Abstract
A growing body of literature indicates that the mental distress experienced by survivors of war is a function of both experienced trauma and stressful life events. However, the majority of these studies are limited in that they 1) employ models of psychological distress that emphasize underlying latent constructs and do not allow researchers to examine the unique associations between particular symptoms and various stressors; and 2) use one or more measures that were not developed for that particular context and thus may exclude key traumas, stressful life events and symptoms of psychopathology. The current study addresses both these limitations by 1) using a novel conceptual model, network analysis, which assumes that symptoms covary with each other not because they stem from a latent construct, but rather because they represent meaningful relationships between the symptoms; and 2) employing a locally developed measure of experienced trauma, stressful life problems and symptoms of psychopathology. Over the course of 2009 to 2011, 337 survivors of the Sri Lankan civil war were administered the Penn-RESIST-Peradeniya War Problems Questionnaire (PRPWPQ). Network analysis revealed that symptoms of psychopathology, problems pertaining to lack of basic needs, and social problems were central to the network relative to experienced trauma and other types of problems. After controlling for shared associations, social problems in particular were the most central, significantly more so than traumatic events and family problems. Several particular traumatic events, stressful life events and symptoms of psychopathology that were central to the network were also identified. Discussion emphasizes the utility of such network models to researchers and practitioners determining how to spend limited resources in the most impactful way possible.
Keywords: Network analysis, Sri Lanka, war survivors, daily stressors, trauma, war trauma
There are currently 65.3 million people who have been displaced by violent conflict and humanitarian disasters, the largest number since the mid-1990s (United Nations High Commission for Refugees, 2016). Numerous studies have documented that refugees and other displaced populations suffer from high rates of emotional distress, which stem from their experience of war trauma (e.g., Neuner & Elbert, 2007) and other stressors related to forced displacement (for a review, see Fazel, Wheeler, & Danesh, 2005). However, there remains a lack of consensus among practitioners and researchers who work with conflict-affected populations on how best to conceptualize and address their mental health needs (van Ommeren, Saxena, & Saraceno, 2005). Practitioners in the field have observed a wide variety of patterns of stressors and distress across different war-affected populations (e.g., Jones & Kafetsios, 2002). Conversely, researchers have typically conceptualized the relationship between stressors and distress as a more limited stressors-distress equation, in which each side of the equation is typically collapsed into a small number of constructs. Stressors are usually operationalized as a set of composite causal indicators (usually scores on a traumatic event checklists, but increasingly inclusive of other types of stressors), and distress usually a set of latent variables reflected by responses to psychological symptom items (often scores from posttraumatic stress disorder [PTSD] or depression questionnaires) on the other. The current study takes a relatively novel approach to this problem, conceptualizing and visualizing traumatic events, other stressors, and distress as nodes in a network of problems. Although the visualization of data points in multidimensional space has a number of time-testing precedents (e.g., Smallest Space Analysis; Guttman, 1968), in psychology network approaches are relatively new (Armour, Fried, Deserno, Tsai & Pietrzak, 2017; Boorsboom & Cramer, 2013; McNally, 2012); only one previous study has included both stressors and distress in a network model within a war-affected population (De Schryver, Vindevogel, Rasmussen & Cramer, 2015).
Conceptualizing psychological symptoms as reflecting underlying latent constructs has several drawbacks. First, these models rest on the assumption that symptoms reflect underlying latent constructs, and therefore do not allow researchers to examine the unique associations between particular stressors and particular symptoms (or even sets of symptoms). Second, latent constructs are indicated by sets of symptoms, which means that symptoms that are not correlated with others will be excluded—without regard for potentially important bivariate associations with stressors (Layne, Olsen, Baker, Legershi, Isakson, et al., 2010). This situation limits the variability that can be observed on the emotional distress side of the stressor-distress equation, not allowing for the full range of potential patterns reported by practitioners in the field. Finally, latent variable models also violate basic statistical assumptions concerning the local independence of their indicators (Boorsboom & Cramer, 2013).
As a solution to violation of local independence in latent variable models, several researchers have proposed that sets of symptoms be modeled as causal networks of concrete indicators (Boorsboom & Cramer, 2013). Network approaches assume that symptoms are variables that indicate only themselves. This does not preclude the discussion of broader psychological constructs—e.g., diagnoses—but rather posits that these broader constructs are best conceptualized as sets of autonomous phenomena (i.e., symptoms) arranged in networks of problems, perhaps even as causal chains of such problems (Schmittmann et al., 2013). For example, PTSD might be conceptualized as a set of symptoms meaningfully related to one another—e.g., trauma-related nightmares causing sleep difficulties which in turn cause anger or irritability—rather than in a somewhat vague association between intrusion, avoidance, negative alterations in cognitions and mood, and hyperarousal (McNally, 2012; McNally et al., 2015). Notably, modeling sets of symptoms as causal networks better reflects much short-term clinical practice, in which clinicians focus on alleviating symptoms that seem to be at the root of other symptoms.
In network models of psychological distress, each symptom is a node, and covariance between symptoms is represented as ties between nodes. Ties may be binary (i.e., symptoms covary or do not) or weighted according to the strength of their covariance. Association networks are based on correlations between nodes, and concentration networks on partial correlations in order to account for background association between nodes in association networks (McNally, 2012). Nodes’ prominence within networks is observed by calculating their centrality. Centrality refers to a related set of measures that capture information about the roles of individual nodes in the network and involves the number, weight, and pattern of ties associated with each node. If an individual endorses a particular node that is central, then the probability of that individual endorsing other nodes is greater than if the individual endorses a node that is peripheral to the network (Fried et al., 2017). Visualizing networks allows researchers to note relative placements of nodes, which indicate central or peripheral roles within networks.
If we accept that both sides of the stressors-distress equation can be composed of diverse and autonomous conceptual entities, it is not a stretch to conceptualize a causal network between these entities. In other words, consistent with social ecological models in psychology (e.g., Bronfenbrenner, 1977, Moos, 1984), a network approach allows various traumatic events, other stressors and symptoms to be linked to one another, illustrating patterns that may better reflect individuals’ emotional experience of distress in the context of traumas and other stressors. De Schryver and colleagues (2015) argued for such an approach and have provided the only demonstration to date of how network analysis can identify relationships between traumatic events, stressors and symptoms. De Schryver et al. (2015) examined ties between stressful wartime events, daily stressors, and PTSD symptoms in a conflict-affected Ugandan sample. Their network revealed that although symptoms clustered closely together on one side in a subnetwork and stressful wartime events and daily stressors clustered closely on the other, there were several important intermediary nodes connecting the two subnetworks. In addition, there was considerable variety in centrality, with traumatic wartime events and daily stressors having greater centrality on average than symptoms.
Network science findings so far are consistent with several established theoretical approaches describing how multiple types of losses and stressors result in multiple forms of distress. The most prominent of these is Conservation of Resources (COR) theory (Hobfoll, 1989; 2001), which proposes that stress results from perceived loss or potential loss. If one’s losses are large—as is often the case among survivors of war—then one has fewer remaining resources that could be used to protect against further loss. COR theory predicts that losses (and trauma, which often represents loss) often interact in loss spirals, i.e., cascading stressors that result in considerable psychological distress (Hobfoll, 2001). COR theory has substantial support in war-affected populations, including Sri Lanka (e.g., Mattock, 2005; Siriwardhana et al., 2013, Somasundaram & Sivayokan, 2013; Witting, Lambert, Wickrama, Thanigaseelan, & Merten, 2016). Other similar theories with empirical support include the daily stressors model, in which the effects of war-related trauma on psychological distress are mediated and moderated by frequent stressors and stressful conditions (Miller & Rasmussen, 2010; 2014; 2017). It is not our intention in the current study to somehow propose new theory via network science, only to present findings using alternative methods.
In the current study, we applied network science methods to understand how war trauma, daily stressors and symptoms of mental distress interacted to create local networks of problems in survivors of the Sri Lankan civil war (E. Jayawickreme, Jayawickreme, & Miller, 2010). The war, which lasted from 1983 to 2009, was fought primarily between the armed forces of the Sri Lankan government and the Tamil separatist group, the Liberation Tigers of Tamil Eelam (LTTE) and resulted in the deaths of at least 100,000 people and the displacement of a further 800,000 (Vhurumuku, Nanayakkara, Petersson, Kumarasiri, & Rupasena, 2012). Civilians caught in the conflict experienced devastating losses, including shelling, aerial bombardment, food and water shortages, loss of shelter, loss of employment, loss of material goods, rape, torture, and forced recruitment into the LTTE (Harrison, 2012). Seven years after the end of the war, over 45,000 internally displaced individuals remain in Sri Lanka, many living in desperate conditions (United Nations High Commission for Refugees, 2016).
In the current study, symptoms of psychological distress, experienced war trauma and daily stressors were assessed using a locally developed measure, the Penn-RESIST-Peradeniya War Problems Questionnaire (PRPWPQ; Jayawickreme, Jayawickreme, Goonasekera, & Foa, 2009; Jayawickreme, Jayawickreme, Atanasov, Goonasekera, & Foa, 2012). Compared to standard instruments developed in the Western world, local measures that incorporate local idioms of distress as well as traumatic events and daily stressors that are unique to that particular setting allow for a more sensitive and accurate assessment (Jayawickreme et al., 2012; Bolton & Tang, 2002). While other studies examining the relationship between experienced trauma, daily stressors and symptoms of psychological distress have used local measures to measure at least one of these variables (e.g., Fernando, Miller, & Berger, 2010; Rasmussen et al., 2010), none have thus far used measures comprised of local idioms to measure all three. Thus, the current study aims to expand our understanding of the dynamic relationship between experienced traumatic events, daily stressors and symptoms of psychological distress in post-war settings by using network analysis and measures developed specifically for those settings.
Method
Participants
Participants were 337 Sri Lankan Tamil survivors of war who received psychosocial assistance from the Family Rehabilitation Center (FRC), a local nongovernmental organization. Data were collected over the course of 2009 through to 2011from FRC clinics in Jaffna, Batticaloa, Trincomalee, Vavuniya, and Nallur. These were all areas that were greatly impacted by the civil war. Participation in the study was voluntary and participants were paid 100 Sri Lankan rupees (approximately 75 U.S. cents) in compensation. The average age of the survivors was 43.41 years (SD = 13.7). Of the participants, 185 were male (54.9%), 149 were female (44.2%) and three did not report their gender (0.9%).
All procedures were approved by the Institutional Review Board at the University of Pennsylvania, Philadelphia, PA, United States, and by the Ethics Committee at the University of Peradeniya, Sri Lanka
Measure
Demographic Form
Participants completed a demographics form that included questions about participants’ ethnicity, gender and age.
The Penn/RESIST/Peradeniya War Problems Questionnaire (PRPWPQ; Jayawickreme et al., 2009, 2012)
The PRPWPQ is a Tamil language questionnaire that assesses a wide range of war-related problems experienced by Sri Lankans living in the North and East of the country. The questionnaire was developed through the coding of 604 individual interviews conducted in North-Eastern Sri Lanka (see Jayawickreme et al., 2009 for more details on measure development).
The PRPWPQ is comprised of three sections that measure 1) Trauma Exposure, 2) War-Related General Problems and 3) War-Related Psychological and Behavioral Problems (WRPBP). The Trauma Exposure section consists of two sub-sections, torture and other war trauma, and focuses on 22 different traumatic experiences (see Table 1). The War-Related General Problems section consists of five sub-sections: family problems (20 items), economic problems (10 items), social problems (26 items), lack of basic needs (9 items) and physical problems (19 items). The WRPBP section consists of three sub-sections: anxiety, depression and negative cognitions. In the Trauma Exposure section, participants indicate whether they have experienced the trauma in question, and if so, indicate the number of times they had experienced that trauma. In the War-Related General Problems section, participants indicate whether or not they have the problem in question. In the WRPBP section, participants rate the severity of problems ranging from 1 (not at all) to 4 (extremely). The questionnaire mostly included culturally specific expressions of general anxiety and depression symptoms (e.g., “Inability to make decisions [not knowing what to talk & what not to talk]”) as well as a few unique idioms of distress (e.g., “Not being able to work with a peaceful mind”). These items are grouped into three sub-scales: an Anxiety subscale and two depression subscales named Depression and Negative Perception (see Jayawickreme et al., 2012 for how these subscales were identified). Only the Anxiety and Depression subscales have been shown to predict functional impairment in this population (Jayawickreme et al., 2012), so the Negative Perception subscale was not used in the current study.
Table 1.
Experienced Trauma as assessed by the Trauma Exposure section of the Penn/RESIST/Peradeniya War Problems Questionnaire (n = 337)
| Percentage who endorsed this item (%) | |
|---|---|
| Witnessed the injury of loved ones | 47.5 |
| Witnessed the death of loved ones | 44.5 |
| Torture (Beaten or electrocuted in detention; force-fed a mosquito coil; beaten with a bag containing gasoline; pricked under nails; burnt with cigarette) | 38.9 |
| Being imprisoned | 35.9 |
| Family members kidnapped | 30 |
| Death of family members due to war | 24.9 |
| Family members handicapped | 13.4 |
| Being kidnapped | 12.5 |
| Caught in a land mine | 3.3 |
| Being raped | 1.2 |
A number of PRPWQ items that represent similar phenomena were collapsed together to create composite variables. For the trauma and stressful event variables, new binary composite variables were created; for example, “Being dependent on relatives” and “Being dependent on wife” were transformed into a new composite variable, “Dependent on Family.”) For symptoms of psychopathology, the mean score of similar items was calculated to create a new composite variable. A total of 68 individual items were collapsed into 25 new composite variables. For a list of composite variables and the individual items that they are comprised of, see Supplementary Table 1. Further, in order to aid interpretation of the networks, variables that were endorsed by fewer than 30 participants (9% of the sample) were not incorporated in the network analyses.
Data Analysis
Percentage of individuals who experienced specific traumas, stressful life events and symptoms of psychopathology
We calculated the percentage of individuals who experienced specific traumas, stressful life events and symptoms of psychopathology as measured by the PRPWPQ. For the purposes of describing percentage endorsement only, participants who endorsed specific symptoms on the WRPBP section of the PRPWPQ as either “quite a bit” (a score of 3) or “extremely” (4) were considered to have that particular symptom. Means and standard deviations for symptoms on the WRPBP section of the PRPWPQ were also calculated.
Association network
In an association network, each edge represents the zero-order correlation between two nodes. We created a matrix of zero-order correlations that reflected Pearson correlation coefficients between all stressful life events, traumatic events, and symptoms of psychopathology and used the R package qgraph (Epskamp, Cramer, Waldorp, Schmittmann, & Borsboom, 2012), to create a visualization of this network. Stressful life events, traumatic events, and symptoms of psychopathology were nodes in the network, and zero-order correlations between variables were ties (i.e., edges) connecting nodes. The Fruchterman and Reingold (1981) algorithm within qgraph placed nodes with stronger correlations between them closer to the center of the network and nodes with weaker correlations further from the center. Due to the large size of the network and consistent with previous work (McNally et al., 2015), we suppressed correlations with effect size less than r = |.30| from the visualization.
Concentration network
In a concentration network, edges depict partial correlations, i.e., correlations between nodes after statistically controlling for all other associations in the network. These networks can illuminate potential causal pathways between nodes (Epskamp & Fried, 2016) and have increasingly been used to model symptoms of psychopathology (Armour et al., 2017; McNally et al., 2015). However, these networks include very small partial correlations between nodes—false positives that are not likely to represent potential causal pathways. In order to reduce the number of these edges, we used the graphical least absolute shrinkage and selection operator (GLASSO) procedure (Tibshirani, 1996) in R package qgraph – a newly established approach for reducing small edges to zero (Epskamp & Fried, 2016), We estimated partial correlations between all stressful life events, traumatic event types, and symptoms using the lavaan package in R which detects ordinal and continuous variables and calculates Pearson, polychoric, and polyserial correlations as appropriate. We set the EBIC hyperparameter to 0.5, which is recommended in order to create a more parsimonious network with greater specificity (Barber & Drton, 2015). The Fruchterman and Reingold (1981) algorithm again placed nodes with stronger correlations between them closer to the center of the network. To assess the accuracy and stability of this network using procedures described by Epskamp, Borsboom, and Fried (2016), we utilized the R package bootnet (Epskamp, 2015). To assess the accuracy of the network edges, we computed 95% confidence intervals of the edges using bootstrapping techniques. To assess stability of the centrality indices, we compared centrality values derived from the original sample to centrality values derived from increasingly smaller bootstrapped subsamples. This also allows calculation of a correlation stability coefficient, which indicates the highest proportion of cases that can be dropped from the sample while preserving a correlation of r = 0.70 or greater between the original and bootstrapped centrality indices.
Node centrality
We used the R package qgraph to measure three types of centrality for each node within both association and concentration networks: betweenness, closeness, and strength. Betweenness represents how often a node falls on the shortest path between pairs of nodes in the network—i.e., the degree to which a given problem, event, or symptom connects other problems, events, or symptoms. Closeness represents the inverse of the mean shortest distance between a particular node and all other nodes in the network—i.e., the greater the closeness, the greater the proximity between a particular problem, traumatic event, or symptom and all other problems, events, and symptoms. Strength represents the sum of correlations between a node and adjacent nodes—i.e., a measure of the number and magnitude of edges connected to the node. Centrality values were normalized on a scale of 0–1 to facilitate interpretation.
Results
Trauma Exposure
The percentage of participants who experienced specific traumatic events can be found in Table 1. Commonly experienced traumas included witnessing the injury of loved ones (47.5%), witnessing the death of loved ones (44.5%), torture (38.9%), and being imprisoned (35.9%).
Stressful Life Events
The percentage of participants who experienced specific stressful life events can be found in Table 2. The vast majority of participants indicated having economic problems, with all six of the items pertaining to this set of problems being endorsed by at least 73% of participants or more. Furthermore, a majority of participants indicated experiencing a lack of five out of the nine assessed basic needs (i.e., clothes, rights, medical help, food and security). Common family problems included strain caused by family members (54.9%), insufficient support from relatives (48.7%), child care stress (48.4%) and no steady life because of duties towards family (46.6%). Common social problems included fear of death (65.6%), inability to travel (63.5%), stress due to relocation (58.2%), being alone (55.8%), fear of being kidnapped (49.3%), and not being able to talk freely (46%). Common physical problems included aches (73.3%), headaches (64.4%) and shivering (41.8%).
Table 2.
War-Related General Problems as assessed by the War-Related General Problems section of the Penn/RESIST/Peradeniya War Problems Questionnaire (n= 337)
| Percentage who endorsed this item (%) | |
|---|---|
| Family Problems | |
| Family member strain | 54.9 |
| Insufficient support from relatives | 48.7 |
| Child care stress | 48.4 |
| No steady life because of duties towards family | 46.6 |
| Dependent on family | 27.9 |
| Unable to get children married/give dowry | 26.7 |
| Lack of caretakers | 23.7 |
| Problems with marriage plans | 11 |
| Alcohol abuse by family members | 10.7 |
| Alcohol abuse by self | 9.2 |
| Not having any children though wanted to have them | 7.4 |
| Economic Problems | |
| Unable to work | 93.8 |
| Lack of money | 91.4 |
| Loss of material goods | 86.1 |
| Financial debt | 82.8 |
| Loss of house/land | 77.2 |
| Loss of work equipment | 73 |
| Social Problems | |
| Fear of death (from bombs/land mines/armed groups) | 65.6 |
| Inability to travel | 63.5 |
| Stress due to relocation | 58.2 |
| Being alone | 55.8 |
| Fear of being kidnapped | 49.3 |
| Not being able to talk freely | 46 |
| Not having official documents | 33.5 |
| Living with others | 32 |
| Isolated from society | 31.8 |
| Unable to participate in cultural events | 21.1 |
| Not cared for by society | 19.6 |
| Having to give bribes to get basic services | 16.9 |
| Living in a camp | 11 |
| Not being able to get married | 7.4 |
| Problems with neighbors or others in the camp | 6.2 |
| Fear of sexual abuse due to being a widow | 5.9 |
| Unable to get married due to stigma | 3.3 |
| Lack of Basic Needs | |
| Lack of proper security | 62.3 |
| Losing your rights | 59.9 |
| Lack of medical facilities | 59.9 |
| Lack of food | 54.9 |
| Lack of clothes | 53.4 |
| Lack of fuel | 49 |
| Not being able to obtain education | 40.1 |
| Lack of water | 34.4 |
| Problems in maintaining cleanliness | 30.9 |
| Physical Problems | |
| Aches | 73.3 |
| Headaches | 64.4 |
| Shivering | 41.8 |
| Cardiovascular problems | 33.8 |
| Eye problems | 33.5 |
| Limb problems | 32.3 |
| War injuries | 21.1 |
| Loss of teeth | 17.8 |
| Burns/boils | 15.4 |
| Fractures | 14.8 |
| Being deaf | 10.1 |
| Head injury | 10.1 |
| Kidney problems | 7.1 |
| Loss of arms or legs of a child or spouse or breadwinner due to landmine | 4.2 |
Symptoms of Psychopathology
The percentage of participants who endorsed specific symptoms of psychopathology as well as the means and standard deviations of those symptoms can be found in Table 3. Symptoms of psychopathology were very common, with the most widely seen symptoms including thinking a lot about the past (54.6%), not being able to sleep (51.6%), expressing harsh emotions when reminded of the past (47.8%), feeling fearful due to traumatic memories (47.8%), and fear for the future (47.5%).
Table 3.
Anxiety and depression symptoms as assessed by the Anxiety and Depression subscales of the Penn/RESIST/Peradeniya War Problems Questionnaire (n= 337)
| Item | Mean | SD | Percentage who endorsed either a “3” (“Quite a Bit”) or a “4” (“Extremely”) for this item (%) |
|---|---|---|---|
| Anxiety | |||
| Thinking a lot about my past (old memories), causing psychological confusion | 2.6 | .92 | 54.6 |
| Expressing harsh emotions when remembering bad things that have happened in the past | 2.35 | .97 | 47.8 |
| Feeling fearful due to images/memories of past traumatic events that come into your head when you don’t want them to | 2.42 | .95 | 47.8 |
| Fear for the future | 2.6 | .84 | 47.5 |
| Affected mental state | 2.4 | .90 | 45.1 |
| Afraid of being with strangers | 2.29 | .98 | 42.8 |
| Being afraid of everything (i.e., being easily scared) | 2.21 | .96 | 39.8 |
| Physical discomfort/tension due to fearfulness | 2.2 | .96 | 39.8 |
| Being extremely agitated/being in a panic situation | 2.19 | .94 | 38.3 |
| Afraid of going out alone | 2.2 | .96 | 38 |
| Not visiting the nearby relatives or friends | 1.98 | .89 | 30.6 |
| Not trusting others | 2.18 | .94 | 28.7 |
| Avoidance due to fear | 2.22 | .80 | 28.6 |
| Depression | |||
| Not being able to sleep | 2.46 | .84 | 51.6 |
| Disappointed in life | 2.34 | .97 | 46 |
| Having memory difficulties | 2.39 | .88 | 45.7 |
| Difficulty in concentrating | 2.34 | .87 | 44.8 |
| Lack of peace of mind | 2.39 | .85 | 44.5 |
| Feelings of frustration | 2.24 | .92 | 42.7 |
| Inability to make decisions (not knowing what to talk and what not to talk) | 2.2 | .91 | 37.7 |
| No happiness | 2.38 | .80 | 36.4 |
| Unstable mind/fluctuations in mind | 2.2 | .88 | 36.2 |
| Feeling unable to pass even one day | 2.11 | .94 | 33.5 |
| Negative changes in the good behavior one had Earlier | 1.96 | .91 | 28.4 |
| Irresponsibility/carelessness/impatience | 1.84 | .86 | 22.9 |
Node Type
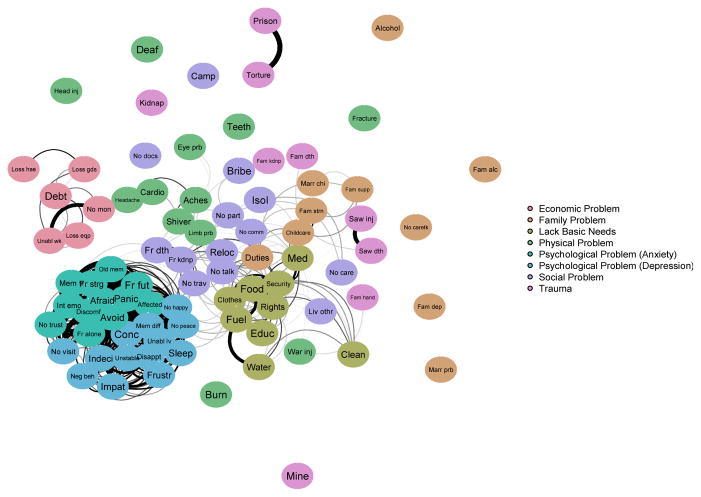
As presented in the association network depicted in Figure 1, in general, nodes of the same type tended to cluster together. Symptoms were all tightly clustered and associated with each other. All lack of basic needs nodes were also tightly clustered with each other, as were all economic problems. With regard to location of nodes within the network, social problems and lack of basic needs appeared relatively central in the network, in contrast to family problems, economic problems, or traumatic events. To facilitate interpretation of the figures in this paper, descriptions of node abbreviations are included in Table 6.
Figure 1.
Association network with ties (i.e., edges) representing zero-order correlations greater than r = |.30| between nodes. Dashed edges represent negative correlations, and edge thickness corresponds to the magnitude of the correlation
Table 6.
Descriptions Corresponding to Variable Abbreviations
| Abbreviation | Variable Description |
|---|---|
| Aches | aches |
| Affected | affected mental state |
| Afraid | being afraid of everything (i.e., being easily scared) |
| Agitated | being extremely agitated/being in a panic situation |
| Alcohol | alcohol abuse by self |
| Avoid | avoidance due to fear |
| Bribe | having to give a bribe in order to get basic needs or services |
| Burn | burns/boils |
| Camp | living in a camp |
| Cardio | cardiovascular problems |
| Childcare | child care stress |
| Clean | problem maintaining cleanliness |
| Clothes | lack of clothes |
| Conc | difficulty in concentrating |
| Deaf | being deaf |
| Debt | financial debt |
| Disappt | disappointed in life |
| Discomf | physical discomfort/tension due to fearfulness |
| Duties | not being able to reach a steady life because of duties towards family |
| Educ | not being able to obtain education |
| Eye prb | eye problems |
| Fam alc | alcohol abuse by family |
| Fam dep | dependent on family |
| Fam dth | death of family members due to war |
| Fam hand | family members handicapped |
| Fam kdnp | family members kidnapped |
| Fam strn | family member strain |
| Fam supp | insufficient support from relatives |
| Food | lack of food |
| Fr alone | afraid of going out alone |
| Fr dth | fear of death (from bombs/land mines/armed groups) |
| Fr fut | fear for the future |
| Fr kdnp | fear of being kidnapped |
| Fr strg | afraid of being with strangers |
| Fract | Fractures |
| Frustr | feelings of frustration |
| Fuel | lack of fuel |
| Head inj | head injury |
| Headache | Headache |
| Impat | irresponsibility/carelessness/impatience |
| Indeci | inability to make decisions (not knowing what to talk, what not to talk) |
| Int emo | expressing harsh emotions when remembering bad things from the past |
| Isol | isolation |
| Kidnap | being kidnapped |
| Limb prb | limb problems |
| Liv othr | living with others |
| Loss eqp | loss of work equipment |
| Loss gds | loss of material goods |
| Loss hse | loss of house/land |
| Marr chi | not being able to get children married or to give dowry |
| Marr prb | problems in marriage plans |
| Med | lack of medical facilities |
| Mem diff | having memory difficulties |
| Mem tr | feeling fearful due to unwanted images of trauma that come to mind |
| Mine | caught in a land mine |
| Neg beh | negative changes in the good behavior one had earlier |
| No care | not cared for by society |
| No caretk | lack of caretakers |
| No comm | being alone |
| No docs | not having needed documents (e.g., identity card) |
| No happy | no happiness |
| No mon | lack of money |
| No part | not being able to participate in cultural events (e.g., weddings, temples) |
| No peace | lack of peace of mind |
| No talk | not being able to talk freely |
| No trav | inability to travel |
| No trust | not trusting others |
| No visit | not visiting nearby relatives or friends |
| Old mem | thinking a lot about past (old memories), causing confusion |
| Prison | being imprisoned |
| Reloc | stress due to relocation |
| Rights | losing rights |
| Saw dth | witnessed the death of loved ones |
| Saw inj | witnessed the injury of loved ones |
| Security | lack of proper security |
| Shiver | Shivering |
| Sleep | not being able to sleep |
| Teeth | loss of teeth |
| Tort | torture |
| Unabl lv | feeling unable to pass even one day |
| Unabl wk | unable to work |
| Unstable | unstable mind/fluctuations in mind |
| War inj | war injuries |
| Water | lack of water |
For the association network, mean betweenness, closeness, and strength by node type are included in Table 4. Symptoms of psychopathology possessed the highest betweenness, closeness, and strength centrality as compared to other node types. In contrast, traumatic events had the lowest values across all three types of centrality relative to other node types. However, one-way ANOVA permutation tests confirmed that of the three types of centrality, only closeness and strength significantly varied by node type (betweenness: p > .05; closeness: p < .001; strength: p < .001). Pairwise permutation tests confirmed significant differences between node types, as reported in Supplementary Tables 2, 3, and 4. Anxiety symptoms had significantly higher closeness than all other node types except for depression symptoms, and depression symptoms had significantly higher closeness than all other node types except for anxiety symptoms and lack of basic needs. Lack of basic needs and social problems also had significantly greater closeness than traumatic events and all other stressors, i.e., family problems, economic problems, and physical problems. These findings are illustrated in Figure 1, where symptoms, lack of basic needs, and social problems appear most central in the network and proximal to many other nodes. With regard to strength centrality, there was a very similar pattern of results. Anxiety and depression symptoms possessed significantly greater strength than all other node types, as did lack of basic needs and social problems when compared to traumatic events and all other stressors. This can be seen in Figure 1, in which symptoms, lack of basic needs, and social problems are densely connected to nodes of the same type.
Table 4.
Descriptive Statistics for Association Network Centrality Measures by Node Type
| Betweenness | Closeness | Strength | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| M | (SD) | M | (SD) | M | (SD) | |
| Economic Problem | 0.065 | (0.037) | 0.650 | (0.048) | 0.469 | (0.079) |
| Family Problem | 0.081 | (0.114) | 0.659 | (0.154) | 0.421 | (0.178) |
| Lack of Basic Need | 0.118 | (0.094) | 0.850 | (0.083) | 0.662 | (0.133) |
| Physical Problem | 0.066 | (0.098) | 0.677 | (0.099) | 0.460 | (0.126) |
| Symptom (Anxiety) | 0.179 | (0.174) | 0.928 | (0.046) | 0.887 | (0.083) |
| Symptom (Depression) | 0.142 | (0.276) | 0.902 | (0.053) | 0.825 | (0.104) |
| Social Problem | 0.125 | (0.186) | 0.794 | (0.119) | 0.597 | (0.152) |
| Trauma | 0.056 | (0.011) | 0.626 | (0.070) | 0.383 | (0.097) |
Note: Centrality values are scaled relative to the largest value.
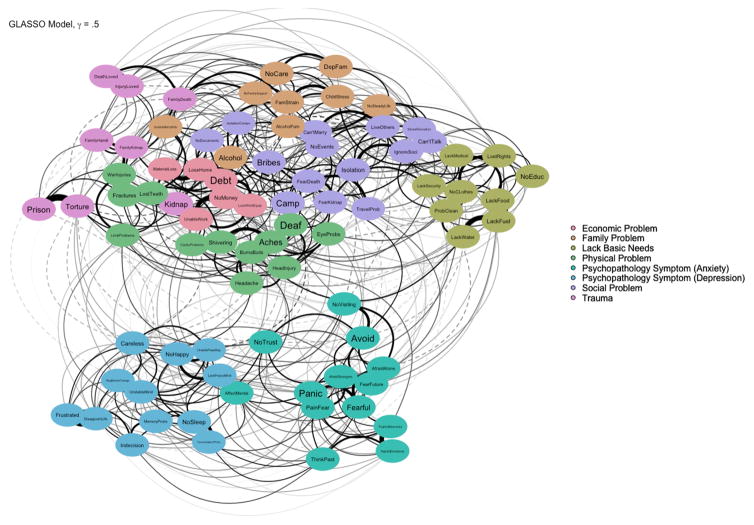
The concentration network is depicted in Figure 2. Similar to the association network, nodes of the same type tended to cluster together. However, symptoms were less tightly clustered together, and there were more connections between stressors or traumatic events and symptoms—representing potential causal pathways between these nodes.
Figure 2.
GLASSO network with ties (i.e., edges) representing partial order correlations between nodes. Dashed edges represent negative correlations, and edge thickness corresponds to the magnitude of the correlation.
Mean betweenness, closeness, and strength by node type for the concentration network are included in Table 5. In contrast to the association network, social problems in had elevated betweenness, strength, and closeness centrality compared to other node types. However, one-way ANOVA permutation tests confirmed that, of each of the three types of centrality, only closeness significantly varied by node type (betweenness: p > .05; closeness: p < .001; strength: p > .05). Pairwise permutation tests reported in Supplementary Tables 5, 6, and 7 confirmed that social problems had significantly greater closeness than traumatic events, family problems, and symptoms. Symptoms had significantly lower closeness than all other node types. This is illustrated in Figure 2, wherein social problems are located near each of the other types of stressors and symptoms are not proximal to other node types. Thus, the relative prominence of social problems in concentration networks indicates that once partial-correlations between nodes were represented – controlling for correlations between all other variables and eliminating third variable correlations – social problems were particularly central to the network.
Table 5.
Descriptive Statistics for GLASSO Centrality Measures by Node Type
| Betweenness | Closeness | Strength | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| M | (SD) | M | (SD) | M | (SD) | |
| Economic Problem | 0.152 | (0.052) | 0.819 | (0.014) | 0.760 | (0.105) |
| Family Problem | 0.137 | (0.118) | 0.779 | (0.045) | 0.660 | (0.158) |
| Lack of Basic Need | 0.157 | (0.096) | 0.801 | (0.057) | 0.713 | (0.136) |
| Physical Problem | 0.173 | (0.114) | 0.830 | (0.054) | 0.660 | (0.122) |
| Symptom (Anxiety) | 0.163 | (0.168) | 0.708 | (0.063) | 0.671 | (0.090) |
| Symptom (Depression) | 0.135 | (0.152) | 0.670 | (0.066) | 0.659 | (0.094) |
| Social Problem | 0.217 | (0.265) | 0.852 | (0.059) | 0.750 | (0.103) |
| Trauma | 0.109 | (0.068) | 0.783 | (0.052) | 0.692 | (0.091) |
Note: Centrality values are scaled relative to the largest value.
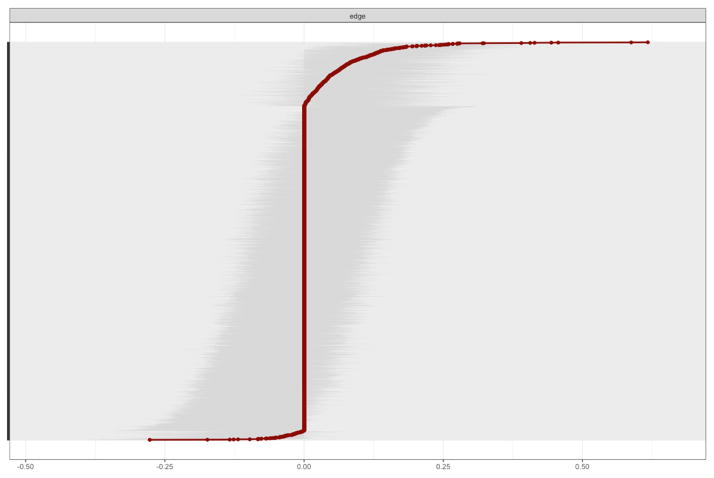
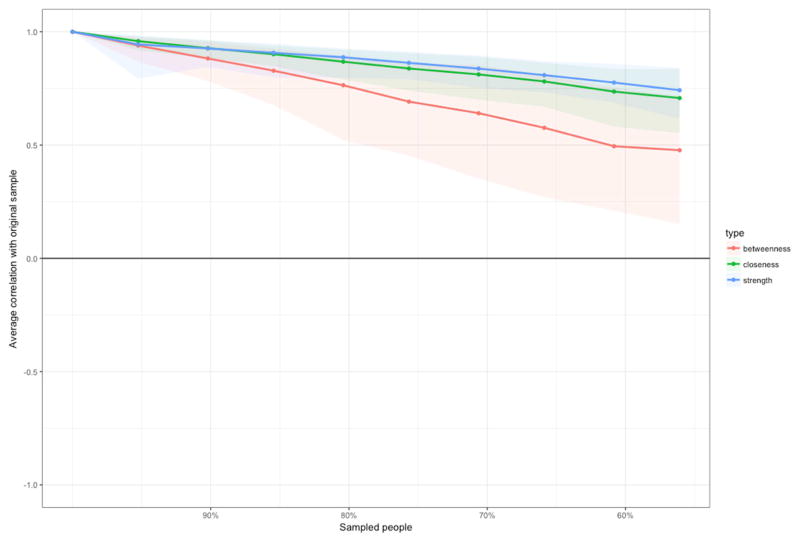
Concentration Network Accuracy and Stability
With regard to accuracy of the concentration network, the bootstrapped confidence intervals for the edge values are represented in Figure 4. The relatively wide and overlapping confidence intervals suggest that the magnitude of the edge values should be interpreted cautiously. With regard to network stability, the average correlations between centrality values from the original sample and centrality values from increasingly smaller bootstrapped subsamples are represented in Figure 3. The correlation stability coefficient –which indicates the highest proportion of cases that can be dropped from the sample while preserving a correlation of r = 0.70 or greater between the original and bootstrapped centrality values – was 0.145 for betweenness, 0.294 for closeness, and 0.341 for strength. Guidelines state that these coefficients should preferably be above 0.50 but not below 0.25 (Epskamp et al., 2016), indicating that the closeness and strength centrality indices meet the minimum requirement for stability but that differences in centrality between nodes should not be over-interpreted (Armour et al., 2017).
Figure 4.
Bootstrapped 95% confidence intervals for estimated GLASSO network edge values. The red line represents the edge values, and the gray regions indicate the confidence intervals
Figure 3.
Average correlations between original centrality indices of the GLASSO network and centrality indices after dropping increasing percentages of participants from the sample.
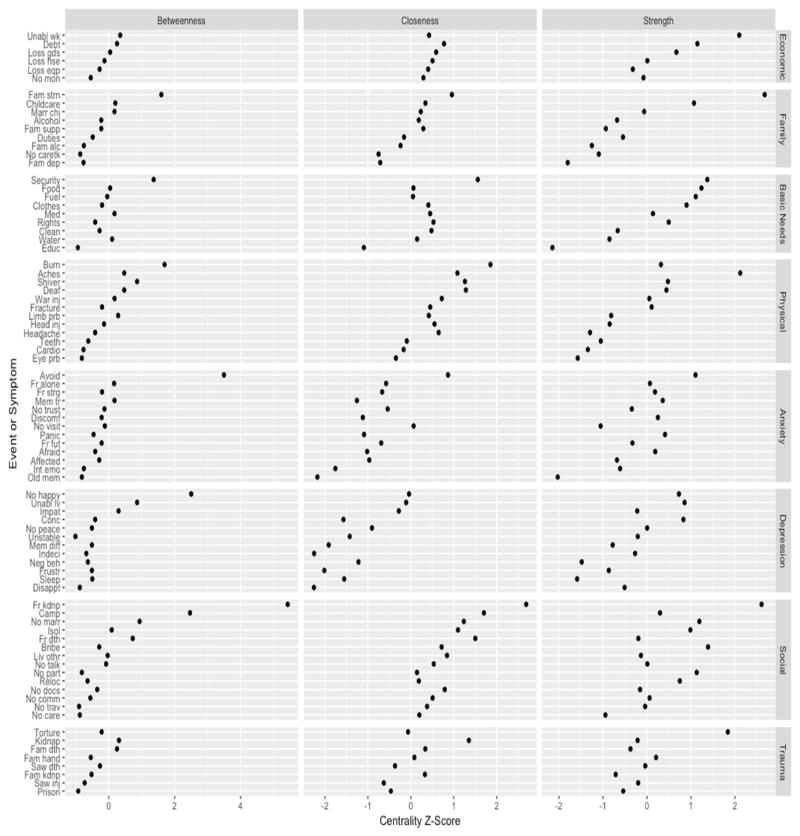
Individual Nodes
Figures 5 and 6 depict the standardized centrality values of individual nodes within the association and concentration networks, respectively. Due to poor stability of the betweenness centrality indices in the concentration network, we will focus on individual nodes with high closeness or strength centrality.
Figure 5.
Standardized centrality scores from association network.
Figure 6.
Standardized centrality scores from GLASSO network.
Nodes with high closeness are proximal to many other nodes in the network and thus may signal that other problems are present. In terms of stressors and traumatic events, in the current study these included fear of being kidnapped (Fr kdnp), experiencing burns or boils (Burn), living in a camp (Camp), lack of proper security (Security), and fear of death, such as facing bombs, land mines, or armed groups (Fr dth). Symptoms with highest closeness included anxiety symptoms of avoidance due to fear (Avoid) and not visiting nearby relatives or friends (No Visit) and depressive symptoms of lack of happiness (No Happy), feeling unable to live even one day, (Unable lv), and impatience (Impat).
Nodes with high strength are strongly linked to multiple other nodes and represent those that tend to co-occur with other nodes. For stressors or traumatic events, these included strain caused by family members (Fam strn), fear of being kidnapped (Fr kdnp), experiencing bodily aches (Aches), being unable to work (Unabl wk), and experiencing torture (Torture). With regard to symptoms with highest strength, these were the same as the ones with greatest closeness, described above.
Discussion
In the current study, we used network analysis – a novel statistical method that conceptualizes emotional distress as stemming from a system of interacting problems – and locally developed measures to better understand the dynamic interaction between traumatic events, stressful life events and symptoms of psychopathology in survivors of war in Sri Lanka. In the association network (which consisted of zero-order correlations between the different variables), symptoms of psychopathology, problems pertaining to lack of basic needs, and social problems were central, in contrast to traumatic events and all other types of stressors (family problems, economic problems, and physical problems). The concentration network indicated that social problems in particular were the most central, significantly more so than traumatic events and family problems, after controlling for shared association. Inspection of the visualization of the concentration network (Figure 2) provides some guidance in interpreting these findings. Social problems are situated between each of the other types of problems in the network, with traumatic events and family problems positioned towards the periphery of the network.
These findings echo holistic theoretical approaches to examining traumatic events, stressors, and distress that provide for complex interactions between them. That there were clusters of multiple types of nodes that appeared to reinforce each other is consistent with the theoretical loss spirals in COR theory (Hobfoll, 2001). That social problems were so central to the network supports the psychosocial emphasis on daily stressors being mediators of the effects of trauma on mental health (Miller & Rasmussen, 2010; 2014; 2017). Whether this is because traumatic events set off chains of stressors or because those exposed to trauma are more likely to rate problems as more stressful and perhaps even generate problems (Neuner, 2010) is subject to some debate, and not likely solved here. Nevertheless, we believe that these findings provide network science support that joins other data gleaned from more conventional approaches to stressors and trauma supporting holistic theoretical approaches (Fernando et al., 2010; Jordans, Semrau, Thornicroft, & van Ommeren, 2014; Newnham, Pearson, Stein, & Betancourt, 2015; Rasmussen et al., 2010), and is in line with the guidelines of numerous aid organizations that recommend psychosocial professionals consider both trauma exposure and daily stressors as precipitating factors among their beneficiaries (Medicins Sans Frontiers, 2005; Inter-Agency Standing Committee, 2007).
When we looked at the centrality of specific trauma and stressful life events in the concentration network, fear of being kidnapped was found to be a key event that was often highly proximal to other nodes in the network and strongly linked to multiple other nodes, as indicated by their high scores on two measures of centrality, closeness and strength. The centrality of this concern reflects a horrifying reality of constant threat and overwhelming fear. This finding is consistent with previous findings from Sri Lanka. Jayasuirya, Jayasuriya, Tay and Silove (2016) collected data from a representative sample of Sri Lankans and concluded that helping individuals with threat or protection issues would significantly reduce mental suffering in post-war Sri Lanka. In addition, experiencing burns or boils, living in a camp, lack of proper security and fear of death were found to have high closeness centrality, indicating that these variables are relatively close to other variables in the network. Strain caused by family members, experiencing bodily aches, being unable to work and torture had high strength centrality, suggesting that these variables co-occur with many other variables in the network.
Avoidance due to fear, not visiting nearby relatives, lack of happiness, feeling unable to live even one day and impatience emerged as key symptoms of psychopathology in the network, with high scores of closeness and strength centrality. The fact that three items measuring avoidance and emotional numbing symptoms– i.e., avoidance due to fear, not visiting nearby relatives, lack of happiness – were highly central to the network is striking, given that avoidance and emotional numbing symptoms have not always been shown to be especially salient in non-Western contexts (Hinton & Lewis Fernandez, 2011) and particularly in non-Western emergency settings (Rasmussen, Keatley, & Joscelyne, 2014). These results indicate that at least in the Sri Lankan context, avoidance/numbing symptoms are closely associated to, and co-occur with many other symptoms, stressors and traumas.
The current results suggest that network analysis provides researchers and practitioners alike with an intelligible map of the dynamic between traumatic events, symptoms and stressful life events in post-war societies. Such an approach allows one to identify those problems that are not especially impactful in a particular context and to highlight a finite set of focus points for possible intervention. For example, our analyses indicated that individuals living in war-affected areas of Sri Lanka who experienced a particular subset of traumatic events, stressful life events and symptoms of psychopathology are more likely to have experienced other traumas and to be struggling with multiple stressors and symptoms. Given that governments, international agencies and local agencies assisting survivors of conflict and disaster often have limited funds for psychosocial services (Saxena, Thornicroft, Knapp, & Whiteford, 2007), knowing which of the multiple war-related problems are both frequent and associated with others is essential if one is to use the resources at hand most efficiently. Problems with high betweenness centrality thus may be key targets for intervention; in other words, removing them may disrupt the causal chain between other problems in the network. Problems with high closeness centrality are the most proximal to other problems in the network and may thus facilitate identifying efficacious opportunities for intervention.
Different war contexts in different cultures would likely produce different networks of problems. Hinton and Good (2016) draw on their empirical work with Cambodian refugees in the United States (e.g., Hinton, Nickerson, & Bryant, 2011) to argue that symptoms of psychological distress interact with contextual variables such as daily stressors to create syndromes of mental illness that are specific to specific locales and cultures. Thus, networks of problems will need to be identified in specific post-war contexts before specific problems can be targeted with interventions. It is possible that as more studies on the networks of problems in post-war contexts are conducted, we will observe that certain problems tend to be central across different cultures and contexts.
Future studies examining war survivors can also broaden their focus beyond examining networks between traumatic events, daily stressors and symptoms of psychology and investigate the role of particular psychological variables that have been hypothesized to impact mental health (Jones, Heeren, & McNally, 2017). For example, selective optimization with compensation (SOC) theory (Baltes & Baltes, 1990) posits that individuals use three particular behavioral strategies, namely selection, optimization and compensation, to maintain their health in the face of stress and change. According to SOC theory, individuals select their own goals, optimize the use of resources to attain those goals and compensate for a lack of resources by using what resources they have effectively or identifying new resources. Network science could examine the relationship between these three behavioral strategies, traumas, daily stressors and symptoms of psychopathology, and determine if use of these strategies are indeed effective in managing the often horrifying post-war environment.
The current study has a number of limitations. First, the data in the current study were cross-sectional, limiting our ability to determine the direction of the relationships between various problems. For example, it is unclear from the current analyses whether tension due to war causes one to feel unable to live due to trauma or vice versa. Longitudinal studies would allow one to create directed networks and so better estimate the direction of the relationships between different problems (Fried et al., 2017). However, in order to fully establish cause-and-effect relationships between problems, experimental studies are needed that intervene in a particular problem area and then measure the impact the intervention has on other problems in the network. Second, we measured stressful life events using a binary scale; participants simply had to indicate if they had a particular stressor or not. Use of a Likert scale would have allowed for a more sensitive measurement of stressful life events and may have resulted in a different network structure. Third, the modest stability of the centrality indices calls for caution in interpreting differences between individual nodes. Finally, even though our sample drew from survivors from different parts of the country that were affected by the civil war (i.e., Jaffna, Batticaloa, Trincomalee, Vavuniya, and Nallur), all participants were survivors who sought psychosocial assistance at clinics run by a specific local non-governmental organization. This may limit the generalizability of the current results to the broader Sri Lankan population living in areas affected by the civil war.
Nevertheless, the current study expands our understanding of the dynamic relationship between experienced trauma, daily stressors and symptoms of psychological distress in post-war settings by using measures developed specifically for the local context in a network science framework. Network analysis presents the opportunity to identify whether symptoms of psychological distress interact with contextual factors such as daily stressors to create culturally specific networks of problems. Network approaches allow us to identity key variables, whether they be symptoms of mental distress or daily stressors, that appear to be central to the network; in other words, their presence substantially increases the likelihood of the presence of the other symptoms and stressors. Such information promises to be of great utility to researchers and practitioners who are determining how to spend limited resources in the most impactful ways possible.
Supplementary Material
Uses network analysis to identify relations between problems in war survivors
Argues that network analysis can allow us to identity key problems in war survivors
Social problems are particularly key problems for Sri Lankan war survivors
Network analysis can be used to determine the best use of limited resources
Acknowledgments
This study was supported by funds from the Asia Foundation, the Science Directorate of the American Psychological Association and the Positive Psychology Center, University of Pennsylvania. Partial support came from a Eunice Kennedy Shriver National Institute of Child Health and Human Development research infrastructure grant, R24 HD042828, to the Center for Studies in Demography & Ecology at the University of Washington.
The authors thank A. Sara Poovendran, Charmila Edirisinghe, and M.I.M.I. Hassan at the Family Rehabilitation Center in Sri Lanka for facilitating data collection, and Jeanine Guthrie at the Asia Foundation, Gameela Samarasinghe at PADHI (University of Colombo, Sri Lanka), and P. Prabu and Nadaraja Balasubramaniam at the Consortium for Humanitarian Agencies in Colombo for providing valuable advice at the initial stages of this project. We also thank three anonymous reviewers for their valuable feedback.
Footnotes
Portions of this article were presented at the 29th Annual Convention of the Association for Psychological Science, Boston, MA, May 2017.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Nuwan Jayawickreme, Manhattan College.
Candace Mootoo, Fordham University.
Christine Fountain, Fordham University.
Andrew Rasmussen, Fordham University.
Eranda Jayawickreme, Wake Forest University.
Rebecca F. Bertuccio, Manhattan College
References
- Armour C, Fried EI, Deserno MK, Tsai J, Pietrzak RH. A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in U.S. military veterans. Journal of Anxiety Disorders. 2017;45:49–59. doi: 10.1016/j.janxdis.2016.11.008. [DOI] [PubMed] [Google Scholar]
- Baltes PB, Baltes MM. Psychological perspectives on successful aging: The model of selective optimization with compensation. In: Baltes PB, Baltes MM, editors. Successful aging: Perspectives from the behavioral sciences. New York, NY: Cambridge University Press; 1990. pp. 1–34. [Google Scholar]
- Bolton P, Tang AM. An alternative approach to cross-cultural function assessment. Social Psychiatry and Psychiatric Epidemiology. 2002;37:537–543. doi: 10.1007/s00127-002-0580-5. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Cramer AOJ. Network Analysis: An Integrative Approach to the Structure of Psychopathology. Annual Review of Clinical Psychology. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. Toward an experimental ecology of human development. American Psychologist. 1977;32:513–531. [Google Scholar]
- De Schryver M, Vindevogel S, Rasmussen AE, Cramer AOJ. Unpacking constructs: A network approach for studying war exposure, daily stressors and post-traumatic stress disorder. Frontiers in Psychology. 2015;6:1896. doi: 10.3389/fpsyg.2015.01896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S. Bootnet: Bootstrap methods for various network estimation routines (R package version 0.2.) [Computer software] 2015 Retrieved from http://CRAN.R-project.org/package_bootnet.
- Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their stability: A tutorial paper. 2016:1–34. doi: 10.3758/s13428-017-0862-1. Arxiv Preprint (ID 160408045) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: Network visualization of relationships in psychometric data. Journal of Statistical Software. 2012;48:1018. [Google Scholar]
- Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. 2016:1–35. doi: 10.1037/met0000167. Arxiv Preprint (ID 1607.01367v5) [DOI] [PubMed] [Google Scholar]
- Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet. 2005;365:1309–1314. doi: 10.1016/S0140-6736(05)61027-6. [DOI] [PubMed] [Google Scholar]
- Fernando GA, Miller KE, Berger DE. Growing pains: The impact of disaster-related and daily stressors on the psychological and psychosocial functioning of youth in Sri Lanka. Child Development. 2010;81:1192–1210. doi: 10.1111/j.1467-8624.2010.01462.x. [DOI] [PubMed] [Google Scholar]
- Fried EI, van Borkulo CD, Cramer AOJ, Boschloo L, Schoevers RA, Borsboom D. Mental disorders as networks of problems: a review of recent insight. Social Psychiatry and Psychiatric Epidemiology. 2017;52:1–10. doi: 10.1007/s00127-016-1319-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber RF, Drton M. High-dimensional Ising model selection with Bayesian information criteria. Electronic Journal of Statistics. 2015;9(1):567–607. [Google Scholar]
- Fruchterman TMJ, Reingold EM. Graph drawing by force-directed placement. Software—Practice and Experience. 1991;21:1129–1164. [Google Scholar]
- Guttman LA. A general nonmetric technique for finding the smallest coordinate space for a configuration of points. Psychometrika. 1968;33:469–506. [Google Scholar]
- Harrison F. Still counting the dead: Survivors of Sri Lanka’s hidden war. London: Portobello; 2012. [Google Scholar]
- Hinton DE, Good BJ. The culturally sensitive assessment of trauma: Eleven analytic perspectives, a typology of errors, and the multiplex models of distress generation. In: Good BJ, Hinton DE, editors. Culture and PTSD: Trauma in global and historical perspective. Philadelphia, PA: University of Pennsylvania Press; 2016. pp. 50–113. [Google Scholar]
- Hinton DE, Lewis-Fernandez The cross-cultural validity of posttraumatic stress disorder: Implications for DSM-5. Depression and Anxiety. 2011;28:783–801. doi: 10.1002/da.20753. [DOI] [PubMed] [Google Scholar]
- Hinton D, Nickerson D, Bryant R. Worry, worry attacks, and PTSD among Cambodian refugees: a path analysis investigation. Social Science and Medicine. 2011;72:1817–1825. doi: 10.1016/j.socscimed.2011.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobfoll S. Conservation of resources theory: a new attempt and conceptualizing stress. American Psychologist. 1989;44(3):513–524. doi: 10.1037//0003-066x.44.3.513. [DOI] [PubMed] [Google Scholar]
- Hobfoll S. The influence of culture, community, and the nested-self in the stress process: advancing conservation of resources theory. Applied Psychology. 2001;50(3):337–369. [Google Scholar]
- Inter-Agency Standing Committee. IASC Guidelines on Mental Health and Psychosocial Support in Emergency Settings. Geneva: IASC; 2007. [DOI] [PubMed] [Google Scholar]
- Jayasuriya D, Jayasuriya R, Tay AK, Silove D. Associations of mental distress with residency in conflict zones, ethnic minority status, and potentially modifiable social factors following conflict in Sri Lanka: a nationwide cross-sectional study. Lancet Psychiatry. 2016;3:145–153. doi: 10.1016/S2215-0366(15)00437-X. [DOI] [PubMed] [Google Scholar]
- Jayawickreme E, Jayawickreme N, Miller E. Triumphalism, fear and humiliation: The psychological legacy of Sri Lanka’s civil war. Dynamics of Asymmetric Conflict. 2010;3:208–222. [Google Scholar]
- Jayawickreme N, Jayawickreme E, Atanasov P, Goonasekera MA, Foa EB. Are Culturally Specific Measures of Trauma-Related Anxiety and Depression Needed? The Case of Sri Lanka. Psychological Assessment. 2012;24:791–800. doi: 10.1037/a0027564. [DOI] [PubMed] [Google Scholar]
- Jayawickreme N, Jayawickreme E, Goonasekera MA, Foa EB. Distress, wellbeing and war: qualitative analyses of civilian interviews from north-eastern Sri Lanka. Intervention: International Journal of Mental Health, Psychosocial Work and Counselling in Areas of Armed Conflict. 2009;7:204–222. [Google Scholar]
- Jones L, Kafetsios K. Assessing adolescent mental health in war-affected societies: the significance of symptoms. Child Abuse & Neglect. 2002;26:1059–1080. [PubMed] [Google Scholar]
- Jones PJ, Heeren A, McNally RJ. Commentary: A network theory of mental disorders. Frontiers in Psychology. 2017;8:1305. doi: 10.3389/fpsyg.2017.01305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordans MJD, Semrau M, Thornicroft G, van Ommeren M. Role of current perceived needs in explaining the association between past trauma exposure and distress in humanitarian settings in Jordan and Nepal. British Journal of Psychiatry. 2014;201:276–281. doi: 10.1192/bjp.bp.111.102137. [DOI] [PubMed] [Google Scholar]
- Layne CM, Olsen JA, Baker A, Legershi JP, Isakson B, Pasalić A, Durakovic-Belko E, Dapo N, Campara N, Arsianagić B, Satlzman WR, Pynoos RS. Unpacking trauma exposure risk factors and differential pathways of influence: predicting postwar mental distress in Bosnian adolescents. Child Development. 2010;81:1053–1076. doi: 10.1111/j.1467-8624.2010.01454.x. [DOI] [PubMed] [Google Scholar]
- Mattock J. Resource loss and psychological distress: An application of the conservation of resources (COR) model to the 2004 Asian tsunami in Sri Lanka. Newcastle, UK: MSc Disaster Management & Sustainable Development; 2005. [Google Scholar]
- McNally RJ. The ontology of posttraumatic stress disorder: Natural kind, social construction, or causal system? Clinical Psychology: Science and Practice. 2012;19:220–228. [Google Scholar]
- McNally RJ, Robinaugh DJ, Wu GW, Wang L, Deserno MK, Borsboom D. Mental Disorders as Causal Systems A Network Approach to Posttraumatic Stress Disorder. Clinical Psychological Science. 2015;3:836–849. [Google Scholar]
- Medicins Sans Frontieres. Lightning Source UK. 2005. Mental Health Guidelines – A Handbook for Implementing Mental Health Programmes in Areas of Mass Violence. [Google Scholar]
- Miller KE, Rasmussen A. War exposure, daily stressors, and mental health in conflict and post-conflict settings: Bridging the divide between trauma-focused and psychosocial frameworks. Social Science and Medicine. 2010;70:7–16. doi: 10.1016/j.socscimed.2009.09.029. [DOI] [PubMed] [Google Scholar]
- Miller KE, Rasmussen A. War experiences, daily stressors and mental health five years on: Elaborations and future directions. Intervention: International Journal of Mental Health, Psychosocial Work and Counselling in Areas of Armed Conflict. 2014;12:33–42. [Google Scholar]
- Miller KE, Rasmussen A. The mental health of civilians displaced by armed conflict: an ecological model of refugee distress. Epidemiology and Psychiatric Science. 2017;26(2):129–138. doi: 10.1017/S2045796016000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH. Context and coping: Toward a unifying conceptual framework. American Journal of Community Psychology. 1984;12:5–36. doi: 10.1007/BF00896933. [DOI] [PubMed] [Google Scholar]
- Neuner F, Elbert T. The mental health disaster in conflict settings: can scientific research help? BMC Public Health. 2007;7:275. doi: 10.1186/1471-2458-7-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuner F. Assisting war-torn populations – Should we prioritize reducing daily stressors to improve mental health? Comment on Miller and Rasmussen (2010) Social Science and Medicine. 2010;71:1381–1384. doi: 10.1016/j.socscimed.2010.06.030. [DOI] [PubMed] [Google Scholar]
- Newnham EA, Pearson RM, Stein A, Betancourt TS. Youth mental health after civil war: The importance of daily stressors. British Journal of Psychiatry. 2015;206:116–121. doi: 10.1192/bjp.bp.114.146324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen A, Keatly E, Joscelyne A. Posttraumatic stress in emergency settings outside North America and Europe: A review of the emic literature. Social Science and Medicine. 2014;109:44–54. doi: 10.1016/j.socscimed.2014.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen A, Nguyen L, Wilkinson J, Vundla S, Raghavan S, Miller KE, Keller AS. Rates and impact of trauma and current stressors among Darfuri refugees in Eastern Chad. American Journal of Orthopsychiatry. 2010;80:227–236. doi: 10.1111/j.1939-0025.2010.01026.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370:878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- Schmittmann VD, Cramer AOJ, Waldorp LJ, Epskamp S, Kievit RA, Borsboom D. Deconstructing the construct: A network perspective on psychological phenomena. New Ideas in Psychology. 2013;31:43–53. [Google Scholar]
- Siriwardhana C, Adikari A, Pannala G, Siribaddana S, Abas M, Sumathipala A, Stewart R. Prolonged internal displacement and common mental disorders in Sri Lanka: The COMRAID Study. PLoS ONE. 2013;8:e64742. doi: 10.1371/journal.pone.0064742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somasundaram D, Sivayokan S. Rebuilding community resilience in a post-war context: Developing insight and recommendations – A qualitative study in Northern Sri Lanka. International Journal of Mental Health Systems. 2013;7 doi: 10.1186/1752-4458-7-3. Article 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tibshirani R. Regression shrinkage and selection via the lasso. Journal of the Royal Statistical Society. Series B (Methodological) 1996;58(1):267–288. [Google Scholar]
- United Nations High Commissioner for Refugees. Global trends: Forced displacement in 2015. Geneva, Switzerland: United Nations High Commissioner for Refugees; 2016. [Google Scholar]
- van Ommeren M, Saxena S, Saraceno B. Mental and social health during and after acute emergencies: Emerging consensus? Bulletin of the World Health Organization. 2005;83:71–75. [PMC free article] [PubMed] [Google Scholar]
- Vhurumuku E, Nanayakkara L, Petersson A, Kumarasiri RHWA, Rupasena LP. Food Security in the Northern and Eastern Provinces of Sri Lanka. Colombo, Sri Lanka: United Nations World Food Program; 2012. [Google Scholar]
- Witting AB, Lambert J, Wickrama T, Thanigaseelan S, Merten M. War and disaster in Sri Lanka: Depression, family adjustment and health among women heading households. International Journal of Social Psychiatry. 2016;62:425–433. doi: 10.1177/0020764016650213. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.