Abstract
Relapsing fever spirochetes are tick- and louse-borne pathogens that primarily afflict those in impoverished countries. Historically the pathogens have had a significant impact on public health, yet currently they are often overlooked because of the nonspecific display of disease. In this review, we discuss aspects of relapsing fever (RF) spirochete pathogenesis including the: (1) clinical manifestation of disease; (2) ability to diagnose pathogen exposure; (3) the pathogen’s life cycle in the tick and mammal; and (4) ecological factors contributing to the maintenance of RF spirochetes in nature.
Keywords: relapsing fever spirochetes, Borrelia, Ornithodoros, argasid, ixodid
1. Introduction
Relapsing fever (RF) spirochetes are a significant cause of disease on five of seven continents, and are transmitted by argasid and ixodid ticks, and the human body louse. The pathogens are categorized as endemic (tick-borne) or epidemic (louse-borne), and all but two species (Borrelia recurrentis and Borrelia duttonii) are maintained in enzootic cycles with humans as accidental hosts [1,2]. In regions of Africa, the ecology and epidemiology of RF spirochetes have been extensively studied and the pathogens are a significant cause of child morbidity and mortality [3,4,5,6,7,8,9,10,11]. Outside of the African continent less is known regarding how RF spirochetes are maintained in nature.
This review primarily examines the ecology of tick-borne RF spirochetes in the Americas, with a focus on argasid-borne RF (ABRF). Moreover, since the epidemiology of ABRF in North America has been comprehensively reviewed [12,13,14,15] and little attention has been given to Latin America, in addition to the disease’s ecology our review also highlights epidemiological findings and case reports from Central and South America. We also review studies on Borrelia miyamotoi, an ixodid-borne RF (IBRF) species transmitted by Ixodes species, which was recently recognized to cause human disease [16]. While the last decade has resulted in a better understanding of how RF spirochetes are maintained in a tick-mammalian transmission cycle, there are deficiencies that remain and should be addressed. We conclude our review by addressing these critical questions and suggest actions suitable for progress in our understanding of ABRF and IBRF in the Americas.
2. Clinical Manifestation of Disease
In humans, ABRF presents with an onset of fever (104–107 °F) within four to 18 days after tick bite [17]. Acute disease is complemented with myalgia, headache, chills, diaphoresis, anorexia, nausea, and vomiting [14]. Febrile episodes may last three to four days, and are followed by an afebrile period of up to 10 days [14]. The cyclic nature of disease can continue for months if left untreated [17,18], and is due to antigenic variation [19]. An antibody response is generated against the predominant variable membrane protein (Vmp) produced on the surface of members within the spirochete population, resulting in pathogen clearance. However, the spirochetes switch to produce a Vmp variant that is not recognized by the host immune response, and a new population of spirochetes emerges in the blood [20,21].
Uncommon, yet severe, clinical manifestations of disease are associated with the systemic nature of the circulating ABRF spirochetes. Patients may develop acute respiratory distress, characterized by bilateral infiltrates and rales on chest X-rays [22]. Central nervous system involvement, including nuchal rigidity, facial paresis, vertigo, positive Kernig’s sign, and myocarditis has been noted [14]. Hepatosplenomegaly is palpable on physical examination, with an elevation of liver enzymes [14]. Cardiac involvement has been rarely reported, with electrocardiographic conduction delays and depression in ejection fraction on echocardiography being observed [23,24]. In the event of pregnancy, transplacental transmission can result in miscarriage [25].
RF spirochetes are susceptible to broad-spectrum antibiotics [14]. However, upon treatment 54% of ABRF patients had a Jarisch-Herxheimer reaction [12], which is characterized by a profound deterioration of symptoms including a sudden onset of fever, tachycardia and tachypnea, and blood pressure [26]. This pathophysiology results from a massive release of tumor necrosis factor by macrophages and is induced by spirochete surface lipoproteins [27].
As a recently recognized human pathogen, the clinical presentation of B. miyamotoi is less severe than ABRF. The spirochetes are neurotropic and can be detected in the cerebrospinal fluid of those displaying symptoms of meningoencephalitis [28]. Patients also present with headache, fever, chills, fatigue [29,30,31]. Although B. miyamotoi possess homologues for Vmps [32], it is unclear whether the pathogens undergo antigenic variation, and the number of relapses in the host is poorly understood.
3. Diagnosis of Exposure to RF Spirochetes
Currently there are no commercial diagnostic tests available for RF spirochetes, with national reference laboratories or academic laboratories providing detection capacities. Two primary methods of evaluating mammalian exposure are microscopy and molecular assays. RF spirochetes attain high densities in mammalian blood, at which point the pathogens can be visualized by dark field microscopy or Giemsa stained thin smears (Figure 1). While high bacterial loads in the blood are associated with fever, accurate diagnosis between febrile episodes is challenging because the pathogens are below the limit of detection [33]. During the course of infection as an antibody response is generated against RF spirochetes, molecular diagnostic assays are an alternative method to confirm mammalian exposure.
Figure 1.
Giemsa-stained peripheral blood smear of a mouse infected by tick bite with Borrelia turicatae. The black bar represents 10 µm.
With the ecological overlap between RF and Lyme disease causing spirochetes, antigenic conservation between species, and observed serological cross-reactivity, identification of diagnostic antigens unique for a given disease group is important. The first diagnostic antigen discovered for RF spirochetes was glycerophosphodiester phosphodiesterase Q (GlpQ) [34]. A homologue of glpQ is absent from B. burgdorferi and the recombinant protein can discriminate between infections caused by RF and Lyme disease causing spirochetes [34]. Moreover, the protein may be used to diagnose early infection as IgM responses to recombinant GlpQ was detected in a cohort of infected patients from Ethiopia within four days after infection [35]. GlpQ also contains highly-conserved serologically cross-reactive epitopes between Old and New World species of RF Borrelia [36,37]. This is important when determining mammalian exposure in regions of the globe where it is unknown if RF spirochetes are circulating in nature.
A more recently discovered diagnostic antigen is the Borrelia immunogenic protein A (BipA). An immunoproteomic approach identified BipA as antigenic using serum samples from human patients and infected mice [35]. Similar to GlpQ, a BipA homologue is absent from Leptospira and Lyme disease-causing spirochetes [38]. BipA may also be a species specific antigen for RF spirochetes as the protein is highly divergent between species of RF spirochetes [39]. For example, serological responses from a canine and rodents experimentally infected by tick bite with B. turicatae failed to cross-react with recombinant BipA that originated from B. hermsii [39]. Currently, recombinant GlpQ and BipA offer the most thorough opportunity of accurate serodiagnosis of RF spirochetes.
4. The Life Cycle of ABRF Spirochetes in the Mammal
Species of RF spirochetes circulate in an infectious cycle between the mammalian host and argasid or ixodid ticks. Salient differences between the biology of the two tick vectors are summarized in Table 1 [1,40,41], and ABRF and IBRF spirochetes have likely evolved unique mechanisms for vector colonization and mammalian infection. Currently, the life cycle of ABRF spirochetes within the mammal and tick is more defined than IBRF spirochetes (B. miyamotoi), and will be further reviewed.
Table 1.
Biological differences between Ixodes and Ornithodros species.
| Biological Traits | Ixodes spp. | Ornithodoros spp. |
|---|---|---|
| Life span | 2–3 years | 5–20 years |
| Nymphal stages | 1 | >7 |
| Feeding strategy | Questing/Nidicolous A | Nidicolous |
| Feeding duration | 5–7 days | 5–60 min |
| Transmission | unknown | ~15 s B |
A Nidicolous-cavity, nest, or den dwelling; B Transmission of Borrelia turicatae.
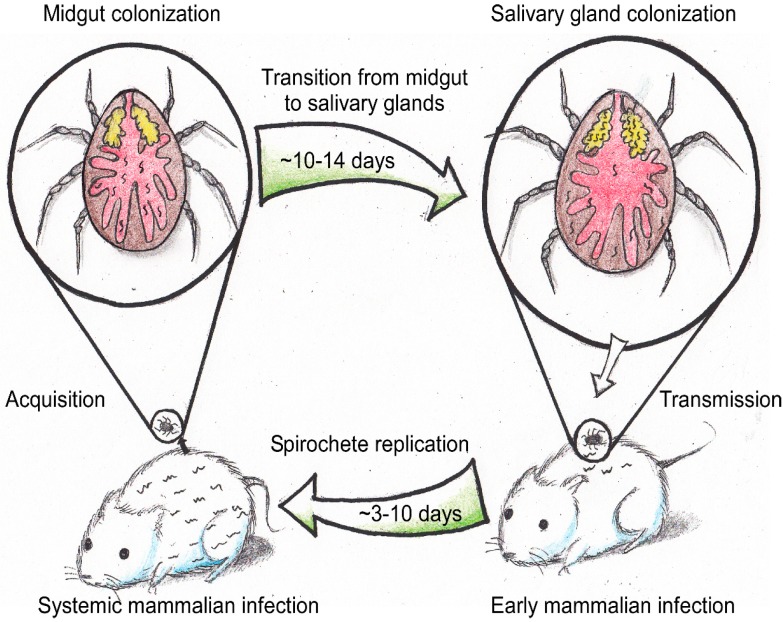
Transmission studies indicate that ABRF spirochetes are likely preadapted in the tick for mammalian entry. While the infectious dose delivered through the tick saliva remains unknown, the observed rapid transmission of Borrelia turicatae within 15 s of tick bite [42] indicates that the subsets of spirochetes preadapted to survive innate immunity will continue their life cycle in the mammal. For example, work by Woodman and Alugupalli demonstrated the importance of macrophages, dendritic cells, and B1 B cells (innate-like B cells) in controlling RF spirochete infection [43,44]. However, during the first three to five days after transmission ABRF spirochetes also replicate. Therefore, early infection is characterized by an interplay between innate immunity and spirochete propagation (Figure 2).
Figure 2.
The tick-mammalian transmission cycle of ABRF spirochetes. In the tick, the salivary gland population of RF spirochetes is essential for mammalian infection because of the rapid feeding behavior of the tick. Entry into the mammal is characterized by early infection, and the pathogens are likely preadapted to evade innate immunity. During the following three to 10 days, RF spirochetes subvert the host antibody response leading to systemic infections. This phase of the pathogen’s life cycle is characterized by evasion of the host antibody response through antigenic variation, and replication to densities upwards of 1 × 107 spirochetes per milliliter of blood. During an acquisition bloodmeal, RF spirochetes enter and colonize the midgut. Within 10–14 days a population exits the midgut and migrates to colonize the salivary glands, completing the life cycle of the spirochetes in the argasid tick vector.
The transition from early infection to systemic infection (Figure 2) is characterized by the upregulation of the expression locus involved with antigenic variation [45]. The pathogens replicate to high densities in the blood, and infection is cyclic with antigenic variation as the driving force to ensure the spirochetes continue their life cycle [19,46]. For example, the inability of Ornithodoros hermsi to become colonized by Borrelia hermsii while feeding on an infected animal between relapses indicated the significance of antigenic variation in providing multiple opportunities for vector acquisition [47].
The number of spirochete relapses in a competent mammalian host was recently modeled in the O. hermsi-B. hermsii system to predict factors required to keep a community endemic [48]. Johnson and colleagues conducted field studies in a unique ecological setting on Wild Horse Island, Flathead Lake, Lake County, MT, USA. The island is endemic with B. hermsii and exclusively inhabited by deer mice (Peromyscus maniculatus) and pine squirrels (Tamiasciurus hudsonicus) [48,49]. These factors provided an opportunity to develop a single and coupled host-vector model to determine the number of relapses predicted for the island to remain endemic, with R0 > 1 indicating endemicity and R0 < 1 is a disease-free equilibrium. In the single host system where pine squirrels are known to maintain B. hermsii, R0 > 1 was observed at four relapses. Interestingly, in a coupled host-vector system that included incompetent deer mouse, seven relapses within pine squirrels were predicted to be required in order to produce an R0 > 1. These studies established a framework for understanding additional RF spirochete systems, and demonstrate the importance of defining the dynamics of mammalian host competency with keeping a community endemic.
5. The Life Cycle of ABRF Spirochetes in the Tick Vector
During an infectious bloodmeal, RF spirochetes enter the midgut (Figure 2). Although the precise infectious dose required for Ornithodoros colonization remains unclear, studies with the B. hermsii-O. hermsi model suggested that as few as 30 spirochetes were sufficient to successfully infect ticks [33,47]. Cohorts of second nymphal O. hermsi were fed for 13 consecutive days on an infected mouse, which spanned two spirochetemic episodes [47]. Estimating the bloodmeal volume for second stage nymphs indicated that they imbibed ~30 spirochetes [33,47], with 50% of the ticks becoming colonized by B. hermsii [47].
After feeding, the midgut serves as the first site of RF spirochete adaptation. Nakajima and coworkers reported that during the bloodmeal the antimicrobial peptides, defensin A and B, were upregulated in Ornithodoros moubata [50,51,52], suggesting that RF spirochetes likely evolved mechanisms to subvert vector immunity. In the following 10 to 14 days after feeding, a population of spirochetes exit the midgut and begin to colonize salivary glands (Figure 2). During migration through the hemocoel and within the salivary glands, ABRF spirochetes continue to face immunological pressures [50,53,54]. Transcriptional and proteomic studies of O. parkeri identified the production antimicrobial peptides in the salivary glands [54], and indicated that the tissues are another environment exerting immunological pressures on RF spirochetes. Thus, in a persistently-infected tick two populations must adapt to vector immunity, those in the midgut and others in the salivary glands [55].
ABRF spirochete transmission occurs within seconds of tick bite [42,56], and the salivary gland population is essential to continue the spirochetes’ life cycle in the mammal. The rapidity of ABRF spirochete transmission indicates that the pathogens are preadapted for mammalian entry [42,46]. Raffel and colleagues demonstrated this by deleting the B. hermsii variable tick protein, which the spirochetes predominantly produce in the tick salivary glands [45]. Inactivating the gene resulted in a noninfectious phenotype after tick bite [46]. Interestingly, the mutant’s ability to colonize O. hermsi salivary glands demonstrated the importance of the protein during early mammalian infection.
Transcriptional assessment of B. turicatae indicated that large linear megaplasmids of RF spirochetes likely play important roles in the vector and preadapting the pathogens for mammalian entry [57]. Over 60% of open reading frames (ORFs) on the megaplasmid were upregulated during in vitro cultivation at a temperature mimicking the tick environment. A cluster of ORFs localized toward the 3’ end was further evaluated in cohorts of O. turicata, which confirmed the genes’ upregulation in the tick [57]. As these proteins are characterized, subsets will likely be identified that are important for midgut and salivary gland colonization, while others may preadapt the spirochetes to evade the selective pressures encountered during early mammalian infection.
A defining characteristic of ABRF spirochete-Ornithodoros interactions is vector specificity [1,58,59]. For example, O. hermsi, O. parkeri, and O. turicata transmit B. hermsii, B. parkeri, and B. turicatae, respectively. While the mechanism is still unknown, the salivary glands may be the restricted environment. Work by Schwan demonstrated that B. hermsii colonized and disseminated from the midgut of O. hermsi, O. parkeri, and O. turicata; however, only O. hermsii subsequently transmitted the pathogens to mice [60]. As the field of transcriptomics has emerged, the determination of salivary gland gene expression from Ornithodoros species is feasible, and defining the intricacies of vector colonization is promising.
6. Ecology of ABRF in North America
In North America, the Ornithodoros vectors for ABRF spirochetes are distributed in endemic foci in Western Canada and the United States, across the southern portion of the country into Mexico [40]. There are four likely argasid tick vectors of RF spirochetes that cause human disease, Ornithodoros parkeri, Ornithodoros hermsi, Ornithodoros turicata, and Ornithodoros talaje, which transmit B. parkeri, B. hermsii, B. turicatae, and B. mazzottii, respectively. Ixodes scapularis and Ixodes pacificus transmit B. miyamotoi, the species of IBRF spirochetes, and the ticks are found in the Western and Northeastern United States [61,62,63]. Since the ecology of Ixodes species has been well described [64], and there is a paucity of information regarding reservoir host competency for B. miyamotoi, we focus the remainder of this review on the ecology of ABRF spirochetes and their vectors.
6.1. O. parkeri-B. parkeri
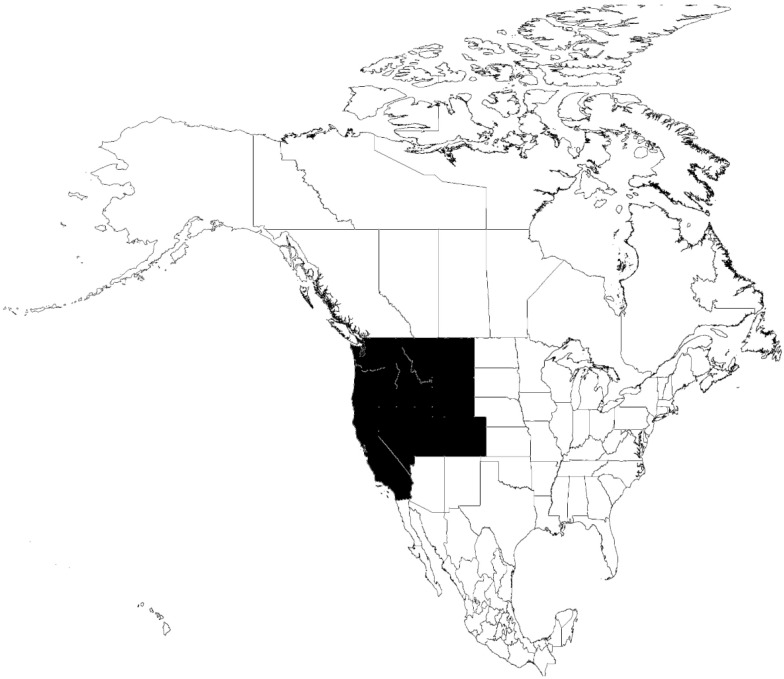
Currently, a human isolate does not exist for B. parkeri, yet the species has been implicated as a possible cause of RF because of tick collections from locations of suspected human exposure [65,66]. These studies date back to 1934, when ticks were obtained within burrows from semi-arid locations at elevations at sea level to over 2000 m [65,66,67]. Burrows were identified throughout the Western United States (Figure 3) in sagebrush and grassy slopes with primary inhabitants of prairie dogs, rabbits, rodents, and owls [66,67]. The ticks are nonselective feeders, engorging off of man, white mice, rats, guinea pigs, and nonhuman primates [66,67]. Furthermore, work by Davis initially reported cannibalism between Ornithodoros ticks, when he observed unfed O. parkeri feeding on engorged ticks, which left the host tick unaffected [66]. These studies suggest that cohorts of fed ticks could continue the life cycle of RF spirochetes within a burrow or nest community by becoming a bloodmeal source to unfed ticks.
Figure 3.
Distribution of Ornithodoros parkeri in North America.
6.2. O. hermsi-B. hermsii
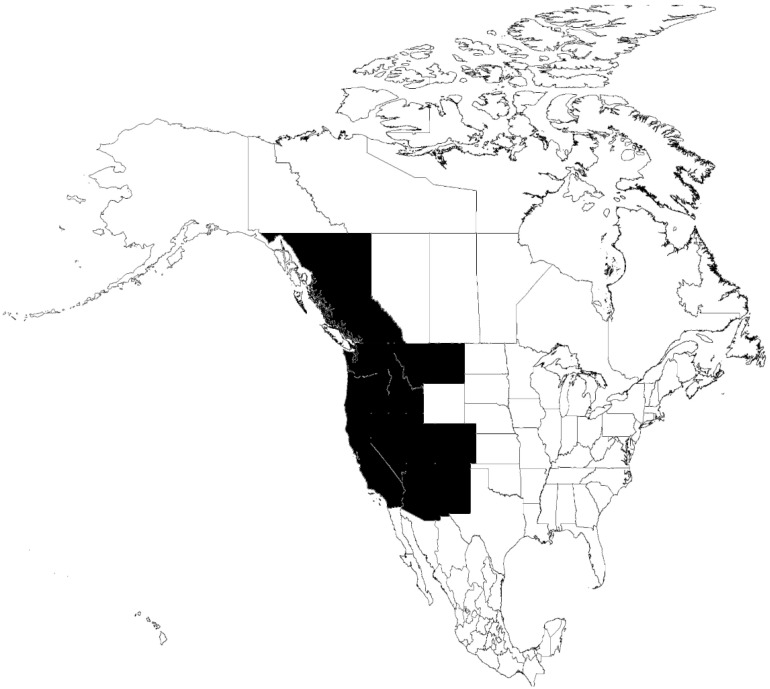
The ecology of B. hermsii and the tick vector is the most studied and defined of the RF spirochete species in the Americas [48,68,69,70]. Throughout the Western United States and Southern British Columbia O. hermsi is distributed above elevations of 900 m [13,40,71] (Figure 4). The spirochetes circulate in enzootic cycles between ticks and rodents, with evidence that woodrats (Neotoma spp.), deer mice (Peromyscus spp.), chipmunks (Tamias spp.), and pine squirrels (Tamiasciurus spp.) are suitable hosts to varying degrees [48,49,68,70,72,73,74].
Figure 4.
Distribution of Ornithodoros hermsi in North America.
Seminal work by Burgdorfer et al. first evaluated vertebrate host competency to B. hermsii [73]. Infection studies by needle inoculation or tick bite were conducted on chipmunks, pine squirrels, flying squirrels, Columbian ground squirrels, golden-mantled ground squirrels, wood rats, white-footed deer mice, and meadow voles. Of these small mammals, B. hermsii only infected pine squirrels, chipmunks, and meadow voles, as determined by microscopic evaluation of blood. However, more recent serological surveillance studies indicated that B. hermsii also propagates in deer mice throughout California [74], indicating that these small mammals are competent reservoirs. Moreover, the study was reported in 1970, and a year later culture medium was developed, to isolate B. hermsii [75]. Consequently, few spirochete isolates existed and it was unknown at the time that B. hermsii separated into two genomic groupings (GGI and GGII) [76]. Repeating the rodent infection studies with GGI and GGII isolates of B. hermsii may expand our understanding on host competency between genomic groups and further clarify the maintenance of B. hermsii in nature.
Evidence is also mounting that migratory birds and large vertebrates are involved in the ecology and dispersal of B. hermsii. The extraction and typing of B. hermsii DNA from the liver of a deceased northern spotted owl suggested that the spirochetes could establish an infection in birds [77,78]. Subsequent identification of identical genotypes of B. hermsii isolated from human patients from Lake Co., Montana and Siskiyou Co., California further indicated a role of migratory animals in spirochete dispersal [76]. The study also reported that chickens and quail support all life cycles of O. hermsi, and that B. hermsii was able to cause spirochetemia after needle inoculating chickens [76]. The ecology of B. hermsii is becoming defined in a forest landscape with terrestrial (chipmunks) and arboreal (squirrels and birds) vertebrates that maintain the pathogens, and squirrels may serve as a bridge for introducing B. hermsii and the vector into migratory bird habitats.
Further evidence that the ecology of B. hermsii may be more complex than a rodent-tick infectious cycle comes from the isolation of the species from a dog and surveillance studies in mule deer [69,79]. B. hermsii was isolated from the blood of a dog in Washington State, which suggests that wild canids may maintain the pathogens [79]. Furthermore, B. hermsii DNA was detected in the blood and lymph nodes of mule deer across Nevada, with seven percent of the animals positive [69]. While O. hermsi is associated within rodent and possibly bird nests [40], Nieto and colleagues pose an interesting scenario for the transmission of B. hermsii by Ornithodros coriaceus, a species primarily identified within leaf litter and deer beds [40]. More studies are warranted to further understand this vector-Borrelia species connection.
6.3. O. turicata-B. turicatae
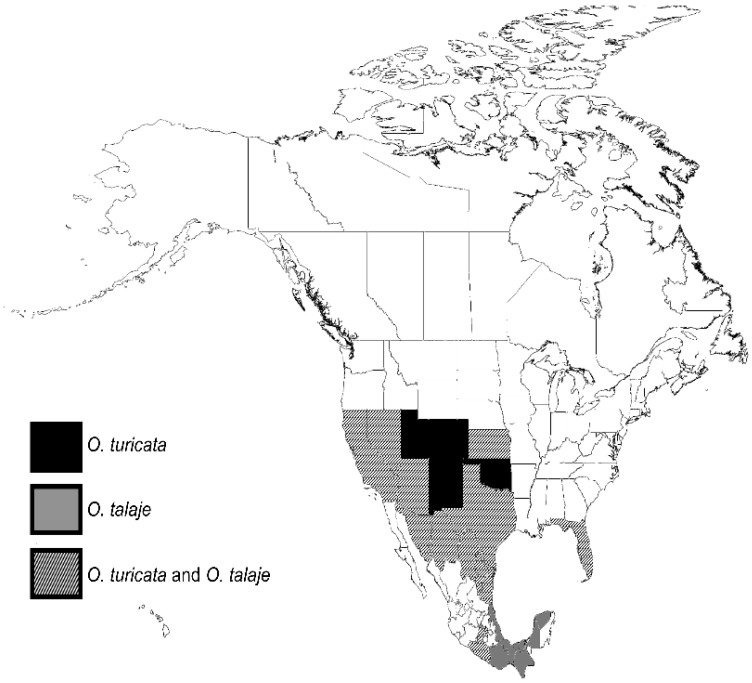
In the Southern United States and Northern Mexico, O. turicata is likely the primary vector of RF spirochetes (Figure 5). Historic reports have described the ticks into Central and South America [80], yet a current understanding of the tick’s distribution remains vague. In the United States, ecological studies of O. turicata have described a western and eastern population of tick, with a geographical gap comprised of Louisiana, Mississippi, and Alabama. O. turicata has consistently been collected from gopher tortoise dens in Florida [81,82,83], while similar field studies throughout Mississippi analyzing arthropod communities of dens failed to recover the ticks [84].
Figure 5.
Distribution of Ornithodoros turicata and Ornithodoros talaje in North America.
The geographical gap between Texas and Florida may be explained by current climate conditions. Utilizing a maximum entropy species distribution model to predict regions where O. turicata circulate, Dondalson and colleagues identified environmental variables that may explain the absence of O. turicata in Louisiana, Mississippi, and Alabama [81]. Low temperatures during the wettest quarter of the year, high temperatures during the driest quarter, and the amount of precipitation in the region during the driest quarter may produce an environment that would not facilitate the establishment of the ticks.
With the two isolated populations of O. turicata, the eastern population has been considered a subspecies [85]. Beck and coworkers proposed that the biological differences and geographic separation warranted the eastern population being designated O. turicata Americanus [85]. Determining vector competency of eastern and western O. turicata populations with isolates of B. turicatae obtained throughout the southern United States is an important step toward understanding pathogen emergence across geographical distances.
Vertebrate host competency for B. turicatae is an additional aspect of infectious disease ecology needing clarity because of the nonselective feeding behavior of O. turicata. Ticks have been collected from a variety of habitats including rodent and burrowing owl nests, coyote and reptile dens, and within caves that are inhabited by a variety of bloodmeal sources [40,81,82,83]. Two likely hosts include rodents and wild canids. Rodents are known hosts for nearly all species of RF spirochete [10,68,72,86,87], and the animals are susceptible to B. turicatae infection by tick bite [39,42]. Evidence for a role of wild canids in the maintenance of B. turicatae comes from the recovery of the species from domestic dogs in Texas and Florida, and laboratory transmission studies with O. turicata [39,88,89].
The biology of O. turicata and dynamics between the vector and B. turicatae facilitate the emergence of the tick and pathogen. O. turicata are promiscuous feeders [40,85,90], and the vector is able to endure at least five years of starvation during which B. turicatae remains infectious upon subsequent feeding [90]. The ticks also maintain B. turicatae transovarially, as first demonstrated by work from Francis after his accidental exposure to two larvae [90]. The resilience of O. turicata, nonselective feeding behavior of the tick, and life cycle of B. turicatae within the vector indicates that the parameters are in place for the emergence of this species of ABRF spirochete.
6.4. O. talaje-B. mazzottii
O. talaje is an understudied vector of RF spirochetes in North, Central, and South America [40] (Figure 5). Transmission studies to humans by Panamanian O. talaje (further detailed below) indicated that the tick is a competent vector of the pathogens [91]. In North America, work by Mazzotti reported the first recovery of a RF spirochete from O. talaje in 1953 from Mexico, and he subsequently sent Dr. Gordon Davis infected ticks to further evaluate [59]. The spirochete was designated Borrelia mazzottii in honor of the researcher’s contribution to the field of RF spirochetes, and the following studies demonstrated vector specificity of this Borrelia strain. O. talaje recovered from Mexico, Guatemala, and Panama, Ornithodoros puertoricensis and Ornithodoros rudis collected in Panama, Colombia, and Ecuador, and Ornithdoros dugesi, Ornithodoros nicollei, and O. turicata from Mexico were infected with B. mazzottii. Upon subsequent tick feedings, only O. talaje from Mexico and Guatemala transmitted the spirochete to mice. The remaining “nontransmitters” were triturated and injected into mice, of which none became infected. This work suggested that B. mazzottii failed to colonize the “nontransmitting” ticks.
Gordon’s transmission studies with O. talaje that originated from North, Central, and South America indicated the complexity of soft tick systematics from this region of the globe. At the nymphal and adult stages, O. talaje is virtually indistinguishable from other closely-related species, such as O. puertoricensis [92]. Moreover, the phylogenetic classification of argasids that was established by Hoogstraal was based on morphological and biological characteristics, behavior, and tick development [93]. Therefore, the species specificity of B. mazzottii for O. talaje collected in Mexico and Guatemala suggests that the biological differences in vectorial competency may separate the tick species from those obtained in Central and South American. Furthermore, since the studies were also conducted with nymphs and adults, it is conceivable that O. talaje collected in Panama may have been O. puertoricensis [59], which is also distributed in the country [94]. Clearly, genetic information from O. talaje obtained throughout the Americas is needed and will clarify ambiguities with the vectors distribution.
An interesting ecological finding of O. talaje is the collection of the ticks in identical niches as O. turicata. Our ongoing field studies in Southern and Central Texas continue to recover O. talaje in the same woodrat and burrowing owl nests as O. turicata. As previously stated, nymphal and adult Ornithodoros ticks can be challenging to specieate [40]. However, keying the collected ticks revealed that two species were recovered [40], with O. talaje adults discernable from O. turicata with the presence of cheeks covering the mouthparts and separation of the first and second coxae (Figure 6).
Figure 6.
Morphological characteristics between Ornithodoros turicata and Ornithodoros talaje. O. turicata (A) and O. talaje (B) that were collected from a burrowing owl nest in Southern Texas. The mouthparts of O. turicata are exposed (A, black arrow) while “cheeks” cover the mouthparts of O. talaje (B, black arrow).
The feeding behavior of O. talaje larvae provides ample opportunity for the vector’s dispersal. Larvae are long-term feeders that remain attached to the vertebrate host for up to five days, while subsequent nymphs and adult O. talaje engorge rapidly [95]. As research attention is focused toward O. talaje, defining the dispersal and public health burden of this understudied tick and pathogen will be possible.
7. ABRF in Central America
Panama had some of the earliest accounts of RF in the Americas. Observations from the country at the turn of the 20th century paralleled those of Dutton and Todd, who first demonstrated that spirochetes were tick-borne pathogens that caused human disease in Africa [96]. For example, in 1907 Darling reported the detection of spirochetes in blood examinations of patients admitted to Commission hospitals in the Canal Zone [97]. During a 26-year period 117 cases were diagnosed [98]. However, as noted by Dunn and Clark, these patients were among employees of the Panama Canal who could afford health care, and the disease burden among the impoverished was unknown [98].
By 1921 it became clear that RF was a tick-borne disease. Bates and colleagues described several cases of RF in young men who were hunting in the Arraiján district of Panama [91]. The hunters “showed marks of many insect bites” and an investigation of their sleeping quarters resulted in the collection of O. talaje from the men’s bamboo-constructed beds. In a series of experiments, rats and nonhuman primates were infected with triturated ticks and by bite, respectively. To conclusively confirm that RF spirochetes caused disease and O. talaje was the vector, human volunteers were inoculated with infected rat blood or by tick bite and disease progression confirmed [91].
Field studies in 1933 from the Gorgas Memorial Laboratory provided clues into the ecology of RF spirochetes in Panama [98]. RF spirochetes were detected in the blood of a variety of mammals, including calves and horses. While it was unclear whether these large mammals maintain RF spirochetes in nature, detection of spirochetes in squirrel monkeys, opossums, and armadillos was more revealing in the pathogen’s ecology [98]. Sixty-one wild-caught opossums were evaluated, and spirochetes were detected in the blood of ~10%. In a small cohort of 21 nine-banded armadillos, two animals had active infections. To determine whether the animals were susceptible to a human isolate of RF spirochete obtained in Panama, two clean armadillos were needle inoculated with infected blood from the patient. One animal became highly spirochetemic by the second day after inoculation and succumbed to infection within nine days. The second armadillo maintained a prolonged cyclic infection for a month and then euthanized. These studies were the first to implicate opossums and armadillos in the ecology of RF spirochetes.
While RF spirochetes and their vectors have been neglected in Central America, evidence exists that the pathogens remain a public health problem. A recent case report of a tourist traveling along the Belize-Guatemala border indicated that the RF spirochetes continue to circulate in northern Central America [99]. Moreover, ongoing studies in Panama continue to identify O. puertoricensis, a putative vector, in domestic settings (Figure 7) and throughout the country [94,100,101,102]. The ecological work from Panama in the 1930s established the framework for current studies to understand RF spirochete maintenance in nature and disease burden on humans.
Figure 7.
Adult Ornithodoros puertoricensis collected in a human dwelling in Ancon, Panama City, Panama (A,B); Immature and adult O. puertoricensis in a reptile terrarium in Escobar, Colon, Panama (C).
8. ABRF in South America
Similar to Central America, there is little information regarding tick-borne RF in South America; however, evidence from Brazil and Bolivia indicate that the pathogens remain endemic. Ornithodoros brasiliensis, locally known as the “mouro” tick, was an implicated vector for RF spirochetes as early as 1931 after patients displayed headache, dyspnea, and fever after tick bites [103]. Through a collaborative effort between de B. Aragão, di Primio and Davis, at the Instituto Oswaldo Crus, Rio de Janeiro, Brazil and the Rocky Mountain Laboratory, Hamilton, MT, USA, transmission studies were described with ticks [104]. Feeding O. brasiliensis collected from human dwellings on rodents resulted with transmission of spirochetes, with guinea pigs becoming febrile. With observed specificity between RF spirochetes and a given tick vector, Davis proposed that the bacteria be named Borrelia brasiliensis [104]. The subsequent half century resulted in an absence of reports of the tick, and it was thought that O. brasiliensis was potentially eradicated or extinct [105].
In 2011, Martins and colleagues reported the public health concern of O. brasiliensis, as the bite was associated with an intense systemic reaction resulting in hospital admissions [106]. Moreover, the patient described the death of a pet that was parasitized by the ticks [106]. The ticks are aggressive toward humans and animals, and have been collected in domestic and peridomestic settings of the Southern Brazilian highlands above 900 m [103,105,107]. O. brasiliensis buries itself in ~5–40 mm of aluminic humic cambisol acidic soil under human dwellings, sheds, and storehouses [105]. In addition to a potential vector of RF spirochetes, the bite of O. brasiliensis is associated with necrosis of the attachment site and delayed wound healing [107,108,109]. More work is needed to understand the ecology and public health significance of O. brasiliensis.
Evidence also exists for RF in Bolivia [110,111]. Ciceroni and colleagues reported that Guarani Indians and mestizos from Camiri, Boyuibe, and Gutierrez, Bolivia had detectable serological responses to B. turicatae and B. parkeri by indirect immunofluorescent assay after adsorption to Treponema phagedenis [111]. Eliminating cross-reactive antibodies between RF- and syphilis-causing spirochetes was important; however, these findings do not rule out the possibility that the patients were exposed to Lyme-causing Borrelia. Furthermore, Parola and coworkers reported the detection of Borrelia DNA in Ornithodoros ticks [110]. The ticks were collected from rocky outcrops in the Cochabama Department, Bolivia, at an elevation of 2500 m. While morphological evaluation of the ticks grouped them as O. talaje, molecular information is absent for this species, and the collected ticks may be closer related to a new species, Ornithodoros rioplatensis [92].
9. Conclusions and Future Directions
RF spirochetes are primarily transmitted by argasid ticks in the genus Ornithodoros, while B. miyamotoi is now emerging as a human pathogen transmitted by Ixodes species. With the recent ability to culture B. miyamotoi [112], it is now possible to understand the intricacies of vector colonization and transmission. For example, given that the tick is a long-term feeder, does B. miyamotoi persistently colonize the salivary glands of Ixodes species? Alternatively, do the spirochetes predominantly reside in the midgut and then migrate to the salivary glands during tick feeding, as observed for Borrelia burgdorferi, and how do co-infections with Lyme disease-causing spirochetes affect vector competency? With recent attention on B. miyamotoi as a human pathogen, it is likely that the next decade will result in a better understanding of the pathogen’s life cycle in the vector.
Important aspects of ABRF spirochete pathogenesis that should be considered are a better understanding of tick and vertebrate host competency, and how it relates to vector and pathogen dispersal throughout the Americas. Furthermore, the disease burden of RF spirochetes in North, Central, and South America is either unknown or likely under reported, yet the tick vector continues to be identified in domestic and peridomestic settings. The ability to accurately serodiagnose exposure to the pathogens will facilitate ecological and epidemiological studies to better understand RF spirochete circulation amongst at-risk populations.
Acknowledgments
We thank Edward Wozniak for providing field collected ticks, Hannah Wilder for critical review of this manuscript, and Wen-Hsiang Chen for artistic rendition of the life cycle of RF spirochetes in the argasid tick vector. This work was supported by AI103724, AI123652, and startup funds provided by the National School of Tropical Medicine at Baylor College of Medicine.
Author Contributions
Job E. Lopez, Aparna Krishnavahjala, and Sergio Bermudez conceived and designed the experiments; Job E. Lopez and Sergio Bermudez performed the experiments and analyzed the data; Melissa Nolan Garcia contributed mapping tools; Job E. Lopez and Sergio Bermudez wrote the paper.
Conflicts of Interest
The authors declare no conflict of interest. The founding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
References
- 1.Varma M.G.R. Transmission of relapsing fever spirochetes by ticks; Proceedings of the Symposia of the Zoological Society of London; Regent’s Park, London, UK. 8 March 1962. [Google Scholar]
- 2.Davis G.E. Ticks and relapsing fever in the United States. Public Health Rep. 1940;55:2347–2351. doi: 10.2307/4583554. [DOI] [Google Scholar]
- 3.Larsson C., Andersson M., Bergstrom S. Current issues in relapsing fever. Curr. Opin. Infect. Dis. 2009;22:443–449. doi: 10.1097/QCO.0b013e32832fb22b. [DOI] [PubMed] [Google Scholar]
- 4.Cutler S. Spirochaetes: Past lessons to future directions. Clin. Microbiol. Infect. 2011;17:481–483. doi: 10.1111/j.1469-0691.2011.03485.x. [DOI] [PubMed] [Google Scholar]
- 5.Cutler S.J. Possibilities for relapsing fever reemergence. Emerg. Inf. Dis. 2006;12:369–374. doi: 10.3201/eid1203.050899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nordstrand A., Bunikis I., Larsson C., Tsogbe K., Schwan T.G., Nilsson M., Bergström S. Tickborne relapsing fever diagnosis obscured by malaria, Togo. Emerg. Infect. Dis. 2007;13:117–123. doi: 10.3201/eid1301.060670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mediannikov O., Socolovschi C., Bassene H., Diatta G., Ratmanov P., Fenollar F., Sokhna C., Raoult D. Borrelia crocidurae infection in acutely febrile patients, Senegal. Emerg. Infect. Dis. 2014;20:1335–1338. doi: 10.3201/eid2008.130550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trape J.F., Duplantier J.M., Bouganali H., Godeluck B., Legros F., Cornet J.P., Camicas J.L. Tick-borne borreliosis in West Africa. Lancet. 1991;337:473–475. doi: 10.1016/0140-6736(91)93404-W. [DOI] [PubMed] [Google Scholar]
- 9.Trape J.F., Godeluck B., Diatta G., Rogier C., Legros F., Albergel J., Pepin Y., Duplantier J.M. Tick-borne borreliosis in West Africa: Recent epidemiological studies. Rocz. Akad. Med. Bialymst. 1996;41:136–141. doi: 10.1016/0140-6736(91)93404-W. [DOI] [PubMed] [Google Scholar]
- 10.Schwan T.G., Anderson J.M., Lopez J.E., Fischer R.J., Raffel S.J., McCoy B.N., Safronetz D., Sogoba N., Maiga O., Traore S.F. Endemic foci of the tick-borne relapsing fever spirochete Borrelia crocidurae in Mali, West Africa, and the potential for human infection. PLoS Negl. Trop. Dis. 2012;6:e1924. doi: 10.1371/journal.pntd.0001924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diatta G., Souidi Y., Granjon L., Arnathau C., Durand P., Chauvancy G., Mane Y., Sarih M., Belghyti D., Renaud F., et al. Epidemiology of tick-borne borreliosis in Morocco. PLoS Negl. Trop. Dis. 2012;6:e1810. doi: 10.1371/journal.pntd.0001810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dworkin M.S., Anderson D.E., Jr., Schwan T.G., Shoemaker P.C., Banerjee S.N., Kassen B.O., Burgdorfer W. Tick-borne relapsing fever in the Northwestern United States and Southwestern Canada. Clin. Infect. Dis. 1998;26:122–131. doi: 10.1086/516273. [DOI] [PubMed] [Google Scholar]
- 13.Dworkin M.S., Schwan T.G., Anderson D.E. Tick-borne relapsing fever in North America. Med. Clin. N. Am. 2002;86:417–433. doi: 10.1016/S0025-7125(03)00095-6. [DOI] [PubMed] [Google Scholar]
- 14.Dworkin M.S., Schwan T.G., Anderson D.E., Jr., Borchardt S.M. Tick-borne relapsing fever. Infect. Dis. Clin. N. Am. 2008;22:449–468. doi: 10.1016/j.idc.2008.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dworkin M.S., Shoemaker P.C., Fritz C.L., Dowell M.E., Anderson D.E., Jr. The epidemiology of tick-borne relapsing fever in the United States. Am. J. Trop. Med. Hyg. 2002;66:753–758. doi: 10.4269/ajtmh.2002.66.753. [DOI] [PubMed] [Google Scholar]
- 16.Krause P.J., Narasimhan S., Wormser G.P., Rollend L., Fikrig E., Lepore T., Barbour A., Fish D. Human Borrelia miyamotoi infection in the United States. N. Engl. J. Med. 2013;368:291–293. doi: 10.1056/NEJMc1215469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Southern P.M., Sanford J.P. Relapsing fever: A clinical and microbiological review. Medicine. 1969;48:129–149. doi: 10.1097/00005792-196903000-00002. [DOI] [Google Scholar]
- 18.Davis G.E. Relapsing fever: The tick Ornithodoros turicata as a spirochetal reservoir. Public Health Rep. 1968;58:839–842. doi: 10.2307/4584474. [DOI] [Google Scholar]
- 19.Barbour A.G., Dai Q., Restrepo B.I., Stoenner H.G., Frank S.A. Pathogen escape from host immunity by a genome program for antigenic variation. Proc. Natl. Acad. Sci. USA. 2006;103:18290–18295. doi: 10.1073/pnas.0605302103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dai Q., Restrepo B.I., Porcella S.F., Raffel S.J., Schwan T.G., Barbour A.G. Antigenic variation by Borrelia hermsii occurs through recombination between extragenic repetitive elements on linear plasmids. Mol. Microbiol. 2006;60:1329–1343. doi: 10.1111/j.1365-2958.2006.05177.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meier J.T., Simon M.I., Barbour A.G. Antigenic variation is associated with DNA rearrangements in a relapsing fever Borrelia. Cell. 1985;41:403–409. doi: 10.1016/S0092-8674(85)80013-1. [DOI] [PubMed] [Google Scholar]
- 22.Davis R.D., Burke J.P., Wright L.J. Relapsing fever associated with ARDS in a parturient woman. A case report and review of the literature. Chest. 1992;102:630–632. doi: 10.1378/chest.102.2.630. [DOI] [PubMed] [Google Scholar]
- 23.Fihn S., Larson E.B. Tick-borne relapsing fever in the Pacific Northwest: An underdiagnosed illness? West. J. Med. 1980;133:203–209. [PMC free article] [PubMed] [Google Scholar]
- 24.Badger M.S. Tick talk: Unusually severe case of tick-borne relapsing fever with acute respiratory distress syndrome—Case report and review of the literature. Wilderness Environ. Med. 2008;19:280–286. doi: 10.1580/07-WEME-CR-140.1. [DOI] [PubMed] [Google Scholar]
- 25.Fuchs P.C., Oyama A.A. Neonatal relapsing fever due to transplacental transmission of Borrelia. JAMA. 1969;208:690–692. doi: 10.1001/jama.1969.03160040098019. [DOI] [PubMed] [Google Scholar]
- 26.Bryceson A.D. Clinical pathology of the Jarisch-Herxheimer reaction. J. Infect. Dis. 1976;133:696–704. doi: 10.1093/infdis/133.6.696. [DOI] [PubMed] [Google Scholar]
- 27.Vidal V., Scragg I.G., Cutler S.J., Rockett K.A., Fekade D., Warrell D.A., Wright D.J., Kwiatkowski D. Variable major lipoprotein is a principal TNF-inducing factor of louse-borne relapsing fever. Nat. Med. 1998;4:1416–1420. doi: 10.1038/4007. [DOI] [PubMed] [Google Scholar]
- 28.Hovius J.W., de Wever B., Sohne M., Brouwer M.C., Coumou J., Wagemakers A., Oei A., Knol H., Narasimhan S., Hodiamont C.J., et al. A case of meningoencephalitis by the relapsing fever spirochaete Borrelia miyamotoi in Europe. Lancet. 2013;382:658. doi: 10.1016/S0140-6736(13)61644-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Platonov A.E., Karan L.S., Kolyasnikova N.M., Makhneva N.A., Toporkova M.G., Maleev V.V., Fish D., Krause P.J. Humans infected with relapsing fever spirochete Borrelia miyamotoi, Russia. Emerg. Infect. Dis. 2011;17:1816–1823. doi: 10.3201/eid1710.101474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Molloy P.J., Telford S.R., 3rd, Chowdri H.R., Lepore T.J., Gugliotta J.L., Weeks K.E., Hewins M.E., Goethert H.K., Berardi V.P. Borrelia miyamotoi disease in the Northeastern United States: A case series. Ann. Intern. Med. 2015;163:91–98. doi: 10.7326/M15-0333. [DOI] [PubMed] [Google Scholar]
- 31.Telford S.R., 3rd, Goethert H.K., Molloy P.J., Berardi V.P., Chowdri H.R., Gugliotta J.L., Lepore T.J. Borrelia miyamotoi disease: Neither Lyme disease nor relapsing fever. Clin. Lab. Med. 2015;35:867–882. doi: 10.1016/j.cll.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barbour A.G. Multiple and Diverse vsp and vlp Sequences in Borrelia miyamotoi, a hard tick-borne zoonotic pathogen. PLoS ONE. 2016;11:e0146283. doi: 10.1371/journal.pone.0146283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCoy B.N., Raffel S.J., Lopez J.E., Schwan T.G. Bloodmeal size and spirochete acquisition of Ornithodoros hermsi (Acari: Argasidae) during feeding. J. Med. Entomol. 2010;47:1164–1172. doi: 10.1603/ME10175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schwan T.G., Schrumpf M.E., Hinnebusch B.J., Anderson D.E., Konkel M.E. GlpQ: An antigen for serological discrimination between relapsing fever and Lyme borreliosis. J. Clin. Microbiol. 1996;34:2483–2492. doi: 10.1128/jcm.34.10.2483-2492.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lopez J.E., Porcella S.F., Schrumpf M.E., Raffel S.J., Hammer C.H., Zhao M., Robinson M.A., Schwan T.G. Identification of conserved antigens for early serodiagnosis of relapsing fever Borrelia. Microbiology. 2009;155:2641–2651. doi: 10.1099/mic.0.029918-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wilder H.K., Wozniak E., Huddleston E., Tata S.R., Fitzkee N.C., Lopez J.E. Case report: A retrospective serological analysis indicating human exposure to tick-borne relapsing fever spirochetes in Texas. PLoS Negl. Trop. Dis. 2015;9:e0003617. doi: 10.1371/journal.pntd.0003617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Porcella S.F., Raffel S.J., Schrumpf M.E., Schriefer M.E., Dennis D.T., Schwan T.G. Serodiagnosis of louse-borne relapsing fever with glycerophosphodiester phosphodiesterase (GlpQ) from Borrelia recurrentis. J. Clin. Microbiol. 2000;38:3561–3571. doi: 10.1128/jcm.38.10.3561-3571.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lopez J.E., Schrumpf M.E., Nagarajan V., Raffel S.J., McCoy B.N., Schwan T.G. A novel surface antigen of relapsing fever spirochetes can discriminate between relapsing fever and Lyme borreliosis. Clin. Vaccine Immunol. 2010;17:564–571. doi: 10.1128/CVI.00518-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lopez J.E., Wilder H.K., Boyle W., Drumheller L.B., Thornton J.A., Willeford B., Morgan T.W., Varela-Stokes A. Sequence analysis and serological responses against Borrelia turicatae BipA, a putative species-specific antigen. PLoS Negl. Trop. Dis. 2013;7:e2454. doi: 10.1371/journal.pntd.0002454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cooley R.A., Kohls G.M. The Agarasidae of North America, Central America, and Cuba. The University Press; Notre Dame, IN, USA: 1944. pp. 1–152. [Google Scholar]
- 41.Balashov Y.S. Bloodsucking ticks (Ixodoidea)-vectors of diseases of man and animals. Misc. Publ. Entomol. Soc. Am. 1972;8:161–376. [Google Scholar]
- 42.Boyle W.K., Wilder H.K., Lawrence A.M., Lopez J.E. Transmission dynamics of Borrelia turicatae from the arthropod vector. PLoS Negl. Trop. Dis. 2014;8:e2767. doi: 10.1371/journal.pntd.0002767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alugupalli K.R., Gerstein R.M., Chen J., Szomolanyi-Tsuda E., Woodland R.T., Leong J.M. The resolution of relapsing fever borreliosis requires IgM and is concurrent with expansion of B1b lymphocytes. J. Immunol. 2003;170:3819–3827. doi: 10.4049/jimmunol.170.7.3819. [DOI] [PubMed] [Google Scholar]
- 44.Woodman M.E., Cooley A.E., Avdiushko R., Bowman A., Botto M., Wooten R.M., van Rooijen N., Cohen D.A., Stevenson B. Roles for phagocytic cells and complement in controlling relapsing fever infection. J. Leukoc. Biol. 2009;86:727–736. doi: 10.1189/jlb.0309169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schwan T.G., Hinnebusch B.J. Bloodstream-versus tick-associated variants of a relapsing fever bacterium. Science. 1998;280:1938–1940. doi: 10.1126/science.280.5371.1938. [DOI] [PubMed] [Google Scholar]
- 46.Raffel S.J., Battisti J.M., Fischer R.J., Schwan T.G. Inactivation of genes for antigenic variation in the relapsing fever spirochete Borrelia hermsii reduces infectivity in mice and transmission by ticks. PLoS Pathog. 2014;10:e1004056. doi: 10.1371/journal.ppat.1004056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lopez J.E., McCoy B.N., Krajacich B.J., Schwan T.G. Acquisition and subsequent transmission of Borrelia hermsii by the soft tick Ornithodoros hermsi. J. Med. Entomol. 2011;48:891–895. doi: 10.1603/ME10283. [DOI] [PubMed] [Google Scholar]
- 48.Johnson T.L., Landguth E.L., Stone E.F. Modeling relapsing disease dynamics in a host-vector community. PLoS Negl. Trop. Dis. 2016;10:e0004428. doi: 10.1371/journal.pntd.0004428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schwan T.G., Policastro P.F., Miller Z., Thompson R.L., Damrow T., Keirans J.E. Tick-borne relapsing fever caused by Borrelia hermsii, Montana. Emerg. Infect. Dis. 2003;9:1151–1154. doi: 10.3201/eid0909.030280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nakajima Y., Saido-Sakanaka H., Taylor D., Yamakawa M. Up-regulated humoral immune response in the soft tick, Ornithodoros moubata (Acari: Argasidae) Parasitol. Res. 2003;91:476–481. doi: 10.1007/s00436-003-0954-y. [DOI] [PubMed] [Google Scholar]
- 51.Nakajima Y., Taylor D., Yamakawa M. Involvement of antibacterial peptide defensin in tick midgut defense. Exp. Appl. Acarol. 2002;28:135–140. doi: 10.1023/A:1025399610947. [DOI] [PubMed] [Google Scholar]
- 52.Nakajima Y., van der Goes van Naters-Yasui A., Taylor D., Yamakawa M. Antibacterial peptide defensin is involved in midgut immunity of the soft tick, Ornithodoros moubata. Insect Mol. Biol. 2002;11:611–618. doi: 10.1046/j.1365-2583.2002.00372.x. [DOI] [PubMed] [Google Scholar]
- 53.Francischetti I.M., Mans B.J., Meng Z., Gudderra N., Veenstra T.D., Pham V.M., Ribeiro J.M. An insight into the sialome of the soft tick, Ornithodorus parkeri. Insect Biochem. Mol. Biol. 2008;38:1–21. doi: 10.1016/j.ibmb.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mans B.J., Andersen J.F., Francischetti I.M., Valenzuela J.G., Schwan T.G., Pham V.M., Garfield M.K., Hammer C.H., Ribeiro J.M. Comparative sialomics between hard and soft ticks: Implications for the evolution of blood-feeding behavior. Insect Biochem. Mol. Biol. 2008;38:42–58. doi: 10.1016/j.ibmb.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schwan T.G., Piesman J. Vector interactions and molecular adaptations of Lyme disease and relapsing fever spirochetes associated with transmission by ticks. Emerg. Infect. Dis. 2002;8:115–121. doi: 10.3201/eid0802.010198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Davis G.E. Ornithodoros turicata: The male; feeding and copulation habits, fertility, span of life, and the transmission of relapsing fever spirochetes. Public Health Rep. 1941;56:1799–1802. doi: 10.2307/4583854. [DOI] [Google Scholar]
- 57.Wilder H.K., Raffel S.J., Barbour A.G., Porcella S.F., Sturdevant D.E., Vaisvil B., Kapatral V., Schmitt D.P., Schwan T.G., Lopez J.E. Transcriptional profiling the 150 kb linear megaplasmid of Borrelia turicatae suggests a role in vector colonization and initiating mammalian infection. PLoS ONE. 2016;11:e0147707. doi: 10.1371/journal.pone.0147707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Brumpt E. Étude du Spirochaeta turicatae, n. sp., agent de la fièvre récurrente sporadique des Etats-Unis trasmise par Ornithodoros turicata. C. R. Soc. Biol. 1933;113:1369. [Google Scholar]
- 59.Davis GE. A relapsing fever spirochete, Borrelia mazzottii (sp. nov.) from Ornithodoros talaje from Mexico. Am. J. Hyg. 1956;63:13–17. doi: 10.1093/oxfordjournals.aje.a119787. [DOI] [PubMed] [Google Scholar]
- 60.Schwan T.G. Ticks and Borrelia: Model systems for investigating pathogen-arthropod interactions. Infect. Agents Dis. 1996;5:167–181. [PubMed] [Google Scholar]
- 61.Fedorova N., Kleinjan J.E., James D., Hui L.T., Peeters H., Lane R.S. Remarkable diversity of tick or mammalian-associated Borreliae in the metropolitan San Francisco Bay area, California. Ticks Tick Borne Dis. 2014;5:951–961. doi: 10.1016/j.ttbdis.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 62.Scoles G.A., Papero M., Beati L., Fish D. A relapsing fever group spirochete transmitted by Ixodes scapularis ticks. Vector Borne Zoon. Dis. 2001;1:21–34. doi: 10.1089/153036601750137624. [DOI] [PubMed] [Google Scholar]
- 63.Centers for Disease Control and Prevention Geographic Distribution of Ticks That Bite Humans. [(accessed on 15 August 2016)]; Avaiable online: http://www.cdc.gov/ticks/geographic_distribution.html.
- 64.Reisen W.K. Landscape epidemiology of vector-borne diseases. Annu. Rev. Entomol. 2010;55:461–483. doi: 10.1146/annurev-ento-112408-085419. [DOI] [PubMed] [Google Scholar]
- 65.Davis G.E. Ornithodoros parkeri: Distribution and host data; spontaneous infection with relapsing fever spirochetes. Public Health Rep. 1939;54:1345–1349. doi: 10.2307/4582963. [DOI] [Google Scholar]
- 66.Davis G.E. Ornithodoros parkeri Cooley: Observations on the biology of this tick. J. Parasitol. 1940;27:425–433. [Google Scholar]
- 67.Cooley R.A. Ornithodoros parkeri, a new species on rodents. Public Health Rep. 1936;51:431–433. doi: 10.2307/4581804. [DOI] [Google Scholar]
- 68.Nieto N.C., Teglas M.B. Relapsing fever group Borrelia in Southern California rodents. J. Med. Entomol. 2014;51:1029–1034. doi: 10.1603/ME14021. [DOI] [PubMed] [Google Scholar]
- 69.Nieto N.C., Teglas M.B., Stewart K.M., Wasley T., Wolff P.L. Detection of relapsing fever spirochetes (Borrelia hermsii and Borrelia coriaceae) in free-ranging mule deer (Odocoileus hemionus) from Nevada, United States. Vector Borne Zoon. Dis. 2012;12:99–105. doi: 10.1089/vbz.2011.0716. [DOI] [PubMed] [Google Scholar]
- 70.Christensen J., Fischer R.J., McCoy B.N., Raffel S.J., Schwan T.G. Tickborne relapsing fever, Bitterroot Valley, Montana, USA. Emerg. Infect. Dis. 2015;21:217–223. doi: 10.3201/eid2102.141276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Piesman J., Schwan T.G. Ecology of Borreliae and Their Arthropod Vectors. Caister Academic Press; Norfolk, UK: 2010. [Google Scholar]
- 72.Schwan T.G., Raffel S.J., Schrumpf M.E., Webster L.S., Marques A.R., Spano R., Rood M., Burns J., Hu R. Tick-borne relapsing fever and Borrelia hermsii, Los Angeles County, California, USA. Emerg. Infect. Dis. 2009;15:1026–1031. doi: 10.3201/eid1507.090223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Burgdorfer W., Mavros A.J. Susceptibility of various species of rodents to the relapsing fever spirochete, Borrelia hermsii. Infect. Immun. 1970;2:256–259. doi: 10.1128/iai.2.3.256-259.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fritz C.L., Payne J.R., Schwan T.G. Serologic evidence for Borrelia hermsii infection in rodents on federally owned recreational areas in California. Vector Borne Zoon. Dis. 2013;13:376–381. doi: 10.1089/vbz.2012.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kelly R. Cultivation of Borrelia hermsi. Science. 1971;173:443–444. doi: 10.1126/science.173.3995.443. [DOI] [PubMed] [Google Scholar]
- 76.Schwan T.G., Raffel S.J., Schrumpf M.E., Porcella S.F. Diversity and distribution of Borrelia hermsii. Emerg. Infect. Dis. 2007;13:436–442. doi: 10.3201/eid1303.060958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Thomas N.J., Bunikis J., Barbour A.G., Wolcott M.J. Fatal spirochetosis due to a relapsing fever-like Borrelia sp. in a northern spotted owl. J. Wildl. Dis. 2002;38:187–193. doi: 10.7589/0090-3558-38.1.187. [DOI] [PubMed] [Google Scholar]
- 78.Bunikis J., Tsao J., Garpmo U., Berglund J., Fish D., Barbour A.G. Typing of Borrelia relapsing fever group strains. Emerg. Infect. Dis. 2004;10:1661–1664. doi: 10.3201/eid1009.040236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kelly A.L., Raffel S.J., Fischer R.J., Bellinghausen M., Stevenson C., Schwan T.G. First isolation of the relapsing fever spirochete, Borrelia hermsii, from a domestic dog. Ticks Tick Borne Dis. 2014;5:95–99. doi: 10.1016/j.ttbdis.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Felsenfeld O. The problem of relapsing fever in the Americas. IMS Ind. Med. Surg. 1973;42:7–10. [PubMed] [Google Scholar]
- 81.Donaldson T.G., Perez de Leon A.A., Li A.I., Castro-Arellano I., Wozniak E., Boyle W.K., Hargrove R., Wilder H.K., Kim H.J., Teel P.D., et al. Assessment of the geographic distribution of Ornithodoros turicata (Argasidae): Climate variation and host diversity. PLoS Negl. Trop. Dis. 2016;10:e0004383. doi: 10.1371/journal.pntd.0004383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Adeyeye O.A., Butler J.F. Population structure and seasonal intra-burrow movement of Ornithodoros turicata (Acari: Argasidae) in gopher tortoise burrows. J. Med. Entomol. 1989;26:279–283. doi: 10.1093/jmedent/26.4.279. [DOI] [PubMed] [Google Scholar]
- 83.Adeyeye O.A., Butler J.F. Field evaluation of carbon dioxide baits for sampling Ornithodoros turicata (Acari: Argasidae) in gopher tortoise burrows. J. Med. Entomol. 1991;28:45–48. doi: 10.1093/jmedent/28.1.45. [DOI] [PubMed] [Google Scholar]
- 84.Largo P.K. A survey of arthropods associated with gopher tortoise burrows in Mississippi. Entomol. News. 1991;102:1–13. [Google Scholar]
- 85.Beck A.F., Holscher K.H., Butler J.F. Life cycle of Ornithodoros turicata americanus (Acari: Argasidae) in the laboratory. J. Med. Entomol. 1986;23:313–319. doi: 10.1093/jmedent/23.3.313. [DOI] [PubMed] [Google Scholar]
- 86.Beck M.D. Present distribution of relapsing fever in California. In: Moulton F.R., editor. Proceedings of the A Symposium on Relapsing Fever in the Americas; Washington, DC, USA: American Association for the Advancement of Science; 1942. pp. 20–25. [Google Scholar]
- 87.Wheeler C.M. The distribution of the spirochete of California relapsing fever within the body of the vector, Ornithodoros hermsi. In: Moulton F.R., editor. Proceedings of the A Symposium on Relapsing Fever in the Americas; Washington, DC, USA: American Association for the Advancement of Science; 1942. pp. 89–99. [Google Scholar]
- 88.Breitschwerdt E.B., Nicholson W.L., Kiehl A.R., Steers C., Meuten D.J., Levine J.F. Natural infections with Borrelia spirochetes in two dogs from Florida. J. Clin. Microbiol. 1994;32:352–357. doi: 10.1128/jcm.32.2.352-357.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Whitney M.S., Schwan T.G., Sultemeier K.B., McDonald P.S., Brillhart M.N. Spirochetemia caused by Borrelia turicatae infection in 3 dogs in Texas. Vet. Clin. Pathol. 2007;36:212–216. doi: 10.1111/j.1939-165X.2007.tb00213.x. [DOI] [PubMed] [Google Scholar]
- 90.Francis E. Longevity of the tick Ornithodoros turicata and of Spirochaeta recurrentis with this tick. Public Health Rep. 1938;53:2220–2241. doi: 10.2307/4582740. [DOI] [Google Scholar]
- 91.Bates L.B., Dunn L.H., St. John J.H. Relapsing fever in Panama. Am. J. Trop. Med. Hyg. 1921;1:183–210. [Google Scholar]
- 92.Venzal J.M., Estrada-Pena A., Mangold A.J., Gonzalez-Acuna D., Guglielmone A.A. The Ornithodoros (Alectorobius) talaje species group (Acari: Ixodida: Argasidae): Description of Ornithodoros (Alectorobius) rioplatensis n. sp. from southern South America. J. Med. Entomol. 2008;45:832–840. doi: 10.1603/0022-2585(2008)45[832:toatsg]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 93.Hoogstraal H. Argasid and nuttalliellid ticks as parasites and vectors. Adv. Parasitol. 1985;24:135–238. doi: 10.1016/s0065-308x(08)60563-1. [DOI] [PubMed] [Google Scholar]
- 94.Bermudez S.E., Miranda R.J., Smith D. Ticks species (Ixodida) in the Summit Municipal Park and adjacent areas, Panama City, Panama. Exp. Appl. Acarol. 2010;52:439–448. doi: 10.1007/s10493-010-9374-8. [DOI] [PubMed] [Google Scholar]
- 95.Need J.T., Butler J.F. Sequential feedings by two species of argasid tick on laboratory mice: Effects on tick survival, weight gain, and attachment time. J. Med. Entomol. 1991;28:37–40. doi: 10.1093/jmedent/28.1.37. [DOI] [PubMed] [Google Scholar]
- 96.Dutton J.E., Todd J.L. The nature of human tick-fever in the eastern part of the Congo Free State with notes on the distribution and bionomics of the tick. Liverp. Sch. Trop. Med. 1905;17:1–18. [Google Scholar]
- 97.Darling S.T. The relapsing fever of Panama. Arch. Intern. Med. 1909;4:150–185. doi: 10.1001/archinte.1909.00050180052005. [DOI] [Google Scholar]
- 98.Dunn L.H., Clark H.C. Notes on relapsing fever in Panama with special reference to animal hosts. Am. J. Trop. Med. Hyg. 1933;13:201–209. [Google Scholar]
- 99.Heerdink G., Petit P.L., Hofwegen H., van Genderen P.J. A patient with fever following a visit to the tropics: Tick-borne relapsing fever discovered in a thick blood smear preparation. Ned. Tijdschr. Geneeskd. 2006;150:2386–2389. [PubMed] [Google Scholar]
- 100.Bermudez S.E., Miranda R., Cleghorn J., Venzal J. Ornithodoros (Alectorobius) puertoricensis (Ixodida: Argasidae) parasitizing exotic reptiles pets in Panama. Rev. FAVE-Cienc. Vet. 2015;14:1–5. doi: 10.14409/favecv.v14i1/3.5095. [DOI] [Google Scholar]
- 101.Bermudez S.E., Miranda R., Kadoch N. Reporte de larvas de Ornithodoros puertoricensis Fox 1947 (Ixodida: Argasidae) parasitando a Rhinella marina (L. 1758) (Anura: Bufonidae) en David, Chiriquí, Panamá. Puente Biol. 2013;5:81–85. [Google Scholar]
- 102.Rangel G., Bermudez S.E. Nota sobre un caso de parasitismo de Ornithodoros sp. (Ixodida: Argasidae) en una mujer proveniente de La Laja, Los Santos, Panamá. Rev. Méd. Panamá. 2013;34:37–39. [Google Scholar]
- 103.Pinto C., Primo R. Contribuicão para a biologia dos Ixodidae so Estado do Rio Grande do Sul (Brazil) Rev. Med. Cir. Braz. 1931;34:5–6. [Google Scholar]
- 104.Davis G.E. Observations on the biology of the argasid tick, Ornithodoros brasiliensis Aragao, 1923; with the recovery of a spirochete, Borrelia brasiliensis, n. sp. J. Parasitol. 1952;38:473–476. doi: 10.2307/3273927. [DOI] [PubMed] [Google Scholar]
- 105.Reck J., Marks F.S., Guimaraes J.A., Termignoni C., Martins J.R. Epidemiology of Ornithodoros brasiliensis (mouro tick) in the southern Brazilian highlands and the description of human and animal retrospective cases of tick parasitism. Ticks Tick Borne Dis. 2013;4:101–109. doi: 10.1016/j.ttbdis.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 106.Martins J.R., Doyle R.L., Barros-Battesti D.M., Onofrio V.C., Guglielmone A.A. Occurrence of Ornithodoros brasiliensis Aragao (Acari: Argasidae) in Sao Francisco de Paula, RS, Southern Brazil. Neotrop. Entomol. 2011;40:143–1444. doi: 10.1590/S1519-566X2011000100022. [DOI] [PubMed] [Google Scholar]
- 107.Reck J., Soares J.F., Termignoni C., Labruna M.B., Martins J.R. Tick toxicosis in a dog bitten by Ornithodoros brasiliensis. Vet. Clin. Pathol. 2011;40:356–360. doi: 10.1111/j.1939-165X.2011.00338.x. [DOI] [PubMed] [Google Scholar]
- 108.Reck J., Bandarra P., Pavarini S., Termignoni C., Driemeier D., Martins J.R., Guimaraes J.A. Experimentally induced tick toxicosis in rats bitten by Ornithodoros brasiliensis (Chelicerata: Argasidae): A clinico-pathological characterization. Toxicon. 2014;88:99–106. doi: 10.1016/j.toxicon.2014.06.017. [DOI] [PubMed] [Google Scholar]
- 109.Reck J., Marks F.S., Termignoni C., Guimaraes J.A., Martins J.R. Ornithodoros brasiliensis (mouro tick) salivary gland homogenates inhibit in vivo wound healing and in vitro endothelial cell proliferation. Parasitol. Res. 2013;112:1749–1753. doi: 10.1007/s00436-013-3333-3. [DOI] [PubMed] [Google Scholar]
- 110.Parola P., Ryelandt J., Mangold A.J., Mediannikov O., Guglielmone A.A., Raoult D. Relapsing fever Borrelia in Ornithodoros ticks from Bolivia. Ann. Trop. Med. Parasitol. 2011;105:407–411. doi: 10.1179/1364859411Y.0000000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ciceroni L., Bartoloni A., Guglielmetti P., Paradisi F., Barahona H.G., Roselli M., Ciarrocchi S., Cacciapuoti B. Prevalence of antibodies to Borrelia burgdorferi, Borrelia parkeri and Borrelia turicatae in human settlements of the Cordillera Province, Bolivia. J. Trop. Med. Hyg. 1994;97:13–17. [PubMed] [Google Scholar]
- 112.Wagemakers A., Staarink P.J., Sprong H., Hovius J.W. Borrelia miyamotoi: A widespread tick-borne relapsing fever spirochete. Trends Parasitol. 2015;31:260–269. doi: 10.1016/j.pt.2015.03.008. [DOI] [PubMed] [Google Scholar]