Abstract
Introduction
Septic shock is a life-threatening condition requiring vasopressor agents to support the circulatory system. Several agents exist with choice typically guided by the specific clinical scenario. We used a network meta-analysis approach to rate the comparative efficacy and safety of vasopressors for mortality and arrhythmia incidence in septic shock patients.
Methods
We performed a comprehensive electronic database search including Medline, Embase, Science Citation Index Expanded and the Cochrane database. Randomised trials investigating vasopressor agents in septic shock patients and specifically assessing 28-day mortality or arrhythmia incidence were included. A Bayesian network meta-analysis was performed using Markov chain Monte Carlo methods.
Results
Thirteen trials of low to moderate risk of bias in which 3146 patients were randomised were included. There was no pairwise evidence to suggest one agent was superior over another for mortality. In the network meta-analysis, vasopressin was significantly superior to dopamine (OR 0.68 (95% CI 0.5 to 0.94)) for mortality. For arrhythmia incidence, standard pairwise meta-analyses confirmed that dopamine led to a higher incidence of arrhythmias than norepinephrine (OR 2.69 (95% CI 2.08 to 3.47)). In the network meta-analysis, there was no evidence of superiority of one agent over another.
Conclusions
In this network meta-analysis, vasopressin was superior to dopamine for 28-day mortality in septic shock. Existing pairwise information supports the use of norepinephrine over dopamine. Our findings suggest that dopamine should be avoided in patients with septic shock and that other vasopressor agents should continue to be based on existing guidelines and clinical judgement of the specific presentation of the patient.
Keywords: Anaesthesia and intensive care, resuscitation, septic shock, vasoactive drugs
Introduction
Septic shock is a life-threatening condition requiring intense patient monitoring and supportive therapy for organ dysfunction.1 Release of inflammatory mediators leads to widespread vasodilatation, capillary leak and reduced systemic vascular resistance. After initial fluid resuscitation, vasopressor therapy is required. These agents have their effect by increasing vascular resistance, raising mean arterial pressure and maintaining perfusion of critical body tissues and organ systems.2
The two main classes of drugs used are adrenergic (alpha, beta or combined) agonists and vasopressin analogues. Alpha-adrenergic agonists increase vascular tone and blood pressure, while beta-agonists increase blood flow via inotropic and chronotropic effects. Both classes of drugs are associated with risks including reduction of cardiac output and regional blood flow for alpha-agonists and myocardial ischaemia with beta-agonists.2,3 In addition to its action on adrenergic receptors, dopamine also acts on dopaminergic receptors which can result in unwanted side effects including immunosuppression, renal impairment and increased risk of arrhythmias.2 Vasopressin analogues simulate the action of the anti-diuretic hormone (also known as vasopressin). They have multiple effects, and in health they play a key role in retention of water in the distal tubules and collecting ducts leading to an increase in circulating volume. In shock states, they act as vasoconstrictors. Despite short-term increase in blood pressure in observational studies, there have been concerns that infusion may reduce blood flow to the heart, kidneys and intestine.4
The latest guidance from the Surviving Sepsis Campaign released in 2012 recommends norepinephrine as the first-choice vasopressor with addition of epinephrine where an additional agent is needed.5 Dopamine has fallen out of favour due to evidence suggesting an increased risk of arrhythmias and higher mortality.6 This guidance is based mainly on findings from meta-analyses published between 2011 and 2012.6–8 In the intervening time, there has been growing interest in vasopressin analogues, although their relative place compared to older vasopressors has yet to be fully characterised.9 The current recommendation from the Surviving Sepsis Campaign is that vasopressin can be added to norepinephrine to raise mean arterial pressure or reduce norepinephrine requirement although sole use of vasopressin is discouraged.5
Existing reviews have predominantly assessed only the direct evidence available in pairwise comparisons of vasopressors.6–9 Network meta-analysis or mixed-treatment comparisons allow simultaneous comparisons of multiple treatments and may permit the ranking of the different treatments relative to other treatments. Network meta-analysis may also provide more accurate effect estimates.10–14 There has been one previous network meta-analysis that included many trials assessing mortality but did not specifically look at safety outcomes.15 The aim of this review was to compare the safety and relative efficacy of different vasopressor agents on 28-day mortality and arrhythmia incidence in septic shock patients.
Methods
Trial identification, selection and extraction of data
A comprehensive electronic search was undertaken. The following databases were searched from inception to September 2014: MEDLINE, Embase, Science Citation Index Expanded, Cochrane Central Register of Controlled Trials, Clinicaltrials.gov and the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) search portal. We used MeSH and free-text terms for various forms of the terms ‘septic’, ‘shock’, ‘vasopressors’ and individual types of vasopressors in an intentionally broad strategy. The exact search strategy is listed in online Appendix 1. Additional articles or abstracts were retrieved by ‘related citation’ search and by manually scrutinising the reference list of relevant publications. There were no restrictions on language.
Publications were selected for review if they satisfied the following inclusion criteria: randomised clinical trial, human adult patients, two or more of the following arms: vasopressor versus another type of vasopressor or no active intervention, reported 28-day mortality or arrhythmias. Two authors (MN, MM) independently examined all retrieved articles for inclusion. Any disagreement over inclusion or exclusion was resolved by consensus. Data were extracted using a pre-designed data collection form by two authors (MN, MM) with disagreements resolved by consensus. The following data-points were extracted: first author, year of publication, inclusion and exclusion criteria, number of patients, baseline patient characteristics including average age, gender and severity score, intervention details including drug, dose and timing, risk of bias assessment, arrhythmia incidence and 28-day mortality. Authors of original trials were contacted by email where reported data were unclear or unavailable.
Risk of bias was assessed using the Cochrane Risk of Bias tool.16 It includes six domains that could affect the effect estimates due to systematic error. These are: sequence generation, allocation concealment, blinding of participants, healthcare providers and outcome assessors, incomplete outcome data, selective reporting, and other potential sources of bias (such as funding). Each domain was rated as low, uncertain or high risk of bias.
Statistical analysis
Network meta-analysis combines direct evidence within trials and indirect evidence across trials.17 Our analysis was based on guidance by the National Institute for Clinical Excellence (NICE) Decision Support Unit (DSU). Execution was similar to previous network meta-analysis reviews by our lead author such as in the field of liver resection.18 Each drug or drug combination was considered a separate treatment. This corresponds to the full interaction model.19 A network plot was created to ensure that the trials were connected by treatments (i.e. there was at least one trial which allowed indirect comparisons of treatments) using Stata/SE 12.1 (StataCorp LP). Any trials that were not connected to the network were excluded. A Bayesian network meta-analysis using the Markov chain Monte Carlo method in WinBUGS 1.4.3 was performed in the presence of sufficient clinical homogeneity using the methods suggested by NICE DSU.20–23 Odds ratios (OR) were calculated for the outcomes. The treatment contrast (i.e. log odds ratio) for any two treatments (‘functional parameters') was modelled as a function of comparisons between each individual treatment and an arbitrarily selected reference group (‘basic parameters').11 The reference group was norepinephrine where possible. The WinBUGS codes utilised in the analysis are presented in online Appendix 2.
Execution of our network analysis was similar to a prior analysis on liver resection by the senior author from our group as summarised below.18 The posterior probabilities (effect estimates or values) of the treatment contrast can vary depending upon the initial values with which the simulations are started. To control the random error due to choice of initial values, we attempted to perform the network analysis for three different sets of initial values (priors) as per the guidance from NICE DSU.20 If the results from the three different priors were similar (convergence, checked by Brooks-Gelman-Rubin plot), then reliability of the results could be assumed.24 We ran the models for at least 30,000 simulations for ‘burn in' for three different chains (sets of initial values). We ran the models for further 30,000 simulations to obtain the effect estimates. We then ensured that the results in the three different chains were similar in order to control for random error due to choice of priors. Visual inspection of convergence obtained after simulations in the burn in was also performed.
Three different models were run for each outcome. The fixed-effect model assumed that the treatment effect was the same across all studies. The random-effects consistency model assumed that the treatment effect was distributed normally across the studies but assumed that the transitivity assumption was satisfied (i.e. the population studied, the definition of outcomes and the methods used were similar across studies and that there was consistency between the direct comparison and indirect comparison). The random-effects inconsistency model did not assume the transitivity assumption. If the inconsistency model resulted in a better model fit than the consistency model, the results of the network meta-analysis could be unreliable and so interpretation would require extreme caution. The choice of the model between fixed-effect model and random-effects model was based on the model fit as per the guidelines of the NICE TSU.20 The model fit was assessed by deviance residuals and deviance information criteria (DIC).25 The DIC takes into account the model fit and the model complexity. The simpler model was used, i.e. fixed-effect model if the DIC was similar between the fixed-effect model and random-effects model. Alternatively, the random-effects model would be used if it resulted in a better model fit as indicated by a DIC lower than that of fixed-effect model by at least three. The effect estimates of each pairwise comparison and the 95% credible intervals (equivalent to 95% confidence intervals in a frequentist meta-analysis) were calculated using the formulae for calculating the effect estimates in indirect comparisons.10 Statistical significance was accepted as 95% confidence excluding a value of one.
Results
Study selection
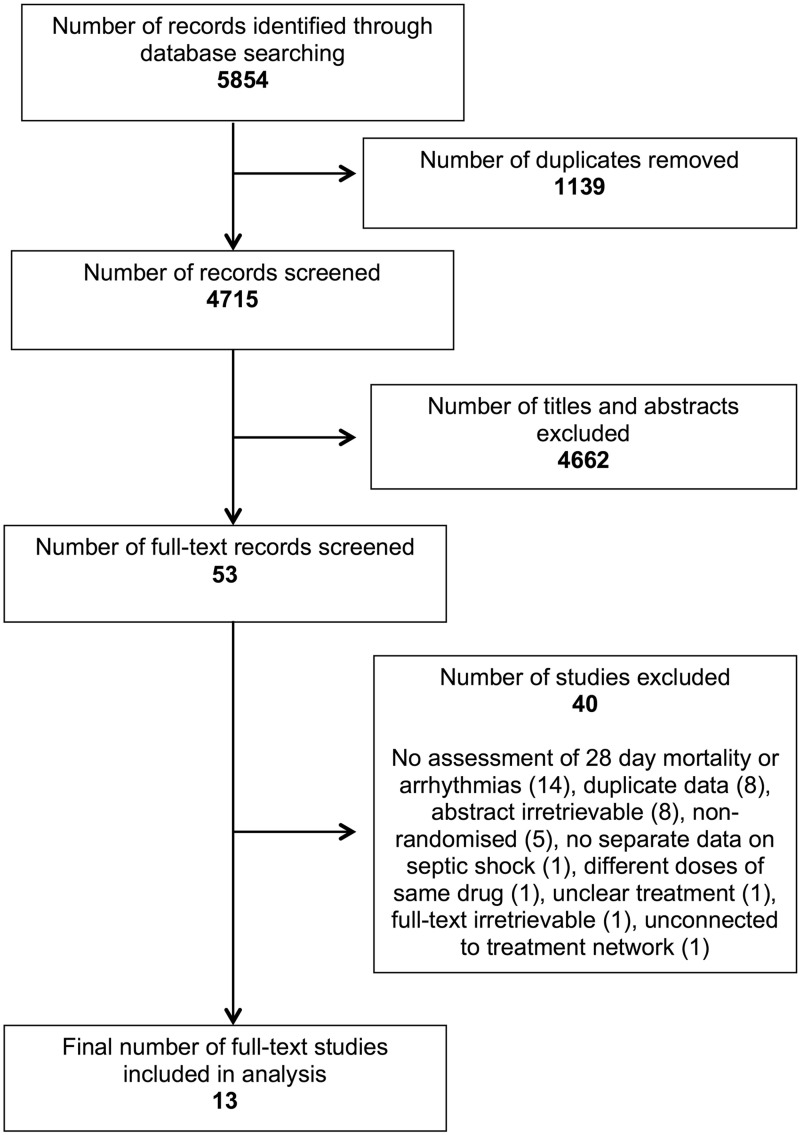
Execution of the search strategy yielded 5854 records from database inception to September 2014. After excluding duplicates, there were 4715 records remaining. A total of 4662 of these records were excluded upon review of title and abstract leaving 53 full-text records for screening. Thirteen full-text studies were selected for inclusion. Reasons for exclusion of full-text records are detailed in Figure 1.
Figure 1.
Flow of records through the study selection process.
Study characteristics
Study and patient characteristics for included studies are presented in Table 1. There were a total of 13 trials (11 full-text articles and 2 reports from ongoing studies). A total of 3146 patients were included in analyses of 28-day mortality, and 2198 patients were included in analyses of arrhythmias. Trial arms were well balanced within trials. The mean age of patients ranged from 51 to 73. The proportion of female patients ranged from 27% to 54%. The range of severity scores is displayed in Table 1.
Table 1.
Characteristics of included trials.
| References | No. of patients | Intervention in group 1 | Intervention in group 2 | Age | Female (%) | Severity score system | Baseline severity score | Therapy duration |
|---|---|---|---|---|---|---|---|---|
| Annane et al. 200726 | 330 | EPI | NOREPI + DOB | 63 | 39 | SAPS II | 53 | As required to day 28 |
| De Backer et al.3 | 1044 | DOPA | NOREPI | NR | NR | NR | NR | As required to day 28 |
| Lauzier et al. 200627 | 23 | VASO | NOREPI | 54 | 39 | APACHE II | 23 | Up to 48 h |
| Mahmoud & Ammar 201228 | 60 | NOREPI + DOB | NOREPI + EPI | 51 | 48 | SOFA | 15 | NR |
| Morelli et al. 200829 | 32 | NOREPI | PHENYL | 70 | 34 | SAPS II | 56 | Up to 12 h |
| Morelli et al.30 | 45 | NOREPI | VASO/TERLI | 66 | 27 | SAPS II | 60 | Up to 48 h |
| Myburgh et al. 200831 | 158 | EPI | NOREPI | NR | NR | NR | NR | Until target MAP without vasopressor |
| Oliveira et al. 201432 | 407 | NOREPI | VASO | NR | NR | NR | NR | NR |
| Patel et al. 200233 | 24 | NOREPI | VASO | 68 | 25 | APACHE II | 23 | Up to 4 h |
| Patel et al. 201034 | 252 | DOPA | NOREPI | NR | 54 | APACHE II | 28 | As required to day 28 |
| Russell et al.4 | 802 | NOREPI | VASO | 61 | 38 | APACHE II | 27 | As required |
| Svoboda et al. 201235 | 32 | TERLI | NOREPI | 73 | 38 | SOFA | 18 | Up to 72 h |
| Zambolim et al.36 | 107 | VASO | NOREPI | NR | NR | NR | NR | NR |
APACHE: acute physiology and chronic health evaluation; DOB: dobutamine; DOPA: dopamine; EPI: epinephrine; MAP: mean arterial pressure; NOREPI: norepinephrine; NR: not reported; PHENYL: phenylephrine; SAPS: simplified acute physiology score; SOFA: sequential organ failure assessment; TERLI: terlipressin; VASO: vasopressin.
Study risk of bias
Risk of bias assessments for included trials is presented in Table 2. Sequence generation and allocation concealment were generally at low risk of bias with the exception of the trial by Patel et al.34 The same was true for blinding of patients, healthcare providers and outcome assessors. Six of the 13 trials were at risk of bias for missing outcome data due to post-randomisation drop outs. In all six cases, the proportion of drop outs relative to the total sample size was not felt to have meaningfully altered the reported effect estimate. Overall, there were 46 reported drop outs from a total of 3192 patients (average 1.4%, range 0 to 6.3% per study were reported).
Table 2.
Risk of bias in included trials.
| References | Sequence generation | Allocation concealment | Blinding of patients and healthcare providers | Blinding of outcome assessors | Missing outcome data | Selective outcome reporting | Source of funding |
|---|---|---|---|---|---|---|---|
| Annane et al. 200726 | Low | Low | Low | Low | Low | Low | Low |
| De Backer et al.3 | Low | Low | Low | Low | Low | Low | Unclear |
| Lauzier et al. 200627 | Low | Low | High | High | High | Unclear | Low |
| Mahmoud & Ammar 201228 | Low | Low | Unclear | Low | Low | Unclear | Low |
| Morelli et al. 200829 | Low | Low | Low | Low | Unclear | Low | Low |
| Morelli et al.30 | Low | Low | Low | Low | Unclear | Low | Low |
| Myburgh et al. 200831 | Low | Low | Low | Unclear | High | Unclear | Low |
| Oliveira et al. 201432 | Unclear | Unclear | Unclear | Unclear | High | Unclear | Unclear |
| Patel et al. 200233 | Low | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Patel et al. 201034 | High | High | High | High | Low | Low | Low |
| Russell et al.4 | Low | Low | Low | Low | High | Low | Low |
| Svoboda et al. 201235 | Low | Low | Unclear | Unclear | High | Unclear | Low |
| Zambolim et al.36 | Unclear | Unclear | Unclear | Unclear | High | Unclear | Unclear |
28-day mortality
Standard pairwise meta-analyses were possible for two combinations. Two studies compared norepinephrine versus dopamine. There was no significant difference in mortality (odds ratio (OR) 0.83 (95% CI 0.67 to 1.03)) (online appendix figure S2). Three studies compared norepinephrine with vasopressin analogues. There was no significant difference in mortality (OR 1.13 (95% CI 0.86 to 1.48)) (online appendix figure S3). There was no change in significance when repeating the analysis with random-effects models. There was no visual or statistical evidence of heterogeneity.
The network plot showing the connection between comparisons (nodes) is presented in online appendix figure S4. There was good convergence of the values in both the fixed- and random-effects models and no evidence of inconsistency. There was no major difference between the DIC of the fixed- and random-effects models (121.7 and 123.6, respectively), and so the fixed-effect model was used for analysis. The relative effect estimates between comparisons in the fixed-effect model are presented in Table 3. Vasopressin was superior to dopamine (OR 0.68 (95% CI 0.5 to 0.94)). There were no statistically significant differences in the remaining comparisons.
Table 3.
28-day mortality effect estimates from network meta-analysis.
| Norepinephrine | Dopamine | Epinephrine | Vasopressins | Norepinephrine and epinephrine | Norepinephrine and dobutamine | |
|---|---|---|---|---|---|---|
| Norepinephrine | – | OR 1.2; 95% CI 0.97 to 1.5 | OR 0.69; 95% CI 0.34 to 1.42 | OR 0.82; 95% CI 0.66 to 1.03 | OR 0.63; 95% CI 0.17 to 2.37 | OR 0.55; 95% CI 0.23 to 1.27 |
| Dopamine | – | – | OR 0.58; 95% CI 0.27 to 1.22 | OR 0.68; 95% CI 0.5 to 0.94 | OR 0.52; 95% CI 0.14 to 2 | OR 0.45; 95% CI 0.19 to 1.09 |
| Epinephrine | – | – | – | OR 1.19; 95% CI 0.56 to 2.52 | OR 0.91; 95% CI 0.2 to 4.1 | OR 0.79; 95% CI 0.26 to 2.39 |
| Vasopressins | – | – | – | – | OR 0.76; 95% CI 0.2 to 2.93 | OR 0.66; 95% CI 0.28 to 1.59 |
| Norepinephrine and epinephrine | – | – | – | – | – | OR 0.87; 95% CI 0.18 to 4.21 |
| Norepinephrine and dobutamine | – | – | – | – | – | – |
Note: The odds ratio represents the odds of mortality in the agent at the top of the table relative to the agent in the first column of the table.
CI, 95% credible intervals (equivalent to 95% confidence intervals); OR: odds ratio.
Arrhythmias
Standard pairwise meta-analyses were possible for two combinations. Two studies compared norepinephrine versus dopamine. There were significantly more arrhythmias in the dopamine group compared to norepinephrine (OR 2.69 (95% CI 2.08 to 3.47)) (online appendix figure S5). Three studies compared norepinephrine with vasopressin analogues. There was no significant difference in arrhythmias between the groups (OR 1.36 (95% CI 0.56 to 3.31)) (online appendix figure S6). There was no change in significance when repeating the analysis with random-effects models. There was evidence of substantial heterogeneity in the vasopressin comparison.
The network plot showing the connection between comparisons (nodes) is presented in online appendix figure S7. There was good convergence of values in both the fixed- and random-effects models with no evidence of inconsistency. However, there was a significant difference between the DIC of the fixed- and random-effects models (63.9 and 60.3). We therefore opted to utilise the random-effects model. The relative effect estimates between comparisons are presented in Table 4. The relative effect estimates between comparisons are presented in Table 4. There were no statistically significant differences. Most of the confidence intervals were extremely wide (the network meta-analysis estimates utilised both direct and indirect information).
Table 4.
Arrhythmia effect estimates from network meta-analysis.
| Norepinephrine | Dopamine | Vasopressins | Phenylephrine | |
|---|---|---|---|---|
| Norepinephrine | – | OR 3.32; 95% CI 0.15 to 75.73 | OR 0.4; 95% CI 0.01 to 11.45 | OR 2.87; 95% CI 0.01 to 584.92 |
| Dopamine | – | – | OR 0.12; 95% CI 0 to 11.79 | OR 0.86; 95% CI 0 to 412.14 |
| Vasopressins | – | – | – | OR 7.18; 95% CI 0.01 to 3863.37 |
| Phenylephrine | – | – | – | – |
The odds ratio represents the odds of arrhythmia incidence in the agent at the top of the table relative to the agent in the first column of the table.
CI 95%: credible intervals (equivalent to 95% confidence intervals); OR: odds ratio.
Discussion
Summary
In this network meta-analysis of trials assessing 28-day mortality of vasopressor agents, we found evidence to suggest superiority of vasopressin over dopamine. Our standard pairwise meta-analyses showed no significant difference between comparisons for which there was more than one trial available (norepinephrine versus dopamine; norepinephrine versus vasopressin analogues). Of trials in the network meta-analysis assessing arrhythmia incidence, we found no evidence to suggest one vasopressor over another. Standard pairwise analyses suggested greater arrhythmias with dopamine compared to norepinephrine.
Comparison to the literature
There have been several existing pairwise meta-analyses of vasopressor agents and one network meta-analysis to date.6–9,15 Our findings differ from the previous literature on this topic in some areas. The most likely reason for the difference relates to our decision to include only trials reporting 28-day mortality for assessment of mortality. This excluded trials in which exposure to the interventional vasopressor was limited (a matter of hours in the case of many trials for which the primary endpoints were haemodynamic variables) or in which the time point of mortality measurement was either ambiguously reported or reported only for early time points.
De Backer et al.6 assessed both observational and randomised trials and concluded that dopamine administration was associated with greater mortality and a higher incidence of arrhythmic events. However, they acknowledged that restricting to the two trials that reported 28-day mortality (also the two largest) resulted in a similar effect estimate size but with confidence intervals crossing one. Our pairwise findings on arrhythmia incidence are in agreement with De Backer et al. suggesting superiority of norepinephrine over dopamine. Serpa Neto et al.9 investigated the effect of vasopressin and terlipressin in vasodilatory shock. They concluded that vasopressin significantly reduced mortality, including the subset of trials assessing septic shock. However, this conclusion is not completely held up by their data which demonstrate non-significant effects when both terlipressin and vasopressin individually are compared to norepinephrine (both sets of confidence intervals include one). Furthermore, their combined analysis of vasopressin and terlipressin together which does demonstrate a significant mortality benefit to vasopressin analogues may be inaccurate due to double counting of a control group in a three-arm trial by Morelli et al.30 Adjustment to take into account this double counting renders the combined effect estimate non-significant.
A meta-analysis by Vasu et al. of six trials concluded that norepinephrine was superior to dopamine for 28-day or in-hospital mortality in patients with shock in which sepsis was the predominant etiology.8 However, by utilizing the entire cohort of the large trial by De Backer et al. (1656 patients) rather than the 1044 who actually had septic shock, they included 612 patients without septic shock.3 This included a subset of 280 patients with cardiogenic shock in which subgroup analysis in the original trial had already shown a significant mortality benefit for norepinephrine. The net effect would be to drown out the effect of the other five septic shock trials (only 364 patients in total). Hence, the effect estimates from this meta-analysis are unlikely to be reliable for the stated cohort of septic shock patients. In contrast, Havel et al.7 found insufficient evidence for superiority of one vasopressor over another among a series of pairwise analyses in their Cochrane review. Correction for an error in the mortality figures extracted for one trial (Mathur et al.37) does not change the non-significance of the original results for dopamine versus norepinephrine.37
The only network meta-analysis performed on this topic concluded with support for norepinephrine (with or without low dose vasopressin) as first-line therapy for septic shock, but suggested no strong evidence for epinephrine over dopamine as second-line.15 Statistical methods between our study and analysis were similar and so the differences in effect estimates once again likely relate to our selection of only trials reporting 28-day mortality and our inclusion of a trial missed in the search by Oba and Lone.15
Strengths and limitations
There were several strengths to this analysis. First, we performed a very broad and sensitive search of the major databases with no restriction on language (reflected in the large number of abstracts and titles screened). Second, by limiting to only those trials in which 28-day mortality was reported, we were afforded a greater deal of homogeneity in our comparisons for this outcome. Third, the network meta-analysis approach allowed us to explore comparative effects between the vasopressors taking into account both direct (pairwise) and indirect information. Finally, we also assessed the safety outcome of arrhythmia incidence which was not assessed in the only other published network meta-analysis of vasopressors in septic shock.15
However, our study conclusions should also be borne in light of several limitations. First, our decision to exclude trials not reporting 28-day mortality may have affected the presented effect estimates and their statistical significance leading to a possible type two error. It should be noted that of the trials excluded on this basis, none were large trials (defined as greater than 100 patients) or low risk of bias trials. A second limitation was that we were only able to assess mortality and arrhythmia incidence as our outcomes. Despite death being a fixed, objective and clinically relevant outcome, it is well recognised that mortality assessment does not capture all of the clinical information relevant to patients and providers.38 For example, adverse events, quality of life, duration of organ support and intensive care unit length of stay are commonly also of interest. However, the lack of reported data in these outcome domains meant that it would be unlikely that such a network meta-analysis would provide fruitful information. This was exemplified by the extremely large confidence intervals in our analysis of arrhythmias. Third, we feel that there was still extensive clinical heterogeneity in trials that were included (though there was no clear statistical evidence of this). Numerous variations in protocols and methods between studies included differences in drug timing, dosage, co-intervention, patient cohort and reporting quality of trials. There has been much literature on the heterogeneous nature of intensive care patients and the difficulties of performing research in this setting. It may be that certain subgroups of patients experience significant benefit when given specific vasopressors. We elected not to perform standard meta-regression analyses, as many of the factors that we hypothesised could have led to such heterogeneity that was not clearly reported. Finally, the small numbers of trials in each pairwise analysis precluded assessment of publication bias.
Implications
Our findings suggest that vasopressin is superior to dopamine in terms of 28-day mortality for septic shock. The comparisons for vasopressin versus norepinephrine and dopamine versus norepinephrine were not statistically significant. There was insufficient evidence to suggest a superior arrhythmia profile of one agent over another in the network meta-analysis though pairwise analysis confirmed the existing paradigm of dopamine leading to more arrhythmias than norepinephrine.
Ongoing trials assessing specific contexts and cohorts are likely to shed further light on this topic. For example, the VANISH trial is assessing whether vasopressin, and its interaction with steroids, is more effective at reducing kidney dysfunction while VANCS II is specifically investigating a cohort of cancer patients.36,39 Finally, our findings suggest that care should be taken when interpreting the findings of nominally significant pairwise meta-analyses. The statistical significance of comparisons in such reviews can be greatly affected by a few small trials in such cases despite their small weight within the Forest plot.
Conclusions
In this network meta-analysis, vasopressin was superior to dopamine for 28-day mortality in septic shock. Existing pairwise information supports the use of norepinephrine over dopamine. Our findings suggest that dopamine should be avoided in patients with septic shock and that other vasopressor agents should continue to be based on existing guidelines and clinical judgement of the specific presentation and circumstances of the patient.
Supplementary Material
Declaration of conflicting interests
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: ACG is the principal investigator for VANISH trial (http://www.isrctn.com/ISRCTN20769191).
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med 2013; 369: 840–851. [DOI] [PubMed] [Google Scholar]
- 2.Vincent JL, De Backer D. Circulatory shock. N Engl J Med 2013; 369: 1726–1734. [DOI] [PubMed] [Google Scholar]
- 3.De Backer D, Biston P, Devriendt J, et al. Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med 2010; 362: 779–789. [DOI] [PubMed] [Google Scholar]
- 4.Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med 2008; 358: 877–887. [DOI] [PubMed] [Google Scholar]
- 5.Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 2013; 41: 580–637. [DOI] [PubMed] [Google Scholar]
- 6.De Backer D, Aldecoa C, Njimi H, et al. Dopamine versus norepinephrine in the treatment of septic shock: a meta-analysis*. Crit Care Med 2012; 40: 725–730. [DOI] [PubMed] [Google Scholar]
- 7.Havel C, Arrich J, Losert H, et al. Vasopressors for hypotensive shock. Cochrane Database Syst Rev 2011; 5: CD003709. [DOI] [PubMed] [Google Scholar]
- 8.Vasu TS, Cavallazzi R, Hirani A, et al. Norepinephrine or dopamine for septic shock: systematic review of randomized clinical trials. J Intensive Care Med 2012; 27: 172–178. [DOI] [PubMed] [Google Scholar]
- 9.Serpa Neto A, Nassar APJ, Cardoso SO, et al. Vasopressin and terlipressin in adult vasodilatory shock: a systematic review and meta-analysis of nine randomized controlled trials. Crit Care 2012; 16: R154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bucher HC, Guyatt GH, Griffith LE, et al. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. J Clin Epidemiol 1997; 50: 683–691. [DOI] [PubMed] [Google Scholar]
- 11.Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med 2004; 23: 3105–3124. [DOI] [PubMed] [Google Scholar]
- 12.Lumley T. Network meta-analysis for indirect treatment comparisons. Stat Med 2002; 21: 2313–2624. [DOI] [PubMed] [Google Scholar]
- 13.Mills EJ, Thorlund K, Ioannidis JP. Demystifying trial networks and network meta-analysis. BMJ 2013; 346: f2914. [DOI] [PubMed] [Google Scholar]
- 14.Salanti G, Higgins JP, Ades AE, et al. Evaluation of networks of randomized trials. Stat Methods Med Res 2008; 17: 279–301. [DOI] [PubMed] [Google Scholar]
- 15.Oba Y, Lone NA. Mortality benefit of vasopressor and inotropic agents in septic shock: a Bayesian network meta-analysis of randomized controlled trials. J Crit Care 2014; 29: 706–710. [DOI] [PubMed] [Google Scholar]
- 16.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011; 343: d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mills EJ, Ioannidis JP, Thorlund K, et al. How to use an article reporting a multiple treatment comparison meta-analysis. JAMA 2012; 308: 1246–1253. [DOI] [PubMed] [Google Scholar]
- 18.Simillis C, Li T, Vaughan J, et al. Methods to decrease blood loss during liver resection: a network meta- analysis. Cochrane Database Syst Rev 2014; 4. [DOI] [PubMed] [Google Scholar]
- 19.Welton NJ, Caldwell DM, Adamopoulos E, et al. Mixed treatment comparison meta-analysis of complex interventions: psychological interventions in coronary heart disease. Am J Epidemiol 2009; 169: 1158–1165. [DOI] [PubMed] [Google Scholar]
- 20.Dias S, Sutton AJ, Ades AE, et al. Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Making 2013; 33: 607–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dias S, Sutton AJ, Welton NJ, et al. Evidence synthesis for decision making 3: heterogeneity – subgroups, meta-regression, bias, and bias-adjustment. Med Decis Making 2013; 33: 618–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dias S, Welton NJ, Sutton AJ, Ades AE. Evidence synthesis for decision making 1: introduction. Med Decis Making 2013; 33(5): 597–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dias S, Welton NJ, Sutton AJ, et al. Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Med Decis Making 2013; 33: 641–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brooks SP, Gelman A. Alternative methods for monitoring convergence of iterative simulations. J Comput Graph Statist 1998; 7: 434–455. [Google Scholar]
- 25.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001; 29: 1303–1310. [DOI] [PubMed] [Google Scholar]
- 26.Annane D, Vignon P, Renault A, et al. Norepinephrine plus dobutamine versus epinephrine alone for management of septic shock: a randomised trial. Lancet 2007; 370: 676–684. [DOI] [PubMed]
- 27.Lauzier F, Lévy B, Lamarre P, et al. Vasopressin or norepinephrine in early hyperdynamic septic shock: a randomized clinical trial. Intensive Care Med 2006; 32: 1782–1789. [DOI] [PubMed]
- 28.Mahmoud KM and Ammar AS. Norepinephrine supplemented with dobutamine or epinephrine for the cardiovascular support of patients with septic shock. Indian J Crit Care Med 2012; 16: 75–80. [DOI] [PMC free article] [PubMed]
- 29.Morelli A, Ertmer C, Rehberg S, et al. Phenylephrine versus norepinephrine for initial hemodynamic support of patients with septic shock: a randomized, controlled trial. Crit Care 2008; 12: R143. [DOI] [PMC free article] [PubMed]
- 30.Morelli A, Ertmer C, Rehberg S, et al. Continuous terlipressin versus vasopressin infusion in septic shock (TERLIVAP): a randomized, controlled pilot study. Crit Care 2009; 13: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Myburgh JA, Higgins A, Jovanovska A, et al. A comparison of epinephrine and norepinephrine in critically ill patients. Intensive Care Med 2008; 34: 2226–2234. [DOI] [PubMed]
- 32.Oliveira S, Dessa F, Rocha C, et al. Early Vasopressin Application in Shock study. Crit Care 2014; 18(Suppl 1): 158.
- 33.Patel BM, Chittock DR, Russell JA, et al. Beneficial effects of short-term vasopressin infusion during severe septic shock. Anesthesiology 2002; 96: 576–582. [DOI] [PubMed]
- 34.Patel GP, Grahe JS, Sperry M, et al. Efficacy and safety of dopamine versus norepinephrine in the management of septic shock. Shock 2010; 33: 375–380. [DOI] [PubMed]
- 35.Svoboda P, Scheer P, Kantorová I, et al. Terlipressin in the treatment of late phase catecholamine-resistant septic shock. Hepatogastroenterology 2012; 59: 1043–1047. [DOI] [PubMed]
- 36.Zambolim C, Nagaoka D, Fukushima J, et al. Vasopressin versus norepinephrine for the management of septic shock in cancer patients. Crit Care 2014; 18: S57. [DOI] [PubMed] [Google Scholar]
- 37.Mathur S, Dhunna R, Chakraborty A. Comparison of norepinephrine and dopamine in the management of septic shock using impedance cardiography. Indian J Crit Care Med 2007; 11: 186–191. [Google Scholar]
- 38.Iwashyna TJ, Angus DC. Declining case fatality rates for severe sepsis: good data bring good news with ambiguous implications. JAMA 2014; 311: 1295–1297. [DOI] [PubMed] [Google Scholar]
- 39.Gordon AC, Mason AJ, Perkins GD, et al. Protocol for a randomised controlled trial of VAsopressin versus Noradrenaline as Initial therapy in Septic sHock (VANISH). BMJ Open 2014; 4: e005866. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.