Abstract
Anxiety typically arises early in childhood and decreases during school age. However, little is known about the earlier developmental course of anxiety in preschool, especially in at risk children, posing a clinically important problem. Given that anxiety in youth has a chronic course for some and also predicts later development of other mental health problems, it is important to identify factors early in development that may predict chronic anxiety symptoms. At-risk children (oversampled for depression) and caregivers completed 6 assessment waves beginning at preschool age (between 3–5.11 years of age) up through 6.5 years later. Growth mixture models revealed 4 distinct trajectories: 2 stable groups (high and moderate) and 2 decreasing groups (high and low). Important to note, the high stable anxiety group had greater baseline depression and social adversity/risk, higher average maternal depression over time, and poorer average social functioning over time compared to the high decreasing group. The high decreasing group also had greater externalizing/attention deficit hyperactivity disorder scores than the low decreasing group. Children with anxiety in early childhood who also experience high depression, social adversity/risk, maternal depression, and poor social functioning may be at risk for chronic symptoms over time.
Anxiety is one of the most common forms of childhood psychopathology (Costello, Mustillo, Erkanli, Keeler, & Angold, 2003; Ford, Goodman, & Meltzer, 2003; Kroes et al., 2001) and is associated with significant impairment in both academic and social domains (e.g., Last, Hansen, & Franco, 1997; Shaffer et al., 1996). Although studies suggest that anxiety often emerges in preschool and is relatively stable (Bufferd, Dougherty, Carlson, & Klein, 2011; Bufferd, Dougherty, Carlson, Rose, & Klein, 2012), most work to date has focused on older children. Little is known about the earlier developmental course of anxiety beginning in preschool, when clinical symptoms may initially arise. Given the relatively high rate of anxiety in preschool children, studies with older children may miss early critical markers of risk. In addition, most studies have investigated symptoms in the normative range in community children (e.g., Hale, Raaijmakers, Muris, van Hoof, & Meeus, 2008a; Keenan, Feng, Hipwell, & Klostermann, 2009). Although important, such community-based studies may not have captured adequate numbers of young children with early expressions of clinical internalizing symptoms to be able to detect a potentially unique at risk trajectory. Therefore, the goals of the current study were to (a) identify trajectories of anxiety symptoms from preschool through school age, using an at-risk sample oversampled for depression, and (b) identify factors early in development that may be associated with chronic anxiety symptoms.
Anxiety symptoms in healthy school-age children and adolescents typically decline across development (Cooper-Vince, Chan, Pincus, & Comer, 2014; Feng, Shaw, & Silk, 2008; Hale, Raaijmakers, Muris, van Hoof, & Meeus, 2008b; Keenan et al., 2009; Van Oort, Greaves-Lord, Verhulst, Ormel, & Huizink, 2009). For example, latent growth curve analyses in a community sample have suggested that anxiety decreases from 6–15 years of age, with a more rapid decline prior to age 9 (Cooper-Vince et al., 2014). Similarly, another group found that separation anxiety in a community sample decreased linearly from 6–12 years of age, whereas social anxiety increased from 6 to 8, plateaued from 8 to 10, then decreased from 10 to 12 years (Keenan et al., 2009). In another community sample, youth ages 12–16 showed that panic, school anxiety, and separation anxiety decreased over time, whereas social anxiety showed no change over that period. Interesting to note, this study also found that symptoms of generalized anxiety disorder decreased for boys but increased in girls (Hale et al., 2008). Despite some unique patterns in specific disorders, most anxiety symptoms appear to decline through school age.
Although anxiety appears to follow a normative decrease on average, there is substantial variability in individual trajectories, especially in younger children (i.e., preschool and early school age). Several studies have found evidence for low, moderate, and high stable classes in community samples followed from 6–12 years of age (e.g., Côté,Tremblay, Nagin, Zoccolillo, & Vitaro, 2002; Duschesne, Vitaro, Larose, & Treblay, 2010). Similarly, others have found stable low and stable high classes in low-income, at-risk boys (ages 2–10) and in a community sample (ages 6–12; Duchesne, Larose, Vitaro, & Tremblay, 2010; Feng et al., 2008). Another study of a community sample of young children (ages 4–11) found a stable four-class (low, medium, high, very high) solution for social anxiety and a stable three-class (low, medium, high) solution for separation anxiety (Broeren, Muris, Diamantopoulou, & Baker, 2013).
Others have identified increasing or decreasing classes in addition to stable classes. For example, one study of community girls found three classes—low decreasing, high decreasing, and high increasing (Zerwas, Von Holle, Watson, Gottfredson, & Bulik, 2014). Another communitysample found low increasing and high decreasing classes(Duchesne et al., 2010; Feng et al., 2008; Zerwas et al., 2014), and results from a sample of young, at-risk boys revealed low, low increasing, high decreasing, and high increasing trajectories (Feng et al., 2008). In a communitybased study of disorder-specific symptoms, two classes emerged for generalized anxiety and specific fear symptoms; one class appeared stable over time, whereas the second evidenced an increasing-decreasing trajectory where anxiety increased until ages 7–8, then decreased (Broeren et al., 2013). Overall, clear developmental patterns in preschool-age children have yet to emerge, and most studies have relied on community samples, suggesting that additional study and replication attempts are necessary.
For some children, early onset anxiety becomes chronic, beginning in childhood and persisting into adolescence and adulthood (Cartwright-Hatton, McNicol, & Doubleday, 2006; Kessler et al., 2005; Last, Perrin, Hersen, & Kazdin, 1996; Ollendick & King, 1994); however, little is known about early predictors of chronic anxiety symptoms. This is a critical gap in the literature, as these data could identify when early childhood anxiety is likely to be time-limited versus chronic and could inform which children to target for earlier and potentially more effective preventive interventions. Drawing from available literature, there is evidence that both child factors and maternal/family factors influence anxiety trajectories. Previous studies have linked several child factors with worse trajectories (e.g., low increasing, high declining, or high classes), including comorbid internalizing problems, inattentiveness and hyperactivity (for those with low-warmth mothers), and lack of prosocial behavior, each of which has been associated with worse trajectories (Broeren et al., 2013; Duchesne et al., 2010; Feng et al., 2008). For example, teachers have been shown to rate children in high-anxiety groups as more inattentive with fewer prosocial behaviors in the classroom (Duchesne et al., 2010), and other internalizing symptoms have also been associated with higher anxiety trajectories (Broeren et al., 2013). To build on these findings, the current study included measures of depression, attention deficit hyperactivity disorder (ADHD) symptoms, and peer relationships.
Maternal and family factors have also been linked with worse trajectories of anxiety symptoms. Maternal depression and controlling parenting behavior have been associated with high increasing trajectories of anxiety in at risk, low-income boys ages 2–10 (Feng et al., 2008). Other known factors associated with child anxiety (although not necessarily developmental trajectories) include maternal anxiety (Beidel & Turner, 1997) and a family history of affective disorders (Weissman et al., 2005). For example, first-degree relatives of anxious children have a higher risk for anxiety disorders compared to relatives of children with ADHD or healthy controls (Last, Hersen, Kazdin, Orvaschel, & Perrin, 1991). Sociofamily adversity has also been associated greater likelihood of belonging to a high anxiety trajectory group (Duchesne et al., 2010). Finally, stressful life events also appear to be an important correlate of anxiety disorders in children (e.g., Muris, 2006). For example, based on maternal reports of stressful life events in school-age and older children, anxious children were more likely than nonanxious children to have experienced significant stressors (Rapee & Szollos, 2002). A longitudinal study suggested that stressful life events at 15 months predicted later mixed anxiety/depression at 5 years (Shaw et al., 1998). Thus, the current study included measures of maternal depression and anxiety, social adversity, an estimate of first-degree relatives with mental illness, and stressful life events.
Differences in latent class trajectories of anxiety have also been linked with negative outcomes. For example, one study found that children with a high increasing or high decreasing trajectory of anxiety symptoms from age 5 years through sixth grade were at an increased risk for disordered eating at age 15 (Zerwas et al., 2014). Another study showed that boys in high increasing/decreasing trajectory groups were 5 times more likely to be diagnosed with an anxiety or depressive disorder at age 10 or 11, compared to a low anxiety symptoms group (Feng et al., 2008). However, the effect of early anxiety trajectories on global outcomes (e.g., school and social functioning) I school age remains understudied.
THE CURRENT STUDY
The current study was designed to identify trajectories of anxiety and factors that may distinguish children at risk for chronic anxiety symptoms. Although the current sample was oversampled for depression, the high rates of comorbidity between anxiety and depression (e.g., Seligman & Ollendick, 1998) suggest that some depressed children in this sample are also likely to have high rates of anxiety. In addition, although anxiety often precedes depression (e.g., Burke, Loeber, Lahey, & Rathouz, 2005; Garber, 2006; Rice, van den Bree, & Thapar, 2004; Wittchen, Kessler, Pfister, & Lieb, 2000), some studies suggest that depression predicts anxiety (Lavigne, Hopkins, Gouze, & Bryant, 2015) or that anxiety and depression precede each other (e.g., Moffitt et al., 2007). Thus, the current sample may be vulnerable to the development or worsening of anxiety symptoms over time and represents an important at-risk group in which to examine early trajectories of anxiety symptoms. The goals of the current study were to identify trajectories of anxiety symptoms from preschool through school age and to characterize these trajectories behaviorally in order to provide indicators of children who may be at risk.
METHOD
Participants
Participants were children and their primary caregivers enrolled in the Preschool Depression Study, an ongoing longitudinal study of preschool children and their families conducted at the Washington University School of Medicine (Luby, Si, Belden, Tandon, & Spitznagel, 2009). Children ages 3 to 5.11 were recruited from May 2003 to March 2005 to participate in the study. Recruitment sites included pediatrician’s offices, daycare centers, and preschools in the St. Louis metropolitan area. Approximately 60,000 Preschool Feelings Checklists (PFCs; Luby, Heffelfinger, Koenig-McNaught, Brown, & Spitznagel, 2004) were distributed to recruitment sites, and 1,474 PFCs were returned to the Early Emotional Development Program. Caregivers who endorsed no items on the PFC, two or more internalizing items, and/or two or more externalizing items (n = 899) were contacted for additional screening. Exclusion criteria were chronic medical illnesses, neurological problems, pervasive developmental disorders, or language and/or cognitive delays, as well as those outside of the study age range.
Children were enrolled in the study at preschool age (Time 1; between ages 3–5.11). Five additional assessments occurred at approximately 1-year follow-up intervals, for a total of six assessment waves. Waves occurred after 1 year (Time 2; M = 5.50 years, SD = .80), 2 years (Time 3; M = 6.50 years, SD = .80), 4.5 years (Time 4; M = 9.0 years, SD = .90), 5.5 years (Time 5; M = 10.20 years, SD = .90), and 6.5 years (Time 6; M = 11.10, SD = .90). Of note, due to the grant funding cycle, a larger gap occurred between the third and fourth possible assessment. Because the planned analyses would include a quadratic term, only subjects with data available for at least three of the six assessment waves were included in the analyses. Of the original 306 subjects in the study, 34 completed fewer than three assessments and were excluded from analyses. Therefore, 272 participants were included in the current study. Demographic characteristics are presented in Of these, 149 completed all six waves, 70 completed five waves, 30 completed four waves, and 23 completed three waves. All study procedures were approved by the Washington University School of Medicine Institutional Review Board prior to data collection.
Measures
Macarthur Health and Behavior Questionnaire– Parent (HBQ-P; Armstrong & Goldstein, 2003)
Similar to the approach used by other studies of the development of child anxiety symptoms over time (e.g., Broeren et al., 2013; Cooper-Vince et al., 2014; Feng et al., 2008; Zerwas et al., 2014), the current study used a parent report of anxiety. The HBQ is a parent-report form comprising items covering four domains: Mental Health, Physical Health, Social Functioning, and School Functioning. Each domain of the HBQ comprises several scales and subscales. The measure overall has shown high test–retest reliability and cross-informant agreement, as well as discriminant validity between internalizing and externalizing groups (for additional details on scales and subscales, see Armstrong & Goldstein, 2003; Essex et al., 2002).
Anxiety
In the current study, the HBQ Overanxious (12 items), Separation Anxiety (10 items), and Social Inhibition (three items) subscales were used to calculate a composite anxiety score. Items are rated on a scale from 0 (never or not true) to 2 (often or very true). Each subscale score is scored as a mean of the total items in that subscale. Overanxious subscale items assess for worry and associated symptoms of generalized anxiety. Sample items include “Worries about things in the future” and “Worries about past behavior.” Separation Anxiety subscale items assess for the child’s fear and distress when separated from loved ones. Sample items include “Worries that something bad will happen to people he/she is close to” and “Avoids school to stay home.” To include coverage of social-anxiety-related symptoms, the Social Inhibition subscale was also added to the composite. Social inhibition has been linked to social anxiety symptoms and a diagnosis of social anxiety disorder (Biederman et al., 2001; Buss et al., 2013; Hirshfeld-Becker et al., 2007). Important to note, the Social Inhibition items measure both child shyness and fear of strangers. Sample items include “Shy with other children” and “Is afraid of strangers.” An overall anxiety score was created by taking the mean of the Overanxious, Separation Anxiety, and Social Inhibition subscale mean scores. Thus, scores range from 0 to 2, with higher scores indicating greater anxiety.
The HBQ Overanxious, Separation Anxiety, and Social Inhibition subscales have been used in many previous studies examining anxiety in young children and have shown strong psychometric properties (e.g., Buss et al., 2013; Goldsmith & Lemery, 2000; Lemery-Chalfant et al., 2007; Volbrecht & Goldsmith, 2010). For example, the Social Inhibition subscale correlated positively with shyness (Kiel, Buss, & Molitor, 2015), and the Overanxious and Separation Anxiety subscales demonstrated good convergent validity with other theoretically related constructs, including behavioral inhibition (Volbrecht & Goldsmith, 2010) and measures of temperament (shyness and fearfulness) and social fearfulness (Goldsmith & Lemery, 2000). Anxiety composite scores in the current study ranged from .79 to .90 across the six assessment waves. Cronbach’s alphas for the Anxiety composite ranged from good to excellent (.79–.90) across the six assessment waves.
Depression
The HBQ Depression subscale (six items) assesses for core features of depression, including unhappy, sad or depressed mood, feelings of worthlessness, sleeping more than most children, and low energy. Each item is rate from 0 (never/not true) to 2 (often or very true). The score is the mean of the six items. Cronbach’s alphas ranged from .63 to .87 across the six assessment waves.
Externalizing and ADHD symptoms
The HBQ Externalizing Symptoms scale is the mean of several subscales: Oppositional Defiant (nine items; e.g., has temper tantrums, angry and resentful), Conduct Problems (12 items; e.g., steals, lies or cheats), Overt Hostility (four items; e.g., gets in many fights, does things that annoy others), and Relational Aggression (six items; e.g., tried to get others to dislike a peer, when mad at peer, keeps that peer from being in the play group). Each item is rated from 0 (never/ not true) to 2 (often or very true) with higher scores indicating greater symptoms. Cronbach’s alpha ranged from .92 to .94 across the six assessment waves.
The ADHD Symptoms scale is the mean of the Inattention and Impulsivity subscales. The Inattention scale (six items) assesses for concentration and distractibility. The Impulsivity scale (nine items) assesses for impulse control problems, including interrupting, difficulty waiting for turn in games, and fidgety/restless behavior. Items are rated from 0 (never/not true) to 2 (often or very true). Higher scores suggest more symptoms. Cronbach’s alpha ranged from .92 to .93 across the assessment waves.
Peer relationships
The HBQ Peer Acceptance/ Rejection (eight items) and Bullied by Peers (three items) subscales measures child friendship quality, extent to which child is liked by peers, and frequency with which the child is teased or picked on. Items are rated from 1 (not at all like) to 4 (very much like), with higher scores indicating better peer relations. The mean of the two subscales is used for the Global Peer Relations scale. Cronbach’s alpha ranged from.87 to .93.
Functional impairment
The HBQ Functional Impairment scale (seven items) assesses the amount of impairment children exhibit across several domains of functioning, such as school, home/family, and social. Items are rated from 0 (none) to 2 (a lot) and averaged for a total score. Cronbach’s alpha ranged from .72 to 88 across the assessment waves in the current study.
School Engagement
The HBQ School Engagement (eight items) subscale assesses a child’s intrinsic motivation and positive attitudes about school. Items are rated from 0 (not at all) to 4 (quite a bit) and averaged. Higher scores indicate greater school engagement. Cronbach’s alpha ranged from .90 to .98 across assessment waves.
The Preschool-Age Psychiatric Assessment and Child and Adolescent Psychiatric Assessment
The Preschool-Age Psychiatric Assessment (PAPA; Egger, Ascher, & Angold, 2003) and Child and Adolescent Psychiatric Assessment (CAPA; Angold & Costello, 2000) consist of a series of developmentally appropriate prompts covering the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; American Psychiatric Association, 1994) criteria for disorders of childhood. These disorders include major depressive disorder (MDD), ADHD, oppositional defiant disorder, conduct disorder, generalized anxiety disorder, posttraumatic stress disorder, separation anxiety disorder, mania, dysthymia, obsessive compulsive disorder, panic disorder, agoraphobia, social anxiety disorder, specific phobia, enuresis, encopresis, nightmare disorder, sleep terror, and sleepwalking. In addition to diagnosis, the PAPA/CAPA also assesses 18 stressful life events (e.g., birth of sibling, change in daycare/ school) and 21 traumatic life events (e.g., death of a loved one). The total number of stressful and traumatic life events was summed for an overall score in the current study.
The PAPA was administered in person to caregivers when children were between 3 years of age and 7 years 11 months. Duration of interviews ranged from 3.5 to 4.5 hr. Both the caregiver and the child completed the CAPA when children were 8.0 years of age or older. Raters were trained to reliability and blind to the child’s previous diagnostic status. To further increase objectivity, diagnosis was derived through a computer-based Diagnostic and Statistical Manual of Mental Disorders algorithm. All interviews were audiotaped, and methods to maintain reliability and prevent drift, including ongoing calibration of interviews by master raters for 20% of each interviewer’s cases, were implemented in consultation with an experienced clinician (JL) at each study wave. This is the standard method for maintaining reliability of this measure as suggested by the authors.
Wechsler Abbreviated Scale of Intelligence
The Wechsler Abbreviated Scale of Intelligence (Wechsler, 1999) is a measure of cognitive functioning for individuals 6–89 years of age and includes four subtests: Vocabulary, Similarities, Block Design, and Matrix Reasoning. The subtests yield Verbal, Performance, and Full-Scale IQ scores. IQ scores are scaled in standard units (M = 100, SD = 15). Concurrent validity of the Wechsler Abbreviated Scale of Intelligence has been demonstrated by significant positive correlations with theoretically comparable estimates from the Kaufman Brief Intelligence Test (all rs > .84; Hays, Reas, & Shaw, 2002) and the Wide Range Intelligence Test (Canivez, Konold, Collins, & Wilson, 2009).
Maternal Psychopathology and Family History of Affective Disorders
The Family Interview for Genetic Studies (Maxwell, 1992) was used to assess for maternal depression, maternal anxiety, and family history of psychiatric disorders (e.g., MDD, bipolar disorder, anxiety, or suicide) in first- and second-degree relatives other than the mother at T1. The Family Interview for Genetic Studies is a structured measure designed to assess diagnostic information about relatives. A senior psychiatrist (JL), blind to the child’s diagnostic status, reviewed questions about the diagnostic status of family members. Maternal depression, maternal anxiety, and family history of affective disorder were each coded dichotomously (present or absent). Mothers also completed the Beck Depression Inventory–II (BDI-II; Beck, Steer, & Brown, 1996) at subsequent time points. The BDI-II is a 21-item self-report measure of depression symptom severity in adults. Items are rated from 0 to 3 and summed for a total score, with higher scores indicating greater depression. Cronbach’s alphas in the current study ranged from .80 to .94.
Income-to-Needs Ratio
The income-to-needs ratio was computed as the total family income at baseline divided by the federal poverty level, based on family size, at the time of data collection.
Social Adversity Risk
Seven social risk factors (described next) were assessed at baseline (e.g., prior to age 5). Cumulative social adversity/ risk scores (occurring prior to age 5) were created by summing the dichotomous indicators (present = 1; absent = 0) of each of the seven social risk factors listed next (Slopen, Koenen, & Kubzansky, 2014). The cumulative social adversity/risk score could range from 0 to 7, with greater scores indicating greater risk. Adversity risk variables included the following: 1. Living in a single-caregiver household, 2. Maternal psychopathology (excluding eating disorders), 3. Parental arrest, 4. Foster care placement, 5. Physical abuse, 6. Sexual abuse, and 7. Caregiver report of being unable to meet the family’s financial needs. A previous confirmatory factor analysis supported a single factor model with acceptable model fit (Whalen et al., 2016). Cronbach’s alpha in the current study was .36.
Data Analysis
Growth Mixture Modeling
Subjects were assessed at six annual waves with an approximate 2.5-year gap between the third and fourth waves. We first estimated the growth mixture models using scores from the PAPA/CAPA worries, separation anxiety, and social anxiety sections at each assessment wave. However, results were not informative and placed mostnparticipants in a single trajectory class. Given that these findings were inconsistent with previous literature, we next analyzed anxiety data from the HBQ, which have several advantages over the PAPA/CAPA. First, parents consistently completed the HBQ across assessment waves, whereas the PAPA was administered to caregivers when children were between the ages of 3 years and 8 years 11 months, and both the caregiver and the child completed the CAPA when children were 9.0 years of age or older. Therefore, there was greater consistency of HBQ measurement across development relative to the PAPA/CAPA. Second, the HBQ anxiety scales had a greater number of items, potentially providing both more coverage of the construct and greater variability in possible scores. Given that we obtained the HBQ at all six study waves and had the biggest data capture (yielding largest overall sample sizes), the HBQ was deemed the best measure to use to estimate longitudinal trajectories in the data set.
Quadratic growth mixture models with anxiety scores obtained at each assessment wave as the dependent variables were used to determine categorical latent class variables for grouping participants with similar anxiety trajectories. Because subject age varied at each assessment wave, anxiety score trajectories were analyzed by age instead of wave.
To determine the model that best fit the data, several quadratic growth mixture models with varying numbers of classes (one to six classes) were compared. The model with the best fit according to a combination of the Bayesian Information Criterion (BIC) and the Lo-Mendell-Rubin adjusted likelihood ratio test (LRT) was selected (Jung & Wickrama, 2008; Nylund, Asparouhov, & Muthén, 2007). Once the best model was determined, it was manipulated by removing any nonsignificant quadratic, linear, or intercept terms for each of the latent classes. The resulting model determined the latent classes to be used for further analyses.
Class Characteristics
Class differences across demographics and baseline child, baseline maternal/family factors, and outcomes at last assessment were examined using multivariate and univariate analyses of variance or chi-square tests as appropriate. Multivariate analyses were used in instances were sets of dependent variables were closely related conceptually, including externalizing symptoms (the HBQ Externalizing and ADHD subscales), peer relations (theHBQPeerAcceptance/Rejection and Bulled subscales), and outcomes at last assessment (HBQ–School Engagement, Global Peer Relations, and Overall Functional Impairment).
RESULTS
Descriptive Statistics
Means and standard deviations for study variables are presented in Table 2. The income-to-needs ratio was calculated at Wave 1 (M = 2.11, SD = 1.16). The social adversity/risk score was calculated at Wave 3 (M = .73, SD = .90). Overall, 86% of the sample had a relative with an affective disorder (excluding maternal anxiety or depression). In addition, 40% of the sample had a maternal depression diagnosis and 14% a maternal anxiety diagnosis.
TABLE 2.
Means, Standard Deviations, and Score Ranges for Study Varables Across Six Waves
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 5 | Wave 6 | Range | |
|---|---|---|---|---|---|---|---|
| HBQ–Anxicty | 0 59 (.29) | 0.55 (.27) | 0.54 (.28) | 0.46 (.29) | 0.41 (.29) | 0.37 (.29) | 0–2 |
| HBQ–Depresstion | 0.31 (.31) | 0.23 (.26) | 0.23 (.26) | 0.23 (.27) | 0.23 (.26) | 0.22 (.27) | 0–2 |
| HBQ–Extemalizing | 0.46 (33) | 0.37 (.28) | 0.37 (.29) | 0.39 (.30) | 0.24 (.24) | 0.21 (.24) | 0–2 |
| HBQ–ADHD | 0.84 (.44) | 0.74 (.44) | 0.71 (.45) | 0.62 (.44) | 0.56 (.47) | 0.55 (.45) | 0–2 |
| HBQ–Peer Acceptance | 141 (.53) | 3.53 (.52) | 3.53 (.59) | 3.47 (.64) | 3.44 (.59) | 3.38 (.67) | 1–4 |
| HBQ–Bullied | 1.50 (.65) | 1.47 (.63) | 1.48 (.67) | 1.52 (.64) | 1.39 (.53) | 1.48 (.70) | 1–4 |
| HBQ–Functional Impairment | 0.28 (.30) | 0.023 (.29) | 0.24 (.31) | 0.27 (.31) | 0.26 (.32) | 0.26 (.33) | 0–2 |
| HBQ–School Engagement | 3.28(1.0) | 3.43 (.63) | 3.54 (.56) | 3.40 (.63) | 3.36 (.61) | 3.36 (.63) | 0–4 |
| Cumulative Stressful Events | 4.944 (.4.80) | 7.64 (14.43) | 8.34 (6.23) | 10.68 (15.97) | 11.78(15.68) | 12.91 (16.43) | 0–226 |
| BDI-II | — | 7.20 (7.24) | 6.85 (7.08) | 6.56 (7.70) | 7.76 (8.92) | 7.61 (8.63) | 0–46 |
Note: Beck Depression Inventory–II (BDI-II) data were not collected at Wave 1. HBQ = Health and Behavior Questionnaire;ADHD = attention deficit hyperactivity disorder.
Growth Mixture Models
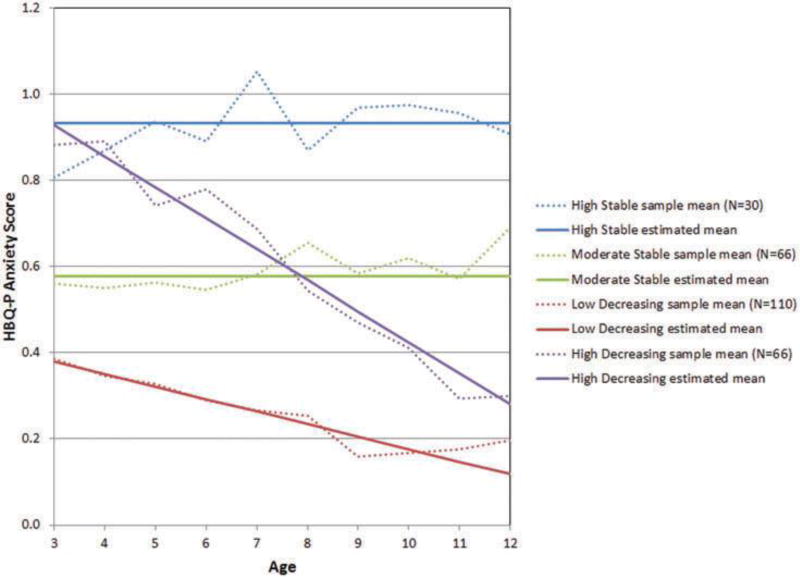
Fit statistics for the quadratic growth mixture models with latent class variables with one, two, three, four, five, and six classes were compared (upper panel of Table 2). Although the five-class and six-class models had the lowest BICs, they did not fit significantly better than the models with one fewer class according to the Lo-Mendell-Rubin adjusted LRT. The four class model had a lower BIC than the three-class model and trended toward a significant improvement over the three-class model according to the Lo-Mendell-Rubin adjusted LRT (p = .0887), so the four-class model was chosen. (See the appendix for additional information on the three-class model). Nonsignificant quadratic, linear, and intercept terms were removed from the model, resulting in a model with two latent classes with only intercept components (Classes 1 and 2) and two latent classes with both intercept and linear components (Classes 3 and 4). None of the classes were characterized by a quadratic trajectory. The classes with only intercept components remained stable over time, whereas the classes with intercept and linear components showed a linear decrease in anxiety over time. As such, each class can be characterized by an initial level of anxiety (low, moderate, high) and by a rate of change (stable or decreasing). Class 1 is characterized as high stable (N = 30),Class 2 asmoderate stable (N = 66),Class 3 as low decreasing (N = 110), and Class 4 as high decreasing (N = 66). The final model is detailed in the lower panel of Table 3, and a graph of the trajectories is shown in Figure 1.
TABLE 3.
Fit Statistics of Potential Quadratic Growth Mixture Models for Health and Behavior Questionnaire–Anxiety andClass Estimates for Final Four-Class Solution
| Latent Class No. | Bayesian information Criterion | Lo-Mendell Rubin Adjusted Likelihood Ratio Test p |
Class Sample Sizes |
|---|---|---|---|
| 1 | 713.2 | — | 272 |
| 2 | 278.0 | < .0001 | 137, 135 |
| 3 | 125.4 | .0004 | 106, 135, 31 |
| 4 | 92.0 | .0887 | 43, 88, 28, 113 |
| 5 | 70.2 | .2398 | 55, 22, 46, 88, 61 |
| 6 | 43.5 | .2398 | 4, 22, 44, 55, 61, 86 |
|
| |||
| Estimate | SE | Estinmate/SE | |
|
| |||
| Class 1: Intercept | 0.932 | 0.043 | 21.646*** |
| Class 2: Intercept | 0.578 | 0.030 | 19.159*** |
| Class 3: Intercept | 0.379 | 0.024 | 15.807*** |
| Class 3: Slope | −0.029 | 0.004 | −8.032*** |
| Class 4: Intercept | 0.928 | 0.061 | 15.311*** |
| Class 4: Slope | −0.072 | 0.008 | −9.335*** |
P <.001.
Figure 1.
HBQ Anxiety scores at T1 differed across groups, with the high stable and high decreasing groups reporting the greatest anxiety. The two high groups did not differ from each other. All significant pairwise group comparisons are p < .001. Group means are presented in Table 3.
Anxiety Diagnoses by Group Membership
To further investigate the validity of the classes, we examined group differences in percentage of anxiety diagnoses (generalized anxiety disorder, separation anxiety disorder, or social anxiety disorder) across time. We examined group differences in (a) anxiety disorder prevalence during preschool (3–5 years of age), (b) the onset of new cases of anxiety disorders at a given age, and (c) anxiety disorder prevalence at the last assessment (Time 6). All post hoc pairwise tests were Bonferroni corrected. Results are presented in Table 5. At preschool age, the high stable group had the greatest percentage of children with an anxiety diagnosis, followed by the high decreasing, moderate stable, and low decreasing groups. There was a significant difference in disorder prevalence across groups. The high stable group had more children with an anxiety diagnosis than the high decreasing, moderate stable, or low decreasing group; the high decreasing group also had more children with a diagnosis than the low decreasing group. Finally, the moderate stable group had more children with an anxiety diagnosis than the low decreasing group.
TABLE 5.
Percentage of Anxiety Diagnoses at Preschool, New Anxiety Disorder Onset by Age. and Anxiety Diagnoses at Last Assessment
| Test Statistics | High Stable | High Decreasing | Moderate Stable | Law Decreasing | |
|---|---|---|---|---|---|
| Anxiety Diagnosis at Preschool | χ2(3)= 41.68*** | 70.0 (21/30)MS LD HD | 54.5 (36/66)HS LD | 31.8 (21 66)HS LD | 14.7 (16/109)HS MS HD |
| Anxiety Onset—Age 3 | χ2(3) = 7.94* | 28.6 (2/7) | 40.0 (6/15) | 9.5 (2/21) | 8.3 (3/36) |
| Anxiety Onset—Age 4 | χ2(3) = 24.13*** | 50.0(10/20)LD | 43.9 (18/41)LD | 27.1 (13/48)LD | 7.1 (6/85)HS MS HD |
| Anxiety Onset—Age 5 | χ2(3) = 14.36** | 34.6 (9/26)MS LD HD | 18.6(11/59)HS | 9.4 (6/64)HS | 6.8 (7/103)HS |
| Anxiety Onset—Age 6 | χ2(3) = 2.55 | 8.7 (2/23) | 10.6 (5/47) | 10.0 (4/40) | 3.1 (2/64) |
| Anxiety Onset—Age 7 | χ2(3) = 4.52 | 22.2 (2/9) | 3.8 (1/26) | 4.2 (1/24) | 2.6 (1/39) |
| Anxiety Onset—Age 8 | χ2(1) =0.00 | 11.1(1/9) | 0.0 (0/24) | 10.7 (3/28) | 0.0 (0/47) |
| Anxiety Onset—Age 9 | χ2(3) = 3.04 | 8.7 (2/23) | 22 (1/46) | 11.l (5/45) | 5.3 (4/76) |
| Anxiety Onset—Age 10 | χ2(3) = 4.32 | 4.3 (1/23) | 4.0 (2/50) | 14.3 (7/49) | 6.2 (5/8l) |
| Anxiety Onset—Age 11 | χ2(1) = 0.14 | 0.0 (0/19) | 0.0 (0/36) | 3.6 (1/28) | 2.1 (1/47) |
| Anxiety Onset—Age 12 | χ2(l) = 0.13 | 0.0 (0/6) | 11.8 (2/17) | 0.0 (0/9) | 7.7 (1/13) |
| Anxiety Diagnosis at Last Assessment | χ2(3) = 31.35*** | 53.3 (16/30)MS LD HD | 27.3 (18/66)HS LD | 18.2 (12/66)HS LD | 3.6 (4/110)HS MS HD |
Note: Percentages indicate number of new anxiety diagnoses at each assessment point The numerator indicates the number of new cases: the denominator is the number of total participants assessed at that time point (including those with and without a diagnosis). Palis of letters indicate significant Bonferroni corrected pairwise t tests (significant p < .00831).
p< .05.
p< .01
p< .001.
Groups also differed in rates of new onset of anxiety diagnoses at 3, 4, and 5 years of age but not ages 6 through 11. Results in Table 5 indicate the number of any first anxiety diagnosis at each assessment wave, relative to the total number of participants assessed at that assessment wave. Participants were counted as a “new” anxiety diagnosis only once, at the time of first diagnosis. As can be seen in the table, at age 3, two of the seven (28.6%) participants in the high stable group reported a new anxiety diagnosis. There was a significant group difference at age 3 years, but corrected post hoc comparisons failed to reach significance. At age 4, 10 of the 20 participants in the high stable group reported a new anxiety diagnosis. This was significantly more than the low decreasing group. In addition, the high decreasing and moderate stable groups had more new cases than the low decreasing group. At age 5, the high stable group had more new anxiety diagnoses than the other three groups.
Groups also differed in anxiety disorder diagnosis prevalence at the time of last assessment. The high stable group had the greatest percentage of children with an anxiety diagnosis compared to all other groups. The high decreasing and moderate stable groups had a greater percentage than the low decreasing group.
Demographic Differences by Group
Demographic differences across groups were first examined. There were no differences by group in child age, proportion of male and female participants, or child IQ. Test statistics and group means are presented in Table 4.
TABLE 4.
Test Statistics, Means, and Standard Deviations for Child and Maternal/Family Factors, Outcomes, and Average Maternal and Psychosocial Factors Over Development by Latent Class Group Membership
| Test Statistic | High Stable | High Decreasing | Moderate Stable | Low Decreasing | ||
|---|---|---|---|---|---|---|
| Demographics | Child Age | F(3, 268) = 1.62 | 4.61 (.73) | 4.61 (.79) | 4.38 (.80) | 4.39 (.79) |
| IQ | F(3, 216)= 1.26 | 100.19 (13.70) | 105.84 (13.85) | 106.67(16.53) | 103.51 (14.59) | |
| Male (%) | χ2(3) = 33.8 | 46.7 | 57.6 | 43.9 | 55.5 | |
| T1 Child Factors | T1 HBQ–Anxiety | F(3, 251) = 3.75*** | .92 (,25)MS .LD | .86 (.24)MS LD | .57 (.18)HD LD | .39(.20)HS MS HD |
| T1 HBQ–Depression | F(3, 253) =21.18*** | 0.60 (.35)MS LD HD | 0.40 (.33)HS LD | 0.29 (.26)HS LD | 0.17(.23)HS MS HD | |
| T1 HBQ–Externalizing | F(3, 248) = 4.68** | 0.50 (.31) | 0.57 (.37)LD | 0.46 (.33) | 0.38 (.29)HD | |
| T1 HBQ–ADHD | F(3, 250) = 3.69* | 0.98 (.32) | 0.94 (.45)LD | 0.80 (.46) | 0.75 (.43)HD | |
| T1 HBQ–Peer Acceptance | F(3, 248) = 3.03* | 3.25 (.59)LD | 3.47 (.45) | 3.40 (.59) | 3.57(.51)HS | |
| T1 HBQ–Bullied | F(3, 250) = 1.32 | 1.63 (.75) | 1.57 (.66) | 1.52 (.66) | 1.41 (.59) | |
| T1 Maternal/Family Factors | Maternal depression (%) | χ2(3)= 9.38* | 53.3% | 40.0%LD | 50.0% | 30.0%HD |
| Social adversity/risk | F(3, 259) = 5.75*** | 1.14 (1.01)LD HD | 0.52 (.67)HS MS | 0.97 (1.00)LD HD | 0.60 (.85)HS MS | |
| Maternal anxiety | χ2(3)=3.23 | 20.0% | 13.9% | 18.2% | 10.0% | |
| Incoine-to-needs ratio | F(3, 268) = 0.98 | 1.88 (1.17) | 2.23 (1.10) | 1.96 (1.35) | 2.13 (1.12) | |
| Stressful Life Events | F(3, 263) = 1.76 | 5.17 (3.36) | 5.14 (3.95) | 521 (3.59) | 4.13 (3.48) | |
| Relative Diagnosis (%) | χ2(3)=7.12 | 83.3 | 95.5 | 93.9 | 84.6 | |
| Developmental Factors | Mean Maternal Depression | F(3, 268) = 9.65*** | 11.33 (7.90)LD HD | 7.66 (5.81)HS | 8.73 (7.64)LD | 5.21 (4.78)HS MS |
| Mean HBQ–Peer Acceptance | F(3, 268)= 11.95*** | 3.09 (57)LD HD | 3.56 (.36)HS MS | 3.34 (.52)LD HD | 3.57 (.41)HS MS | |
| Mean HBQ–Bullied | F(3, 268) = 8.45*** | 1.77 (.43)LD HD | I.42(.37)HS | 1.59 (.58)LD | 1.36 (.40)HS MS | |
| Cumulative stressful life events | F(3, 212) = 2.38 | 14.24 (7.22) | 12.18 (7.55) | 13.80 (9.35) | 10.48 (8.00) | |
| Outcomes | Final HBQ–School Engagement | F(3, 265) = 12.96*** | 2.86 (.66)MS LD HD | 3.47 (.48)HS | 3.23 (.71)HS LD | 3.54 (.52)HS MS |
| Final HBQ–Peer Relations | F(3, 268) = 9.50*** | 3.07 (.72)LD HD | 3.64 (.45)HS MS | 3.30 (.69)LD HD | 3.57 (.56)HS MS | |
| Final HBQ–Functional Impairment | F(3, 268) = 7.45*** | 0.44 (.31)LD HD | 0.22 (.25)HS | 0.34 (.44)LD | 0.18 (.24)HS MS |
Note: Pairs of tellers indicate significant Bonferroni corrected pairwise significant (p < .0083).
p < .05.
p < .01.
p < .001
Associations Between Baseline Child Factors and Group Membership
Group differences in baseline child factors were examined. Test statistics, Bonferroni-adjusted post hoc pairwise t tests, and group means are presented in Table 4. First, groups differed in HBQ–Depression. The high stable group had the greatest depression; the low decreasing group had lower depression than the other three groups. Second, groups differed in externalizing symptoms, Wilks’s Λ, F(6, 490) = 2.96, p = .007. The effects for both HBQ–Externalizing and HBQ–ADHD were significant. The high decreasing group reported greater HBQ–Externalizing and HBQ–ADHD scores than the low decreasing Group. Third, the multivariate effect for peer relationships (HBQ–Peer Acceptance/Rejection and HBQ– Bullied) was not significant, Wilks’s Λ, F(6, 494) = 2.18, p = .03, although the univariate effect for peer acceptance/ rejection was significant.
Associations Between Baseline Maternal and Family Factors and Group Membership
Group differences were next examined across maternal depression, social adversity/risk, maternal anxiety, income to needs, stressful life events, and first-degree relatives with mental illness. Groups differed in proportion of maternal MDD diagnosis. The high decreasing group had more maternal MDD cases than the low decreasing group. Groups also differed in terms of social adversity/risk. The high stable group reported greater social adversity/risk than the high decreasing and low decreasing groups, and the high decreasing group also had greater risk than the moderate stable group; in turn the moderate stable group had greater risk than the low decreasing group. Groups did not differ in proportion of maternal anxiety diagnosis, income-to-needs ratio, stressful life events, or prevalence of a first-degree relative with mental illness.
Factors That Distinguish Chronic From Decreasing Anxiety Symptom Trajectories
As previously described (see Figure 1), of particular interest were a pair of high groups (high stable and high decreasing). Given that one group goes on to experience a decrease in anxiety over time whereas the other displays chronicity, we were interested in further examining variables that may explain why some children experience improvement in anxiety over time whereas others experience chronic anxiety over time. Drawing on previous literature, we examined associations between average levels of (a) maternal depression (BDI-II) over time, (b) the quality of social relationships (HBQ–Peer Acceptance/Rejection and HBQ–Bullied) over time, and (c) cumulative stressful life events over time. Mean scores for the six assessment waves were calculated for maternal depression and social relationships and entered as dependent variables.
Groups differed on mean maternal depression over time. The high stable group had greater mean maternal depression over time than the high decreasing group and the low decreasing group. Of interest, the moderate stable group also reported greater mean maternal depression than the low decreasing group. Groups also differed in the quality of social relationships over time,Wilks’s Λ, F(6, 534) = 6.11, p < .001,with significant effects for both HBQ–Peer Acceptance/Rejection, and HBQ– Bullied. The high stable group had lower average peer acceptance over time compared to the decreasing groups (high decreasing and low decreasing). Of interest, the moderate stable group also reported lower peer acceptance than the decreasing groups (high decreasing and low decreasing). The high stable group also reported higher average bullying than both decreasing groups, and the moderate stable group reported more bullying than the low decreasing groups. Groups did not differ on cumulative stressful life events.
Differences in Outcomes by Group Membership
Groups differed on all three outcomes, Wilks’s Λ, F(9, 640.22) = 5.55, p < .001, including HBQ–School Engagement, HBQ–Global Peer Relations, and HBQ– Functional Impairment. First, the high stable had lower HBQ–School Engagement scores at last assessment thanthe other three groups; the moderate stable group also had lower engagement than the high decreasing group. Second, the high stable and moderate stable groups had poorer peer relations at the last assessment than both decreasing groups. Finally, the high stable and moderate stable groups had greater functional impairment at the last assessment than both decreasing groups.
DISCUSSION
Identifying Latent Classes of Anxiety Symptoms From Preschool Through School Age
Results from the current study identified four trajectories of anxiety symptoms from preschool through school age, including two stable groups (high and moderate) and two decreasing groups (high and low). These findings were further supported by corresponding rates of anxiety disorder diagnoses, with the high stable group reporting the greatest proportion of anxiety disorder diagnoses at both preschooland the last assessment. The high decreasing and low decreasing classes are consistent with other studies using parent-report data showing a developmentally normative decrease in anxiety symptoms for some (e.g., Cooper-Vince et al., 2014; Feng et al., 2008; Hale et al., 2008b; Zerwas et al., 2014) and the high stable and moderate stable classes are consistent with the stable, ordered (high, moderate, low) classes revealed by others (Broeren et al., 2013; Duchesne et al., 2010; Feng et al., 2008). Important to note, although many children followed the low decreasing trajectory (N = 110), a substantial portion followed a course characterized by persistent anxiety (moderate stable, N = 66; high stable, N = 30), highlighting the need to identify early indicators of those at risk.
It is of note that measurement method influenced the class solution results. The initial analysis using interview data from the PAPA/CAPA yielded a single-class solution, which contrasts with the four-class solution derived from the parent-report HBQ. The four-class solution for anxiety symptoms in youth is more consistent with existing literature that has also used self-report data (e.g., Duchesne et al., 2010; Feng et al., 2008; Hale et al., 2008) than a single-class solution. We were unable to locate any other studies comparing latent class models of youth internalizing psychopathology using interview versus self-report data. Additional work comparing class solutions across instruments administered in the same sample will be beneficial in further determining the impact of method of measurement and response patterns on models of psychopathology. Until then, models derived from one measurement method in one study should not be compared to models derived from another study using other measurement methods (e.g., self report vs. interview).
Factors That Distinguish High Stable from High Decreasing Anxiety Symptom Trajectories
Children with high stable anxiety in this sample had greater baseline depression and social adversity/risk, greater maternal depression over time, and poorer social relationships over time compared to children with high decreasing anxiety. Others have also linked preschool depression with high chronic anxiety (Broeren et al., 2013), suggesting that children with comorbid depression symptoms may be at particularly high risk for chronic anxiety symptoms.Alternatively, it may be that anxiety symptoms are a marker for more global negative affect, which functions as risk for later psychopathology that is expressed as a function of other environmental factors. As such, children with baseline levels of high negative affect may continue to experience affective symptoms in an environment with high levels of social adversity/risk, maternal depression, and problems with peers. In contrast, initially at-risk children may see improvement of affective symptoms over time in the context of lower social adversity/risk, maternal depression, and peer relationships.
The association between greater social adversity/risk and high stable anxiety is consistent with one other study linking sociofamily adversity with a high anxiety trajectory (Duchesne et al., 2010). Conceptually, results are also in line with Barlow’s Triple Vulnerability Model of anxiety (Barlow, 2002), which highlights the critical role of early experiences that contribute to perceptions of uncontrollability and unpredictability in the development of anxiety. Social adversity/risk likely increases unpredictability and perceptions of a lack of control in young children, thereby increasing risk for anxiety symptoms. In addition, results further highlight the critical role of environmental factors in the developmental course of chronic anxiety in young children. Life experiences and environmental context appear to be key in determining if children’s high anxiety decreases in developmentally normative way or persists over time. As such, intervening on environmental factors may have a powerful impact on decreasing the likelihood of a child developing chronic symptoms of anxiety through school age.
Children with chronic high anxiety symptoms had mothers with greater average depression scores compared to children with high decreasing anxiety. Maternal depression is hypothesized to increased affective symptoms in children through multiple mechanisms, including genetics, impaired neuroregulation (e.g., impaired HPA axis function), modeling of negative maternal cognition, affect, and behavior, and stressful life events (Goodman & Gotlib, 1999). These same processes likely contribute to not only the etiology of child anxiety but also its maintenance across development. Increasing maternal involvement in treatment for childhood symptoms may be beneficial for improving child outcomes.
Finally, poor social functioning distinguished the high stable anxiety group from the high decreasing anxiety group. Children with lower average peer acceptance and higher average rates of being bullied over time were more likely to experience persistent anxiety compared to the decreasing groups. These results are in line with others linking children’s social adjustment problems with anxiety (e.g., Fox, Henderson, Marshall, Nichols, & Ghera, 2005; Olson & Rosenblum, 1998) and greater likelihood of belonging to increasing anxiety trajectories (Duchesne et al., 2010). Young children with elevated anxiety may be initially reluctant to approach social situations and avoid others, interfering with normative social development. In turn, this may decrease peer acceptance and increase bullying behaviors, further contributing to chronic anxiety. Thus, anxious children may be locked in a cycle of social avoidance, anxious apprehension, and social rejection. To date, these are untested hypotheses and the direction of the effects is unclear (i.e., does poor social functioning lead to anxiety or does anxiety lead to poor social functioning). However, current findings underscore the importance of social experiences (acceptance/rejection) in the perpetuation of anxiety in childhood and suggest future research in this area is warranted.
Factors That Distinguish High Anxiety Trajectories From Other Trajectories
Externalizing and ADHD symptoms distinguished the high decreasing from low decreasing groups, consistent with others who have linked inattention symptoms with high stable anxiety trajectories (Duchesne et al., 2010). Some hypothesize that associations between ADHD and anxiety are due to the academic difficulty experienced by children with ADHD symptoms, which are thought to begin a downward spiral. Poor academic performance is thought to become an ongoing stressor, increasing anxiety, which in turn decreases attentional resources and results in continued (or worsening) academic difficulty (Duchesne et al., 2010). It will be important for future work to examine reciprocal associations between these variables over time to better understand potential points of intervention in the association between anxiety, attention, and ADHD symptoms.
Outcomes Associated With Anxiety Symptom Trajectories
Anxiety trajectories beginning in preschool were associate with later outcomes during school age. Stable anxiety groups (high and moderate) had lower school engagement, poorer global peer relations, and greater functional impairment compared to the low decreasing anxiety group at the time of last assessment. Important to note, children with high but decreasing anxiety (high decreasing) had better school and social outcomes than children in the high stable and evenmoderate stable groups. In fact, the high decreasing and low decreasing groups were not significantly different at the last assessment wave. This suggests that early interventions targeted at decreasing anxiety have the potential to make a significant impact on outcomes, shifting children with high anxiety onto a pathway resulting in greater school engagement, peer relations, and functional impairment. Given the social nature of the risk factors just described, school-based-interventions may be particularly helpful. At the individual level, social skills training for anxious at-risk children may facilitate development of appropriate prosocial behaviors and improve peer relationships.
Limitations of the Current Study
Findings from this study should be interpreted in light of several limitations. First, the sample was originally recruited for a study examining preschool depression and was therefore oversampled for depressive symptoms. Therefore, findings may be specific to this risk group and may not generalize to community samples or other at risk groups. Second, as indicated in the Methods section, growth mixture models were also estimated using the PAPA/CAPA; however, the model suggested that most participants were characterized by a single class. Given that this contradicts previous studies (e.g., Duchesne et al., 2010; Feng et al., 2008; Zerwas et al., 2014), we used the HBQ as an alternate measure of anxiety that had more power, given the larger sample size. As we were not able to replicate findings across these two measures, additional study in this area is needed. Third, some risk factors previously associated with anxiety in children were not examined in this study, such as parenting behaviors characterized by autonomy granting and warmth (McLeod, Wood, & Weisz, 2007; Vasey & Dadds, 2001). Fourth, the composite measure of anxiety used in this study included three “social inhibition” items. Although these items assessed both shyness and fear, the measure’s overlap with behavioral inhibition limits its utility as a pure assessment of social anxiety. Finally, the sample comprised primarily Caucasian caregivers and children, which may potentially limit the generalizability of the findings to other racial and ethnic groups. Additional work in this area is needed to address these limitations.
Conclusion
Overall, the current study identified four distinct anxiety symptom trajectories from preschool through school age in at-risk youth: two stable groups (high and moderate) and two decreasing groups (high and low). Children with chronic high anxiety (high stable) experienced greater baseline depression, greater social adversity/risk, higher maternal depression over time, and poorer social functioning over time compared to those with high but decreasing (high decreasing) symptoms. Greater externalizing/ADHD scores were also associated with high decreasing compared to low decreasing trajectories. High stable anxiety beginning in preschool was associated with lower school engagement, poorer global peer relations, and greater functional impairment during later school age compared to high decreasing anxiety. Taken together, these findings point to the critical role of the early environment and psychosocial experiences in the risk trajectory.
TABLE 1.
Characteristics of the Sample
| M (SD) | |
|---|---|
|
| |
| Age at Baseline (Years) | 4.47 (0.79) |
| IQ | 104.58 (14.87) |
|
| |
| %(n) | |
| Male Gender | 52.2 (142) |
| Race | |
| White | 55.5 (151) |
| Black | 31.6(86) |
| Other | 12.9 (35) |
| Baseline Parental Education | |
| High School Diploma or Less | 15.1 (41) |
| Some College | 39.0(106) |
| 4-Year College Degree | 21.0(57) |
| Graduate Education | 25.0 (68) |
| Baseline Total Family Income | |
| $0–$20,000 | 22.4 (61) |
| $20,001–$40,000 | 18.0 (49) |
| $40,00l–$60,000 | 18.8(51) |
| $60,001+ | 40.8(111) |
| Baseline Diagnoses | |
| Major Depressive Disorder | 24.3 (66) |
| ADHD | 14.0 (38) |
| Oppositional Defiant Disorder | 23.2 (63) |
| Conduct Disorder | 11.0(30) |
| Generalized Anxiety Disorder | 6.3 (17) |
| PTSD | 1.8 (5) |
| Separation Anxiety Disorder | 17.7 (48) |
| Mania | 7.7(21) |
Note: N = 272. ADHD = attention deficit hyperactivity disorder; PTSD = posttraumatic stress disorder.
Acknowledgments
FUNDING
Funding was provided by the National Institute of Mental Health: R01 MH064769.
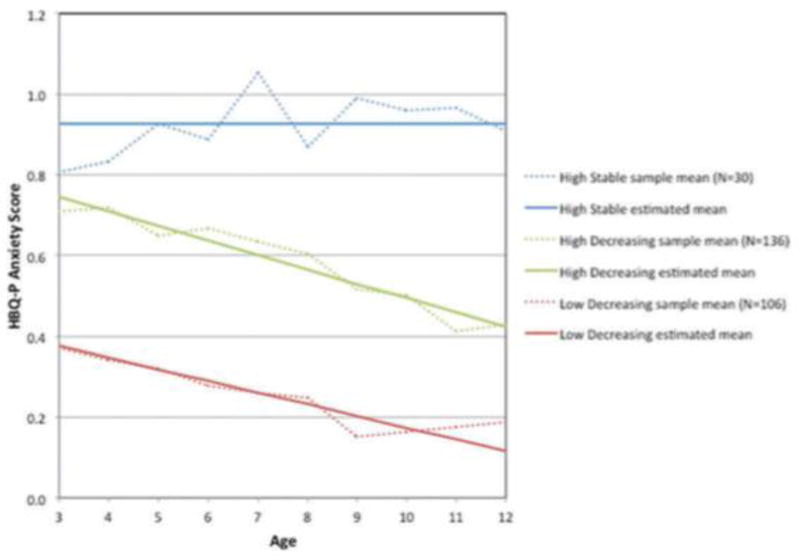
Appendix
TABLE A1.
Growth Mixture Model With “Three Classes
| Class | No. of Subjects |
|---|---|
| Low Decreasing | 106 |
| High Decreasing | 136 |
| High Stable | 30 |
Note: N =272.
TABLE A2.
Model Results of Three-Glass Growth Mixture Model
| Class | Term | Estimate | SE | Est/SE | P |
|---|---|---|---|---|---|
| Low Decreasing | Intercept | 0.377 | 0.024 | 15.591 | < .001 |
| Slope | −0.029 | 0.004 | −7.623 | < .00l | |
| Quadratic | Nonsignificant, so removed from model | ||||
| High Decreasing | Intercept | 0.746 | 0.028 | 26.998 | < .001 |
| Slope | −0.036 | 0.005 | −6.680 | <.001 | |
| Quadratic | Nonsignificant, so removed from model | ||||
| High Stable | Intercept | 0.926 | 0.043 | 21.452 | < .001 |
| Slope | Nonsignificant, so removed from model | ||||
| Quadratic | Nonsignificant, so removed from model | ||||
TABLE A3.
Test Statistics, Means, and Standard Deviations for Child and Maternal/Family Factors by Latent Class Group Membership
| Test Statistics | High Stable |
High Decreasing |
Low Decreasing |
||
|---|---|---|---|---|---|
| Demographics | Child Age | F(2, 269) =1.04 | 4.61 (.73) | 4.49 (.80) | 4.39 (.79) |
| 1Q | F(2, 217) = 2.64 | 99.95 (13.41) | 106.64(15.21) | 103.04 (14.46) | |
| Male (%) | χ2 = .67 | 47 | 52 | 55 | |
| T1 Child Factors | T1 HBQ–Anxiety | F(2, 252) - 76.59*** | .90(.30)HD LD | .72(.27)HD LD | .37(.21)HS HD |
| T1 HBQ–Depression | F(2, 254) = 27.28*** | 0.59 (.37)LD HD | 0.35 (.30)HS LD | 0.17 (.22)HS LD | |
| T1 HBQ–Externalizing | F(2, 247) = 5.23** | 0.50 (.31) | 0.51 (.35)LD | 0.37 (29)HD | |
| T1 HBQ–ADHD | F(2, 247) = 3.63* | 0.96 (.31)LD | 0 86 (.46) LD | 0.75 (43)HS | |
| T1 HBQ–Peer Acceptance | F(2, 249) = 3.53* | 3.28 (.50)LD | 3.43 (.52) | 3.57 (.52)HS | |
| T1 HBQ–Bullied | F(2, 249) = 2.16 | 1.58 (.74) | 1.56 (.67) | 1.39 (.58) | |
| T1 Maternal/ Family Factors |
Maternal Depression (%) | χ2(2) = 10.53* | 53LS | 46 | 28HD |
| Social Adversity/risk | F(2, 260) = 3.59* | 1.11 (.99) LD | 0.75 (.88) | 0.61 (.86)HS | |
| Maternal Anxiety | χ2(2) = 3.42 | 17 | 18 | 9 | |
| Income-to-needs ratio | F(2, 247) = 0.41 | 2.00 (122) | 2.07 (120) | 2.19(1.10) | |
| Stressful Life Events | F(2, 264) = .46 | 5.10(3 39) | 5.17(3.98) | 4.57 (6.03) | |
| Relative Diagnosis (%) | χ2(2)=8.69 | 83 | 95 | 84 |
Note: Pairs of letters indicate significant Bonferroni correted pairwise significant (P< .0083).
P< .05.
P< .01.
P< .001.
Figure A1.
Latent class trajectories of Health and Behavior Questionnaire–Parent(HBQ-P) anxiety—three-class solution.
Contributor Information
Sarah J. Kertz, Department of Psychology, Southern Illinois University-Carbondale
Chad Sylvester, Department of Psychiatry, Washington University School of Medicine.
Rebecca Tillman, Department of Psychiatry, Washington University School of Medicine.
Joan L. Luby, Department of Psychiatry, Washington University School of Medicine
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Angold A, Costello EJ. The Child and Adolescent Psychiatric Assessment (CAPA) Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(1):39–48. doi: 10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- Armstrong J, Goldstein L. MacArthur Foundation Research Network on Psychopathology and Development. University of Pittsburgh; Pittsburgh, PA: 2003. Manual for the MacArthur health and behavior questionnaire (HBQ 1.0) [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York: Guilford Press; 2002. [Google Scholar]
- Beck AT, Steer RA, Brown GK. In: Manual for the Beck Depression Inventory-II. Beidel DC, Turner MS, editors. San Antonio, TX: Psychological Corporation; 1996. Jul, At risk for anxiety: I. [Google Scholar]
- Psychopathology in the offspring of anxious parents. Journal of the American Academy of Child & Adolescent Psychiatry. 36:918–924. doi: 10.1097/00004583-199707000-00013. [DOI] [PubMed] [Google Scholar]
- Biederman J, Hirshfeld-Becker DR, Rosenbaum JF, Hérot C, Friedman D, Snidman N, Faraone SV. Further evidence of association between behavioral inhibition and social anxiety in children. The American Journal of Psychiatry. 2001;158:1673–1679. doi: 10.1176/appi.ajp.158.10.1673. [DOI] [PubMed] [Google Scholar]
- Broeren S, Muris P, Diamantopoulou S, Baker JR. The course of childhood anxiety symptoms: Developmental trajectories and child-related factors in normal children. Journal of Abnormal Child Psychology. 2013;41(1):81–95. doi: 10.1007/s10802-012-9669-9. [DOI] [PubMed] [Google Scholar]
- Bufferd SJ, Dougherty LR, Carlson GA, Klein DN. Parent-reported mental health in preschoolers: Findings using a diagnostic interview. Comprehensive Psychiatry. 2011;52(4):359–369. doi: 10.1016/j.comppsych.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bufferd SJ, Dougherty LR, Carlson GA, Rose S, Klein DN. Psychiatric disorders in preschoolers: Continuity from ages 3 to 6. The American Journal of Psychiatry. 2012;169(11):1157–1164. doi: 10.1176/appi.ajp.2012.12020268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. Journal of Child Psychology and Psychiatry. 2005;46(11):1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- Buss KA, Davis EL, Kiel EJ, Brooker RJ, Beekman C, Early MC. Dysregulated fear predicts social wariness and social anxiety symptoms during kindergarten. Journal of Clinical Child & Adolescent Psychology. 2013;42(5):603–616. doi: 10.1080/15374416.2013.769170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canivez GL, Konold TR, Collins JM, Wilson G. Construct validity of the Wechsler abbreviated scale of intelligence and wide range intelligence test: Convergent and structural validity. School Psychology Quarterly. 2009;24(4):252–265. [Google Scholar]
- Cartwright-Hatton S, McNicol K, Doubleday E. Anxiety in a neglected population: Prevalence of anxiety disorders in pre-adolescent children. Clinical Psychology Review. 2006;26(7):817–833. doi: 10.1016/j.cpr.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Cooper-Vince CE, Chan PT, Pincus DB, Comer JS. Paternal autonomy restriction, neighborhood safety, and child anxiety trajectory in community youth. Journal of Applied Developmental Psychology. 2014;35(4):265–272. doi: 10.1016/j.appdev.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60(8):837. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Côté S, Tremblay RE, Nagin D, Zoccolillo M, Vitaro F. The development of impulsivity, fearfulness, and helpfulness during childhood: Patterns of consistency and change in the trajectories of boys and girls. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2002;43(5):609–618. doi: 10.1111/1469-7610.00050. [DOI] [PubMed] [Google Scholar]
- Duchesne S, Larose S, Vitaro F, Tremblay RE. Trajectories of anxiety in a population sample of children: Clarifying the role of children’s behavioral characteristics and maternal parenting. Development and Psychopathology. 2010;22(2):361–373. doi: 10.1017/S0954579410000118. [DOI] [PubMed] [Google Scholar]
- Egger HL, Ascher B, Angold A. Department of Psychiatry and Behavioral Sciences. Duke University Medical Center; Durham, NC: 2003. The Preschool Age Psychiatric Assessment: Version 1.4. Center for Developmental Epidemiology. [Google Scholar]
- Essex MJ, Boyce WT, Goldstein LH, Armstrong JM, Kraemer HC, Kupfer DJ. The confluence of mental, physical, social, and academic difficulties in middle childhood. II: Developing the MacArthur Health and Behavior Questionnaire. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41(5):588–603. doi: 10.1097/00004583-200205000-00017. [DOI] [PubMed] [Google Scholar]
- Feng X, Shaw DS, Silk JS. Developmental trajectories of anxiety symptoms among boys across early and middle childhood. Journal of Abnormal Psychology. 2008;117(1):32–47. doi: 10.1037/0021-843X.117.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford T, Goodman R, Meltzer H. The British Child and Adolescent Mental Health Survey 1999: The prevalence of DSM-IV disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(10):1203–1211. doi: 10.1097/00004583-200310000-00011. [DOI] [PubMed] [Google Scholar]
- Fox NA, Henderson HA, Marshall PJ, Nichols KE, Ghera MM. Behavioral inhibition: Linking biology and behavior within a developmental framework. Annual Review of Psychology. 2005;56:235–262. doi: 10.1146/annurev.psych.55.090902.141532. [DOI] [PubMed] [Google Scholar]
- Garber J. Depression in children and adolescents: Linking risk research and prevention. American Journal of Preventive Medicine. 2006;31(Suppl. 6):S104–125. doi: 10.1016/j.amepre.2006.07.007. [DOI] [PubMed] [Google Scholar]
- Goldsmith H, Lemery KS. Linking temperamental fearfulness and anxiety symptoms: A behavior-genetic perspective. Biological Psychiatry. 2000;48(12):1199–1209. doi: 10.1016/s0006-3223(00)01003-9. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106(3):458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Hale WW, Raaijmakers Q, Muris P, van Hoof A, Meeus W. Developmental trajectories of adolescent anxiety disorder symptoms: A 5-year prospective community study. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(5):556–564. doi: 10.1097/CHI.0b013e3181676583. [DOI] [PubMed] [Google Scholar]
- Hays JR, Reas DL, Shaw JB. Concurrent validity of the Wechsler abbreviated scale of intelligence and the Kaufman brief intelligence test among psychiatric inpatients. Psychological Reports. 2002;90(2):355–359. doi: 10.2466/pr0.2002.90.2.355. [DOI] [PubMed] [Google Scholar]
- Hirshfeld-Becker DR, Biederman J, Henin A, Faraone SV, Davis S, Harrington K, Rosenbaum JF. Behavioral inhibition in preschool children at risk is a specific predictor of middle childhood social anxiety: A five-year follow-up. Journal of Developmental & Behavioral Pediatrics. 2007;28(3):225–233. doi: 10.1097/01.DBP.0000268559.34463.d0. [DOI] [PubMed] [Google Scholar]
- Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;2(1):302–317. [Google Scholar]
- Keenan K, Feng X, Hipwell A, Klostermann S. Depression begets depression: Comparing the predictive utility of depression and anxiety symptoms to later depression. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2009;50(9):1167–1175. doi: 10.1111/j.1469-7610.2009.02080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kiel EJ, Buss KA, Molitor JG. Kindergarteners’ self-reported social inhibition and observed social reticence: Moderation by adult-reported social inhibition and social anxiety disorder symptoms. Journal of Abnormal Child Psychology. 2015;43(3):531–542. doi: 10.1007/s10802-014-9925-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroes M, Kalff AC, Kessels AGH, Steyaert J, Feron F, Someren V, Vles J. Child psychiatric diagnoses in a population of Dutch schoolchildren aged 6 to 8 years. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1401–1409. doi: 10.1097/00004583-200112000-00010. [DOI] [PubMed] [Google Scholar]
- Last CG, Hansen C, Franco N. Anxious children in adulthood: A prospective study of adjustment. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(5):645–652. doi: 10.1097/00004583-199705000-00015. [DOI] [PubMed] [Google Scholar]
- Last CG, Hersen M, Kazdin A, Orvaschel H, Perrin S. Anxiety disorders in children and their families. Archives of General Psychiatry. 1991;48(10):928–934. doi: 10.1001/archpsyc.1991.01810340060008. [DOI] [PubMed] [Google Scholar]
- Last C, Perrin S, Hersen M, Kazdin AE. A prospective study of childhood anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35(11):1502–1510. doi: 10.1097/00004583-199611000-00019. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, Hopkins J, Gouze KR, Bryant FB. Bidirectional influences of anxiety and depression in young children. Journal of Abnormal Child Psychology. 2015;43(1):163–176. doi: 10.1007/s10802-014-9884-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemery-Chalfant K, Schreiber JE, Schmidt NL, Van Hulle CA, Essex MJ, Goldsmith HH, Tinklenberg J. Assessing internalizing, externalizing, and attention problems in young children: Validation of the MacArthur HBQ. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1315–1323. doi: 10.1097/chi.0b013e3180f616c6. [DOI] [PubMed] [Google Scholar]
- Luby JL, Heffelfinger A, Koenig-McNaught AL, Brown K, Spitznagel E. The preschool feelings checklist: A brief and sensitive screening measure for depression in young children. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(6):708–717. doi: 10.1097/01.chi.0000121066.29744.08. [DOI] [PubMed] [Google Scholar]
- Luby JL, Si X, Belden AC, Tandon M, Spitznagel E. Preschool depression: Homotypic continuity and course over 24 months. Archives of General Psychiatry. 2009;66(8):897–905. doi: 10.1001/archgenpsychiatry.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell ME. Family Interview for Genetic Studies (FIGS): A manual for FIGS. Bethesda, MD: Clinical Neurogenetics Branch, Intramural Research Program, National Institute of Mental Health; 1992. [Google Scholar]
- McLeod BD, Wood JJ, Weisz JR. Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review. 2007;27(2):155–172. doi: 10.1016/j.cpr.2006.09.002. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, Poulton R. Depression and generalized anxiety disorder: Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Archives of General Psychiatry. 2007;64(6):651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- Muris P. The pathogenesis of childhood anxiety disorders: Considerations from a developmental psychopathology perspective. International Journal of Behavioral Development. 2006;30(1):5–11. [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14(4):535–569. [Google Scholar]
- Ollendick TH, King NJ. Diagnosis, assessment, and treatment of internalizing problems in children: The role of longitudinal data. Journal of Consulting and Clinical Psychology. 1994;62(5):918–927. doi: 10.1037//0022-006x.62.5.918. [DOI] [PubMed] [Google Scholar]
- Olson SL, Rosenblum K. Preschool antecedents of internalizing problems in children beginning school: The role of social maladaptation. Early Education & Development. 1998;9(2):117–129. [Google Scholar]
- Rapee RM, Szollos AA. Developmental antecedents of clinical anxiety in childhood. Behaviour Change. 2002;19:146–157. [Google Scholar]
- Rice F, van den Bree MBM, Thapar A. A population-based study of anxiety as a precursor for depression in childhood and adoles-cence. BMC Psychiatry. 2004;4(1) doi: 10.1186/1471-244X-4-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman LD, Ollendick TH. Comorbidity of anxiety and depression in children and adolescents: An integrative review. Clinical Child and Family Psychology Review. 1998;1(2):125–144. doi: 10.1023/a:1021887712873. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Dulcan MK, Davies M, Piacentini J, Schwab-Stone ME, Regier DA. The NIMH diagnostic interview schedule for children version 2.3 (DISC-2.3): Description, acceptability, prevalence rates, and performance in the MECA Study. Methods for the Epidemiology of Child and Adolescent Mental Disorders Study. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35(7):865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Keenan K, Vondra JI, Giovannelli J. Antecendents of preschool children’s internalizing problems: A longitudinal study of low-income families. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;36(12):1760–7. [PubMed] [Google Scholar]
- Slopen N, Koenen KC, Kubzansky LD. Cumulative adversity in childhood and emergent risk factors for long-term health. The Journal of Pediatrics. 2014;164(3):631–638. doi: 10.1016/j.jpeds.2013.11.003. [DOI] [PubMed] [Google Scholar]
- Van Oort FVA, Greaves-Lord K, Verhulst FC, Ormel J, Huizink AC. The developmental course of anxiety symptoms during adolescence: The TRAILS study. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2009;50:1209–1217. doi: 10.1111/j.1469-7610.2009.02092.x. [DOI] [PubMed] [Google Scholar]
- Vasey MW, Dadds MR. The developmental psychopathology of anxiety. New York: Oxford University Press; 2001. [Google Scholar]
- Volbrecht MM, Goldsmith HH. Early temperamental and family predictors of shyness and anxiety. Developmental Psychology. 2010;46(5):1192–1205. doi: 10.1037/a0020616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: Psychological Corporation; 1999. [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Verdeli H, Pilowsky DJ, Bruder G. Families at high and low risk for depression: A 3-generation study. Archives of General Psychiatry. 2005;62(1):29–36. doi: 10.1001/archpsyc.62.1.29. [DOI] [PubMed] [Google Scholar]
- Whalen DJ, Luby JL, Tilman R, Mike A, Barch D, Belden AC. Latent class profiles of depressive symptoms from early to middle childhood: Predictors, outcomes, and gender effects. Journal of Child Psychology and Psychiatry. 2016;57:794–804. doi: 10.1111/jcpp.12518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen HU, Kessler RC, Pfister H, Lieb M. Why do people with anxiety disorders become depressed? A prospective-longitudinal community study. Acta Psychiatrica Scanadinavica. 2000;102:14–23. [PubMed] [Google Scholar]
- Zerwas S, Von Holle A, Watson H, Gottfredson N, Bulik CM. Childhood anxiety trajectories and adolescent disordered eating: Findings from the NICHD Study of Early Child Care and Youth Development. The International Journal of Eating Disorders. 2014;47(7):784–792. doi: 10.1002/eat.22318. [DOI] [PMC free article] [PubMed] [Google Scholar]