Abstract
The Intensive Care Foundation, in partnership with the James Lind Alliance, has supported a national project to identify and prioritise unanswered questions about adult intensive care that are important to people who have been critically ill, their families, and the health professionals who care for them. We conducted a secondary analysis to explore differences in priorities determined by different respondent groups in order to identify different groups’ perceptions of gaps in knowledge. There were two surveys conducted as part of the original project. Survey 1 comprised a single open question to identify important research topics; survey 2 aimed to prioritise these topics using a 10-point Likert scale. In survey 1, despite clear differences in suggestions amongst the respondent groups, themes of comfort/communication and post-ICU rehabilitation were the within the top 2 suggestions across all groups. Patients and relatives suggested research topics to which they could easily relate, whereas there was a greater breadth of suggestions from clinicians. In survey 2, the number of research priorities that received a mode score of 10 varied from 1 to 36. Patients scored 36 out of the 37 topics with a mode score of 10. All other groups scored topics with more discrimination, with the number of topics with a mode score of 10 ranging from 1 to 20. Differences in the proportions of the representative groups are therefore unlikely to have translated to an impartial conclusion. Clinicians, patients, and family members have jointly identified the research priorities for UK ICM practice.
Keywords: Adult, consensus, intensive care, research, uncertainty
Introduction
Clinical research is integral to improving patient outcomes. Traditionally, research topics were determined by scientists or clinical researchers and largely dominated by physicians. Whilst this has allowed significant progress in healthcare, it is recognised that patients and their families, along with other healthcare professionals are able to provide novel insight into the identification of relevant research questions. Organisations such as the James Lind Alliance (JLA) bring together diverse healthcare professionals, patients, and carers to identify research priorities. The UK Intensive Care Society led a JLA priority setting partnership which conducted a nationwide research prioritisation project over 18 months. The results of the research prioritisation process have been published.1
Objective
The aim of this secondary analysis was to explore differences in priorities determined by different respondent groups in order to identify different groups’ perceptions of gaps in knowledge.
Methods
The full methodology of this JLA partnership has been previously published.1 In brief, an online nationwide survey was conducted to identify areas of uncertainty in adult intensive care that should be prioritised for future research (survey 1). This survey was completed by intensive care healthcare professionals, intensive care patients (present and past) and their families. Over 1200 responses were generated. The responses from survey 1 were categorised into pre-defined themes based on the intensive care scientific literature and intensive care training modules. Existing evidence was identified using a detailed literature review of Medline, Cochrane Controlled Clinical trials register and clinicaltrials.gov. Preliminary editing and verification permitted us to summarise these suggestions within 151 treatment ‘uncertainties’; further iterative review by members of the Steering Group produced 37 themes.1
A second nationwide survey was conducted asking participants to rate the importance of each proposed research theme using a 10-point Likert scale. The research uncertainties were ranked by mode. The top 19 suggestions from survey 2 were taken to a nominal group consisting of 21 clinicians, patients and family representatives for ranking into the top 12 research priorities.
For this current paper, an in-depth analysis of the results of survey 2 was conducted to ascertain if there were any differences in profile of research priorities between different respondent groups.
Results
Survey 1
There were 484 respondents for survey 1. This comprised of clinical staff (88%), patients (8%) and family members (4%).
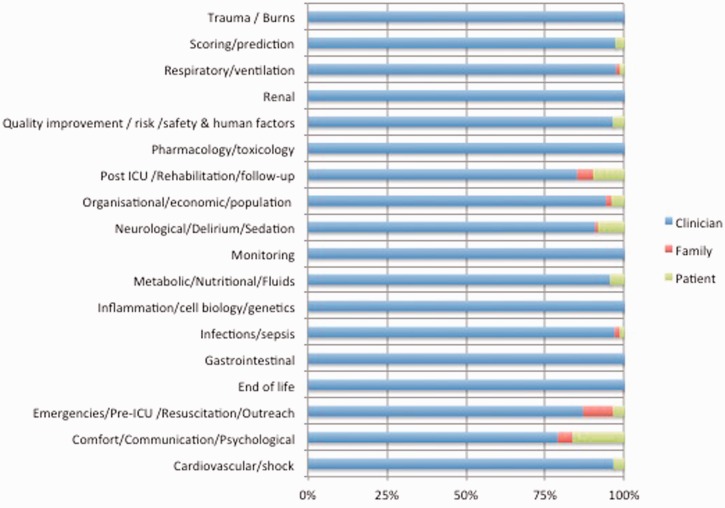
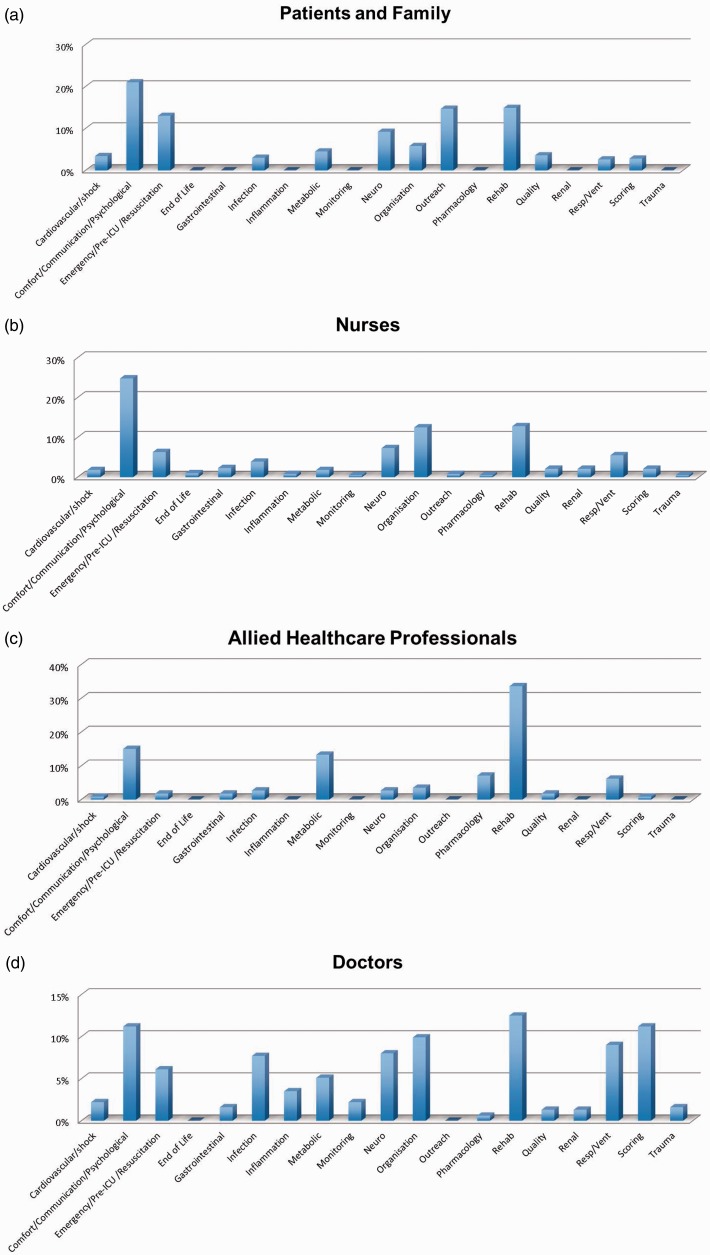
There were clear differences amongst the respondent groups, with no patients or relatives providing suggestions for almost half of the research themes (Figures 1 and 2). However, comfort/communication and post-ICU rehabilitation were the within the top 2 suggestions across all groups (Table 1). There was also significant overlap between the other top suggestions between groups.
Figure 1.
Research themes – proportion of responses by group.
Figure 2.
Results from survey 1 – responses by groups. (a) Patients and family, (b) allied healthcare professional, (c) nurses, (d) doctors.
Table 1.
Top 5 research themes identified by each group (survey 1).
| Clinicians (n = 425; suggestions n = 1069) | Patient (n = 41; suggestions n = 95) | Family (n = 18; suggestions n = 46) | |
|---|---|---|---|
| 1 | Comfort/communication/psychological (16.8%) | Comfort/communication/ psychological (42.3%) | Post-ICU/rehabilitation/follow-up (37.5%) |
| 2 | Post-ICU/rehabilitation/follow-up (16.8%) | Post-ICU/rehabilitation/follow-up (30.8%) | Comfort/communication/psychological (18.8%) |
| 3 | Organisational/economic/population (11.9%) | Organisational/economic/ population (7.7%) | Emergency/pre-ICU/resuscitation/outreach (15.6%) |
| 4 | Respiratory/ventilation (6.8%) Scoring/prediction (6.6%) | Emergency/pre-ICU/resuscitation/outreach (3.8%) | Organisational/economic/ population (6.3%) |
| 5 | Scoring/prediction (1.9%) Neurological/delirium/sedation (1.9%) Metabolic/nutritional/fluids (1.9%) | Respiratory/ventilation (3.1%) Neurological/delirium/sedation (3.1%) Infections/sepsis (3.1%) |
The most frequent themes across all groups are shaded for ease of reference.
The staff group was comprised of nurses (49%), doctors (31%), allied healthcare professionals from six disciplines (10%) and others including advanced practitioners, clinical academics, technicians and administrators (10%). The nurses comprised of ICU/HDU nurses (73%), research nurses (14%), nurse consultants/managers (8%) and other nurses (including outreach nurses, 5%). Doctors were mainly consultant grade (68%) with trainees making up 30%. There was dissimilarity between the different professional groups (Figure 1). Within each subgroup of professional category, either comfort/communication or post-ICU rehabilitation was listed as one of the top 2 research priorities (Tables 2 and 3). Only nurse managers and trainee doctors had top suggestions (organisational/economic/population and scoring/prediction, respectively) that were neither comfort/communication nor post-ICU rehabilitation. Although small in number when considered separately, Allied Health professionals tended to prioritise topics within their respective spheres of practice (Table 4).
Table 2.
Top 5 research themes identified by different nurse groups (survey 1).
| Nurse – ICU/HDU (n = 152; suggestions n = 381) | Nurse – Research (n = 30; suggestions n = 74) | Nurse – Manager (n = 16; suggestions n = 38) | Nurse – Other (n = 10; suggestions n = 20) | |
|---|---|---|---|---|
| 1 | Comfort/communication/psychological (24.8%) | Post-ICU/rehabilitation/follow-up (27.0%) | Organisational/economic/population (27.5%) | Comfort/communication/psychological (29.6%) |
| 2 | Post-ICU/rehabilitation/follow-up (12.8%) | Comfort/communication/ psychological (21.6%) | Comfort/communication/psychological (17.5%) | Organisational/economic/population (14.8%) |
| 3 | Organisational/economic/ population (12.5%) | Infections/sepsis (6.8%) | Post-ICU/rehabilitation/follow-up (10.0%) Respiratory/ventilation (10.0%) Emergency/pre-ICU/resuscita tion/outreach (10.0%) | Emergency/pre-ICU/resuscitation/outreach (14.8%) |
| 4 | Neurological/delirium/sedation (7.3%) | Respiratory/ventilation (8.1%) | Scoring/prediction (11.1%) Infections/sepsis (11.1%) | |
| 5 | Emergency/pre-ICU/ resuscitation/outreach (6.3%) | Infections/sepsis (6.8%) |
The most frequent themes across all groups are shaded for ease of reference.
Table 3.
Top 5 research themes identified by consultant and trainee doctors (survey 1).
| Doctor–Consultant (n = 89; suggestions n = 237) | Doctor–Trainee (n = 38; suggestions n = 82) | |
|---|---|---|
| 1 | Post-ICU/rehabilitation/follow-up (13.7%) | Scoring/prediction (17.3%) |
| 2 | Organisational/economic/population (11.0%) | Comfort/communication/psychological (12.0%) |
| 3 | Comfort/communication/psychological (10.6%) | Respiratory/ventilation (8.0%) Post-ICU/rehabilitation/follow-up (8.0%) Neurological/delirium/sedation (8.0%) Infections/sepsis (8.0%) |
| 4 | Scoring/prediction (9.7%) | |
| 5 | Respiratory/ventilation (8.8%) |
The most frequent themes across all groups are shaded for ease of reference.
Table 4.
Top 5 research themes identified by allied health professionals (survey 1).
| AHPs (all) (n = 43; suggestions n = 113) | Physiotherapist (n = 13; suggestions n = 38) | Dietician (n = 11; suggestions: n = 25) | SALT (n = 9; suggestions n = 21) | Pharmacist (n = 7; suggestions n = 25) | |
|---|---|---|---|---|---|
| 1 | Post-ICU/rehabilitation/follow-up (35.5%) | Post-ICU/rehabilitation/follow-up (71.1%) | Metabolic/nutrition/fluids (52.0%) | Comfort/Communication/Psychological (38.1%) | Pharmacology (36.8%) |
| 2 | Metabolic/nutrition/ fluids (14.6%) | Comfort/communication/psychological (10.5%) | Post-ICU/rehabilitation/follow-up (16.0%) | Respiratory/ventilation (14.3) | Post-ICU/Rehabilitation/follow-up (15.8%) |
| 3 | Comfort/communication/psychological (11.7%) | Respiratory/ventilation (2.5%) | Other (8.0%) | Metabolic (9.5%) Post ICU/rehabilitation/follow-up (9.5%) Organisational/economic/population (9.5%) | Infection (10.5%) neuro logical/delirium/sedation (10.5%) |
| 4 | Pharmacology (7.8%) | Infection (2.5%) Other (2.5%) | Organisational/economic/population (4%) Pharmacology (4%) Quality (4%) | ||
| 5 | Respiratory/ventilation (4.9%) | Organisational/economic/population (5.3%) Metabolic/nutrition/fluids (5.3%) Quality (5.3%) Gastrointestinal/liver (5.3%) Cardiovascular (5.3%) |
The most frequent themes across all groups are shaded for ease of reference.
Survey 2
There were 513 respondents in survey 2.1 The demographics of respondents were similar to survey 1, with nursing staff making up the greatest number of respondents (40.7%), followed by doctors (26.1%), allied healthcare professionals (20.9%) and patients and relatives (12.3%).
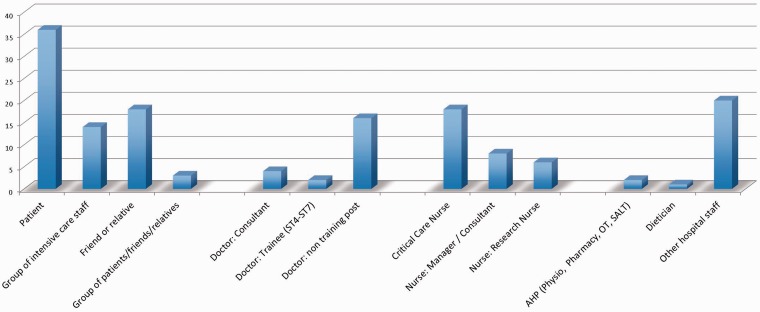
The number of research priorities that received a mode score of 10 varied from 1 to 36. Patients prioritised the most number of topics, with 36 out of the 37 topics with a score mode of 10 (Figure 3). In contrast, groups of patients (e.g. local intensive care patient support groups), consultants, trainee doctors and allied healthcare professionals ranked fewer than five topics with a mode score of 10.
Figure 3.
Number of topics scored with mode 10 by group (survey 2).
The question ‘How can patients who may benefit from intensive care be identified early and admitted to the ITU at the right time?’ had a mode score of 10 by the most number of groups of respondents. This was eventually ranked the top priority for intensive care.1 All topics presented in survey 2 had a mode score of 10 by at least one group of respondents.
Discussion
The results of the secondary analysis shed some light onto the similarities and differences in research priorities between different professional groups and patients/families. There were a disproportionate number of clinicians for both surveys 1 and 2. However, it is reassuring that the top 2 themes suggested across all groups in survey 1 were similar (‘comfort/communication’ and ‘post-ICU/rehabilitation’). Furthermore, there was also significant overlap between the other top suggestions between groups. This finding should dispel any concerns that the results of survey 1 were entirely a reflection of what healthcare professionals perceived were important research agenda items, adding internal validity to the study.
Patients and relatives suggested research topics to which they could easily relate. Research themes that were symptom related (‘comfort/communication’ and ‘post-ICU rehabilitation’) made up the majority of patients and families’ responses (73 and 56% of responses, respectively). Although these themes were also the most common themes selected by clinicians, they made up a much smaller proportion of responses (34%).
Similarly, topics about the organisation of care (‘organisational/economic/population’) and care prior to or at admission to the ICU (‘emergency/pre-ICU/resuscitation/outreach’) were also high on the agenda for patients and family. In contrast, most disease-specific and treatment-related research themes (e.g. ‘liver/gastrointestinal’, ‘renal’, ‘monitoring’) were suggested only by clinicians.
Professional subgroups also had a tendency to prioritise what was directly relevant to their daily practice. For instance, nurse managers most frequently suggested ‘organisational/economic/population’ topics whilst ICU trainee doctors identified ‘scoring/prediction’ most frequently. However, the purpose of the research prioritisation process was to ascertain research priorities from a wide range of groups, which is reflected in the differences between groups in survey 1.
In survey 2, patients rated 36 out of the 37 topics with a mode score of 10. As all but one topic had an identical mode score, the responses from patients had almost no discriminatory value. It is unclear if this would have been any different had there been more patients taking part in survey 2. All other groups scored topics with more discrimination, with the number of topics with a mode score of 10 ranging from 1 to 20.
Conclusion
We have demonstrated that the differences in the proportions of the representative groups are unlikely to have translated to an impartial conclusion. Clinicians, patients and family members have collectively identified the research priorities for UK ICM practice. The Intensive Care Foundation has announced a themed call for research proposals based on one or more of the identified priorities and will award a grant of £50,000 to fund a pilot study in 2015. The results of this are eagerly awaited.
Acknowledgments
The JLA Intensive Care PSP gratefully acknowledges the support and contribution of all participating ICUs, and the staff, patients and families who participated in this project. In particular:
Steering Group Members: Nishkantha Arulkumaran, Stephen Brett, Tessa Clarke, Catherine Plowright, Mo Peskett, Pam Ramsay, Hannah Reay, Carl Waldmann, Keith Young.
JLA Advisors: Tessa Clarke, Sheela Upadhyaya, David Crowe, Lester Firkins.
Intensive Care Foundation: Jenny Dixon, Paola Battisegola, Nina Taylor.
Nominal Group Participants, Facilitators and Observers: Nishkantha Arulkumaran, Oliver Boney, Stephen Brett, David Crowe, Irene Francis, Judy Heller, Richard Howard-Griffin, Lauren Maher, Michelle Mantripp, Gary Masterson, Isabel McDonnell, John McDonnell, Jackie McRae, Leanne Metcalf, Sarah Moreton, Mollie Peberdy, William Peberdy, Mo Peskett, Catherine Plowright, Richard Pugh, Hannah Reay, Dawn Roe, Harriet Shannon, Ganesh Suntharalingam, David Tanqueray, Tamsin Mary Tanqueray, Sheela Upadhyaya, Julie Walford, Keith Young.
Declaration of conflicting interests
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Hannah Reay: Intensive Care Foundation Deputy Director of Research. Stephen Brett: Intensive Care Society, President. Nishkantha Arulkumaran: None
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Intensive Care Foundation and was a National Institute for Health Research Portfolio project. SJB is supported by the NIHR Comprehensive Biomedical Research Centre based at Imperial College Healthcare NHS Trust and Imperial College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Reference
- 1.Reay H, Arulkumaran N, Brett SJ. Priorities for future intensive care research in the UK: results of a James Lind Alliance Priority Setting Partnership. J Intens Care Soc 2014; 15: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]