Abstract
Purpose
This study compares the clinical features and physician selection of either Regional Anesthesia (peribulbar or retrobulbar block) with Monitored Anesthesia Care (RA-MAC) or General Anesthesia (GA) for open globe injury repair.
Design
A non-randomized, comparative, retrospective case series at a University Referral Center.
Participants
All adult repairable open globe injuries receiving primary repair between January 1st, 2004 and December 31st, 2014 (11 years). Exclusion criteria were patients less than 18 years of age and those treated with primary enucleation.
Methods
Data was gathered via retrospective chart review.
Main Outcome Measures
Data collected from each patient was age, gender, injury type, location, length of wound, presenting visual acuity, classification of anesthesia used, duration of the procedure performed, months of clinical follow-up, and final visual acuity.
Results
During the 11 years study period, 448 patients were identified who had open globe injuries with documented information on zone of injury. Globe injury repair was performed using RA-MAC in 351/448 (78%) patients and general anesthesia in 97/448 (22%) patients. Zone 1, 2 and 3 injuries were recorded in 241, 135, and 72 patients respectively. The rates in specific zones, of RA-MAC versus GA were as follows: Zone 1 – 213/241 (88%) vs 28/241 (12%), Zone 2 – 104/135 (77%) vs 31/135 (23%) and Zone 3 – 34/72 (47%) vs 38/72 (53%). Open globe injuries repaired under RA-MAC had significantly shorter wound length (p<0.001), more anterior wound location (p<0.001) and shorter operative times (p<0.001). RA-MAC cases also had a better presenting and final visual acuity (p<0.001). Neither class of anesthesia conferred a greater visual acuity improvement (p=0.06). The use of GA did not cause any delay in the time elapsed from injury until surgical repair (p=0.74).
Conclusions
RA-MAC is a reasonable alternative to GA for the repair of open globe injuries in selected adult patients. RA-MAC was selected more often for Zone 1 and Zone 2 injuries. For eyes with Zone 3 injuries, there are equal selection ratio for RA-MAC and GA.
Introduction
Open globe injuries are one of the more challenging emergent conditions that ophthalmologists encounter. General anesthesia (GA) has been conventionally preferred for primary closure due to the concern of extrusion of intraocular contents from the displacement of volume caused by regional anesthesia (peri- or retrobulbar block) with monitored anesthesia care (RA-MAC) in the fixed space of the orbit.1 However, the emergent nature of the treatment of these injuries may preclude general anesthesia.2 Conversely, there are a number of factors associated with the use of GA that can likewise cause increases in intraocular pressure. These include direct pressure on the globe during manual ventilation, rapid sequence induction on patients without empty stomach,3,4 laryngoscopy, and placement of an endotracheal tube,5 as well as coughing, bucking on the endotracheal tube, emesis, or Valsalva retinopathy. For these reasons, controversy exists regarding the preferred modality of anesthesia.6–8 A review of the current literature revealed few reports of using RA-MAC compared to the traditional GA for OGI.
The current study compares the clinical features and outcomes in a large series of patients with open globe injuries repaired under RA-MAC versus GA in eyes that did not undergo enucleation at time of primary closure for open globe injury.
Methods
The current study is a non-randomized, comparative, retrospective case series. A search identifying all cases of open globe injury was performed within a computerized database at the Bascom Palmer Eye Institute between January 1, 2004 and December 31, 2014 (11 years). Medical records, including clinical and operative notes were reviewed in retrospect. This study protocol was approved by the Institutional Review Board of the University of Miami Miller School of Medicine, Miami, Florida and was compliant with the Health Insurance Portability and Accountability Act. All patients gave informed consent for treatment and the study protocol adhered to declaration of Helsinki requirements.
Inclusion criteria were a diagnosis consistent with an open globe injury from the operative report and consisted of the following International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes: 360.5 - retained IOFB magnetic, 360.6 - retained IOFB nonmagnetic, 871 - open wound of eyeball, 918.1 - injury of cornea. Patients younger than 18 years old and those receiving primary enucleation were excluded from study. Such exclusions were made due the necessity of GA in the pediatric population, and the inherent lack of postoperative visual acuity in those treated with primary enucleation. Patients with open globe injuries (OGI) and closure prior to referral were not included in the current study.
Demographics of age and gender were obtained for each patient. Open globe injuries were characterized by the type (blunt rupture, sharp laceration, retained intraocular foreign body, perforation, or mixed mechanism), location (Zone 1 – cornea and limbus, Zone 2 – ≤ 5 millimeters posterior to the limbus, or Zone 3 – greater than 5 millimeters posterior to the limbus), and length of wound,9 as well as the initial presenting visual acuity. Operative data obtained included the classification of anesthesia used and the duration of the procedure performed, from the initial incision to the completion of closure. Postoperative data included months of clinical follow-up and final visual acuity. Final visual acuity data was not recorded for patients with less than 2 months of follow-up.
Regional anesthesia was accomplished with a peri- or retro-bulbar block of a one to one mixture of 0.75% bupivacaine and 2–4% lidocaine with up to 75 units of hyaluronidase. This was administered preoperatively in the holding area just before the patient was taken into the operating room. Volumes were variable starting with a minimal peribulbar injection and supplementing with additional volumes until satisfactory anesthesia was achieved. All uses of regional anesthesia were accompanied by monitored anesthesia care with intravenous conscious sedation, administered by the anesthesia staff. Per patient’s needs, selected cases received supplemental block which was administered during the surgical procedure with a blunt cannula after conjunctival peritomy.
Visual acuity was converted to LogMAR for data analysis. Visual acuities recorded as counting fingers (CF), hand motions (HM), light perception (LP), and no light perception (NLP) in were converted to LogMAR values of 2, 2.3, 3 and 3.2 for the purposes of statistical analysis. Statistical analysis was carried out to compare each of the observed variables between patients who received RA-MAC and those who received GA. Student’s t-test was used for continuous variables, and χ2 test was used for categorical variables.
Results
Using the ICD-9CM codes listed for the postoperative diagnosis of open globe injury, 1,341 records were identified. Among these records, 290 (21%) were younger than 18 years of age, 173 (13%) either underwent a procedure other than primary closure or were treated with primary enucleation and 74 records were miscoded. During the 11 years study period, 804 patients were identified who had open globe injuries repaired and fulfilled inclusion criteria of the study. Among these patients, the information on zone of injury was available for 448 patients.
Comparison of demographics and physician selection of either regional anesthesia (peribulbar or retrobulbar block) with monitored anesthesia care (RA-MAC) or general anesthesia (GA) for open globe injury repair (N=448) from 2004–2014 is shown in Table 1. The anesthesia rates were RA-MAC in 351/448 (78.3%) patients and general anesthesia in 97/448 (21.7%) patients (Table 1). Mean age among two groups was comparable (51.8 years in RA-MAC group versus 49.3 years in GA group). There was no significant difference in gender between the two groups, with the majority of patients being male (RA-MAC - 244/351[69%], GA – 69/97[71%]).
Table 1.
Demographics, wound characteristics, and visual outcomes of patients with open globe injury that did not undergo enucleation at time of primary closure for open globe injury from 2004–2014.
| Regional Anesthesia | General Anesthesia | |
|---|---|---|
|
| ||
| Number of patients | 351/448 (78 %) | 97/448 (22 %) |
|
| ||
| Average age in years (range) | 51.8 ± 22.2 (18–98) | 49.3 ± 20.3 (18–95) |
|
| ||
| Male:Female | 244:107 | 69:28 |
|
| ||
| Average wound length in millimeters | 7.0 ± 5.6 (n/N=151/351) | 11.9 ± 6.6 (n/N=42/97) |
|
| ||
| Zone of Injury (N=448) | (N=351) | (N=97) |
| • Zone (1) – 241/448 eyes | 213/351 (61%) | 28/97 (29%) |
| • Zone (2) – 135/448 eyes | 104/351 (30%) | 31/97 (32%) |
| • Zone (3) – 72/448 eyes | 34/351 (10%) | 38/97 (39%) |
|
| ||
| Mean Final visual acuity (N=290) (Included VA of patients with ≥ 2 months follow-up) | ||
| • ≥ 20/400 (n/N=173/290) | 155/173 (90%) | 18/173 (10%) |
| • < 20/400 (n/N=117/290) | 84/117 (72%) | 33/117 (28%) |
|
| ||
| Follow-up in months | 12.7 ± 18.9 (n/N=307/351) | 8.5 ± 14.2 (n/N=82/97) |
Zones of open globe injuries: Zone 1 – cornea and limbus, Zone 2 – ≤ 5 millimeters posterior to the limbus, Zone 3 – greater than 5 millimeters posterior to the limbus.
The rates of RA-MAC versus GA were reported for Zone 1 open globe injuries (213 vs 28), Zone 2 open globe injuries (104 vs 31) and Zone 3 open globe injuries (34 vs 38). Average wound length among RA-MAC group and GA group was 7.0mm versus 11.9mm. The mean duration of follow-up in the current study was 11 months, range 0 to 113 months (13 months among RA-MAC group and 9 months among GA group). Evaluation of anesthetic use by Zone showed a decrease of RA-MAC use and an increase in GA use with more posterior Zones of injury (Figure 1). Injury type 1 and 2 (rupture and laceration) accounted for >80% injuries in all three zone of injuries and were distributed equally among RA-MAC group and GA group.
Figure 1.
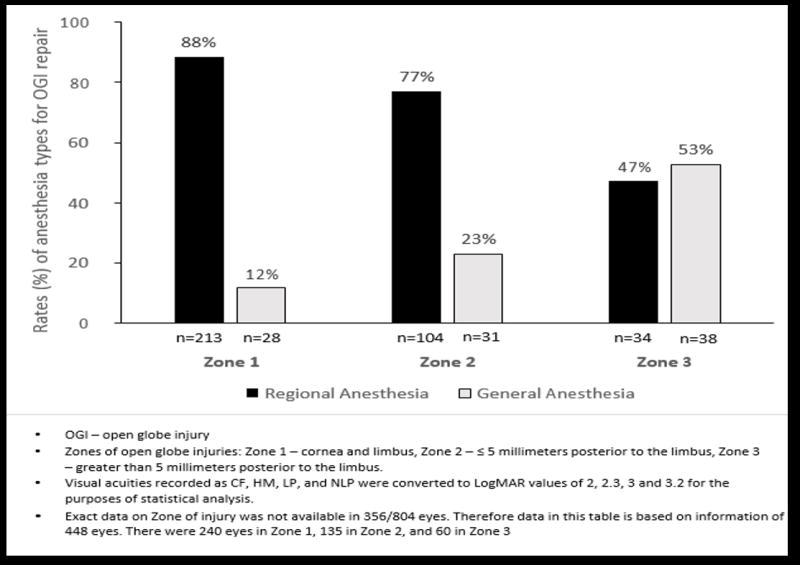
Frequency of regional (peribulbar or retrobulbar block) with monitored anesthesia care versus general anesthesia use by zone of injury from 2004 to 2014. Regional anesthesia was preferential anesthesia type in Zone 1 injury (88% vs 12%) and Zone 2 injury (77% vs 23%) but both anesthesia types (regional and general anesthesia) were used equally in Zone 3 injury (47% vs 53%).
In patients with Zone 1 open globe injury (Supplemental Table 1 available at http://www.ophthalmology-retina.org), shorter wound length and shorter procedure time were more commonly noted among RA-MAC group compared to GA-group (p=0.02 and p=0.007 respectively). Patients presenting with bad visual acuity were more likely to undergo surgery under general anesthesia (p<0.001).
In patients with Zone 2 open globe injury (Supplemental Table 2 available at http://www.ophthalmology-retina.org), shorter wound length and shorter procedure time were more commonly noted among RA-MAC group compared to GA-group (p=0.02 and p=0.004 respectively).
In patients with Zone 3 open globe injury (Supplemental Table 3 available at http://www.ophthalmology-retina.org), no significant difference was noted for wound length and procedure time among RA-MAC group compared to GA-group (p=0.21 and p=0.028 respectively). Patients presenting with Zone 2 or 3 open globe injury had poor final visual acuities.
Visual acuity at final follow-up was available for 290/448 patients (Table 2). Among these patients, 173/290 (60%) achieved 20/400 or better at final follow-up (155/173, 90% – operated under RA-MAC while 18/173, 10% – operated under GA). Among 173 patients with 20/400 or better visual acuity, 117 patients had zone 1 injury (110/117– operated under RA-MAC while – 7/117 operated under GA), 47 patients had zone 2 injury (39/47 – operated under RA-MAC while 8/47 – operated under GA), and 9 patients had zone 3 injury (6/9 – operated under RA-MAC while 3/9 – operated under GA).
Table 2.
Visual outcomes among two anesthesia types (RA-MAC and GA). Visual acuity of 20/400 or better among patients with follow-up of ≥2 months, was achieved in 173/290 patients (155/173, 90% – operated under RA-MAC while 18/173, 10% – operated under GA).
| Visual acuity ≥ 20/400 | Visual acuity < 20/400 | |||||
|---|---|---|---|---|---|---|
| N | Regional Anesthesia | General Anesthesia | N | Regional Anesthesia | General Anesthesia | |
| Zone 1 | 117 | 110 | 7 | 46 | 36 | 10 |
| Zone 2 | 47 | 39 | 8 | 38 | 31 | 7 |
| Zone 3 | 9 | 6 | 3 | 33 | 17 | 16 |
| Total | 173 | 155 (90%) | 18 (10%) | 117 | 84 (72%) | 33 (28%) |
Patients having minimum follow-up of 2 months were included for this analysis.
Comparison of current study with earlier literature showed that use of RA-MAC during the current study period was significantly higher than earlier study periods (p<0.001): 64% in 1995–1999, and 41% in 2000–2003, to 80% from 2004–2014 (Table 3).6,7
Table 3.
Comparison of regional (peribulbar or retrobulbar block) with monitored anesthesia care and general anesthesia use at Bascom Palmer Eye Institute in past 20 years (1994–2014).
| Total | Regional Anesthesia | General Anesthesia | |
|---|---|---|---|
| 1995 – 1999* | 220 | 140 (64%) | 80 (36%) |
| 2000 – 2003** | 238 | 97 (41%) | 141 (59%) |
| 2004 – 2014 | 804 | 643 (80%) | 161 (20%) |
American Journal of Ophthalmology 2002;134:707–711.
Ophthalmic Surgery Lasers and Imaging 2005;36:122–128.
Discussion
Both RA-MAC and GA have unique and inherent risks that may cause extrusion of intraocular contents with open globe injuries.1,3,5,10,11 The current study demonstrates that neither type of anesthesia, for any single zone of injury, confers a clear advantage for postoperative improvement of visual acuity. Reported visual outcomes are more likely related to the degree of injury than the type of anesthesia used.
The current study was limited by its retrospective nature and the fact that the decision to use RA-MAC versus GA reflects the selection bias of the individual physicians at our institution. Data regarding intraoperative complications was collected from the dictated operative notes. Because the study had no standardized forms for data collection, it is likely that intraoperative complications were not recorded. In general, those with less severe injuries were prone to receive RA-MAC, and those with more severe injuries were more commonly repaired under GA. The concern for expulsion of intraocular contents with larger injuries, or intraocular infiltration of regional anesthesia in more posterior injuries may influence the surgeon to use GA. However, even among the most posterior of injuries (Zone 3), no difference in the size of the injury, final VA vs postoperative VA improvement or worse was identified between the 2 groups. None of the reviewed operative records suggested the expulsion of intraocular contents related to either RA-MAC or GA.
Patients who received GA were generally younger. This finding may reflect a reluctance to perform GA for older patients who are inherently more likely to have a greater number of systemic comorbidities. However, in the current study, average time of injury until repair was found to be no different between the RA-MAC and GA groups. This study provides the surgeon with further data on to choose the type of anesthesia without concern of delaying the repair.
During the current study, RA-MAC was more commonly utilized compared to previously reported series from our institution.6,7 Based on data in the current study, ophthalmologists and anesthesiologists may consider this type of anesthesia as a reasonable alternative to general anesthesia for the repair of open globe injuries in selected patients.
Supplementary Material
Supplemental Table 1: Demographics, wound characteristics, and visual outcomes of zone 1 (n= 241) salvageable adult open globe injuries from 2004–2014.
Supplemental Table 2: Demographics, wound characteristics, and visual outcomes of zone 2 (n-135) salvageable adult open globe injuries from 2004–2014.
Supplemental Table 3: Demographics, wound characteristics, and visual outcomes of zone 3 (n=72) salvageable adult open globe injuries 2004–2014.
Acknowledgments
Statistical analysis of data - Wei Shi Li
Financial Support: National Institute of Health Center Core Grant P30EY014801 (Bethesda, Maryland), Research to Prevent Blindness Unrestricted Grant (New York, New York), and the Department of Defense W81XWH-13-1-0048 (Washington, DC)
The sponsor or funding organization had no role in the design or conduct of this research.
Footnotes
Conflict of Interest: No conflicting relationship exists for any author.
This article contains additional online-only material. The following should appear online-only: Supplemental Tables 1, 2, and 3. Supplemental material is available at http://www.ophthalmology-retina.org.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Meyer D, Hamilton RC, Loken RG, Gimbel HV. Effect of combined peribulbar and retrobulbar injection of large volumes of anesthetic agents on the intraocular pressure. Canadian journal of ophthalmology. Journal canadien d’ophtalmologie. 1992;27(5):230–232. [PubMed] [Google Scholar]
- 2.Parke DW, 3rd, Flynn HW, Jr, Fisher YL. Management of intraocular foreign bodies: a clinical flight plan. Canadian journal of ophthalmology. Journal canadien d’ophtalmologie. 2013;48(1):8–12. doi: 10.1016/j.jcjo.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 3.Lincoff HA, Breinin GM, De Voe AG. The effect of succinylcholine on the extraocular muscles. Am J Ophthalmol. 1957;43(3):440–444. doi: 10.1016/0002-9394(57)92344-9. [DOI] [PubMed] [Google Scholar]
- 4.Kelly RE, Dinner M, Turner LS, Haik B, Abramson DH, Daines P. Succinylcholine increases intraocular pressure in the human eye with the extraocular muscles detached. Anesthesiology. 1993;79(5):948–952. doi: 10.1097/00000542-199311000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Igboko JO, Desalu I, Akinsola FB, Kushimo OT. Intraocular pressure changes in a Nigerian population--effects of tracheal tube and laryngeal mask airway insertion and removal. Niger Postgrad Med J. 2009;16(2):99–104. [PubMed] [Google Scholar]
- 6.Scott IU, McCabe CM, Flynn HW, et al. Local anesthesia with intravenous sedation for surgical repair of selected open globe injuries. Am J Ophthalmol. 2002;134(5):707–711. doi: 10.1016/s0002-9394(02)01692-6. [DOI] [PubMed] [Google Scholar]
- 7.Scott IU, Gayer S, Voo I, Flynn HW, Jr, Diniz JR, Venkatraman A. Regional anesthesia with monitored anesthesia care for surgical repair of selected open globe injuries. Ophthalmic Surg Lasers Imaging. 2005;36(2):122–128. [PubMed] [Google Scholar]
- 8.Chakraborty A, Bandyopadhyay SK, Mukhopadhyay S. Regional anaesthesia for surgical repair in selected open globe injuries in adults. Saudi J Ophthalmol. 2013;27(1):37–40. doi: 10.1016/j.sjopt.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pieramici DJ, Sternberg P, Jr, Aaberg TM, Sr, et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol. 1997;123:820–31. doi: 10.1016/s0002-9394(14)71132-8. [DOI] [PubMed] [Google Scholar]
- 10.Edge KR, Nicoll JM. Retrobulbar hemorrhage after 12,500 retrobulbar blocks. Anesth Analg. 1993;76(5):1019–1022. doi: 10.1213/00000539-199305000-00019. [DOI] [PubMed] [Google Scholar]
- 11.Meyers EF. Brain-stem anesthesia after retrobulbar block. Arch Ophthalmol. 1985;103(9):1278, 1282. doi: 10.1001/archopht.1985.01050090030017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1: Demographics, wound characteristics, and visual outcomes of zone 1 (n= 241) salvageable adult open globe injuries from 2004–2014.
Supplemental Table 2: Demographics, wound characteristics, and visual outcomes of zone 2 (n-135) salvageable adult open globe injuries from 2004–2014.
Supplemental Table 3: Demographics, wound characteristics, and visual outcomes of zone 3 (n=72) salvageable adult open globe injuries 2004–2014.


