Abstract
Communication is central to the safe and effective delivery of critical care. We present a retrospective analysis of hospital incident reports attributed to communication that were generated by 30 intensive care units in the North West of England from 2009 to 2014. We reviewed when during the critical care pathway incidents occur, the personnel involved, the method of communication used, the type of information communicated and the level of harm associated with the incident. We found that patient safety incidents tend to occur when patients are transferred into or out of the intensive care unit and when information has to be communicated to other teams during the critical care stay. We then examine ways that the patient handover process may be modified to improve communication and safety.
Keywords: Communication, patient handover, hospital incident reporting
Introduction
The care of critically ill patients is a complex process that requires the exchange of information within the critical care team and with other teams. Communication is required during the critical care stay and at transfer of care into and out of the critical care unit. Information also has to be shared with patients and their relatives. It is inevitable that these communication processes sometimes fail, resulting in potential harm to patients. We present a review of patient safety incidents that we classified as involving communication that were reported by critical care units in the North West of England between 2009 and 2014. A patient safety incident is defined as an incident where a patient was harmed or potentially harmed as a result of care.1 We go on to suggest potential areas to focus improvement efforts to improve communication safety.
Methods
Incidents were reported by staff from up to 30 critical care units in the North West of England between 2009 and 2014; the staff used incident reporting software to record a free text description of the incident and to provide a classification of the incident. The free text descriptions of the incidents together with any manager’s report were all stored by hospital trusts for submission to the UK National reporting and learning system.
The critical care units provided us with Excel spread sheets that contained the date of the report, the free text incident reports and, where available, the manager’s report. The units also provided us with annual reports of their ways of working and clinical activity. The text of the incident and manager’s report allowed the incident to be placed into one or more of a number of main incident groups, one group being ‘Communication’. A detailed description of the classification process is currently available on the Greater Manchester Critical Care Network website.2 The classification was either carried out by a senior member of staff on the reporting unit who then sent the completed database table to the lead investigator for checking or the incidents were classified by the lead investigator. Training material for classifiers was provided on the Greater Manchester website,2 and this was augmented by a one-day course for classifiers facilitated by the lead investigator. The incidents were classified according to the harm to patients described in the incident report; so, for example, if a transmissible infection was not handed over but no other patient was described as acquiring the infection, then the incident was not associated with described harm even if the potential for harm was significant. We then subdivided harm to temporary or more than temporary harm.
We provided units with annual reports describing a summary of their incidents with comparative, anonymised data from the other units for all of their patient safety incidents. Apart from providing these reports, there was no specific quality improvement project to try and improve staff safety over the period of the study. We calculated the rate of incident reports per 1000 patient days from the number of patient days as defined by the UK Department of Health’s minimum dataset for critical care.3
From the complete dataset of patient safety incidents, we then extracted incidents classified as ‘Communication incident’ to reclassify them into more detailed subgroups than those in the original dataset. The summary of this classification is shown in Table 1.
Table 1.
Classification of communication incidents.
| Level of harm: No documented harm, temporary harm, more than temporary harm. |
| Method of communication: Verbal, written, verbal/written combined, bleeps and telephone, other electronic methods, other methods (up to two methods allowed). |
| Stage in the critical care pathway: Transfer into critical care from theatre, wards, emergency departments, other hospitals and other or non-defined locations. During the critical care stay. Transfer from critical care. |
| Staff group/service user involved: Between medical staff, between nursing staff, between medical and nursing staff, within the clinical team, with other staff groups (for example, radiologists, porters, etc.) |
| Issue being communicated/problem: Medications, bed management, equipment, infection control, clinical condition of patient, other, staff/relative, requesting and test results, radiology, blood products, contacting other teams, technical failure of communication system, management plan, surgical issues and drains, notes and records, no handover, nutrition and swallow assessment, pressure sore, consultant attribution, past medical history, staffing issues, about transfer journey, staff/patient, unprofessional behavior, estates and facilities management, identification of the patient, procedures, death certification, other team not informed, spinal precautions, theatre preparation, observations, contacting ICU doctors. |
Results
Thirty critical care units submitted incidents from the three critical care networks in the North West of England. Units joined and left the reporting process such that 16 units submitted incident reports during 2009 and 26 units provided reports during 2014.
There were 23,818 incident reports categorised over the six years, of which 1694 (7.1 %) were classified as involving communication problems (communication incidents). The original incident text for the communication incidents contained a median of 285 characters per report (IQR 238–605); manager’s reports were provided in 1395 incidents, and these contained a median of 188 characters (IQR 42–327). There were 122 communication incidents reported in 57,009 patient days during 2009 (2.1 per 1000 days) and 474 incidents in 132,384 patient days in 2014 (3.6 per 1000 patient days). For individual units in 2014, there was a median of 3.3 communication incidents reports per 1000 days (IQR 2.6–5.9/1000 days). Of the 1694 communication incidents, 1385 were also categorised in other incident groups (excluding documentation), 422 in more than one other group; the two groups most commonly described were access and transfer (365 incidents) and medications (351 incidents).
With respect to the stages in the critical care pathway, 419 communication incidents occurred during transfer into critical care (105 associated with harm). There were 827 incidents (190 with harm) described during the critical care stay and 325 incidents (59 with harm) occurred on transfer from critical care. A more detailed description of the distribution of incidents by stages in the critical care pathway is shown in Table 2.
Table 2.
Distribution of incident numbers and harm, staff groups, methods of communication and teams involved by stages in the critical care pathway, communication with relatives and patients are not included.
| Stage in critical care pathway | Incident Numbers (Total (and with harm)) | Staff groups (Total and (with harm)) |
Method of communication (Total and (with harm)) |
Teams involved |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| D/D | D/N | D/N team | N/N | Other staff group* | Verbal | Written | V/W | Bleep/ phone | Other | CC only | CC and other teams | Other teams | ||
| Admission from emergency department | 67 (12) | 5 (2) | 8 (1) | 35 (5) | 13 (3) | 3 (1) | 22 (5) | 7 (1) | 30 (4) | 24 (6) | 4 (0) | 3 (1) | 59 (11) | 5 (0) |
| Admission from theatre | 232 (49) | 9 (2) | 17 (4) | 157 (34) | 43 (9) | 4 (0) | 50 (9) | 37 (4) | 136 (34) | 29 (8) | 7 (2) | 5 (2) | 220 (45) | 7 (2) |
| Admission from the ward | 123 (23) | 11 (5) | 6 (0) | 46 (6) | 52 (11) | 3 (0) | 37 (6) | 20 (5) | 56 (11) | 31 (5) | 6 (0) | 5 (2) | 107 (18) | 11 (3) |
| All admissions including other and not defined | 120 (21) | 23 (8) | 10 (1) | 51 (9) | 17 (3) | 9 (0) | 45 (9) | 10 (1) | 45 (7) | 52 (9) | 3 (2) | 14 (2) | 89 (17) | 17 (2) |
| During the stay on the critical care unit | 827 (190) | 86 (29) | 135 (39) | 161 (40) | 101 (16) | 266 (37) | 274 (75) | 89 (60) | 275 (69) | 255 (59) | 99 (13) | 337 (86) | 432 (96) | 58 (8) |
| Transfer of care from critical care | 325 (59) | 47 (1) | 8 (2) | 108 (24) | 117 (27) | 33 (3) | 88 (11) | 45 (5) | 159 (40) | 94 (11) | 22 (5) | 30 (3) | 287 (56) | 8 (0) |
Note: D: doctor; N: nurse; V/W: verbal and written; CC: critical care.
*radiographers, porters, laboratory workers, etc.
Of the staff groups communicating, communication between medical staff was involved in 181 incidents (47 with harm), between nursing staff in 343 incidents (69 with harm), between medical and nursing staff in 183 incidents (46 with harm). The whole clinical team was involved in 558 incidents (118 with harm) and other staff, for example, radiographers, porters and laboratory staff, were involved in 307 incidents (39 with harm). The staff group was not defined in 14 incidents. There were also 80 incidents involving communication with relatives and 14 with patients. Communication within the critical care team caused 394 incidents, (96 with harm), with other teams caused 1194 incidents (243 with harm) and between two or more other teams 106 incidents (15 with harm).
When classified by methods of communication, more than one method of communication was described in 357 incidents. Verbal communication was described in 516 incidents (115 with harm), written communication was described in 208 incidents (25 with harm) and a combination of both written and verbal communication (for example, where a patient is being handed over from theatre using both a verbal and written handover) was described in 701 incidents (171 with harm). The use of bleeps and phones, including technical failures, was described in 485 incidents (98 with harm), while electronic records and requests were described in 97 incidents (15 with harm). Other methods (for example, emergency buzzers and call systems) were described in 44 incidents (seven with harm).
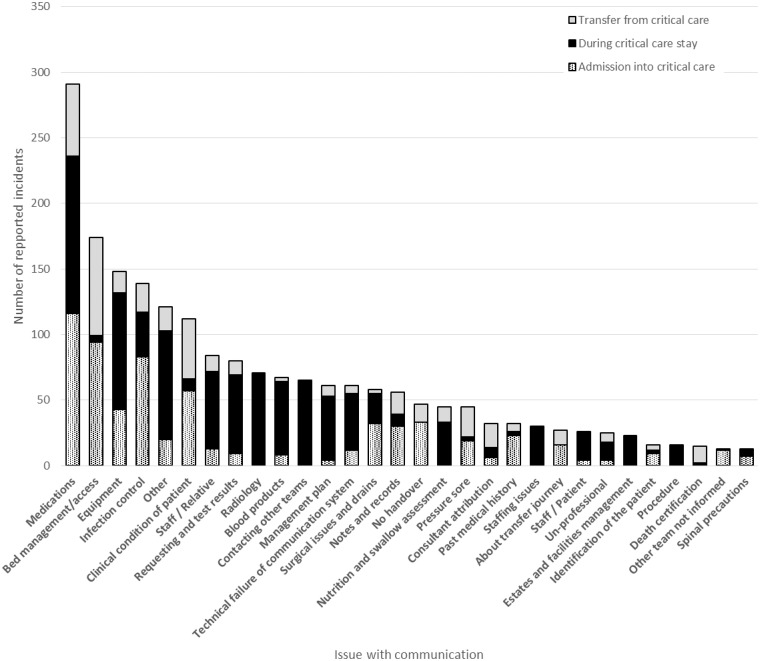
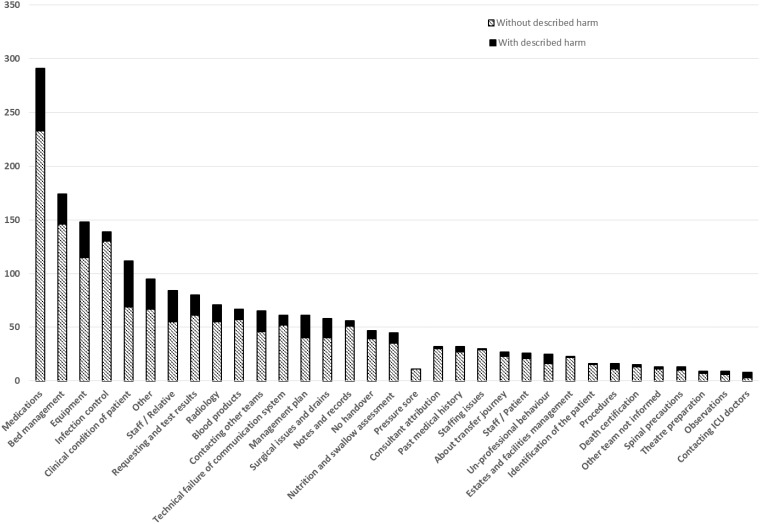
With respect to themes in the communication issues, these varied between stages in the communication process. Figure 1 shows the themes that we identified showing the rates with and without described harm. Figure 2 shows the rates for admission, during stay and during transfer from critical care. Some themes, for example, bed management issues and infection control were seldom associated with harm, whilst others, for example, description of the clinical condition of the patient, were associated with harm in half of the reported incidents.
Figure 1.
The frequency of different communication issues with and without described harm.
Figure 2.
The frequency of different communication issues described at critical care admission, during the critical care stay and at transfer from critical care.
Communication with relatives was described in 80 incidents, 14 involving telephone calls, 8 with linking the relatives to the wrong patient, including where patients had died, and 3 where the relatives were unhappy with the limited information provided. There were 13 incidents where members of staff were intimidated by relatives. Communication with patients often focused on compliance and cooperation with treatment (8 of 14 incidents). Otherwise, there were very wide themes in communication with patients and relatives in a relatively small number of incidents.
Medication use was the most common issue described as a theme in communication. During admission to critical care, common problems involved identification of syringe contents (10 incidents). These were particularly important where the concentration of drug used was unclear, for example, noradrenaline (3 incidents) and propofol (4 incidents). Communication of allergy status (12 incidents) was important in all stages of the pathway, while issues with gentamicin, vancomycin and insulin dosing were important on transfer from critical care.
Equipment issues were also important in all stages in the patient journey (115 incidents, 33 with harm), although the types of equipment were influenced by the stage in the patient journey. The most common types of equipment described were central lines (39 incidents, 9 from theatre, 25 during critical care stay), nasogastric tubes (22 incidents, 20 during critical care stay), epidurals (16 incidents, 8 from theatre, 7 during critical care stay) and arterial lines (15 incidents, 13 from theatre).
There were 71 incidents involving radiology, and this high number reflects the multiple problems with requesting radiology, patient identification and infection control status (31 incidents). Problems with patient preparation (15 incidents) including administration of contrast, line placement and magnetic resonance checks and transfer to the department (seven incidents). Problems during image capture (15 incidents) and finally problems with communication of results (14 incidents), with some incidents describing problems in several stages of the process. A few incidents resulted in significant harm. For example, a patient developed renal failure after contrast and a patient becoming profoundly hypotensive during image capture. Also, there were delays in lifesaving interventions and an inappropriate lumbar puncture occurred in a patient with cerebral oedema. Ten incidents involved problems with conformation of nasogastric tube placement, three with patients receiving intra pulmonary feed and two correctly placed tubes being removed.
More than temporary harm was described in 61 incidents of the total 1694 incidents; examples included: In bed management, a delay in treatment contributing to amputation; in medication, two episodes of respiratory arrest associated with lack of syringe labelling and a loss of a transplanted organ due to omitted medications; in equipment, an episode of sepsis associated with misunderstandings about line removal; and in communication with other teams, a death associated with delay in laparotomy. The nature of these incidents suggests that the patterns of incident that are associated with significant harm are similar to non-harm incidents suggesting a progression model4 where measures to control all communication incidents will influence those relatively unusual incidents associated with significant harm.
Discussion
The study has reviewed all the reported patient safety incidents from the participating units; however, these incidents will only represent a sample of all incidents, as many will have gone unreported.5 It was also a subjective judgment that an incident is categorised as involving a problem with communication; the attribution is probably more judgmental than other categorisations. For example, it is clearer that an incident involves a drug or piece of equipment. The level of harm associated with the incidents also tends to be underestimated because of the requirement for harm to be actually described in the reports.
Although the study has limitations, it allows us to draw a number of conclusions; problems with communication are more likely to occur when care is being transferred into or out of critical care and when information has to be communicated to other teams during the critical care stay. The incidents suggest that transitions of care should be considered as a staged process; the patient’s infection control status should be communicated with enough time to allow appropriate systems to be put in place prior to transfer. The clinical condition of the patient should be reviewed immediately prior to transfer as it may well have changed following the decision to transfer the patient. Structured handovers should be focused around the particular problems commonly associated with the care transition, for example, transfers to the ward should review antibiotic and insulin dosing and ensure that appropriate transfusion thresholds are recorded, while patients admitted from theatre should have the labelling of infusions and arterial lines reviewed. There are well-described processes for the structured handover of patients from theatre,6 for the handover of information during the critical care stay7 and on transfer from critical care.8 The communication of information is also central to effective crew resource management in stressful situations, and processes to improve communication during these difficult situations have been described.9 The clear challenge remains in the implementation of these processes, it’s clear from our results that patients may be transferred with no handover. When patients are transferred to critical care after a period in the recovery unit, they may not have any surgical or anaesthetic handover, and when patients leave the unit around shift handover, the accompanying staff may never have met the patient and may then not be able to find a qualified member of staff to hand over to. The continuing chaotic flow of patients through critical care, where 8% of patients are transferred at night and 11% wait over 24 h from transfer,10 will damage the development of structured handovers.
For radiological procedures, the booking request should be structured to ensure that information about glomerular filtration, magnetic resonance compatibility and infection control status are captured in the request while instructions around venous access and preprocedure contrast are communicated. A structured internal transfer form11 may help with this process.
With respect to contacting other teams, the first requirement is to identify the clinical team responsible for the patient’s whole hospital stay. This is often difficult where patients have multiple pathologies and where they move between different departments; the issue is addressed in recent UK guidance12 and is a particular issue for medical patients who may be transferred from critical care to the care of medical staff who have no prior knowledge of the patient. Communication would also be helped by access to up to date on-call rotas; the shift patterns and staff changes are very complex in most hospitals. Consideration should be given to moving to more modern communications than traditional hospital bleeps and fax machines, technical problems with communication systems being surprisingly common. Where information is handed over from other teams, there should be structured ways of recording this and checking that the instructions are reviewed; there is no point in a surgeon recording postoperative instructions, if there are no standardised ways of ensuring these are reviewed.
In summary, problems with communication cause harm to patients, these failures could be controlled by increased use of structured methods of communication, for example, checklists and more formal handover processes.
Acknowledgements
We would like to acknowledge the members of staff from the critical care units throughout the North West of England who were involved in highlighting, documenting and investigating the reported incidents described in this review and the help of those staff who helped in the classification and collection of the patient safety incidents.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.National Patient Safety Agency. What is a patient safety incident? http://www.npsa.nhs.uk/nrls/reporting/what-is-a-patient-safety-incident/ (accessed 5 October 2015).
- 2.Thomas AN. Resources supporting the implementation of a classification system for patient safety incidents 2010–13, http://www.gmccn.org.uk/patient-safety-review (accessed 5 October 2015).
- 3.Department of Health (Information Standards Board). Data set change notice: 02/2005. Critical care minimum data set. London: Department of Health (Information Standards Board), 2005.
- 4.Tramer MR, Moore RA, Reynolds DJM, et al. Quantitative estimation of rare adverse events which follow a biological progression: a new model applied to chronic NSAID use. Pain 2000; 85: 169–182. [DOI] [PubMed] [Google Scholar]
- 5.Naessens JM, Campbell CR, Huddleston JM, et al. A comparison of hospital adverse events identified by three widely used detection methods. Int J Qual Health Care 2009; 21: 301–307. [DOI] [PubMed] [Google Scholar]
- 6.Segall N, Bonifacio AS, Schroeder RA, et al. Can we make postoperative patient handovers safer? A systematic review of the literature. Anesth Analg 2012; 115: 102–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scheunemann LP, McDevitt M, Carson SS, et al. Randomized controlled trials of interventions to improve communication in intensive care. Chest 2011; 139: 543–554. [DOI] [PubMed] [Google Scholar]
- 8.van Sluisveld N, Hesselink G, van der Hoeven JG, et al. Improving clinical handover between intensive care unit and general ward professionals at intensive care unit discharge. Intensive Care Med 2015; 41: 589–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.LeSage P, Dyar JT, Evans B. Crew resource management: principles and practice, Sudbury, MA: Jones and Bartlett Learning, 2009. [Google Scholar]
- 10.Key statistics from the Case Mix Programme 2012/2013, London, UK: ICNARC, 2014. [Google Scholar]
- 11.Brunsveld-Reinders AH, Arbous MS, Kuiper SG, et al. A comprehensive method to develop a checklist to increase safety of intra-hospital transport of critically ill patients. Crit Care 2015; 19: 214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Academy of Medical Royal Colleges: guidance for taking responsibility: accountable clinicians and informed patients, http://www.aomrc.org.uk/images/dmdocuments/aomrc_papers_takingresponsibility_final.pdf (accessed 5 October 2015).