Abstract
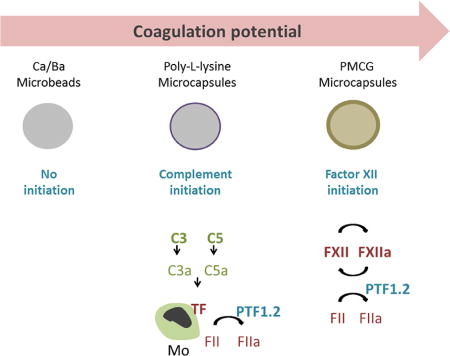
Alginate microspheres are presently under evaluation for future cell-based therapy. Their ability to induce harmful host reactions needs to be identified for developing the most suitable devices and efficient prevention strategies. We used a lepirudin based human whole blood model to investigate the coagulation potentials of alginate-based microspheres: alginate microbeads (Ca/Ba Beads), alginate poly-L-lysine microcapsules (APA and AP microcapsules) and sodium alginate-sodium cellulose sulfate-poly(methylene-co-cyanoguanidine) microcapsules (PMCG microcapsules). Coagulation activation measured by prothrombin fragments 1+2 (PTF1.2) was rapidly and markedly induced by the PMCG microcapsules, delayed and lower induced by the APA and AP microcapsules, and not induced by the Ca/Ba Beads. Monocytes tissue factor (TF) expression was similarly activated by the microcapsules, whereas not by the Ca/Ba Beads. PMCG microcapsules-induced PTF1.2 was abolished by FXII inhibition (corn trypsin inhibitor), thus pointing to activation through the contact pathway. PTF1.2 induced by the AP and APA microcapsules was inhibited by anti-TF antibody, pointing to a TF driven coagulation. The TF induced coagulation was inhibited by the complement inhibitors compstatin (C3 inhibition) and eculizumab (C5 inhibition), revealing a complement-coagulation cross-talk. This is the first study on the coagulation potentials of alginate microspheres, and identifies differences in activation potential, pathways and possible intervention points.
Keywords: Alginate microcapsules, coagulation, complement, cross-talk, factor XII, Tissue factor
Graphical abstract
1. Introduction
Alginate microspheres are currently under development as protecting devices for islet transplantation in diabetes type 1 treatment. As for biomaterials in general [1], the devices are under constant attack by the host defense system [2]. Defining low-activating materials and inhibitory points to reduce the pressure from the host defense system are some of the strategies to move the concept forward. The complement and coagulation systems represent two potent first-line defense systems and gateways to leukocyte-adhesion and inflammation.
The complement system is activated by alginate microspheres in variable amounts depending on their compositions [3]. We have previously shown that the inflammatory cytokine release is dependent on the complement deposition of C3b/iC3b to the biomaterial surface, which promotes subsequent cell-adhesion involving complement receptor 3 [4]. This response can be prevented by complement inhibition at the level of complement protein C3 [5]. The activation also leads to formation of cleavage products including the anaphylatoxins C3a and C5a, serving as potent chemoattractants and activators of inflammation [3]. The coagulation cascade represents a second gateway promoting cell-adhesion and potentially inflammation. Coagulation-induced cell adhesion can be initiated and lead to fibrinogen deposition on the biomaterial surface, which is formed in the last step of coagulation, and exposing motifs serving as CR3 ligands [6]. Since the biomaterial encounters complement and coagulation proteins and potentially blood during the transplantation, the ability to activate coagulation represents one additional factor to the overall host tolerability.
The complement and coagulation systems are both parts of a phylogenetic ancient defense system, containing sequentially activated zymogens converting to active proteinases. The complement system is activated by three different pathways, i.e. the classical, lectin and alternative pathways. The pathways assemble in a common step at the level of complement C3, followed by downstream activation of complement protein 5 (C5), resulting in the formation of the terminal C5b-9 complement complex (TCC). The coagulation system is activated through the extrinsic and intrinsic pathways. The extrinsic pathway is initiated through tissue factor (TF) exposed on damaged endothelia, exposed fibroblasts or activated blood monocytes under the aid of factor (F) VIIa. The intrinsic pathway is initiated by FXII conversion to FXIIa by negatively charged surfaces, as naturally present by activated platelets, DNA or collagen, or present on a biomaterial. FXIIa constitutes a part of the plasma kinin or contact pathway acting in a complex manner, and serving as a positive feedback activation of XII [7]. Further downstream, FXIIa propagates the coagulation cascade through activation of the surface bound FXI to XIa. The pathways emerge at the level of FX with further cleavage of FII (prothrombin) to FIIa (Thrombin), and finally the cleavage of fibrinogen to fibrin with subsequent clot formation.
The coagulation and complement systems are not separated systems, but rather cross-talks. For instance, the coagulation proteases (FXIa, FXa, FIXa, FIIa) are capable of directly cleave C3 and C5 [8], a finding that might be of physiological relevance [9]. Complement can also be a gateway into coagulation activation as C5a is shown to induce endothelial TF [10], monocyte TF [11, 12], TF on microparticles [13] and in certain cases on neutrophils [14]. In addition, platelets contain complement receptors for C3a and C5a [15], and C5b-9 triggers platelet prothrombinase activity [16]. The regulation of complement and coagulation is also coordinated by the protease inhibitor C1-esterase inhibitor (C1-INH) [7, 17]. In summary, findings show the existence of reciprocal cross-talk between the coagulation and complement systems, which also is of importance to biomaterial-induced inflammation.
Previously we demonstrated the complement activation potential of alginate microspheres to vary from high to low in the respective sequence; alginate poly-L-lysine microcapsules (APA and AP microcapsules), sodium alginate-sodium cellulose sulfate-poly(methylene-co-cyanoguanidine) microcapsules (PMCG microcapsules) and the alginate microbeads (Ca/Ba Beads) [3]. We further demonstrated that the inflammatory cytokine responses were linked at the complement activation, and particularly the complement on the microcapsules surface [4, 5]. These patterns of activation have corresponded well with the in vivo findings in various mice models investigating Ca/Ba Beads and poly-L-lysine microcapsules as reviewed in [2]. The multicomponent character of PMCG microcapsule provides the possibility to tune membrane properties depending on concentrations of polycationic and polyanionic components as well as the manufacturing process. This microcapsule type has shown the promise in both rodent and primate animal models [2].
The host responses might vary depending on the microspheres constructions, including the coagulation response. The lepirudin based human whole blood model specifically inhibits thrombin, but does not interfere with the complement system or rest of the coagulation system, so mutual interactions between these systems and with the blood cells can be investigated. Following the cleavage of prothrombin to thrombin, split fragments 1+2+3 are formed [18], where the prothrombin fragments 1+2 (PTF1.2) serve as a measure of the coagulation activation potential. Herein we investigate for the first time the coagulation activating potential of the different alginate microspheres using a human whole blood model and emphasize the cross-talk between the coagulation and complement systems based on both PTF1.2 and tissue factor (TF).
2. Materials and Methods
2.1 Reagents and materials
Alginates delivered from FMC BioPolymer AS (Novamatrix, Norway): Ultrapure Laminaria hyperborean (67% guluronic acid, UP-LVG, Lot nr. FP603-04) and Macrocystis pyrifera (44% guluronic acid, UP-100M, Lot nr. FP-209-02). Alginate derived from Kelko (San Diego, CA); SA-HV alginate, 59 % mannuronic acid and MW = 235 kDa, was provided by ISP Alginates (Girvan, Ayrshire, UK). Sodium cellulose sulfate (CS) was purchased from Acros Organics (New Jersey, NJ, USA) and poly(methylene-co-cyanoguanidine), (PMCG), from Scientific Polymer Products Inc. (Ontario, NY, USA). D-mannitol BDH Anala R., VWR International (Ltd, Pool, England), analytical grade calcium and barium chlorides were from Merck (Darmstadt, Germany). Poly-L-lysine hydrochloride (P2658, lot nr.091K5120), zymosan A (Z-4250), PBS with calcium and magnesium, ethylenediaminetetraacetic acid (EDTA), paraformaldehyde, and bovine serum albumin (BSA) were all purchased from Sigma-Aldrich (St. Louis, MO, USA). Non-pyrogenic sterile saline (0.9% NaCl) and endotoxin free, non-pyrogenic, water from B. Braun (Melsungen, Germany). The anti-coagulant lepirudin (Refludan®) was obtained from Celgene Europe (Windsor, GB).
The C3 inhibitor compstatin analog CP20 (Ac-Ile-[Cys-Val-Trp(Me)-Gln-Asp-Trp-Sar-Ala-His-Arg-Cys]-mlle-NH2) [19], CP40 ((D)Tyr-Ile-[Cys-Val-Trp(Me)-Gln-Asp-Trp-Sar-Ala-His-Arg-Cys]-mIle-NH2) [20], and a control peptide (Sar-Sar-Trp(Me)-Ala-Ala-Asp-Ile-His-Val-Gln-Arg-mlle-Trp-Ala-NH2) were synthesized as previously described [19, 20]. The C5 inhibitor eculizumab (Soliris®, Lot A78966DO2), a humanized monoclonal antibody, was derived from Alexion Pharmaceuticals (New Haven, CT, USA). The complement inhibitors were carefully titrated to give full inhibition of complement activation as measured by generation of complement activation products, specific for C3 (compstatin) and C5 (eculizumab).
The inhibitory antibody against human TF (Sekisui 4509) was obtained from American Diagnostica GmbH (Pfungstadt, Germany) with corresponding Ultra-leaf purified Mouse IgG1, isotype control (MG1-45, Biolegend, 400165). The factor XII inhibitor was corn trypsin inhibitor (CTI-01) from Haemotologic Technologies Inc. (Essex Junction, VT). In addition, the following antibodies utilized in these studies were; FITC conjugated anti-human Tissue factor (Sekisui, 4508CJ, American Diagnostica GmbH) and the corresponding FITC-conjugated isotype control Mouse IgG1 (BD 345815, clone X40), anti-CD14 PE (BD Biosciences, 345784), anti-human C5b-9 clone aE11 (Diatec, Oslo, Norway), and biotinylated 9C4 was an in-house made antibody as described in [21]. Streptavidin was from BioLegend (San Diego, USA) and substrate reagent A and B from R&D Systems (Minneapolis, USA). Commercial ELISAs used were Enzygnost F1+2 (monoclonal, OPBD035) Siemens Healthcare AS (Marburg, Germany) and Hycult human TCC ELISA kit (HK328-02, Uden, the Netherlands). Equipment for blood: Polypropylene vials (NUNC, Roskilde, Denmark) with BD vacutainer tops and BD vacutainer glass (Belliver Industrial Estate, Plymouth, UK) used for blood sampling and glass control, respectively.
2.2 Microsphere preparation
Alginate microspheres, ie: alginate microbeads (Ca/Ba Beads) and poly-L-lysine microcapsules (APA; alginate-poly-L-lysine-alginate, AP; alginate-poly-L-lysine) were made as previously described [3] using ultrapure and GMP alginate (UP-LVG) for the microbead formation, PLL as coating, and UP-100 alginate to screen the PLL residual charges. The Ca/Ba Beads and the APA/AP microcapsules were made utilizing a high-voltage electrostatic bead generator (7kV), and by 4 needles of internal diameter of 0.4 mm and a flow rate of alginate solution 10 ml/h per needle. Droplets of alginate solution (5 ml, 1.8% sodium alginate dissolved in 300 mM mannitol) were dropped into a gelling bath consisting of 50 mM CaCl2/1mM BaCl2/150 mM mannitol for the Ca/Ba Beads, and 50mM CaCl2/150 mM mannitol for the beads coated in the next step by PLL (formation of APA/AP microcapsules). After the last droplet, the beads were gelled for 10 min. The AP microcapsules were prepared by incubation in 0.1% PLL (25 ml) for 10 min, while the APA microcapsules were made with a subsequent incubation step of 0.1% UP-100M (10 ml) for 10 min. Between each step, the microcapsules were washed in 30 ml saline. Finally, the microbeads and microcapsules were harvested and stored in saline that a total volume was 10 ml (approximately 1:1 microspheres and saline). The sodium alginate – sodium cellulose sulfate – poly(methylene-co-cyanoguanidine) microcapsules (PMCG microcapsules) were produced in a multi-loop reactor with a continuous process and defined gelling time as described in [22] with following specifications: The PMCG1 microcapsules were formed by complexing of the polyanions 0.90% SA-HV alginate/0.9% CS in 0.9% NaCl with the polycation solution 1.2% PMCG/1% CaCl2 in 0.9% NaCl. The PMCG2 microcapsules were formed by the polyanions 0.9% UP-LVG alginate/0.90% CS in 0.9% NaCl and the polycation solution 1.2% PMCG/1% CaCl2 in 0.9% NaCl/0.025% Tween 20. Both PMCG microcapsule types gelled for 40s, treated with 50 mM citrate solution in 0.9% NaCl for 10 mins to sequester calcium and further coated with 0.1% CS solution in 0.9% NaCl for 10 min. The microspheres were made under strictly sterile conditions and with sterile solutions, and using autoclaved equipment and sterile hood in all steps. The endotoxin content of the alginates and reagents used for microspheres formation was measured by Endpoint Chromogenic LAL assays (Lonza) and resulted in following values: alginates UP-LVG (10 EU/g), UP-100 (26 EU/g), SA-HV (4070 EU/g), cellulose sulfate (80 EU/g) and PLL (316 EU/g). Prior to analysis, microspheres were stored in 0.9 % NaCl in a refrigerator.
2.3 Whole blood model
Whole blood from voluntary donors was collected in polypropylene vials containing lepirudin (50 µg/ml)). As previously described [3], 100 µl of samples (containing 50 µl microspheres, saline, zymosan (10 µg/vial) or LPS (final 10 ng/ml)), 100 µl PBS (w/Ca2+/Mg2+) and 500 µl blood were incubated for 60 and 240 min. Inhibitors were pre-incubated with the blood for 7 min (in 1:5 of inhibitor versus blood), thereafter, 600 µl of the pre-incubated blood was exposed to the microspheres. The final concentration of the complement inhibitors CP20 and CP40 was 20 µM, eculizumab was 100 µg/ml, whereas the FXIIa inhibitor corn trypsin inhibitor (CTI) was 40 µg/ml. EDTA (final 10 mM) was added to stop the complement and coagulation responses. Aliquots of plasma were stored at −20°C prior to analysis. Since CTI was not of clinical grade, the endotoxin content was measured by the Endpoint Chromogenic LAL; CTI (Lot BB1205 of 371800 EU/g) and (Lot CC0403 of 1600 EU/g). This corresponds to a final concentration of approximately 1400 and 6 pg/ml LPS during the experimental conditions (with 1EU resembling approximately 100 pg LPS).
2.4 Complement activation
The terminal sC5b-9 complex (TCC) was quantified in an ELISA using TCC specific capture Ab (aE11 detecting an antibody exposed in activated C9) and detection Ab (biotinylated anti-human C6). The assay was either performed with in-house made antibodies as described previously [21], or by the commercially available TCC ELISA (Hycult) containing the same antibodies, following the manufacturer’s protocol.
2.5 Prothrombin fragments 1+2
The concentration of PTF1.2 was measured by the Enzygnost® F1+2 monoclonal ELISA kit (Siemens Healthcare Diagnostics, Marburg, Germany) according to the manufacturer’s instructions.
2.6 Monocyte TF expression
Monocyte tissue factor (TF) was measured by flow cytometry (BD FACSCantoTM II flow cytometer). The various microspheres were incubated for 4 hours: thereafter EDTA (final concentration 10 mM) was incubated for 10 min to detach the adhered leukocytes. Whole blood (25 µl) was incubated with 2.5 µl anti-human TF (FITC)/anti-human CD14 (PE) or the isotype CTR (FITC mouse IgG1)/anti-human CD14 (PE) for 15 min on ice, thereafter leucocytes were fixed and RBCs lysed using BD fix/lyse solution (1 ml, 15 min in dark). Finally, leukocytes were centrifuged (210 g, 5 min, RT) and washed twice with 2 ml PBS. Monocytes and granulocytes were separated in a SSC/CD14 dot plot. The percentages of TF positive monocytes were determined by using the isotype CTR for setting the threshold values in a histogram. Of note, the eosinophilic granulocyte population had a strong autofluorescence in the FITC channel which easily could be misinterpreted as TF positive staining. For the granulocyte populations no specific staining above the isotype control was detected, pointing to the lack of TF expression by the granulocytes.
2.7 TF mRNA
PBS was added to whole blood pellets (equal amounts to retracted plasma), before adding PaxGene solution (1 ml blood sample/2.76 ml PaxGene solution) for RNA stabilization. Total RNA was extracted by the MagNa Pure 96 Cellular RNA large volume kit (Roche Diagnostics GmbH, Roche Applied BioScience, Mannheim, Germany) according to the manufacturer’s instructions. The extractions of the RNA were completed through MagNa Pure 96 instrument from Roche. The RNA concentration was estimated by the NanoDrop 2000c spectrophotometer (Thermo Fisher Scientific, Wilmington, DE). The cDNA was synthesized using High Capacity cDNA reverse transcription kit and 2720 Thermal cycler (Applied Biosystems) and stored at −80°C. The TF mRNA levels were measured using the 7500 Fast Real-Time PCR system (Applied Biosystems), TaqMan Fast Universal PCR Master Mix reagents and predeveloped TaqMan® gene expression assays. The target gene TF (TF, Hs 0017225, Applied Biosystems), and the reference gene human beta-2-microglobulin (TaqMan B2M Probe Dye Fam, 4333766 – 0804015, Applied Biosystems), were analyzed using qPCR with cycle conditions according to the manual. This reference gene was chosen because the expression of this gene was stable through the whole blood assay.
2.8 Statistical analysis
The results were analyzed using one-way repeated measurement ANOVA (multiple comparison test) using Dunnett’s post hoc test for comparison to the saline control, and Sidak’s post hoc test when comparing to an inhibitor. Data were beforehand transferred logarithmically due to the low number of donors. The analysis was performed using GraphPad Prism, version 6.04 (GraphPad Software, San Diago, CA, USA). Statistically significant values were considered as P<0.05. The level of significance is also given as * P<0.05, ** P<0.01, *** P<0.001, **** P<0.0001.
2.9 Ethics
The use of human whole blood for basal experiments was approved by the Regional Ethic Committee for medical and health research ethics under REK2009/2245 in accordance with their recommendation.
3. Results
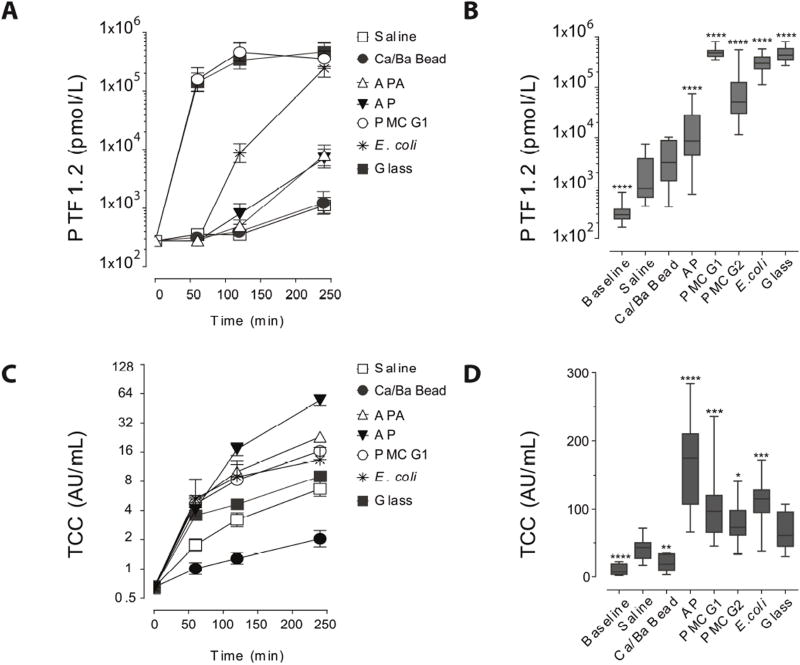
3.1 Coagulation (PTF1.2) and complement (TCC) activation
The time-dependent course of coagulation activation in human whole blood by the various types of microspheres pointed to the PMCG1 microcapsules as the strongest activators of coagulation. The marked increase in PTF1.2 from 280±20 pmol/l (mean± SEM) at baseline to 158000±91000 pmol/l after 60 min by the PMCG1 microcapsules was at a comparable level of the positive controls (glass and E. coli) (Fig. 1A). The APA and AP microcapsules showed a delayed and less pronounced PTF1.2 increase reaching 8000±4100 pmol/l at 240 minutes (Fig. 1A). The Ca/Ba Beads induction of PTF1.2 after 240 min was at 1200±700 pmol/l which was comparable to the saline control of 1100±400 pmol/l (Fig. 1A). For quantitative and statistical analyses, an extended number of blood donors (N=11–14) was investigated at 240 minutes (Fig. 1B). Except for the Ca/Ba Beads, the other microsphere types significantly enhanced the PTF1.2 levels above the saline control. The PMCG microcapsules were the most potent inducers of PTF1.2 with increases from the baseline to 1504× times for PMCG1 and 388× times for PMCG2. The increase in AP microcapsules was 55× times. In comparison the Ca/Ba Beads and the saline control showed an increase of 13× and 11× times after 240 min, respectively.
Figure 1.
Effect of alginate microspheres (alginate microbeads and microcapsules) on coagulation (PTF1.2) and complement (TCC) responses in the human whole blood model. A) Time-dependent effect on PTF1.2 (mean±SEM, N=4 donors), B) PTF1.2 at 240 min (N=11–14 donors), C) Time effect on TCC (mean±SEM, N=4 donors), D) TCC after 240 min (N=12–14). The data in B and D are given as box whisker plots with median, 25th and 75th percentiles and min/max values, and the level of significance shown as * P<0.05, ** P<0.01, *** P<0.001, **** P<0.0001.
The complement activating potential was tested in parallel (Fig. 1C–D). It showed a slightly different pattern with the AP microcapsules as the most potent complement activators, followed by the APA and PMCG microcapsules (Fig. 1C and 1D). Consistent with previous findings [3], the Ca/Ba Beads did not induce TCC, which was significant lower than the saline control (Fig. 1C and 1D). Thus, the Ca/Ba Beads induced neither PTF1.2 nor complement activation. It has to be noted that different ELISAs were used for quantification of the arbitrary units of TCC (see section 2.4), the in-house ELISA for the data presented in Fig. 1C and the commercial ELISA for the data in Fig. 1D.
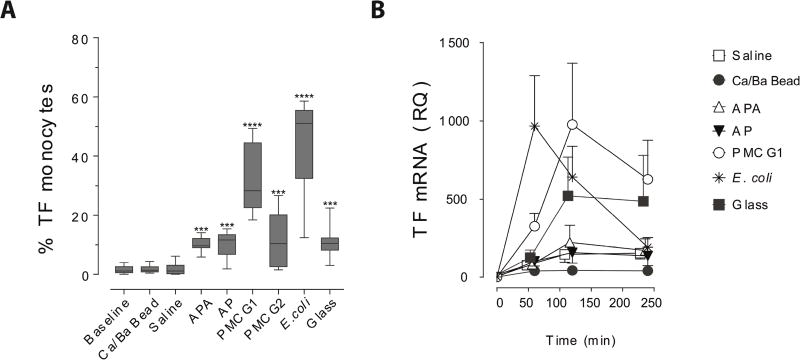
3.2 Monocyte tissue factor
TF is expressed by monocytes following stimulation by complement, LPS [12, 23] and the interleukins IL-6, IL-8, MCP-1 or PDGF-BB [24, 25], and could therefore potentially be induced by the various alginate microspheres. The PMCG, APA and AP microcapsules significantly increased monocyte TF surface expression compared to the saline control (Fig. 2A). Notably, the Ca/Ba Beads did not induce monocyte TF above the baseline levels or saline control.
Figure 2.
Effect of alginate microbeads (Ca/Ba Beads) and microcapsules (APA, AP, PMCG1, PMCG2) on monocyte TF expression in human whole blood. A) Monocyte TF expression (% positive cells) after 240 min incubation (box whisker plots giving median, 25th and 75th percentiles and min/max values of N=8), B) TF mRNA synthesis with time (relative quantitation (RQ) to baseline, mean ±SEM of N=3). The level of significance is *** P<0.001, **** P<0.0001.
The TF mRNA synthesis in whole blood was measured over time in three donors. The most potent TF inducer among the microspheres was the PMCG1 microcapsule, peaking after 120 min of incubation (Fig. 2B). The glass control showed the same activation pattern, although with less potency. The APA and AP microcapsules showed a smaller increase peaking after 120 min, and were only slightly more potent than the saline control. The Ca/Ba Beads showed lower values than the saline control, indicating no new synthesis of TF mRNA. The activation kinetics of the microspheres were slower than for the positive control (E. coli) peaking after 60 min.
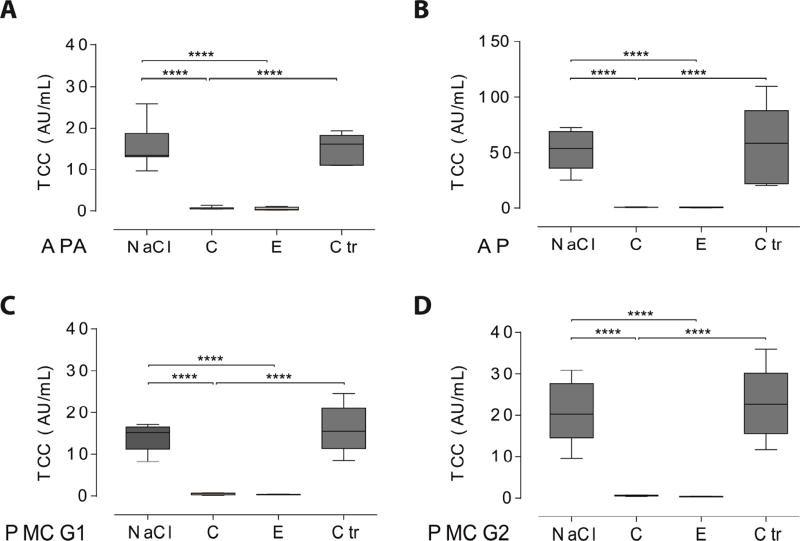
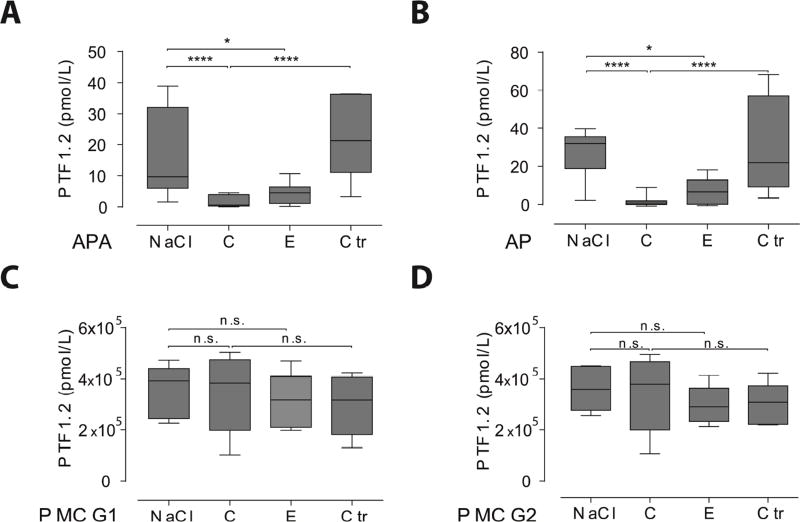
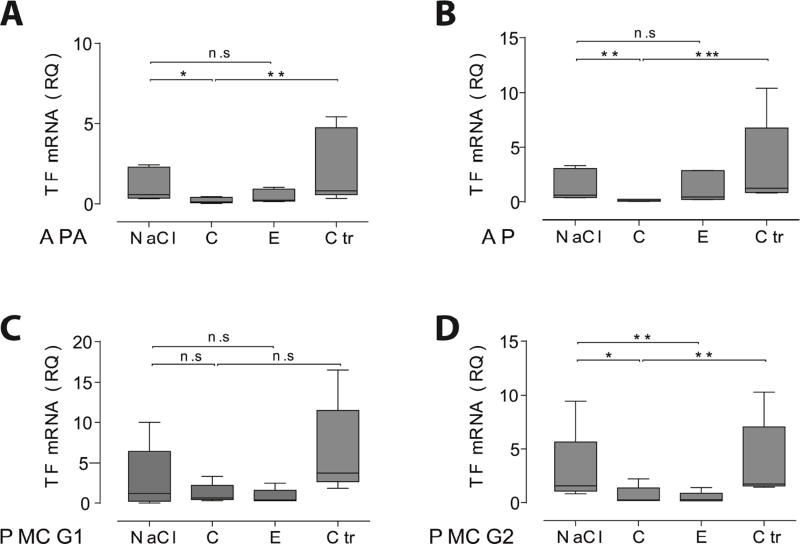
3.3 Complement and coagulation cross-talk
We further tested the interaction between complement and coagulation by selectively inhibiting complement prior to microcapsule exposure. A complete and significant effect of selective complement inhibition was first confirmed at the level of C3 and C5 by compstatin and eculizumab, respectively (Fig. 3A–D). The coagulation activation (PTF1.2) induced by the APA and AP microcapsules was inhibited completely and significantly by complement inhibition at the level of C3 (Fig. 4A–B). A significant inhibition was also found by selective inhibition of complement at the level of C5 (Fig. 4A–B). Complement inhibition significantly reduced the TF mRNA synthesis (Fig. 5A–B). The coagulation activation induced by the APA and AP microcapsules was therefore found to be mediated through complement. Notably, the complement inhibitors had no effect on the PTF1.2 generation by the PMCG microcapsules, (Fig. 4C–D), whereas TF mRNA synthesis was completely inhibited as compared to the saline control both by compstatin and eculizumab (Fig. 5C–D). In summary, these findings indicated that complement activation was responsible for the coagulation effects observed in this study, except for PMCG microcapsule-induced PTF1.2 formation.
Figure 3.
Complement inhibition at the level of C3 (compstatin, C) or C5 (eculizumab, E) abolish the TCC induction. A) APA microcapsules (N=7, N=5 for Ctr), B) AP microcapsules (N=7, N=5 for Ctr), PMCG1 microcapsules (N=5) and PMCG2 microcapsules (N=5). The x-axis abbreviations reflect the responses by the given microcapsule under incubation with either NaCl, compstatin (C), eculizumab (E) or the control peptide (Ctr). Graphs are given as box whisker plots with median, 25th and 75th percentiles and min/max values. The level of significance is **** P<0.0001.
Figure 4.
Effect of complement inhibition at the level of C3 (compstatin, C) and C5 (eculizumab, E) on the PTF1.2 induction. A) APA microcapsules (N=9, N=5 for Ctr), B) AP microcapsules (N=9, N=5 for Ctr), C) PMCG1 microcapsules (N=5) and D) PMCG2 microcapsules (N=5). The x-axis abbreviations reflect the responses by the given microcapsule under incubation with either NaCl, compstatin (C), eculizumab (E) or the control peptide (Ctr). Graphs are given as box whisker plots with median, 25th and 75th percentiles and min/max values. The level of significance was at * P<0.05, **** P<0.0001 whereas the non-significant differences are given as n.s.
Figure 5.
Effect of complement inhibition at the level of C3 (compstatin, C) and C5 (eculizumab, E) on tissue factor (TF) mRNA from human whole blood. A) APA microcapsules (N=4), B) AP microcapsules (N=4), PMCG1 microcapsules (N=4) and PMCG2 microcapsules (N=4). The x-axis abbreviations reflect the responses by the given microcapsule under incubation with either NaCl, compstatin (C), eculizumab (E) or the control peptide (Ctr). Data are relative to the saline control (without microspheres) and given as box whisker plots with median, 25th and 75th percentiles and min/max values. The level of significance are * P<0.05, ** P<0.01, *** P<0.001 whereas non-significant differences are given as n.s.
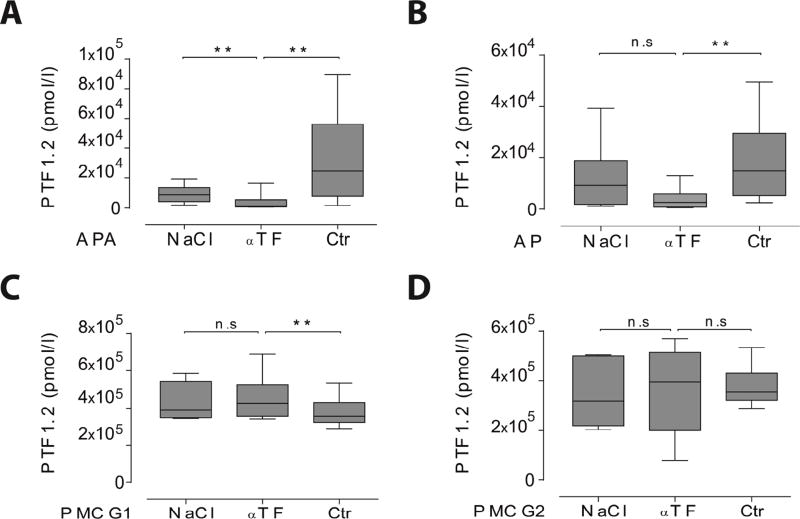
3.4 Inhibiting the extrinsic and intrinsic coagulation pathways
Next, we inhibited the TF pathway (extrinsic pathway) and the FXII-mediated contact pathway (intrinsic pathway). The monoclonal anti-TF antibody significantly reduced APA and AP induced PTF1.2 compared to the isotype control antibody (Fig. 6A–B). Despite the elevated level of TF expression on monocytes following addition of PMCG microcapsules, no inhibition of coagulation was found with the inhibitory anti-TF antibody (Fig. 6C–D).
Figure 6.
Effect of TF inhibition on microcapsule-induced coagulation (PTF1.2) in human whole blood after 240 min incubation. The microcapsules were either incubated with NaCl only, inhibitory TF antibody ( TF) or its respective isotype control antibody (Ctr, mouse IgG1). A) APA microcapsules (N=8), B) AP microcapsules (N=8), C) PMCG1 microcapsules (N=6), D) PMCG2 microcapsules (N=6). Data are given as box whisker plots with median, 25th and 75th percentiles and min/max values. The level of significance was ** P<0.01, whereas non-significant differences are given as n.s.
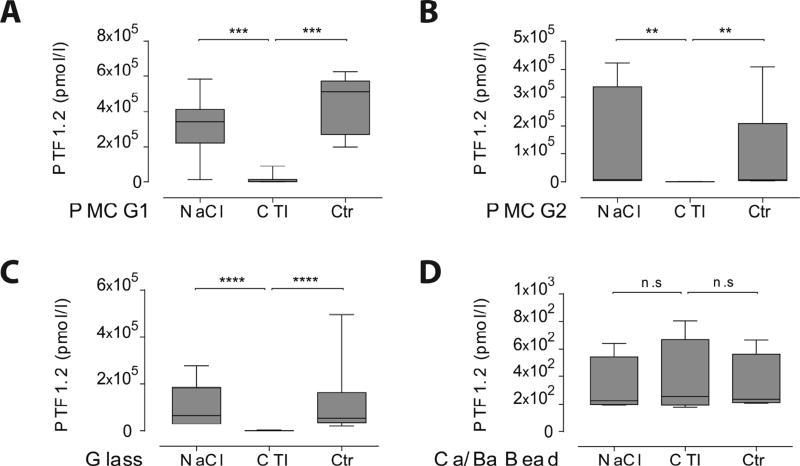
Since the TF induction could not explain the PTF1.2 induced by the PMCG microcapsules, the role of FXII was further investigated. The CTI inhibitor is interfering with FXIIa in a molar ratio of 1:1 [26], and can be used to inhibit the contact activation pathway of coagulation. The factor XII inhibitor CTI blocked PTF1.2 totally and significantly with short-time exposure (Fig. 7A–B), thus pointing to a contact-dependent activation. Glass is a potent contact pathway activator, and was also completely and significantly inhibited by CTI (Fig. 7C). The surface charge of alginate microbeads has been shown to be negative [27], and thus FXII could potentially be involved explaining the slightly elevated coagulation potential as compared to the complement activation potential by the Ca/Ba Beads. However, no effect of CTI was found after 30 min of incubation (Fig. 7D), thus the FXII was not activated by the Ca/Ba Beads.
Figure 7.
Effect of FXII inhibition on microcapsules induced coagulation (PTF1.2) in human whole blood after 30 min. The microcapsules were either incubated with NaCl only, the factor XII inhibitor CTI or albumin (Ctr). A) PMCG1 microcapsules (N=7), B) PMCG2 microcapsules (N=7), C) Glass (N=4) and D) Ca/Ba Beads (N=4). Data are given as box whisker plots with median, 25th and 75th percentiles and min/max values. The level of significance was **<0.01 and *** P<0.001, **** P<0.0001, whereas non-significant differences are given as n.s.
4. Discussion
The coagulation activation potential of various alginate microspheres is for the first time presented herein using the following microspheres, namely alginate microbeads (Ca/Ba Beads), poly-L-lysine containing alginate microcapsules (AP and APA) and multicomponent alginate–cellulose sulfate – poly(methylene-co-cyanoguanidine) microcapsules (PMCG1 and PMCG2). A large variability in coagulation activation potential was found, with the PMCG microcapsules being the most reactive, the APA and AP microcapsules being intermediately reactive and the Ca/Ba Beads being poor inducers of coagulation. Taking complement reactivity into account, as evaluated previously [5] and in agreement with the present data, the Ca/Ba Beads stand out as the overall least reactive. Further on, the APA and AP reactivity is mainly triggered by complement with a secondary effect on coagulation, while the PMCG microcapsules initially were activating coagulation through FXII in a complement-independent manner. It is now well recognized that the complement and coagulation systems are cross-talking at different points [17]. In the present study we found further evidence that complement activation could be directly responsible for induction of the TF-driven coagulation pathway, which explain pathophysiological mechanisms and may have future therapeutic implications, as outlined below.
The PMCG microcapsules induced a strong coagulation response mainly due to the activation of FXII. The PMCG microcapsules contain cellulose sulfate, a highly negatively charged polymer with sulfated groups in the outer coatings, and also in the membrane complexed with PMCG [28]. It is well recognized that negatively charged surfaces are strong inductors of coagulation through the contact activation pathway, thus our data are consistent with the physicochemical properties of the PMCG microcapsules and the established knowledge of coagulation activation. We also found contribution from the TF driven pathway, with the PMCG microcapsules inducing TF mRNA synthesis as well as monocyte TF. Still, inhibition with anti-TF had no effect on coagulation activation, showing that the overall contribution to coagulation activation from the TF pathway was minor, which probably was related to the fast activation of FXII.
Previously, Huber-Lang and Amara et al. have demonstrated the coagulation proteases (FXIa, FXa, FIXa and thrombin) to promote a direct cleavage of complement C3 and C5 [8, 9, 29]. Due to the strong coagulation activity by the PMCG microcapsules, a direct cleavage of C5 by the coagulation proteases could provide an explanation for their complement activating potential. An early complement TCC formation has often been apparent by the PMCG microcapsules, but over time the PMCG microcapsules are less reactive than the poly-L-lysine microcapsules [3], which might be in agreement with a direct cleavage. Further on, a relatively low formation of C3 convertase on the PMCG microcapsule surfaces [3] might further point to a fluid phase initiated TCC formation in agreement with a direct cleavage. In addition, platelets activation by sulfated polysaccharides (sulfated glycosaminoglycan) previously have shown to mediate TCC, a phenomenon blocked by compstatin [30]. Since sulfated groups are present in cellulose sulfate, we cannot exclude similar mechanisms also for the PMCG microcapsule.
The APA and AP microcapsules activated coagulation through monocyte TF, which was connected to initial complement activation. This was evident by the monocyte TF up-regulation and blockage by anti-TF, and further with the complement inhibition. It must be emphasized that only monocytes expressed TF on the surface. A possible contribution from platelets was not investigated, however, according to Osterud and his investigation of blood derived TF sources, platelets are not synthesizing TF [31]. Also, coagulation activation by platelets involving complement has been found to be mediated through the contact system [26], while the TF pathway was the main initiator by the APA and AP microcapsules. The inhibitory effect of complement, as also manifested on the TF mRNA level, therefore most likely explains the effects of complement inhibition on monocyte TF upregulation.
The complete inhibition of coagulation by compstatin at the level of C3 as presently shown, does not distinguish between the contribution from C3a and C5a, since both are inhibited. The residual coagulation activation by inhibition at the C5 level by eculizumab could thus reflect the contribution from C3a, and further points to C5a as the most potent TF inductor. Since also the formation of C3b/iC3b, cell-adhesion and cytokines is prevented by compstatin [4], we cannot exclude also their involvement. The involvement of inflammatory cytokines on monocyte TF expression would however most likely be secondary to the effect of the rapidly produced complement activation products [3]. Since complement activation also is a pre-requisite for cytokine induction by the microcapsules [4, 5], we conclude that complement activation including the anaphylatoxins most probably is the main inducer of TF in the present investigation.
Coagulation activation with formation of fibrin may be one of the gateways to bio-incompatibility in a transplantation situation. The most common transplantation site for islets encapsulated in microbeads or microcapsules is the peritoneal cavity, due to the space requirements for a therapeutic amount of transplanted islets. Although the continuous exposure to blood is avoided, there is likely that the transplanted microspheres are exposed to blood particularly during implantation. The high coagulation reactivity of the PMCG microcapsules and their independence of complement activation might be a challenge during transplantation with blood contamination, since it could lead to surface deposition of fibrin. Since fibrin exposes epitopes serving as ligands for CR3 (CD11b/CD18) [6], the fibrin deposition is a potential starting point for leukocyte-attachment. It might therefore be of high importance to avoid bleeding during a transplantation situation using the PMCG microcapsules. A short-time inhibition of FXII could be a way of inhibiting the coagulation potential of the PMCG microcapsules during the critical phase of implantation, since currently there are ongoing FXII-inhibition studies for thrombosis treatments [32]. Despite the coagulation reactivity, the PMCG microcapsules can be low activators of fibrotic overgrowth reactions as shown in mice [22] and baboons [33]. This demonstrates that these type of microcapsules can be well tolerated and, thus, that there may not be the lack of a direct link between the coagulation activation potential and the fibrotic responses. This reported toleration may simply indicate the absence of microcapsule exposure to blood; a controlled bleeding experiment could contribute to clarifying these questions. On the other hand, the reactivity of the APA and AP microcapsules, points a definite complement-dependent reactivity, probably as the most important mechanism promoting leukocyte adhesion as previously shown [4].
The additional measurements of coagulation activation in addition to complement and inflammatory cytokines provide together an efficient screening system for the immediate host reactivity promoted by the protein cascades in concert with the leukocytes. In transplantation setting there will also be encapsulated cells within the devices, which add complexity to the situation by secreted cellular component provoking other parts of the host immune system as addressed in [2]. The whole blood model is, first of all, efficient to measure the surface reactivity and the material response, and, therefore, this model is strongly recommended to design low-reactive devices. However, as the model also contains the blood leukocytes containing the damage-associated molecular patterns (DAMPs) receptors sensing release of dying or stress cells components, the model possibly can be used to evaluate the impact of encapsulated cells. In summary, the host immune system evolves a complex set of mechanisms that will contribute in a transplantation setting and that we need to carefully examine in order to enhance our understanding in the design of immunoprotective devices. The coagulation response evaluated in this work represents an important part of this learning curve.
5. Conclusions
In conclusion, our data identifies for the first time the reactivity of the various alginate microspheres on coagulation, identifying PMCG microcapsules as pro-coagulative, the APA and AP microcapsules to be weaker inducers and the Ca/Ba Beads as low/inert to coagulation activation. Further on, we found the coagulation activation of the PMCG microcapsules was strongly dependent on direct activation by FXII, whereas by the APA and AP microcapsules were highly dependent on initial complement activation promoting TF in monocytes, thus further defining a complement-coagulation cross-talk in these interactions.
Statement of significance.
Alginate microcapsules are prospective candidate materials for cell encapsulation therapy. The material surface must be free of host cell adhesion to ensure free diffusion of nutrition and oxygen to the encapsulated cells. Coagulation activation is one gateway to cellular overgrowth through deposition of fibrin. Herein we used a physiologically relevant whole blood model to investigate the coagulation potential of alginate microcapsules and microbeads. The coagulation potentials and the pathways of activation were depending on the surface properties of the materials. Activation of the complement system could also be involved, thus emphasizing a complement-coagulation cross-talk. Our findings points to complement and coagulation inhibition as intervention point for preventing host reactions, and enhance functional cell-encapsulation devices.
Acknowledgments
This work has been financially supported by The Liaison Committee for education, research and innovation in Central Norway (RHA) under grants 46049600, 46056819 and 46062127 in coordination with the Norwegian University of Science and Technology (NTNU). This work has also been supported by the Research Council of Norway through its Centers of Excellence funding scheme, project number 223255; the JDRF (Juvenile Diabetes Research Foundation) under grant number 2-SRA-2014-288-Q-R; The Odd Fellow Foundation [OFF-2014]; The Simon Fougner Hartmann Family Fund [SFHF-12/14], The European Community's Seventh Framework Programme under grant agreement n° 602699 (DIREKT), and by National Institutes of Health Grants AI068730 and AI030040 and by the Slovak Research and Development Agency under contract number APVV-14-858. Dr. Gabriela Kollarikova is thanked for preparation of PMCG1 and PMCG2 microcapsules.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure
The authors declare no conflicts of interests. J.D.L. is the inventor of patents and/or patent applications that describe the use of complement inhibitors for therapeutic purposes and the founder of Amyndas Pharmaceuticals, which is developing complement inhibitors for clinical applications. We confirm that all authors have approved the final article.
References
- 1.Anderson JM, Rodriguez A, Chang DT. Foreign body reaction to biomaterials. Semin. Immunol. 2008;20(2):86–100. doi: 10.1016/j.smim.2007.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rokstad AM, Lacik I, de Vos P, Strand BL. Advances in biocompatibility and physicochemical characterization of microspheres for cell encapsulation. Advanced drug delivery reviews. 2014;67–68:111–30. doi: 10.1016/j.addr.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 3.Rokstad AM, Brekke OL, Steinkjer B, Ryan L, Kollarikova G, Strand BL, Skjak-Braek G, Lacik I, Espevik T, Mollnes TE. Alginate microbeads are complement compatible, in contrast to polycation containing microcapsules, as revealed in a human whole blood model. Acta Biomater. 2011;7(6):2566–2578. doi: 10.1016/j.actbio.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 4.Orning P, Hoem KS, Coron AE, Skjak-Braek G, Mollnes TE, Brekke OL, Espevik T, Rokstad AM. Alginate microsphere compositions dictate different mechanisms of complement activation with consequences for cytokine release and leukocyte activation. J Control Release. 2016;229:58–69. doi: 10.1016/j.jconrel.2016.03.021. [DOI] [PubMed] [Google Scholar]
- 5.Rokstad AM, Brekke OL, Steinkjer B, Ryan L, Kollarikova G, Strand BL, Skjak-Braek G, Lambris JD, Lacik I, Mollnes TE, Espevik T. The induction of cytokines by polycation containing microspheres by a complement dependent mechanism 1. Biomaterials. 2013;34(3):621–630. doi: 10.1016/j.biomaterials.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 6.Hu WJ, Eaton JW, Ugarova TP, Tang L. Molecular basis of biomaterial-mediated foreign body reactions. Blood. 2001;98(4):1231–1238. doi: 10.1182/blood.v98.4.1231. [DOI] [PubMed] [Google Scholar]
- 7.Kaplan AP, Ghebrehiwet B. The plasma bradykinin-forming pathways and its interrelationships with complement. Mol Immunol. 2010;47(13):2161–9. doi: 10.1016/j.molimm.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 8.Amara U, Rittirsch D, Flierl M, Bruckner U, Klos A, Gebhard F, Lambris JD, Huber-Lang M. Interaction between the coagulation and complement system. Adv. Exp. Med. Biol. 2008;632:71–79. doi: 10.1007/978-0-387-78952-1_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huber-Lang M, Sarma JV, Zetoune FS, Rittirsch D, Neff TA, McGuire SR, Lambris JD, Warner RL, Flierl MA, Hoesel LM, Gebhard F, Younger JG, Drouin SM, Wetsel RA, Ward PA. Generation of C5a in the absence of C3: a new complement activation pathway. Nat. Med. 2006;12(6):682–687. doi: 10.1038/nm1419. [DOI] [PubMed] [Google Scholar]
- 10.Ikeda K, Nagasawa K, Horiuchi T, Tsuru T, Nishizaka H, Niho Y. C5a induces tissue factor activity on endothelial cells. Thromb Haemost. 1997;77(2):394–8. [PubMed] [Google Scholar]
- 11.Landsem A, Nielsen EW, Fure H, Christiansen D, Ludviksen JK, Lambris JD, Osterud B, Mollnes TE, Brekke OL. C1-inhibitor efficiently inhibits Escherichia coli-induced tissue factor mRNA up-regulation, monocyte tissue factor expression and coagulation activation in human whole blood. Clin Exp Immunol. 2013;173(2):217–29. doi: 10.1111/cei.12098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Landsem A, Fure H, Christiansen D, Nielsen EW, Osterud B, Mollnes TE, Brekke OL. The key roles of complement and tissue factor in Escherichia coli-induced coagulation in human whole blood. Clin Exp Immunol. 2015;182(1):81–9. doi: 10.1111/cei.12663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ovstebo R, Hellum M, Aass HC, Troseid AM, Brandtzaeg P, Mollnes TE, Henriksson CE. Microparticle-associated tissue factor activity is reduced by inhibition of the complement protein 5 in Neisseria meningitidis-exposed whole blood. Innate Immun. 2014;20(5):552–60. doi: 10.1177/1753425913502099. [DOI] [PubMed] [Google Scholar]
- 14.Ritis K, Doumas M, Mastellos D, Micheli A, Giaglis S, Magotti P, Rafail S, Kartalis G, Sideras P, Lambris JD. A novel C5a receptor-tissue factor cross-talk in neutrophils links innate immunity to coagulation pathways. J. Immunol. 2006;177(7):4794–4802. doi: 10.4049/jimmunol.177.7.4794. [DOI] [PubMed] [Google Scholar]
- 15.Ward MV, Conway DL. A severe case of acute suppurative dermatitis with disseminated intravascular coagulation in a dog. Vet Med Small Anim Clin. 1980;75(10):1564–8. [PubMed] [Google Scholar]
- 16.Wiedmer T, Esmon CT, Sims PJ. On the mechanism by which complement proteins C5b-9 increase platelet prothrombinase activity. J Biol Chem. 1986;261(31):14587–92. [PubMed] [Google Scholar]
- 17.Conway EM. Reincarnation of ancient links between coagulation and complement. J Thromb Haemost. 2015;13(Suppl 1):S121–32. doi: 10.1111/jth.12950. [DOI] [PubMed] [Google Scholar]
- 18.Rabiet MJ, Blashill A, Furie B, Furie BC. Prothrombin fragment 1 × 2 × 3, a major product of prothrombin activation in human plasma. J. Biol. Chem. 1986;261(28):13210–13215. [PubMed] [Google Scholar]
- 19.Qu H, Ricklin D, Bai H, Chen H, Reis ES, Maciejewski M, Tzekou A, Deangelis RA, Resuello RR, Lupu F, Barlow PN, Lambris JD. New analogs of the clinical complement inhibitor compstatin with subnanomolar affinity and enhanced pharmacokinetic properties. Immunobiology. 2012 doi: 10.1016/j.imbio.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qu H, Magotti P, Ricklin D, Wu EL, Kourtzelis I, Wu YQ, Kaznessis YN, Lambris JD. Novel analogues of the therapeutic complement inhibitor compstatin with significantly improved affinity and potency. Mol Immunol. 2011;48(4):481–9. doi: 10.1016/j.molimm.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mollnes TE, Redl H, Hogasen K, Bengtsson A, Garred P, Speilberg L, Lea T, Oppermann M, Gotze O, Schlag G. Complement activation in septic baboons detected by neoepitope-specific assays for C3b/iC3b/C3c, C5a and the terminal C5b-9 complement complex (TCC) Clin. Exp. Immunol. 1993;91(2):295–300. doi: 10.1111/j.1365-2249.1993.tb05898.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lacik I, Brissova M, Anilkumar AV, Powers AC, Wang T. New capsule with tailored properties for the encapsulation of living cells. J. Biomed. Mater. Res. 1998;39(1):52–60. doi: 10.1002/(sici)1097-4636(199801)39:1<52::aid-jbm7>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 23.Brekke OL, Waage C, Christiansen D, Fure H, Qu H, Lambris JD, Osterud B, Nielsen EW, Mollnes TE. The Effects of Selective Complement and CD14 Inhibition on the E. coli-Induced Tissue Factor mRNA Upregulation, Monocyte Tissue Factor Expression, and Tissue Factor Functional Activity in Human Whole Blood. Adv. Exp. Med. Biol. 2013;734:123–136. doi: 10.1007/978-1-4614-4118-2_8. [DOI] [PubMed] [Google Scholar]
- 24.Ernofsson M, Siegbahn A. Platelet-derived growth factor-BB and monocyte chemotactic protein-1 induce human peripheral blood monocytes to express tissue factor. Thromb Res. 1996;83(4):307–20. doi: 10.1016/0049-3848(96)00139-9. [DOI] [PubMed] [Google Scholar]
- 25.Neumann FJ, Ott I, Marx N, Luther T, Kenngott S, Gawaz M, Kotzsch M, Schomig A. Effect of human recombinant interleukin-6 and interleukin-8 on monocyte procoagulant activity. Arterioscler Thromb Vasc Biol. 1997;17(12):3399–405. doi: 10.1161/01.atv.17.12.3399. [DOI] [PubMed] [Google Scholar]
- 26.Hojima Y, Pierce JV, Pisano JJ. Hageman factor fragment inhibitor in corn seeds: purification and characterization. Thromb Res. 1980;20(2):149–62. doi: 10.1016/0049-3848(80)90381-3. [DOI] [PubMed] [Google Scholar]
- 27.You JO, Park SB, Park HY, Haam S, Chung CH, Kim WS. Preparation of regular sized Ca-alginate microspheres using membrane emulsification method. J Microencapsul Journal of Microencapsulation. 2001:521–532. doi: 10.1080/02652040010018128. [DOI] [PubMed] [Google Scholar]
- 28.Lacik I, Anilkumar AV, Wang TG. A two-step process for controlling the surface smoothness of polyelectrolyte-based microcapsules. J. Microencapsul. 2001;18(4):479–490. doi: 10.1080/02652040010018137. [DOI] [PubMed] [Google Scholar]
- 29.Amara U, Flierl MA, Rittirsch D, Klos A, Chen H, Acker B, Bruckner UB, Nilsson B, Gebhard F, Lambris JD, Huber-Lang M. Molecular intercommunication between the complement and coagulation systems. J. Immunol. 2010;185(9):5628–5636. doi: 10.4049/jimmunol.0903678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hamad OA, Ekdahl KN, Nilsson PH, Andersson J, Magotti P, Lambris JD, Nilsson B. Complement activation triggered by chondroitin sulfate released by thrombin receptor-activated platelets. J. Thromb. Haemost. 2008;6(8):1413–1421. doi: 10.1111/j.1538-7836.2008.03034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Osterud B. Tissue factor expression in blood cells. Thromb. Res. 2010;125(Suppl 1):S31–S34. doi: 10.1016/j.thromres.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 32.May F, Krupka J, Fries M, Thielmann I, Pragst I, Weimer T, Panousis C, Nieswandt B, Stoll G, Dickneite G, Schulte S, Nolte MW. FXIIa inhibitor rHA-Infestin-4: Safe thromboprotection in experimental venous, arterial and foreign surface-induced thrombosis. Br J Haematol. 2016;173(5):769–78. doi: 10.1111/bjh.13990. [DOI] [PubMed] [Google Scholar]
- 33.Qi M, Lacik I, Kollarikova G, Strand BL, Formo K, Wang Y, Marchese E, Mendoza-Elias JE, Kinzer KP, Gatti F, Paushter D, Patel S, Oberholzer J. A recommended laparoscopic procedure for implantation of microcapsules in the peritoneal cavity of non-human primates. J. Surg. Res. 2011;168(1):e117–e123. doi: 10.1016/j.jss.2011.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]