Abstract
Accountable care organizations (ACOs) and similar reforms aim to improve coordination between health care providers; however, due to the fragmented nature of the US health care system, successful coordination will hinge in large part on the ability of health care organizations to successfully partner across organizational boundaries. Little is known about new partnerships formed under the ACO model. We use mixed methods data from the National Survey of ACOs, Medicare ACO performance data and interviews with executive leaders across 31 ACOs to examine the prevalence, characteristics, and capabilities of partnership ACOs and why and how ACO partnerships form. We find that a striking percentage of ACOs – 81% – involve new partnerships between independent health care organizations. These “partnership ACOs” generally report lower capabilities on care management, care coordination, and health information technology. Additionally, under Medicare ACO programs partnership ACO achieved somewhat lower quality performance. Qualitative interviews revealed that providers are motivated to partner for resource complementarity, risk reduction, and legislative requirements, and are using a variety of formal and informal accountability mechanisms. Most partnership ACOs were formed out of existing, positive relationships, but a minority of ACOs formed out of previously competitive or conflictual relationships. Our findings suggests that the success of the ACO model will hinge in large part upon the success of new partnerships, with important implications for understanding ACO readiness and capabilities, the relatively small savings achieved to date by ACO programs, and the path to providers bearing more risk for population health management. In addition, ACO partnerships may provide an important window to monitor a potential wave of health care consolidation or, in contrast, a new model of independent providers successfully coordinating patient care.
Keywords: health policy, health care reform, health care costs, health care quality, alliances, mixed methods research, health care organizations
INTRODUCTION
Despite the growth in the number of physicians joining group practices and physician practices joining hospital and health systems, the US health care system remains largely a patchwork of independent health care provider organizations, including hospitals, physician practices, and nursing facilities. As a result, coordination of clinical care often requires working across organizational boundaries – for example coordination between hospitals and office-based physicians, or between primary care practices and the specialty practices to which they refer patients. This is particularly true when providing care to complex or high need patients who often require care from post-acute care facilities such as skilled nursing facilities, rehabilitation centers, and home health agencies. Thus, a central challenge facing US health care providers is how to best coordinate care across organizational boundaries.
Payment and delivery reforms such as accountable care organizations (ACOs) aim to encourage coordination through financial incentives. For example, ACOs include rewards for meeting quality performance targets and total cost of care benchmarks. Proponents hope that ACOs and similar reforms will reward and encourage better coordination of clinical care. To achieve such coordination, many providers under ACO contracts will need to build new ways of partnering across organizational boundaries. ACO success will largely depend on their ability to build effective new partnerships. The challenges include issues of governance, leadership, building trust, developing shared goals, managing highly interdependent work, clarifying roles and responsibilities and managing potential conflict.
Currently, little is known about the extent to which ACOs are developing partnerships, the types of partnerships developed, or the extent to which they are meeting desired cost and quality objectives. While a handful of studies have examined the involvement of particular types of providers in ACOs (e.g. hospitals or community health centers) and associated issues of partnering with those organizations,1–4 these studies cannot provide broader insight into the phenomenon of providers partnering under ACO contracts. In this paper, we address this gap in the literature by using mixed methods analysis (survey data, performance data, and semi-structured interviews) to describe the landscape of new partnerships between health care provider organizations associated with ACOs. We specifically examine the following questions: 1) to what extent are ACOs formed from new linkages between independent organizations versus from organizations that were previously part of the ACOs; 2) in what ways are partnership ACOs similar and different from ACOs that are existing organizations?; and 3) are there differences in performance between the different types of ACO partnerships? We discuss the implications of our findings for both policy and practice.
CURRENT LANDSCAPE OF US HEALTH CARE
Although there have been trends in consolidation of US health care providers over the last few decades,5,6 a large proportion of US health care providers still currently practice outside of integrated systems or large practices. For example, as of 2013, 65% of office-based physicians were in groups of five or fewer physicians.7 Against this backdrop of consolidation, accountable care organizations are a popular reform aimed at improving health care outcomes and costs. ACOs mirror reforms taking place in other countries that also aim to better coordinate and standardize care, improve quality, and reduce health care costs, such as the vanguard health care systems in the United Kingdom and primary care provider networks in France. Accountable care organizations are groups of providers collectively held responsible for the cost and quality of care they deliver to a defined group of patients. There are over 800 Medicare and commercial ACOs in the country covering about 23 million lives and located in almost every state.8 Proponents of ACOs hope that financial incentives around both cost and quality will encourage coordination among providers. While visionaries hope to move US health care rapidly to value-based payment models such as accountable care organizations, most physicians are not practicing in organizations that have the capabilities or patient population necessary to undertake value-based contracts.7 Most office based physicians in the United States still practice in groups of five or fewer physicians; these groups are too small to undertake new payment models alone because ACO program requirements generally require a minimum number of patients to accurately measure providers’ cost and quality performance. The fragmentation of health care providers in US health care markets will necessitate that providers partner with others to participate in accountable care organizations or similar value-based payment reforms. The strategic alliances literature based on an understanding of the foundations provided by resource dependence, transaction cost economics, and institutional theories provides a useful framework for understanding these types of new partnerships.
THEORETICAL FRAMEWORK
Strategic alliances are formal arrangements between two or more independent organizations to achieve shared or compatible goals. There was a significant growth in such relationships in the health care sector in the 1980s and 1990s as hospitals, in particular, merged with each other.9–11 Notably, these are arrangements between autonomous organizations and refer to non-ownership-based relationships. Throughout this section we draw on the literature about strategic alliances; throughout the paper we refer specifically to ACOs that include independent providers working together in an alliance as “partnership ACOs.”
The development of risk-based contracts through the ACO model may have triggered a new wave of strategic alliance formation involving not only physician practices, but potentially hospitals and post acute care facilities as well. The underlying motivation for these strategic alliance arrangements lie in understanding ACOs’ need for resources and capabilities; the need to limit transaction costs; and the need to respond to external requirements from Medicare.
Potential benefits to joining an alliance include economic benefits such as sharing risk or gaining resources; personnel benefits, including improved recruitment and management capabilities; and organizational benefits, including growth, opportunities to learn and gain new competencies, and mutual support and group synergy.11 Resource dependence theory highlights the organizations need to minimize uncertainty on its environment by engaging in behaviors (including forming alliances with others) that will bring additional resources or capabilities that the organization does not possess on its own.12,13 Given the emphasis of ACO contracts on finances and controlling costs, it is likely that ACO providers are motivated to partner for economic benefits such as sharing risk and gaining resources.
Of course, there are also costs to participating in alliances, including loss of autonomy and control; shared costs of failure; loss of resources or technical superiority; potential conflict over goals or methods; and coordination challenges.14 Transaction cost economics, in particular, suggest that ACOs may have to weigh the cost of purchasing services from other providers against the costs of building capacity internally or vertically integrating.15 Providers in partnership ACOs would certainly face costs. For example, an ACO that is bearing downside risk and fails to achieve performance benchmarks would be jointly responsible for any fiscal losses.
Finally, ACOs must respond to the institutional legitimacy demands of the CMS regulations requiring a minimum number of enrollees as well as cost and quality reporting requirements.16
Partnership Selection and Development Considerations
Issues of resources, transaction costs, and maintaining legitimacy are particularly salient in the choice of alliance partners. Key factors associated with partner selection are complementarity, commitment, and trust.17,18
Complementarity refers to skills and resources organizations have that are complementary as opposed to competitive; a classic example in health care would be the complementary roles of a rural community hospital and a large tertiary care center partnering. Providers entering into partnership ACOs will face challenges of partnership selection, and the literature would predict that successful partnership ACOs will have chosen partners carefully. Specifically, ACOs that consist of partners who complement each others’ resources rather than compete are more likely to be successful. This might apply to a variety of domains, such as services offered (e.g. primary care physicians partnering with hospitals) or organizational resources (e.g. an organization with substantial financial capital partnering with an organization with significant experience in population health). The literature suggests alliances would be less likely to form between providers who are competing.
Second, commitment refers to tangible contributions from partners to the alliance; it has been defined more broadly as a willingness to make short term sacrifices (e.g. time, money) for long term benefits of the alliance. The most successful partnership ACOs may have partners demonstrate commitment, such as through contribution of resources (such as money) to the partnership.
Finally, trust between potential partners reduces uncertainty and the threat of opportunism and is a key factor in partnership selection.19,20 Partnership ACOs will be most likely to form out of partners that have an initial level of trust. Some ACOs may form out of partners without an initial level of trust; these ACOs would to find ways to overcome the lack of trust to form a successful partnership. In addition, recent work has shown that contract structures can affect trust and continued collaboration.21
Partnership maturity and transition
Additionally, partnership ACOs likely face challenges to coordination as well as potential conflict over how to pursue goals. Once partners have been chosen and an alliance has formed, the alliance moves through processes of transition and maturity. In the transition phase, largely focused on design and governance, studies suggest that success depends on finding effective ways to coordinate alliance efforts.22 Trust and goodwill can facilitate this process, and contracts may specify roles and responsibilities of members. The continued development of trust and methods for conflict resolution is important in this phase, as mature alliances that are creating value (e.g. achieving shared savings under ACO contracts) must distribute value, and this can lead to conflict between partners that must be navigated. Partnership ACOs will need to develop governance as well as find ways to resolve conflict and build trust.
The Research Gap
Because of the fragmented nature of much of the US health care system, it is likely that many health care providers will need to partner to form ACOs, either to have the patient population to allow for stable population estimation of cost and quality, or to allow the ACO to influence more of a patients care along a continuum. To date, little is known about how prominent partnership ACOs are and how these ACOs’ capabilities and characteristics compare to ACOs formed by existing organizations. Additionally, there is no evidence on why and how ACO partnerships form, how health care providers approach partnership selection for ACO alliances, the types of commitment or accountability mechanisms ACOs use internally between partners, or how ACO partnerships function.
METHODS
Our goal was to describe the landscape of partnership ACOs and develop an in-depth understanding of how ACO partnerships operate. We used a mixed methods approach, combining analysis of several years of nationally representative survey data on ACOs with semi-structured qualitative interviews with ACO executives. We chose this approach to capture both prevalence and performance as well understand how and why ACOs were choosing to undertake a partnership approach.
Survey Data and Analysis
The National Survey of Accountable Care Organizations (NSACO) is a comprehensive survey of ACOs with questions on organizational characteristics, contract features, and a range of clinical and technical capabilities. The respondent at each organization was an executive or director-level administrator identified as being the most knowledgeable person to respond. Three waves of the NSACO were included in our analyses, fielded in 2012–2015; these surveys were all baseline for new ACOs formed since the previous wave. The overall survey response rate was 61%. At the same time as wave 3 was fielded, a brief follow up survey was sent to wave 1 respondents. This survey included questions added to the NSACO survey instrument after the initial wave 1 survey, largely due to improvements in the instrument between Waves 1 and 2 following advancements in the literature during the first year of Medicare ACO programs. The wave 1 follow-up survey was completed by 47.4% of Wave 1 respondents. Analysis has found no systematic non-response bias in the characteristics of respondents or performance on Medicare ACO measures.23,24
Notably, the first wave of NSACO data did not include any items measuring partnerships, as the research team did not anticipate the importance of new partnerships to ACO development. After a set of qualitative interviews in 2013, it became clear that partnerships would be highly important to understanding ACOs. As a result, we added two questions on ACO partnerships in waves 2–3 and the wave 1 follow up. The key survey question on partnerships asked, “Have the organizations participating in your ACO pursued a risk-based payment contract together in the past?” Possible responses included “Yes – all ACO participant organizations have,” “Yes – some ACO participant organizations have,” and “No – this is our first payment contract together.” We used this measure to compare new partnerships to pre-existing partnerships.
We compared these partnership categories on measures of prior collaboration, provider composition, services provided, and ACO contracts. We also compared the proportion of ACOs that reported high capabilities on measures of care management and quality improvement. These comparisons rely exclusively on the NSACO data. Our total sample analyzed was 275 ACOs who responded to the ACO partnership questions across waves.
In addition to survey analysis, we linked the survey data to quality and cost performance data released by the Center of Medicare and Medicaid Services (CMS) for the subset of survey respondents who were Medicare ACOs with available performance data. We analyzed performance across partnerships for Medicare ACOs joining the program through January 2014 on all quality metrics, composite measures, and savings generated. The sample of ACOs that have both NSACO data and Medicare performance data totaled 163.
We do not use formal tests of multiple testing in our analysis. Because of the small sample size, such corrections would make it mathematically difficult to detect differences in our data; we feel that despite this limitation, our data can make an important contribution. First, we emphasize differences that are large in magnitude. Second, we generally rely on patterns of results across multiple measures instead of individual measures. Finally, unlike in many traditional survey analyses where a survey sample represents a very small proportion of a population (typically <1%, or even <.1%), our ACO data represent a very large share of all ACOs (61%) since the NSACO was sent to not a sample of ACOs but to the census of all ACOs. Thus, while it is still possible from a mathematical standpoint that our results are due to random noise, our estimates are likely much more accurate than traditional survey sample estimates.
Qualitative Data and Analysis
In addition to our survey data, we conducted 56 semi-interviews across 31 distinct ACOs. We selected sites from the population of ACOs that received the NSACO on a number of elements, most notably the structure of the ACO (e.g. if there appeared to be a mix of new providers or single existing organization, as determined in background research) and the inclusion of safety net providers (to ensure a diversity of patient populations served by interviewed ACOs). We also examined the distribution of sites by leadership structure (physician vs. hospital-led), provider composition (e.g. number of primary care and specialty physicians), region, urban location, and ACO contracts (ensuring we had at Medicare, Medicaid, and commercial ACO contracts represented in our sample).
The semi-structured interviews were conducted by phone across two time periods: June-December 2013 and July-August 2014. In total, we conducted outreach by phone and email to 42 ACOs; 33 agreed to participate, and we completed interviewed with 31 ACOs (at two, the site initially agreed but we were unable to schedule an interview). Fourteen ACOs were interviewed during both time periods. In addition, in 2013 we conducted multiple interviews at 7 ACOs.
The particular individual(s) at an ACO participating in our interview was identified by the site based on an a project description we sent in advance; interviewees came from a variety of leadership positions, such as CEO of the ACO, ACO President, ACO board chair, or ACO director. In addition to interviews with executive leadership, at 7 sites we conducted multiple interviews; at these sites we conducted an interview with the leadership of a participating practice in the ACO to gain a broader perspective on the ACO.
Three distinct interview guides were used, two in the first time period and another for the second time period. Drawing on the strategic alliance literature, all guides included questions on the structure of the ACO, formation processes, leadership structures, motivations to participate in an ACO, and care delivery changes. Interviews were approximately an hour in length. Interviews were recorded, transcribed, and imported into QRS NVivo qualitative analysis software.
Our analytical approach was inductive, and our codes were empirically derived following the constant comparative method of analysis.25 Two team members (KT and VL) developed a coding definition for “partnerships” based on preliminary reading of transcripts. A single coder (KT) coded all of the transcripts for partnership related data, queried these data, and wrote a brief memo on initial themes in the data. A second team member (VL) reviewed the coded data, and the two met and discussed issues in the coding. After this initial process, we narrowed the focus from all types of partnerships to solely non-ownership relationships between ACO health care providers internal to the ACO (for example, removing from our coding definition topics such as partnerships with insurers). This narrowed definition aligned our coding and data with the concepts of strategic alliances as opposed to any partnerships more broadly.
The research team reviewed initial findings and generated sub-codes, and transcripts were subsequently sub-coded by a single coder (KT) and coding was again reviewed by a second team member (VL). The sub-codes included motivations to partner; partnership selection; partnership formation processes; challenges in partnerships; and solutions to partnership issues. This information was summarized in several memos and examined and discussed by members of the research team through a series of meetings. Initial themes and sub-themes were revised iteratively over several months until team consensus of the themes was achieved.
RESULTS
Quantitative results: Composition, characteristics, and capabilities of ACOs across partnership types
Addressing our first question, the survey data revealed that new partnerships were very common among ACOs. Overall, only 19% of ACOs responded that their ACO was an existing organization; 27% indicated that their ACO involved some new partners, and 55% indicated that their ACO was comprised of all new partners. Further analysis (not shown) indicated differences across ACO cohorts. Pioneers and Medicare Shared Savings Program (MSSP) ACOs starting in 2012 had a higher proportion of existing organizations, with 0% of Pioneers and 45% of 2012 MSSPs comprised of all new partners, whereas MSSPs starting 2013–2015 were a higher proportion (61%–65%) new partners.
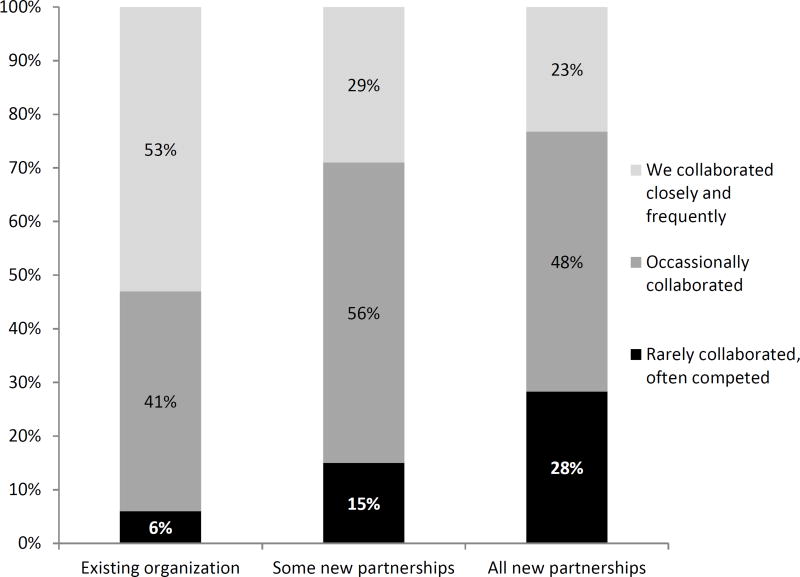
The NSACO asked respondents about the level of collaboration present prior to ACO formation (Figure 1). Among existing organizations, there was a relatively high degree of collaboration among participating providers prior to becoming an ACO, with only 6% indicating rare collaboration. Among all new partners, in contrast, 28% reported that prior to becoming an ACO the participating providers rarely collaborated and, in fact, often competed.
Figure 1.
Level of previous collaboration by ACO partnership type; data from the National Survey of ACOs.
ACO provider composition, services offered, and capabilities
Descriptive data on ACOs by partnership type are reported in Table 1. ACOs formed of all new partners were less likely to have a hospital or nursing facility compared to other types of ACOs, as well as less likely to involve an integrated delivery system. ACOs of all new partners were also the most likely to include only physician practices. ACOs that had some new partners were more likely to have a hospital, community health center, or nursing facility than other ACOs. Services offered within the ACO are largely not statistically distinguishable.
Table 1.
Descriptive characteristics of ACOs that are existing organizations, some new partners, and all new partners; data from the National Survey of Accountable Care Organizations
| Existing organization (N=51) |
Some new partners (N=74) |
All new partners (N=150) |
Chi-square or F-statistic |
|
|---|---|---|---|---|
| Composition | ||||
| Hospital in ACO | 0.69 | 0.75 | 0.57 | 7.1* |
| CHC in ACO | 0.16 | 0.41 | 0.29 | 8.4* |
| Nursing facility in ACO | 0.33 | 0.34 | 0.20 | 5.8+ |
| Integrated Delivery system | 0.67 | 0.58 | 0.45 | 8.5* |
| Physician groups only | 0.16 | 0.13 | 0.33 | 13.2** |
| Physicians | ||||
| Total physicians (FTE) | 521 | 517 | 324 | 4.2* |
| Percent physicians that are PCPs | 0.52 | 0.54 | 0.64 | 4.6* |
| Services offered within the ACO | ||||
| Primary care | 0.98 | 0.95 | 0.98 | 2.3 |
| Routine specialty care | 0.72 | 0.63 | 0.61 | 1.8 |
| Highly specialized care | 0.13 | 0.24 | 0.16 | 2.9 |
| Hospital inpatient care | 0.62 | 0.65 | 0.59 | 0.92 |
| Emergency Care | 0.63 | 0.63 | 0.53 | 2.4 |
| Urgent care | 0.66 | 0.58 | 0.60 | 0.83 |
| Inpatient rehab | 0.51 | 0.45 | 0.42 | 1.2 |
| Outpatient rehab | 0.55 | 0.49 | 0.40 | 3.7 |
| Behavioral health | 0.43 | 0.40 | 0.46 | 0.82 |
| Skilled nursing | 0.19 | 0.18 | 0.22 | 0.51 |
| Pediatric health | 0.75 | 0.52 | 0.52 | 8.4* |
| Palliative or hospice care | 0.56 | 0.45 | 0.39 | 4.2 |
| Home health | 0.48 | 0.38 | 0.35 | 2.6 |
| Outpatient pharmacy | 0.45 | 0.30 | 0.23 | 8.8* |
| Dental | 0.00 | 0.13 | 0.10 | 4.4 |
| Contracts | ||||
| Medicare ACO contract | 0.69 | 0.78 | 0.81 | 3.6 |
| Medicaid ACO contract | 0.35 | 0.26 | 0.18 | 6.5* |
| Private payer ACO contract | 0.86 | 0.64 | 0.52 | 19.1*** |
| Multipayer ACO | 0.71 | 0.67 | 0.54 | 8.4* |
| Have a contract with downside risk | 0.51 | 0.31 | 0.15 | 27.7*** |
Note:
indicates p<0.10;
indicates p <0.05;
indicates p <0.01;
indicates p <0.001
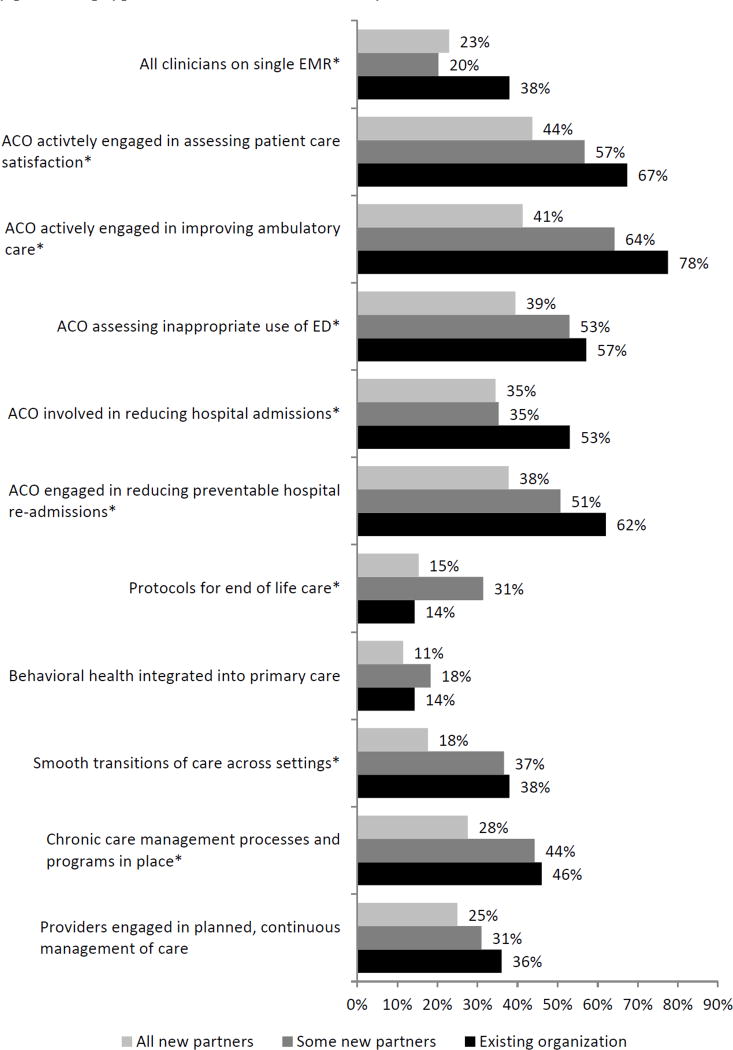
Addressing our second question, capabilities varied by ACO partnership types, as shown in Figure 2. ACOs that were an existing organization were most likely to have all clinicians on a single electronic medical record and to be actively engaged in assessing patient care satisfaction, working to improve ambulatory care, assessing inappropriate use of the emergency department, and engaged in reducing hospital admissions and preventable hospital re-admissions. ACOs formed of all new partners were generally lower on these measures. ACOs with some new partners fell in the middle, with some capabilities mirroring ACOs with all new partners (e.g. clinicians on a single EMR) and some capabilities mirroring existing organizations (e.g. smooth transitions of care). The only capability where existing organizations performed worse than partnership ACOs was on protocols for end of life care.
Figure 2.
Care management, quality improvement, and health information technology capabilities of ACOs by partnership type; data from the National Survey of ACOs
Note: + indicates p<0.10; * indicates p<0.05; ** indicates p<0.01; *** indicates p<0.001
Performance Outcomes
Addressing our third question, we next examined the performance of Medicare ACOs across partnership types (Table 2). There were no statistically significant differences in cost savings across partnership types; overall, a small proportion of ACOs achieved shared savings in the first year of contracts. In quality outcomes, there were significant differences across partnership types on eighteen out of 35 measures. The most consistent set of differences was in measures focused on at-risk populations. Existing organizations outperformed partnership ACOs on four out of five measures of diabetes care and the diabetes composite, controlled hypertension, two measures of ischemic vascular disease, and two measures of coronary artery disease care and the associated composite. On these performance measures, ACOs with some and all new partnerships generally were similar in performance. New partnership ACOs also fared worse on a few preventive health measures, with lower rates of colorectal cancer screening, mammography screening, and pneumococcal vaccinations, as well as lower percentages of primary care physicians qualifying for EHR incentive pay. Finally, new partnership ACOs had lower scores on some measures of patient/caregiver experience, although these differences were substantively very small.
Table 2.
Performance of Medicare ACOs in our sample on Medicare ACO cost and quality measures; data from the National Survey of ACOs and CMS performance data.
| Existing organization Mean (SD) |
Some new partners Mean (SD) |
All new partners Mean (SD) |
F-statistic | |
|---|---|---|---|---|
| Savings per beneficiary, Year 1 | $89 (538) | $4 (632) | $32 (459) | 0.23 |
| Received a shared savings bonus | 0.25 (.44) | 0.23 (.42) | 0.17 (.38) | 0.95 |
| Patient/Caregiver experience | ||||
| Getting Timely Care | 82.3 (2.3) | 80.8 (4.1) | 80.5 (3.3) | 2.9+ |
| How Well Your Doctors Communicate | 93.2 (.75) | 92.2 (2.0) | 92.9 (1.6) | 3.8* |
| Patients’ Rating of Doctor | 92.3 (.94) | 91.5 (1.7) | 92.0 (1.6) | 2.8+ |
| Access to Specialists | 85.4 (2.2) | 84.3 (2.9) | 84.8 (1.9) | 2.1 |
| Health Promotion and Education | 59.2 (3.6) | 58.0 (3.0) | 58.0 (4.1) | 1.1 |
| Shared Decision Making | 74.8 (2.2) | 74.0 (2.6) | 74.7 (2.3) | 1.4 |
| Health Status/Functional Status | 71.0 (3.2) | 71.1 (1.9) | 70.6 (2.3) | 0.77 |
| Care coordination and patient safety | ||||
| Risk-Standardized, All Readmission | 15.1 (.84) | 15.3 (.78) | 14.9 (.64) | 5.9** |
| Admissions: COPD or Asthma | 1.08 (.33) | 1.18 (.52) | 1.11 (.34) | 0.68 |
| Admissions: CHF | 1.16 (.19) | 1.23 (.28) | 1.19 (.25) | 0.72 |
| % PCPs qualifying for EHR incentive pay | 74.1 (23.5) | 62.0 (24.2) | 70.3 (20.7) | 3.1* |
| Med Rec after discharge from inpatient | 76.1 (30.6) | 81.4 (21.3) | 75.2 (26.1) | 0.83 |
| Falls: Screening for Fall Risk | 44.5 (27.7) | 34.0 (18.3) | 34.2 (23.4) | 2.25 |
| Preventive health | ||||
| Influenza Immunization | 58.8 (13.2) | 52.6 (16.7) | 55.0 (14.9) | 1.36 |
| Pneumococcal Vaccination | 62.9 (19.1) | 48.6 (21.0) | 51.2 (19.2) | 4.79** |
| Adult Weight Screening and Follow-Up | 60.4 (13.0) | 60.2 (18.7) | 58.7 (15.2) | 0.18 |
| Tobacco assessment & cessation intervention | 86.6 (18.0) | 83.8 (16.3) | 83.5 (13.0) | 0.48 |
| Depression Screening | 35.5 (26.9) | 30.1 (19.5) | 28.5 (21.2) | 1.07 |
| Colorectal Cancer Screening | 63.1 (11.3) | 54.5 (15.9) | 54.0 (17.5) | 3.41* |
| Mammography Screening | 67.6 (11.5) | 58.7 (16.0) | 59.5 (14.1) | 3.9* |
| Screening for High Blood Pressure | 59.7 (28.2) | 71.5 (21.6) | 67.7 (25.0) | 1.9 |
| At-risk populations | ||||
| Diabetes: Hemoglobin A1c Control | 71.8 (11.4) | 66.2 (13.2) | 68.1 (9.8) | 2.1 |
| Diabetes: Low Density Lipoprotein | 61.6 (10.7) | 53.5 (12.1) | 53.2 (10.2) | 6.7** |
| Diabetes: Blood Pressure <140/90 | 73.7 (9.6) | 66.5 (12.8) | 67.9 (11.2) | 3.6* |
| Diabetes: Tobacco Non-Use | 78.8 (12.9) | 66.1 (26.4) | 65.3 (24.6) | 3.5* |
| Diabetes: Aspirin Use | 84.5 (17.1) | 71.6 (23.2) | 76.1 (16.8) | 3.9* |
| Diabetes composite | 31.2 (10.9) | 21.0 (10.4) | 20.6 (10.7) | 11.0*** |
| Diabetes: Hemoglobin A1c Poor Control | 19.1 (12.1) | 24.9 (14.2) | 22.7 (10.5) | 2.0 |
| Hypertension: Controlling High Bl Pressure | 71.4 (6.7) | 65.0 (13.1) | 66.1 (10.9) | 3.1* |
| IVD: Complete Lipid Panel & LDL Control | 62.2 (7.9) | 53.7 (14.2) | 53.5 (13.7) | 4.9** |
| IVD: Use of Aspirin or Another Antithrombotic | 85.6 (9.0) | 72.3 (23.7) | 76.4 (18.3) | 4.2* |
| Heart failure: Beta-Blocker Therapy for LVSD | 82.7 (12.9) | 79.6 (20.9) | 82.9 (16.5) | 0.53 |
| CAD: Drug Therapy for Lowering LDL-Cholest | 78.9 (9.9) | 69.6 (19.9) | 70.9 (14.2) | 3.5* |
| CAD: ACE inhibitor or ARB Therapy for patients w/ CAD and diabetes and/or LVSD | 76.6 (10.8) | 68.7 (18.1) | 70.7 (13.9) | 2.5+ |
| CAD composite | 72.1 (9.1) | 61.1 (19.0) | 62.6 (14.6) | 4.99** |
| N | 28 | 44 | 91 | |
Note:
indicates p <0.10;
indicates p <0.05;
indicates p <0.01;
indicates p <0.001
Qualitative results
Motivations for partnering to form an ACO
Our data identified four main reasons providers or organizations came together to form an ACO; all consistent with the resource dependence, transaction cost economics, and institutional foundations for developing strategic alliances. These included resource complementarity, reducing risk (perceived or actual), patient attribution requirements, and legislation. The most common reason stated for partnering was resource complementarity. Fourteen ACOs interviewed explained that a partner was providing a resource or expertise the ACO perceived it needed. Specifically, sites mentioned seeking partners for primary care expertise; specialists and specialty expertise; data, analytic, or other technical capabilities; experience with care management; and ability to contribute capital or assume financial risk.
A second common reason providers looked to partner was to reduce the risk in undertaking an ACO contract, either direct financial risks or indirect, perceived risks. Most directly, some practices partnered with hospitals because the hospital either provided financial capital to initiate the ACO, such as to hire new care coordination staff or purchase analytic tools. Additionally, indirect risks or the perception of risk often drove partnerships between organizations that were interdependent. For example, two integrated delivery systems partnered to form one ACO because they served heavily overlapping geographic regions, and patients often saw providers in both systems. By partnering, the systems ensured that a higher portion of their patients’ care was retained within the ACO network, felt better able to monitor utilization, and therefore felt more confident in meeting cost and quality benchmarks.
A third reason providers formed partnerships to pursue ACOs was to meet minimum patient attribution requirements. Most ACO contracts require a minimum number of patients; for example, Medicare’s Shared Savings Program requires 5,000 beneficiaries. This requirement prompted smaller practices to partner to pursue an ACO. In addition, hospital-led ACOs reached out to local primary care practices to ensure enough physicians to meet attribution requirements. In the latter case, the hospital often shouldered the financial risk of an ACO (as discussed above) while the practices provided the necessary physician panels to create a viable ACO.
Finally, a handful of ACOs in states with Medicaid ACO programs noted that state legislation was a core driver of partnering since they were required to partner in order to form an ACO. Some states have developed ACO programs that are deliberately regional in nature, requiring providers in the region partner to pursue a Medicaid ACO contract. For example, Oregon requires that ACOs include both physical and behavioral health providers in a region to participate in the state’s Coordinated Care Organization program.
While some partnership ACOs were using partnerships to expand in scale (e.g. multiple primary care practices), others were using partnerships to expand in scope (e.g. expand the continuum of care by linking primary care and hospitals within one ACO). The specific motivations discussed above were common across ACOs that were horizontal and vertical partnerships, although the manifestations or specifics may have differed. For example, providers motivated to partner for resource complementary sometimes were looking to resources that would expand the scope of care within an ACO, but other times were looking for resources that were found among similar partners, such as an ACO adding particular primary care practices with expertise on managing specific types of patients, information or experience that would be valuable to share with other practices in the ACO.
ACO Partnership Formation Processes
The preceding section addressed why partnerships were formed; equally important is how these partners came together. The data suggests three formation processes. First, one method of adding providers was through recruitment. In this model, one organization interested in pursuing an ACO contract went to other providers and invited them to participate. This method of partnership formation was commonly used by hospitals or hospital systems that were pursuing an ACO and wanted (or needed) a larger physician base for their ACO. For example, at one ACO several physician leaders of a hospital recruited local private practice physicians to the ACO by visiting local practices to meet with physicians and talk about joining the ACO, emphasizing the benefits of joining the ACO. These physicians likely would not have participated in an ACO if not approached directly by the hospital. This recruitment was usually targeted rather than broad, meaning the instigating organization identified potential partners to invite rather than broadly recruiting all providers in a local area.
A second process of ACO partnership development was characteristic of ACOs forming out of a set of mutual associates. In these partnerships no single player instigated the ACO; instead a group of provider organizations decided jointly to pursue an ACO. For example, one ACO we interviewed formed out of a state primary care association. At an association meeting, a group discussed new ACO legislation and decided it was worth investigating more thoroughly, and a few members volunteered to do additional research on the ACO model. At a subsequent association meeting these members presented details on how practices might form an ACO together. From there, a group of interested practice leaders began meeting regularly to flesh out details of a possible ACO, eventually signing an ACO contract as a group.
Finally, larger systems or provider organizations added new providers through acquiring other practices or consolidation. This method of adding providers is predominately used by ACOs initiated by a single system or stand-alone practice.
Commitment and Accountability Mechanisms
After identifying and forming partnerships, many ACOs aimed to solidify commitments. The accountability and commitment mechanisms used by ACOs generally fell into two types: formal-legal mechanisms and informal-social mechanisms.
Informal or social mechanisms included two approaches: pacts and group norms. A number of ACOs used the “pact” mechanism. The word “pact” was how one site we interviewed described a type of non-contractual agreement; the ACO described the pact as a “code of responsibility for clinical efficiency.” We define pacts as non-contractual agreements about the roles and responsibilities of providers within an ACO. Often these pacts involved providing guides, regulations or information about how clinicians should behave as part of the ACO. Pacts were also used to ensure participating providers understood the expectations of being an ACO provider. For example, one ACO had a pact for specialist physicians joining the ACO that outlined clinical expectations around the use of generic medications, outpatient imaging facilities, and outpatient stays rather than inpatient stays, along with an agreement that no referrals should be made by the specialist without the approval of a primary care provider.
In addition to more explicit pacts, several ACOs established and maintained group norms both in early stages (when attempting to formalize their ACO contracts) as well as in later stages, when trying to improve participation. In the formation process of the ACO, norms were important in ensuring partners felt that they were being adequately represented. As ACOs moved beyond formation, norms remained an important mechanism for accountability. Often norms were integrated into the functioning of ACO committees and governing bodies. For example, one ACO leadership group established early a norm of weekly, full attendance at ACO board meetings by executives of each participating practice. This frequent, regular meeting encouraged accountability among partners.
In addition to informal-social mechanisms, some ACOs used formal or legal mechanisms, including pre-requirements to join the ACO, mandatory contributions, and legal contracts. Several ACOs required potential partners have certain capabilities before allowing them to join the ACO. For example, one ACO vetted any practices that wanted to participate; this process was comprised of a two-hundred question survey that assessed compliance with medical home operational requirements, HIPAA regulations, adequacy of information technology networks, and identified gaps in compliance that the potential partner may have. Another ACO required practices and providers joining the ACO to have an electronic medical record for ACO patients and be in the process of patient centered medical home certification.
Other ACOs required a contribution of resources from all members of the ACO in order to formalize commitment, such as financial capital or staff time. Financial contributions were structured in varied ways, including a fixed amount per provider organization or a contribution per physician full-time-equivalent in an organization. For example, one ACO was set up as a LLC legal entity, and to join the ACO, members contributed $1,000 per FTE physician to purchase shares of the LLC. Additionally, staff time was a valuable contribution. For example, at one ACO a member clinic contributed 50% of their medical director’s time to play the role of medical director for the ACO.
The final formal-legal approach was the use of legal contracts. This approach refers to ACOs either creating new organizations to participate in an ACO program (e.g. a new LLC) or embedding protocols or policies into legal contracts. For example, one physician hospital organization (PHO) rewrote its bylaws and membership agreement when they undertook ACO contracts to require practices participating in the PHO to participate in ACO activities, such as regularly reviewing quality data.
Tense prior relationships and conflict
Most new partnership ACOs interviewed had developed out of positive prior relationships between partners. However, a handful of ACOs (five interviewees) had developed between partners with some pre-existing tension, such as previous competition or distrust. For example, in one ACO one partner was suing another partner. In another, the practices participating in the ACO had a history of “ruthless competition”, such as hiring away each other’s executive leaders and well-loved clinicians. Notably, ACOs without positive relationships were often brought together by an external force, such as legislation requiring partnership or a perceived threat. Among those ACOs with tense relationships, we identified three strategies used to improve relationships: transparency among partners, having a facilitator, and contracting solutions.
Transparency among partners helped some ACOs overcome challenges of tense relationships. The first aspect of transparency was honestly and clearly articulating goals and challenges. For example, at one ACO member organization were very transparent about what they termed “bright lines.” In one case, some of the partners vocalized they were uncomfortable mutualizing risk; partners were able to talk through and resolve these issues and prevent conflict over shared financial risk at a later time. A second important aspect of transparency was around performance across participating organizations. One ACO used monthly quality meetings to present performance data across members on quality and cost measures. Presenting transparent data reduced interpersonal issues between clinical staff because it allowed staff to engage in shared learning and discussions based on performance, helping set aside personal differences and opinions that had plagued earlier interactions between clinics.
Second, some new partners with strained relationships relied on a neutral facilitator. In some cases, these facilitators were used to support effective meetings. For example, one ACO had a facilitator help support the new partners working toward an ACO agreement while negotiating and signing ACO contracts for the first time; the ACO credits the facilitator with successfully helping them meet their timeline for signing a contract. Additionally, a more global facilitator role existed at other ACOs. In some cases, an additional partner was brought on as a facilitator or administrator of the ACO. For example, at one ACO, a third party administrator did much of the centralized work of the ACO, such as monitoring compliance, completing required reporting, and implementing centralized care management provided by phone or in patients’ homes. This use of a global facilitator removed partners with tense relationships from directly negotiating ACO issues, and allowed them to function together as an ACO through a facilitator.
Finally, two ACOs we spoke with used contracting solutions to overcome conflicts that arose during ACO discussions and negotiations. In particular, these ACOs used financial contracting solutions around dispensing shared savings across partners to overcome conflicts between outpatient providers and hospitals. In both cases, hospital partners were worried about losing too much revenue too quickly due to ACO initiatives to reduce hospital admissions. Each ACO created a shared savings distribution plan to overcome these conflicts and keep hospital and outpatient partners participating together in the ACO. These financial contracting solutions helped overcome conflicting interests among partners.
DISCUSSION
The likely success of the ACO model will in large part hinge on the success of new partnerships between health care providers. These new partnership ACOs, are very common: upwards of three-quarters of ACOs involve new partners. These partnership ACOs in many ways face greater challenges than ACOs formed from existing organizations. At baseline they have lower capabilities around care management, quality improvement, and health information technology. Partnership ACOs have lower scores than existing organizations on some quality measures, particularly those measures focused on at-risk populations and preventive health. In early years, they are achieving cost savings at the same pace as existing organizations, although the proportion of ACOs receiving savings is low overall. These findings suggest that partnership ACOs are likely to benefit from technical assistance and participation in learning collaboratives that address such issues as formal and informal collaborative mechanisms, data sharing, and conflict management.
Qualitative research revealed multiple insights about partnerships in ACOs. ACOs were motivated to partner by attribution requirements, legislation, resource complementarity, and risk reduction. Partnership development typically happened through either a process of mutual agreement among equal partners, or the recruitment of providers by one organization catalyzing an ACO effort. New partners solidified commitments through both formal mechanisms (e.g. contracts or pre-requisites) and informal mechanisms (e.g. pacts or norms). Alliances were most often formed out of positive prior relationships, although several ACOs we interviewed had tense prior relationships; to overcome tension, ACOs employed tactics such as third party facilitators, transparency in both data and goals, and contracting solutions.
Our findings are generally consistent with the literature on health care strategic alliances and add to this literature by highlighting the important effects of broader contextual forces, such as policies that promote (or force) partnerships. For example, policy requirements about minimum number of patients or requirements about regional partners have encouraged providers to partner, sometimes despite other negative factors. Several ACOs interviewed as well as in our survey data revealed that ACOs were forming out of prior negative relationships, such as ones that were competitive rather than collaborative or exhibited a lack of trust. ACOs may provide a fruitful field to study how partners can use informal and formal mechanisms to successfully overcome issues of trust.
Partnership ACOs potentially present either positive or negative consequences for the US health care system, as well as some issues with unknown consequences. On the positive side, health care providers, particularly those in smaller provider organizations, may prefer working in alliance settings than consolidating through purchasing or ownership. Provider autonomy has long been a value in American health care and among physicians;26,27 the simple fact that so many US health care providers have remained in small provider organizations suggests a preference among some providers to be in smaller organizations where they retain autonomy and control, rather than become employees of a very large system or group practice. Successful models of partnership ACOs may present a more palatable option to independent health care providers, practices, or organizations who wish to retain a degree of organizational autonomy while participating in value-based payment reforms and having a venue to work toward goals of better coordinated care and population health.
Additionally, it is possible that partnership ACOs may produce better outcomes for patients than providers would deliver outside alliances. Overall, research has found that collaboration between organizations spurs innovation and learning in the organizations involved.28,29 The focus of ACOs on improving quality as well as coordinating care across providers may improve patient outcomes, and partnership ACOs may provide a venue or platform for independent providers to develop systems and processes to coordinate and manage care jointly that otherwise is lacking. The financial incentives in ACO contracts may encourage a greater degree of commitment to these joint efforts than exist in more diffuse ventures such as regional or local quality initiatives.30
The proliferation of partnership ACOs also carries potential negative consequences. First, it is possible (that depending on regulations) partnership ACOs may begin collectively negotiating to raise prices or keep out unwanted competition.31,32 Other demonstrated downsides of consolidation may also appear among partnership ACOs. For example, evidence has shown that when health care providers consolidate, referrals follow patterns of ownership over quality; that is, patient are more likely to stay within a health care system for a provider referral, even when the provider within the system has lower quality of care than a provider outside the system.33 This could improve care in an ACO setting if providers are in fact coordinating care, but not if it comes at a cost of forgoing higher quality providers to simply stay within an ACO network.
Finally, it is unclear what the future of ACO partnerships may be, and if partnership ACOs are a sustainable model on their own, or if instead partnership ACOs are an interim phase. Partnership ACOs may be precursors to further consolidation as alliance participants consolidate into fewer organizations over time. Alternatively, partnership ACOs may fail to fully solidify and dissolve into fully independent, component parts. ACOs may be an important window to monitor a potential wave of further consolidation.
The dominance of ACO programs by new partnerships may be a surprise to policymakers. For example, Medicare’s ACO programs contain few regulations or statements related to alliances. Given evidence on the high proportion of ACOs that are new partnerships, policymakers may consider ways to best support and monitor alliance activity. It is unlikely the ACO model will be able to improve health care costs or quality at a reasonable scale if new partners do not by and large succeed. As a result, policymakers may consider ways to encourage success among partnership ACOs. Some examples include helping build collaborative capacity or providing support for care management or patient centered medical home capabilities. As evidenced in our findings, specific policy requirements around things like attribution or particular types of required partners can spur partnership activity.
Understanding partnership activity may help explain other evidence or questions about ACOs. For example, Medicare ACOs have achieved relatively small savings in their first years. While some policymakers or economists have suggested that Medicare’s ACO programs need higher risks and higher rewards to achieve better results, our results suggest potential alternative explanations. Findings here might imply that one reason ACOs are not achieving larger savings is that many ACOs have had some organizational start up in forming partnerships, such as settling on accountability mechanisms and formalizing contracts or agreements between partners and overcoming previous conflicts, that may necessarily precede successful efforts on cost and quality. Understanding the path, trajectory, and challenges of partnership ACOs may also help policymakers refine attempts at pushing or encouraging health providers to take greater financial risk for population health management, for example potentially modifying Medicare’s timelines to risk bearing in the Medicare Shared Savings Program.
In addition to understanding mechanisms supporting successful strategic alliance relationships, there are several other important avenues for future work in this area. First, it is unclear at this point what specific aspects of ACO partnerships may be associated with success on cost and quality of care. Second, it would be important to examine not just the nature of ACOs, but how ACO strategic alliances change the organizations participating in them.34 Finally, understanding the reasons for and consequences of dissolution of or withdrawal from ACO partnerships could be another productive area of study.
For health care providers considering such strategic alliances, our findings suggest a few key issues for success. Partnership selection is an important factor in forming a successful alliance: carefully selected partners with complementary resources and similar organizational culture will likely have the easiest time forming alliances. For those who encounter issues of trust or conflict, tools such as facilitators or the use of data transparency may help build stronger working relationships. More in-depth work on the interplay of informal-social and formal-legal mechanisms in partnership ACOs may provide additional insight into how providers with a history of conflict or distrust can form successful ACOs. Given the fragmented and competitive nature of many US health care markets and segments, this insight could prove invaluable in helping transition to a more coordinated, clinically integrated and value-based US health care system.
Supplementary Material
Contributor Information
Valerie A. Lewis, The Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth, Lebanon, NH
Katherine I. Tierney, The Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth, Lebanon, NH
Carrie H. Colla, The Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth, Lebanon, NH
Stephen M. Shortell, School of Public Health and Haas School of Business, University of California, Berkeley, Berkeley, CA.
References
- 1.Lewis VA, Colla CH, Schoenherr KE, Shortell SM, Fisher ES. Innovation in the safety net: integrating community health centers through accountable care. J Gen Intern Med. 2014;29(11):1484–1490. doi: 10.1007/s11606-014-2911-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Colla CH, Lewis VA, Bergquist SL, Shortell SM. Accountability across the Continuum: The Participation of Postacute Care Providers in Accountable Care Organizations. Health Serv Res. 2016 Jan; doi: 10.1111/1475-6773.12442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Colla CH, Lewis VA, Tierney E, Muhlestein DB. Hospitals Participating In ACOs Tend To Be Large And Urban, Allowing Access To Capital And Data. Health Aff (Millwood) 2016;35(3):431–439. doi: 10.1377/hlthaff.2015.0919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dupree JM, Patel K, Singer SJ, et al. Attention To Surgeons And Surgical Care Is Largely Missing From Early Medicare Accountable Care Organizations. Health Aff. 2014;33(6):972–979. doi: 10.1377/hlthaff.2013.1300. [DOI] [PubMed] [Google Scholar]
- 5.Goldstein L. The new wave of hospital consolidation. Healthc Financ Manage. 2012;66(4):60–67. [PubMed] [Google Scholar]
- 6.Peterson LE, Baxley E, Jaén CR, Phillips RL. Fewer Family Physicians Are in Solo Practices. J Am Board Fam Med. 2015;28(1):11–12. doi: 10.3122/jabfm.2015.01.140217. [DOI] [PubMed] [Google Scholar]
- 7.Burns LR, Goldsmith JC, Sen A. Horizontal and vertical integration of physicians: a tale of two tails. Adv Health Care Manag. 2013;15:39–117. doi: 10.1108/s1474-8231(2013)0000015009. [DOI] [PubMed] [Google Scholar]
- 8.Muhlestein DB, McClellan MB. Accountable Care Organizations In 2016: Private And Public-Sector Growth And Dispersion. [Accessed May 2, 2016];Health Affairs. 2016 Apr; http://healthaffairs.org/blog/2016/04/21/accountable-care-organizations-in-2016-private-and-public-sector-growth-and-dispersion/
- 9.Kaluzny AD, Zuckerman HS. Strategic Alliances: Two Perspectives for Understanding Their Effects on Health Services. Hospital & Health Services Administration. 1992;37(4):477. [PubMed] [Google Scholar]
- 10.Longest BB., Jr Interorganizational linkages in the health sector. Health Care Manage Rev. 1990;15(1):17–28. doi: 10.1097/00004010-199001510-00006. [DOI] [PubMed] [Google Scholar]
- 11.Zuckerman HS, Kaluzny AD, Ricketts TC. Alliances in health care: what we know, what we think we know, and what we should know. Health Care Manage Rev. 1995;20(1):54–64. doi: 10.1097/00004010-199502010-00007. [DOI] [PubMed] [Google Scholar]
- 12.Pfeffer J, Salancik G. The External Control of Organizations: A Resource Dependence Perspective. 1. Stanford, Calif: Stanford Business Books; 2003. [Google Scholar]
- 13.Aldrich HE, Pfeffer J. Environments of Organizations. Annual Review of Sociology. 1976;2(1):79–105. [Google Scholar]
- 14.Zuckerman HS. Multi-Institutional Systems: Promise and Performance. Inquiry. 1979;16(4):291–314. [PubMed] [Google Scholar]
- 15.Mick SSF, Shay PD. Accountable Care Organizations and Transaction Cost Economics. Med Care Res Rev. 2016 Mar; doi: 10.1177/1077558716640411. 1077558716640411. [DOI] [PubMed] [Google Scholar]
- 16.Arndt M, Bigelow B. Presenting Structural Innovation in an Institutional Environment: Hospitals’ Use of Impression Management. Administrative Science Quarterly. 2000;45(3):494–522. [Google Scholar]
- 17.Shah RH, Swaminathan V. Factors influencing partner selection in strategic alliances: the moderating role of alliance context. Strategic Management Journal. 2008;29(5):471–494. [Google Scholar]
- 18.Zajac EJ, D’Aunno TA, Burns LR. Managing Strategic Alliances. In: Burns LR, Bradley EH, Weiner BJ, editors. Shortell and Kaluzny’s Health Care Management Organizational Design and behavior. Sixth. Clifton Park, NY: Delmar Cengage Learning; 2012. pp. 321–346. [Google Scholar]
- 19.Ariño A, de la Torre J, Ring PS. Relational quality and inter-personal trust in strategic alliances. European Management Review. 2005;2(1):15–27. [Google Scholar]
- 20.Das TK, Teng B-S. Trust, Control, and Risk in Strategic Alliances: An Integrated Framework. Organization Studies. 2001;22(2):251–283. [Google Scholar]
- 21.Malhotra D, Lumineau F. Trust and Collaboration in the Aftermath of Conflict: The Effects of Contract Structure. ACAD MANAGE J. 2011;54(5):981–998. [Google Scholar]
- 22.Kale P, Singh H. Managing Strategic Alliances: What Do We Know Now, and Where Do We Go from Here? Academy of Management Perspectives. 2009;23(3):45–62. [Google Scholar]
- 23.Albright BB, Lewis VA, Ross JS, Colla CH. Preventive Care Quality of Medicare Accountable Care Organizations: Associations of Organizational Characteristics With Performance. [Accessed March 17, 2016];Medical care. 2016 doi: 10.1097/MLR.0000000000000477. http://europepmc.org/abstract/med/26759974. [DOI] [PMC free article] [PubMed]
- 24.Colla CH, Lewis VA, Shortell SM, Fisher ES. First National Survey Of ACOs Finds Physicians Are Playing Strong Leadership And Ownership Roles. Health Affairs (Millwood) 2014;33(6):964–971. doi: 10.1377/hlthaff.2013.1463. [DOI] [PubMed] [Google Scholar]
- 25.Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago: Aldine Pub. Co; 1967. [Google Scholar]
- 26.Emanuel EJ, Pearson SD. Physician autonomy and health care reform. JAMA. 2012;307(4):367–368. doi: 10.1001/jama.2012.19. [DOI] [PubMed] [Google Scholar]
- 27.Mechanic D. The Rise and Fall of Managed Care. Journal of Health and Social behavior. 2004;45:76–86. [PubMed] [Google Scholar]
- 28.Goes JB, Park SH. Interorganizational Links and Innovation: The Case of Hospital Services. The Academy of Management Journal. 1997;40(3):673–696. [Google Scholar]
- 29.Hagedoorn J, Duysters G. External Sources of Innovative Capabilities: The Preferences for Strategic Alliances or Mergers and Acquisitions. Journal of Management Studies. 2002;39(2):167–188. [Google Scholar]
- 30.McHugh M, Shi Y, Ramsay PP, et al. Patient-Centered Medical Home Adoption: Results From Aligning Forces For Quality. Health Aff. 2016;35(1):141–149. doi: 10.1377/hlthaff.2015.0495. [DOI] [PubMed] [Google Scholar]
- 31.Berenson R. Addressing Pricing Power in Integrated Delivery: The Limits of Antitrust. Journal of Health Politics, Policy and Law. 2015;40(4):711–744. doi: 10.1215/03616878-3150026. [DOI] [PubMed] [Google Scholar]
- 32.Feinstein DL, Kuhlmann P, Mucchetti PJ. Accountable Care Organizations and Antitrust Enforcement: Promoting Competition and Innovation. Journal of Health Politics, Policy and Law. 2015;40(4):875–886. doi: 10.1215/03616878-3150112. [DOI] [PubMed] [Google Scholar]
- 33.Baker LC, Bundorf MK, Kessler DP. The effect of hospital/physician integration on hospital choice. 2015 Aug; [Google Scholar]
- 34.Hearld LR, Alexander JA. Governance processes and change within organizational participants of multi-sectoral community health care alliances: the mediating role of vision, mission, strategy agreement and perceived alliance value. Am J Community Psychol. 2014;53(1–2):185–197. doi: 10.1007/s10464-013-9618-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.