Abstract
The developmental period of the nervous system is carefully orchestrated and highly vulnerable to alterations. One crucial factor of a properly-functioning nervous system is the synapse, as synaptic signaling is critical for the formation and maturation of neural circuits. Studies show that genetic and environmental impacts can affect diverse components of synaptic function. Importantly, synaptic dysfunction is known to be associated with neurologic and psychiatric disorders, as well as more subtle cognitive, psychomotor, and sensory defects. Given the importance of the synapse in numerous domains, we wanted to delineate the effects of pesticide exposure on synaptic function. In this review, we summarize current epidemiologic and molecular studies that demonstrate organochlorine, organophosphate, and pyrethroid pesticide exposures target the developing synapse. We postulate that the synapse plays a central role in synaptic vulnerability to pesticide exposure during neurodevelopment, and the synapse is a worthy candidate for investigating more subtle effects of chronic pesticide exposure in future studies.
Keywords: dopamine, GABA, glutamate, neurodevelopment, neurotoxicity, organochlorine, organophosphate, pesticide, pyrethroid, synapse
1. Neurodevelopment
Neurodevelopment is comprised of a highly orchestrated sequence of biological processes, including proliferation, migration, differentiation, and synaptogenesis, which must occur for the normal development and function of the nervous system. In utero, the human nervous system arises from the neuroepithelium of the neural tube around day 18. The ventricular zone contains progenitors that form all the cell types that comprise the central nervous system (CNS). These cell types include glia, which have various supportive roles such as the protection and nourishment of neurons. Neurons are the major signaling cells of the nervous system and they generally consist of a cell body with a single, outgoing axon and numerous projecting dendrites. Once neurons differentiate in the ventricular zone they then migrate to specific regions throughout the brain, using radial glia as their guides to this localization. In humans, the majority of neuronal migration is completed around month five in utero and neuronal axons further refine the formation of neural circuits by extending their processes along highly regulated pathways to facilitate communication with proximal or distal neurons. To guide this process, growth cones form at the end of developing axons with long, thin filopodia that respond to chemotactic signals serving to either attract or repel the advancing growth cone [1,2].
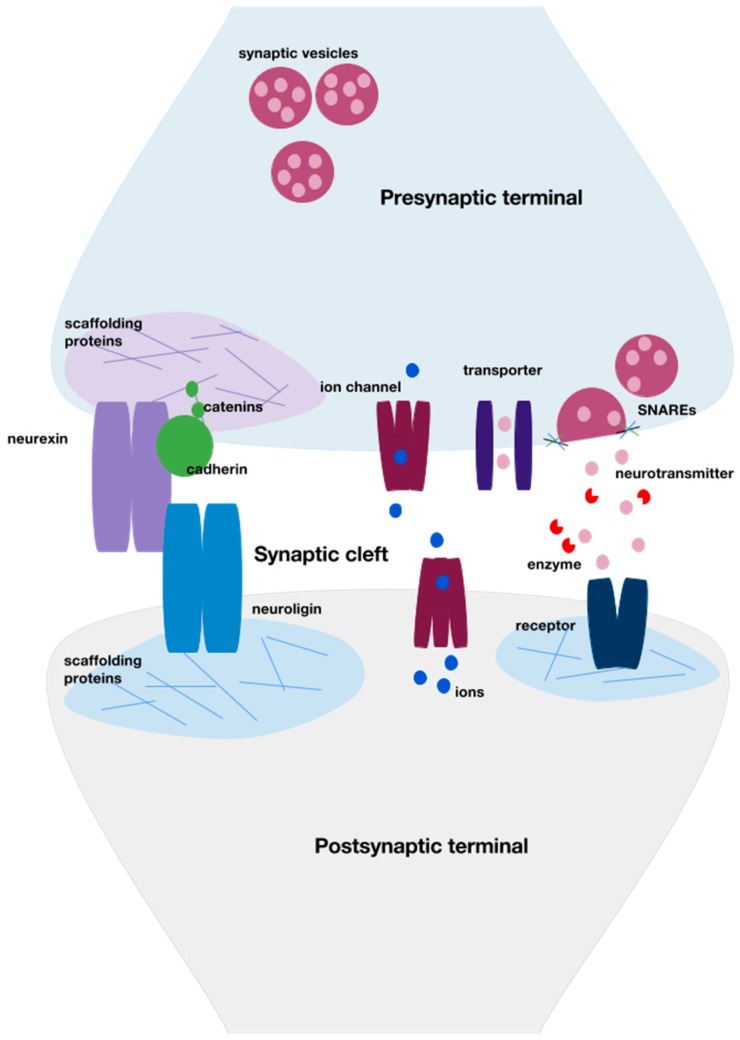
Crucial to the establishment of neural circuits are neuronal synapses, which allow for communication between neurons. When an axonal growth cone comes into contact with another neuron to form a synapse, the filopodia retract and intercellular signals from surrounding glia, the extracellular matrix (ECM) of the neuron, and other nearby neurons initiate development of the synapse. Cell adhesion is an important process for initially connecting the pre- and postsynaptic aspects of the neurons. Two important synaptic cell adhesion molecules are neurexins and neuroligins (Figure 1). The neurexins and neuroligins bind to form a trans-synaptic complex that then binds to PDZ-domain-containing proteins on either side. The PDZ domain is a protein-binding domain that binds short peptide motifs at the extreme carboxy terminal, which allows scaffolding proteins to form large modular complexes. The domain is named after the first three proteins found to contain the domain: post synaptic density protein (PSD95), Drosophila disc large tumor suppressor (Dlg1), and zonula occludens-1 protein (zo-1). The neurexin-neuroligin complex places the pre- and postsynaptic terminals in apposition and allows for further protein scaffolding construction via the two attached PDZ domains [3]. Neurexins primarily reside on the presynaptic side and induce presynaptic specialization. In contrast, neuroligins primarily reside on the postsynaptic side and initiate postsynaptic specialization. Various additional synaptic cell adhesion molecules localize to the developing synapse and are utilized to strengthen and align the connection. One such molecule is cadherin, a calcium-dependent transmembrane protein that binds with catenins, which then connect to actin components of the cytoskeleton [4] (Figure 1). Similarly, nectins also play a calcium-dependent role in cell adhesion at the developing synapse, through interactions with the actin cytoskeleton of the presynaptic active zone [2].
Figure 1.
General schematic of neuronal synapse structure. A critical aspect of neurodevelopment is synaptogenesis, a highly organized series of intra- and intercellular events. These form the pre- and postsynaptic terminals and allow for neural activity between neurons. Cellular adhesion molecules, such as neurexin and neuroligin, create a physical interaction between the two terminals. The neurexin-neuroligin complex is bound on either side by scaffolding proteins, which create a specialized area within the terminal for receptors, ion channels, and transporters. Other cellular adhesion molecules such as cadherin-catenin complexes, connect actin components to the cytoskeleton scaffold and strengthen the connection. Once the synapse is formed, neurotransmitter is stored in synaptic vesicles. Some of these vesicles are attached to the presynaptic cytoskeleton as a reserve pool, awaiting depolarization via movement of ions. Once the presynaptic neuron depolarizes, the vesicle docks to the plasma membrane and fuses with it via soluble N-ethylmaleimide sensitive fusion attachment protein receptors (SNAREs). Neurotransmitter diffuses across the cleft and interacts with postsynaptic receptors. Excess neurotransmitter in the cleft is broken down via enzymes or transported back into the presynaptic terminal via reuptake transporters.
Following alignment of the pre- and postsynaptic terminals, the intracellular machinery necessary for the function of these elements begins to take shape. On the presynaptic side, a preassembled active zone is transported to the presynaptic terminal. This active zone is a region of the presynaptic terminal characterized by large amounts of scaffolding proteins, such as bassoon and piccolo for example, which help organize the active zone and the intracellular components necessary for normal function of the presynaptic terminal. The proteins bassoon and piccolo are large scaffolding proteins that reside at some presynaptic terminals, and they play an important role in forming the cytoskeleton structure [5]. One important function of scaffolding in the active zone is localization of neurotransmitter reuptake transporters close to the synapse. Once neurotransmitter is released presynaptically and interacts with postsynaptic receptors, these presynaptic reuptake transporters play a large role in clearing many synapses, and in regulating extracellular neurotransmitter levels. Of note, there are additional mechanisms of clearing neurotransmitter from the synapse. These mechanisms include reuptake by transporters on surrounding astrocytes, diffusion of neurotransmitter away from postsynaptic receptors, and enzymatic degradation [6].
Postsynaptically, one of the major proteins neuroligins bind to is postsynaptic density protein 95 (PSD-95), a membrane-associated guanylate kinase highly concentrated in the postsynaptic density. The postsynaptic density is a region somewhat analogous to the active zone of the presynaptic terminal. It is a densely packed region that ensures apposition of receptors to neurotransmitters diffusing across the synaptic cleft. Other scaffolding proteins that bind membrane receptors to the cytoskeleton include Shank and guanylate kinase-associated protein (GKAP) in CNS excitatory synapses [7] and gephyrin, used for γ-aminobutyric acid (GABA) receptor clustering [2,3]. Once receptors are in place, activation of these receptors via neurotransmitter released across the synapse further regulates receptor expression. Generally, increased receptor activation leads to downregulation of receptor expression and upregulation of receptor internalization [2].
Chemical synapses are polarized, allowing only unidirectional signals in a highly regulated manner. The presynaptic terminal contains thousands of neurotransmitter-filled synaptic vesicles (SVs) that are attached to the cytoskeleton as a reserve pool. To release its contents, a SV is mobilized from the cytoskeleton via phosphorylation of synapsin I and myosin II on the cytoskeleton by calcium/calmodulin kinase II (CAMKII) and myosin light chain kinase (MLCK). The SV then docks and connects to the active zone plasma membrane. Calcium (Ca2+) triggers membrane fusion, via soluble N-ethylmaleimide sensitive fusion protein attachment receptors (SNAREs). There are several types of SNAREs, including synaptobrevin, syntaxin 1, and SNAP-25 (synaptosomal-associated protein of 25 kDa). SNAREs form a crucial helical bundle that mediates the interaction between the vesicular and plasma membranes. Neurotransmitter left in the synaptic cleft is then taken up into the presynaptic terminal by plasma membrane transporters, while empty SVs are recycled via clathrin-mediated endocytosis [8] (Figure 1).
Once synapses are formed, their connectivity and function is continuously refined during adulthood, leading to a unique ability to form new neural networks throughout life. As part of this refinement process, heterosynaptic depression takes place. In heterosynaptic depression there is more synaptic activity in one synapse than a second related synapse, and the less active synapse regresses. Studies show that intracellular Ca2+ and other Ca2+-binding proteins are necessary for heterosynaptic depression to occur. One of these Ca2+-binding proteins is CAMKII, which is able to regulate the number of synaptic connections that are made and also plays a role in the regulation of cell adhesion molecules at the synapse to influence synaptic stability [2]. Thus, while the nervous system structure is largely in place early in life, refinement of neural circuits, especially at the synapse, occurs as late as the mid-twenties [9,10].
The nervous system is uniquely vulnerable to disturbances due to the need for careful organization and the fast rate of development that occurs. Synaptogenesis appears to be an especially sensitive period of neurodevelopment given its molecular complexity and elaborated length of time from gestation to adulthood [11]. Increasingly, molecular and genetic studies of neurodevelopmental diseases have pointed to alterations in synaptic proteins and their role in disease pathophysiology. For example, mutations in the cell adhesion molecules neurexins and neuroligins are associated with autism spectrum disorder (ASD) and other cognitive disorders. As discussed above, the neurexin-neuroligin complex stabilizes and connects the pre- and postsynaptic neurons, and also plays a role in synapse maturation [3]. A mouse model of an ASD-associated mutation in Neuroligin 3 exhibits increased expression of inhibitory synaptic markers, increased frequency of inhibitory signaling, and alterations of the hippocampus and cortex [12,13]. The mice also have impaired social behavior and increased repetitive behavior, mimicking the behavioral symptoms of patients with ASD [13,14]. Similar behavioral effects are also reported in mouse models of the Neuroligin 1 and Neuroligin 4 genes, exemplifying that neuroligins play an important role in the synaptic pathophysiology of ASD [15,16].
Scaffolding proteins lead to the proper stabilization of synapses. Disruption of this process could potentially contribute to the observed learning and memory deficits seen when scaffolding proteins are altered. For example, detrimental changes in synaptic scaffolding and receptor transport are associated with neurobehavioral and cognitive disorders. SNX27 is a PDZ-domain binding protein enriched in the brain, and also regulates recycling of postsynaptic receptors. Mutations in SNX27 are associated with Down syndrome, as well as learning and memory deficits, and this is thought to be due to alterations in localization of postsynaptic α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) and (N-methyl-D-aspartate) NMDA receptors. Mutations in SHANK genes are also associated with ASD, Phelan McDermid syndrome (a form of intellectual disability), schizophrenia, and Alzheimer disease (AD). Shank proteins are scaffolding proteins at glutamatergic synapses and play roles in dendritic spine morphogenesis, glutamate receptor trafficking and activity-dependent neuronal signaling [3,17]. Multiple SHANK isoforms have been associated with ASD, intellectual disability, and schizophrenia in genetic studies [18,19,20,21]. Mouse models lacking SHANK2 exhibit differential ultrasound vocalization patterns, whereas mice lacking SHANK1 exhibit altered self-grooming and marble burying behaviors that were modified by social context [22,23,24]. In mouse models carrying SHANK3 mutations and deletions, investigators identified synaptic deficiencies in the hippocampus and striatum with concomitant increases in repetitive behaviors, social behavior deficits, impaired learning and memory, alterations in spine morphology, and glutamate receptor changes [25,26,27,28,29,30,31,32,33,34].
Beyond scaffolding, other synaptic structure proteins have also been implicated in neurodevelopmental deficits. Angelman syndrome, which leads to neurodevelopmental regression in young girls, is associated with maternal deletions of Ube3A. The Ube3A gene encodes the E3 ubiquitin ligase, which is an enzyme that marks synaptic proteins for degradation with ubiquitin. The E3 ubiquitin ligases are known to play important regulatory roles in nervous system development [35]. We know that synaptic refinement is an important component of neurodevelopment, and thus alterations in degradation processes necessary for heterogeneous depression and synaptic refinement could change the ability of stable neural circuits to form. Another important component of synapse structure is synapsins–these proteins are responsible for tethering the synaptic vesicle to the actin cytoskeleton and also assist with synaptic vesicle exocytosis. Mutations in Synapsin genes have been associated with behavioral and learning deficits, as well as schizophrenia. Mice lacking Synapsin genes have reduced object recognition and emotional memory abilities, as well as social interaction deficits [36,37]. Lastly, actin, which is a critical component of the neuronal architecture, helps form the cytoskeleton of the synapse so that scaffolding and stability can properly take place, and alterations in actin-related pathways are associated with neurodevelopmental deficits. In a knock-out mouse model of actin-depolymerizing proteins there is a deficit of actin dynamics and reduced recruitment of synaptic vesicles to the presynaptic active zone [38]. This correlates with human studies associating synaptic actin deficits with severe mental disorders [39].
In addition to synaptic structure, alterations that cause differential synaptic activity are also associated with neurodevelopmental disorders. For example, mutations in the SNAP-25 gene have been associated with Attention-deficit Hyperactivity Disorder (ADHD) [40,41,42] and bipolar disorder [43]. SNAP-25 is an integral part of the SNARE complex and mediates apposition of the synaptic vesicle to the presynaptic membrane for exocytosis [44]. Ablation of SNAP-25 in Drosophila results in a block of synaptic transmission [45,46], and in mouse models with reduced SNAP-25 expression there are behavioral changes such as hyperactivity and impaired learning and memory [47,48,49]. Studies of Swedish children with a single nucleotide polymorphism (SNP) of the SNAP-25 gene show decreased working memory capacity of the GG allele compared to the GA and AA alleles [44]. The SNP was also associated with gray matter density in the posterior cingulate cortex, an area previously associated with attention [50]. Studies of other SNARE proteins discovered a de novo mutation in the syntaxin gene STXBP1 in a patient with Rett Syndrome, which is a disorder associated with severe cognitive impairment [51]. Mutations in the STXBP1 gene are associated with significantly decreased neurotransmission in an in vitro model, suggesting that synaptic activity plays a role in the disease process [52]. In a mouse model, the Parkinson disease (PD)-associated mutation in LRRK2 affects excitatory postsynaptic signaling in the hippocampus and LRRK2 kinase activity increases as mice age, suggesting that developmental alterations of excitatory synaptic activity relate to long-term outcomes [53]. In addition to alterations in overall synaptic activity, studies have associated neurodevelopmental disease with changes in the excitatory/inhibitory balance at the synapse as well. This balance plays a role in the cortex and hippocampus in intellectual disability, ASD, schizophrenia, and AD [54], leading to differential dendritic spine morphology and maintenance [55]. Studies of schizophrenia pathophysiology have shown that hypoactivity of the NMDA receptor affects excitatory glutamate signaling, which then leads to compensatory changes in inhibitory GABA in the hippocampus, prefrontal cortex, and cingulate cortex [56].
2. Environmental Toxicants and Neurodevelopmental Disorders
Synapses start forming in utero and continue to develop and reorganize throughout life through highly coordinated cellular events. While genetics has been shown to play a critical role in these processes, recent epidemiologic and molecular work has demonstrated an important contribution of exposure to environmental chemicals on the proper development and function of the nervous system, especially at the level of the synapse [57,58,59,60,61,62,63,64,65,66,67,68].
Pesticide exposure has previously been linked to neurologic and psychiatric disease in children and adults in various epidemiologic studies. Exposure to various classes of pesticides has been associated with increased risk of ASD [59,69,70], ADHD [71,72], motor and learning impairment [73], structural brain differences [74], as well as neurodegenerative diseases, such as PD [75,76,77], and AD [78]. Pesticides may pass through the placenta based on their lipid solubility properties, and the immaturity of the blood-brain barrier early in development enables pesticide effects very early in life. The lipophilic properties of many pesticides also makes them more likely to concentrate in fatty organs such as the brain [79]. Enzymes involved in metabolizing pesticides have differential activity and expression levels throughout development, and this may also predispose the developing nervous system to elevated concentrations of toxic chemicals. For example, the paraoxonase 1 (PON1) enzyme metabolizes organophosphate compounds and plasma PON1 levels differ throughout development [80]. Additionally, developmental vulnerability to pesticide exposure can continue postnatally, as children may also be highly exposed to environmental toxicants via breast feeding. Given the wide range of neuropsychiatric disorders associated with neurodevelopmental and synaptic disruptions, as well as the multitude of molecular synaptic targets noted above, we explore the potential role of synaptic alterations caused by pesticides in the development of these disorders. Our findings are summarized for ease of reference in Table 1 at the end of this review.
Table 1.
Studies associating pesticide exposure and neurologic function 1.
| Subject | Findings | Reference(s) |
|---|---|---|
| Organochlorines | ||
| Human (Children) | Decr. cognitive, quantitative, verbal, sensory, memory functions; hyporeflexia | [81,82,83,84,85,86,87] |
| Human (Adults) | Decr. neurobehavioral performance | [88] |
| Incr. serum and brain DDE levels associated with AD | [78] | |
| Presence of heptachlor assoc. with Lewy body pathology | [89] | |
| Mice | Incr. DAT, increased DA uptake, VMAT2, TH in striatum | [90,91,92] |
| DA neuron loss in substantia nigra, gliosis in ventral midbrain | [93,94,95,96] | |
| Incr. NE in hippocampus, brainstem | [97] | |
| Incr. 5HT in frontal cortex, decr. 5HT in striatum | [98] | |
| Altered GABAA, GluN2B, D2 receptors in frontal cortex | [58] | |
| Altered CAMKII, GluR1, tau in hippocampus and frontal cortex | [99] | |
| Parkinsonism-like movement | [93] | |
| Motor, cognitive behavioral deficits | [99] | |
| Developmental exposure potentiates MPTP toxicity | [91,100] | |
| Rats | Incr. DAT binding | [101] |
| Mouse cortex primary culture | Decr. synaptic puncta, neurite outgrowth, synaptogenesis | [56,102] |
| Altered MAPK, PI3K/Akt, estrogen receptor pathways | [94] | |
| Incr. NMDA receptor internalization and decr. mGLUR5 levels | [103] | |
| Mouse cerebellum primary culture | Decr. GABAA and NMDA receptors | [104] |
| Organophosphates | ||
| Human (Children) | Decr. IQ, working memory index, cognition | [68,72] |
| Incr. risk of ADHD | [68] | |
| Human (Adults) | Self-reported memory, fatigue, muscle strength issues | [105] |
| Mice | Altered 5HT transporter, 5HT receptors in forebrain, brainstem | [106,107,108] |
| Reduced ChAT, vAchT | [109,110,111] | |
| Learning, memory defects, incr. locomotion | [112,113,114] | |
| Decr. CAMKII in hippocampus, synaptophysin in frontal cortex | [114] | |
| Rats | Decr. muscarinic receptors, decr. AChE activity, ChAT, vAchT | [115,116,117,118,119] |
| Pyrethroids | ||
| Mice | ADHD-like behaviors: working memory and attention deficits, hyperactivity, impulse-like behaviors | [71] |
| Incr. striatal DA uptake mediated by DAT, incr. D1 receptor | [71,120] | |
| Altered GluR1 in hippocampus, altered tau in frontal cortex | [99] | |
| Rats | Striatal administration causes altered extracellular 5HT release | [121] |
| Incr. extracellular glutamate, decr. GABA | [122] | |
1 DDE, 1,1-dichloro-2,2-bis(p-chlorophenyl) ethylene; AD, Alzheimer Disease; DAT, dopamine transporter; DA, dopamine; VMAT2, vesicular monoamine transporter 2; GluN2B, glutamate receptor; CAMKII, calcium/calmodulin-dependent kinase II; GluR1, glutamate receptor 1; MPTP, 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine; MAPK, mitogen-activated protein kinase; NMDA, N-methyl-D-aspartate; ADHD, Attention-Deficit Hyperactivity Disorder; 5HT, serotonin; ChAT, choline acetyltransferase; vAchT, vesicular acetylcholine transporter; AChE, acetylcholinesterase; GABA, γ-aminobutyric acid.
2.1. Organochlorines
Organochlorine (OC) pesticides were mainly used from the 1930s through the 1980s but due to their long half-lives and high degree of lipophilicity persist in our environment and bodies today [123]. OCs are highly chlorinated hydrocarbons that include dichlorodiphenyltrichloroethane (DDT), dieldrin, heptachlor, and endosulfan. OCs bioaccumulate due to their lipophilicity and are known to cross the placenta and excrete in breastmilk [124,125,126,127]. Perhaps most well-known is DDT, whose manufacture and use was banned in the US in 1972 but is still in use for malaria control internationally. DDT slowly metabolizes, primarily into 1,1-dichloro-2,2-bis(p-chlorophenyl) ethylene (DDE), dichlorodiphenyldichloroethane (DDD), and dichlorodiphenylacetic acid (DDA) metabolites. The DDE metabolite is lipophilic and stores in adipose tissue, and is often used as a biomarker of exposure to DDT. While DDT has a variety of effects on neuronal targets it is most effective at holding sodium (Na+) channels in the axonal membrane open, which then leads to prolonged depolarization of the neuron [128,129]. Other OC compounds such as heptachlor, dieldrin, and endosulfan also inhibit the GABAA receptor and Ca2+ ATPase, further contributing to neuronal hyperexcitation [130,131,132,133,134,135,136].
A few epidemiologic exposure studies have examined the relationship between OC pesticide exposure and neurodevelopment. These studies link prenatal OC exposure to numerous functional domains, including reduced cognitive index and memory [81,82], mental and psychomotor development, [83,84,85,137,138,139], fine motor skills [140], reflexes [86,141], social development, attentional processes, and persistently impaired visual processing [87]. Interestingly, while all offspring studied were exposed in utero, effects were still seen up to 11 years later. Furthermore, maternal proximity to agricultural OC pesticide use was associated with increased risk of ASD. Adult cohort studies bolster the evidence that these pesticides affect neurologic function. Although not explicitly focused on neurodevelopment, these other studies are beneficial for understanding the impact of OC exposure on neurologic dysfunction. Notably, such studies observe alterations in the same functional domains studied in children in chronically exposed adults; they perform worse on cognitive, motor, and sensory neurobehavioral tests [88,142]. Additional evidence suggests exposure to OCs is associated with neurodegeneration. Several epidemiologic studies have associated OC exposure with PD risk [75,143,144,145,146,147,148,149,150,151]. Contributing to the epidemiologic evidence are studies that identified OCs in brain samples and blood serum of patients with PD [152,153,154,155]. Additionally, OC exposure is associated with Lewy body pathology, another neurodegenerative process [89]. Taken together, these studies suggest that OCs are associated with impaired neurologic dysfunction in a wide range of functional arenas. Perhaps, common pathways and targets lead to vulnerability that appears either developmentally or later in life. Given the complexity and high level of regulation that must occur during proper neurodevelopment, there are many points at which a misstep could cause downstream consequences. Since the nervous system continues to develop throughout adulthood, these sequelae may not become clinically apparent until much later in life. Furthermore, small alterations early on could potentially cascade into more widespread neurodegenerative changes or neurodegenerative susceptibility as the brain continues to develop and refine.
Molecular and genetic studies elucidate possible pathways of neurologic insult and implicate diverse pre- and postsynaptic components. Presynaptically, our group has identified alterations in key dopaminergic proteins in response to OC pesticides in the striatum and substantia nigra [90,91,102,156]. Additionally, we have observed effects in GABAergic, glutamatergic, and dopaminergic response to endosulfan in the frontal cortex [58]. Others have identified similar dopaminergic changes upon heptachlor exposure, in addition to changes in GABAA, NMDA, and mGluR5 receptors in vitro [93,101,103,104]. Thus, exposure to these OC pesticides induces alterations in presynaptic transport of many neurotransmitter circuits. Altered neurotransmitter transport would likely affect synaptic activity and refinement. Postsynaptically, we observe analogous changes in GABAA receptor, glutamate receptor (GluN2B), and dopamine (D2) receptor levels in the frontal cortex in response to developmental endosulfan exposure [58]. The wide range of neurotransmitter systems affected both pre- and postsynaptically might explain why neurologic effects are observed in an extensive array of functional domains. This is supported by behavioral studies showing defects in motor and cognitive areas of mice exposed to endosulfan [99], as well as tremors and hyperthermia identified in rats exposed to p, p’-DDT [157].
While there are likely changes in overall synaptic activity that occur, alterations in specific brain regions are also important to consider when examining motor, cognitive, and sensory effects. In the hippocampus, for example, developmental endosulfan exposure leads to changes in proteins that regulate the postsynaptic density, synaptic plasticity, and synaptic scaffolding (CAMKII, glutamate receptor 1 (GluR1), and tau, respectively). As one might expect, behavioral alterations also occur in the endosulfan-exposed animals, including differences in spontaneous behavior and habituation deficits [99]. Another postnatal exposure model elicited an increase in norepinephrine in the hippocampus, as well as in the brainstem [97]. Interestingly, a third study that exposed mice to endosulfan during gestation and lactation noted an increase in serotonin (5HT) in the frontal cortex, but a decrease in 5HT in the striatum [98]. Additional studies have looked at frontal cortex neurons in vitro and found a multitude of effects in response to endosulfan exposure. Mouse primary cultures of the frontal cortex have reduced synaptic puncta and neurite outgrowth, with corresponding decreased synaptogenesis in response to endosulfan exposure [58,102]. Molecular pathways associated with synaptogenesis were also altered, such as mitogen-activated protein kinase (MAPK) and phosphatidylinositol-3 kinase (PI3K)/Akt, as well as pathways associated with synaptic plasticity, such as neuronal estrogen receptors [94]. These molecular changes, as well as the associated behavioral outcomes exemplified by animal exposure models, suggest that the aforementioned epidemiologic associations may be mediated by a wide range of alterations to synaptic integrity.
Neurodegenerative studies also provide insight into some of the developmental pathways that are altered because the synapse is a target of these processes as well. Perhaps, early OC pesticide contact leads to similar neurodegenerative effects in humans over an extended period of time. Adult mice exposed to heptachlor exhibit a loss of dopamine (DA) neurons and gliosis in the substantia nigra, a pathologic hallmark of PD. Similarly, adult mice exposed to dieldrin exhibit oxidative damage in the dopaminergic system of the striatum [95]. Interestingly, OC-exposed mice have corresponding motor deficits in the pole and gait tests [93] and alterations in expression and function of the dopamine transporter (DAT) [96]. We know that loss of DA neurons in the substantia nigra is characteristic of PD, but it is possible that earlier exposure causes neurodevelopmental changes of the dopaminergic system that predispose an individual to dopaminergic circuit damage later in adulthood. This was exemplified in studies that exposed mice to dieldrin [91] and heptachlor [100] developmentally and then observed susceptibility of dopaminergic neurons to adult 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) exposure. Thus, alterations in dopaminergic circuitry influence synaptic activity and refinement during development, and this could potentially cause vulnerability to further dopaminergic damage later in life.
2.2. Organophosphates
The first commercial organophosphate (OP) pesticide, parathion, was produced in 1944. Since then, hundreds of OP pesticides have been manufactured and utilized worldwide. Mechanistically, OP function involves phosphorylation and inactivation of acetylcholinesterase. Acetylcholinesterase is the enzyme responsible for hydrolyzing the neurotransmitter acetylcholine at cholinergic synapses in the peripheral and central nervous system. Without hydrolysis, acetylcholine accumulates at the synapse, leading to over-activation of muscarinic and nicotinic receptors on the post-synaptic neuron. Sequelae include uncontrollable salivation, lacrimation, urination, diaphoresis, gastrointestinal upset, emesis, miosis, and muscle spasms due to cholinergic hyperactivity [130].
Several epidemiologic studies illustrate neurotoxic effects of OP exposure that may not be fully explained by the acute acetylcholinesterase action of OPs, as they show additional transmitter systems to also be targeted or disrupted by OP exposure. Neurodevelopmental studies have focused on cognitive, motor, and brain structure abnormalities in children exposed to OP pesticides, uncovering effects that span other neurotransmitter systems and persist well into childhood. One cohort of pregnant women in the Salinas Valley, California, looked at a more chronic exposure scenario and found the women exhibited elevated levels of OP metabolites in urine. The IQ of the offspring at seven years of age was significantly lower in the more highly exposed group [158]. Similarly, exposure to another OP pesticide—chlorpyrifos—was negatively associated with IQ and working memory index, and a Taiwanese cohort of children exposed to OPs were at an increased risk of ADHD. These studies suggest OP exposure may lead to cognitive deficits [68,72], and further cognitive effects are recapitulated in additional cohorts of children [159,160,161,162,163,164,165,166,167,168,169,170]. Studies that investigated more specific cognitive domains show deficits in attention and risk of ADHD [171,172], as well as abnormal psychomotor and reflex development [173,174,175].
Moreover, OP metabolite levels in maternal blood and urine during the third trimester are associated with decreased mental development at 12 months amongst African-Americans and Hispanics. A subset of these subjects with the PON1 Q192R QR/RR genotype appear to have a potentiated association [141]. An additional study shows that lower maternal PON1 enzyme activity levels during pregnancy might potentiate the association between OP exposure during gestation and offspring cognitive development [60]. This is an interesting set of findings because PON1 is one of the enzymes that detoxicates OP pesticides. Differential capabilities to detoxicate OPs may lead to altered susceptibility to OP intoxication. Previous studies show that PON1 activity follows a developmental enzymatic curve, and the previously-described CHAMACOS cohort exhibits differences in PON1 activity between OP-exposed mothers and their neonates [176,177]. Thus, we now know that there is both age-related and genetic vulnerability to OP pesticides associated with PON1 expression, and that this contributes to the evidence suggesting there is neurodevelopmental susceptibility in OP exposures. Besides cognitive development, there also seem to be behavioral effects related to OP exposure. In a study of children in New York City, OP exposure during pregnancy is associated with deficits in social functioning, more so in boys and in African-Americans [178], and in another study in Shenyang, China, OP exposure during pregnancy is associated with decreased neonatal neurobehavioral development [61]. Perhaps most importantly, these aforementioned cognitive and psychomotor alterations have been shown to persist once the exposure is removed, and well into adulthood in several studies [105,179,180,181,182]. Interestingly, in addition to cognitive and behavioral deficits, OP exposure is associated with gross structural changes as well, including decreased cortical thickness and a loss of expected morphologic sex differences in the brains of offspring exposed to chlorpyrifos in utero [74]. Lastly, acute OP exposure in infancy, another highly vulnerable time point of exposure, is associated with deficits in verbal learning and inhibitory motor control in school-aged children [73]. Taken together, these diverse neurodevelopmental changes are probably not wholly explained by the target effects of OPs on acetylcholinesterase and instead suggest there may be a more widespread mechanism.
Contributing to the observations made in epidemiologic studies, molecular studies suggest that multiple components necessary for a properly-functioning synapse are affected in the context of OP pesticide exposure. For example, 5HT neurotransmission plays an important role in regulation and differentiation throughout the developing brain, and alterations therein would likely affect multiple functional domains. Indeed, exposure to chlorpyrifos is associated with altered expression of presynaptic 5HT transporter, postsynaptic 5HT receptors (5HT1a, 5HT2), and downstream 5HT signal transduction in various brain regions, including the forebrain and brainstem [106,107,108]. There may therefore be changes occurring in the serotonergic system during critical windows of neurodevelopment, but also during later periods of neurotransmission-related refinement of serotonergic circuits. In addition to the serotonergic system, the cholinergic system appears to be affected as well. Although AChE is the target during acute OP intoxication, chronic low-level exposure also appears to affect components of the cholinergic system both prenatally and postnatally. For instance, offspring of chlorpyrifos-exposed mice showed reductions in the presynaptic choline transporter (ChAT), which returns choline to the neuron once acetylcholine is broken down by AChE [109]. Other cholinergic system proteins, such as the vesicular acetycholine transporter (vAchT), which transports acetylcholine into synaptic vesicles for release, and muscarinic receptors, which interact with acetylcholine once it is released, are affected as well [110]. These findings correlate well with animal behavior findings that indicate offspring have learning and memory defects, and increased locomotor activity [112]. Interestingly, chlorpyrifos exposure in mice in utero is associated with a decrease in activity of the presynaptic ChAT, but this association occurs neonatally, disappears during weaning, and then reappears in adolescence and adulthood [111]. Given that neurodevelopment proceeds all the way through adolescence and young adulthood, it is likely that cholinergic changes affect neurotransmission across more than one developmental window. These molecular results are supported by electrophysiology studies that indicate repeated chlorpyrifos administration initially enhances and then decreases synaptic transmission in the hippocampus [183], and by behavioral studies showing that cholinergic dysfunction affects working and reference memory [112]. Further studies of postnatal OP exposure also indicate the cholinergic system is affected in ways analogous to prenatal OP exposure; there are reductions in muscarinic and nicotinic receptors that normally interact with acetylcholine, as well as reductions in transporters ChAT and vAchT [115,116,117,118,119,184,185]. These data suggest exposure in various neurodevelopmental stages can affect major neurotransmitter systems, and these effects persist, as indicated by cognitive task studies performed several months after mice were initially exposed to chlorpyrifos [113]. It has also been proposed that OP-mediated disturbances of the choline and DA systems, instead of neurotransmitter-specific system pathologies, could lead to the OP-associated neurologic outcomes [186]. Further studies indicate that changes occur not only at synapses of specific neurotransmitter systems. Rather, alterations in proteins more ubiquitously expressed in synapses occur too. For example, CAMKII plays a role in synaptic plasticity as well as learning and memory, and neonatal chlorpyrifos exposure is associated with decreased CAMKII in the hippocampus and decreased habituation in behavioral studies. A process important for learning is synaptic vesicle recycling, and synaptophysin—a CAMKII substrate—is a mediator of this process. A decrease in synaptophysin occurs in the frontal cortex of the neonatally exposed mice and this might also contribute to a common pathway that results in habituation and learning deficits [114]. Thus, various functional synapse components are altered in response to OP pesticide exposure. Perhaps the wide range of neurologic and psychiatric effects observed in epidemiologic studies are due to a common synapse pathology.
2.3. Pyrethroids
Exposure to pyrethroids has been characterized worldwide, and occurs via agriculture, household use, and dietary ingestion [187,188,189,190,191,192]. Pyrethroids are synthetic analogues of pyrethrins, compounds derived from Chrysanthemum cinerariaefolium, that bind the α subunit of voltage-gated Na+ channels to hold them open and cause neuronal hyperexcitability [130]. Type II pyrethroids can also inhibit GABAA-gated and voltage-gated chloride channels and increase excitability [193]. Off-target effects on the Ca2+ ATPase and voltage-gated Ca2+ channels have also been reported [194]. While actions at these channels do not appear to explain the acute intoxication syndromes, actions at these channels could explain some neurodevelopmental effects [195].
Of note, this is the newest class of pesticides discussed in this review. To our knowledge, few epidemiologic studies have been published and neurodevelopmental data is limited. There are a few studies, though, indicating that pyrethroid exposure is still of interest in examining adverse neurodevelopmental outcomes. Notably, children in the NHANES study with pyrethroid metabolites detectable in urine have an increased risk of ADHD [71], and this association appears to be higher in boys and with hyperactive-impulse symptoms [63]. Also, prenatal exposure to piperonyl butoxide, an additive that potentiates the action of pyrethroids, is negatively associated with cognitive and motor development at 36 months of age in a cohort of black, Dominican mothers [196]. Furthermore, there is an association between urinary pyrethroid metabolites and parent-reported behavioral problems [197] and IQ [198]. These results suggest there may be cognitive and motor sequelae associated with pyrethroid exposure. Conversely, a Thai case-control study saw no statistically significant differences in urinary pyrethroid metabolites and neurobehavioral testing at six month intervals [199]. As such, there is not yet a definitive body of work indicating pyrethroids are linked to neurodevelopmental or neurodegenerative outcomes. Taken together, however, the newer use of pyrethroids may be contributing to the lack of definitive epidemiologic data and further study of longitudinal, neurodevelopmental exposure effects are still of interest.
Like the effects observed in OP and OC pesticide exposure, biological studies again identify synaptic components as potentially vulnerable to neurodevelopmental pyrethroid exposure. Alterations in neurotransmitter systems and synaptic structure have been illustrated. The dopaminergic system was implicated in a developmental deltamethrin exposure model, where mice exhibited increased DAT and dopamine D1 receptor expression and coincident ADHD-like behaviors, such as working memory deficits, attention deficits, hyperactivity, and impulse-like behaviors [71]. Cypermethrin exposure in the neonatal period led to alterations in GluR1 in the hippocampus and tau in the frontal cortex. As discussed earlier, GluR1 and tau both play important roles in synaptic plasticity and scaffolding, respectively. These structural changes likely contribute to the observed behavioral outcomes: decreased rearing, locomotion, and habituation in the exposed mice [99].
More of the molecular data pertains to adult models, but these studies hint at pathways likely to be affected in neurodevelopment as well. Reflecting dopaminergic changes seen in neonatal exposure, treatment of adult mice with deltamethrin and permethrin increased maximal DA uptake and permethrin treatment also increased striatal DAT levels [92,200]. This increase in DA uptake is mediated by DAT [65], and alterations in DA efflux were replicated in experiments directly injecting allethrin, deltamethrin, and cyhalothrin into the rat striatum. Perhaps, alterations in Na+ and Ca2+ channel activity in either DA synaptic terminals or GABA interneurons lead to the observed changes in DA efflux [120]. As with OC and OP pesticides, pyrethroid pesticide exposure causes changes in other neurotransmitter systems beyond DA. Administration of allethrin, cyhalothrin and deltamethrin into the rat striatum also causes changes in extracellular 5HT release. The striatum is highly innervated with serotonergic neurons, and earlier studies have shown that a reduction of 5HT leads to increased aggressive and locomotor behaviors, while a rise in 5HT leads to the opposite behavioral effects [121]. These dopaminergic and serotonergic changes could contribute to the motor and cognitive behaviors observed in epidemiologic studies and animal behavior models. Beyond neurotransmitter-specific synaptic components, pyrethroid exposure alters the balance of inhibitory and excitatory signaling. This could potentially affect neuronal signaling and synaptic activity, and the related processes of synaptic plasticity and refinement. In the hippocampus, for example, the balance of inhibitory GABAergic and excitatory glutamatergic signaling affects learning and memory. Indeed, exposure to allethrin, deltamethrin, and cyhalothrin in a rat exposure model leads to compound-specific alterations to GABA and glutamate release in the hippocampus, suggesting that these pyrethroids could play a role in cognitive outcomes observed in other studies [122]. All of these effects on synaptic function occur in adult animals, but given the high degree of coordination necessary for proper neurodevelopment, could potentially have similar or even more devastating effects in developmental models.
3. Summary
Considerable evidence suggests that exposure to a variety of pesticides can contribute to neurodevelopmental disorders. While the cellular and molecular underpinnings that motivate these deficits are still being investigated, it appears that the synapse is a vulnerable target for disruption by these compounds. Of the current studies, developmental exposure to OC, OP, and pyrethroid pesticides each appears to impact expression of neuronal targets critical to synaptic function. These synaptic targets include both pre- and postsynaptic components. The synaptic alterations appear to be relatively promiscuous, and not selective for a particular neurotransmitter circuit or brain region. This highlights the importance of the developing synapse for toxicant-mediated neurodevelopmental disease.
There are a multitude of neurodevelopmental effects associated with pesticide exposure, and these effects span from axonal outgrowth and synaptogenesis to synaptic activity and refinement. Given the level of complexity and organization demanded of neural circuits for proper neurologic function, it is highly likely that even subtle changes in synapse structure, function, and stability could lead to lasting modifications of cognition, movement, and sensation that are not necessarily drastic pathologically. Chronic low-level exposure of pesticides has been shown to affect various pathways related to the synapse. As such, synaptic endpoints should be considered when identifying potential harm of pesticides and other environmental exposures. Observed changes in dopaminergic, serotonergic, GABAergic, and glutamatergic neurotransmission could contribute to behavioral changes and alterations in learning and memory. In addition, changes in pathways related to synaptogenesis, such as altered expression of CAMKII, tau, and GluR1, could further contribute to the observed phenotypes.
4. Future Directions
Further work examining the consequences of synaptic aberrations can yield a better understanding of neurodevelopment and the progression of neurological disease in general. As exemplified in this review, the impact of altered synapse development and function is widespread and persistent. In the context of environmental toxicant exposure, the synapse appears to be a common target for damage. However, using lab-based model systems with acute, high-dose pesticide exposure may not accurately represent an environmentally-relevant exposure paradigm, which is often comprised of chronic, low dose exposures. This subthreshold exposure scenario is critical to consider as more people may be exposed in this manner, and exposed individuals likely experience unmonitored, off-target effects that could take years to manifest as neurological disorders.
Given the vast amount of pesticides currently in use and the wide range of effects synapse dysfunction has on neurologic outcomes, it is beneficial to hone in on more sensitive biomarkers of synaptic dysfunction. Developing more sensitive synaptic measures allows for a more accurate assessment of synaptic damage that occurs. Additionally, these endpoints enable detection of damage in specific neuronal populations, which then pinpoint more explicit functional outcomes. To this end, high-throughput proteomic and metabolomic techniques could be utilized to more broadly identify synapse pathology and screen multiple compounds at a faster pace. Evaluating alterations to these targets can be furthered at a molecular level by using epigenetics to pinpoint possible toxicant-induced modifications to protein expression. These protein expression modifications might then lead to an elaborated understanding of the mechanisms of synapse pathology. Previous studies show that pesticide exposure induces epigenetic changes [201] that lead to neurotoxicity. More specifically, it has been shown that exposure to the OC pesticide dieldrin increases histone acetylation and subsequently induces apoptosis in dopaminergic neurons [202]. Furthermore, exposure to the pyrethroid pesticide permethrin induces changes in DNA methylation of Nurr1, a transcription factor that regulates TH, DAT, and dopamine receptor expression [203]. Our group showed that exposure to the organochlorine pesticides heptachlor and dieldrin also induces changes in not only methylation of Nurr1, but also Pitx3, another transcription factor involved in regulating DAT, as well as vesicular monoamine transporter 2 (VMAT2) expression [91,100]. Thus, pesticide exposure elicits changes in DNA transcription that may precede the molecular changes discussed in this review, or that may predispose individuals to respond more significantly to continued pesticide exposures. Identifying these transcription changes will be crucial for piecing together the molecular cascades that affect synapses upon exposure to pesticides.
In developing more sensitive endpoints and advancing our understanding of neurodevelopmental effects of pesticides, it will be important to identify thresholds at which synaptic dysfunction leads to alterations in neural circuitry development and behavior. It is possible that synaptic changes that produce subthreshold developmental outcomes eventually do meet a threshold, causing neurodegeneration and other neuropsychiatric disorders. This work would contribute evidence to the fetal basis of adult disease (FOAD) hypothesis, first introduced by David Barker in the context of cardiovascular disease [204]. Barker proposed that developmental aberrations occurring in the fetal stage might in part predict adult disease outcomes. This has been studied somewhat in neurologic disease, but warrants further study—prospective animal studies show that brain inflammation associated with maternal inflammation may potentiate vulnerability to heavy metals and pesticides later in life [205], and previously-mentioned epidemiologic studies show that earlier pesticide exposure increases the risk of developing neurodegenerative diseases such as PD. Thus, adding to the currently available longitudinal studies of children exposed during neurodevelopment would provide valuable information about the potential development of neuropsychiatric disorders such as schizophrenia and bipolar disorder, which are often not seen until early adulthood, as well as the development of neurodegenerative disorders such as PD and AD, which are usually not apparent until the second half of life. Lastly, studying which brain regions are susceptible to synaptic dysfunction in response to environmental exposure enables us to anticipate important endpoints to examine in later chemical risk assessments. To do so, imaging studies could be used to analyze the entire brain in animal exposure models throughout development. Identifying regions vulnerable to specific pathologies and associated behavioral outcomes allows for more targeted exposure measurements in subsequent tissue samples.
A large body of work has provided correlations of molecular changes and behavioral abnormalities, but there is a general lack of integration of the molecular and behavioral findings, so that there is little more beyond the associative data. Crucial to our understanding will be further functional studies that examine the mechanistic sequelae of these identified synaptic changes. This will allow the field to make causal deductions, in addition to the correlational ones, about the role of synapse effects in neurodevelopment. Functional studies might include additional electrophysiology or functional MRI studies. Discovery of new synaptic endpoints and regional vulnerability described above will contribute to the development of these functional experiments, and will allow us to prove more specific pathways. Moreover, adding epidemiologic and clinical data to molecular data will push our understanding even further. Epidemiologic studies could be used to assess genetic factors that would modify the effects of environmental exposures. For example, studying the interaction of genetic variation and pesticide exposure in neurodevelopment could provide additional information about the susceptibility of individuals to disease development. De Felice et al. recently conducted a study in which a validated idiopathic autism transgenic mouse was prenatally exposed to chlorpyrifos at a sub-toxic dose. The authors found that the chlorpyrifos-exposed mice displayed delayed motor maturation in pups, as well as an altered pattern of sexual partner interaction associated with increased ultrasound vocalization in adult males [67]. Similar studies could examine polymorphisms of synaptic protein genes and vulnerability to pesticide exposure effects. Given the extended length of neurodevelopmental processes, it would be important to study effects of continued exposure from the prenatal to adult stages. As an initial step, the neuronal synapse proves to be a valuable objective because many of the pesticide compounds currently available target synaptic components in some way. Based on the wide range of disorders linked to synaptic alterations, improper synaptogenesis and synaptic activity appears to play a central role in the development of neurologic and psychiatric disorders after pesticide exposure.
Acknowledgments
This work was supported by National Institutes of Health grant R00ES017477 to W.M.C.
Author Contributions
A.V. and W.M.C. both wrote the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Purves D., Augustine G.J., Fitzpatrick D., Katz L.C., LaMantia A.-S., McNamara J.O., Williams S.M. Neuroscience. 5th ed. Sinauer Associates; Sunderland, MA, USA: 2001. Neuronal Migration. [Google Scholar]
- 2.Sanes D.H., Reh T.A., Harris W.A. Development of the Nervous System. 3rd ed. Academic Press; Cambridge, MA, USA: 2000. [Google Scholar]
- 3.Sudhof T.C. Neuroligins and neurexins link synaptic function to cognitive disease. Nature. 2008;455:903–911. doi: 10.1038/nature07456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arikkath J., Reichardt L.F. Cadherins and catenins at synapses: Roles in synaptogenesis and synaptic plasticity. Trends Neurosci. 2008;31:487–494. doi: 10.1016/j.tins.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ivanova D., Dirks A., Fejtova A. Bassoon and piccolo regulate ubiquitination and link presynaptic molecular dynamics with activity-regulated gene expression. J. Physiol. 2016 doi: 10.1113/JP271826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Purves D. Neuroscience. Sinauer Associates; Sunderland, MA, USA: 2012. [Google Scholar]
- 7.Sala C., Vicidomini C., Bigi I., Mossa A., Verpelli C. Shank synaptic scaffold proteins: Keys to understanding the pathogenesis of autism and other synaptic disorders. J. Neurochem. 2015;135:849–858. doi: 10.1111/jnc.13232. [DOI] [PubMed] [Google Scholar]
- 8.Lin R.C., Scheller R.H. Mechanisms of synaptic vesicle exocytosis. Annu. Rev. Cell Dev. Biol. 2000;16:19–49. doi: 10.1146/annurev.cellbio.16.1.19. [DOI] [PubMed] [Google Scholar]
- 9.Ropper A.H., Samuels M.A., Klein J.P. Adams and Victor’s Principles of Neurology, 10e. The McGraw-Hill Companies; New York, NY, USA: 2014. Chapter 28. Normal development and deviations in development of the nervous system. [Google Scholar]
- 10.Waxman S.G. Clinical Neuroanatomy, 27e. The McGraw-Hill Companies; New York, NY, USA: 2013. Chapter 2. Development and cellular constituents of the nervous system. [Google Scholar]
- 11.Rice D., Barone S., Jr. Critical periods of vulnerability for the developing nervous system: Evidence from humans and animal models. Environ. Health Perspect. 2000;108:511–533. doi: 10.1289/ehp.00108s3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Etherton M., Foldy C., Sharma M., Tabuchi K., Liu X., Shamloo M., Malenka R.C., Sudhof T.C. Autism-linked neuroligin-3 R451c mutation differentially alters hippocampal and cortical synaptic function. Proc. Natl. Acad. Sci. USA. 2011;108:13764–13769. doi: 10.1073/pnas.1111093108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tabuchi K., Blundell J., Etherton M.R., Hammer R.E., Liu X., Powell C.M., Sudhof T.C. A neuroligin-3 mutation implicated in autism increases inhibitory synaptic transmission in mice. Science. 2007;318:71–76. doi: 10.1126/science.1146221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burrows E.L., Laskaris L., Koyama L., Churilov L., Bornstein J.C., Hill-Yardin E.L., Hannan A.J. A neuroligin-3 mutation implicated in autism causes abnormal aggression and increases repetitive behavior in mice. Mol. Autism. 2015;6 doi: 10.1186/s13229-015-0055-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jamain S., Radyushkin K., Hammerschmidt K., Granon S., Boretius S., Varoqueaux F., Ramanantsoa N., Gallego J., Ronnenberg A., Winter D., et al. Reduced social interaction and ultrasonic communication in a mouse model of monogenic heritable autism. Proc. Natl. Acad. Sci. USA. 2008;105:1710–1715. doi: 10.1073/pnas.0711555105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blundell J., Blaiss C.A., Etherton M.R., Espinosa F., Tabuchi K., Walz C., Bolliger M.F., Sudhof T.C., Powell C.M. Neuroligin-1 deletion results in impaired spatial memory and increased repetitive behavior. J. Neurosci. 2010;30:2115–2129. doi: 10.1523/JNEUROSCI.4517-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sheng M., Kim E. The shank family of scaffold proteins. J. Cell Sci. 2000;113:1851–1856. doi: 10.1242/jcs.113.11.1851. [DOI] [PubMed] [Google Scholar]
- 18.Peykov S., Berkel S., Schoen M., Weiss K., Degenhardt F., Strohmaier J., Weiss B., Proepper C., Schratt G., Nothen M.M., et al. Identification and functional characterization of rare shank2 variants in schizophrenia. Mol. Psychiatry. 2015;20:1489–1498. doi: 10.1038/mp.2014.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cochoy D.M., Kolevzon A., Kajiwara Y., Schoen M., Pascual-Lucas M., Lurie S., Buxbaum J.D., Boeckers T.M., Schmeisser M.J. Phenotypic and functional analysis of shank3 stop mutations identified in individuals with asd and/or id. Mol. Autism. 2015;6 doi: 10.1186/s13229-015-0020-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Soorya L., Kolevzon A., Zweifach J., Lim T., Dobry Y., Schwartz L., Frank Y., Wang A.T., Cai G., Parkhomenko E., et al. Prospective investigation of autism and genotype-phenotype correlations in 22q13 deletion syndrome and shank3 deficiency. Mol. Autism. 2013;4:18. doi: 10.1186/2040-2392-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leblond C.S., Nava C., Polge A., Gauthier J., Huguet G., Lumbroso S., Giuliano F., Stordeur C., Depienne C., Mouzat K., et al. Meta-analysis of shank mutations in autism spectrum disorders: A gradient of severity in cognitive impairments. PLoS Genet. 2014;10 doi: 10.1371/journal.pgen.1004580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ey E., Torquet N., Le Sourd A.M., Leblond C.S., Boeckers T.M., Faure P., Bourgeron T. The autism prosap1/shank2 mouse model displays quantitative and structural abnormalities in ultrasonic vocalisations. Behav. Brain Res. 2013;256:677–689. doi: 10.1016/j.bbr.2013.08.031. [DOI] [PubMed] [Google Scholar]
- 23.Sungur A.O., Vorckel K.J., Schwarting R.K., Wohr M. Repetitive behaviors in the shank1 knockout mouse model for autism spectrum disorder: Developmental aspects and effects of social context. J. Neurosci. Methods. 2014;234:92–100. doi: 10.1016/j.jneumeth.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 24.Wohr M. Ultrasonic Vocalizations in Shank Mouse Models for Autism Spectrum Disorders: Detailed Spectrographic Analyses and Developmental Profiles. Neurosci. Biobehav. Rev. 2014;43:199–212. doi: 10.1016/j.neubiorev.2014.03.021. [DOI] [PubMed] [Google Scholar]
- 25.Kouser M., Speed H.E., Dewey C.M., Reimers J.M., Widman A.J., Gupta N., Liu S., Jaramillo T.C., Bangash M., Xiao B., et al. Loss of predominant shank3 isoforms results in hippocampus-dependent impairments in behavior and synaptic transmission. J. Neurosci. 2013;33:18448–18468. doi: 10.1523/JNEUROSCI.3017-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jaramillo T.C., Speed H.E., Xuan Z., Reimers J.M., Liu S., Powell C.M. Altered striatal synaptic function and abnormal behaviour in shank3 exon4–9 deletion mouse model of autism. Autism Res. 2016;9:350–375. doi: 10.1002/aur.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jiang Y.H., Ehlers M.D. Modeling autism by shank gene mutations in mice. Neuron. 2013;78:8–27. doi: 10.1016/j.neuron.2013.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Speed H.E., Kouser M., Xuan Z., Reimers J.M., Ochoa C.F., Gupta N., Liu S., Powell C.M. Autism-associated insertion mutation (InsG) of shank3 exon 21 causes impaired synaptic transmission and behavioral deficits. J. Neurosci. 2015;35:9648–9665. doi: 10.1523/JNEUROSCI.3125-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kozol R.A., Cukier H.N., Zou B., Mayo V., De Rubeis S., Cai G., Griswold A.J., Whitehead P.L., Haines J.L., Gilbert J.R., et al. Two knockdown models of the autism genes syngap1 and shank3 in zebrafish produce similar behavioral phenotypes associated with embryonic disruptions of brain morphogenesis. Hum. Mol. Genet. 2015;24:4006–4023. doi: 10.1093/hmg/ddv138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Uppal N., Puri R., Yuk F., Janssen W.G., Bozdagi-Gunal O., Harony-Nicolas H., Dickstein D.L., Buxbaum J.D., Hof P.R. Ultrastructural analyses in the hippocampus CA1 field in shank3-deficient mice. Mol. Autism. 2015;6:41. doi: 10.1186/s13229-015-0036-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang X., Bey A.L., Katz B.M., Badea A., Kim N., David L.K., Duffney L.J., Kumar S., Mague S.D., Hulbert S.W., et al. Altered mglur5-homer scaffolds and corticostriatal connectivity in a shank3 complete knockout model of autism. Nat. Commun. 2016;7:11459. doi: 10.1038/ncomms11459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang X., McCoy P.A., Rodriguiz R.M., Pan Y., Je H.S., Roberts A.C., Kim C.J., Berrios J., Colvin J.S., Bousquet-Moore D., et al. Synaptic dysfunction and abnormal behaviors in mice lacking major isoforms of shank3. Hum. Mol. Genet. 2011;20:3093–3108. doi: 10.1093/hmg/ddr212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bozdagi O., Sakurai T., Papapetrou D., Wang X., Dickstein D.L., Takahashi N., Kajiwara Y., Yang M., Katz A.M., Scattoni M.L., et al. Haploinsufficiency of the autism-associated SHANK3 gene leads to deficits in synaptic function, social interaction, and social communication. Mol. Autism. 2010;1:15. doi: 10.1186/2040-2392-1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Duffney L.J., Zhong P., Wei J., Matas E., Cheng J., Qin L., Ma K., Dietz D.M., Kajiwara Y., Buxbaum J.D., et al. Autism-like deficits in shank3-deficient mice are rescued by targeting actin regulators. Cell Rep. 2015;11:1400–1413. doi: 10.1016/j.celrep.2015.04.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mabb A.M., Judson M.C., Zylka M.J., Philpot B.D. Angelman Syndrome: Insights into genomic imprinting and neurodevelopmental phenotypes. Trends Neurosci. 2011;34:293–303. doi: 10.1016/j.tins.2011.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Porton B., Wetsel W.C., Kao H.T. Synapsin Iii: Role in neuronal plasticity and disease. Semin. Cell Dev. Biol. 2011;22:416–424. doi: 10.1016/j.semcdb.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cesca F., Baldelli P., Valtorta F., Benfenati F. The synapsins: Key actors of synapse function and plasticity. Prog. Neurobiol. 2010;91:313–348. doi: 10.1016/j.pneurobio.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 38.Kevenaar J.T., Hoogenraad C.C. The axonal cytoskeleton: From organization to function. Front. Mol. Neurosci. 2015;8:44. doi: 10.3389/fnmol.2015.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Benesh A.E., Fleming J.T., Chiang C., Carter B.D., Tyska M.J. Expression and localization of myosin-1d in the developing nervous system. Brain Res. 2012;1440:9–22. doi: 10.1016/j.brainres.2011.12.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barr C.L., Feng Y., Wigg K., Bloom S., Roberts W., Malone M., Schachar R., Tannock R., Kennedy J.L. Identification of DNA variants in the snap-25 gene and linkage study of these polymorphisms and attention-deficit hyperactivity disorder. Mol. Psychiatry. 2000;5:405–409. doi: 10.1038/sj.mp.4000733. [DOI] [PubMed] [Google Scholar]
- 41.Brophy K., Hawi Z., Kirley A., Fitzgerald M., Gill M. Synaptosomal-associated protein 25 (snap-25) and attention deficit hyperactivity disorder (adhd): Evidence of linkage and association in the Irish population. Mol. Psychiatry. 2002;7:913–917. doi: 10.1038/sj.mp.4001092. [DOI] [PubMed] [Google Scholar]
- 42.Kustanovich V., Merriman B., McGough J., McCracken J.T., Smalley S.L., Nelson S.F. Biased paternal transmission of snap-25 risk alleles in attention-deficit hyperactivity disorder. Mol. Psychiatry. 2003;8:309–315. doi: 10.1038/sj.mp.4001247. [DOI] [PubMed] [Google Scholar]
- 43.Etain B., Dumaine A., Mathieu F., Chevalier F., Henry C., Kahn J.P., Deshommes J., Bellivier F., Leboyer M., Jamain S. A snap25 promoter variant is associated with early-onset bipolar disorder and a high expression level in brain. Mol. Psychiatry. 2010;15:748–755. doi: 10.1038/mp.2008.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Antonucci F., Corradini I., Fossati G., Tomasoni R., Menna E., Matteoli M. Snap-25, a known presynaptic protein with emerging postsynaptic functions. Front. Synaptic. Neurosci. 2016;8:7. doi: 10.3389/fnsyn.2016.00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Littleton J.T., Chapman E.R., Kreber R., Garment M.B., Carlson S.D., Ganetzky B. Temperature-sensitive paralytic mutations demonstrate that synaptic exocytosis requires snare complex assembly and disassembly. Neuron. 1998;21:401–413. doi: 10.1016/S0896-6273(00)80549-8. [DOI] [PubMed] [Google Scholar]
- 46.Kidokoro Y. roles of snare proteins and synaptotagmin I in synaptic transmission: Studies at the drosophila neuromuscular synapse. Neurosignals. 2003;12:13–30. doi: 10.1159/000068912. [DOI] [PubMed] [Google Scholar]
- 47.Hess E.J., Jinnah H.A., Kozak C.A., Wilson M.C. Spontaneous locomotor hyperactivity in a mouse mutant with a deletion including the snap gene on chromosome 2. J. Neurosci. 1992;12:2865–2874. doi: 10.1523/JNEUROSCI.12-07-02865.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ohira K., Kobayashi K., Toyama K., Nakamura H.K., Shoji H., Takao K., Takeuchi R., Yamaguchi S., Kataoka M., Otsuka S., et al. Synaptosomal-associated protein 25 mutation induces immaturity of the dentate granule cells of adult mice. Mol. Brain. 2013;6:12. doi: 10.1186/1756-6606-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Steffensen S.C., Wilson M.C., Henriksen S.J. Coloboma contiguous gene deletion encompassing snap alters hippocampal plasticity. Synapse. 1996;22:281–289. doi: 10.1002/(SICI)1098-2396(199603)22:3<281::AID-SYN11>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 50.Soderqvist S., McNab F., Peyrard-Janvid M., Matsson H., Humphreys K., Kere J., Klingberg T. The snap25 gene is linked to working memory capacity and maturation of the posterior cingulate cortex during childhood. Biol. Psychiatry. 2010;68:1120–1125. doi: 10.1016/j.biopsych.2010.07.036. [DOI] [PubMed] [Google Scholar]
- 51.Romaniello R., Saettini F., Panzeri E., Arrigoni F., Bassi M.T., Borgatti R. A de-novo stxbp1 gene mutation in a patient showing the rett syndrome phenotype. Neuroreport. 2015;26:254–257. doi: 10.1097/WNR.0000000000000337. [DOI] [PubMed] [Google Scholar]
- 52.Patzke C., Han Y., Covy J., Yi F., Maxeiner S., Wernig M., Sudhof T.C. Analysis of conditional heterozygous stxbp1 mutations in human neurons. J. Clin. Investig. 2015;125:3560–3571. doi: 10.1172/JCI78612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sweet E.S., Saunier-Rebori B., Yue Z., Blitzer R.D. The parkinson’s disease-associated mutation lrrk2-g2019s impairs synaptic plasticity in mouse hippocampus. J. Neurosci. 2015;35:11190–11195. doi: 10.1523/JNEUROSCI.0040-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Penzes P., Buonanno A., Passafaro M., Sala C., Sweet R.A. Developmental vulnerability of synapses and circuits associated with neuropsychiatric disorders. J. Neurochem. 2013;126:165–182. doi: 10.1111/jnc.12261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Penzes P., Cahill M.E., Jones K.A., VanLeeuwen J.E., Woolfrey K.M. Dendritic spine pathology in neuropsychiatric disorders. Nat. Neurosci. 2011;14:285–293. doi: 10.1038/nn.2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Coyle J.T. Glutamate and schizophrenia: Beyond the dopamine hypothesis. Cell. Mol. Neurobiol. 2006;26:365–384. doi: 10.1007/s10571-006-9062-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Howard A.S., Bucelli R., Jett D.A., Bruun D., Yang D., Lein P.J. Chlorpyrifos exerts opposing effects on axonal and dendritic growth in primary neuronal cultures. Toxicol. Appl. Pharmacol. 2005;207:112–124. doi: 10.1016/j.taap.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 58.Caudle W.M. Vulnerability of synapses in the frontal cortex of mice developmentally exposed to an insecticide: Potential contribution to neuropsychiatric disease. Neurotransmitter (Houst.) 2015;2 doi: 10.14800/nt.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shelton J.F., Geraghty E.M., Tancredi D.J., Delwiche L.D., Schmidt R.J., Ritz B., Hansen R.L., Hertz-Picciotto I. Neurodevelopmental disorders and prenatal residential proximity to agricultural pesticides: The charge study. Environ. Health Perspect. 2014;122:1103–1109. doi: 10.1289/ehp.1307044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Eskenazi B., Kogut K., Huen K., Harley K.G., Bouchard M., Bradman A., Boyd-Barr D., Johnson C., Holland N. Organophosphate pesticide exposure, pon1, and neurodevelopment in school-age children from the chamacos study. Environ. Res. 2014;134:149–157. doi: 10.1016/j.envres.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang Y., Han S., Liang D., Shi X., Wang F., Liu W., Zhang L., Chen L., Gu Y., Tian Y. Prenatal exposure to organophosphate pesticides and neurobehavioral development of neonates: A birth cohort study in shenyang, China. PLoS ONE. 2014;9:e88491. doi: 10.1371/journal.pone.0088491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Quiros-Alcala L., Mehta S., Eskenazi B. Pyrethroid pesticide exposure and parental report of learning disability and attention deficit/hyperactivity disorder in US. children: Nhanes 1999–2002. Environ. Health Perspect. 2014;122:1336–1342. doi: 10.1289/ehp.1308031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wagner-Schuman M., Richardson J.R., Auinger P., Braun J.M., Lanphear B.P., Epstein J.N., Yolton K., Froehlich T.E. Association of pyrethroid pesticide exposure with attention-deficit/hyperactivity disorder in a nationally representative sample of US. children. Environ. Health. 2015;14:44. doi: 10.1186/s12940-015-0030-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shafer T.J., Meyer D.A., Crofton K.M. Developmental neurotoxicity of pyrethroid insecticides: Critical review and future research needs. Environ. Health Perspect. 2005;113:123–136. doi: 10.1289/ehp.7254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Elwan M.A., Richardson J.R., Guillot T.S., Caudle W.M., Miller G.W. Pyrethroid pesticide-induced alterations in dopamine transporter function. Toxicol. Appl. Pharmacol. 2006;211:188–197. doi: 10.1016/j.taap.2005.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ansari R.W., Shukla R.K., Yadav R.S., Seth K., Pant A.B., Singh D., Agrawal A.K., Islam F., Khanna V.K. Cholinergic dysfunctions and enhanced oxidative stress in the neurobehavioral toxicity of lambda-cyhalothrin in developing rats. Neurotox. Res. 2012;22:292–309. doi: 10.1007/s12640-012-9313-z. [DOI] [PubMed] [Google Scholar]
- 67.De Felice A., Scattoni M.L., Ricceri L., Calamandrei G. Prenatal exposure to a common organophosphate insecticide delays motor development in a mouse model of idiopathic autism. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0121663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rauh V., Arunajadai S., Horton M., Perera F., Hoepner L., Barr D.B., Whyatt R. Seven-year neurodevelopmental scores and prenatal exposure to chlorpyrifos, a common agricultural pesticide. Environ. Health Perspect. 2011;119:1196–1201. doi: 10.1289/ehp.1003160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sealey L.A., Hughes B.W., Sriskanda A.N., Guest J.R., Gibson A.D., Johnson-Williams L., Pace D.G., Bagasra O. Environmental factors in the development of autism spectrum disorders. Environ. Int. 2016;88:288–298. doi: 10.1016/j.envint.2015.12.021. [DOI] [PubMed] [Google Scholar]
- 70.Shelton J.F., Hertz-Picciotto I., Pessah I.N. Tipping the balance of autism risk: Potential mechanisms linking pesticides and autism. Environ. Health Perspect. 2012;120:944–951. doi: 10.1289/ehp.1104553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Richardson J.R., Taylor M.M., Shalat S.L., Guillot T.S., 3rd, Caudle W.M., Hossain M.M., Mathews T.A., Jones S.R., Cory-Slechta D.A., Miller G.W. Developmental pesticide exposure reproduces features of attention deficit hyperactivity disorder. FASEB J. 2015;29:1960–1972. doi: 10.1096/fj.14-260901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yu C.J., Du J.C., Chiou H.C., Chung M.Y., Yang W., Chen Y.S., Fuh M.R., Chien L.C., Hwang B., Chen M.L. Increased risk of attention-deficit/hyperactivity disorder associated with exposure to organophosphate pesticide in Taiwanese children. Andrology. 2016;4:695–705. doi: 10.1111/andr.12183. [DOI] [PubMed] [Google Scholar]
- 73.Kofman O., Berger A., Massarwa A., Friedman A., Jaffar A.A. Motor inhibition and learning impairments in school-aged children following exposure to organophosphate pesticides in infancy. Pediatr. Res. 2006;60:88–92. doi: 10.1203/01.pdr.0000219467.47013.35. [DOI] [PubMed] [Google Scholar]
- 74.Rauh V.A., Perera F.P., Horton M.K., Whyatt R.M., Bansal R., Hao X., Liu J., Barr D.B., Slotkin T.A., Peterson B.S. Brain anomalies in children exposed prenatally to a common organophosphate pesticide. Proc. Natl. Acad. Sci. USA. 2012;109:7871–7876. doi: 10.1073/pnas.1203396109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ascherio A., Chen H., Weisskopf M.G., O’Reilly E., McCullough M.L., Calle E.E., Schwarzschild M.A., Thun M.J. Pesticide exposure and risk for parkinson’s disease. Ann. Neurol. 2006;60:197–203. doi: 10.1002/ana.20904. [DOI] [PubMed] [Google Scholar]
- 76.Bhatt M.H., Elias M.A., Mankodi A.K. Acute and reversible parkinsonism due to organophosphate pesticide intoxication: Five cases. Neurology. 1999;52:1467–1471. doi: 10.1212/WNL.52.7.1467. [DOI] [PubMed] [Google Scholar]
- 77.Hancock D.B., Martin E.R., Mayhew G.M., Stajich J.M., Jewett R., Stacy M.A., Scott B.L., Vance J.M., Scott W.K. Pesticide exposure and risk of parkinson’s disease: A family-based case-control study. BMC Neurol. 2008;8:6. doi: 10.1186/1471-2377-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Richardson J.R., Roy A., Shalat S.L., von Stein R.T., Hossain M.M., Buckley B., Gearing M., Levey A.I., German D.C. Elevated serum pesticide levels and risk for alzheimer disease. JAMA Neurol. 2014;71:284–290. doi: 10.1001/jamaneurol.2013.6030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Andersen H.R., Nielsen J.B., Grandjean P. Toxicologic evidence of developmental neurotoxicity of environmental chemicals. Toxicology. 2000;144:121–127. doi: 10.1016/S0300-483X(99)00198-5. [DOI] [PubMed] [Google Scholar]
- 80.Cole T.B., Jampsa R.L., Walter B.J., Arndt T.L., Richter R.J., Shih D.M., Tward A., Lusis A.J., Jack R.M., Costa L.G., et al. Expression of human paraoxonase (Pon1) during development. Pharmacogenetics. 2003;13:357–364. doi: 10.1097/00008571-200306000-00007. [DOI] [PubMed] [Google Scholar]
- 81.Torres-Sanchez L., Schnaas L., Rothenberg S.J., Cebrian M.E., Osorio-Valencia E., Hernandez Mdel C., Garcia-Hernandez R.M., Lopez-Carrillo L. Prenatal P,P’-Dde exposure and neurodevelopment among children 3.5–5 years of age. Environ. Health Perspect. 2013;121:263–268. doi: 10.1289/ehp.1205034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ribas-Fito N., Torrent M., Carrizo D., Munoz-Ortiz L., Julvez J., Grimalt J.O., Sunyer J. In Utero exposure to background concentrations of ddt and cognitive functioning among preschoolers. Am. J. Epidemiol. 2006;164:955–962. doi: 10.1093/aje/kwj299. [DOI] [PubMed] [Google Scholar]
- 83.Torres-Sanchez L., Rothenberg S.J., Schnaas L., Cebrian M.E., Osorio E., Del Carmen Hernandez M., Garcia-Hernandez R.M., Del Rio-Garcia C., Wolff M.S., Lopez-Carrillo L. In Utero P,P’-Dde Exposure and infant neurodevelopment: A perinatal cohort in mexico. Environ. Health Perspect. 2007;115:435–439. doi: 10.1289/ehp.9566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rogan W.J., Gladen B.C. Pcbs, Dde, and child development at 18 and 24 months. Ann. Epidemiol. 1991;1:407–413. doi: 10.1016/1047-2797(91)90010-A. [DOI] [PubMed] [Google Scholar]
- 85.Eskenazi B., Marks A.R., Bradman A., Fenster L., Johnson C., Barr D.B., Jewell N.P. In Utero exposure to dichlorodiphenyltrichloroethane (Ddt) and dichlorodiphenyldichloroethylene (Dde) and neurodevelopment among young Mexican American children. Pediatrics. 2006;118:233–241. doi: 10.1542/peds.2005-3117. [DOI] [PubMed] [Google Scholar]
- 86.Rogan W.J., Gladen B.C., McKinney J.D., Carreras N., Hardy P., Thullen J., Tinglestad J., Tully M. Neonatal effects of transplacental exposure to Pcbs and Dde. J. Pediatr. 1986;109:335–341. doi: 10.1016/S0022-3476(86)80397-3. [DOI] [PubMed] [Google Scholar]
- 87.Cartier C., Muckle G., Jacobson S.W., Jacobson J.L., Dewailly E., Ayotte P., Chevrier C., Saint-Amour D. Prenatal and 5-year P,P’-Dde exposures are associated with altered sensory processing in school-aged children in nunavik: A visual evoked potential study. Neurotoxicology. 2014;44:8–16. doi: 10.1016/j.neuro.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 88.Van Wendel de Joode B., Wesseling C., Kromhout H., Monge P., Garcia M., Mergler D. Chronic nervous-system effects of long-term occupational exposure to Ddt. Lancet. 2001;357:1014–1016. doi: 10.1016/S0140-6736(00)04249-5. [DOI] [PubMed] [Google Scholar]
- 89.Ross G.W., Duda J.E., Abbott R.D., Pellizzari E., Petrovitch H., Miller D.B., O’Callaghan J.P., Tanner C.M., Noorigian J.V., Masaki K., et al. Brain organochlorines and lewy pathology: The honolulu-asia aging study. Mov. Disord. 2012;27:1418–1424. doi: 10.1002/mds.25144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Caudle W.M., Richardson J.R., Wang M., Miller G.W. Perinatal heptachlor exposure increases expression of presynaptic dopaminergic markers in mouse striatum. Neurotoxicology. 2005;26:721–728. doi: 10.1016/j.neuro.2004.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Richardson J.R., Caudle W.M., Wang M., Dean E.D., Pennell K.D., Miller G.W. Developmental exposure to the pesticide dieldrin alters the dopamine system and increases neurotoxicity in an animal model of parkinson’s disease. FASEB J. 2006;20:1695–1697. doi: 10.1096/fj.06-5864fje. [DOI] [PubMed] [Google Scholar]
- 92.Bloomquist J.R., Barlow R.L., Gillette J.S., Li W., Kirby M.L. Selective effects of insecticides on nigrostriatal dopaminergic nerve pathways. Neurotoxicology. 2002;23:537–544. doi: 10.1016/S0161-813X(02)00031-1. [DOI] [PubMed] [Google Scholar]
- 93.Hong S., Hwang J., Kim J.Y., Shin K.S., Kang S.J. Heptachlor induced nigral dopaminergic neuronal loss and parkinsonism-like movement deficits in mice. Exp. Mol. Med. 2014;46:e80. doi: 10.1038/emm.2014.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Briz V., Molina-Molina J.M., Sanchez-Redondo S., Fernandez M.F., Grimalt J.O., Olea N., Rodriguez-Farre E., Sunol C. Differential estrogenic effects of the persistent organochlorine pesticides dieldrin, endosulfan, and lindane in primary neuronal cultures. Toxicol. Sci. 2011;120:413–427. doi: 10.1093/toxsci/kfr019. [DOI] [PubMed] [Google Scholar]
- 95.Hatcher J.M., Richardson J.R., Guillot T.S., McCormack A.L., Di Monte D.A., Jones D.P., Pennell K.D., Miller G.W. Dieldrin exposure induces oxidative damage in the mouse nigrostriatal dopamine system. Exp. Neurol. 2007;204:619–630. doi: 10.1016/j.expneurol.2006.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kirby M.L., Barlow R.L., Bloomquist J.R. Neurotoxicity of the organochlorine insecticide heptachlor to murine striatal dopaminergic pathways. Toxicol. Sci. 2001;61:100–106. doi: 10.1093/toxsci/61.1.100. [DOI] [PubMed] [Google Scholar]
- 97.Cabaleiro T., Caride A., Romero A., Lafuente A. Effects of in Utero and lactational exposure to endosulfan in prefrontal cortex of male rats. Toxicol. Lett. 2008;176:58–67. doi: 10.1016/j.toxlet.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 98.Lafuente A., Pereiro N. Neurotoxic effects induced by endosulfan exposure during pregnancy and lactation in female and male rat striatum. Toxicology. 2013;311:35–40. doi: 10.1016/j.tox.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 99.Lee I., Eriksson P., Fredriksson A., Buratovic S., Viberg H. Developmental neurotoxic effects of two pesticides: Behavior and neuroprotein studies on endosulfan and cypermethrin. Toxicology. 2015;335:1–10. doi: 10.1016/j.tox.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 100.Richardson J.R., Caudle W.M., Wang M.Z., Dean E.D., Pennell K.D., Miller G.W. Developmental heptachlor exposure increases susceptibility of dopamine neurons to n-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (Mptp)in a gender-specific manner. Neurotoxicology. 2008;29:855–863. doi: 10.1016/j.neuro.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Purkerson-Parker S., McDaniel K.L., Moser V.C. Dopamine transporter binding in the rat striatum is increased by gestational, perinatal, and adolescent exposure to heptachlor. Toxicol. Sci. 2001;64:216–223. doi: 10.1093/toxsci/64.2.216. [DOI] [PubMed] [Google Scholar]
- 102.Wilson W.W., Onyenwe W., Bradner J.M., Nennig S.E., Caudle W.M. Developmental exposure to the organochlorine insecticide endosulfan alters expression of proteins associated with neurotransmission in the frontal cortex. Synapse. 2014;68:485–497. doi: 10.1002/syn.21764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Briz V., Galofre M., Sunol C. Reduction of glutamatergic neurotransmission by prolonged exposure to dieldrin involves nmda receptor internalization and metabotropic glutamate receptor 5 downregulation. Toxicol. Sci. 2010;113:138–149. doi: 10.1093/toxsci/kfp244. [DOI] [PubMed] [Google Scholar]
- 104.Babot Z., Vilaro M.T., Sunol C. Long-term exposure to dieldrin reduces gamma-aminobutyric acid type a and N-Methyl-D-Aspartate receptor function in primary cultures of mouse cerebellar granule cells. J. Neurosci. Res. 2007;85:3687–3695. doi: 10.1002/jnr.21433. [DOI] [PubMed] [Google Scholar]
- 105.Steenland K., Dick R.B., Howell R.J., Chrislip D.W., Hines C.J., Reid T.M., Lehman E., Laber P., Krieg E.F., Jr., Knott C. Neurologic function among termiticide applicators exposed to chlorpyrifos. Environ. Health Perspect. 2000;108:293–300. doi: 10.1289/ehp.00108293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Aldridge J.E., Seidler F.J., Meyer A., Thillai I., Slotkin T.A. Serotonergic systems targeted by developmental exposure to chlorpyrifos: Effects during different critical periods. Environ. Health Perspect. 2003;111:1736–1743. doi: 10.1289/ehp.6489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Aldridge J.E., Seidler F.J., Slotkin T.A. Developmental Exposure to chlorpyrifos elicits sex-selective alterations of serotonergic synaptic function in adulthood: Critical periods and regional selectivity for effects on the serotonin transporter, receptor subtypes, and cell signaling. Environ. Health Perspect. 2004;112:148–155. doi: 10.1289/ehp.6713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Raines K.W., Seidler F.J., Slotkin T.A. Alterations in serotonin transporter expression in brain regions of rats exposed neonatally to chlorpyrifos. Brain Res. Dev. Brain Res. 2001;130:65–72. doi: 10.1016/S0165-3806(01)00211-5. [DOI] [PubMed] [Google Scholar]
- 109.Qiao D., Seidler F.J., Padilla S., Slotkin T.A. Developmental neurotoxicity of chlorpyrifos: What is the vulnerable period? Environ. Health Perspect. 2002;110:1097–1103. doi: 10.1289/ehp.021101097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Richardson J.R., Chambers J.E. Neurochemical effects of repeated gestational exposure to chlorpyrifos in developing rats. Toxicol. Sci. 2004;77:83–90. doi: 10.1093/toxsci/kfh014. [DOI] [PubMed] [Google Scholar]
- 111.Qiao D., Seidler F.J., Tate C.A., Cousins M.M., Slotkin T.A. Fetal chlorpyrifos exposure: Adverse effects on brain cell development and cholinergic biomarkers emerge postnatally and continue into adolescence and adulthood. Environ. Health Perspect. 2003;111:536–544. doi: 10.1289/ehp.5828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Levin E.D., Addy N., Baruah A., Elias A., Christopher N.C., Seidler F.J., Slotkin T.A. Prenatal chlorpyrifos exposure in rats causes persistent behavioral alterations. Neurotoxicol. Teratol. 2002;24:733–741. doi: 10.1016/S0892-0362(02)00272-6. [DOI] [PubMed] [Google Scholar]
- 113.Sanchez-Santed F., Canadas F., Flores P., Lopez-Grancha M., Cardona D. Long-term functional neurotoxicity of paraoxon and chlorpyrifos: Behavioural and pharmacological evidence. Neurotoxicol. Teratol. 2004;26:305–317. doi: 10.1016/j.ntt.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 114.Lee I., Eriksson P., Fredriksson A., Buratovic S., Viberg H. Developmental neurotoxic effects of two pesticides: Behavior and biomolecular studies on chlorpyrifos and Carbaryl. Toxicol. Appl. Pharmacol. 2015;288:429–438. doi: 10.1016/j.taap.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 115.Guo-Ross S.X., Chambers J.E., Meek E.C., Carr R.L. Altered muscarinic acetylcholine receptor subtype binding in neonatal rat brain following exposure to chlorpyrifos or methyl parathion. Toxicol. Sci. 2007;100:118–127. doi: 10.1093/toxsci/kfm195. [DOI] [PubMed] [Google Scholar]
- 116.Liu J., Olivier K., Pope C.N. Comparative neurochemical effects of repeated methyl parathion or chlorpyrifos exposures in neonatal and adult rats. Toxicol Appl. Pharmacol. 1999;158:186–196. doi: 10.1006/taap.1999.8693. [DOI] [PubMed] [Google Scholar]
- 117.Richardson J.R., Chambers J.E. Effects of repeated oral postnatal exposure to chlorpyrifos on cholinergic neurochemistry in developing rats. Toxicol. Sci. 2005;84:352–359. doi: 10.1093/toxsci/kfi081. [DOI] [PubMed] [Google Scholar]
- 118.Tang J., Carr R.L., Chambers J.E. Changes in rat brain cholinesterase activity and muscarinic receptor density during and after repeated oral exposure to chlorpyrifos in early postnatal development. Toxicol. Sci. 1999;51:265–272. doi: 10.1093/toxsci/51.2.265. [DOI] [PubMed] [Google Scholar]
- 119.Zhang H., Liu J., Pope C.N. Age-related effects of chlorpyrifos on muscarinic receptor-mediated signaling in rat cortex. Arch. Toxicol. 2002;75:676–684. doi: 10.1007/s00204-001-0309-3. [DOI] [PubMed] [Google Scholar]
- 120.Mubarak Hossain M., Suzuki T., Sato N., Sato I., Takewaki T., Suzuki K., Tachikawa E., Kobayashi H. Differential effects of pyrethroid insecticides on extracellular dopamine in the striatum of freely moving rats. Toxicol. Appl. Pharmacol. 2006;217:25–34. doi: 10.1016/j.taap.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 121.Lucki I. The spectrum of behaviors influenced by serotonin. Biol Psychiatry. 1998;44:151–162. doi: 10.1016/S0006-3223(98)00139-5. [DOI] [PubMed] [Google Scholar]
- 122.Hossain M.M., Suzuki T., Unno T., Komori S., Kobayashi H. Differential presynaptic actions of pyrethroid insecticides on glutamatergic and gabaergic neurons in the hippocampus. Toxicology. 2008;243:155–163. doi: 10.1016/j.tox.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 123.Jorgenson J.L. Aldrin and Dieldrin: A review of research on their production, environmental deposition and fate, bioaccumulation, toxicology, and epidemiology in the United States. Environ. Health Perspect. 2001;109:113–139. doi: 10.1289/ehp.01109s1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Smith D. Worldwide trends in ddt levels in human breast milk. Int J. Epidemiol. 1999;28:179–188. doi: 10.1093/ije/28.2.179. [DOI] [PubMed] [Google Scholar]
- 125.LaKind J.S., Amina Wilkins A., Berlin C.M., Jr. Environmental Chemicals in Human Milk: A review of levels, infant exposures and health, and guidance for future research. Toxicol. Appl. Pharmacol. 2004;198:184–208. doi: 10.1016/j.taap.2003.08.021. [DOI] [PubMed] [Google Scholar]
- 126.Shen H., Main K.M., Andersson A.M., Damgaard I.N., Virtanen H.E., Skakkebaek N.E., Toppari J., Schramm K.W. Concentrations of persistent organochlorine compounds in human milk and placenta are higher in Denmark Than in Finland. Hum. Reprod. 2008;23:201–210. doi: 10.1093/humrep/dem199. [DOI] [PubMed] [Google Scholar]
- 127.Shen H., Main K.M., Virtanen H.E., Damggard I.N., Haavisto A.M., Kaleva M., Boisen K.A., Schmidt I.M., Chellakooty M., Skakkebaek N.E., et al. From mother to child: Investigation of prenatal and postnatal exposure to persistent bioaccumulating toxicants using breast milk and placenta biomonitoring. Chemosphere. 2007;67:S256–S262. doi: 10.1016/j.chemosphere.2006.05.106. [DOI] [PubMed] [Google Scholar]
- 128.Holan G. New halocyclopropane insecticides and the mode of action of ddt. Nature. 1969;221:1025–1029. doi: 10.1038/2211025a0. [DOI] [PubMed] [Google Scholar]
- 129.Vijverberg H.P., van der Zalm J.M., van der Bercken J. Similar mode of action of pyrethroids and ddt on sodium channel gating in Myelinated Nerves. Nature. 1982;295:601–603. doi: 10.1038/295601a0. [DOI] [PubMed] [Google Scholar]
- 130.Klaassen C.D. Casarett and Doull’s Toxicology: The Basic Science of Poisons. 8th ed. McGraw-Hill; New York, NY, USA: 2013. [Google Scholar]
- 131.Narahashi T., Carter D.B., Frey J., Ginsburg K., Hamilton B.J., Nagata K., Roy M.L., Song J.H., Tatebayashi H. Sodium channels and gabaa receptor-channel complex as targets of environmental toxicants. Toxicol. Lett. 1995;82–83:239–245. doi: 10.1016/0378-4274(95)03482-X. [DOI] [PubMed] [Google Scholar]
- 132.Abalis I.M., Eldefrawi M.E., Eldefrawi A.T. Effects of insecticides on gaba-induced chloride influx into rat brain microsacs. J. Toxicol. Environ. Health. 1986;18:13–23. doi: 10.1080/15287398609530844. [DOI] [PubMed] [Google Scholar]
- 133.Bloomquist J.R., Soderlund D.M. Neurotoxic insecticides inhibit gaba-dependent chloride uptake by mouse brain vesicles. Biochem. Biophys. Res. Commun. 1985;133:37–43. doi: 10.1016/0006-291X(85)91838-8. [DOI] [PubMed] [Google Scholar]
- 134.Cole L.M., Casida J.E. Polychlorocycloalkane insecticide-induced convulsions in mice in relation to disruption of the gaba-regulated chloride ionophore. Life Sci. 1986;39:1855–1862. doi: 10.1016/0024-3205(86)90295-X. [DOI] [PubMed] [Google Scholar]
- 135.Matsumura F., Ghiasuddin S.M. Evidence for similarities between cyclodiene type insecticides and picrotoxinin in their action mechanisms. J. Environ. Sci. Health B. 1983;18:1–14. doi: 10.1080/03601238309372355. [DOI] [PubMed] [Google Scholar]
- 136.Gant D.B., Eldefrawi M.E., Eldefrawi A.T. Cyclodiene insecticides inhibit gabaa receptor-regulated chloride transport. Toxicol. Appl. Pharmacol. 1987;88:313–321. doi: 10.1016/0041-008X(87)90206-7. [DOI] [PubMed] [Google Scholar]
- 137.Fenster L., Eskenazi B., Anderson M., Bradman A., Hubbard A., Barr D.B. In Utero exposure to ddt and performance on the brazelton neonatal behavioral assessment scale. Neurotoxicology. 2007;28:471–477. doi: 10.1016/j.neuro.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 138.Ribas-Fito N., Cardo E., Sala M., Eulalia de Muga M., Mazon C., Verdu A., Kogevinas M., Grimalt J.O., Sunyer J. Breastfeeding, exposure to organochlorine compounds, and neurodevelopment in infants. Pediatrics. 2003;111:e580–e585. doi: 10.1542/peds.111.5.e580. [DOI] [PubMed] [Google Scholar]
- 139.Gladen B.C., Rogan W.J., Hardy P., Thullen J., Tingelstad J., Tully M. Development after exposure to polychlorinated biphenyls and dichlorodiphenyl dichloroethene transplacentally and through human milk. J. Pediatr. 1988;113:991–995. doi: 10.1016/S0022-3476(88)80569-9. [DOI] [PubMed] [Google Scholar]
- 140.Boucher O., Simard M.N., Muckle G., Rouget F., Kadhel P., Bataille H., Chajes V., Dallaire R., Monfort C., Thome J.P., et al. Exposure to an organochlorine pesticide (chlordecone) and development of 18-month-old infants. Neurotoxicology. 2013;35:162–168. doi: 10.1016/j.neuro.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 141.Engel S.M., Wetmur J., Chen J., Zhu C., Barr D.B., Canfield R.L., Wolff M.S. Prenatal exposure to organophosphates, paraoxonase 1, and cognitive development in childhood. Environ. Health Perspect. 2011;119:1182–1188. doi: 10.1289/ehp.1003183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kamel F., Hoppin J.A. Association of pesticide exposure with neurologic dysfunction and disease. Environ. Health Perspect. 2004;112:950–958. doi: 10.1289/ehp.7135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Elbaz A., Clavel J., Rathouz P.J., Moisan F., Galanaud J.P., Delemotte B., Alperovitch A., Tzourio C. Professional exposure to pesticides and parkinson disease. Ann. Neurol. 2009;66:494–504. doi: 10.1002/ana.21717. [DOI] [PubMed] [Google Scholar]
- 144.Kamel F. Epidemiology. paths from pesticides to parkinson’s. Science. 2013;341:722–723. doi: 10.1126/science.1243619. [DOI] [PubMed] [Google Scholar]
- 145.Weisskopf M.G., Knekt P., O’Reilly E.J., Lyytinen J., Reunanen A., Laden F., Altshul L., Ascherio A. Persistent organochlorine pesticides in serum and risk of parkinson disease. Neurology. 2010;74:1055–1061. doi: 10.1212/WNL.0b013e3181d76a93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Rhodes S.L., Fitzmaurice A.G., Cockburn M., Bronstein J.M., Sinsheimer J.S., Ritz B. Pesticides that inhibit the ubiquitin-proteasome system: Effect measure modification by genetic variation in Skp1 in parkinsons disease. Environ. Res. 2013;126:1–8. doi: 10.1016/j.envres.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Richardson J.R., Roy A., Shalat S.L., Buckley B., Winnik B., Gearing M., Levey A.I., Factor S.A., O’Suilleabhain P., German D.C. Beta-hexachlorocyclohexane levels in serum and risk of parkinson’s disease. Neurotoxicology. 2011;32:640–645. doi: 10.1016/j.neuro.2011.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Le Couteur D.G., McLean A.J., Taylor M.C., Woodham B.L., Board P.G. Pesticides and parkinson’s disease. Biomed. Pharmacother. 1999;53:122–130. doi: 10.1016/S0753-3322(99)80077-8. [DOI] [PubMed] [Google Scholar]
- 149.Priyadarshi A., Khuder S.A., Schaub E.A., Shrivastava S. A meta-analysis of parkinson’s disease and exposure to pesticides. Neurotoxicology. 2000;21:435–440. [PubMed] [Google Scholar]
- 150.Semchuk K.M., Love E.J., Lee R.G. Parkinson’s disease and exposure to agricultural work and pesticide chemicals. Neurology. 1992;42:1328–1335. doi: 10.1212/WNL.42.7.1328. [DOI] [PubMed] [Google Scholar]
- 151.Tanner C.M., Goldman S.M. Epidemiology of parkinson’s disease. Neurol. Clin. 1996;14:317–335. doi: 10.1016/S0733-8619(05)70259-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Corrigan F.M., Murray L., Wyatt C.L., Shore R.F. Diorthosubstituted polychlorinated biphenyls in caudate nucleus in parkinson’s disease. Exp. Neurol. 1998;150:339–342. doi: 10.1006/exnr.1998.6776. [DOI] [PubMed] [Google Scholar]
- 153.Corrigan F.M., Wienburg C.L., Shore R.F., Daniel S.E., Mann D. Organochlorine insecticides in substantia nigra in parkinson’s disease. J. Toxicol. Environ. Health A. 2000;59:229–234. doi: 10.1080/009841000156907. [DOI] [PubMed] [Google Scholar]
- 154.Richardson J.R., Shalat S.L., Buckley B., Winnik B., O’Suilleabhain P., Diaz-Arrastia R., Reisch J., German D.C. Elevated serum pesticide levels and risk of parkinson disease. Arch. Neurol. 2009;66:870–875. doi: 10.1001/archneurol.2009.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Fleming L., Mann J.B., Bean J., Briggle T., Sanchez-Ramos J.R. Parkinson’s disease and brain levels of organochlorine pesticides. Ann. Neurol. 1994;36:100–103. doi: 10.1002/ana.410360119. [DOI] [PubMed] [Google Scholar]
- 156.Wilson W.W., Shapiro L.P., Bradner J.M., Caudle W.M. Developmental exposure to the organochlorine insecticide endosulfan damages the nigrostriatal dopamine system in male offspring. Neurotoxicology. 2014;44:279–287. doi: 10.1016/j.neuro.2014.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Hudson P.M., Chen P.H., Tilson H.A., Hong J.S. Effects of P,P’-Ddt on the rat brain concentrations of biogenic amine and amino acid neurotransmitters and their association with P,P’-Ddt-induced tremor and hyperthermia. J. Neurochem. 1985;45:1349–1355. doi: 10.1111/j.1471-4159.1985.tb07199.x. [DOI] [PubMed] [Google Scholar]
- 158.Bouchard M.F., Chevrier J., Harley K.G., Kogut K., Vedar M., Calderon N., Trujillo C., Johnson C., Bradman A., Barr D.B., et al. Prenatal exposure to organophosphate pesticides and IQ in 7-year-old children. Environ. Health Perspect. 2011;119:1189–1195. doi: 10.1289/ehp.1003185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Abdel Rasoul G.M., Abou Salem M.E., Mechael A.A., Hendy O.M., Rohlman D.S., Ismail A.A. Effects of occupational pesticide exposure on children applying pesticides. Neurotoxicology. 2008;29:833–838. doi: 10.1016/j.neuro.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 160.Eckerman D.A., Gimenes L.S., de Souza R.C., Galvao P.R., Sarcinelli P.N., Chrisman J.R. Age related effects of pesticide exposure on neurobehavioral performance of adolescent farm workers in Brazil. Neurotoxicol. Teratol. 2007;29:164–175. doi: 10.1016/j.ntt.2006.09.028. [DOI] [PubMed] [Google Scholar]
- 161.Eskenazi B., Marks A.R., Bradman A., Harley K., Barr D.B., Johnson C., Morga N., Jewell N.P. Organophosphate pesticide exposure and neurodevelopment in young Mexican-American children. Environ. Health Perspect. 2007;115:792–798. doi: 10.1289/ehp.9828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Grandjean P., Harari R., Barr D.B., Debes F. Pesticide exposure and stunting as independent predictors of neurobehavioral deficits in ecuadorian school children. Pediatrics. 2006;117:546–556. doi: 10.1542/peds.2005-1781. [DOI] [PubMed] [Google Scholar]
- 163.Guodong D., Pei W., Ying T., Jun Z., Yu G., Xiaojin W., Rong S., Guoquan W., Xiaoming S. Organophosphate pesticide exposure and neurodevelopment in young Shanghai children. Environ. Sci. Technol. 2012;46:2911–2917. doi: 10.1021/es202583d. [DOI] [PubMed] [Google Scholar]
- 164.Handal A.J., Harlow S.D., Breilh J., Lozoff B. Occupational exposure to pesticides during pregnancy and neurobehavioral development of infants and toddlers. Epidemiology. 2008;19:851–859. doi: 10.1097/EDE.0b013e318187cc5d. [DOI] [PubMed] [Google Scholar]
- 165.Handal A.J., Lozoff B., Breilh J., Harlow S.D. Effect of community of residence on neurobehavioral development in infants and young children in a flower-growing region of Ecuador. Environ. Health Perspect. 2007;115:128–133. doi: 10.1289/ehp.9261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Harari R., Julvez J., Murata K., Barr D., Bellinger D.C., Debes F., Grandjean P. Neurobehavioral deficits and increased blood pressure in school-age children prenatally exposed to pesticides. Environ. Health Perspect. 2010;118:890–896. doi: 10.1289/ehp.0901582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Lizardi P.S., O’Rourke M.K., Morris R.J. The effects of organophosphate pesticide exposure on hispanic children’s cognitive and behavioral functioning. J. Pediatr. Psychol. 2008;33:91–101. doi: 10.1093/jpepsy/jsm047. [DOI] [PubMed] [Google Scholar]
- 168.Rohlman D.S., Arcury T.A., Quandt S.A., Lasarev M., Rothlein J., Travers R., Tamulinas A., Scherer J., Early J., Marin A., et al. Neurobehavioral performance in preschool children from agricultural and non-agricultural communities in Oregon and North Carolina. Neurotoxicology. 2005;26:589–598. doi: 10.1016/j.neuro.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 169.Rohlman D.S., Lasarev M., Anger W.K., Scherer J., Stupfel J., McCauley L. Neurobehavioral performance of adult and adolescent agricultural workers. Neurotoxicology. 2007;28:374–380. doi: 10.1016/j.neuro.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 170.Ruckart P.Z., Kakolewski K., Bove F.J., Kaye W.E. Long-term neurobehavioral health effects of Methyl Parathion exposure in children in Mississippi and Ohio. Environ. Health Perspect. 2004;112:46–51. doi: 10.1289/ehp.6430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Bouchard M.F., Bellinger D.C., Wright R.O., Weisskopf M.G. Attention-deficit/hyperactivity disorder and urinary metabolites of organophosphate pesticides. Pediatrics. 2010;125:1270–1277. doi: 10.1542/peds.2009-3058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Marks A.R., Harley K., Bradman A., Kogut K., Barr D.B., Johnson C., Calderon N., Eskenazi B. Organophosphate pesticide exposure and attention in young mexican-american children: The chamacos study. Environ. Health Perspect. 2010;118:1768–1774. doi: 10.1289/ehp.1002056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Engel S.M., Berkowitz G.S., Barr D.B., Teitelbaum S.L., Siskind J., Meisel S.J., Wetmur J.G., Wolff M.S. Prenatal organophosphate metabolite and organochlorine levels and performance on the brazelton neonatal behavioral assessment scale in a Multiethnic Pregnancy Cohort. Am. J. Epidemiol. 2007;165:1397–1404. doi: 10.1093/aje/kwm029. [DOI] [PubMed] [Google Scholar]
- 174.Dahlgren J.G., Takhar H.S., Ruffalo C.A., Zwass M. Health effects of diazinon on a family. J. Toxicol. Clin. Toxicol. 2004;42:579–591. doi: 10.1081/CLT-200026979. [DOI] [PubMed] [Google Scholar]
- 175.Young J.G., Eskenazi B., Gladstone E.A., Bradman A., Pedersen L., Johnson C., Barr D.B., Furlong C.E., Holland N.T. Association between in Utero organophosphate pesticide exposure and abnormal reflexes in Neonates. Neurotoxicology. 2005;26:199–209. doi: 10.1016/j.neuro.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 176.Sheets L.P. A consideration of age-dependent differences in susceptibility to organophosphorus and pyrethroid insecticides. Neurotoxicology. 2000;21:57–63. [PubMed] [Google Scholar]
- 177.Holland N., Furlong C., Bastaki M., Richter R., Bradman A., Huen K., Beckman K., Eskenazi B. Paraoxonase polymorphisms, haplotypes, and enzyme activity in latino mothers and newborns. Environ. Health Perspect. 2006;114:985–991. doi: 10.1289/ehp.8540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Furlong M.A., Engel S.M., Barr D.B., Wolff M.S. Prenatal exposure to organophosphate pesticides and reciprocal social behavior in childhood. Environ. Int. 2014;70:125–131. doi: 10.1016/j.envint.2014.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Brown M.A., Brix K.A. Review of health consequences from high-, intermediate- and low-level exposure to organophosphorus nerve agents. J. Appl. Toxicol. 1998;18:393–408. doi: 10.1002/(SICI)1099-1263(199811/12)18:6<393::AID-JAT528>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 180.Jamal G.A., Hansen S., Pilkington A., Buchanan D., Gillham R.A., Abdel-Azis M., Julu P.O., Al-Rawas S.F., Hurley F., Ballantyne J.P. A clinical neurological, neurophysiological, and neuropsychological study of sheep farmers and dippers exposed to organophosphate pesticides. Occup Environ. Med. 2002;59:434–441. doi: 10.1136/oem.59.7.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Rosenstock L., Keifer M., Daniell W.E., McConnell R., Claypoole K. Chronic central nervous system effects of acute organophosphate pesticide intoxication. the pesticide health effects study group. Lancet. 1991;338:223–227. doi: 10.1016/0140-6736(91)90356-T. [DOI] [PubMed] [Google Scholar]
- 182.Steenland K. Chronic neurological effects of organophosphate pesticides. BMJ. 1996;312:1312–1313. doi: 10.1136/bmj.312.7042.1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Speed H.E., Blaiss C.A., Kim A., Haws M.E., Melvin N.R., Jennings M., Eisch A.J., Powell C.M. Delayed reduction of hippocampal synaptic transmission and spines following exposure to repeated subclinical doses of organophosphorus pesticide in adult mice. Toxicol. Sci. 2012;125:196–208. doi: 10.1093/toxsci/kfr253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Chakraborti T.K., Farrar J.D., Pope C.N. Comparative neurochemical and neurobehavioral effects of repeated chlorpyrifos exposures in young and adult rats. Pharmacol. Biochem. Behav. 1993;46:219–224. doi: 10.1016/0091-3057(93)90344-S. [DOI] [PubMed] [Google Scholar]
- 185.Chanda S.M., Harp P., Liu J., Pope C.N. Comparative developmental and maternal neurotoxicity following acute gestational exposure to chlorpyrifos in rats. J. Toxicol. Environ. Health. 1995;44:189–202. doi: 10.1080/15287399509531954. [DOI] [PubMed] [Google Scholar]
- 186.Hatcher J.M., Pennell K.D., Miller G.W. Parkinson’s disease and pesticides: A toxicological perspective. Trends Pharmacol. Sci. 2008;29:322–329. doi: 10.1016/j.tips.2008.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Panuwet P., Prapamontol T., Chantara S., Barr D.B. Urinary pesticide metabolites in school students from Northern Thailand. Int. J. Hyg. Environ. Health. 2009;212:288–297. doi: 10.1016/j.ijheh.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 188.Rohitrattana J., Siriwong W., Robson M., Panuwet P., Barr D.B., Fiedler N. Pyrethroid insecticide exposure in school-aged children living in rice and aquacultural farming regions of Thailand. Risk Manag. Healthc. Policy. 2014;7:211–217. doi: 10.2147/RMHP.S67208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Singleton S.T., Lein P.J., Farahat F.M., Farahat T., Bonner M.R., Knaak J.B., Olson J.R. Characterization of alpha-cypermethrin exposure in Egyptian agricultural workers. Int. J. Hyg. Environ. Health. 2014;217:538–545. doi: 10.1016/j.ijheh.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Ostrea E.M., Jr., Villanueva-Uy E., Bielawski D., Birn S., Janisse J.J. Trends in Long term exposure to propoxur and pyrethroids in young children in the Philippines. Environ. Res. 2014;131:13–16. doi: 10.1016/j.envres.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 191.Qi X., Zheng M., Wu C., Wang G., Feng C., Zhou Z. urinary pyrethroid metabolites among pregnant women in an agricultural area of the province of Jiangsu, China. Int. J. Hyg. Environ. Health. 2012;215:487–495. doi: 10.1016/j.ijheh.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 192.Babina K., Dollard M., Pilotto L., Edwards J.W. Environmental exposure to organophosphorus and pyrethroid pesticides in South Australian preschool children: A cross sectional study. Environ. Int. 2012;48:109–120. doi: 10.1016/j.envint.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 193.Burr S.A., Ray D.E. Structure-activity and interaction effects of 14 different pyrethroids on Voltage-Gated chloride ion channels. Toxicol. Sci. 2004;77:341–346. doi: 10.1093/toxsci/kfh027. [DOI] [PubMed] [Google Scholar]
- 194.Clark J.M., Symington S.B. Neurotoxic implications of the agonistic action of cs-syndrome pyrethroids on the N-type ca(v)2.2 calcium channel. Pest. Manag. Sci. 2008;64:628–638. doi: 10.1002/ps.1573. [DOI] [PubMed] [Google Scholar]
- 195.Anand S.S., Kim K.B., Padilla S., Muralidhara S., Kim H.J., Fisher J.W., Bruckner J.V. Ontogeny of hepatic and plasma metabolism of deltamethrin in vitro: Role in Age-Dependent Acute Neurotoxicity. Drug. Metab. Dispos. 2006;34:389–397. doi: 10.1124/dmd.105.007807. [DOI] [PubMed] [Google Scholar]
- 196.Horton M.K., Rundle A., Camann D.E., Boyd Barr D., Rauh V.A., Whyatt R.M. Impact of prenatal exposure to piperonyl butoxide and permethrin on 36-month neurodevelopment. Pediatrics. 2011;127:e699–e706. doi: 10.1542/peds.2010-0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Oulhote Y., Bouchard M.F. Urinary metabolites of organophosphate and pyrethroid pesticides and behavioral problems in Canadian children. Environ. Health Perspect. 2013;121:1378–1384. doi: 10.1289/ehp.1306667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Viel J.F., Warembourg C., Le Maner-Idrissi G., Lacroix A., Limon G., Rouget F., Monfort C., Durand G., Cordier S., Chevrier C. Pyrethroid insecticide exposure and cognitive developmental disabilities in children: The pelagie mother-child cohort. Environ. Int. 2015;82:69–75. doi: 10.1016/j.envint.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 199.Fiedler N., Rohitrattana J., Siriwong W., Suttiwan P., Ohman Strickland P., Ryan P.B., Rohlman D.S., Panuwet P., Barr D.B., Robson M.G. Neurobehavioral effects of exposure to organophosphates and pyrethroid pesticides among Thai children. Neurotoxicology. 2015;48:90–99. doi: 10.1016/j.neuro.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Gillette J.S., Bloomquist J.R. Differential up-regulation of striatal dopamine transporter and alpha-synuclein by the pyrethroid insecticide permethrin. Toxicol Appl. Pharmacol. 2003;192:287–293. doi: 10.1016/S0041-008X(03)00326-0. [DOI] [PubMed] [Google Scholar]
- 201.Collotta M., Bertazzi P.A., Bollati V. Epigenetics and pesticides. Toxicology. 2013;307:35–41. doi: 10.1016/j.tox.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 202.Song C., Kanthasamy A., Anantharam V., Sun F., Kanthasamy A.G. Environmental neurotoxic pesticide increases histone acetylation to promote apoptosis in dopaminergic neuronal cells: Relevance to epigenetic mechanisms of neurodegeneration. Mol. Pharmacol. 2010;77:621–632. doi: 10.1124/mol.109.062174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Bordoni L., Nasuti C., Mirto M., Caradonna F., Gabbianelli R. Intergenerational effect of early life exposure to permethrin: Changes in global dna methylation and in nurr1 gene expression. Toxics. 2015;3:451–461. doi: 10.3390/toxics3040451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Barker D.J. The developmental origins of adult disease. J. Am. Coll. Nutr. 2004;23:588s–595s. doi: 10.1080/07315724.2004.10719428. [DOI] [PubMed] [Google Scholar]
- 205.Tartaglione A.M., Venerosi A., Calamandrei G. Early-life toxic insults and onset of sporadic neurodegenerative diseases-an overview of experimental studies. Curr. Top. Behav. Neurosci. 2015;29:231–264. doi: 10.1007/7854_2015_416. [DOI] [PubMed] [Google Scholar]