpretation and writing. TB, DV, DR, KRP, PR, EPM, SMB and DB contributed to the conception of the study, data interpretation and writing. All authors read and approved the manuscript.
References
- 1.Herridge MS, Tansey CM, Matté A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med 2011; 364: 1293–1304. [DOI] [PubMed] [Google Scholar]
- 2.Iwashyna TJ, Ely EW, Smith DM, et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 2010; 304: 1787–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pandharipande PP, Girard TD, Jackson JC, et al. Long-term cognitive impairment after critical illness. N Engl J Med 2013; 369: 1306–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bienvenu OJ, Colantuoni E, Mendez-Tellez PA, et al. Depressive symptoms and impaired physical function after acute lung injury: A 2-year longitudinal study. Am J Respir Crit Care Med 2012; 185: 517–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med 2011; 39: 371–379. [DOI] [PubMed] [Google Scholar]
- 6.Fan E, Dowdy DW, Colantuoni E, et al. Physical complications in acute lung injury survivors: A 2-year longitudinal prospective study. Crit Care Med 2014; 42: 849–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Needham DM. Mobilizing patients in the intensive care unit: Improving neuromuscular weakness and physical function. JAMA 2008; 300: 1685–1690. [DOI] [PubMed] [Google Scholar]
- 8.Brummel NE, Jackson JC, Pandharipande PP, et al. Delirium in the ICU and subsequent long-term disability among survivors of mechanical ventilation. Crit Care Med 2014; 42: 369–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gosselink R, Bott J, Johnson M, et al. Physiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill Patients. Intensive Care Med 2008; 34: 1188–1199. [DOI] [PubMed] [Google Scholar]
- 10.Engel HJ, Needham DM, Morris PE, et al. ICU early mobilization: from recommendation to implementation at three medical centers. Crit Care Med 2013; 41: S69–S80. [DOI] [PubMed] [Google Scholar]
- 11.Morris PE, Goad A, Thompson C, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med 2008; 36: 2238–2243. [DOI] [PubMed] [Google Scholar]
- 12.Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet 2009; 373: 1874–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zanni JM, Korupolu R, Fan E, et al. Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care 2010; 25: 254–262. [DOI] [PubMed] [Google Scholar]
- 14.Nydahl P, Ruhl AP, Bartoszek G, et al. Early mobilization of mechanically ventilated patients: a 1-day point-prevalence study in Germany. Crit Care Med 2014; 42: 1178–1186. [DOI] [PubMed] [Google Scholar]
- 15.Berney SC, Harrold M, Webb SA, et al. Intensive care unit mobility practices in Australia and New Zealand: A point prevalence study. Crit Care Resusc 2013; 15: 260–265. [PubMed] [Google Scholar]
- 16.Bailey P, Thomsen GE, Spuhler VJ, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med 2007; 35: 139–145. [DOI] [PubMed] [Google Scholar]
- 17.Thomasen GE, Snow GL, Rodriguez L, et al. Patients with respiratory failure increase ambulation after transfer to an intensive care unit where early activity is a priority. Crit Care Med 2008; 36: 1119–1124. [DOI] [PubMed] [Google Scholar]
- 18.Burtin C, Clerckx B, Robbeets C, et al. Early exercise in critically ill patients enhances short-term functional recovery. Crit Care Med 2009; 37: 2499–2505. [DOI] [PubMed] [Google Scholar]
- 19.Needham DM, Korupolu R, Zanni JM, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: A quality improvement project. Arch Phys Med Rehabil 2010; 91: 536–542. [DOI] [PubMed] [Google Scholar]
- 20.Adler J, Malone D. Early mobilization in the intensive care unit: A systematic review. Cardiopulm Phys Ther J 2012; 23: 5–13. [PMC free article] [PubMed] [Google Scholar]
- 21.Kayambu G, Boots R, Paratz J. Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Crit Care Med 2013; 41: 1543–1554. [DOI] [PubMed] [Google Scholar]
- 22.Li Z, Peng X, Zhu B, et al. Active mobilization for mechanically ventilated patients: a systematic review. Arch Phys Med Rehabil 2013; 94: 551–561. [DOI] [PubMed] [Google Scholar]
- 23.Lord RK, Mayhew CR, Korupolu R, et al. ICU early physical rehabilitation programs: financial modeling of cost savings. Crit Care Med 2013; 41: 717–724. [DOI] [PubMed] [Google Scholar]
- 24.Engel HJ, Tatebe S, Alonzo PB, et al. Physical therapist-established intensive care unit early mobilization program: quality improvement project for critical care at the University of California San Francisco Medical Center. Phys Ther 2013; 93: 975–985. [DOI] [PubMed] [Google Scholar]
- 25.Wahab R, Yip NH, Chandra S, et al. Implementation of an early rehabilitation program in multiple intensive care units reduces length of stay. Am J Respir Crit Care Med 2013; 187: A3622. [Google Scholar]
- 26.Urbach DR, Govindarajan A, Saskin R, et al. Introduction of surgical safety checklists in Ontario, Canada. N Engl J Med 2014; 370: 1029–1038. [DOI] [PubMed] [Google Scholar]
- 27.Schneider EB, Hyder O, Wolfgang CL, et al. Provider versus patient factors impacting hospital length of stay after pancreaticoduodenectomy. Surgery 2013; 154: 152–161. [DOI] [PubMed] [Google Scholar]
- 28.Selvin S. Three statistical models for estimating length of stay. Health Serv Res 1977; 12: 322–330. [PMC free article] [PubMed] [Google Scholar]
- 29.Clark DE, Lowman JD, Griffin RL, et al. Effectiveness of an early mobilization protocol in a trauma and burns intensive care unit: A retrospective cohort study. Phys Ther 2013; 93: 186–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hodgson C, Needham D, Haines K, et al. Feasibility and inter-rater reliability of the ICU mobility scale. Heart Lung 2013; 43: 19–24. [DOI] [PubMed] [Google Scholar]