Abstract
Purpose
This survey investigated current practice in intensive care unit radiology reporting using a survey tool. We ascertained physician attitudes regarding best practice.
Methods
A national survey was sent by email to a sample of intensive care units throughout UK between March and October 2014. The questionnaire determined current practice in reporting chest X-ray in intensive care units. It also identified differences between ‘routine’ and emergency and out-of-hours service. Further, it investigated how reports were documented and physician preferences for perceived best practice.
Results
Of 146 intensive care units contacted, 55% completed the survey. Of the sample, radiologists were solely responsible for chest X-ray reporting in 43.7%, intensive care unit clinicians in 33.7% and joint reporting in 25% of intensive care units. The reporting clinician on intensive care unit was a consultant in 67% of the centres. Written reports by radiologists were provided in 71.7% of cases. This was only 54.5% when intensive care unit clinicians reported chest X-rays. For all routine and emergency films, written reports by radiologists occurred in 63.1% of responders. Out-of-hours, 54.9% of clinicians described different reporting practice to normal hours. Regarding perceived best practice, 64.8% of clinicians preferred joint daily reporting, whilst 27% preferred a radiologist’s formal report. For emergencies, 55.2% of the survey recipients preferred a joint report.
Conclusion
Based on this cohort of UK intensive care units, at present, there appears to be a lack of a standardised system for image reporting. There are discrepancies in who reports chest X-rays, written documentation and the timing of reports, more so out-of-hours. Clinicians suggest that joint reporting should be the standard.
Keywords: Chest radiograph, X-ray in ICU, image-reporting system in ICUs in UK
Introduction
Chest radiography (or chest X-ray, CXR) is an integral part of the initial assessment and daily review of critically ill patients. Sudden clinical deterioration often requires prompt, accurate, identification of critical radiological abnormalities that may require necessary intervention.
Conversely, misinterpretation or missed diagnosis could lead to delayed or inappropriate and potentially harmful treatment, exposing the critically ill patient to further risk of deterioration. Therefore, accurate and timely radiograph reporting are essential requirements.
Since the advent of Picture Archiving and Communication System (PACS), there has been a major change in the way radiographs are processed and reported. Anecdotal evidence indicates the benefits of daily rounds involving radiologists and intensivists as part of the intensive care unit (ICU) routine, allowing abnormalities to be detected early, problems to be shared and imaging solutions to be implemented. In UK, there currently exists no standardised system for reporting ICU CXRs.
Some units rely exclusively on radiologists for reporting, whereas on other units, ICU clinicians are solely responsible for CXR reporting. A small number of centres run a daily joint radiology/ICU multidisciplinary team (MDT) meeting, where radiographs are interpreted together and subsequently reports are generated.1
Doctors working in intensive care often come from different specialty backgrounds and are at various levels in their training and hence diagnostic competencies.
This survey arose as a result of a number of drivers, following extensive discussion regarding practice around UK and abroad, anecdotally (S Singh, personal communication). First, through clinical case reviews, where patients became acutely unwell and in retrospect, management was delayed due to either lack of utilisation of CXRs or inadequate/untimely interpretation of CXRs on the ICU. Second, that ICU CXRs were often being reported and recorded in the radiology department with few clinical details of progress, and that ICUs did not review the written reports. Third, a previous national survey in 2007 had suggested that pre- and post-PACS joint reporting frequency remained at <10% of ICUs (S Singh, personal, communication). Fourth, a lack of structure for reading and recording the ICU CXRs amongst trainees and senior ICU clinicians was apparent. It was therefore considered important to address these concerns on a larger scale. Thus, we sought to investigate current national practice in radiology reporting by surveying a sample of UK ICUs. We also determined prevailing attitudes with regard to perceived best practice in ICU CXR reporting.
The primary outcome was the description of current practice used to report ICU CXR films in the ICU cohort. Secondary outcomes were to identify discrepancies in the modality used to report ‘routine’ and emergency CXR films and out-of-hours practice. Participants were asked to provide information regarding the modality (i.e. verbal, written or electronic) used to document the report. Clinicians were also asked to comment on their preferred reporting system.
Methods
A survey was conducted between March and October 2014. The CHERRIES checklist was followed as best practice for electronically conducted surveys.1 The CHERRIES format focuses on web-based surveys but is also valid for surveys administered via email.
The survey was not advertised. It was a ‘closed’ survey sent by email. The questionnaire was administered online using the survey tool provided by Survey Monkey.2 The target study population were ICU clinicians (lead clinicians, senior consultants or clinical directors) working across ICUs in UK. A mixed-methodology was used to recruit participants. First, a list of ICUs across UK was identified online. The senior consultant email address was then obtained either via telephone or Internet search. Recruitment was often challenging due to privacy and confidentiality rules that do not allow easy release of email addresses.
Senior consultants working on adult ICU in UK were eligible for inclusion in the survey. Trainees, senior registrars, clinical fellows, clinicians working in paediatric ICU, short-term contract staff or clinicians that opted out of Survey Monkey were excluded from this study.
A questionnaire (Appendix) was sent to 146 ICUs in UK. If the first clinician contacted from a centre did not respond, a reminder email was sent twice. If the recipient did not respond, their details and email address were investigated to confirm the recipient was still working in intensive care and there was no mistake in the email address or spelling. Incorrect email addresses were updated and invitation emails were re-sent where possible. Some of the recipients were no longer in their positions; therefore, another clinician was identified within the same institution and survey was sent.
Responses were automatically captured in the Survey Monkey database and also entered manually into an excel database. No incentives were offered.
Consent
Respondents who accepted the invitation to take part in the study, and used the link provided to access the survey web page, were taken to the survey introductory page. Here, the participants were provided with information about the project, an outline of what participants were required to do and how long it will take to complete the questions, an assurance that every attempt will be made to maintain the confidentiality of the data and a statement indicating that participation is voluntary and that withdrawal from the survey is possible at any stage. Potential participants were asked to click on a link to confirm that they have read the participant information before proceeding. The act of clicking on this link was considered consent to participate in the study. Only the research team at Chelsea and Westminster Hospital had access to the data.
Results
Characteristics of participants were described for the sample as a whole. Data were collected in an eight months timeframe (March–October 2014). No adaptive questioning was applied.1 The number of survey items investigated was 17. The selection of response option was enforced by the option ‘Not Applicable’ in selected questions. Duplicate entries were avoided. The survey was never displayed a second time once the users had filled it in. No statistical correction was applied.
The participation rate was 80/146 (55%). Of responders, 17.5% were head of the department, 27.5% were lead clinician and 55% ICU consultant.
Regarding the type of ICU the recipients were working in: 92.5% worked in a General Medico-surgical ICU, 16.2% in a Trauma ICU, 12.5% in Cardiac ICU, 10% Burns ICU, 11% Neuro ICU and 12% other (total >100% on account of the multidisciplinary nature of 20% of the ICUs). All units had level three beds and level two beds. All responders used PACS.
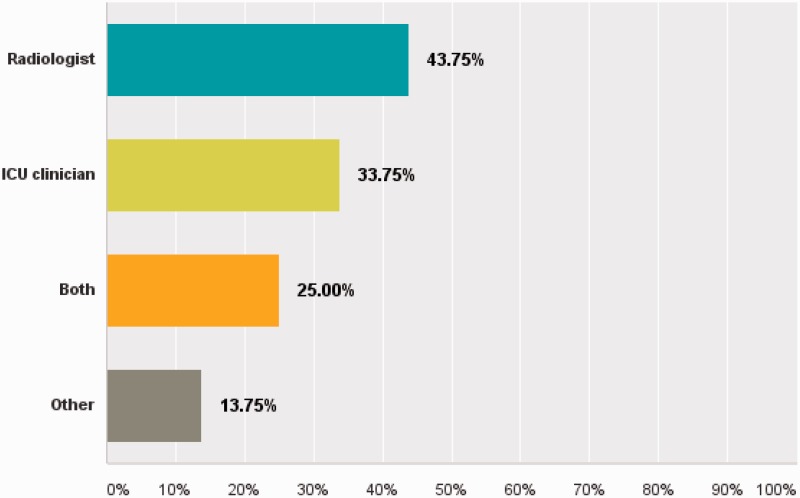
The questionnaire investigated those who reported the daily CXR (Figure 1). Radiologists were solely responsible for 43.7% of CXR reporting, ICU clinicians were solely responsible for 33.7%, and 25% of respondents confirmed joint reporting (total > 100% on account of the non-standardised system and variability according to daytime, weekends and out-of-hours practice). The option ‘other’ was also given to encourage recipients to respond to the question and elaborate their answers as free text.
Figure 1.
How are chest radiographs reported in your unit? The radiologist report only 43.7%, ICM clinician reports 33.7% and in 25% of the units, CXRs are reported from both in daily meeting/joint report; 13.7% of the responders elaborated their choice (as explained in the text) in the descriptive text box ‘other’.
13.5% of the responders selected the option ‘other’ and expressed comments such as ‘not usually reported’, ‘clinicians look at them but do not formally report them’, ‘largely unreported but interpreted by ICU clinicians’, ‘personal discussion with radiologist as required’, ‘very variable, sometimes never reported’.
With regard to the question about the timing of the CXR report (i.e. end of ward rounds, lunch time), 94.4% of the responders stated that the reporting did not happen at a fixed time.
When the reporting person was identified as the Intensive Care Medicine (ICM) clinician, 67.2% of the responders stated that the reporting clinician was a consultant. It was stated that 36% of the units (where ICM clinicians were responsible of reporting ICM) allowed trainees to report CXRs.
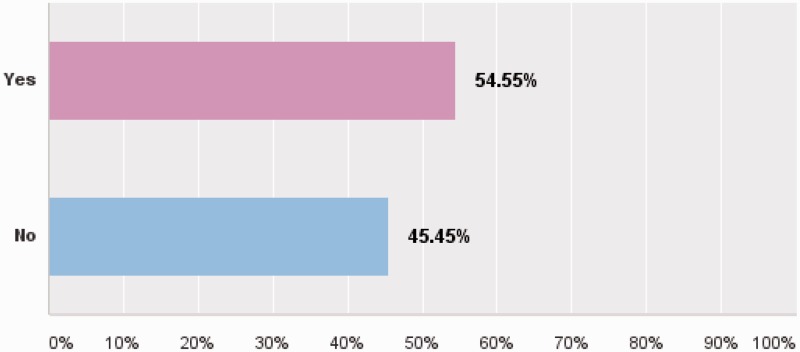
The modality of documentation of the CXR report was also investigated (Figure 2). Where ICU clinicians were responsible for reporting, only 54.5% documented the reports in the patient’s medical notes.
Figure 2.
If reported by ICM clinician, is a report of the radiograph recorded in the patient’s notes? 54.5% say ‘yes’ and 45.4% say ‘no’.
When reported by radiologists, written reports were provided on PACS in 71.7% of units. Also 16.6% of these radiologists (responsible for reporting) were said to have phoned to communicate critical findings.
Only 22.7% of the units were said to have a MDT meeting with radiologist and ICM clinicians (and only 3% daily). In units where radiologists were responsible for reporting, the practice of reporting routine and emergency films occurred in 63.1% of responders.
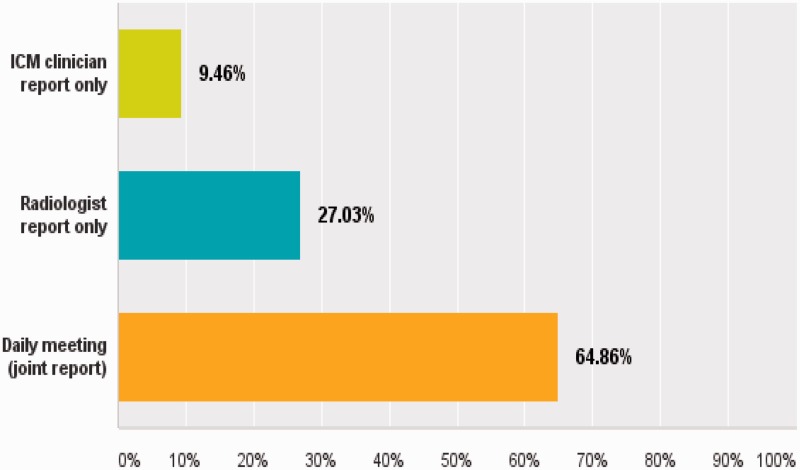
Out-of-hours, 54.9% of clinicians described different reporting practice to normal hours. In consideration of perceived ideal standards (Figure 3), 64.8% of clinicians believed that the reporting routine films would be best provided by a joint daily meeting; 27% of clinicians preferred a radiologist’s formal report. Only 9% of the responders opted for an ICM clinician report only.
Figure 3.
What do you think should be the best practice in reporting routine films? 9.4% choose ICM clinician report only, 27% radiologist report only and 64.8% daily meeting/joint report.
In the setting of emergencies, 55.2% of the survey recipients preferred a joint report, 32.8% radiologist report only and 11.8% ICM clinician only.
Discussion
In the experience of the authors, joint radiology reporting rounds frequently highlight abnormalities that require active management and would have been otherwise missed.
For example, the misdiagnoses of an opaque hemi thorax as a large pleural effusion, missing the signs that indicate the presence of complete lung collapse. This misinterpretation was by multiple staff members (with different backgrounds and levels of training). A senior clinician on review, correctly interpreted the findings, undertook thoracic ultrasound, ruling out significant effusion and so instigated a bronchoscopy instead of pleural drainage.
A second example is a missed ‘deep sulcus sign’ on sequential CXRs. This patient deteriorated overnight and the cause of the deterioration was thought to be sepsis. Later in the night, echocardiogram changes appeared, and acute myocardial infection was taken into consideration. After subsequent reviews, computed-tomography (CT) scan of the chest detected an anterior pneumothorax, necessitating insertion of a CT-guided pleural drain. Although patient eventually received the appropriate treatment, adequate CXRs reporting, with a level of reporting experience, may have allowed earlier treatment and reduced the risk of life-threatening complications. Of course, not all non-urgent CXR reporting leads to changes in clinical management, and some may argue that its value in regard to clinical decisions is overvalued. However, when considered from the aspect of good process-of-care, a standardised approach to interpretation and reporting should be considered best practice. The analogy of standard reporting of echocardiography on most ICU provides precedence for the suggested need in CXR reporting on ICU.
Survey Monkey has been successfully used in published research, as described in detail by Dobrow et al.2
To avoid bias, resulting from a non-representative nature of the Internet population and the self-selection of participants, we identified online a sample of ICUs and addressed the survey to the senior person in the unit in the first instance. In doing so, the survey remained ‘closed’.1
With regard to the results, this survey reinforced the hypothesis that there is a discrepancy in the system used to report ICU CXRs in UK.
The questionnaire contained items with open text options. Some recipients expressed concerns regarding the reporting system and the documentation of the reports.
The main concern was the delay in reporting the CXRs.
Typical comments included
‘… the delay could be from 1–2 days to several days’,
‘largely unreported but interpreted by ICU clinicians’,
‘very variable, sometimes never reported’,
‘not usually reported’,
‘reviewed by ICU clinician but no official report’.
In regard to the documentation of the report, some of the clinicians stated that often
‘No formal reporting. Will write something in the notes’,
‘Not formally reported on paper’.
When investigating whether the same service of radiologist reported films was used for routine and emergency films, discrepancies were identified once again.
Some commented on the definition of ‘routine’ CXR. For the present study, ‘routine’ was defined as any CXR not done in an emergency setting and guided by the clinical condition.
One of the responders highlighted that
‘a significant proportion of chest films are performed for position checking of lines/tubes and are rarely diagnostic in other respects in an ITU setting (but can give a gauge of the extent of any lung disease/injury and are useful in diagnosis of collapses/pneumothoraxes etc). Does this require consultant-level radiology input?’
Once more, clinicians expressed concerns and pitfalls that might need to be formally addressed.
The survey items that investigated the out-of-hours practice described concerns due to
‘Outsourcing of reporting out-of-hours and therefore limited opportunity to discuss findings’;
‘Emergency CXRs are only reported immediately in the trauma setting. All other CXR are sent for generic reporting which can take weeks’;
‘All films (routine and emergency) reported in daily weekday meeting but no out-of-hours reporting occurs’;
Some of the clinicians stated that ‘At night an agency is used, emergency CTs are reported immediately, CXR are still reported by ICU clinicians’;
‘Night hawk out-of-hours service. No on-call PAs in radiologist job plans’.
The joint reporting of CXRs in ICU between radiologist and intensivists may be reasonably considered a gold standard practice. It allows patient-centred, multidisciplinary specialist interaction, with a potentially important educational training opportunity (although that was not addressed in this survey). The findings suggested a low percentage (25%) of ICU with joint reporting.
This survey should raise awareness of the lack of standardised current practice in reporting ICU CXRs in UK. This warrants further investigation if improved process of care is desirable, as part of improved service and educational provision. The lack of a formal written report is also noted. This would not be the case if, for instance echocardiograms, or electroencephalography, were requested for patients on ICU.
If ICM clinicians are to increasingly become the reporting operators, further training and perhaps standardised reporting templates should be considered. Our impression is that ICU clinicians suggest a joint review system involving both radiologist and intensivist, perhaps using a telemedicine tool or face-to-face daily meetings should be the gold standard, with notes documentation at the time, and subsequent radiology reports being generated and recorded on the PACS system. The standard of review by ICU clinicians might improve with regular joint reporting due to the educational benefit for junior and senior staff. The joint daily meeting could support ICM clinicians in developing a systematic approach in CXR reporting. Perhaps most importantly, the requirement and scheduling of CT and ultrasound investigations, prompted by the radiology review, could then be arranged in a timely manner. Indeed in the experience of one author (SP), this approach of shared interpretation and co-operative problem solving usually results in one or two additional imaging investigations each day, which are then reviewed at the next joint interpretation daily meeting. There are a number of challenges to best practice, and the lack of formal reporting and review structures revealed by this survey highlight the difficulties that will need to be overcome to institute daily joint radiology review seven days per week.
Conclusion
Based on this cohort of UK ICUs, at present, there appears to be inconsistency and a lack of a standardised CXR image reporting system. This warrants further study. Notably, there remains a low level of joint reporting.
Joint reporting may provide an incentive for radiologists and intensivists to incorporate joint working practice to mutual service and training benefit. Alternatively, more formal training in radiology reporting for intensivists could be developed.
Acknowledgements
We thank all the doctors that took time out of their busy schedules to complete the survey. We would also like to thank Dr S Patel, T Pirani and J Martin for helping with the contact list.
Appendix. Questionnaire
| Survey items | ||
|---|---|---|
| Which hospital is your ITU based at? | ||
| What is your job role? | ||
| Which types of beds are available? | General/Cardiac/Trauma/Burn/Neuro/Other | |
| How many beds are available on your unit? | Level 2/Level 3 | |
| Do you use PACS(Picture archiving and communication system)? | Yes/No | If no, please abandon survey |
| How are CXR reported in your unit? | Radiologist/ ICU clinician/Both | Other (please specify) |
| If CXRs are reported by an ICU clinician, does this happen at a fixed time (i.e. end of ward rounds, lunch time)? | Yes/No | |
| Is the reporting clinician on ICU a consultant? | Yes/No | |
| If the ICU reporting doctor is in training, which is the required grade? | FY1/FY2/CT/SHO ST/SPR/ST6/ICM/ADV/Trainee/SR | Not applicable |
| If reported by ICM clinician, is a report of the radiograph recorded in the patient’s notes? | Yes/No/Other | |
| If the chest radiographs are reported by radiologists, do the radiologists | Come to the unit to report the chest radiographs/Phone to communicate findings/Phone to communicate only critical findings/Write report on PACS/Not applicable | |
| Do you have a regular MDT meeting with ICU clinicians and radiologists to discuss chest radiographs? | Yes/No | |
| If Yes, how often does this happen? | Daily/Weekly/Variable | Not applicable |
| Is the same service of radiologist reported films used for routine and emergency films? | Yes/No | Other (please specify) |
| Is the same service of radiologist reported films available at weekends and nights? | Yes/No | Other (please specify) |
| What do you think should be the best practice in reporting routine films? | ICM clinician report only/Radiologist report only/Daily meeting (joint report) | Other |
| What do you think should be the best practice in reporting emergency films? | ICM clinician report only/Radiologist report only/Joint report | Other |
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Eysenbach G. Improving the quality of Web surveys: the checklist for reporting results of Internet E-surveys (CHERRIES). J Med Internet Res 2004; 6: e34 . DOI: 10.2196/jmir.6.3.e34. http://www.jmir.org/2004/3/e34/v6e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dobrow MJ, Orchard MC, Golden B, et al. Response audit of an Internet survey of health care providers and administrators: implications for determination of response rate. J Med Internet Res 2008; 10: e30. [DOI] [PMC free article] [PubMed] [Google Scholar]