Abstract
Objective
Obesity is prevalent in midlife women and contributes to poor health outcomes. Understanding mechanisms leading to weight gain in this population is of importance for prevention and intervention. The current study investigated the association between depressive symptoms and weight in midlife women by examining (1) stress eating as a mediator between depressive symptoms and weight, and (2) menopausal status as a moderator of the associations of depressive symptoms, stress eating, and weight.
Methods
An archival analysis was performed using data from the Midlife in the United States II study (MIDUS II). The sample consisted of 815 premenopausal and postmenopausal women. Measures included the CIDI-SF, a coping questionnaire, and BMI.
Results
Moderated mediation analyses were conducted with ordinary least squares path analyses using Hayes’ PROCESS macro. Controlling for covariates, depressive symptoms were not directly associated with weight, b= −0.4, 95% CI [−0.4, 0.1]. However, stress eating was a significant mediator between depressive symptoms and weight, b= 0.3, 95% CI [0.06, 0.3]. The mediation was conditional on menopausal stage, b= 0.2, 95% CI [0.05, 0.4], with depressive symptoms and stress eating significantly associated in postmenopausal, not premenopausal women, b= 0.3, 95% CI [0.2, 0.5].
Conclusions
Both stress eating and menopausal status significantly contributed to the depressive symptom—weight association. Psychosocial factors play an important role in the association between depressive symptoms and weight, and the results highlight the need to focus on both behavioral factors as well as menopausal status when identifying who is at risk for the development of poor weight outcomes.
Keywords: stress eating, depressive symptoms, weight, BMI, midlife women, menopause
Women in midlife are at an increased risk for the development of poor weight outcomes including obesity.1 Obesity, defined as having a body mass index (BMI) greater than or equal to 30,2 increases the risk for insulin resistance which can lead to weight-related diseases such as metabolic syndrome, diabetes, and cardiovascular disease.3 As of 2014, 40% of women in midlife were classified as overweight or obese.1 Many factors account for the change in weight status in this age group, one of which is the menopausal transition.4, 5, 6 Given that weight gain during this time period is common and associated with extremely poor health outcomes, it is of importance to investigate mechanisms that contribute to increases in BMI in this population.
While biological mechanisms such as fluctuating estrogen levels and changes in body fat distribution are commonly associated with weight gain during midlife,1 psychosocial factors also contribute to increases in BMI during this time. Changes in health status, “empty-nest” adjustment issues, and financial difficulties have all been shown to relate to poor weight outcomes in midlife women populations.1, 7, 8 One additional psychological factor that is linked to weight gain in midlife women is depression and depressive symptoms.9 Depression is prevalent in this population, with the menopausal transition cited as a “window of vulnerability” for the development of depressive symptoms given changes in hormonal levels and lifestyle factors.10, 11, 12
While depression leads to poor weight outcomes across many different populations, it is of specific importance to investigate the association in midlife women given the high prevalence of both conditions in this population.1, 9, 13, 14 Previous research has shown depression to be related to obesity and higher caloric intake in midlife women.9 Depression and poor weight outcomes have also been linked to menopausal status with women in the menopausal transition (peri and postmenopause) at greater risk for the development of both depression and obesity than women in premenopause.8 Reasons for this increase in risk is due to the combination of hormonal changes and environmental stress. 8, 21
The co-occurrence of depression and weight gain in midlife women is particularly concerning given that both conditions are linked to significant economic costs, high rates of disability, and are associated with health issues such as cardiovascular disease, stroke, metabolic syndrome, diabetes, and mental health problems such as anxiety and substance use.15, 9 Consequently, there is a need to investigate underlying mechanisms that connect these conditions in order to identify both prevention and intervention targets. As depression is commonly linked to increases in caloric intake, one potential mechanism linking depressive symptoms and weight gain is eating behavior. Certain eating behavior such as stress eating, is related to mood fluctuations and depressive symptomology and is also recognized as a risk factor for obesity.16, 17, 18 Stress eating, defined as eating in response to stressors and/or negative emotions, involves overconsumption of food and/or consumption of energy dense food.19, 20 Stress and/or negative emotion can influence appetite by either decreasing or increasing appetite, with a typical response to acute stress and emotion fluctuation (e.g., threat to safety) presenting as decreased appetite, 21 and chronic stress and chronic distress (e.g., job pressure, financial stress, caregiving responsibility) tending to increase appetite and desire for energy dense food.19
Women in midlife experience significant stress and mood fluctuations, both of which are predictive of poor eating habits and maladaptive coping behavior such as stress eating.18, 19, 22 In addition, the impact of depression, stress, and menopause can serve to exacerbate stress responses and biological processes.21 For example, depression, menopause, and environmental stress are associated with lowered estrogen levels. Thus, the combination of biological, psychological, and social factors create a hormonal imbalance, which influences maladaptive coping responses including stress eating.21 Furthermore, decreases in estrogen increases eating in response to emotion and stress.23 As women in midlife experience fluctuations in estrogen, with the greatest decreases during and after the menopausal transition, 8,22 it is of value to investigate the interconnectedness between depression, menopausal status, and stress eating on weight gain in this population. Furthermore, as postmenopausal women are more likely to experience increases in appetite due to depression compared to premenopausal women,8 it is likely that the interconnectedness between depression, menopausal status, and stress eating is relevant to explore in this population. This is especially important given the impact of these factors on subsequent weight gain.
Investigating stress eating as a potential link between depression and weight is relevant in midlife women given that stress eating is empirically linked to both depression and weight18, 22, 24 and is a common yet relatively unexplored behavior through which depression is linked to weight gain specifically in midlife women. While depression has been linked to greater fast food consumption in midlife, and women have been shown to be more at risk for stress eating and emotional eating when depressed,17, 18, 22 less is known about (1) how stress eating may serve as a mediator between depression and weight in samples of midlife women, and (2) how menopausal status may affect the associations between depression, stress eating, and weight. Stress eating is an important factor to examine given that it is a modifiable behavior to target for obesity prevention and weight loss in this population. Furthermore, understanding the role of menopausal stage in these associations can help to identify subsets of midlife women who may be most at risk for the development of obesity in combination with depression.
Therefore, the current study aims to (1) examine the association between depressive symptoms and weight in midlife women, (2) investigate stress eating as a mediator of the depressive symptom-weight association, and (3) examine the moderating influence of menopausal status on this association. We anticipate that that depressive symptom will be associated with higher weight outcomes in the current sample. Building on previous research identifying a link between depressive symptoms and stress eating,18 we also hypothesize that higher endorsement of depressive symptoms will be associated with greater endorsement of stress eating and thus higher weight outcomes. Given previous work that has demonstrated that postmenopausal women are more likely to endorse depressive symptoms and more likely to have higher BMI than women in premenopause,8 we anticipate menopausal status to be a moderator of the associations between depressive symptoms and weight, depressive symptoms and stress eating, and stress eating and weight. We anticipate that postmenopausal status will exacerbate the depressive symptom—weight, depressive symptoms—stress eating and stress eating—weight associations.
Method
Participants
Participants are from the Midlife in the United States (MIDUS) II study, a longitudinal telephone and paper-and-pencil follow-up survey of the original MIDUS I study. Data collection for MIDUS II took place from 2004–2006. All eligible participants were non-institutionalized, English-speaking adults, and between 35–86 years of age. The MIDUS II sample included approximately 4963 participants and consisted of four sub-projects. Data for the current study are taken from Project 1 of the MIDUS II study. Project 1 investigated the role of behavioral, psychological, and social factors in age-related differences in health (both mental and physical health).
The current study consists of a sub-sample of 815 female MIDUS II participants between the ages of 40–64 who completed Project 1 of the MIDUS II study. Participants were included if they were in the specified age range (i.e., 40–64) and completed demographic, psychological, and physical health measures. The sample consists of 392 premenopausal women and 423 postmenopausal women. Perimenopausal women were not included in the current study due to too few women meeting criteria in the current sample (n = 71).
Procedures
An archival analysis was performed using data collected in the Midlife in the United States (MIDUS II) study. MIDUS II is funded through the National Institute on Aging at the University of Wisconsin Madison (P01-AG020166). In MIDUS II, Project 1, participants completed a phone interview and two self-administered questionnaires (SAQs) measuring psychological constructs, demographic variables, and mental and physical health. Additionally, subsets of participants in MIDUS II, Project 1 completed an in-person physical examination where body index measurements (e.g., BMI) were taken using a standardized method by MIDUS II staff members. The physical exam data was collected during an overnight stay at one of three General Clinical Research Centers in Madison, WI, Los Angeles, CA, or Washington, DC. The current study used data from participants who were involved in both Project 1 (completion of the phone and self-administered questionnaires) and participants who participated in the in-person physical examination.
Materials
Depressive Symptoms
Depressive symptoms were measured with the World Health Organization Composite International Diagnostic Interview–Short Form (CIDI-SF).26 The CIDI-SF interview is based on definitions and criteria as described by the third edition-revised of the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders (DSM III-R).27 Although this version of the CIDI was based on the third edition of the Diagnostic and Statistical Manual of Mental Disorders(DSM–III–R),27 the criteria for major depression episode and major depressive disorder are the same as those specified in the DSM–5.27 For the diagnosis of major depression, a period of at least two weeks of either depressed affect or anhedonia felt most of the days was required over the 12 months prior to the interview, with at least of four other associated symptoms including disrupted eating or sleeping habits, problems with concentration, or suicidal thoughts or actions. The final variable ranged from 0 to 7, where 0 represented participants diagnosed as negative for current diagnosis of major depression, and scores between one and seven represented the range of the symptoms severity. The CIDI-SF has demonstrated good test-retest reliability and clinical validity.28 In the current study, depressive symptoms were examined on a continuous scale, as depressive symptoms have been found to be related to eating behavior and weight outcomes in this population regardless of official depression diagnosis.24, 29, 30 For demographic purposes, participants were categorized dichotomously to determine a current diagnoses of major depression (Table 1). In all subsequent analyses, depressive symptoms were treated as a continuous variable.
Table 1.
Participant characteristics for overall sample. N = 815.
| Variable | Overall (N = 815) | Premenopause (N = 392) | Postmenopause (N = 423) |
|---|---|---|---|
| Age, mean (SD) | 51.1 (7.2) | 45.1 (3.7) | 56.7 (4.7) |
| Annual Income, mean (SD) | $70,535 ($54,322) | $85,015 ($53,633) | $56,055 ($54,981) |
| Race, N (%) | |||
| White | 752 (92.3) | 359 (91.6) | 393 (92.9) |
| Black/African American | 31 (3.8) | 21 (5.4) | 10 (2.4) |
| Asian American | 3 (.4) | 1 (.3) | 2 (.5) |
| Native American/Alaska Native | 7 (.9) | 1 (.3) | 6 (1.4) |
| Other/Don’t Know | 22 (2.7) | 10 (2.6) | 12 (2.9) |
| Education, N (%) | |||
| Professional Degree | 26 (3.2) | 12 (3.1) | 14 (3.3) |
| Master’s Degree | 102 (12.5) | 56 (14.3) | 46 (10.9) |
| Some Graduate School | 32 (3.9) | 17 (4.3) | 15 (3.5) |
| Bachelors | 180 (22.1) | 98 (25.0) | 82 (19.4) |
| Two-Year | 67 (8.2) | 35 (8.9) | 32 (7.6) |
| 3+ college | 33 (4.4) | 19 (4.8) | 14 (3.3) |
| 1–2 college | 148 (18.2) | 66 (16.8) | 82 (19.4) |
| High school | 189 (23.2) | 79 (20.2) | 110 (26.0) |
| GED | 10 (1.2) | 4 (1.0) | 6 (1.4) |
| Did not graduate high school | 28 (3.4) | 6 (1.6) | 22 (5.2) |
| Self-Rated Health, N (%) | |||
| Excellent (1) | 179 (22.0) | 100 (25.5) | 79 (18.7) |
| Very Good (2) | 335 (41.1) | 172 (43.9) | 163 (38.5) |
| Good (3) | 226 (27.7) | 93 (23.7) | 133 (31.4) |
| Fair (4) | 60 (7.4) | 21 (5.4) | 39 (9.2) |
| Poor | 15 (1.8) | 6 (1.5) | 9 (2.1) |
| BMI, mean (SD) | 27.4 (6.7) | 26.9 (6.0) | 28.0 (7.2)* |
| Less than 18.5 (underweight), N (%) | 11 (1.3) | 5 (1.3) | 6 (1.4) |
| 18.63 – 25 (healthy), N (%) | 331 (40.6) | 168 (42.9) | 163 (38.5) |
| 25.0 – 29.9 (overweight), N (%) | 238 (29.2) | 115 (29.3) | 123 (29.1) |
| Greater than or equal to 30 (obese), N (%) | 235 (28.8) | 104 (26.5) | 131 (31.0) |
| Stress Eating, mean (SD) | 4.2 (2.0) | 4.2 (2.0) | 4.2 (2.0) |
| High, N (%) | 327 (40.1) | 153 (39.0) | 174 (41.1) |
| Moderate, N (%) | 251 (30.9) | 130 (33.2) | 121 (28.6) |
| Low, N (%) | 237 (29.1) | 109 (27.8) | 128 (30.3) |
| Depressive Symptoms, mean (SD) | .70 (1.9) | .80 (1.9) | .70 (1.9) |
| Major Depression (No), N (%) | 699 (85.8) | 332 (84.5) | 367 (86.8) |
| Major Depression (Yes), N (%) | 116 (14.2) | 60 (15.3) | 56 (13.2) |
Self-rated health consists of scale ranging from 1 to 5 with items reversed scored such that 1 indicates “excellent” and 5 indicates “poor.”
* Indicates a statistically significant difference between pre and postmenopausal women.
The high stress eating group consisted of individuals who answered the questions about food quantity and preference with “a lot” and/or “a medium amount” (i.e., score of 6–8). The moderate stress eating group consisted of individuals who responded with “a medium amount, and/or “only a little” (i.e., score of 4–5). The low stress eating group consisted of individuals who answered “only a little” and/or “not at all” (i.e., score of 2–3). Stress eating was split into high, moderate, and low stress eating groups for descriptive analyses only. A continuous measure of stress eating was used in all additional analyses.
A current diagnosis of major depression was determined if participants indicated a score of “1” or above on the CIDI-SF. A score of “1” indicates a current diagnosis of major depression as specified in the DSM-III-R. A score of “0” indicated that a participant did not meet criteria for a current diagnosis of major depression.
Stress Eating
Stress eating was measured via a self-administered coping questionnaire where participants are asked to indicate how they “usually experience a stressful event.” Two choices include, “I eat more of my favorite foods to make myself feel better” and “I eat more than I usually do.” Responses ranged from 1 = a lot to 4 = not at all. Responses to the two items were reverse coded and summed so that higher scores indicated greater use of food in response to stress. The two questions were combined as the variable, “Use Food to Cope” and scores range from 2 (not all) to 8 (a lot). A continuous measure of stress eating was used in all analyses. For descriptive purposes, stress eating was split into three categories in Table 1 (i.e., high, moderate, low). These designations were based on previous work using this scale.24 The “high” stress eating group consisted of individuals who answered the questions about food quantity and preference with “a lot” and/or “a medium amount” (i.e., score between 6–8). The “moderate” stress eating group consisted of individuals who responded with “a medium amount, and/or “only a little” (i.e, score between 4–5). The “low” stress eating group consisted of individuals who answered “only a little” and/or “not at all” (i.e., score between 2–3). The correlation between the two “Use Food to Cope” items was.80 in the full MIDUS II analytical sample. Cronbach’s alpha for the “Use Food to Cope Scale” is .90 for the full MIDUS II sample and .91 for the current sample.
Weight
Weight in the current study was assessed using body mass index (BMI), which was measured during a physical exam using a standardized procedure. BMI was calculated by dividing body weight in kilograms by height in meters squared. Having a BMI of 18.5 to 24.9, is considered healthy. A BMI of 25 to 29.9 is considered overweight, and a BMI of 30 or higher is considered obese.2 BMI was analyzed as a continuous variable in the current study.
Menopausal Stage
Menopausal stage was calculated using participant responses to a medical history questionnaire specific to women’s health. Participant’s answered the questions, “Have you have a menstrual period in the last year?” and “Do you know if your menstrual period stopped due to menopause?” Women were classified into premenopausal group if they answered “Yes” to having a menstrual period in the last year. Women were classified as perimenopausal if they answered, “Yes, part of the year” to having a menstrual period in the last year and answered “Yes” to, “Do you know if your menstrual period stopped due to menopause?” In the current study, perimenopausal women were not included given that too few women met this criteria (N = 71). Lastly, women were classified as postmenopausal if they answered, “No, none of the year” to, “Have you have a menstrual period in the last year?” and “Yes” to, “Do you know if your menstrual period stopped due to menopause?”
Data Analyses
SPSS 23.00 was used for all data analyses. Using G*Power31 to run power calculations, we determined that for a mediation analysis with 8 predictors, a sample size of at least 759 participants was needed to predict a small effect size of .02 at an alpha of 0.05, with a power of .80
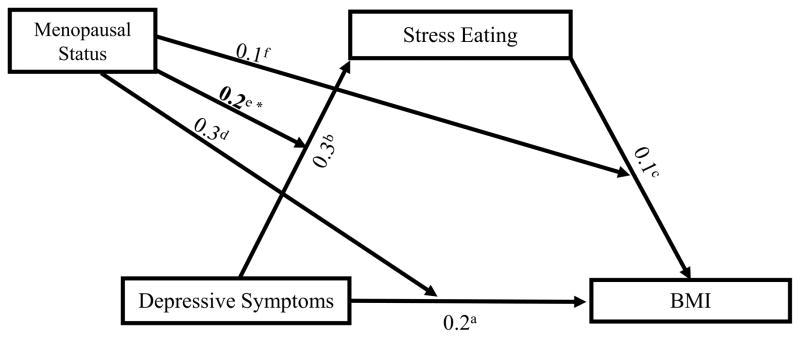
Pearson correlation coefficients were calculated to identify significant bivariate associations between weight, stress eating, depressive symptoms, and covariates. Pearson correlations were calculated for the overall sample as well as for each menopausal status group (i.e., premenopausal, postmenopausal). Independent-sample t-tests were run to examine differences in the mean values of each primary outcome variable (depressive symptoms, stress eating, BMI) by menopausal status (premenopause, postmenopause). Finally, Hayes’ SPSS PROCESS32 macro was used to test the direct association of depressive symptoms with BMI, the mediating role of stress eating in the depressive symptom-BMI association, and the moderation by menopausal status of the depressive symptom-BMI, depressive symptom-stress eating, and stress eating-BMI associations. Specifically, moderated mediation models were used to assess BMI as the outcome, testing for stress eating as an indirect pathway between depression and BMI and menopausal status as a moderator of the depressive symptom-BMI, depressive symptom-stress eating, and stress eating-BMI pathways (Figure 1). The model controlled for possible confounders including annual income, race, age, and self-reported ratings of physical health.33, 34, 35 Using the PROCESS macro, the direct association of depressive symptoms with weight was tested using ordinary least squares path analysis. The indirect effect of stress eating was tested using a non-parametric, bias-corrected bootstrapping procedure that provided an empirical approximation of the sampling distribution of the product of the estimated coefficients in the indirect paths using 5,000 resamples from the data set. To assess the moderating influences of menopausal status, the PROCESS macro automatically generated the proportion of variance in BMI and stress eating that are be uniquely attributed to the moderation of the effect of depressive symptoms and stress eating by menopausal stage (Figure 1).
Figure 1.
Results indicate p values for the direct relation between depressive symptoms and BMIa, depressive symptoms and stress eatingb, and stress eating and BMIc. P values indicating the interaction (moderation) effects between depressive symptoms and menopausal status on BMId, depressive symptoms and menopausal status on stress eatinge, and stress eating and menopausal status on BMIf are also represented.
* p < .05.
Results
Descriptive statistics of demographics, covariates and predictors are presented in Table 1. Participants were primarily white and had an average age of 51.1 (SD = 7.2). Postmenopausal women were older (M=56.7, SD=4.7) than the premenopausal group (M=45.1, SD=3.7). On average, participants had an annual income of $70,535 (SD = $54,322) and rated their physical health as 2.3 (SD = 1.0) on a five-point scale, with higher scores indicating worse self-rated health. Pearson correlations were conducted to examine bivariate associations between all main variables of interest (Table 2).
Table 2.
Pearson correlation coefficients among BMI, stress eating, depressive symptoms, menopausal status, and covariate variables in overall sample and by menopausal status. N =815.
| BMI | Stress Eating | Depressive Symptoms | Menopausal Status | |
|---|---|---|---|---|
| BMI | - | |||
| Premenopausal | - | |||
| Postmenopausal | - | |||
| Stress Eating | 0.4** | - | ||
| N | 815 | |||
| Premenopausal | 0.3** | - | ||
| N | 392 | |||
| Postmenopausal | 0.4** | - | ||
| N | 423 | |||
| Depressive Symptoms | 0.1* | 0.1** | - | |
| N | 815 | 815 | ||
| Premenopausal | 0.02 | 0.07 | - | |
| N | 392 | 392 | ||
| Postmenopausal | 0.1** | 0.2** | - | |
| N | 423 | 423 | ||
| Menopausal Status | 0.1* | 0.01 | −0.01 | - |
| N | 815 | 815 | 815 | |
| C1 Age | 0.1** | 0 | −0.1* | 0.8** |
| N | 815 | 815 | 815 | 815 |
| Premenopausal | 0.1** | 0.04 | −0.1* | - |
| N | 392 | 392 | 392 | |
| Postmenopausal | 0 | 0 | −0.1** | - |
| N | 423 | 423 | 423 | |
| C2 Self-rated Health | 0.3** | 0.1** | 0.2** | 0.1** |
| N | 815 | 815 | 815 | 815 |
| Premenopausal | 0.4** | 0.1* | 0.2** | - |
| N | 392 | 392 | 392 | |
| Postmenopausal | 0.3** | 0.2** | 0.3** | - |
| N | 423 | 423 | 423 | |
| C3 Annual Income | −0.1** | 0 | −0.1* | −0.3** |
| N | 815 | 815 | 815 | 815 |
| Premenopausal | −0.1** | 0.06 | −0.1* | - |
| N | 392 | 392 | 392 | |
| Postmenopausal | −0.1* | −0.05 | −0.1 | - |
| N | 423 | 423 | 423 | |
| C4 Race | 0 | −0.1** | 0 | 0.01 |
| N | 815 | 815 | 815 | 815 |
| Premenopausal | 0.01 | −.02** | 0.02 | - |
| N | 392 | 392 | 392 | |
| Postmenopausal | 0 | −0.08 | 0 | - |
| N | 423 | 423 | 423 |
Independent-sample t-tests were run to compare the mean differences of depressive symptoms, stress eating, and BMI in premenopausal vs. postmenopausal women. The overall sample had a mean BMI of 27.4 with women in the postmenopausal group having significantly higher BMI values (M = 28.0, SD = 7.2) compared to the premenopausal group (M = 26.9, SD = 6.0), p < .05. Both groups moderately endorsed stress eating (M = 4.2; Table 1) however this difference was not statistically significant, p = 0.9. Overall, the sample endorsed low levels of depressive symptoms (M = 0.8) with the premenopausal group endorsing more symptoms on average (M = 0.8, SD = 1.9) than the postmenopausal group (M = 0.7, SD = 1.9), although this difference was not statistically significant, p = 0.8.
The association between depressive symptoms and BMI
Moderated mediation models were run with BMI as the outcome, examining stress eating as an indirect pathway between depressive symptoms and BMI and menopausal status (pre, post) as a moderator of the depression—BMI, depression—stress eating, and stress eating—BMI pathways (see Table 3 and Figure 1). First, the direct association between depressive symptoms and BMI was investigated. While the overall model, after controlling for annual income (b = 0.0, 95% CI [0.0, 0.0]), race (b = −0.1, 95% CI [−0.4, 0.2]), age (b = 0.1, 95% CI [0.0, 0.2]), and self-reported ratings of physical health (b = 2.0, 95% CI [1.6, 2.5]) was significant, F(9, 763) = 25.4, p < .001, R2 = 0.2, depressive symptoms were not significantly associated with BMI, b = −0.4, 95% CI [−1.1, 0.3] (Table 3, Row 2, Column 7). When closely examining the overall model, it appeared that both self-rated health and age were driving the association to BMI (Table 3, Rows 7 & 10, Column 7).
Table 3.
Coefficients for moderated mediation models with BMI as outcome. N = 815.
| Predictor Variables | Outcome Variables | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| M (Stress Eating) | Y (BMI) | |||||
|
|
|
|||||
| Coeff. | SE | p | Coeff. | SE | p | |
| Figure 1 | ||||||
| Constant | 2.4 | 0.8 | < .05 | 17.9 | 2.8 | < .001 |
| X (Depressive Symptoms) | −0.1 | 0.1 | 0.3 | −0.4 | 0.4 | 0.3 |
| M (Stress Eating) | ––– | ––– | ––– | 0.6 | 0.4 | 0.1 |
| W (Menopausal Status) | −0.3 | 0.2 | 0.2 | −2.2 | 0.2 | 0.1 |
| Depressive Symptoms x Status | ––– | ––– | ––– | 0.2 | 0.2 | 0.4 |
| Stress Eating x Status | 0.2 | 0.1 | < .05 | 0.3 | 0.2 | 0.2 |
| C1 Self-Rated Health | 0.3 | 0.1 | < .001 | 2.0 | 0.2 | < .001 |
| C2 Annual Income | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.1 |
| C3 Race | 0.0 | 0.1 | 0.7 | −0.1 | 0.2 | 0.4 |
| C4 Age | 0.0 | 0.0 | 0.2 | 0.1 | 0.1 | < .05 |
| R2 = 0.1 | R2 = 0.2 | |||||
| F(7, 765) = 6.3, p < .001 | F(9, 763) = 25.4, p < .001 | |||||
Labels within the table reflect the following: X refers to the independent variable (depressive symptoms), Y refers to the dependent variable (BMI), M refers to the mediator (stress eating), W refers to the moderator (menopausal status), and Cx refer to covariates (self-rated health, annual income, race, age).
p values in bold indicate a statistically significant effect.
“Status” in the “Depressive Symptoms x Status” and “Stress Eating x Status” refers to menopausal status (W).
Stress eating as a mediator in the depressive symptom-BMI association
Bootstrapping analyses then assessed the indirect effect of stress eating on the depressive symptom-BMI association. After controlling for selected covariates of annual income (b = 0.0, CI [0.0, 0.0]), race (b = 0.0, CI [−0.1, 0.1]), age (b = 0.0, CI [−0.0, 0.1]), and self-rated health (b = 0.3, CI [0.1, 0.4]; Table 3, Rows 7–10, Column 4), stress eating was a significant mediator of the depressive symptom and BMI association, b = 0.2, 95% CI [0.06, 0.3]. Depressive symptoms predicted greater endorsement of stress eating, which, in turn, predicted higher BMI. Of the selected covariates, only self-rated health was significantly associated with stress eating. Age, annual income, and race were not independently associated with stress eating. The association between selected covariates and BMI were the same as indicated above (i.e., self-rated health and age were significantly associated with BMI).
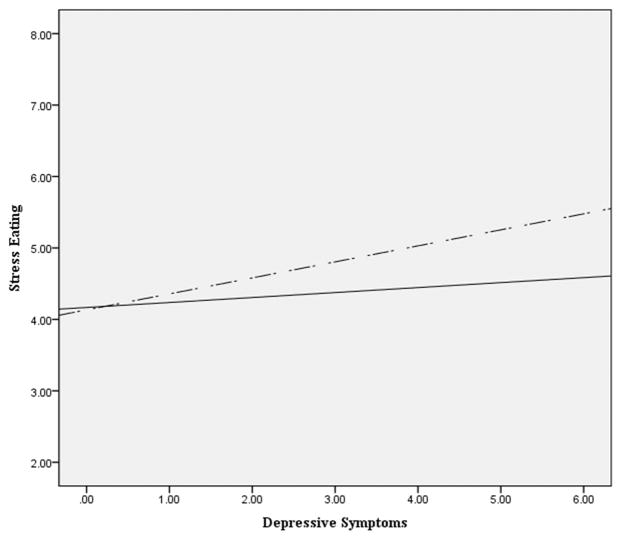
Menopausal status as a moderator of depressive symptom-BMI, depressive symptom-stress eating, and stress eating-BMI associations
Next, menopausal status was assessed as a moderator of the depressive symptom—BMI, depressive symptom—stress eating, and stress eating—BMI paths using moderated mediation. A significant moderation was present in the depressive symptom-stress eating association, b= 0.2, p < .05, indicating that menopausal status moderates the association between depressive symptoms and stress eating (Figure 2). For premenopausal women, there was no association between depressive symptoms and stress eating, b = .06, 95% CI [−0.04, 0.2]. However, for postmenopausal women, there was a significant association between depressive symptoms and stress eating, b = 0.3, 95% CI [0.1, 0.5]. Additionally, the mediation of the depressive symptoms and BMI association by stress eating was contingent on menopausal status such that the indirect pathway of stress eating exists for postmenopausal women but not for premenopausal women, b = 0.2, 95% CI [0.05, 0.4]. No significant moderating effects of menopausal status were found for the depressive-symptom—BMI, b = 0.2, 95% CI [−0.3, 0.7], and stress eating—BMI associations, b = 0.3, 95% CI [−0.1, 0.7]. Additional information regarding the association between all variables and menopausal status are located in Table 3.
Figure 2.
Covariates for moderation analysis include annual income, race, and self-reported ratings of physical health.
Solid line (\) indicates pre-menopausal status. Dashed line (
 ) indicates post-menopausal status.
) indicates post-menopausal status.
Follow-up analysis: Menopausal status as a moderator of major depression diagnosis-BMI and major depression diagnosis -stress eating associations
As menopausal status served as a significant moderator between depressive symptoms and stress eating when depressive symptoms were measured continuously, it was of interest to examine whether menopausal status also moderated the association between a diagnosis of major depression and stress eating, as well as BMI. Thus, additional PROCESS moderation analyses were conducted to assess whether a diagnosis of major depression (Table 1) was associated with stress eating and BMI in the current sample and whether this association was moderated by menopausal status. Results indicated that diagnosis of major depression did not directly predict BMI (b = −2.9, 95% CI [−6.9, 1.1]) or stress eating (b = −0.6, 95% CI [−1.8, 0.7]) in the overall sample. However, when menopausal status was included as a moderator, there was a significant interaction between diagnosis of major depression and menopausal status, b = 0.8, p <.05, indicating that engagement in stress eating was strengthened by menopausal status. Specifically, there was a significant association between major depression diagnosis and stress eating for postmenopausal women, b = 1.0, 95% CI [0.4, 1.6], not premenopausal women, b = 0.2, 95% CI [−0.3, 0.8]. Results are similar to the findings between depressive symptoms, stress eating, and BMI. Specifically, the results highlight that for postmenopausal women, stress eating is predicted by both a diagnosis of major depression, as well as increases in overall depressive symptoms.
Follow-up analysis: The association between the endorsement of stress eating and BMI among postmenopausal women
Given the significant moderated mediation by stress eating and menopausal status in the indirect association between depressive symptoms and BMI, it was of interest to further explore the association between stress eating and BMI among postmenopausal women. An ANCOVA was conducted to assess whether differences in stress eating (i.e., low, moderate, high) among postmenopausal women significantly predicted BMI outcomes when controlling for relevant covariates (i.e., age, self-rated health, annual income, race). Findings indicated a significant difference between stress eating condition and BMI after controlling for covariates, F(2, 394) = 23.0, p < .001 (Table 4). Specifically, pairwise comparisons using the Bonferroni correction revealed that participants who endorsed low levels of stress eating had lower BMI outcomes than those with high levels of stress eating, p < .001, 95% CI [−7.4, −3.5]. Additionally, participants with moderate levels of stress eating had lower BMI compared to participants with high levels of stress eating, p <.05, 95% CI [−4.5, −0.4), and participants with low levels of stress eating had significantly lower BMI outcomes than participants who endorsed moderate levels of stress eating, p < .01, 95% CI [−5.0, −1.1] (Table 5). Results indicate that both moderate and high levels of stress eating predicted higher BMI outcomes in comparison to low levels of stress eating in postmenopausal women (3 and 5.5 point differences in BMI, respectively).
Table 4.
ANCOVA results and descriptive statistics for BMI by stress eating condition and self-rated health in 423 postmenopausal women.
| BMI | |||||
|---|---|---|---|---|---|
|
|
|||||
| Observed Mean | Adjusted Mean | SD | n | ||
| Low Stress Eating | 25.2 | varies | 5.5 | 174 | |
| Moderate Stress Eating | 28.3 | varies | 7.0 | 121 | |
| High Stress Eating | 31.4 | varies | 8.0 | 128 | |
|
| |||||
| Source | SS | df | MS | F | |
|
| |||||
| Stress Eating | 1981.1 | 2 | 990.6 | 23.0* | |
| Self-Rated Health | 1033.7 | 1 | 1033.7 | 24.0* | |
| Age | 72.2 | 1 | 72.2 | 1.7 | |
| Annual Income | 13.9 | 1 | 13.9 | 0.3 | |
| Race | 0.1 | 1 | 0.1 | .003 | |
| Error | 17739.6 | 419 | 42.3 | - | |
R2 = 0.2
*p < .001
Table 5.
Bonferroni comparison of mean differences in BMI by stress eating condition in 423 postmenopausal women.
| Comparisons | Mean Weight Difference (lbs) | Std. Error | 95% CI | |
|---|---|---|---|---|
|
| ||||
| Lower Bound | Upper Bound | |||
| Low Stress Eating (n = 174) vs. High Stress Eating (n = 128) | −5.5** | 0.8 | −7.4 | −3.5 |
| Moderate Stress Eating (n =121) vs. High Stress Eating (n = 128) | −2.4* | 0.9 | −4.5 | −0.4 |
| Low Stress Eating (n = 174) vs. Moderate Stress Eating (n =121) | −3.0** | 0.8 | −5.0 | −1.1 |
Mean difference is significant at the .05 level.
*p < 0.05, **p < .001.
Discussion
The aims of the current study were to: 1) examine the association between depressive symptoms and weight in midlife women; 2) to assess stress eating as a mechanism to explain the association between depressive symptoms and higher weight outcomes in midlife women; and 3) to examine the impact of menopausal status on the depressive symptoms—weight, depressive symptoms—stress eating, and stress eating—weight associations. While depressive symptoms did not directly predict BMI in the current sample, depressive symptoms were indirectly associated with BMI through stress eating. Depressive symptoms predicted greater endorsement of stress eating, which, in turn, predicted higher BMI. Additionally, menopausal stage moderated the association between depressive symptoms and stress eating whereby depressive symptoms were associated with stress eating in postmenopausal, but not premenopausal women. Importantly, given the cross-sectional study design, the observed significant pathways may be also be bidirectional and we cannot assume causal linkages. Furthermore, stress eating was measured as a tendency to use food to cope with stress, rather than as an objective assessment of food consumption. Consequently, the results reflect coping tendencies rather than actual observed behavior.
Results from the current study add to the growing literature on the role of psychosocial factors linking depressive symptoms to weight outcomes in midlife women. The current study also provides novel findings regarding the association between depressive symptoms and the tendency to use food to cope with stress in this population. Consistent with current findings, previous studies have found associations between stress eating, depression, and weight outcomes in women across the adult lifespan. For example, stress eating served as a mediator in the relation between depression and obesity in a sample of low-income, minority, adult women aged 18–59 (M= 43.7).18 Similarly, depressive symptoms were positively associated with emotional (i.e., stress) eating within a broad age range of adult women (25–64, M = 46.5).36 The current study adds to existing literature, as it is the first to examine stress eating as a mediator between depressive symptoms and weight specifically in midlife women while also considering the influence of menopausal status in this association.
The finding that the association between depressive symptoms and stress eating differed by menopausal status is consistent with prior research demonstrating that depression is differentially expressed in women depending on menopausal status.37, 38 For example, postmenopausal women are less likely to experience decreased appetite associated with depression compared to premenopausal women.38 Specifically, lower estrogen levels are associated with an increased stress response, which can influence eating in response to emotion and stress.21 As women in postmenopause have lower estrogen levels compared to premenopausal women, they may be more likely to experience heightened sympathetic arousal when experiencing emotional fluctuations, stress, and menopausal symptoms. As a result, postmenopausal women are possibly more at risk for stress eating compared to premenopausal women, who have higher estrogen levels. These differences introduce potential mechanisms to explain current findings. First, previous work identifying that appetite differences when experiencing depressive symptoms can help to explain why postmenopausal women in the current study reported more of tendency to use food to cope when experiencing depressive symptoms. The experience of continued appetite when experiencing depressive symptoms could lead postmenopausal women to engage in stress eating while premenopausal women may not have the same tendencies given their greater likelihood to experience decreases in appetite. This reasoning is consistent with previous work which has demonstrated that a potential mechanism through which depressive symptoms lead to emotional eating is through differences in appetite and an inability distinguish hunger from other emotional states.36, 39 Importantly, the association between depressive symptoms and stress-eating may also be bidirectional, such that greater depressive symptoms are reported in association with stress eating. 36, 39
Secondly, postmenopausal women are shown to experience more sympathetic arousal when experiencing depression compared to premenopausal women, which can also have implications for stress eating.38 Specifically, as postmenopausal women are more likely to experience a heightened stress response,40 and heightened stress reactivity is associated with weight gain and increases in stress eating in midlife women,41, 42 it is possible that postmenopausal women endorsing depressive symptoms are more sympathetically reactive to stressors which can lead to increases in stress eating. While both premenopausal and postmenopausal women experience mood fluctuation and stressors, postmenopausal women have lower levels of estrogen compared to premenopausal women. Lower estrogen levels can exacerbate stress responses and influence maladaptive coping responses.23, 25 Also, the combination of a heightened stress response and negative mood can exacerbate stress eating in midlife women.41 Therefore, it is possible that women who are postmenopausal with depressive symptoms experience more sympathetic arousal when stressed, and thus, are more likely to overeat and consume energy dense foods, leading to later weight gain. Alternatively, given that premenopausal women are not as sympathetically reactive to stress when experiencing depressive symptoms, it is possible that depressive symptoms do not exacerbate the stress response in this subset of women. This may help premenopausal women choose coping mechanisms alternative to stress eating. Of additional importance, type of stress can also affect stress eating responses. As chronic stress is often associated with stress eating, it is also possible that stress is different for postmenopausal women compared to premenopausal women. Additional work needs to explore this connection further.
Conclusions and Implications
Results of the current study highlight the dynamic interplay of factors that are associated with depressive symptoms and weight in midlife women. The current study identified a tendency to use food to cope in association with depressive symptoms as one pathway that can help to explain why women in midlife have poor weight outcomes. Interestingly, the study also demonstrates that menopausal status likely plays a role in the pathway from depressive symptoms to weight, with depressive symptoms linked to stress eating in a particular subset of women in midlife (i.e., postmenopausal women). Specifically, the current study found evidence for a significant difference in weight outcomes in postmenopausal women depending on their level of stress eating. In addition to being statistically significant, the differences in BMI appear to have clinical significance with a 5.5-point difference in BMI for high tendencies to stress eat compared to low tendencies. Specifically, high stress eaters are more likely to meet overweight and obese criteria compared to low stress eaters, given that a 5.5-point difference in BMI moves an individual across BMI categories (e.g., healthy to overweight, overweight to obese). Given that previous work has demonstrated that postmenopausal women are more likely to experience poor weight outcomes compared to premenopausal women,8 the current study aids in identifying a potential risk factor. Additional work needs to further disentangle the association between depressive symptoms, menopausal status, stress eating, and weight in this population.
As women in midlife are subject to a variety of stressors, compounded by many physiological and lifestyle changes in this period, the current study has several clinical implications. First, the current study provides a potential intervention target to prevent weight gain in this population. As women in midlife are at an increased risk for the development of poor weight outcomes and obesity due to multiple factors (i.e., hormonal changes, changes in fat distribution, mood changes, lifestyle factors, socioeconomic status),1, 7, 8, 43 it is often challenging to identify specific pathways in which to effectively intervene. The current results suggest that depressive symptoms may serve to exacerbate poor weight outcomes through certain coping strategies and emotional responses (i.e., stress eating). Therefore, beyond the treatment of depressive symptoms alone, the targeting of specific coping strategies, stress management techniques, and maladaptive eating behaviors may serve to prevent and decrease poor weight outcomes in midlife women.9, 41 Secondly, we identified a particular subset of midlife women who are at risk of stress eating when experiencing depressive symptoms. As postmenopausal women presenting with depressive symptoms may be more likely to stress eat, and potentially gain weight, it is of clinical value to identify and target specific subsets of women when identifying who is at risk for poor weight outcomes.
However, there are several limitations of the current study that limit the generalizability and breadth of the current findings. First, the study used cross-sectional data. Therefore, causality or directionality cannot be determined. Regarding measures, we assessed for endorsement of stress eating using two questions rather than a comprehensive scale. The small number of items decreases variability of the measure and could potentially bias results. The stress eating measure also inquired about general tendency to stress eat and did not assess for actual endorsement of stress eating. Therefore, results of the current study are limited and are subject to recall bias as well as potential over or underestimation of stress eating behavior. The current study was also not able to measure dietary habits, current stress levels, or hormonal factors including estrogen, so it is unclear how stress eating may be affecting food consumption in terms of types of food consumed, amount of food consumed, current stress levels, or hormonal fluctuation may be affecting this behavior. Regarding our depressive symptoms measure, our sample consisted of midlife women with relatively low levels of depressive symptoms and stress eating. However, even in a sample reporting low levels of these variables, we found significant association between depressive symptoms and stress eating. In terms of our sample, we had more postmenopausal women (n=423) than premenopausal women (n=392). Thus, this may have influenced results, as there was more power to detect associations in the postmenopausal group. In addition, due to the small available sample of perimenopausal women (n = 71), we were not able to assess the impact of perimenopausal status on the association between depressive symptoms, stress eating, and BMI. While we did find a significant difference between premenopausal and postmenopausal in regards to depressive symptoms, stress eating, and subsequent weight outcomes, we were not able to determine how perimenopausal status may influence this association. This is an important limitation as perimenopausal women experience significant hormonal fluctuations, which may influence depressive symptoms, stress reactivity, and thus, stress eating, appetite, and BMI outcomes. Consequently, future work needs to include perimenopausal women when investigating of the role of menopausal status on eating behavior and weight outcomes. Lastly, We also had a lack of racial diversity in the current sample. As a majority of the women were white, generalizability of results to midlife women of different races and ethnicities is limited.
Despite limitations, the current study has several strengths. This includes a large sample size, an objective measure of BMI, and a well-validated measure of depressive symptoms. The study is also one of the first to conceptualize stress eating as a mediator in the relationship between depressive symptoms and weight outcomes specifically in midlife women. It is also the first to identify the role of menopausal status in the association between depressive symptoms and stress eating. Therefore, the current study can inform future research regarding how stress eating and menopausal status can affect mental and physical health of midlife women. More research, specifically longitudinal research, is needed to further explore these associations and to identify the causal associations among depressive symptoms, stress eating, and weight outcomes in this population.
Acknowledgments
Funding/support: The MIDUS I study (Midlife in the U.S.) was supported by the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development. The MIDUS II research was supported by a grant from the National Institute on Aging (P01-AG020166) to conduct a longitudinal follow-up of the MIDUS I investigation.
D.S. contributed to the study concept and D.S. and N.D. contributed to study design. Testing and data collection was performed by MIDUS II study staff who were supported by the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development. D.S. analyzed the data and drafted the manuscript, which was critically reviewed by N.D. All authors approve the final version of the manuscript for submission.
Footnotes
Financial disclosure/conflicts of interest: Natalie D. Dautovich serves as a sleep consultant for Merck Sharp & Dohme Corp.
References
- 1.Ogden C, Carroll M, Fryar C, Flegal K. Prevalence of obesity among adults and youth: United States. NCHS data brief. 2015;219:1–8. [PubMed] [Google Scholar]
- 2.World Health Organization. Obesity: Preventing and managing the global epidemic: Report of a WHO consultation. WHO Technical Report Series. 2000;894:1–253. [PubMed] [Google Scholar]
- 3.Su M-C, Lin H-R, Chu N-F, Huang C-H, Tsao L. Weight loss experiences of obese perimenopausal women with metabolic syndrome. J Clin Nurs. 2015;24:1849–1859. doi: 10.1111/jocn.12806. [DOI] [PubMed] [Google Scholar]
- 4.Cooke P, Naaz A. Role of estrogens in adipocyte development and function. ExpBiol Med. 2004;229:1127–1135. doi: 10.1177/153537020422901107. [DOI] [PubMed] [Google Scholar]
- 5.Geiselman P, Smith S. Estrogen’s role in the regulation of appetite and body fat. In: Kohlstadt I, editor. Scientific Evidence for Musculoskeletal, Bariatric, and Sports Nutrition. Boca Raton, London/New York: CRC Press, an imprint of Taylor and Francis Group; 2006. pp. 231–251. [Google Scholar]
- 6.Lovejoy J, Champagne C, de Longe L, Xie H, Smith S. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes. 2008;32:949–958. doi: 10.1038/ijo.2008.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Safi Z, Polotsky A. Obesity and menopause. Best Pract Res Clin Obstet Gynaecol. 2015;29(4):548–553. doi: 10.1016/j.bpobgyn.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Jasienska G, Ziomkiewicz A, Górkiewicz M, Pająk A. Body mass, depressive symptoms and menopausal status: an examination of the “Jolly Fat” hypothesis. Womens Health Iss. 2005;15(3):145–151. doi: 10.1016/j.whi.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Simon G, Ludman E, Linde J, et al. Association between obesity and depression in middle-aged women. Gen Hosp Psychiatry. 2008;30(1):32–39. doi: 10.1016/j.genhosppsych.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bromberger J, Matthews K, Schott L, et al. Depressive symptoms during the menopausal transition: The Study of Women’s Health Across the Nation (SWAN) J Affect Disord. 2007;103(1):267–272. doi: 10.1016/j.jad.2007.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen L, Soares C, Vitonis A, Otto M, Harlow B. Risk for new onset of depression during the menopausal transition: The Harvard study of moods and cycles. Arch Gen Psychiatry. 2006;63(4):385–390. doi: 10.1001/archpsyc.63.4.385. [DOI] [PubMed] [Google Scholar]
- 12.Soares C. Mood disorders in midlife women: understanding the critical window and its clinical implications. Menopause. 2014;21(2):198–206. doi: 10.1097/GME.0000000000000193. [DOI] [PubMed] [Google Scholar]
- 13.Blaine B. Does depression cause obesity? A meta-analysis of longitudinal studies of depression and weight control. J Health Psychol. 2008;13(8):1190–1197. doi: 10.1177/1359105308095977. [DOI] [PubMed] [Google Scholar]
- 14.Luppino F, de Wit L, Bouvy P, et al. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 15.Druss B, Rosenheck R, Sledge W. Health and disability costs of depressive illness in a major US corporation. Am J Psychiatry. 2000;157:1274–1278. doi: 10.1176/appi.ajp.157.8.1274. [DOI] [PubMed] [Google Scholar]
- 16.Konttinen H, Manniesto S, Sarlio-Lahteenkorva S, Silventoinen K, Haukkala A. Emotional eating, depressive symptoms and self-reported food consumption: A population-based study. Appetite. 2010;54:473–479. doi: 10.1016/j.appet.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 17.van Strien T, Konttinen H, Homberg J, Engels R, Winkens L. Emotional eating as a mediator between depression and weight gain. Appetite. 2016;100:216–224. doi: 10.1016/j.appet.2016.02.034. [DOI] [PubMed] [Google Scholar]
- 18.Yu J, Fei K, Fox A, Negron R, Horowitz C. Stress eating and sleep disturbance as mediators in the relationship between depression and obesity in low-income, minority women. Obes Res Clin Pract. 2015 doi: 10.1016/j.orcp.2015.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schiffman SS, Graham BG, Sattely-Miller EA, Peterson-Dancy M. Elevated and sustained desire for sweet taste in African-Americans: A potential factor in the development of obesity. Nutrition. 2000;16:886–893. doi: 10.1016/s0899-9007(00)00403-2. [DOI] [PubMed] [Google Scholar]
- 20.Oliver G, Wardle J, Gibson L. Stress and food choice: A laboratory study. Psychosom Med. 2000;62:853–865. doi: 10.1097/00006842-200011000-00016. [DOI] [PubMed] [Google Scholar]
- 21.Ballinger S. Stress as a factor in lowered estrogen levels in the early postmenopause. Ann N Y AcadSci. 1990;592(1):95–113. doi: 10.1111/j.1749-6632.1990.tb30318.x. [DOI] [PubMed] [Google Scholar]
- 22.Crawford G, Khedkar A, Flaws J, Sorkin J, Gallicchio L. Depressive symptoms and self-reported fast-food intake in midlife women. Prev Med. 2011;52(3):254–257. doi: 10.1016/j.ypmed.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klump KL, Culbert KM, Edler C, Keel PK. Ovarian hormones and binge eating: Exploring associations in community samples. Psychol Med. 2008;38:1749–1757. doi: 10.1017/S0033291708002997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsenkova V, Boylan J, Ryff C. Stress eating and health. Findings from MIDUS, a national study of US adults. Appetite. 2013;69:151–155. doi: 10.1016/j.appet.2013.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Charmandari E, Tsigos C, Chrousos G. Endocrinology of the stress response 1. Annu Re Physiol. 2005;67:259–84. doi: 10.1146/annurev.physiol.67.040403.120816. [DOI] [PubMed] [Google Scholar]
- 26.Kessler R, Andrews G, Mroczek D, Ustun B, Wittchen H. The World Health Organization composite international diagnostic interview short-form (CIDI-SF) Int J Methods Psychiatr Res. 1998;7(4):171–185. [Google Scholar]
- 27.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Arlington, VA: American Psychiatric Publishing; 2015. [Google Scholar]
- 28.Blazer D, Kessler R, McGonagle K, Swartz M. The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry. 1994;151:979–986. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- 29.Akbaraly TN, et al. Dietary pattern and depressive symptoms in middle age. Br J Psychiatry. 2009;195:408–413. doi: 10.1192/bjp.bp.108.058925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jeffery RW, et al. Reported food choices in older women in relation to body mass index and depressive symptoms. Appetite. 2009;52:238–240. doi: 10.1016/j.appet.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Faul F, Erdfelder E, Buchner A, Albert-Georg L. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 32.Hayes A. An Introduction to Mediation, Moderation, and Conditional Process Analysis. New York: The Guilford Press; 2013. [Google Scholar]
- 33.Campbell L, Samaras K. What is the evidence, reasons for and impact of weight gain during menopause? Med J Aust. 2000;173:S100–S101. doi: 10.5694/j.1326-5377.2000.tb139435.x. [DOI] [PubMed] [Google Scholar]
- 34.Lahmann P, Lissner L, Gullberg B, Berglund G. Sociodemographic factors associated with long-term weight gain, current body fatness and central adiposity in Swedish women. Int J ObesRelatMetabDisord. 2000;24:685–694. doi: 10.1038/sj.ijo.0801219. [DOI] [PubMed] [Google Scholar]
- 35.Wing R, Matthews K, Kuller L, Meilahn E, Plantinga P. Waist to hip ratio in middle-aged women. Associations with behavioral and psychosocial factors and with changes in cardiovascular risk factors. ArteriosclerThromb. 1991;11:1250–1257. doi: 10.1161/01.atv.11.5.1250. [DOI] [PubMed] [Google Scholar]
- 36.Konttinen H, Silventoinen K, Sarlio-Lähteenkorva S, Männistö S, Haukkala A. Emotional eating and physical activity self-efficacy as pathways in the association between depressive symptoms and adiposity indicators. Am J ClinNutr. 2010;92(5):1031–1039. doi: 10.3945/ajcn.2010.29732. [DOI] [PubMed] [Google Scholar]
- 37.Bromberger J, Schott L, Kravitz H, et al. Longitudinal change in reproductive hormones and depressive symptoms across the menopausal transition: Results from the Study of Women’s Health Across the Nation (SWAN) Arch Gen Psychiatry. 2010;67(6):598–607. doi: 10.1001/archgenpsychiatry.2010.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kornstein S, Young E, Harvey A, et al. The influence of menopausal status and postmenopausal use of hormone therapy on presentation of major depression in women. Menopause. 2010;17(4):828–839. doi: 10.1097/gme.0b013e3181d770a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ouwens M, van Strien T, van Leeuwe J. Possible pathways between depression, emotional and external eating. A structural equation model. Appetite. 2009;53:245–248. doi: 10.1016/j.appet.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 40.Owens J, Stoney C, Matthews K. Menopausal status influences ambulatory blood pressure levels and blood pressure changes during mental stress. Circulation. 1997;88(6):2794–2802. doi: 10.1161/01.cir.88.6.2794. [DOI] [PubMed] [Google Scholar]
- 41.Epel E, Lapidus R, McEwen B, Brownell K. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology. 2001;26(1):37–49. doi: 10.1016/s0306-4530(00)00035-4. [DOI] [PubMed] [Google Scholar]
- 42.Vicennati V, Pasqui F, Cavazza C, Pagotto U, Pasquali R. Stress-related Development of Obesity and Cortisol in Women. Obesity. 2009;17(9):1678–1683. doi: 10.1038/oby.2009.76. [DOI] [PubMed] [Google Scholar]
- 43.Flegal K, Carroll M, Ogden C, Curtin L. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]