Abstract
Objectives. To assess whether the use of firearms explains rural–urban differences in suicide rates.
Methods. We performed a retrospective analysis on all 6196 well-characterized adult suicides in Maryland from 2003 through 2015. We computed rate ratios by using census data and then stratified by sex, with adjustment for age and race.
Results. Suicide rates were higher in rural compared with urban counties. However, the higher rural suicide rates were limited to firearm suicides (incident rate ratio [IRR] = 1.66; 95% confidence interval [CI] = 1.20, 2.31). Nonfirearm suicide rates were not significantly higher in rural settings. Furthermore, 89% of firearm suicides occurred in men and the higher rural firearm suicide rate was limited to men (IRR = 1.36; 95% CI = 1.09, 1.69). Women were significantly less likely to complete suicide in rural areas (IRR = 0.63; 95% CI = 0.43, 0.94), regardless of method.
Conclusions. Male firearm use drives the increased rate of suicide in rural areas. The opposite associations between urbanicity and suicide in men and women may be driven by the male preference for firearms as a method for committing suicide.
The suicide rate in the United States has risen to 13.3 deaths per 100 000 in 2015, the highest rate in 30 years, up from a nadir of 10.4 in 2000.1 Suicide rates are higher in rural counties than in urban ones, with rural rates in 2015 reaching as high as 19 per 100 000, compared with 11 per 100 000 in central urban settings.2 However, the reasons for this difference in rates remain elusive. The prevalence estimates of major depression and other common mental disorders are in fact lower in rural compared with urban settings.3,4 Differences in access to more lethal means may explain the increased suicide rate despite lower prevalence of mental illness. Firearms are one of the most lethal means of completing suicide,5 remain the most common method in the United States,2 and are typically more accessible in rural settings.6 Although firearm homicides are much more common in urban settings, firearm suicides have been found to predominate in rural areas.7 In a nonconcurrent prospective nationwide study of veterans from 2003 to 2007, McCarthy et al.8 found a greater than 20% higher suicide rate in rural areas, with the highest proportion utilizing firearms. Reports of higher suicide rates by firearms in rural than in urban areas are not unique to the United States. Studies in Canada, the United Kingdom, Australia, and India also indicate a similar pattern of urban–rural differences.9–14
This study contributes to the investigation of urban–rural variations in suicide in the United States and the role of firearms as a possible explanation for these variations. More specifically, we investigated urban–rural variations in completed suicides in Maryland from 2003 to 2015 segregated by suicide method. On the basis of past research, we hypothesized that the urban–rural variations in completed suicide can be explained by the use of firearms and, hence, that the urban–rural variations are limited to firearm suicides. We further conducted analyses to assess whether the urban–rural association with suicide and suicide by firearms is limited to specific sociodemographic groups or is uniform across the different population groups.
Maryland is especially suited for this study because it is one of the few states to utilize appointed medical examiners exclusively, as opposed to elected coroners, who may not be forensic pathologists. As a result, Maryland possesses uniform death investigations and autopsies performed under a set of standardized operating procedures. Previous studies have substantiated the greater accuracy of medical examiner determination of suicide death.15–18 Furthermore, unlike the rural communities in the less densely populated states, most of the rural communities in Maryland are in close proximity to urban and suburban areas. In this regard, Maryland rural communities may be considered more representative of rural communities in the more populated states and in the nation as a whole.
METHODS
We attained a complete listing of all 6875 suicides recorded in Maryland from 2003 through 2015 from the Office of the Chief Medical Examiner for the State of Maryland (OCME-MD). The OCME-MD evaluates all violent, sudden, suspicious, or unexpected deaths; deaths without a physician in attendance; and deaths in a penal institution in the State of Maryland. There were no significant changes in medical examiner investigative or recording procedures during the study period.
A board-certified psychiatrist (P. S. N.) reviewed 5% of these cases via police and OCME-MD reports, and then interviewed the chief medical examiner to confirm agreement with the OCME-MD definitions of suicide. From the OCME-MD records, we extracted age, sex, race/ethnicity (as defined by the OCME-MD), county of residence, method of suicide, and police reports.
Study Design
To examine urban versus rural setting, we assigned each case to county of residence. We chose to use county of residence instead of county of death because, although suicides may occur outside of the decedent’s home county, the county of residence often plays a greater role in a decedent’s life than the county where the body may be discovered. In a sensitivity analysis, the county of death was different from the county of residence with regard to urban–rural classification in only 1.08% of cases. County names and borders did not change in Maryland during our study period, making them more stable and useful than zip codes. Counties were categorized by urbanicity according to the US Department of Agriculture’s Rural–Urban Continuum Codes (RUCCs), which differentiate among 9 different categories of urbanicity on the basis of population size and adjacency to metropolitan areas, with the lowest category indicating the highest degree of urbanicity. Of Maryland’s 24 counties, 13 fall under RUCC category 1 (metro areas of more than 1 million population), 4 fall under category 2 (metro areas of 250 000 to 1 million population), 2 under category 3 (metro areas of < 250 000 population), and 5 under category 6 (urban population of 2500–19 999, adjacent to a metro area). No Maryland county is categorized as RUCC 4, 5, 7, 8, or 9, which are also among the least common RUCCs in the greater United States.
Of the original set of 6875 decedents, 257 resided outside Maryland but were found deceased within the state borders. We excluded these decedents from the analyses. We also excluded 267 decedents who had no recorded counties of residence, many of whom were likely from outside of Maryland, and 91 decedents who were of unknown race/ethnicity or who were listed as being from “other” race/ethnicity, to be able to examine and control for the 4 predominant racial/ethnic groups in Maryland (i.e., non-Hispanic White, African American, Hispanic, and Asian). We also excluded another 9 decedents with missing age data. As the combined number of decedents missing information on either age or race/ethnicity added up to less 2% of the cohort, we conducted the analyses after “listwise” deletion of cases with missing data.
We further limited the sample of suicide to those aged 15 years and older as there were only 55 suicide decedents younger than 15 years in the sample. Ages were binned into census-congruent 10-year age bins starting at age 15 years, with the final bin consisting of anyone older than 85 years (Table 1). The final sample included 6196 Maryland resident decedents aged 15 years and older with full data on age, sex, race/ethnicity, and method of suicide.
TABLE 1—
Demographic Characteristics of Firearm and Nonfirearm Suicide Decedents: Maryland, 2003–2015
| Characteristic | Total Suicides, No. (%)a | Firearm Suicides, No. (%)b | Nonfirearm Suicides, No. (%)c |
| Sex | |||
| Male | 4930 (79.6) | 2633 (89.3) | 2297 (70.7) |
| Female | 1266 (20.4) | 314 (10.7) | 952 (29.3) |
| χ2 (df 1) = 330.49; P < .001 | |||
| Race/ethnicity | |||
| Non-Hispanic White | 4952 (79.9) | 2448 (83.1) | 2504 (77.1) |
| African American | 966 (15.6) | 445 (15.1) | 521 (16.0) |
| Hispanic | 130 (2.1) | 33 (1.1) | 97 (3.0) |
| Asian | 148 (2.4) | 21 (0.7) | 127 (3.9) |
| χ2 (df 3) = 99.56; P < .001 | |||
| Age, y | |||
| 15–24 | 774 (12.5) | 311 (10.6) | 463 (14.3) |
| 25–34 | 904 (14.6) | 361 (12.2) | 543 (16.7) |
| 35–44 | 1081 (17.4) | 436 (14.8) | 645 (19.9) |
| 45–54 | 1368 (22.1) | 601 (20.4) | 767 (23.6) |
| 55–64 | 961 (15.5) | 490 (16.6) | 471 (14.5) |
| 65–74 | 522 (8.4) | 328 (11.1) | 194 (6.0) |
| 75–84 | 408 (6.6) | 297 (10.1) | 111 (3.4) |
| ≥ 85 | 178 (2.9) | 123 (4.2) | 55 (1.7) |
| χ2 (df 7) = 258.48; P < .001 | |||
| County type (RUCC) | |||
| Metro area > 1 000 000 population (RUCC 1) | 5245 (84.7) | 2407 (81.7) | 2838 (87.3) |
| Metro area 250 000–1 000 000 population (RUCC 2) | 460 (7.4) | 250 (8.5) | 210 (6.5) |
| Metro area < 250 000 population (RUCC 3) | 273 (4.4) | 158 (5.4) | 115 (3.5) |
| Rural area (RUCC 6) | 218 (3.5) | 132 (4.5) | 86 (2.6) |
| χ2 (df 3) = 40.75; P < .001 |
Note. RUCC = Rural–Urban Continuum Code. Population included suicide decedents aged 15 years or older.
n = 6196.
n = 2947 (47.6%).
n = 3249 (52.4%).
To calculate rates of suicide within the population of Maryland and rate ratios across urban versus rural counties and sexes, we obtained denominator data on the population of the state for years 2006 to 2011, a time period in the middle of our study period, from the US Census Bureau online database (http://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml). Availability of geographic and demographic information in both the suicide data and the census data allowed us to compute overall incidence rates for suicide and for firearm and nonfirearm suicides according to the county of residence while adjusting for sex, age, and race/ethnicity.
Statistical Analyses
We undertook regression analysis to compute incidence rate ratios (IRRs), using suicide deaths as numerator and county population as denominator, and to compare them between the 4 categories of urbanicity. We tested the fit of a number of models to the data, including Poisson, zero-inflated Poisson, negative binomial, and zero-inflated negative binomial (Table A, available as a supplement to the online version of this article at http://www.ajph.org). According to the lowest Akaike information criterion and Bayesian information criterion, we chose the negative binomial model, accounting for overdispersion of the data. Three regression models were run, 1 each for total suicide rate, firearm suicide rate, and nonfirearm suicide rate. The models adjusted for potential confounding by sex, race/ethnicity, and age that were found to be associated with suicide rates in unadjusted analyses (Table B, available as a supplement to the online version of this article at http://www.ajph.org). Furthermore, we tested interaction terms between urbanicity and each of the other independent variables for all 3 outcomes (i.e., suicide overall, firearm suicide, and nonfirearm suicide) to assess whether the association of urbanicity with suicide and means of suicide is limited to or more pronounced in specific population groups or is uniform across these groups.
We considered using the availability of mental health providers as a covariate, as national rural deficits in access to care have been suspected as a contributor to elevated suicide rates in rural areas.19 However, we found no significant differences in mental health care provider availability across urban–rural counties of Maryland on the basis of the 2009 Health Professional Shortage Area codes as a measure of mental health care provider availability (χ2 = 6.78; df = 6; P = .342). These codes are calculated primarily by using per capita numbers of psychiatrists and other mental health professionals as well as mental health professionals in contiguous areas.
We calculated variance inflation factors for all independent variables in the models including indicator variables for urbanicity, race/ethnicity, age group, and sex. No variables demonstrated a variance inflation factor greater than 5, ruling out collinearity among predictors. The analyses focused on comparing RUCC category 1 counties, which were the most common in Maryland and represented the most urban settings, with RUCC category 6 counties, which represented the most rural counties present in the state and also the most common category of rural county in the United States by both population and county count. RUCC 1 counties will be referred to as urban and RUCC 6 counties will be referred to as rural. Categories 2 and 3 often consist of a mixture of urban and suburban populations. We conducted all analyses with Stata version 14.0 (StataCorp LP, College Station, TX).
RESULTS
The characteristics of suicide decedents overall and separately by firearm use are presented in Table 1. Consistent with national patterns, the majority of suicide decedents were male and non-Hispanic White. The most common age group was the group aged 45 to 54 years. These sex, racial/ethnic, and age patterns were more pronounced in firearm suicides compared with nonfirearm suicides: there was a larger proportion of men, non-Hispanic Whites, and those in the 45- to 54-year age range among the firearm suicides compared with nonfirearm suicides (Table 1).
The majority of the state population resides in metropolitan counties with populations greater than 1 million (RUCC category 1) and, as a result, the majority of both firearm and nonfirearm suicides occurred in these counties (Table 1). The distribution of firearm and nonfirearm suicides varied across the urban–rural spectrum (χ2 = 40.75; df = 3; P < .001), with firearm suicides being 53% more common than nonfirearm suicides in the most rural counties and being less common than nonfirearm suicides in the most urban counties.
In the analysis of the whole population of the state, suicide rates varied significantly across counties (χ2 = 12.42; df = 3; P < .001) and were lowest in the most urban counties compared with all other counties. We found the largest difference between the most urban and rural counties (IRR = 1.35; 95% confidence interval [CI] = 1.07, 1.71), indicating a 35% higher suicide rate in rural counties compared with the most urban counties.
We observed a similar pattern in regression analyses for firearm suicides. Suicide rates varied significantly across county types (χ2 = 13.93; df = 3; P = .003), with a 66% higher firearm suicide rate in the most rural compared with the most urban counties (IRR = 1.66; 95% CI = 1.20, 2.31). However, there were no significant differences in nonfirearm suicide rates between these counties (IRR = 1.05; 95% CI = 0.81, 1.37). State suicide rates in urban and rural counties are shown in Table C (available as a supplement to the online version of this article at http://www.ajph.org by clicking the “Reprints” link).
In the interaction analysis, we found a significant interaction between urbanicity and sex, with adjustment for race/ethnicity and age, in predicting the total suicide rates (χ2 = 8.79; df = 3; P = .032), but not in firearm or nonfirearm suicide rates. Men were more likely to complete suicides in rural counties compared with the most urban counties (IRR = 1.19; 95% CI = 1.01, 1.40), whereas women were less likely to complete suicide in rural compared with the most urban counties (IRR = 0.63; 95% CI = 0.43, 0.94). The adjusted and unadjusted suicide rates per 100 000 for each sex are shown in Table 2. There were no statistically significant interactions between urbanicity and race/ethnicity or urbanicity and age groups.
TABLE 2—
Incidence Rate Ratios of Firearm and Nonfirearm Suicide Across Urban–Rural Counties: Maryland, 2003–2015
| Total Suicides |
Firearm Suicides |
Nonfirearm Suicides |
||||
| County Type | Unadjusted IRR (95% CI) | Adjusteda IRR (95% CI) | Unadjusted IRR (95% CI) | Adjusteda IRR (95% CI) | Unadjusted IRR (95% CI) | Adjusteda IRR (95% CI) |
| Men | ||||||
| Metro area > 1 000 000 population (RUCC 1; Ref) | 1 | 1 | 1 | 1 | 1 | 1 |
| Metro area 250 000–1 000 000 population (RUCC 2) | 1.23 (1.00, 1.51) | 1.08 (0.93, 1.24) | 1.38 (1.04, 1.84) | 1.17 (0.97, 1.42) | 1.06 (0.84, 1.34) | 0.93 (0.76, 1.14) |
| Metro area < 250 000 population (RUCC 3) | 1.42 (1.08, 1.86) | 1.20 (1.00, 1.43) | 1.54 (1.06, 2.22) | 1.33 (1.06, 1.69) | 1.21 (0.89, 1.64) | 1.00 (0.77, 1.30) |
| Rural area (RUCC 6) | 1.50 (1.20, 1.87) | 1.19 (1.01, 1.40) | 1.75 (1.30, 2.37) | 1.36 (1.09, 1.69) | 1.17 (0.88, 1.56) | 0.97 (0.75, 1.26) |
| Women | ||||||
| Metro area > 1 000 000 population (RUCC 1; Ref) | 1 | 1 | 1 | 1 | 1 | 1 |
| Metro area 250 000–1 000 000 population (RUCC 2) | 1.33 (0.98, 1.79) | 1.17 (0.93, 1.46) | 1.51 (0.92, 2.48) | 1.2 (0.81, 1.84) | 1.30 (0.94, 1.80) | 1.15 (0.88, 1.50) |
| Metro area < 250 000 population (RUCC 3) | 1.30 (0.87, 1.96) | 1.01 (0.74, 1.38) | 1.51 (0.79, 2.89) | 1.19 (0.69, 2.04) | 1.24 (0.79, 1.95) | 0.96 (0.66, 1.39) |
| Rural area (RUCC 6) | 0.80 (0.52, 1.24) | 0.63 (0.43, 0.94) | 1.00 (0.47, 2.10) | 0.74 (0.36, 1.49) | 0.74 (0.45, 1.22) | 0.60 (0.37, 0.96) |
Note. CI = confidence interval; IRR = incident rate ratio; RUCC = Rural–Urban Continuum Code. Population included suicide decedents aged 15 years or older.
Adjusted analyses controlled for age and race/ethnicity.
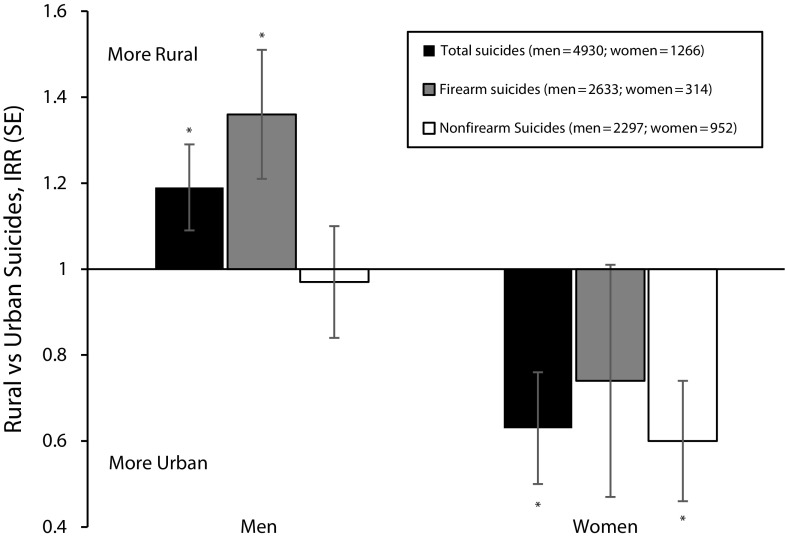
Because the association of urban–rural setting with suicide rate differed between men and women, we conducted all further analyses after stratifying the sample by sex and adjusting for race/ethnicity and age. The IRRs in comparisons of the rural to the most urban counties are shown for firearm, nonfirearm, and total suicides in Figure 1.
FIGURE 1—
Incidence Rate Ratios (IRR) for Suicide in Rural Counties (Rural–Urban Continuum Code 6) Compared With the Most Urban Counties (Rural–Urban Continuum Code 1): Maryland, 2003–2015
Note. The results are presented separately for men and women, adjusted for age and race/ethnicity.
*The IRR was significantly different from 1 at P < .05.
Among men, suicide by firearm was more common in the rural counties than in the most urban counties (IRR = 1.36; 95% CI = 1.10, 1.69), whereas there were no significant differences in the nonfirearm suicide rates across counties (IRR = 0.97; 95% CI = 0.75, 1.26).
Among women, there were no significant differences between firearm suicides in rural compared with the most urban counties (IRR = 0.74; 95% CI = 0.36, 1.49). However, just as with total female suicides, nonfirearm suicide was significantly less common in rural counties than in the most urban counties (IRR = 0.60; 95% CI = 0.37, 0.96).
DISCUSSION
We found that, although there is a higher suicide rate in rural Maryland counties than urban ones, this rate difference is limited to firearm suicides and does not exist when one is exclusively evaluating nonfirearm suicides. In the sex-stratified analysis, this pattern is seen to be driven by male decedents. Just as with the total sample, men in rural counties had a higher suicide risk than those in urban counties, and this higher rural risk is again limited to those who die by firearm. However, women in rural Maryland actually had a 37% lower rate of completed suicide than their urban counterparts. These opposite associations between urbanicity and suicide depending on sex may be driven by the male preference for firearms as a method for committing suicide.
The reasons for the higher prevalence of firearm suicides among men in rural areas remain elusive. Availability of firearms in rural areas may provide one possible explanation.20 We were unable, however, to control for firearm availability in each county. Indeed, little data are available on prevalence of firearm ownership and availability at the county level. Small national surveys have recently attempted this characterization,21 but state-specific data are not available. In the absence of such data, past studies have relied on the ratio of firearm suicides to total suicides to estimate firearm ownership in a region,22 but this may not be an appropriate proxy when the study outcome is itself suicide.
It has been suggested that increased suicide rates in rural areas may be the result of increased isolation, economic disparities, or decreased access to care.23,24 However, the findings from this study suggest that the impact of these contextual factors may be overshadowed by the differences in access to means of suicide, as the rural–urban rate difference was limited to firearm suicides. Maryland is relatively urbanized, with a lower proportion of rural population than the nation at large and a more truncated range of rurality. This limits the generalizability of this study to less densely populated states. However, our focus on Maryland demonstrates that the rural risk phenomenon is not limited to states with significant swathes of sparsely populated land, and is a problem for all states and that the study of rural risk factors like firearm use may be generalizable and contribute to a better understanding of the suicide risk factors even in the more densely populated states.
This study illustrates the important role of firearms in suicide mortality, especially in rural settings. Several interventions have shown preliminary successes in addressing firearm suicides, including laws regulating firearm access and exposure.25 Other interventions, such as encouraging safe storage,26 smart guns,27 and initiating safety campaigns in collaboration with firearm retailers and firearm advocates28 show great promise and warrant further study. Furthermore, patients with mental health problems in clinical settings are not often assessed for firearm access or safety practices.29 Further research is required to evaluate which firearm safety interventions are most acceptable and most likely to be used in rural populations, potentially including policies allowing for emergency transfer of firearms from at-risk patients.30
Limitations
The study had several limitations. First, data on suicide were drawn from medical examiner records and not psychological autopsies. However, as noted, Maryland is one of the few states to utilize exclusively appointed medical examiners, as opposed to elected coroners, who may not be forensic pathologists. As a result, Maryland possesses uniform death investigations and autopsies performed under a set of standardized operating procedures, which is not always the case in other states.
Second, the data are limited to 1 state and may not generalize to the whole country. This is particularly the case for the interaction between sex and rurality in suicide rates. In contrast to the Maryland findings, national data indicate higher rates of suicide among women in rural areas than urban.2 However, national data on suicides are limited. The National Vital Statistics and Centers for Disease Control and Prevention data sets, though much larger, contain reports of causes of death that may not have been informed by formal autopsy and detailed investigation.31
Third, there were relevant policy changes regarding firearm purchasing in the state of Maryland and the country that we did not examine in this study but that may affect firearm access and suicide rates.25,32 In Maryland, the pertinent change took place in late 2013, when the state passed a permit-to-purchase law that made the purchase of a new firearm somewhat more difficult statewide. Studies of similar permit laws in other states have shown them to affect suicide rates.25,32 The impact of these policies needs to be examined in future research. We also did not examine the potential impact of more recent surges in national suicide rates. There is some evidence that the recent surge has been more pronounced in rural than urban settings.2
Fourth, past studies examining the association of urbanicity with suicide adjusted for various countywide factors such as per capita income, employment, percentage of persons living alone, marriage rate, average education, prevalence of substance abuse, or availability of mental health care.7,24 We did not adjust for these characteristics because many of these contextual factors are assessed at county level and the number of counties in our study was quite limited, resulting in limited range of the variables. Furthermore, fewer cross-correlated covariates produce more easily interpretable results.33 Future studies should examine the possible relevance of these important contextual factors to firearms accessibility and firearm suicides in studies involving a larger number of counties.
Fifth, we did not have access to Maryland county-level suicide attempt rates. Other studies have reported higher suicide attempt rates in rural versus urban areas for both adults34 and adolescents.35 Future studies including data on suicide attempts may further elucidate urban–rural differences in firearm suicides.
In the context of these limitations, the results of the study shed light on the long-observed urban–rural variations in suicide in the United States by highlighting the role of firearms in the increased rural rates. The study provides more recent data on suicide rates and means of suicide than any previously published studies and examines risk factors in Maryland, a state that has not been studied in this way in the past and represents a more representative set of rural–urban spectra. If corroborated in future studies from other states and national studies, the results suggest that efforts to mitigate risk of suicide completion among at-risk male individuals living in rural areas with easy access to high lethality means for suicide should be explored. Curbing the growing trend in suicide rates in the country would probably require a multidisciplinary approach involving greater collaboration among policymakers, public health practitioners, and mental health providers.
Public Health Implications
Ranking as the 10th leading cause of death in the United States, with an estimated annual cost of more than $50 billion annually, suicide remains a pressing public health problem. The risk for suicide is higher in rural than urban settings. Our findings suggest that the higher rural suicide rates are driven by firearm suicides in men. The findings also highlight the potential benefits of more robust rural firearm safety and control initiatives on decreasing the rural suicide rates.
ACKNOWLEDGMENTS
The study was supported by MCIC Risk Reduction grant JHM-152 to P. S. Nestadt and P. Triplett, as well as a National Institute of Mental Health T32 MH014592-40 training grant to P. S. Nestadt. R. Mojtabai receives financial support as an author for UpToDate.com.
HUMAN PARTICIPANT PROTECTION
The study was approved by the Johns Hopkins School of Medicine institutional review board.
Footnotes
REFERENCES
- 1.Curtin SC, Warner M, Hedegaard H. Increase in suicide in the United States, 1999–2014. NCHS Data Brief. 2016;(241):1–8. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Web-Based Injury Statistics Query and Reporting System (WISQARS). Fatal injury reports. 2017. Available at: http://www.cdc.gov/injury/wisqars/fatal_injury_reports.html. Accessed March 30, 2017.
- 3.Peen J, Schoevers RA, Beekman AT, Dekker J. The current status of urban–rural differences in psychiatric disorders. Acta Psychiatr Scand. 2010;121(2):84–93. doi: 10.1111/j.1600-0447.2009.01438.x. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication [erratum: Arch Gen Psychiatry. 2005;62(7):709] Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spicer RS, Miller TR. Suicide acts in 8 states: incidence and case fatality rates by demographics and method. Am J Public Health. 2000;90(12):1885–1891. doi: 10.2105/ajph.90.12.1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nordstrom DL, Zwerling C, Stromquist AM, Burmeister LF, Merchant JA. Rural population survey of behavioral and demographic risk factors for loaded firearms. Inj Prev. 2001;7(2):112–116. doi: 10.1136/ip.7.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Branas CC, Nance ML, Elliott MR, Richmond TS, Schwab CW. Urban–rural shifts in intentional firearm death: different causes, same results. Am J Public Health. 2004;94(10):1750–1755. doi: 10.2105/ajph.94.10.1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCarthy JF, Blow FC, Ignacio RV, Ilgen MA, Austin KL, Valenstein M. Suicide among patients in the Veterans Affairs health system: rural–urban differences in rates, risks, and methods. Am J Public Health. 2012;102(suppl 1):S111–S117. doi: 10.2105/AJPH.2011.300463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Judd F, Cooper A, Fraser C, Davis J. Rural suicide—people or place effects? Aust N Z J Psychiatry. 2006;40(3):208–216. doi: 10.1080/j.1440-1614.2006.01776.x. [DOI] [PubMed] [Google Scholar]
- 10.Klieve H, Sveticic J, De Leo D. Who uses firearms as a means of suicide? A population study exploring firearm accessibility and method choice. BMC Med. 2009;7:52. doi: 10.1186/1741-7015-7-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ngamini Ngui A, Apparicio P, Moltchanova E, Vasiliadis H. Spatial analysis of suicide mortality in Québec: spatial clustering and area factor correlates. Psychiatry Res. 2014;220(1-2):20–30. doi: 10.1016/j.psychres.2014.07.033. [DOI] [PubMed] [Google Scholar]
- 12.Alston M. Rural male suicide in Australia. Soc Sci Med. 2012;74(4):515–522. doi: 10.1016/j.socscimed.2010.04.036. [DOI] [PubMed] [Google Scholar]
- 13.Bustamante F, Ramirez V, Urquidi C, Bustos V, Yaseen Z, Galynker I. Trends and most frequent methods of suicide in Chile between 2001 and 2010. Crisis. 2016;37(1):21–30. doi: 10.1027/0227-5910/a000357. [DOI] [PubMed] [Google Scholar]
- 14.Davies MJ, Wells C, Squires PA, Hodgetts TJ, Lecky FE. Civilian firearm injury and death in England and Wales. Emerg Med J. 2012;29(1):10–14. doi: 10.1136/emj.2009.085837. [DOI] [PubMed] [Google Scholar]
- 15.Payne-James J, Busuttil A, Smock W. Forensic Medicine: Clinical and Pathological Aspects. Cambridge, England: Cambridge University Press; 2003. [Google Scholar]
- 16.Kapusta ND, Tran US, Rockett IR et al. Declining autopsy rates and suicide misclassification: a cross-national analysis of 35 countries. Arch Gen Psychiatry. 2011;68(10):1050–1057. doi: 10.1001/archgenpsychiatry.2011.66. [DOI] [PubMed] [Google Scholar]
- 17.Timmermans S. Suicide determination and the professional authority of medical examiners. Am Sociol Rev. 2005;70(2):311–333. [Google Scholar]
- 18.National Research Council. Strengthening Forensic Science in the United States: A Path Forward. Washington, DC: The National Academies Press; 2009. [Google Scholar]
- 19.Searles VB, Valley MA, Hedegaard H, Betz ME. Suicides in urban and rural counties in the United States, 2006–2008. Crisis. 2014;35(1):18–26. doi: 10.1027/0227-5910/a000224. [DOI] [PubMed] [Google Scholar]
- 20.Siegel M, Rothman EF. Firearm ownership and suicide rates among US men and women, 1981–2013. Am J Public Health. 2016;106(7):1316–1322. doi: 10.2105/AJPH.2016.303182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pew Research Center. The demographics and politics of gun-owning households. 2014. Available at: http://www.pewresearch.org/fact-tank/2014/07/15/the-demographics-and-politics-of-gun-owning-households. Accessed April 12, 2017.
- 22.Azrael D, Cook PJ, Miller M. State and local prevalence of firearms ownership measurement, structure, and trends. J Quant Criminol. 2004;20(1):43–62. [Google Scholar]
- 23.Hirsch JK. A review of the literature on rural suicide. Crisis. 2006;27(4):189–199. doi: 10.1027/0227-5910.27.4.189. [DOI] [PubMed] [Google Scholar]
- 24.Fontanella CA, Hiance-Steelesmith DL, Phillips GS et al. Widening rural–urban disparities in youth suicides, United States, 1996–2010. JAMA Pediatr. 2015;169(5):466–473. doi: 10.1001/jamapediatrics.2014.3561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anestis MD, Anestis JC. Suicide rates and state laws regulating access and exposure to handguns. Am J Public Health. 2015;105(10):2049–2058. doi: 10.2105/AJPH.2015.302753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grossman DC, Mueller BA, Riedy C et al. Gun storage practices and risk of youth suicide and unintentional firearm injuries. JAMA. 2005;293(6):707–714. doi: 10.1001/jama.293.6.707. [DOI] [PubMed] [Google Scholar]
- 27.Mann JJ, Michel CA. Prevention of firearm suicide in the United States: what works and what is possible. Am J Psychiatry. 2016;173(10):969–979. doi: 10.1176/appi.ajp.2016.16010069. [DOI] [PubMed] [Google Scholar]
- 28.Vriniotis M, Barber C, Frank E, Demicco R. New Hampshire Firearm Safety Coalition. A suicide prevention campaign for firearm dealers in New Hampshire. Suicide Life Threat Behav. 2015;45(2):157–163. doi: 10.1111/sltb.12123. [DOI] [PubMed] [Google Scholar]
- 29.Betz ME, Miller M, Barber C et al. Lethal means access and assessment among suicidal emergency department patients. Depress Anxiety. 2016;33(6):502–511. doi: 10.1002/da.22486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCourt AD, Vernick JS, Betz ME, Brandspigel S, Runyan CW. Temporary transfer of firearms from the home to prevent suicide: legal obstacles and recommendations. JAMA Intern Med. 2017;177(1):96–101. doi: 10.1001/jamainternmed.2016.5704. [DOI] [PubMed] [Google Scholar]
- 31.Garlow SJ, Purselle D, Heninger M. Ethnic differences in patterns of suicide across the life cycle. Am J Psychiatry. 2005;162(2):319–323. doi: 10.1176/appi.ajp.162.2.319. [DOI] [PubMed] [Google Scholar]
- 32.Crifasi CK, Meyers JS, Vernick JS, Webster DW. Effects of changes in permit-to-purchase handgun laws in Connecticut and Missouri on suicide rates. Prev Med. 2015;79:43–49. doi: 10.1016/j.ypmed.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 33.Kraemer HC. A source of false findings in published research studies. JAMA Psychiatry. 2015;72(10):961–962. doi: 10.1001/jamapsychiatry.2015.1178. [DOI] [PubMed] [Google Scholar]
- 34.Rost K, Zhang M, Fortney J, Smith J, Smith GR., Jr Rural–urban differences in depression treatment and suicidality. Med Care. 1998;36(7):1098–1107. doi: 10.1097/00005650-199807000-00015. [DOI] [PubMed] [Google Scholar]
- 35.Forrest S. Suicide and the rural adolescent. Adolescence. 1988;23(90):341–347. [PubMed] [Google Scholar]